Abstract
Background
Studies assessing consumers’ knowledge of the rational use of antibiotics are essential to understand the knowledge gap before intervention strategies are instituted.
Objectives
To assess the knowledge of rational use of antibiotics among consumers in Dar es Salaam, Tanzania.
Methods
A cross-sectional study assessing knowledge of rational use of antibiotics among 960 consumers was conducted in Dar es salaam in March 2021. Participants were consecutively enrolled from outpatient pharmacies in selected public and private hospitals and marketplaces in Ilala Municipality. Data were collected using the WHO-validated questions on knowledge of consumers of antibiotic uses.
Results
Overall, 196 (20.4%) and 503 (52.4%) participants demonstrated good knowledge of rational antibiotic use and conditions that can be treated with antibiotics, respectively. However, 678 (70.6%) responded that they stopped using antibiotics after dose completion, 515 (53.6%) would request the same antibiotic if it had helped to treat a similar condition in the past and 406 (42.3%) are willing to use the same antibiotic if a friend or family member used the medication previously to treat similar signs and symptoms. Besides, the following conditions were mentioned as being treatable with antibiotics: influenza (50.7%), sore throat (61.4%) and urinary tract infection (60.5%).
Conclusions
The majority of the consumers had poor knowledge of the rational uses of antibiotics and a moderate proportion had good knowledge of the conditions that are treatable with antibiotics. Those with a high level of education and with health insurance had good knowledge of rational uses of antibiotics.
Introduction
Antibiotic resistance (AR) is a major global health challenge. It is defined as the ability of microbes such as bacteria or fungi to resist standard dose(s) of antibiotics that were previously effective.1 Inappropriate use of antibiotics in treating infectious diseases, animal keeping and agricultural activities are the major contributing factors towards the emergence and spread of AR.2 A recent update on antibiotic susceptibility profiles from Tanzania reported that most of the clinical bacterial isolates tested were resistant to most first- and second-line antibiotics.3 Another study from Tanzania on the susceptibility of reserved antibiotics demonstrated that 68% of the clinical isolates of Staphylococcus aureus tested were resistant to clindamycin, and 8.5% and 75.6% of the tested Klebsiella spp. were resistant to meropenem and cefepime, respectively.4 Similar trends of resistance of clinical bacterial isolates toward commonly used antibiotics have been reported in Kenya and Malawi, which are located in the same geographical location.5–7
Antibiotics are misused in low- and middle-income countries.8,9 Shortage of healthcare services, dispensing of antibiotics as over-the-counter medication, profit inclination and weak regulatory authorities contribute to the observed misuse of antibiotics in developing countries.10,11 Also, lack of knowledge of antibiotic uses, potential side effects, correct dose and dosage, indication and drug–drug interaction have been associated with the observed poor patient management and occurrence of AR.11 Due to inadequate healthcare services in developing countries, most people rely on private community drug outlets, which embrace self-medication practice, as their primary level of care.12 Private drug outlets are claimed to be profit-oriented businesses, provide poor quality services and employ incompetent dispensers that significantly contribute to inappropriate use of medications.9 For instance, Minzi et al. (2013)13 observed a massive violation of antibiotic use in accredited drug dispensing outlet shops in Tanzania, where patients would be irrationally given antibiotics, including undergoing intramuscular injection of penicillins.
Shortage of guidelines on how to dispense and treat patients using antibiotics, lack of surveillance systems; lack of updated local treatment guidelines and continuing education to healthcare providers on uses of antibiotics;12 poor regulation on the use of human antibiotics in veterinary and agricultural activities; and misuses of antibiotics by livestock keepers (wrong dose, route of administration and antibiotic combination) have been suggested as the source of AR in developing countries.14 In addition, lack of knowledge of the consequences of inappropriate use and poor disposal of antibiotics among consumers contribute significantly to the emergence and spread of AR.15,16
AR poses a burden and stress to the resource-scarce healthcare system already existing in developing countries through increasing treatment costs, increasing the risk of adverse drug reactions, long duration of hospital stays and increased mortality due to manageable conditions. Globally, it is estimated that by 2050, 10 million people will die of infectious diseases if new antibiotics are not discovered, or if the existing ones are not protected from resistance.14 Several measures have been proposed to fight AR, such as raising the level of knowledge of the community on the appropriate use of antibiotics and the consequences of using the drugs without medical consultation.17,18 However, understanding the knowledge gap among antibiotic consumers before intervention strategies are instituted is of paramount importance.16 Therefore, this study aimed to assess the knowledge of appropriate uses of antibiotics among consumers exiting public hospitals, private hospitals and market vendors as representative of antibiotic consumers who were not sick.
Methods
Study design and setting
This cross-sectional study was initiated in March 2021 in Dar es Salaam, Tanzania. Dar es Salaam is the largest city in Tanzania, and the 2012 census reported a population of 4.36 million within the region, accounting for 10% of the total Tanzania Mainland population. It is also Tanzania’s major business city.19 Three different areas were used to recruit participants: patients who exited outpatient pharmacies in the selected public and private hospitals and people in marketplaces in Ilala Municipality. The permission for data collection was obtained in three regional referral public hospitals (Temeke, Mwananyamala and Amana), two private hospitals (Ekenywa and Mvungi) and the three most prominent markets in Ilala Municipality (Kariakoo, Karume and Buguruni).
Study population
Adult patients who purchased drugs from pharmacies in the private and public hospitals with at least one antibiotic in their prescription and market vendors who provided written informed consent were recruited.
Sample size and sampling
The sample size was calculated using the formula for cross-sectional study [Z2p(1−p)/d2]. Using a proportion (p) of 25% of the consumers with adequate knowledge of antibiotic uses obtained from a study by Mboya et al (2020),20 the confidence level of 95% (Z = 1.96) and precision (d) of 5%, a minimum sample size of 288 antibiotic consumers was obtained. Considering 10% to be non-respondents, a total of 320 antibiotic consumers was obtained. To get the most significant representation of the community, 320 consumers were assessed from public hospitals, 320 from private hospitals and 320 from the marketplaces to reach a target of 960 participants. In each setting, participants were recruited using a convenience sampling technique.
Data collection
A questionnaire comprised of two sections was used to collect data. Section A collected sociodemographic characteristics of the participants, including age, gender, marital status, residence, health insurance status, educational level, employment status and data collection setting. Section B contained two parts of the WHO-validated questions that assessed the consumers’ knowledge of appropriate uses of antibiotics.20
Part I consisted of three questions that were analysed individually. Respondents who answered correctly for all three questions were regarded as having good knowledge of the uses of antibiotics. Part II asked whether consumers know if antibiotics can or cannot be used to treat the following nine infections: malaria, sore throat, influenza, diarrhoea, headache, body aches, fever, infected skin wounds and urinary tract infections (UTIs). A participant was regarded as having good knowledge of treatable conditions using antibiotics if he/she managed to answer a minimum of four conditions correctly.
Data analysis
Data were entered in an MS Excel sheet and transferred to SPSS version 25 (IBM SPSS Statistics for Windows, Version 25.0, released 2017; IBM Corp., Armonk, NY, USA) for data cleaning and analysis. Results were summarized using frequency and percentages. A binary logistic regression model was used to check for the determinants of the consumers’ knowledge of antibiotic uses and conditions that can be treated with antibiotics. A P value of <0.05 was considered statistically significant.
Ethical considerations
Ethical clearance was granted by the director of research and publication ethics committee of Muhimbili University of Health and Allied Sciences (MUHAS). Permission to conduct the study was sought from the respective hospitals and markets administration before commencement of data collection. The purpose of the study was explained to every participant and informed written consent was obtained: i.e. an individual purchased an antibiotic, the drug dispenser informed the clients of the ongoing study (for hospital settings) and directed the patient to the room that was used for data collection within the pharmacy building. After obtaining informed consent, face-to-face interviews were conducted using a Swahili version of the questionnaire.
Data availability
The dataset generated and/or analysed during the current study is available from the corresponding author upon reasonable request.
Results
Out of 960 respondents, 494 (51.5%) were female and 559 (58.2%) were married. More than a third (344, 35%) of the participants had primary education, 457 (47.6%) were self-employed and the majority (568, 59.2%) were not covered by health insurance (Table 1).
Table 1.
Demographic characteristics of the respondents and area of recruitment (n = 960)
| Variables | n (%) |
|---|---|
| Gender | |
| Male | 466 (48.5) |
| Female | 494 (51.5) |
| Age | |
| 18–35 | 539 (56.1) |
| 36–55 | 333 (34.7) |
| >55 | 88 (9.2) |
| Marital status | |
| Married | 559 (58.2) |
| Unmarried | 401 (41.8) |
| Residence | |
| Urban | 736 (76.7) |
| Semi-urban | 224 (23.3) |
| Employment | |
| Self-employed | 457 (47.6) |
| Employed | 278 (29.0) |
| Unemployed | 225 (23.4) |
| Education level | |
| Primary | 344 (35.8) |
| Secondary | 328 (34.2) |
| Tertiary | 288 (30.0) |
| Health insurance status | |
| Yes | 392 (40.8) |
| No | 568 (59.2) |
| Place of recruitment | |
| Community | 320 (33.3) |
| Public hospitals | 320 (33.3) |
| Private hospitals | 320 (33.3) |
Knowledge of the rational use of antibiotics
In total, 406 (42%) of the antibiotic consumers responded it is okay to use the same antibiotic if a friend or family member had used it previously to treat similar signs and symptoms. More than half (515, 53.6%) of respondents said it is okay to request the same antibiotic if it helped you treat the same symptoms/disease previously. The majority (678, 70.6%) replied that they stop using antibiotics after finishing the dose indicated. Generally, 196 (20.4%) of the consumers had adequate knowledge of the uses of antibiotics (Table 2).
Table 2.
Consumers’ knowledge of the uses of antibiotics (n = 960)
| Variable | n (%) |
|---|---|
| Do you think it is good to use the same antibiotic if a friend or family member used it to treat the same symptom or disease before? | |
| Yes | 406 (42.3) |
| No | 517 (53.8) |
| I don’t know | 37 (3.9) |
| Do you think it is good to ask/request the same antibiotic if it helped you treat the same symptoms/disease previously? | |
| Yes | 515 (53.6) |
| No | 429 (44.7) |
| I don’t know | 16 (1.7) |
| When do you think you should stop taking antibiotics once you have started treatment? | |
| When I finish the dose as directed | 678 (70.6) |
| When I feel better | 251 (26.2) |
| I don’t know | 31 (3.2) |
| Overall knowledge | |
| Good | 196 (20.4) |
| Poor | 764 (79.6) |
Consumers’ knowledge of conditions that can be managed using antibiotics
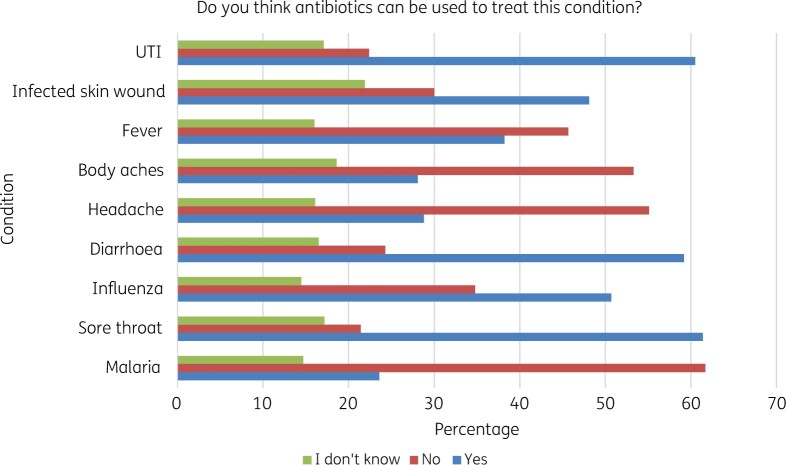
The participants responded that the following conditions could be treated using antibiotics: UTI 581 (60.5%), infected skin wound 462 (48.1%), fever 367 (38.2%), diarrhoea 568 (59.2%), influenza 487 (50.7%) and sore throat 589 (61.4%). In total, 592 (62%) and 511 (53.3%) of the respondents said antibiotics could not treat malaria and body aches, respectively. Overall, 503 (52.4%) of the respondents had good and 457 (47.6%) poor knowledge of the conditions treated with antibiotics (Figure 1).
Figure 1.
Response of the respondents on conditions that are treatable using antibiotics (n = 960).
Determinants of consumers’ knowledge of the uses of antibiotics
Following binary logistic regression, participants with secondary education [adjusted OR (aOR)=1.5, 95% CI = 1.01–2.38, P = 0.04], unemployed (aOR = 1.5, 95% CI = 1.03–2.33, P = 0.04) and those who attended public hospitals (aOR = 1.92, 95% CI = 1.21–3.04, P = 0.005) were more likely to have low knowledge of antibiotic uses, and the differences were statistically significant. Gender, age, marital status, health insurance status and residence showed no effect on the level of knowledge of antibiotic uses among the consumers following multivariate binary logistic regression analysis (Table 3).
Table 3.
Determinants of consumers’ knowledge of the uses of antibiotics (n = 960)
| Variables | cOR (95% CI) | P value | aOR (95% CI) | P value |
|---|---|---|---|---|
| Gender | ||||
| Male | 0.98 (0.72–1.33) | 0.89 | 1 (0.75–1.44) | 0.79 |
| Female | 1 | 1 | ||
| Age | ||||
| 18–35 | 0.5 (0.22–1.03) | 0.06 | 1.84 (0.81–4.16) | 0.14 |
| 36–55 | 1.5 (1.06–2.13) | 0.02 | 1.2 (0.80–1.82) | 0.38 |
| >55 | 1 | 1 | ||
| Marital status | ||||
| Married | 1.2 (0.88–1.65) | 0.25 | 1.1 (0.77–1.58) | 0.58 |
| Unmarried | 1 | 1 | ||
| Residence | ||||
| Urban | 1 (0.72–1.52) | 0.81 | 1.1 (0.93–1.59) | 0.72 |
| Semi-urban | 1 | 1 | ||
| Employment | ||||
| Self employed | 1 | 1 | ||
| Employed | 1.2 (0.72–1.85) | 0.55 | 1.5 (0.93–2.50) | 0.1 |
| Unemployed | 1.6 (1.12–2.44) | 0.01 | 1.5 (1.03–2.33) | 0.04 |
| Education level | ||||
| Primary | 1.09 (0.72–1.64) | 0.68 | 1.2 (0.76–2.04) | 0.4 |
| Secondary | 1.6 (1.08–2.33) | 0.02 | 1.5 (1.01–2.38) | 0.04 |
| Tertiary | 1 | 1 | ||
| Health insurance status | ||||
| Yes | 1.2 (0.90–1.70) | 0.19 | 0.9 (0.64–1.39) | 0.76 |
| No | 1 | 1 | ||
| Place of recruitment | ||||
| Community | 1.3 (0.92–1.90) | 0.14 | 1.7 (0.82–1.82) | 0.34 |
| Public hospitals | 2.12 (1.37–3.25) | 0.001 | 1.92 (1.21–3.04) | 0.005 |
| Private hospitals | 1 | 1 | ||
cOR, crude OR; aOR, adjusted OR.
Determinants of consumers’ knowledge of conditions that are treated with antibiotics
Following binary logistic regression analysis, gender, residence and marital status showed no association with the consumers’ knowledge of conditions that can be treated using antibiotics. Consumers with primary education were about two times more likely to have poor knowledge than those with tertiary education (aOR = 1.77, 95% CI = 1.19–2.61, P = 0.004). Respondents from the community markets and public hospitals were 1.67 and 1.46 times more likely to have poor knowledge of conditions that are treated with antibiotics compared with those who attended private hospitals (aOR = 1.67, 95% CI = 1.18–2.36, P = 0.004 and aOR = 1.46, 95% CI = 1.03–2.08, P = 0.03, respectively). Good knowledge of the conditions that are treatable with antibiotics was significantly associated with age and health insurance. Those aged between 26 and 35 years were 1.72 times more likely to have good knowledge compared with those >55 years (aOR = 1.72, 95% CI = 1.25–2.36, P = 0.001); individuals with health insurance were 1.69 times more likely to have good knowledge compared with those with no insurance (aOR = 1.69, 95% CI = 1.24–2.32, P = 0.001) (Table 4).
Table 4.
Determinants of good knowledge of conditions that are treatable with antibiotics among consumers of antibiotics (n = 960)
| Variables | cOR (95% CI) | P value | aOR (95% CI) | P value |
|---|---|---|---|---|
| Gender | ||||
| Male | 0.88 (0.68–1.14) | 0.35 | 0.84 (0.64–1.09) | 0.19 |
| Female | 1 | 1 | ||
| Age | ||||
| 18–35 | 1.98 (1.23–3.19) | 0.01 | 1.57 (0.94–2.63) | 0.09 |
| 36–55 | 1.69 (1.28–2.24) | 0.00 | 1.72 (1.25–2.36) | 0.001 |
| >55 | 1 | 1 | ||
| Marital status | ||||
| Married | 0.64 (0.49–0.83) | 0.001 | 0.75 (0.56–1.01) | 0.05 |
| Unmarried | 1 | 1 | ||
| Residence | ||||
| Urban | 1.06 (0.78–1.43) | 0.72 | 1.05 (0.76–1.44) | 0.77 |
| Semi-urban | 1 | 1 | ||
| Employment | ||||
| Employed | 1.64 (1.15–2.34) | 0.01 | 1.39 (0.95–2.04) | 0.09 |
| Unemployed | 1.17 (0.87–1.59) | 0.28 | 0.97 (0.70–1.35) | 0.88 |
| Self-employed | 1 | 1 | ||
| Education level | ||||
| Primary | 2.01 (1.46–2.76) | 0.00 | 1.77 (1.19–2.61) | 0.004 |
| Secondary | 1.10 (0.79–1.52) | 0.55 | 0.93 (0.65–1.33) | 0.68 |
| Tertiary | 1 | 1 | ||
| Health insurance status | ||||
| Yes | 2.00 (1.54–2.61) | 0.00 | 1.69 (1.24–2.32) | 0.001 |
| No | 1 | 1 | ||
| Place of recruitment | ||||
| Community | 2.17 (1.58–2.98) | 0.00 | 1.67 (1.18–2.36) | 0.004 |
| Public hospitals | 1.65 (1.20–2.26) | 0.002 | 1.46 (1.03–2.08) | 0.03 |
| Private hospitals | 1 | 1 | ||
cOR, crude OR; aOR, adjusted OR.
Discussion
WHO highlighted several measures to fight AR worldwide, including raising the community level of knowledge of the rational use of antibiotics. To design and formulate interventions accordingly, understanding the baseline knowledge of the community is of importance. This study aimed to assess the level of knowledge and its determinants among consumers of the rational uses of antibiotics in Dar es Salaam, Tanzania.
Generally, the study found that the majority (79.6%) of respondents had inadequate knowledge of the uses of antibiotics. Specifically, 42.3% and 53.6% of the consumers responded that it is okay to use/request the same antibiotics if a friend or family member previously used them or it helped to treat the same symptom or disease, respectively. Also, 70.6% of the respondents said they stopped using antibiotics after finishing the dose as directed. Regarding the knowledge of conditions that are treatable using antibiotics, 52.4% demonstrated good knowledge. Most respondents said it is okay to use antibiotics to treat sore throat (61.4%) and influenza (50.7%) despite the conditions being viral diseases. However, a satisfactory (60.5%) number of consumers know that UTIs are treated using antibiotics and a good proportion agreed that body aches (53.3%) and malaria (60.5%) are not treatable using antibiotics. Respondents with tertiary education, with health insurance, who were employed and who attended private health facilities demonstrated good knowledge of the uses of antibiotics and conditions that can be treated using antibiotics.
Studies conducted in developing countries like Tanzania, Ethiopia, Nepal and Jordan on knowledge of antibiotic use among consumers reported similar findings.15,20–22 However, studies conducted in developed countries like Norway and Sweden reported that the majority of consumers have moderate to high knowledge.23,24 The observed inconsistency could be due to differences in respondents’ socioeconomic status. Low knowledge of antibiotic use observed in developing countries could be attributed to the lack of awareness campaigns and the fact that the majority have no formal education. Lack of formal education and having primary and secondary education levels have been associated with having poor knowledge of antibiotic uses among consumers in developing countries.2,16,21,25
The current study demonstrated that a significant number of respondents reported that it is okay to use/request the same antibiotics if a friend or family member had used them or it helps him/her to treat the same symptom or disease as previously. Uses of antibiotics without medical consultation have been reported in many places and are among the contributors to AR.26,27 Unfortunately, most consumers believe that antibiotics are ‘wonder drugs’ that can cure any diseases.11 Studies around the region report a misunderstanding within the community, particularly with respiratory diseases. People believe that antibiotics help to accelerate healing from conditions like cough and sore throat, which primarily are due to viral infection.28
Although self-medication has its own advantages, the approach has been associated with the emergence and spread of AR.29,30 Due to weak regulatory systems, poor availability of medicine in healthcare facilities and the distance from residences to health facilities, the majority of people in developing countries depend on private drug outlets as the place for getting healthcare services.31,32 Unfortunately, studies show that private drug outlets embrace self-medication.33–35 In 2011 and 2013, studies conducted in Riyadh and Jeddah reported that 77.6% and 97.9% of the community pharmacies dispense antibiotics to consumers without a prescription.36,37 Most of the dispensers in private outlets have inadequate knowledge of the pharmacology of antibiotics, which is likely to contribute to irrational dispensing. In order to curb the emerging challenge of antibiotic overuse and misuse by the community in Tanzania, the regulatory authority introduced a guideline that each community outlet should have a prescription book to record the dispensed antibiotics. However, this approach has been ineffective due to weak supervision and inspection capacity of the authorities, hence the self-medication practice has not changed.
Besides, a satisfactory (60.5%) number of consumers know that UTI is treated using antibiotics. UTI is one of the infections that affect people living in low-income countries, especially women.38Escherichia coli is the main bacteria causing UTI and is among the three bacterial agents listed by WHO as a threat to public health.5 The remaining common ones are Klebsiella pneumoniae and S. aureus.5 Studies conducted around the East African region show that most isolated clinical isolates of E. coli were resistant to the standard antibiotics used as a first- or second-line regimen.6,7 The high level of resistance demonstrated indicates that patients use antibiotics frequently to manage the condition, which could be the reason why most of the consumers are knowledgeable on the uses of antibiotics in the treatment of UTI.
The study also demonstrated that a good proportion of consumers agreed that antibiotics could not treat body aches (53.3%) and malaria (60.5%). These findings differ from what was reported in a study conducted in the Northern Zone, Tanzania, whereby 68.4% of the respondents agreed that antibiotics could be used to treat malaria.20 The difference in the study settings, sample size and prevalence of malaria between Dar es Salaam and Kilimanjaro could be reasons for the observed discrepancy. Several studies conducted in the malaria-endemic region to assess consumers’ behaviour towards the uses of antimalarial drugs reported that most patients visit community drug outlets to purchase the medication without medical consultation. The studies described further that because people living in the malaria-endemic region get malaria repeatedly, their level of awareness on drugs used to manage malaria is high.39 However, 39.5% still believe that antibiotics can be used to treat malaria, which signifies the importance of raising community awareness on the rational uses of antibiotics.
Again, the study demonstrated that respondents with a tertiary education level, having health insurance, who are employed and who attended private hospitals were more likely to have more knowledge of the uses of antibiotics and conditions that are treatable with antibiotics. Similar findings were reported in Tanzania in 2017 and 2020, in which those with tertiary education levels had good knowledge of antibiotic uses. Mboya et al. (2020)20 reported that those with health insurance had good knowledge of antibiotic uses. Studies conducted in other developing countries (Trinidad and Tobago, Nepal) and a developed country (Norway) reported similar findings.21–23 Usually, education increases the level of understanding and changes the attitude and practice of most individuals. A study conducted in Portugal on the knowledge of students of antibiotics reported that a lack of formal education on the subject of interest can be a contributing factor.40 Nevertheless, in developing countries, most individuals with health insurance are employed and are also more likely to have high education. Besides, to avoid traffic in public hospitals, most individuals with health insurance opt to obtain health services from private health facilities.
The strength of the study is that it assessed a large number of antibiotic consumers from different catchment points (market vendors and antibiotic consumers in public and private hospitals). Also, the study adopted a validated WHO tool for assessing consumers’ knowledge of rational antibiotic uses. Lastly, filling out the questionnaire was supervised by an investigator for the purpose of offering clarification when it was needed.
Despite the strengths, because the study was cross-sectional it cannot establish any causal relationship between the variables. Since some of the respondents were exiting outpatients’ pharmacies in the hospitals with antibiotic prescriptions, this might have exaggerated the reported level of knowledge.
Conclusions
The majority of consumers had poor knowledge of the rational uses of antibiotics and a moderate proportion had good knowledge of conditions that are treatable with antibiotics. Those with a high level of education and health insurance demonstrated good knowledge of the rational uses of antibiotics. This study recommends that interventions are needed to raise the level of knowledge of the community of rational uses of antibiotics as a measure to fight AR.
Acknowledgements
We would like to thank medical officers in-charge of both private and public hospitals and the head of the retail markets in Ilala Municipality for providing permission to conduct this study. Moreover, much appreciation is offered to all participants in all visited data collection settings.
Funding
This study was supported by internal funding.
Transparency declarations
None to declare.
Author contributions
S.G. and M.K. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: S.G., L.M., O. Mkusa, M.K., W.P.M., H.J.M., A.I.M. and R.F.M. Acquisition, analysis or interpretation of data: S.G., L.M., O. Minzi, R.F.M. and M.K. Drafting the manuscript: M.K. Critical revision of the manuscript for important intellectual content: all authors. All authors read and approved the final manuscript.
References
- 1. The Review on Antimicrobial Resistance. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. 2016. https://amr-review.org/sites/default/files/160518_Final%20paper_with%20cover.pdf.
- 2. Sindato C, Mboera LEG, Katale BZ. et al. Knowledge, attitudes and practices regarding antimicrobial use and resistance among communities of Ilala, Kilosa and Kibaha districts of Tanzania. Antimicrob Resist Infect Control 2020; 9: 194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Minzi OM, Kilonzi M, Mikomangwa WP. et al. Update on bacterial and antibiotic susceptibility profiles among patients attending a tertiary referral hospital in Tanzania. J Glob Antimicrob Resist 2021; 25: 87–8. [DOI] [PubMed] [Google Scholar]
- 4. Mikomangwa WP, Bwire GM, Kilonzi M. et al. The existence of high bacterial resistance to some reserved antibiotics in tertiary hospitals in Tanzania: a call to revisit their use. Infect Drug Resist 2020; 13: 1831–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wangai FK, Masika MM, Lule GN. et al. Bridging antimicrobial resistance knowledge gaps: the East African perspective on a global problem. PLoS One 2019; 14: e0212131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Maina D, Makau P, Nyerere A. et al. Antimicrobial resistance patterns in extended-spectrum β-lactamase producing Escherichia coli and Klebsiella pneumoniae isolates in a private tertiary hospital, Kenya. Microbiol Discov 2013; 1: 5. [Google Scholar]
- 7. Musicha P, Cornick JE, Bar-Zeev N. et al. Trends in antimicrobial resistance in bloodstream infection isolates at a large urban hospital in Malawi (1998–2016): a surveillance study. Lancet Infect Dis 2017; 17: 1042–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chilongola J, Msoka E, Juma A. et al. Antibiotics prescription practices for provisional malaria cases in three hospitals in Moshi, northern Tanzania. Tanzania J Health Res 2017; 17: 1–10. [Google Scholar]
- 9. Irunde H, Minzi O, Moshiro C.. Assessment of rational medicines prescribing in healthcare facilities in four regions of Tanzania. J Pharm Pract Community Med 2017; 3: 225–31. [Google Scholar]
- 10. Viberg N, Kalala W, Mujinja P. et al. “Practical knowledge” and perceptions of antibiotics and antibiotic resistance among drug sellers in Tanzanian private drugstores. BMC Infect Dis 2010; 10: 270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jairoun A, Hassan N, Ali A.. Knowledge, attitude and practice of antibiotic use among university students: a cross sectional study in UAE. BMC Public Health 2019; 19: 518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Valimba R, Liana J, Joshi MP. et al. Engaging the private sector to improve antimicrobial use in the community: experience from accredited drug dispensing outlets in Tanzania. J Pharm Policy Pract 2014; 7: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Minzi OM, Manyilizu VS.. Application of basic pharmacology and dispensing practice of antibiotics in accredited drug-dispensing outlets in Tanzania. Drug Healthc Patient Saf 2013; 5: 5–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. World Bank Group. Pulling Together to Beat Superbugs: Knowledge and Implementation Gaps in Addressing Antimicrobial Resistance. 2019. https://www.worldbank.org/en/topic/agriculture/publication/pulling-together-to-beat-superbugs-knowledge-and-implementation-gaps-in-addressing-antimicrobial-resistance.
- 15. Jifar A, Ayele Y.. Assessment of knowledge, attitude, and practice toward antibiotic use among Harar City and its surrounding community, Eastern Ethiopia. Interdiscip Perspect Infect Dis 2018; 2018: 8492740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mbwambo G, Emidi B, Mgabo MR. et al. Community knowledge and attitudes on antibiotic use in Moshi Urban, Northern Tanzania: findings from a cross sectional study. Afr J Microbiol Res 2017; 11: 1018–26. [Google Scholar]
- 17. Earnshaw S, Mendez A, Monnet DL. et al. Global collaboration to encourage prudent antibiotic use. Lancet Infect Dis 2013; 13: 1003–4. [DOI] [PubMed] [Google Scholar]
- 18. Earnshaw S, Mancarella G, Mendez A. et al. European Antibiotic Awareness Day: a five-year perspective of Europe-wide actions to promote prudent use of antibiotics. Euro Surveill 2014; 19: pii=20928. [DOI] [PubMed] [Google Scholar]
- 19. 2012 Population and Housing Census. National Bureau of Statistics, United Republic of Tanzania; 2013. http://tanzania.countrystat.org/fileadmin/user_upload/countrystat_fenix/congo/docs/Census%20General%20Report-2012PHC.pdf.
- 20. Mboya EA, Davies ML, Horumpende PG. et al. Inadequate knowledge on appropriate antibiotics use among clients in the Moshi municipality Northern Tanzania. PLoS One 2020; 15: e0239388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nepal A, Hendrie D, Robinson S. et al. Knowledge, attitudes and practices relating to antibiotic use among community members of the Rupandehi District in Nepal. BMC Public Health 2019; 19: 1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shehadeh M, Suaifan G, Darwish RM. et al. Knowledge, attitudes and behavior regarding antibiotics use and misuse among adults in the community of Jordan. A pilot study. Saudi Pharm J 2012; 20: 125–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Waaseth M, Adan A, Røen IL. et al. Knowledge of antibiotics and antibiotic resistance among Norwegian pharmacy customers – a cross-sectional study. BMC Public Health 2019; 19: 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. André M, Vernby A, Berg J. et al. A survey of public knowledge and awareness related to antibiotic use and resistance in Sweden. J Antimicrob Chemother 2010; 65: 1292–6. [DOI] [PubMed] [Google Scholar]
- 25. Gebeyehu E, Bantie L, Azage M.. Inappropriate use of antibiotics and its associated factors among urban and rural communities of Bahir Dar City Administration, Northwest Ethiopia. PLoS One 2015; 10: e0138179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shafie M, Eyasu M, Muzeyin K. et al. Prevalence and determinants of self-medication practice among selected households in Addis Ababa community. PLoS One 2018; 13: e0194122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rather IA, Kim B-C, Bajpai VK. et al. Self-medication and antibiotic resistance: crisis, current challenges, and prevention. Saudi J Biol Sci 2017; 24: 808–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gaarslev C, Yee M, Chan G. et al. A mixed methods study to understand patient expectations for antibiotics for an upper respiratory tract infection. Antimicrob Resist Infect Control 2016; 5: 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fainzang S. Managing medicinal risks in self-medication. Drug Saf 2014; 37: 333–42. [DOI] [PubMed] [Google Scholar]
- 30. Panda A, Pradhan S, Mohapatra G. et al. Drug-related problems associated with self-medication and medication guided by prescription: a pharmacy-based survey. Indian J Pharmacol 2016; 48: 515–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Goel P, Ross-Degnan D, Berman P. et al. Retail pharmacies in developing countries: a behavior and intervention framework. Soc Sci Med 1996; 42: 1155–61. [DOI] [PubMed] [Google Scholar]
- 32. Kwena Z, Sharma A, Wamae N. et al. Provider characteristics among staff providing care to sexually transmitted infection self-medicating patients in retail pharmacies in Kibera slum, Nairobi, Kenya. Sex Transm Dis 2008; 35: 480–3. [DOI] [PubMed] [Google Scholar]
- 33. Horumpende PG, Said SH, Mazuguni FS. et al. Prevalence, determinants and knowledge of antibacterial self-medication: a cross sectional study in North-eastern Tanzania. PLoS One 2018; 13: e0206623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lansang MA, Lucas-Aquino R, Tupasi TE. et al. Purchase of antibiotics without prescription in Manila, the Philippines. Inappropriate choices and doses. J Clin Epidemiol 1990; 43: 61–7. [DOI] [PubMed] [Google Scholar]
- 35. Desalegn AA. Assessment of drug use pattern using WHO prescribing indicators at Hawassa University Teaching and Referral Hospital, south Ethiopia: a cross-sectional study. BMC Health Serv Res 2013; 13: 170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bin Abdulhak AA, Al Tannir MA, Almansor MA. et al. Non prescribed sale of antibiotics in Riyadh, Saudi Arabia: a cross sectional study. BMC Public Health 2011; 11: 538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Al-Mohamadi A, Badr A, Bin Mahfouz L. et al. Dispensing medications without prescription at Saudi community pharmacy: extent and perception. Saudi Pharm J 2013; 21: 13–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Stamm WE, Norrby SR.. Urinary tract infections: disease panorama and challenges. J Infect Dis 2001; 183 Suppl 1: S1–4. [DOI] [PubMed] [Google Scholar]
- 39. Watsierah CA, Jura WG, Raballah E. et al. Knowledge and behaviour as determinants of anti-malarial drug use in a peri-urban population from malaria holoendemic region of western Kenya. Malar J 2011; 10: 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Azevedo MM, Pinheiro C, Yaphe J. et al. Portuguese students' knowledge of antibiotics: a cross-sectional study of secondary school and university students in Braga. BMC Public Health 2009; 9: 359. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset generated and/or analysed during the current study is available from the corresponding author upon reasonable request.