Abstract
Neutropenia is a rare haematological complication of COVID-19 infection in immunocompetent patients. There is sparse literature on neutropenia in patients with COVID-19, except a few case reports. We encountered a similar case in an intensive care unit that developed severe neutropenia on day 24 of illness. Neutropenia resolved spontaneously on 4th day of its appearance. The patient was isolated and kept under close observation, antibiotics were upgraded and strict asepsis was maintained. Thus, we observed in a patient with no comorbidities and uncomplicated neutropenia that strict measures to prevent infection may suffice and the undue risk of hematopoietic therapy can be avoided. An expert opinion should always be sought in such cases as the presence of complications may require an aggressive approach.
Keywords: COVID-19, haematology (incl blood transfusion), intensive care
Background
Infection with SARS-CoV-2 or COVID-19 has been linked with a range of haematological manifestations. Lymphocytopenia is the most commonly reported among hematopoietic abnormalities.1 Severe neutropenia is a rarely observed phenomenon in patients infected with COVID-19 with only a few case reports.2 3 The available literature is insufficient about its management in such a scenario. In our patient, the neutropenia was self-limited and resolved on its own within 3 days of its onset with the following conservative measures only. As the safety of administration of hematopoietic agents such as granulocyte-colony stimulating factor (G-CSF) in patients with COVID-19 is still not established, its prescription in uncomplicated neutropenia could be avoided. Furthermore, an expert opinion from a haematologist should always be sought while managing such cases.
Case presentation
A 33-year-old man with no known comorbidities and a confirmed severe SARS-CoV-2 was admitted with the severe disease with impending respiratory failure in the intensive care unit (ICU); his condition improved subsequently and mode of oxygen support gradually titrated from high-flow nasal cannula, non-rebreathing mask and face mask to nasal cannula. The patient had improved clinically and was about to be shifted to the ward. The transfer to the ward was held due to incidental findings of severe neutropenia (an absolute neutrophil count (ANC) of 119/µL) on the 24th day of illness (ie, day 14th of the admission) on a routine investigation. It was a sudden drop in ANC from 4500/µL in the last 48 hours. The patient had received antibiotic ceftriaxone 1 g 12 hourly for 12 days, dexamethasone 8 mg two times per day and dalteparin 5000 U once daily. The patient had also received an intravenous injection of remdesivir 200 mg on day 1 of admission followed by 100 mg for the next 4 days (at the day of illness 11th–15th). The lymphopenia was present since early in the disease. Total leucocyte count (TLC) was 0.970 x109/L, ANC 119/µL (12.3% of TLC) and lymphocytes 261 (27% of TLC). No decrease in absolute count of other granulocytes, red blood cells or platelets was observed. Monocyte count was 299/µL (30.9% of TLC), basophil count was 27/µL (2.8% of TLC), eosinophil count was 805/µL (8.3% of TLC) and platelet count was 253×109/L. A haematologist was consulted for any further workup to rule out the possibility of any concurrent haematological disorder. A multidisciplinary team of ICU decided to hold any hematopoietic therapy until a full evaluation of the patient while keeping the patient under close observation for any infectious complications. ANCs showed a slight increase in the next day to 195/µL. The patient was afebrile and vital signs were stable. Antibiotics and other supportive treatments were continued as per the standard of practice of the institution. By the 3rd day (27th day of illness) of onset of the neutropenia, ANC recovered spontaneously to >1200 /µL followed by >4000/µL on the 4th day (28th day of the illness). The patient remained symptom free throughout thereafter, oxygen therapy discontinued, antibiotics de-escalated and then stopped as none of the specimens revealed positivity on culture sensitivity. The patient was asymptomatic and discharged to home on the 34th day of illness.
Investigations
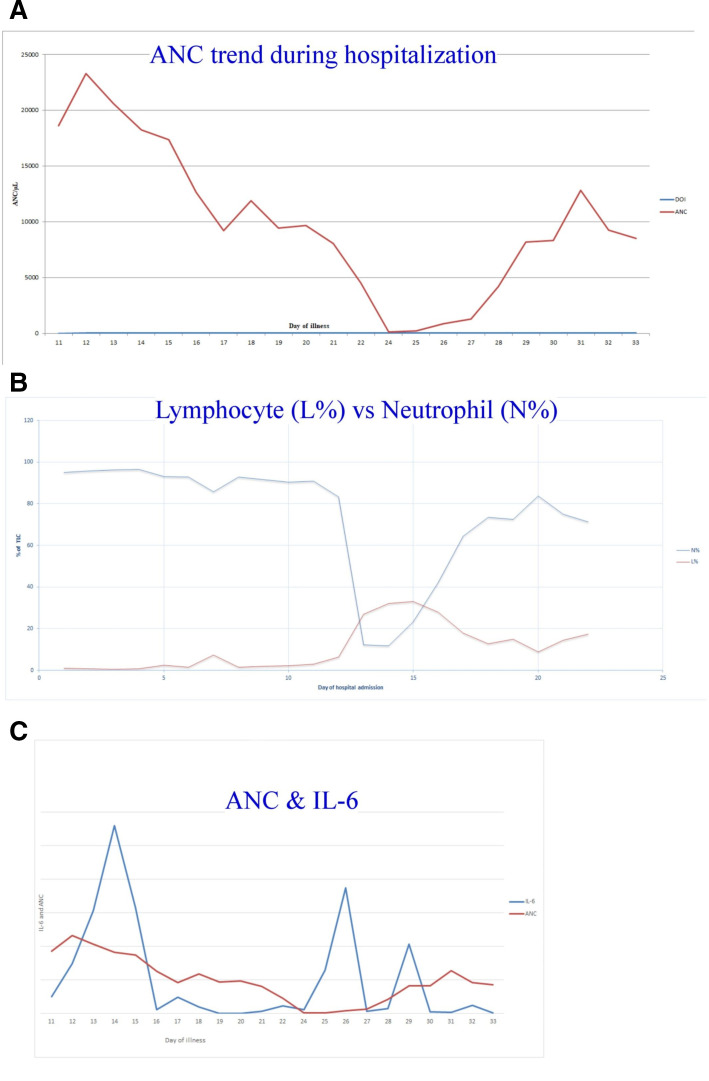
In blood sample from same day when neutropenia was detected, the levels of inflammatory markers were interleukin-6 (IL-6) 1.2 pg/mL (normal range 0–4.4 pg/mL), C reactive protein 0.1 mg/mL (normal range 0–0.5 mg/dL), procalcitonin 0.06 ng/mL (normal<0.1 ng/mL), lactate dehydrogenase 242 U/L, ferritin 476 ng/mL and D-dimer 251 ng/mL. Liver, kidney and hemostatic function tests were normal. Trend of ANC, a relationship between percentage of lymphocyte and neutrophil, and IL-6 levels during hospitalisation in our patient is shown in figure 1.
Figure 1.
Trend of absolute neutrophil count (ANC) (A). Relationship between percentage of lymphocyte (L%) and neutrophil (N%) (B) and interleukin-6 (IL-6) levels and ANC (C) during hospitalisation in our patient.
The blood, urine and sputum samples were taken for culture sensitivity and a peripheral smear for malaria was also negative. A repeat nasopharyngeal swab for reverse transcriptase-PCR for SARS-CoV-2 tested positive.
To rule out the viral, protozoal, autoimmune and nutritional causes for neutropenia following tests were done. Viral serology for HIV, hepatitis B surface antigen, hepatitis C virus, Epstein-Barr virus, parvovirus B19 and toxoplasma was negative or inconclusive. A peripheral smear was negative for malaria parasites. The autoimmune screening was negative for antinuclear antibodies, antineutrophil cytoplasmic antibodies, anti-dsDNA, β2 glycoprotein IgG and IgM, direct antiglobulin test and antithyroid antibodies. Serum Igs level and protein electrophoresis revealed a normal study. Serum vitamin B12, folate and iron parameters were also within normal limits.
No evidence of any lymph node enlargement or organomegaly was observed in ultrasonography of the abdomen and pelvis and whole-body CT scan.
Differential diagnosis
The possibility of iatrogenic neutropenia was ruled out as none of the drugs in the regimen including remdesivir or ceftriaxone were strongly associated with isolated neutropenia with such a short duration of treatment. Viral, protozoal, autoimmune and nutritional causes for neutropenia were also ruled out with appropriate testing. No history of malignancy in the family or any clinical or diagnostic features suggestive of it were found on evaluation.
Treatment
Antibiotics and antifungals were upgraded according to the sensitivity pattern of local flora of ICU to meropenem and teicoplanin and voriconazole. The patient was shifted to an isolated cabin to prevent cross-infection and was kept under close observation and the ICU staff were instructed to maintain strict asepsis.
Outcome and follow-up
The patient remained symptom free throughout the neutropenia phase, gradually oxygen therapy discontinued, antibiotics were de-escalated and then were stopped as none of the specimens revealed positivity on culture sensitivity. The patient was asymptomatic and was discharged home on the 34th day of illness. The patient was followed up for 2 weeks over a telephonic conversation, was symptom free, healthy and had resumed his job.
Discussion
Among haematological abnormalities in patients with COVID-19, the incidence of lymphocytopenia ranged from 39% to 83%, with thrombocytopenia 5%–36% and leucopenia 17%–33% across various previous studies.1 The previous studies do not mention neutropenia as a manifestation of COVID-19 infection. There are only a few previous case reports on neutropenia in otherwise immunocompetent adult patients2–4 and an infant.5 The neutropenia in patients with COVID-19 with haematological malignancy6 7 or solid tumour8 has also been reported. Drug-induced neutropenia could also be the reason as described in the previous two reports.9 10 We had also screened our patients for any drug-induced cytopenia but did not found any offending agent. The patient was further evaluated for neutropenia as described in the previous studies2–4 11 After a thorough clinical history and physical examination, we evaluated the patient for any other concurrent viral or protozoan infections known to cause cytopenia. An autoimmune screening, peripheral blood smear and blood level of folate, vitamin B12 and iron were also done. No significant findings could be found on screening for any concurrent viral or protozoan infections, autoimmune screening, peripheral blood smear and blood level of folate, vitamin B12 and imaging studies. Our multidisciplinary team of ICU decided to hold any further invasive testing including bone marrow examination and administration of any hematopoietic agent as G-CSF and kept the patient under close watch. A similar approach was observed in one of the previous case reports where in an otherwise healthy patient with delayed neutropenia after recovery from COVID-19, non-invasive laboratory tests to rule out the most likely causes were performed and a watchful-waiting approach was followed rather than performing invasive investigations such as bone marrow biopsy or administering G-CSF4 but we differ in this aspect with respect to other previous reports,2 3 as the patient in our case was more stable and asymptomatic and also did not have any family history of malignancy. The administration of G-CSF in COVID-19 could be detrimental and may cause early development of acute respiratory distress syndrome and worsening of the condition of the patient by modulating the immune system.12 13 On day 3, ANCs were>1200/µL, other routine laboratory investigations were also normal and the patient also improved clinically from COVID-19. Thus, it is learnt from this experience and available literature that an early or delayed severe neutropenia could be found during severe COVID-19 infection2–4 and could be a result of transient bone marrow suppression by significant inflammatory response during viral infection.4 It could be the possibility that like certain other viral illnesses, it is one of the haematological manifestations that is yet under-reported as most cases are asymptomatic and may go unnoticed. Haematologists should be involved in the management of such cases and any concurrent illnesses causing neutropenia should be ruled out. Strict asepsis should be maintained and close monitoring for any signs and symptoms of infectious complications should be done.
Learning points.
Neutropenia is a rare but prevalent haematological complication in patients with COVID-19.
The incidence of neutropenia in COVID-19 could be underestimated as many cases might go unnoticed due to the self-limiting nature of neutropenia.
All cases might not require painful and invasive investigations such as bone marrow to rule out other relevant causes.
All cases with neutropenia might not require haematopoietic therapy and the decision to administer must be balanced against benefit and harm.
Specialist haematologist consultation or opinion is a must in such cases.
Footnotes
Twitter: @sirohiyap
Contributors: RS: Planning, manuscript writing, reporting the work and case management and also acts as the guarantor. BKR: Editing, final approval of manuscript and case management. PS: Final approval and case management. SB: Critical review and Final approval
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.Erdinc B, Sahni S, Gotlieb V. Hematological manifestations and complications of COVID-19. Adv Clin Exp Med 2021;30:101–7. 10.17219/acem/130604 [DOI] [PubMed] [Google Scholar]
- 2.Devi YM, Sehrawat A, Panda PK, et al. Febrile neutropenia due to COVID-19 in an immunocompetent patient. BMJ Case Rep 2021;14:e242683. 10.1136/bcr-2021-242683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.López-Pereira P, Iturrate I, de La Cámara R, et al. Can COVID-19 cause severe neutropenia? Clin Case Rep 2020;8:3348–50. 10.1002/ccr3.3369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mank VMF, Mank J, Ogle J, et al. Delayed, transient and self-resolving neutropenia following COVID-19 pneumonia. BMJ Case Rep 2021;14:e242596. 10.1136/bcr-2021-242596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bouslama B, Pierret C, Khelfaoui F, et al. Post-COVID-19 severe neutropenia. Pediatr Blood Cancer 2021;68:e28866. 10.1002/pbc.28866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spencer HC, Wurzburger R. COVID-19 presenting as neutropenic fever. Ann Hematol 2020;99:1939–40. 10.1007/s00277-020-04128-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hernandez JM, Quarles R, Lakshmi S, et al. Pancytopenia and profound neutropenia as a sequela of severe SARS-CoV-2 infection (COVID-19) with concern for bone marrow involvement. Open Forum Infect Dis 2021;8:ofab017. 10.1093/ofid/ofab017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Figuero-Pérez L, Olivares-Hernández A, Escala-Cornejo RA, et al. Management of febrile neutropenia associated with SARS-CoV-2 infection in a patient with cancer. JCO Oncol Pract 2020;16:348–9. 10.1200/OP.20.00197 [DOI] [PubMed] [Google Scholar]
- 9.Meyre PB, Radosavac M, Baumann L, et al. COVID-19 in a patient with accidental drug-induced neutropenia. Eur J Case Rep Intern Med 2020;7:001848. 10.12890/2020_001848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gee S, Taylor D. The effect of COVID-19 on absolute neutrophil counts in patients taking clozapine. Ther Adv Psychopharmacol 2020;10:204512532094093. 10.1177/2045125320940935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Newburger PE, Dale DC. Evaluation and management of patients with isolated neutropenia. Semin Hematol 2013;50:198–206. 10.1053/j.seminhematol.2013.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tralongo AC, Extermann M. Older patients with cancer and febrile neutropenia in the COVID-19 era: a new concern. J Geriatr Oncol 2020;11:1329–30. 10.1016/j.jgo.2020.06.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Selim S. Leukocyte count in COVID-19: an important consideration. Egypt J Bronchol 2020;14. 10.1186/s43168-020-00045-8 [DOI] [Google Scholar]