Abstract
Background
A year after the start of the COVID-19 outbreak, the global rollout of vaccines gives us hope of ending the pandemic. Lack of vaccine confidence, however, poses a threat to vaccination campaigns. This study aims at identifying individuals’ characteristics that explain vaccine willingness in Flanders (Belgium), while also describing trends over time (July–December 2020).
Methods
The analysis included data of 10 survey waves of the Great Corona Survey, a large-scale online survey that was open to the general public and had 17,722–32,219 respondents per wave. Uni- and multivariable general additive models were fitted to associate vaccine willingness with socio-demographic and behavioral variables, while correcting for temporal and geographical variability.
Results
We found 84.2% of the respondents willing to be vaccinated, i.e., respondents answering that they were definitely (61.2%) or probably (23.0%) willing to get a COVID-19 vaccine, while 9.8% indicated maybe, 3.9% probably not and 2.2% definitely not. In Flanders, vaccine willingness was highest in July 2020 (90.0%), decreased over the summer period to 80.2% and started to increase again from late September, reaching 85.9% at the end of December 2020. Vaccine willingness was significantly associated with respondents’ characteristics: previous survey participation, age, gender, province, educational attainment, household size, financial situation, employment sector, underlying medical conditions, mental well-being, government trust, knowing someone with severe COVID-19 symptoms and compliance with restrictive measures. These variables could explain much, but not all, variation in vaccine willingness.
Conclusions
Both the timing and location of data collection influence vaccine willingness results, emphasizing that comparing data from different regions, countries and/or timepoints should be done with caution. To maximize COVID-19 vaccination coverage, vaccination campaigns should focus on (a combination of) subpopulations: aged 31–50, females, low educational attainment, large households, difficult financial situation, low mental well-being and labourers, unemployed and self-employed citizens.
Keywords: Vaccine willingness, Vaccine hesitancy, Trust, COVID-19, Socio-demographics, Online survey
Abbreviations: BIC, Bayesian Information Criterion; CI, confidence interval; EMA, European Medicines Agency; GLM, Generalized linear model; HCW, healthcare worker; GAM, generalized additive model; MMR, Measles Mumps Rubella; NPI, non-pharmaceutical intervention; NS, not selected; OR, odds ratio; REF, reference model; UK, United Kingdom; WHO, World Health Organisation
1. Introduction
The COVID-19 pandemic has exerted exceptional pressure on healthcare systems on a global scale, forcing policymakers to take highly restrictive measures [1]. Such measures aim to balance between safeguarding public health, protecting individuals’ well-being and preventing healthcare systems from collapsing on the one hand, while carefully considering the economic and social impact on the other hand. Even though non-pharmaceutical interventions (NPIs), such as social distancing and mask wearing, have proven useful in reducing the pressure on healthcare systems in the short run, COVID-19 vaccines are considered as the most important and sustainable strategy to control the pandemic in the long run [2]. Indeed, with the COVID-19 pandemic rapidly evolving and the majority of countries in a severe state of crisis, vaccine rollout should enable governments to slowly reverse NPIs.
As of 10 February 2021, 242 vaccines are under development worldwide, of which 63 in clinical stages [3], [4]. While some vaccines are being developed using more traditional platforms (e.g. inactivated virus or live-attenuated virus), the majority of COVID-19 vaccines are being developed using more innovative platforms, such as adenovirus-based, RNA- or DNA-based vaccines [3]. In order to speed up vaccine development, regulators have facilitated a fast-track procedure, while ensuring that safety, quality and efficacy standards are still being met [5], [6]. In addition, an emergency use listing procedure was initiated to speed up vaccine rollout during a public health emergency [7]. The European Commission has been coordinating negotiations with vaccine manufacturers securing a portfolio of, to date, more than 2 billion COVID-19 vaccines, in anticipation of further approvals by the European Medicines Agency (EMA) [8]. The EMA currently only granted approval for three vaccines: one developed by BioNTech-Pfizer (21 December 2020), one by Moderna (6 January 2021) and another by AstraZeneca (29 January 2021). Large-scale vaccination has become an integral part of the governments’ strategies to control the COVID-19 pandemic. Vaccination campaigns have started early January 2021 in most European countries, applying a variety of prioritisation schemes, mainly focussing on people most at risk for severe illness as well as healthcare workers (HCWs) [9].
Meanwhile, COVID-19 vaccine hesitancy has taken root in society. Vaccine hesitancy is defined by the World Health Organisation (WHO) as “a delay in acceptance or refusal of vaccination despite availability of vaccination services” [10]. Vaccine hesitancy is complex and context specific, varying across time, place and vaccines. Recent studies have shown that a significant proportion of the world population is reluctant to take a COVID-19 vaccine, with reluctance often detected among specific (sub-)populations [11], including HCWs [12]. More specifically, such studies describe widespread – though unfounded – concerns with respect to vaccines’ safety and are mostly centred around the speed at which vaccines are being developed, about ‘unknown’ long-term side-effects and fear about the innovative platforms being used [13], [14], [15], [16]. Having emerged for a variety of vaccines, such as the measles, mumps, rubella (MMR) and whole-cell pertussis vaccine [17], [18], vaccine hesitancy is not a new obstacle policymakers are facing [19]. Indeed, the WHO described vaccine hesitancy as one of the 10 most important threats to global health in 2019 [20]. However, the spread of misinformation and the development of anti-vaccine communities has been highly facilitated by the widespread use of social media [19]. Strategies for addressing vaccine hesitancy show different rates of success in increasing vaccination coverage, yet multicomponent strategies, as well as dialogue-based interventions were found to be the most effective [reviewed in [21], [22]].
A discrete-choice experiment in Flanders, Belgium found that the decision to vaccinate is a multi-factorial one, mostly influenced by individuals’ perception about vaccine related side-effects followed by the vaccine’s accessibility, effectiveness as well as the vaccine-preventable disease burden [23]. In addition, trust is important, and in the case of vaccine hesitancy, the lack thereof [24]. Vaccine-related trust depends, in turn, on a balance between product trust (the vaccine), political or system trust (the health system) and provider trust (e.g., HCW administering the vaccine) [24]. The vast majority of people believe their HCW to be the most trusted source of information [25]. In agreement, the Wellcome Global Monitor [26] states that 73% of people worldwide would trust a doctor or nurse above any other source of health advice, including family, friends, religious leaders or famous people. In the current COVID-19 crisis, governments and experts act as an important source of information and both play a central role in defining the crisis management and prevention strategies, including vaccination. Furthermore, a recent study in Belgium found trust in the government to be positively associated with vaccine willingness [27]. In addition to building government trust, HCWs are pivotal in achieving sufficient vaccination coverage and they are thus essential for the success of the COVID-19 vaccination campaign.
The willingness to be vaccinated can vary over time, which is acknowledged by the WHO Global Advisory Committee on Vaccine Safety [28]. Since vaccine willingness is influenced by external factors and can change in light of developments over time, researchers and policymakers should not draw permanent conclusions based on a cross-sectional observation [29].
A high vaccination coverage is essential to reduce the burden of COVID-19 on healthcare systems, the economy and society as a whole and to control viral transmission. In light of the COVID-19 vaccination campaign in Belgium, this study aims to characterise factors that explain the willingness to be vaccinated in Flanders. Furthermore, this paper describes trend data on vaccine willingness (July 2020–December 2020), while also mapping the slope of the COVID-19 related hospitalization curve, the sequence of governmental measures (NPIs) and impactful media reporting on vaccines to the vaccine willingness curve.
2. Material and methods
2.1. Survey design
We used data from a citizen science project called the ‘Great Corona Survey’ [30], an ethically approved (EC 20/13/146), modular, online survey, hosted by the University of Antwerp, in collaboration with Hasselt University and KU Leuven, which has been repeated over 27 waves since 17th March 2020 (every week until 5th May, every other week thereafter). The survey is based on anonymous self-reporting and open to the general population. The study seeks to monitor the general public’s attitudes on and adherence to measures against COVID-19 transmission, their mental health, and their opinion on a wide range of Corona-related topics.
2.2. Data
Belgium has three official regions: 1) Flanders, the northern half of Belgium (5,4 million adults > 17 years) , 2) Wallonia, the southern half of Belgium (2,9 million adults) and 3) the Brussels capital region (945,000 adults). Furthermore, Belgium has three official communities: the Flemish community (Dutch), the French community (French) and the German-speaking community (German). The survey was presented in the 3 official country languages and in English. Preventive healthcare authorities, including the vaccination campaign, are governed at the level of the communities/regions in Belgium. We included data from all ten waves between July 2020 and December 2020 that included a vaccination module1 , which assessed the willingness to be vaccinated against COVID-19. Although participation rates per wave were high, during the ten waves used here, there was a substantial underrepresentation of youngsters under 18 years and participants that live in French and German speaking communities of Belgium. We therefore restricted our analysis to adults (equal to and over 18 years old) living in Flanders, Belgium’s Dutch speaking northern part that excludes Brussels (selection based on postal code and language). This resulted in 230,979 data records.
In each of the selected surveys, participants were asked whether they would be willing to be vaccinated with an effective and safe COVID-19 vaccine, that is recommended for their age group, available free of charge and administered in their home town. Response options were “definitely”, “probably”, “maybe”, “probably not” and “definitely not”. Following [11], we dichotomised the outcome into a binary response variable, “vaccine willingness”, which distinguishes between “willing” (“definitely” and “probably”) and “less or not willing” (“maybe,” “probably not”, and “definitely not”) to be vaccinated. Participants who expressed doubts with regards to being vaccinated, were presented a list of ten potential reasons for being vaccine hesitant and were asked to indicate which of those reasons were important for their decision not to accept the vaccine.
In this study, we linked this response variable to a set of explanatory variables: date of participation, previous participation, age, gender, residential location (province), educational attainment, household size, household composition, financial situation, employment sector, underlying medical conditions (indicator variables for heart condition, lung condition, kidney disease, diabetes, high blood pressure, immune suppression and recent cancer diagnosis), mental well-being (quantified by the General Health Questionnaire-12 [31]; a score between 0 and 12 with higher scores indicating more mental distress), government trust, and boolean variables indicating whether the participant knew someone with severe COVID-19 symptoms, whether the respondent had installed the Coronalert mobile app [32], had physical contacts outside their household (social distancing adherence) and whether participants with at least one underaged child (<18 years old) were willing to vaccinate their underaged children. The Coronalert app is an information & alert app that informs you when you have been in close contact with someone who tested positive and its use is recommended by the Flemish government [32]. Detailed variable descriptions are provided in Table 1, Table 2, Table 3 .
Table 1.
Description of participants’ characteristics across all waves and results of the multivariable analysis. Odds ratios are presented for all variables that were part of the final model after variable selection. The effect of “Participation in previous rounds” interacted with the gender and time effect, the latter of which is depicted in Fig. 2. “Province” was not taken up in the model; instead, we used a two-dimensional spline to assess the spatial effect (Fig. 3). “Household composition” was removed from the model during backwards model selection. For “COVID-19 vaccine willingness”, unweighted and weighted percentages are shown, “(unweighted/weighted)”. Note that percentages may not sum exactly to 100% due to rounding.
| Participants (%) | Vaccine willingness % unweighted/weighted |
Vaccine willingness OR (95% CI) | ||
|---|---|---|---|---|
| Participation date | ||||
| July 14 | 24,756 (10.7) | 89.2/89.9 | REF | |
| July 28 | 32,219 (13.9) | 89.3/90.0 | 0.96 (0.84–1.11) | |
| August 25 | 22,788 (9.9) | 80.7/82.6 | 0.47 (0.42–0.53) | |
| September 08 | 20,490 (8.9) | 78.1/80.7 | 0.40 (0.36–0.45) | |
| September 22 | 17,722 (7.7) | 77.7/80.2 | 0.38 (0.34–0.43) | |
| November 03 | 22,953 (9.9) | 81.8/83.1 | 0.49 (0.44–0.56) | |
| November 17 | 23,902 (10.3) | 82.1/83.1 | 0.47 (0.41–0.53) | |
| December 01 | 20,813 (9.0) | 81.0/81.7 | 0.43 (0.38–0.48) | |
| December 15 | 19,953 (8.6) | 83.1/83.9 | 0.44 (0.39–0.50) | |
| December 29 | 25,383 (11.0) | 85.1/85.9 | 0.48 (0.42–0.55) | |
| Participation in previous waves | ||||
| Every wave | 59,901 (25.9) | 85.3/86.1 | ||
| A few waves/often | 159,621 (69.1) | 82.9/84.0 | Fig. 2 | |
| Once | 5,549 (2.4) | 79.7/79.6 | ||
| No | 5,908 (2.6) | 78.0/76.5 | ||
| Gender | ||||
| Female | 159,449 (69.0) | 80.9/81.0 | ||
| Male | 71,530 (31.0) | 88.8/87.3 | ||
| (Gender, Participation in previous waves) | ||||
| (Female, every wave) | 42,376 (18.3) | 82.8/82.3 | REF | |
| (Male, every wave) | 17,525 (7.6) | 91.5/90.7 | 2.10 (1.99–2.22) | |
| (Female, a few waves/often) | 110,844 (48.0) | 80.4/80.9 | REF | |
| (Male, a few waves/often) | 48,777 (21.1) | 88.6/87.2 | 1.64 (1.59–1.69) | |
| (Female, once) | 3,238 (1.4) | 76.5/75.3 | REF | |
| (Male, once) | 2,311 (1.0) | 84.1/82.0 | 1.60 (1.41–1.81) | |
| (Female, No) | 2,991 (1.3) | 74.9/74.3 | REF | |
| (Male, No) | 2,917 (1.3) | 81.1/77.4 | 1.27 (1.12–1.43) | |
| Age | ||||
| 18–30 | 21,762 (9.4) | 81.7/82.4 | REF | |
| 31–50 | 77,798 (33.7) | 78.4/79.0 | 0.93 (0.89–0.96) | |
| 51–70 | 113,766 (49.3) | 85.7/86.5 | 1.36 (1.30–1.42) | |
| 71+ | 17,653 (7.6) | 91.8/91.2 | 1.80 (1.69–1.92) | |
| Province | ||||
| Antwerp | 113,218 (49.0) | 83.4/84.3 | ||
| East Flanders | 39,999 (17.3) | 83.3/84.3 | ||
| Flemish Brabant | 34,438 (14.9) | 84.9/85.8 | Fig. 3 | |
| Limburg | 20,389 (8.8) | 81.4/82.4 | ||
| West Flanders | 22,935 (9.9) | 82.3/83.4 | ||
| Educational attainment | ||||
| Primary education | 2,870 (1.2) | 79.8/80.7 | 0.62 (0.56–0.68) | |
| Secondary education | 62,423 (27.0) | 80.2/80.8 | 0.72 (0.70–0.74) | |
| Higher education | 158,370 (68.6) | 84.3/85.0 | REF | |
| PhD | 7,316 (3.2) | 90.7/91.3 | 1.54 (1.42–1.66) | |
| Family size | ||||
| Single | 43,790 (19.0) | 81.6/83.0 | REF | |
| Two persons | 95,104 (41.2) | 86.7/87.4 | 1.20 (1.16–1.24) | |
| 3–5 persons | 87,013 (37.7) | 80.9/81.5 | 1.14 (1.10–1.17) | |
| 5 + persons | 5,072 (2.2) | 76.5/77.2 | 0.89 (0.82–0.95) | |
| Family composition | ||||
| Children age 12 or lower | 37,743 (16.3) | 78.2/78.7 | NS | |
| Children age 13 or higher | 31,402 (13.6) | 78.6/79.0 | NS | |
| Elderly above 70 | 21,778 (9.4) | 89.1/90.2 | NS | |
| Financial situation | ||||
| Very easy | 52,932 (22.9) | 89.0/89.3 | REF | |
| Easy | 89,584 (38.8) | 85.5/86.0 | 0.80 (0.77–0.82) | |
| Somewhat easy | 64,433 (27.9) | 80.2/81.4 | 0.62 (0.60–0.65) | |
| Somewhat difficult | 20,459 (8.9) | 72.5/73.2 | 0.43 (0.41–0.45) | |
| Difficult | 3,571 (1.5) | 62.8/61.5 | 0.27 (0.25–0.29) | |
| Employment statute/sector | ||||
| Employee/official | 79,718 (34.5) | 82.2/82.5 | REF | |
| Student | 7,087 (3.1) | 83.4/84.4 | 1.35 (1.27–1.43) | |
| Labourer | 4,692 (2.0) | 70.9/69.2 | 0.62 (0.58–0.66) | |
| Education | 18,946 (8.2) | 83.2/83.9 | 1.07 (1.02–1.12) | |
| Health worker | 13,634 (5.9) | 80.9/80.9 | 1.05 (1.00–1.11) | |
| Self-employed | 11,339 (4.9) | 78.5/79.4 | 0.78 (0.74–0.83) | |
| Unemployed | 22,646 (9.8) | 76.8/76.8 | 0.86 (0.83–0.90) | |
| Retired | 66,194 (28.7) | 89.6/90.4 | 1.36 (1.30–1.43) | |
| Other | 6,723 (2.9) | 78.2/79.9 | 0.95 (0.89–1.01) | |
| Know someone with severe COVID-19 symptoms | ||||
| Yes | 132,953 (57.6) | 83.9/84.8 | 1.18 (1.16–1.21) | |
| No | 98,026 (42.4) | 82.5/83.2 | REF | |
| Underlying medical conditions | ||||
| Heart condition | 11,438 (5.0) | 88.9/89.0 | 1.04 (0.98–1.11) | |
| Lung condition | 12,817 (5.5) | 87.0/87.3 | 1.34 (1.27–1.42) | |
| Kidney disease | 2,521 (1.1) | 85.5/86.6 | 0.97 (0.87–1.10) | |
| Diabetes | 9,550 (4.1) | 89.7/90.8 | 1.43 (1.33–1.53) | |
| High blood pressure | 35,724 (15.5) | 88.0/88.7 | 1.22 (1.18–1.27) | |
| Immune suppression | 8,889 (3.8) | 83.4/84.7 | 1.25 (1.17–1.34) | |
| Recent cancer diagnosis | 3,231 (1.4) | 87.5/89.1 | 1.27 (1.13–1.42) | |
| COVID-19 vaccine willingness | ||||
| Definitely | 137,851 (59.7/61.2) | |||
| Probably | 54,609 (23.6/23.0) | |||
| Maybe | 24,293 (10.5/9.8) | |||
| Probably not | 9,109 (3.9/3.9) | |||
| Definitely not | 5,117 (2.2/2.2) | |||
OR: odds ratio, CI: confidence interval, NS: not selected, REF: reference level.
Table 2.
Reported reasons for hesitating to accept a COVID-19 vaccine. Each participant could select multiple reasons. The percentages are computed conditional on the respondent being vaccine hesitant.
| Reason for being vaccine hesitant | weightedpercentage |
|---|---|
| I don't think the safety of COVID-19 vaccines can be guaranteed sufficiently | 61.0 |
| I don't think the vaccine is good because it has been developed too quickly | 54.0 |
| I'd like to wait until enough other people have been vaccinated before I get the vaccine myself | 45.9 |
| It depends exactly which COVID-19 vaccine I am offered | 28.4 |
| I can't find any reliable information about vaccines | 26.6 |
| I'd like to wait until enough other people have been vaccinated so that I don't have to be vaccinated myself | 14.0 |
| I don't think COVID-19 is serious enough | 8.0 |
| I think I'm allergic to a COVID-19 vaccine | 5.1 |
| I'm against all forms of vaccination | 3.1 |
| I don't think I need a COVID-19 vaccine because I've already had COVID-19 | 2.6 |
Table 3.
Behaviour-related outcomes and their influence on vaccine willingness. Odds ratios relate to the effect of these behaviour-related outcomes in a multivariate logistic GLM of vaccination willingness towards one behaviour-related outcome and the main confounders: date of participation, age, gender and educational attainment. This table only contains the odds ratios for the behaviour-related outcome; full model results are available in the Supplementary material.
| Participants (%) | Vaccine willingness % unweighted/weighted |
Vaccine willingness OR (95% CI) | ||
|---|---|---|---|---|
| Installation Coronalert app* | ||||
| Installed | 41,057 (60.7) | 87.7/88.6 | REF | |
| Not installed | 26,611 (39.3) | 72.4/73.2 | 0.33 (0.32–0.35) | |
| Physical contact outside household last week | ||||
| No | 180,091 (78.0) | 84.6/85.6 | REF | |
| Yes | 50,888 (22.0) | 78.7/79.1 | 0.66 (0.64–0.68) | |
| Government trust* | ||||
| 7 Trust completely | 2,529 (5.9) | 93.8/94.5 | REF | |
| 6 | 8,038 (18.8) | 90.8/91.5 | 0.67 (0.56–0.80) | |
| 5 | 8,972 (21.0) | 87.6/88.8 | 0.51 (0.43–0.61) | |
| 4 | 7,574 (17.7) | 82.3/84.4 | 0.36 (0.30–0.43) | |
| 3 | 5,457 (12.8) | 77.9/79.8 | 0.25 (0.21–0.30) | |
| 2 | 4,776 (11.2) | 73.3/74.5 | 0.17 (0.15–0.21) | |
| 1 do not trust at all | 4,617 (10.8) | 62.1/64.5 | 0.10 (0.08–0.12) | |
| No opinion | 721 (1.7) | 75.3/78.4 | 0.28 (0.22–0.35) | |
| GHQ-12 mental well-being score | ||||
| 0 | 112,953 (48.9) | 85.0/85.7 | REF | |
| 1–4 | 59,501 (25.8) | 83.9/84.6 | 0.97 (0.94–1.00) | |
| 5–8 | 28,609 (12.4) | 81.6/82.6 | 0.88 (0.85–0.91) | |
| 9–12 | 29,916 (13.0) | 77.5/78.8 | 0.70 (0.68–0.73) | |
| Vaccine willingness child** | ||||
| Willing | 30,607 (77.5) | 97.4/97.5 | REF | |
| Not willing | 8,867 (22.5) | 24.1/23.9 | 0.01 (0.01–0.01) | |
* Coronalert app and governmental trust questions were not present in all of the ten survey waves analysed, hence the lower total participant count on these questions. ** Question only presented to participants with children aged below 18. OR: odds ratio, CI: confidence interval.
2.3. Statistical analysis
We calculated summary statistics for all variables and improved representativeness using inverse probability weighting based on participation date, age, gender and province. We mapped the weighted sample-based proportion of willingness to be vaccinated over time against a series of governmental decisions on NPI regulation and other impactful news, as well as a curve representing the number of new COVID-19 related hospitalizations.
Next, in Analysis 1, we fitted a cross-sectional multi-variable logistic generalized additive model (GAM), where we investigated the association between a participant’s willingness to be vaccinated and their participation behaviour in the ‘Great Corona Survey’; their demographic characteristics, i.e. variables age, gender, educational attainment, household size, household composition, financial situation and employment sector; their residential location, i.e. longitude-latitude coordinates of the centre of the postal code of a participant’s place of residence; whether the participant knew someone with severe COVID-19 symptoms; underlying medical conditions; and time, which is represented by the wave ID. The spatial effect was modelled by estimating a smooth two-dimensional spline and was validated through a sensitivity analysis in which a spatially-discrete geostatistical logistic model [33] was fitted. The main purpose of Analysis 1 was to attribute variation in vaccine willingness to multiple characteristics of participants that can be targeted in policy making. Note that we implemented a cross-sectional, instead of a longitudinal, analysis approach, because records of returning individuals could not be linked throughout multiple waves. Since within-subject correlation induced by returning participants cannot be taken into account, the widths of the covariate effects’ confidence intervals are likely underestimated; we have taken this into account in the interpretation of our results. Interaction effects between time and all other explanatory variables were included; backwards model selection using the Bayesian Information Criterion (BIC) was applied to propose a final model.
In Analysis 2, we investigated the association between vaccine willingness and five variables that only allowed a limited scope for identifying target groups for policy interventions, as compared to those included in Analysis 1: “government trust”, “mental well-being”, “social distancing adherence”, an indicator whether a participant “had installed the Coronalert app”, and the participant’s “willingness to vaccinate their children”. Despite the limited opportunities to pinpointing target groups, this analysis can increase the understanding of the profiles of those willing to get vaccinated. We fitted five separate models, using multi-variable logistic generalized linear models (GLMs), while correcting for basic confounding factors: date of participation, age, gender, and educational attainment. We avoided including the five variables jointly in one linear predictor because of complex, not well-understood, causal interrelations.
Model parametrisations are presented in the Supplementary material.
3. Results
3.1. Participant characteristics
Table 1 lists participant characteristics across all waves. Participation rates of profiles meeting the selection criteria per wave were high with counts varying from 17,722 to 32,219 per survey. People aged 51–70 (49.3%), females (69.0%) and those living in the province of Antwerp (49.0%) are strongly represented in our survey, whereas those aged 18–30 (9.4%), male (31.0%) and living in the province of Limburg (8.8%) are underrepresented. Most participants have attained a higher educational attainment (68.6%) and have a comfortable financial situation. Employees and officials (combined 34.5%) and retirees (28.7%) are well represented in the study, whereas relatively few labourers (2.0%) participated. Slightly over half of the participants in these waves were directly acquainted (family member, colleague or friend) with someone who has had (undefined) “severe” COVID-19 symptoms at some point (57.6%). A considerable proportion of the respondents (36.4%) reported at least one underlying medical condition. The most commonly reported condition was high blood pressure (15.5%). All subsequent presentations of summary statistics and statistical analyses are based on the use of inverse probability weighting, such as explained in the statistical analysis section.
3.2. Evolution of the willingness to be vaccinated, the pandemic, governmental decisions and other impactful news
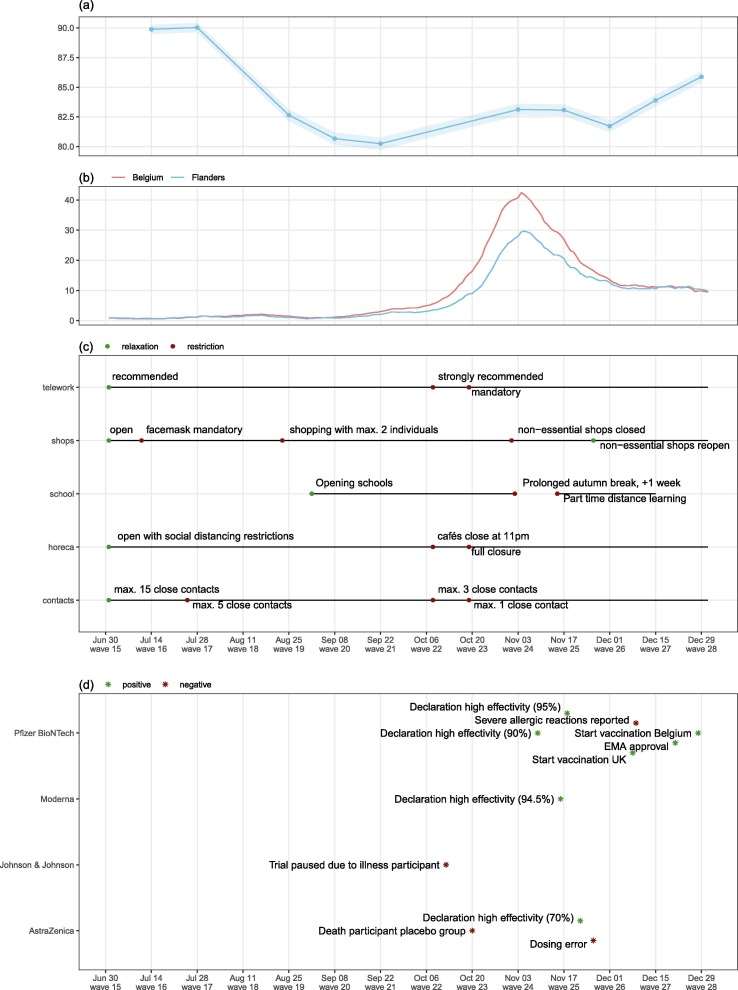
Of the respondents, 84.2% was willing to be vaccinated with a safe, effective and free of charge COVID-19 vaccine after weighting (61.2% definitely and 23.0% probably), while 15.9% was vaccine-hesitant (9.8% maybe, 3.9% probably not and 2.2% definitely not). Fig. 1 (a) visualizes the evolution of the weighted vaccine willingness reported per wave. Vaccine willingness was high in July 2020, with a peak willingness rate of 90.0% on July 28, 2020. It subsequently decreased in August until it reached an 80.2% willingness rate low point on September 22, 2020. It gradually recovered afterwards to reach an acceptance rate of 85.9% on December 29, which is still well below the willingness level of July.
Fig. 1.
Evolution of vaccine willingness over time and reference to the evolution of the pandemic, the sequence of governmental decisions and impactful media reporting on vaccines. (a) Percentage of COVID-19 vaccine acceptance, (b) New COVID-19 related hospitalizations per 100,000 inhabitants per week, (c) COVID-19 governmental measures and (d) Vaccine related media reporting.
Panels in Fig. 1 align the evolution in COVID-19 vaccine willingness with the evolution of the weekly number of new hospitalizations (b), governmental measures (NPIs) (c) and impactful media reporting on vaccines (d).
3.3. Reason for vaccine hesitancy
The main reasons for unwillingness to be vaccinated were non-specific safety concerns (61.0%, Table 2), concerns related to the fast development of the vaccine (54%) and expressing the preference to wait until more people are vaccinated (45.9%). Of the vaccine hesitant respondents, 28.4% indicates that the decision depends on which vaccine is offered to them. We opted not to present any ranges in this Table, because the (number of) response options slightly varied in the different waves because of the adaptive survey design and presenting ranges could be misinterpreted because of that.
3.4. Participant characteristics influencing vaccine willingness
Using backward variable selection based on BIC, all covariates in Table 1, except household composition, were retained as main effects in the model, while interactions between time and previous participation and between gender and previous participation were the only selected second-order effects, based on the selection process.
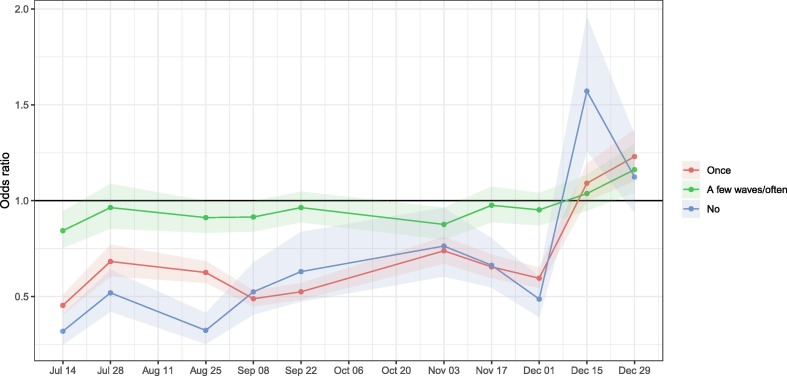
Before December 15, new participants were less likely to accept a vaccine than those who filled out the survey every time (July 14, OR 0.32, 95% confidence interval (CI) (0.25–0.41); Fig. 2 ). This effect of participation behaviour on vaccine willingness disappeared in the two most recent waves (Dec 15 and Dec 29).
Fig. 2.
Evolution of the odds ratio for vaccine willingness with 95% CI for outcomes of ‘participation in previous waves’ relative to participants who participated in every wave.
Male respondents indicate higher vaccine acceptance than female respondents, but the strength of this effect depends on the respondent’s past participation behaviour in our study. This interaction with participation behaviour signals sampling bias on the gender level. This demands caution when extrapolating findings related to gender to the whole population of Flanders, including those who never participated in our study, since their gender effect is likely to differ from the observed gender effects.
Table 1 additionally shows that, relative to respondents aged 18–30, those aged 31–50 were slightly less likely to accept a vaccine, while respondents aged 51–70 and 71 + were more likely to accept a vaccine. We found a strong positive association between COVID-19 vaccine willingness and both the respondent’s educational attainment and their financial comfort. Families consisting of two to five members were more willing to be vaccinated, when compared to singles and those living in large households (5+ members). Relative to employees and officials, students (OR 1.35 95% CI (1.27–1.43)) and retirees (OR 1.36 95% CI (1.30–1.43)) were more likely to accept a COVID-19 vaccine, while unemployed (OR 0.86, 95% CI (0.83–0.90)), self-employed (OR 0.78, 95% CI (0.74–0.83)) and labourers (OR 0.62, 95% CI (0.58–0.66)) were less willing to be vaccinated. There were no convincing differences in vaccine willingness between HCWs, employees/officials, and participants working in education. Participants who knew someone with severe COVID-19 symptoms were more willing to get vaccinated than others (OR 1.18 95% CI (1.16–1.21)). Most respondents suffering from an underlying medical condition showed higher vaccine willingness than those without comorbidities. This effect was strongest for people with diabetes (OR 1.43, 95% CI (1.33–1.53)), while no significant effect was found for those suffering from kidney disease (OR 0.97, 95% CI (0.87–1.10)).
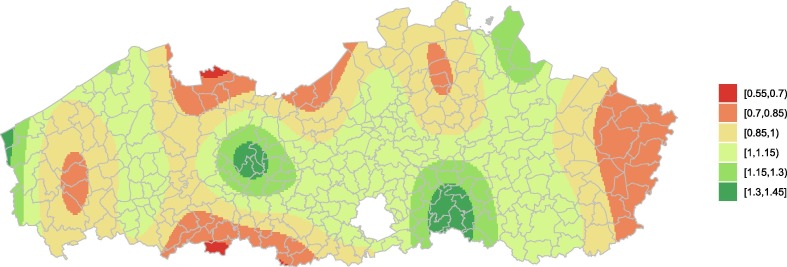
Vaccine acceptance in Flanders is presented in Fig. 3 . Several clusters of increased vaccine hesitancy can be detected around the borders of Flanders with The Netherlands (North and East) and Wallonia (South). Remarkably, regions around Ghent (East-Flanders) and Leuven (Flemish-Brabant) show relatively high vaccine willingness.
Fig. 3.
Spatially smoothed odds ratios for vaccine willingness based on the longitude, latitude coordinate of a participant’s residence as based on their postal code, relative to the Flemish average. The mean OR is scaled to one. Lower OR corresponds to higher vaccine hesitancy.
3.5. Behaviour-related outcomes associated with vaccine willingness
Table 3 shows that respondents who continued to have physical contact (hugs, kisses, shaking hands) outside their household were less likely to accept a COVID-19 vaccine compared to respondents that complied with social distancing (OR 0.66, 95% CI (0.64–0.68)). Similarly, people who did not install the Coronalert app, were less likely to accept a COVID-19 vaccine, compared to those who did (OR 0.33 95% CI (0.32–0.35)). There was a strong positive correlation between answering positively to the vaccine willingness question and showing trust towards the federal government. A small negative association was found between high scores on the GHQ-12 score (indicating strongly decreased mental well-being) and vaccine acceptance. A total of 77.5% of the respondents would let their child be vaccinated with a safe and effective COVID-19 vaccine. Vaccination acceptance for parents is very strongly associated with the vaccine acceptance for their children.
4. Discussion
Understanding the willingness and unwillingness to be vaccinated against COVID-19 is a crucial element in the development of targeted and effective vaccination campaigns, including tailored communication activities. More specifically, identifying drivers of vaccine willingness provides an opportunity to diversify intervention measures that are aimed at reaching a sufficiently high vaccination coverage. In this study, we reported on the intention to accept a COVID-19 vaccine and described changes in that willingness over time. We investigated and assessed a variety of background characteristics that influence vaccine willingness in Flanders, Belgium.
We found a high vaccine willingness in Flanders (84.2%), which is largely in line with recent published research investigating COVID-19 vaccine willingness in other European countries, e.g. the United Kingdom (UK) [34], Spain, Italy, Germany, Sweden [11], [35] and Flanders [36], where it was found that about 65 to 75% was willing to be vaccinated, whereas about 25% was in doubt, and 9 to 12% was unwilling to get vaccinated. Beware that in some of these studies, Likert-scales did not allow for more balanced responses like ‘probably yes’ or ‘probably no’, like in our study. Based on the results of their global survey, Lazarus et al. raised the concern that an insufficient proportion of people might be willing to accept a COVID-19 vaccine and that changes in vaccination coverage across countries might endanger worldwide control of the pandemic through community immunity [11]. Nevertheless, given uncertainty about the vaccines’ effectiveness against transmission [37], the emergence of new virus variants exhibiting greater transmissibility [38] and evolving compliance with NPIs, a so-called ‘herd immunity threshold’ remains unknown. Yet, it is clear that high vaccination coverage will be required to decrease the virus’ burden on healthcare systems as well as society. Hence, it is essential to understand individuals’ vaccine willingness and to identify subpopulations that might not reach sufficient coverage. In this regard, a single time point survey in Belgium identified people in favour of vaccination in general, but hesitant about COVID-19 vaccines, as an important target group for tailored vaccination campaigns [39].
4.1. What characteristics explain vaccine willingness?
The effects of age and gender on the willingness to be vaccinated have been described in several studies, though the results appear ambiguous [11], [34], [36], [40]. In our study, the age group of 31–50 years old was least likely to accept a vaccine. Participants aged 51–70 and 71+ were instead most willing to be vaccinated, which is in line with most COVID-19 vaccine willingness studies and can be explained by their higher risk for severe illness [41]. In another study, participants aged 18–24 have been identified as the most unwilling, even though they would be more willing to accept a vaccine in response to their employer’s recommendation [11]. In agreement with other studies [11], [36], [40], we found women less likely to accept a COVID-19 vaccine, compared to men. Note that the estimated gender effect in our study interacts with participation behaviour: female participants were always significantly less willing to be vaccinated than males, regardless of the participation history, but we observed larger differences between males and females among respondents that participated more frequently as compared to others. We therefore stress that the interpretation of the gender effect should not be extrapolated to the unobserved population.
Households with 2–5 persons were most willing to be vaccinated. Furthermore, parents in our study tended to answer similarly about vaccination for themselves and their children. In another study (UK, 1200 participants), respondents were more likely to accept a COVID-19 vaccine for themselves than for their child(ren) [42]. In a global study, the majority (65%) of caregivers intended to vaccinate their children against COVID-19 [14].
Lower educational attainment has repeatedly been associated with increased vaccine refusal [11], [40], [43]. The effect of education is substantial in our study, with markedly greater vaccine willingness in respondents with tertiary education, which increased even more for respondents with a PhD, compared to respondents with a primary or secondary education.
Although the (federal) government has decided that all vaccinations will be provided free of charge, families that are in a difficult financial situation, were less likely to accept a vaccine. Similarly, survey participants (UK) from lower-income households were found more likely to reject a COVID-19 vaccine [40], [42]. In Lazarus et al. [11], respondents, regardless of nationality, reported that they would be less likely to accept a COVID-19 vaccine under coercion (by employers), an observation that supports most governments decisions to offer vaccination on a voluntary basis, including in Belgium.
Our analyses show that the sector of employment also influences vaccine willingness. A particular finding is that only 81% of the HCWs in Flanders is willing to be vaccinated, which is similar to employees, officials and those working in education. Vaccination willingness is lower in labourers, self-employed and unemployed respondents, but higher in students and retired respondents. This is an important result, since HCWs remain the most trusted source of information about vaccines [25], [26] and are hence likely to play a crucial role in the recently started vaccination campaign. Indeed, a study in the US showed a positive association between vaccine willingness and HCWs’ recommendation [44]. Moreover, social norms and peer-influence were found important in vaccination decisions in Flanders as well [23], enforcing the role of HCWs, who were identified as a priority group in the Belgian vaccination strategy. These findings emphasize the need to provide well-designed and easy to reach information and support for HCWs.
Individuals who know someone who experienced severe COVID-19 symptoms, were more likely to accept a COVID-19 vaccine. The importance of risk perception on the intention to be vaccinated has been shown for COVID-19 [36], [43] and other vaccines [23], [45]. We also show that suffering from at least one underlying medical condition increases vaccine willingness, which may be explained by an increased fear for severe illness [41]. Furthermore, participants with lower mental well-being were more vaccine hesitant.
A worldwide survey with data collected in June 2020 revealed high vaccine acceptance in China and other Asian nations [11], which has been associated with their strong trust in the government. Our study confirms that trust in the government is strongly associated with vaccine willingness. Furthermore, a cross-sectional analysis of the ‘Great Corona Survey’ data from August 2020 [27], showed that trust in the government has a positive, but rather small effect on the willingness to vaccinate, while trust in experts had a more pronounced influence.
Vaccine willingness showed regional differences in Flanders. After correcting for the spatial distributions of explanatory variables in the model, parts of Flemish Brabant and East Flanders showed additional willingness to be vaccinated, while areas close to borders, such as Limburg, were generally less accepting. The two largest universities of Flanders (Ghent and Leuven) are located in areas with a relatively high willingness to get vaccinated (see Fig. 3).
Preventive behaviour such as installing a contact tracing App and social distancing adherence was positively associated with vaccine willingness. This observation emphasizes the value of engaging the public and stresses the importance of vaccination and the measures that are being taken. Across the study period, the three main reasons for vaccine hesitancy were safety concerns (61.0%), concerns related to the fast development of the vaccine (54.0%) and expressing the wish to wait until more people are vaccinated (45.9%). These are sentiments that have been picked up in other contemporary studies [15], [35], [40].
While in this study, we focused on longitudinal vaccine willingness and the identification of important target groups, other studies have looked into vaccine preferences. Discrete-choice experiments (DCEs) have, in particular, been instrumental in assessing vaccine-related preferences. That is, the studies of Motta et al. and Kreps et al. found that the probability of choosing a hypothetical COVID-19 vaccine increases when the vaccine has a longer protection duration, when there is a lower incidence of major/minor adverse effects and when the vaccine has received a full FDA approval (instead of FDA Emergency Use Authorisation) [46], [47]. DCE studies in Belgium too had already stressed the importance of risk perception and vaccines’ effectiveness in people’s vaccination decisions before the onset of the COVID-19 pandemic, with significant preference heterogeneities observed, mostly between different age groups [23], [45], [48].
In addition to identifying important target groups and assessing vaccine-related preferences, a successful vaccination campaign should also consider ethical concerns about motivational efforts to increase public support [49]. More specifically, public support for vaccination campaign related incentives, like legal compulsion or accountability, depends on the target group and disease scenario [50], while attitudes towards vaccination are in large part related to a person’s social orientation [49], [51].
4.2. Observation of trends
A unique aspect of this study is that we monitored COVID-19 vaccine willingness over a period of 6 months, with a remarkably high number of respondents. To date, little information was available about changes in COVID-19 vaccine willingness over time within the same population and what affects the dynamics of the willingness curve. One study in Italy showed that COVID-19 vaccine willingness was correlated to trust in research and in vaccines, which decreased between wave 1 and wave 2 of the Italian pandemic [52]. Another study investigated vaccine willingness over time by reviewing 126 international surveys and by pooling information from different populations [15], showing an overall declining vaccine willingness between March and October 2020. In Flanders, the willingness to vaccinate was highest in July 2020 (survey wave of July 28, 2020, 90.0%), it decreased over the summer period to 80.2% and started to increase again from late September, reaching 85.9% at the end of December after a small dip to 81.7% at the beginning of December (Fig. 1). Following the tail of the first Belgian COVID-wave, a relatively low disease burden was observed in July 2020. By the end of July, it became clear that there was an increase in clusters of cases in urban areas, which were locally controlled by more stringent NPIs, including a curfew in Antwerp. In addition, between late July and early October there was a heavily mediatized divide between experts of various backgrounds about the relaxation of NPIs, which may have influenced the credibility of infectious disease experts and may have affected trust in future COVID-19 vaccines. In the second half of September, the number of hospital admissions due to COVID-19 rose above 50 and deaths due to COVID-19 rose above 10 for the first time since mid-August. Although we were able to associate an extensive set of explanatory variables with vaccine willingness, some of the remaining variability in vaccine willingness could not be explained by these. This may be related to opportunistic sampling bias, which is signalled in the analysis by the significant interaction between the effects of gender and participation behaviour. This phenomenon might be complex and requires methodological developments, which extend those documented by Neyens et al. [33]. The small decrease in willingness early December coincides with the announcement that the lockdown measures will hold during the Christmas holidays on 27 November 2020 and the announcement of a dosing error in the AstraZeneca vaccine trial on 26 November 2020 (no causal effect was investigated). Announcements in the media about high vaccine efficacies published by Pfizer and BioNTech on 9 November 2020, by Moderna on 16 November 2020 and by AstraZeneca on 23 November 2020 (perceived low efficacy compared the other vaccines) may be important in the timeline of vaccine willingness, because they may have provided perspective and hope. However, reports from clinical studies being paused, may be a cause of concern and may have elicited questions about specific vaccines (see timeline in Fig. 1).
Extrapolating results beyond Flanders should be done with much caution, because even within Flanders, as in any general population, substantial variability in vaccine willingness exists (over time), that cannot be fully explained by the factors investigated in this study.
It is important to keep in mind that vaccine willingness does not necessarily reflect the expected vaccination coverage. This is illustrated by the observation that in the state of vaccine confidence in the EU (2018), Belgium scores rather poorly [29]. With regard to adult vaccination in Belgium, annual influenza vaccination coverage is estimated at 22.6% of the population at any age and 46.2% in elderly (65+) and risk groups (2018). This influenza vaccine coverage has kept a stable pace since 2004 [53]. During the H1N1 pandemic in 2009, a total of 6.9% of the Belgian population was vaccinated (18.8% in elderly 65+). Vaccinations mainly occurred after the pandemic threat subsided [54]. Note however, that we only included the Flemish population in the current study, with typically higher vaccination rates, compared to the other regions, as recently demonstrated in the context of human papillomavirus (HPV) vaccination [55]. Indeed, to date, Flanders remains relatively unphased by vaccine hesitancy or refusal as the year 2016 vaccine coverage study documented high and stable immunization coverage, although in a different context [56]. There are some limitations to our study. Participation in the surveys was voluntary and open to all, such that non-response might be driven by unobserved factors, which in turn might be related to vaccine willingness itself, e.g., perception of the pandemic’s severity. Correcting for this so-called preferential sampling requires complex joint modelling procedures, the implementation of which lies beyond the scope of this manuscript and which is further complicated by a second, convoluted, latent phenomenon; the survey frame, i.e., the portion of the intended study population that has a non-zero probability to become part of the survey sample, consists of a subset of the Flemish population that is difficult to define, since it depends on internet use and proficiency in the languages in which the survey was made available (Dutch, English, French, and German). The complexity of and relationships between mechanisms that underlie participation and vaccine willingness are illustrated by the observation that those who filled in the survey every time showcased a higher vaccine willingness than first-time participants - an effect that disappeared in the two most recent waves – in addition to its interaction with the gender effect. We are currently developing statistical methodology that will allow us to disentangle these latent phenomena to a considerable extent.
5. Conclusions
Our findings could help the government, policymakers and HCWs in Flanders to design more efficient and more tailored communication strategies about COVID-19 vaccination. Overall vaccine willingness in Flanders is high. However, based on our data, we identified important target groups for vaccination campaigns: aged 31–50, females, low educational attainment, large households, difficult financial situation, low mental well-being and labourers, unemployed and self-employed citizens. Furthermore, vaccine literacy, critical thinking and trust in science should be encouraged in the public, in order to reduce the vulnerability to fake news. Trust in the government should be a priority goal. These are vital interventions, since a clear link has been described between susceptibility to misinformation and both vaccine hesitancy and a reduced likelihood to comply with health guidance measures [57]. Importantly, our study also emphasizes that in the rapidly evolving COVID-19 pandemic, results from different studies are only comparable to a limited extent, as both the timing and the region of data collection influence the results of vaccine willingness studies.
Disclosures
PB, KP, PVD, TN and NH initiated the study, and designed, formulated and implemented the questionnaires. JC, TN and MV performed statistical analyses. SV, GH and FV retrieved relevant background literature. SV, GH, FV, JC and TN wrote the first draft. All authors interpreted the results and revised the manuscript for important intellectual content. All authors attest they meet the ICMJE criteria for authorship and have approved the final article.
Funding
The Great Corona Survey is supported by the Research Foundation Flanders (Grant G0G1920N, 2020) and the University of Antwerp Fund. Authors FV, NH and PB acknowledge funding from the European Union’s Horizon 2020 research and innovation programme (Project EpiPose - No. 101003688, 2020). All VAXINFECTIO authors acknowledge funding as part of the Methusalem-Centre of Excellence consortium VAX–IDEA. Support from the Methusalem finance programme of the Flemish Government is gratefully acknowledged. These funding sources had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Unrelated to the work reported here, the University of Antwerp has received unrestricted grants and compensation for meeting attendance with GSK and Pfizer. The University of Antwerp obtains research grants from vaccine manufacturers for the conduct of vaccine trials for which PVD is principal investigator. The authors have no other competing interest to declare.
Acknowledgements
The authors acknowledge the expert assistance of Linguapolis for linguistical support (for the Great Corona Survey) and Peter De Meyer for distributing news and media items to promote participation in the Great Corona Survey.
Footnotes
waves 15 (14/07/2020), 16 (28/07/2020), 18 (25/08/2020), 19 (08/09/2020), 20 (22/09/20202), 23 (3/11/2020), 24 (17/11/2020), 25 (1/12/2020), 26 (15/12/2020) and 27 (29/12/2020).
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2021.10.073.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Verelst F., Kuylen E., Beutels P. Indications for healthcare surge capacity in European countries facing an exponential increase in coronavirus disease (COVID-19) cases, March 2020. Euro Surveill. 2020;25(13) doi: 10.2807/1560-7917.ES.2020.25.13.2000323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.European Commission. Coronavirus vaccine strategy; 2020. https://ec.europa.eu/info/live-work-travel-eu/coronavirus-response/public-health/coronavirus-vaccines-strategy_en [accessed: 10/02/2021].
- 3.Krammer F. SARS-CoV-2 vaccines in development. Nature. 2020;586(7830):516–527. doi: 10.1038/s41586-020-2798-3. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organisation. Draft landscape and tracker of COVID-19 candidate vaccines; 2021. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines [accessed: 10/02/2021].
- 5.European Medicines Agency. COVID-19 vaccines: development, evaluation, approval and monitoring; 2020. https://www.ema.europa.eu/en/human-regulatory/overview/public-health-threats/coronavirus-disease-covid-19/treatments-vaccines/covid-19-vaccines-development-evaluation-approval-monitoring [accessed: 10/02/2021].
- 6.U.S. Food and Drug Administration. COVID-19 Vaccines; 2020. https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines [accessed: 10/02/2021].
- 7.World Health Organisation. Emergency Use Listing Procedure; 2020. https://www.who.int/teams/regulation-prequalification/eul#:~:text=The%20WHO%20Emergency%20Use%20Listing,by%20a%20public%20health%20emergency [accessed: 10/02/2021].
- 8.European Commission. Questions and Answers: COVID-19 vaccination in the EU; 2020. https://ec.europa.eu/commission/presscorner/detail/en/qanda_20_2467 [accessed: 10/02/2021].
- 9.European Centre for Disease Prevention and Control. COVID-19 vaccination and prioritisation strategies in the EU/EEA; 2020. https://www.ecdc.europa.eu/en/publications-data/covid-19-vaccination-and-prioritisation-strategies-eueea [accessed: 10/02/2021].
- 10.MacDonald N.E., Hesitancy S.W.G.O.V. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 11.Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K., et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2020 doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Verger P., Scronias D., Dauby N., Adedzi K.A., Gobert C., Bergeat M., Gagneur A., Dube E. Attitudes of healthcare workers towards COVID-19 vaccination: a survey in France and French-speaking parts of Belgium and Canada, 2020. Euro Surveill. 2021;26(3) doi: 10.2807/1560-7917.ES.2021.26.3.2002047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freeman D., Loe B.S., Chadwick A., Vaccari C., Waite F., Rosebrock L., et al. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. 2020:1–15. doi: 10.1017/S0033291720005188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goldman R.D., Yan Tyler D., Seiler Michelle, Parra Cotanda Cristina, Brown Julie C., Klein Eileen J., et al. Caregiver willingness to vaccinate their children against COVID-19: Cross sectional survey. Vaccine. 2020;38(48):7668–7673. doi: 10.1016/j.vaccine.2020.09.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin C., Tu Pikuei, Beitsch Leslie M. Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines (Basel) 2020;9(1):16. doi: 10.3390/vaccines9010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Williams L., Gallant A.J., Rasmussen S., Brown Nicholls L.A., Cogan N., Deakin K., et al. Towards intervention development to increase the uptake of COVID-19 vaccination among those at high risk: Outlining evidence-based and theoretically informed future intervention content. Br J Health Psychol. 2020;25(4):1039–1054. doi: 10.1111/bjhp.v25.410.1111/bjhp.12468. [DOI] [PubMed] [Google Scholar]
- 17.Amirthalingam G., Gupta S., Campbell H. Pertussis immunisation and control in England and Wales, 1957 to 2012: a historical review. Euro Surveill. 2013;18(38) doi: 10.2807/1560-7917.es2013.18.38.20587. [DOI] [PubMed] [Google Scholar]
- 18.Guillaume L.R., Bath P.A. The Impact of Health Scares on Parents’ Information Needs and Preferred Information Sources: A Case Study of the MMR Vaccine Scare. Health Inform J. 2004;10(1):5–22. [Google Scholar]
- 19.Larson H.J., Cooper L.Z., Eskola J., Katz S.L., Ratzan S. Addressing the vaccine confidence gap. Lancet. 2011;378(9790):526–535. doi: 10.1016/S0140-6736(11)60678-8. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organisation. 10 threats to global health in 2019; 2019. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 [accessed: 10/02/2021].
- 21.Jarrett C., Wilson R., O’Leary M., Eckersberger E., Larson H.J., Hesitancy S.W.G.O.V. Strategies for addressing vaccine hesitancy - A systematic review. Vaccine. 2015;33(34):4180–4190. doi: 10.1016/j.vaccine.2015.04.040. [DOI] [PubMed] [Google Scholar]
- 22.Dube E., Gagnon D., MacDonald N.E., Hesitancy S.W.G.O.V. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine. 2015;33(34):4191–4203. doi: 10.1016/j.vaccine.2015.04.041. [DOI] [PubMed] [Google Scholar]
- 23.Verelst F., Willem L., Kessels R., Beutels P. Individual decisions to vaccinate one's child or oneself: A discrete choice experiment rejecting free-riding motives. Soc Sci Med. 2018;207:106–116. doi: 10.1016/j.socscimed.2018.04.038. [DOI] [PubMed] [Google Scholar]
- 24.Larson Heidi J., Clarke Richard M., Jarrett Caitlin, Eckersberger Elisabeth, Levine Zachary, Schulz Will S., et al. Measuring trust in vaccination: A systematic review. Hum Vaccin Immunother. 2018;14(7):1599–1609. doi: 10.1080/21645515.2018.1459252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.European Commission. Special Eurobarometer 488; 2019. https://ec.europa.eu/health/sites/health/files/vaccination/docs/20190426_special-eurobarometer-sp488_en.pdf [accessed: 10/02/2021].
- 26.Wellcome. Wellcome global monitor 2018; 2018. https://wellcome.org/reports/wellcome-global-monitor/2018 [accessed: 10/02/2021].
- 27.Wynen J, Op de Beeck S, Verhoest K, Glavina M, Six F, Van Damme P, et al. Taking the Covid-19 vaccine or not? Understanding vaccination attitude using trust in experts and trust in government. In Paper presented at TRUSTGOV conference; 2020.
- 28.World Health Organisation. COVID-19 vaccines: Safety Surveillance Manual; 2020. https://apps.who.int/iris/bitstream/handle/10665/338400/9789240018280-eng.pdf?sequence=1&isAllowed=y [accessed: 10/02/2021].
- 29.Larson H., de Figueiredo A., Karafillakis E., Rawal M. State of vaccine confidence in the European Union in 2018. Eur J Public Health. 2019;29:141. [Google Scholar]
- 30.Corona study. How are you dealing with the coronavirus?; 2020. https://www.uantwerpen.be/en/projects/corona-study/ [accessed: 10/02/2021].
- 31.Goldberg D.P. User's guide to the General Health Questionnaire. Windsor; 1988.
- 32.Coronalert; 2020. https://coronalert.be/nl/ [accessed: 10/02/2021].
- 33.Neyens T., Faes C., Vranckx M., Pepermans K., Hens N., Van Damme P., et al. Can COVID-19 symptoms as reported in a large-scale online survey be used to optimise spatial predictions of COVID-19 incidence risk in Belgium? Spat Spatio-Temporal. 2020;35:100379. doi: 10.1016/j.sste.2020.100379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sherman S.M., Smith L.E., Sim J., Amlot R., Cutts M., Dasch H., et al. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum Vacc Immunother. 2020 doi: 10.1080/21645515.2020.1846397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Neumann-Böhme S., Varghese N.E., Sabat I., Barros P.P., Brouwer W., van Exel Job, et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020;21(7):977–982. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krouwer S, Poels K, Vandebosch H. Onderzoek naar de attitudes van Vlamingen ten opzichte van de COVID-19 vaccinaties; 2020. http://www.simonekrouwer.com/wp-content/uploads/2020/12/Rapport-Onderzoek-naar-de-attitudes-van-Vlamingen-ten-opzichte-van-de-COVID-19-vaccinaties-de-eerste-resultaten.pdf [accessed: 10/02/2021].
- 37.Hodgson Susanne H, Mansatta Kushal, Mallett Garry, Harris Victoria, Emary Katherine R W, Pollard Andrew J. What defines an efficacious COVID-19 vaccine? A review of the challenges assessing the clinical efficacy of vaccines against SARS-CoV-2. Lancet Infect Dis. 2021;21(2):e26–e35. doi: 10.1016/S1473-3099(20)30773-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leung K., Shum M.H., Leung G.M., Lam T.T., Wu J.T. Early transmissibility assessment of the N501Y mutant strains of SARS-CoV-2 in the United Kingdom, October to November 2020. Euro Surveill. 2021;26(1) doi: 10.2807/1560-7917.ES.2020.26.1.2002106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kessels Roselinde, Luyten Jeroen, Tubeuf Sandy. Willingness to get vaccinated against COVID-19 and attitudes toward vaccination in general. Vaccine. 2021;39(33):4716–4722. doi: 10.1016/j.vaccine.2021.05.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Paul E., Steptoe A., Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. Lancet Reg Health. 2020:100012. doi: 10.1016/j.lanepe.2020.100012. Online first. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Centers for disase control and prevention. People with Certain Medical Conditions; 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html [accessed: 10/02/2021].
- 42.Bell S., Clarke R., Mounier-Jack S., Walker J.L., Paterson P. Parents' and guardians' views on the acceptability of a future COVID-19 vaccine: A multi-methods study in England. Vaccine. 2020;38(49):7789–7798. doi: 10.1016/j.vaccine.2020.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guidry Jeanine P.D., Laestadius Linnea I., Vraga Emily K., Miller Carrie A., Perrin Paul B., Burton Candace W., et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021;49(2):137–142. doi: 10.1016/j.ajic.2020.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine. 2020;38(42):6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Luyten J., Kessels R., Goos P., Beutels P. Public Preferences for Prioritizing Preventive and Curative Health Care Interventions: A Discrete Choice Experiment. Value Health. 2015;18(2):224–233. doi: 10.1016/j.jval.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 46.Motta Matt. Can a COVID-19 vaccine live up to Americans’ expectations? A conjoint analysis of how vaccine characteristics influence vaccination intentions. Soc Science & Med. 2021;272:113642. doi: 10.1016/j.socscimed.2020.113642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kreps S., Prasad S., Brownstein J.S., Hswen Y., Garibaldi B.T., Zhang B., et al. Factors associated with US Adult’s likelyhood of accepting COVID-19 vaccination. JAMA Net Open. 2020;3(10) doi: 10.1001/jamanetworkopen.2020.25594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Verelst Frederik, Kessels Roselinde, Willem Lander, Beutels Philippe. No such thing as a free-rider? Understanding drivers of childhood and adult vaccination through a multicountry discrete choice experiment. Vaccine. 2021;9(3):264. doi: 10.3390/vaccines9030264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Luyten J., Vandevelde A., Van Damme P., Beutels P. Vaccination policy and ethical challenges posed by herd immunity, suboptimal uptake and subgroup targeting. Public health ethics. 2011;4(3):280–291. [Google Scholar]
- 50.Luyten J., Dorgali V., Hens N., Beutels P. Public preferences over efficiency, equity and autonomy in vaccination policy: an epirical study. Soc Sci Med. 2013;77:84–89. doi: 10.1016/j.socscimed.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 51.Luyten J., Desmet P., Dorgali V., Hens N., Beutels P. Kicking against the pricks: vaccine sceptics have different social orientation. Eur J Pub Health. 2014;24(2):310–314. doi: 10.1093/eurpub/ckt080. [DOI] [PubMed] [Google Scholar]
- 52.Palamenghi L., Barello S., Boccia S., Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur J Epidemiol. 2020;35(8):785–788. doi: 10.1007/s10654-020-00675-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sciensano. Gezondheidsenquete 2018; 2018. https://his.wiv-isp.be/nl/Gedeelde%20%20documenten/summ_PR_NL_2018.pdf [accessed: 14/07/2021].
- 54.Wetenschappelijk Instituut Volksgezondheid. Surveillance van griep in België – Seizoen 2009–2010; 2011. https://epidemio.wiv-isp.be/ID/diseases/SiteAssets/Pages/Influenza/FLU%202009-2010%20%20NL.pdf [accessed: 14/07/2021].
- 55.Tjalma W.A.A., Brasseur C., Top G., Ribesse N., Morales I., Van Damme P.A. HPV vaccination coverage in the federal state of Belgium according to regions and their impact. Facts Views Vis Obgy. 2018;10(2):101–105. [PMC free article] [PubMed] [Google Scholar]
- 56.Vandermeulen C, Hoppenbrouwers K, Roelants M, Theeten H, Braeckman T, Maertens K, et al. Studie van de vaccinatiegraad in Vlaanderen; 2016. https://www.zorg-en-gezondheid.be/sites/default/files/atoms/files/Vaccinatiegraadstudie%202016.pdf [accessed: 14/07/2021].
- 57.Roozenbeek Jon, Schneider Claudia R., Dryhurst Sarah, Kerr John, Freeman Alexandra L.J., Recchia Gabriel, et al. Susceptibility to misinformation about COVID-19 around the world. R Soc Open Sci. 2020;7(10):201199. doi: 10.1098/rsos.201199. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.