Abstract
Early studies suggest that adults with mental health conditions are at greater risk for COVID-19 infection, severe complications, and higher mortality, yet face barriers in accessing timely health services. Data from the Census Bureau's Household Pulse Survey, a large, nationally representative survey fielded from March 17–29, 2021 (n = 77,104) were analyzed to examine COVID-19 vaccination and intention among adults with mental health symptoms. Separate multivariable regression models were conducted to examine associations between symptoms of anxiety, depression, and anxiety or depression on vaccine receipt (≥ 1 dose) and intention to be vaccinated. Reasons for not being vaccinated were also assessed. Approximately 35% of adults had symptoms of anxiety or depression. This population was less likely to receive COVID-19 vaccination (adjusted prevalence ratio (aPR) = 0.94, 95%CI: 0.91–0.98) but more likely to intend to get a vaccine (aPR = 1.13, 95%CI: 1.08–1.19) than those without these conditions. Females with mental health symptoms were less likely to receive a COVID-19 vaccination but more likely to intend to get vaccinated, while there were fewer significant associations between mental health symptoms and vaccination coverage and intentions to vaccinate among males. Reasons for not getting vaccinated, including concerns about possible vaccine side effects, efficacy, cost, dislike of vaccines, as well as lack of trust in the government and vaccines, were all greater among those with any symptoms of anxiety or depressive disorders than those without symptoms. Efforts are needed to increase vaccination uptake and confidence among this vulnerable population by increasing vaccine confidence and addressing concerns about the vaccine.
Keywords: COVID-19 vaccine, Vaccine hesitancy, Vaccine confidence, Mental health conditions, Anxiety, Depression, Disparities
1. Introduction
Early studies suggest that adults with mental health or psychiatric disorders are at greater risk for COVID-19 infection, severe complications, and higher mortality (Cipriani et al., 2021; Wang et al., 2021; Nemani et al., 2021). During the COVID-19 pandemic, the prevalence of depressive symptoms increased by more than 3-fold compared to before the pandemic, and the percentage of adults with symptoms of an anxiety or depressive disorder increased from 36% to 42% from August 2020 to February 2021 (Ettman et al., 2020; Estimates of Mental Health Symptomatology, by Month of Interview: United States, 2019; Symptoms of Generalized Anxiety Disorder Among Adults: United States, 2019; Symptoms of Depression Among Adults: United States, 2019; Vahratian et al., 2021; Anxiety and Depression, 2021; Cai et al., 2021; Twenge and Joiner, 2020). People with existing mental health conditions may have experienced relapses or worsening of symptoms due to increased stressors, lack of access to regular psychosocial treatments, and unmet mental health care needs (Yao et al., 2020; Pfefferbaum and North, 2020). Some people may be more vulnerable to the psychosocial effects of the pandemic than others, such as people who contract COVID-19, those at increased risk for the disease, and people with preexisting medical, psychiatric, or substance use problems (Rajkumar, 2020).
There have been several calls for the prioritization of COVID-19 vaccines for those with psychiatric disorders and mental illness because of their greater risk of infection and related morbidity and mortality (Mazereel et al., 2021; Stip et al., 2021; Siva, 2021). Scientists have described patients with severe mental illness as among the most vulnerable populations affected by the COVID-19 pandemic (Druss, 2020). Reasons for the disproportionate burden of COVID-19 among those with mental illness include both increased exposure to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus responsible for COVID-19, and barriers to health service utilization. For example, persons with mental illness may have cognitive impairment, limited awareness of risk, and reduced efforts regarding personal protection, which places them at higher risk for infection (Mazereel et al., 2021). Second, if individuals with these disorders are infected, they may experience greater barriers to accessing timely health services due to stigmatization and other barriers as a result of levels of education, income and being uninsured (Kahl and Correll, 2020). Studies found that less than half of those who need mental health services get them, possibly due to cost, availability, acceptability or access (Steele et al., 2007). Third, state and national regulations on travel, lockdown/stay at home advisories, and quarantine have made access to regular outpatient visits for evaluations and prescriptions more difficult for people with mental health conditions (Kahl and Correll, 2020; Steele et al., 2007). Fourth, people with mental health conditions may need extra support during the pandemic; however, this may not be possible due to social distancing, quarantine, and other prevention measures. These barriers contribute to disparities in healthcare utilization and prevention services, which are often overlooked in this marginalized population, and may result in increased risk for exposure and adverse outcomes from COVID-19.
Since the COVID-19 vaccine became available in December 2020, people with mental health conditions may have comorbidities that prioritized them for the COVID-19 vaccines (Sartorious, 2013; Roca et al., 2009; Dooling et al., 2020; Dooling et al., 2021). However, COVID-19 vaccination receipt and intention to vaccinate among this population are not known. Studies have shown that women are more likely to be treated for mental health symptoms such as anxiety and depression than men (Afifi, 2007; World Health Organization, 2002; Rosenfield and Mouzon, 2013). Furthermore, other studies have shown that women are less likely to receive health services such as COVID-19 vaccinations and testing, particularly in developing countries (https://www.who.int/news/item/03-05-2021-expanding-reach-addressing-gender-barriers-in-covid-19-vaccine-rollout, n.d.). The goal of this study is to examine receipt of ≥1 dose of the COVID-19 vaccine, intention to vaccinate, and reasons for not vaccinating among people with symptoms of anxiety, depression, and anxiety or depression and stratified by sex using data from the Census Bureau's Household Pulse Survey (HPS), which is a large, nationally representative survey that collects data on COVID-19 vaccination coverage and intentions, as well as other social and economic characteristics during the pandemic.
2. Methods
2.1. Survey design
The Household Pulse Survey (HPS), conducted by the U.S. Census Bureau in collaboration with other federal agencies, is a nationally presentative survey of adults ≥18 years using a probability-based sample design. It has been collecting data on household experiences during the COVID-19 pandemic since April 2020 and data collection is ongoing. The survey design has been published previously (Fields et al., 2020; https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/Phase%203%20Questionnaire_02.25.21_English.pdf, n.d.; Source of the Data and Accuracy of the Estimates for the Household Pulse Survey – Phase 3, 2021). The sample size for the survey fielded from March 17 to 29, 2021 was 77,104 with a response rate of 7.2% (Source of the Data and Accuracy of the Estimates for the Household Pulse Survey – Phase 3, 2021). This study was reviewed by the Tufts University Health Sciences Institutional Review Board and was not considered to be human subjects research.
2.2. COVID-19 questions
On January 6, 2021, the HPS added questions on COVID-19 vaccination coverage, intent, and reasons for not vaccinating. COVID-19 vaccination receipt (≥1 dose) was assessed with the following question: “Have you received a COVID-19 vaccine?” (yes/no) Among unvaccinated adults, intent to be vaccinated was assessed with the following question: “Once a vaccine to prevent COVID-19 is available to you, would you...definitely, probably, probably not, or definitely not get a vaccine.” Because the question on vaccination intent was only asked of those who were not vaccinated, assessing intent over time would show bias as more people got vaccinated (by reducing the sample size in this group). As a result, vaccination intent was defined as those who were vaccinated, or definitely or probably will get vaccinated. Definite or probable responses were combined into one response because there were no significant differences in the characteristics of respondents who definitely or probably plan to be vaccinated. Among those who had not been vaccinated or did not definitely plan to get vaccinated, respondents were asked reasons for not getting vaccinated: “Which of the following, if any, are reasons that you [probably will/probably won't/definitely won't] get a COVID-19 vaccine”. Response options were: 1) I am concerned about possible side effects of a COVID-19 vaccine, 2) I don't know if a COVID-19 vaccine will work, 3) I don't believe I need a COVID-19 vaccine, 4) I don't like vaccines, 5) My doctor has not recommended it, 6) I plan to wait and see if it is safe and may get it later, 7) I think other people need it more than I do right now, 8) I am concerned about the cost of a COVID-19 vaccine, 9) I don't trust COVID-19 vaccines, 10) I don't trust the government, and 11) Other.
2.3. Symptoms of anxiety and depression
Questions on anxiety and depression were modified from a validated two-item Patient Health Questionnaire (PHQ-2) and the two-item Generalized Anxiety Disorder (GAD-2) scale (Arroll et al., 2010; Plummer et al., 2016). The questions adapted from the PHQ-2 were: 1) “Over the last 7 days, how often have you been bothered by … having little interest or pleasure in doing things? Would you say not at all, several days, more than half the days, or nearly every day?” 2) “Over the last 7 days, how often have you been bothered by … feeling down, depressed, or hopeless? Would you say not at all, several days, more than half the days, or nearly every day?” Questions adapted from the GAD-2 were: “Over the last 7 days, how often have you been bothered by the following problems … Feeling nervous, anxious, or on edge? Would you say not at all, several days, more than half the days, or nearly every day?” 2) “Over the last 7 days, how often have you been bothered by the following problems … Not being able to stop or control worrying? Would you say not at all, several days, more than half the days, or nearly every day?” For each scale, responses were assigned a numerical value: not at all = 0, several days = 1, more than half the days = 2, and nearly every day = 3. The two responses for each scale were summed and a score equal to three or greater on the PHQ-2 was categorized as symptoms of depression (hereafter referred to as depression) (Anxiety and Depression, 2021). A sum equal to three or greater on the GAD-2 was categorized as symptoms of anxiety (hereafter referred to as anxiety) (Anxiety and Depression, 2021). Adults who had either symptoms of anxiety or depression were categorized as having either disorder.
2.4. Sociodemographic variables
Sociodemographic variables assessed were: age group, sex, race/ethnicity, educational status, annual household income, insurance status, and previous COVID-19 diagnosis. Age was categorized as 18–49, 50–64, and ≥ 65 years. Race/ethnicity was categorized as non-Hispanic (NH) white, NH black, Hispanic, NH Asian, and NH other/multiple races. Annual household income was categorized as <$35,000, $35,000–$49,999, $50,000–$74,999, ≥ $75,000, or not reported. Insurance status was defined as having or not having insurance. Previous COVID-19 diagnosis as defined as a “yes” response to the following question: “Has a doctor or other healthcare provider ever told you that you have COVID-19?”
Respondents were also asked about receipt of medical services during the past four weeks. For example, respondents were asked if they needed medical care for something unrelated to coronavirus at any time in the last 4 weeks, but did not get it; if they delayed getting medical care at any time in the last 4 weeks because of the coronavirus pandemic; if they needed counseling or therapy from a medical health professional at any time in the last 4 weeks, but did not get it for any reason; if they received counseling or therapy at any time in the last 4 weeks from a mental health professional such as a psychiatrist, psychologist, psychiatric nurse, or clinical social worker; and if they take prescription medication at any time in the last 4 weeks to help with any emotions or with concentration, behavior or mental health. Response categories for these questions were yes or no.
2.5. Analysis
Socioeconomic characteristics and receipt of medical services among respondents with anxiety, depression, either anxiety or depression, and those without any symptoms were analyzed. Separate multivariable logistic regression models were conducted to examine the association between anxiety, depression, and either disorder on ≥1 dose COVID-19 vaccination receipt and intention to vaccinate, stratified by sex, after controlling for age group, race/ethnicity, educational status, annual household income, insurance status, and previous COVID-19 diagnosis (Bieler et al., 2010). Proportions and 95% confidence intervals (CI) for reasons for not getting vaccinated were examined among those with varying intentions to vaccinate (e.g., probably, probably won't, and definitely won't get a COVID-19 vaccine) and stratified by those with anxiety, depression, either disorder, or none. Contrast tests for the differences in proportions, comparing each category to the referent category were conducted with a 0.05 significance level (α = 0.05). Missing responses contributed to less than 2% of responses of the variables used in this study and were removed from the analyses. Analyses accounted for the survey design and weights to ensure a nationally representative sample using STATA 16.1.
3. Results
Approximately 30%, 25%, and 35% of adults have anxiety, depression, or either disorders, respectively, in March 2021 (Table 1 ). Adults with anxiety or depression were more likely to be younger in age, female, NH Black, Hispanic, or other NH races compared to adults without either of these disorders. Adults with anxiety or depression were also more likely to have low educational attainment, low household incomes, lack health insurance, and either lack or delay medical care during the past four weeks compared with their counterparts. For example, a higher proportion of adults with anxiety or depression needed medical care, counseling, or therapy and did not get it, or had a delay in getting medical care during the past 4 weeks compared to adults who did not have either disorders.
Table 1.
Characteristics of people with mental health symptoms- United States- Household Pulse Survey- March 17–29- 2021.
| Anxiety (n = 16–244) |
Depression (n = 12–615) |
Anxiety or depression (n = 18–948) |
No symptoms (n = 44–731) |
|
|---|---|---|---|---|
| % (95%CI) | % (95%CI) | % (95%CI) | % (95%CI) | |
| All adults (≥18 years) | 30.01 (29.3–30.9)a | 24.7 (23.9–25.4)a | 35.1 (34.4–35.8)a | 64.9 (63.2–65.6) |
| Age groups (in years) | ||||
| 18–49 | 62.6 (61.2–63.9)a | 62.4(60.9- 63.9)a | 61.7 (60.4–63.0)a | 44.3 (43.6–45.1) |
| 50–64 | 23.6 (22.5–24.7)a | 23.4 (22.2–24.7)a | 23.7 (22.7–24.7)a | 28.1 (27.5–28.7) |
| ≥65 | 13.8 (13.0–14.7)a | 14.2 (13.2–15.2)a | 14.6 (13.8–15.5)a | 27.5 (26.9–28.0) |
| Sex | ||||
| Male | 42.0 (40.4–43.7)a | 45.1 (43.3–46.9) | 43.4(42.0–44.8)a | 50.5 (39.7–51.3) |
| Female | 58.0 (56.3–59.6)a | 54.9(53.1–56.7)a | 56.6(55.2–58.0)a | 49.5(48.7–50.3) |
| Race/ethnicity | ||||
| Non-Hispanic white | 62.1 (60.8–63.5)a | 60.6(58.8–62.3)a | 61.8(60.0–63.2)a | 67.3 (66.6–68.1) |
| Non-Hispanic black | 11.0 (10.1–12.0)a | 11.3 (10.2–12.5)a | 11.1 (10.3–12.1)a | 9.9 (9.4–10.4) |
| Hispanic | 18.2 (16.9–19.5)a | 18.1 (16.8–19.6)a | 17.9 (16.8–19.1)a | 14.5 (13.8–15.3) |
| Non-Hispanic Asian | 4.6 (4.0–5.3) | 5.0 (4.3–6.0) | 4.8 (4.2–5.5) | 5.2 (4.9–5.6) |
| Non-Hispanic other/multiple races | 4.1 (3.6–4.6)a | 4.9 (4.9–5.5)a | 4.3 (3.9–4.7)a | 3.1 (2.8–3.3) |
| Educational status | ||||
| High school or less | 38.0 (36.4–39.7)a | 39.5 (37.8–41.2) a | 37.9 (36.5–39.3)a | 35.6 (34.7–36.5) |
| Some college or college graduate | 50.1 (49.3–52.1)a | 51.5 (50.0–53.0)a | 51.1 (49.9–52.3)a | 47.9 (47.1–48.7) |
| Above college graduate | 11.2 (10.7–11.8)a | 9.0 (8.5–9.6)a | 11.0 (10.5–11.4)a | 16.5 (16.1–17.0) |
| Annual household income | ||||
| <$35–000 | 30.0 (28.7–31.4)a | 31.5 (30.0–33.0)a | 29.8 (28.4–31.2)a | 18.4 (17.6–19.2) |
| $35–000-$49–999 | 11.9 (11.1–12.7)a | 12.4 (11.5–13.4)a | 11.9 (11.3–12.7)a | 10.2 (9.6–10.8) |
| $50–000-$74–999 | 16.8 (15.7–17.9) | 17.0 (15.8–18.3) | 16.8 (15.8–17.9) | 16.4 (15.7–17.1) |
| ≥$75–000 | 29.5 (28.3–30.8)a | 27.3 (25.9–28.7)a | 29.7 (18.4–30.7)a | 44.8 (43.9–45.7) |
| Did not report | 11.8 (10.7–13.0) | 11.9 (10.7–13.1)a | 11.9 (10.9–13.0)a | 10.2 (9.7–10.8) |
| Insurance status | ||||
| Insured | 87.2 (86.2–88.2)a | 86.8 (85.6–88.0)a | 87.7 (86.7–88.6)a | 92.4 (91.6–93.1) |
| Not insured | 12.8 (11.8–13.8)a | 13.2 (12.0–14.4)a | 12.2 (11.4–13.3)a | 7.6 (6.9–8.4) |
| Previous COVID-19 diagnosis | ||||
| Yes | 14.3 (13.4–15.2)a | 14.0 (13.0–15.0) | 13.9 (13.1–14.7) | 12.9 (12.2–13.6) |
| No | 84.6 (83.7–85.5)a | 84.6 (83.5–85.6)a | 85.0 (84.1–85.8)a | 86.4 (85.7–87.1) |
| Not sure | 1.1 (0.8–1.5) | 1.4 (1.0–2.0)a | 1.1 (0.8–1.5) | 0.7 (0.5–0.9) |
| Need medical care for something unrelated to coronavirus- but did not get it | 33.0 (31.5–34.6)a | 35.4 (33.4–37.5)a | 32.2 (30.6–33.7)a | 12.4 (11.8–13.1) |
| Delay getting medical care because of the coronavirus pandemic | 40.7 (39.3–42.2)a | 42.8 (41.1–44.7)a | 39.9 (38.6–41.3)a | 17.1 (16.4–17.8) |
| Needed counseling or therapy from a mental health professional- but did not get it for any reason | 26.8 (25.4–28.3)a | 29.7 (28.1–31.5)a | 25.3 (24.0–26.6)a | 3.6 (3.2–4.1) |
| Receive counseling or therapy from a mental health professional such as a psychiatrist- psychologist- psychiatric nurse- or clinical social worker | 19.1 (18.0–20.2)a | 18.9 (17.9–20.1)a | 18.1 (17.1–19.1)a | 5.9 (5.5–6.3) |
| Take prescription medication to help with any emotions or with concentration- behavior or mental health | 35.8 (34.1–37.4)a | 37.2 (35.4–39.0)a | 34.6 (33.1–36.1)a | 13.1 (12.4–13.7) |
Significant differences in proportions comparing each group to the referent group (no anxiety or depression).
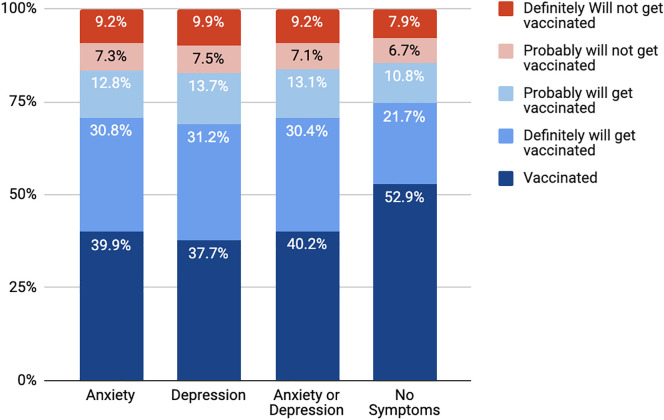
COVID-19 vaccination and intention to vaccinate was lower among adults with anxiety and depression compared to people without these symptoms (Fig. 1 ). A lower proportion of adults with anxiety (39.9%), depression (37.7%), and either disorder (40.2%) received at least 1 dose of the COVID-19 vaccine compared to adults without any symptoms (52.9%). Adults with anxiety or depression were less likely to receive COVID-19 vaccination (adjusted prevalence ratio (aPR) = 0.94, 95%CI: 0.91–0.98) and more likely to intend to get a vaccine (aPR = 1.13, 95%CI: 1.08–1.19) than those without these conditions (Table 2 ). By sex, females with anxiety (aPR) = 0.94, 95%CI: 0.89–0.99), depression aPR = 0.88, 95%CI = 0.83–0.94), or anxiety or depression (aPR = 0.94, 95%CI: 0.89–0.99) were less likely to be vaccinated for COVID-19 than those without any symptoms; males with depression were also less likely to be vaccinated (aPR = 0.91, 95%CI: 0.83–0.99). While females with mental health symptoms had lower vaccination coverage than those without any symptoms, females with mental health symptoms were more likely to intend to be vaccinated. For example, females with anxiety were 1.11 times as likely to intend to be vaccinated (95%CI: 1.06–1.16), those with depression were 1.08 times as likely to intend to be vaccinated (95%CI: 1.03–1.13), and those with anxiety or depression were 1.11 times as likely to be vaccinated (95%CI: 1.06–1.16) than those without the respective symptoms. There were no significant associations between mental health symptoms and vaccination intent among males.
Fig. 1.
COVID-19 vaccination receipt (≥1 dose) and intent to get vaccinated by mental health status- United States- Household Pulse Survey- March 17–29- 2021.
Stacked bar graph of vaccination coverage and willingness to get vaccinated, by those without any symptoms, those with anxiety symptoms, those with depressive symptoms, and those with anxiety or depressive symptoms.
Table 2.
Prevalence of and factors associated with COVID-19 vaccination (≥1 dose), overall and by sex, Household Pulse Survey- March 17–29- 2021.
| COVID-19 vaccination (≥ 1 dose) |
COVID-19 vaccination intenta |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall |
Male |
Female |
Overall |
Male |
Female |
|||||||
| % (95%CI) | aPR (95%CI)b | % (95%CI) | aPR (95%CI)b | % (95%CI) | aPR (95%CI)b | % (95%CI) | aPR (95%CI)b | % (95%CI) | aPR (95%CI)b | % (95%CI) | aPR (95%CI)b | |
| Anxiety | ||||||||||||
| Yes | 39.9 (38.1–41.7)c | 0.94 (0.91–0.98) | 36.2 (33.0–39.5) c | 0.93 (0.85–1.2) | 42.6 (40.7–44.5) c | 0.94 (0.89–0.99) | 43.5 (41.8–45.2)c | 1.13 (1.08, 1.19) | 73.6(70.5–76.5) | 1.03(0.99–1.08) | 71.7(69.2–74.1) c | 1.11 (1.06–1.16) |
| No (reference) | 52.2 (51.2–53.2) | Reference | 49.1 (47.5–50.7) | 55.4 (54.2–56.5) | 33.0 (32.1–34.0) | Reference | 71.8 (69.8–73.8) | 66.5 (64.6–68.3) | ||||
| Depression | ||||||||||||
| Yes | 37.7 (35.8–39.6)c | 0.91 (0.87–0.95) | 34.9 (32.0–38.0) c | 0.91 (0.83–0.99) | 40.0 (37.5–42.5) c | 0.88 (0.83–0.94) | 44.8 (42.9–46.7)c | 1.16 (1.10, 1.22) | 73.2(69.5–76.6) | 1.04 (0.98–1.09) | 71.1(68.4–73.6) c | 1.08(1.03–1.13) |
| No (reference) | 52.0 (51.0–52.9) | Reference | 48.8 (47.4–50.2) | 55.0 (53.9–56.1) | 33.4 (32.6–34.3) | Reference | 72.2(70.2–74.1) | 67.3 (65.6–68.9) | ||||
| Anxiety or depression | ||||||||||||
| Yes | 40.2 (38.6–41.9)c | 0.94 (0.90–0.97) | 36.4(33.6–39.2) c | 0.92 (0.85–1.0) | 43.2 (41.4–45.1) c | 0.94 (0.89–0.99) | 43.4 (41.8–45.0)c | 1.15 (1.10–1.20) | 74.1 (71.0–77.0) | 1.05 (1.00–1.10) | 71.7 (69.4–73.9) c | 1.11 (1.06–1.16) |
| No (reference) | 52.9 (51.9–53.9) | Reference | 50.0 (48.4–51.5) | 55.9(54.8–57.0) | 32.4 (31.4–33.3) | Reference | 71.5 (69.3–73.5) | 66.0 (64.1–67.9) | ||||
Abbreviations: CI = confidence interval; aPR = adjusted prevalence ratio.
Defined as being vaccinated with 1 or more doses, or being definitely or probably likely to get vaccinated.
Separate multivariable regression models assessed symptoms of anxiety- depression- and anxiety or depression on COVID-19 vaccination receipt and intent- adjusting for age group- race/ethnicity- educational status- annual household income- insurance status- and previous COVID-19 diagnosis.
Significant differences in proportions comparing each group to the referent group (no anxiety or depression).
Reasons for not getting vaccinated also differed among those with anxiety, depression, or either disorder (Table 3). Among those who probably will get vaccinated, concerns about side effects and uncertainty about whether the vaccine will work were higher among people with anxiety or depressive symptoms than those without any symptoms (56.9% compared to 47.1%, and 19.6% compared to 13.5%, respectively). Among those who probably will or probably will not get vaccinated, both a lack of trust in COVID-19 vaccines and in the government were higher among people with anxiety or depression compared to people without these disorders. Among people who definitely will not get a vaccine, dislike of vaccines was higher among those with anxiety or depression compared to those without either disorder (24.4% compared to 16.2%, respectively).
Table 3.
Reasons for not getting vaccinated by mental health status and vaccination intent- United States- Household Pulse Survey- March 17–29-2021.
| Anxiety |
Depression |
Anxiety or depression |
No symptoms |
|
|---|---|---|---|---|
| % (95%CI) | % (95%CI) | % (95%CI) | % (95%CI) | |
| Probably | ||||
| Concerned about possible side effects | 58.4 (53.6–63.0)a | 57.0 (52.9–61.1)a | 56.9 (62.8–61.0)a | 47.1 (43.6–50.6) |
| Don't know if a vaccine will work | 20.3 (16.5–24.6)a | 20.5 (16.8–24.9)a | 19.6 (16.4–23.3)a | 13.5 (10.8–16.8) |
| Don't believe I need a vaccine | 4.6 (3.1–6.8) | 5.2 (3.4–7.7) | 4.4 (3.1–6.2) | 6.6 (5.2–8.4) |
| Don't like vaccines | 7.4 (5.7–9.6) | 6.3 (4.6–8.5) | 6.9(5.4–8.8) | 6.0 (4.2–8.4) |
| Doctor has not recommended it | 5.0 (3.6–6.8) | 4.2 (3.0–5.8) | 4.7 (3.5–6.3) | 5.9 (4.5–7.8) |
| Plan to wait and see if it is safe and may get it later | 56.6(52.0–61.1) | 55.9 (51.3–60.5) | 56.7 (52.6–60.7) | 52.0 (49.0–55.0) |
| Other people need it more right now | 37.6 (32.8–42.7) | 35.6 (30.3–41.3) | 36.2 (31.7–40.9) | 36.6 (33.7–39.7) |
| Concerned about the cost | 14.2 (10.2–19.3)a | 13.8 (9.5–19.7)a | 12.9 (9.3–17.7) | 5.0 (3.7–6.7) |
| Don't trust COVID-19 vaccines | 12.8 (10.5–15.3)a | 13.9 (10.9–17.7)a | 13.3 (10.9–16.2)a | 7.3 (5.8–9.1) |
| Don't trust the government | 13.8 (10.8–17.5)a | 15.6 (11.8–20.3)a | 13.9 (10.8–17.9)a | 8.1 (6.4–10.2) |
| Other reason for not getting vaccine | 9.9 (8.1–12.2) | 9.5 (7.1–12.4) | 9.6 (7.8–11.8) | 9.7 (7.9–11.8) |
| Probably not | ||||
| Concerned about possible side effects | 53.6 (48.5–58.5) | 52.8 (47.8–57.8) | 53.9 (49.5–58.2) | 52.8 (48.7–56.9) |
| Don't know if a vaccine will work | 22.5 (18.5–27.0) | 23.4 (19.1–28.4) | 22.1 (18.7–26.0) | 20.7 (18.2–23.4) |
| Don't believe I need a vaccine | 15.9 (12.2–20.4)a | 16.2 (12.4–20.8)a | 16.2 (13.0–20.0)a | 23.6(20.2–27.5) |
| Don't like vaccines | 11.4 (8.2–15.6) | 11.3 (8.3–15.3) | 11.3 (8.4–14.9) | 10.7 (8.7–13.0) |
| Doctor has not recommended it | 7.0 (4.6–10.4) | 6.1 (4.0–9.2) | 6.3 (4.2–9.3) | 7.5 (5.3–10.7) |
| Plan to wait and see if it is safe and may get it later | 54.5 (49.1–59.7) | 55.8 (50.6–60.8) | 55.9 (51.0–60.7) | 56.5 (53.1–59.8) |
| Other people need it more right now | 26.0 (21.9–30.6) | 24.4 (19.8–29.6) | 25.3 (21.4–29.6) | 27.3 (24.2–30.6) |
| Concerned about the cost | 8.9 (6.2–12.5)a | 10.0(7.1-13.8)a | 8.4 (6.1–11.4) a | 3.1 (2.0–4.6) |
| Don't trust COVID-19 vaccines | 26.4 (21.6–31.8) | 2.7 (22.7–32.7) | 27.5 (22.9–32.7)a | 25.3 (22.2–28.7) |
| Don't trust the government | 22.9 (18.6–27.8)a | 20.8 (17.7–25.6) | 21.9 (18.1–26.3)a | 16.8 (14.3–19.7) |
| Other reason for not getting vaccine | 11.4 (8.4–15.4) | 11.9 (8.4–16.5) | 11.6 (8.8–15.2) | 9.1 (8.8–9.3) |
| Definitely not | ||||
| Concerned about possible side effects | 53.3 (47.0–59.4)a | 53.6 (46.5–60.5)a | 51.7(45.8–57.5) | 44.6 (40.3–49.0) |
| Don't know if a vaccine will work | 24.9 (18.0–33.5) | 27.9 (20.5–36.6)a | 24.7(18.6–32.1) | 18.3 (15.6–21.5) |
| Don't believe I need a vaccine | 35.0 (28.5–42.1) | 34.4 (27.7–42.3) | 34.8(28.6–41.4) | 37.4 (33.2–41.8) |
| Don't like vaccines | 24.4 (18.4–31.5)a | 26.2 (19.5–34.3)a | 24.4(19.1–30.6)a | 16.2 (13.3–19.6) |
| Doctor has not recommended it | 8.1 (4.6–14.0) | 8.0 (4.3–14.6) | 7.6 (4.4–12.8) | 3.9 (3.0–5.0) |
| Plan to wait and see if it is safe and may get it later | 21.2 (16.8–26.4) | 20.0 (15.3–25.7) | 20.5 (16.4–25.2) | 17.9 (15.0–21.2) |
| Other people need it more right now | 12.5 (8.1–18.8) | 15.0 (9.5–23.0) | 12.9 (8.5–19.0) | 9.6 (7.4–12.2) |
| Concerned about the cost | 6.1 (2.8–12.6) | 6.9 (3.1–14.5)a | 5.9 (2.9–11.6) | 1.5 (0.7–3.0) |
| Don't trust COVID-19 vaccines | 52.4 (45.6–59.2) | 52.7 (45.7–59.6) | 50.6 (44.4–56.8) | 47.1 (43.3–50.1) |
| Don't trust the government | 44.6 (38.3–51.1)a | 48.9 (42.1–55.8)a | 44.6 (38.6–50.9)a | 36.3 (32.8–40.0) |
| Other reason for not getting vaccine | 22.8 (18.4–27.9) | 23.4(18.6–29.1) | 23.0 (18.9–27.7) | 21.0 (17.9–24.5) |
Significant differences in proportions comparing each group to the referent group (no anxiety or depression).
4. Conclusion and discussion
This study found that more than 1 in 3 individuals in the population had symptoms of anxiety or depression in March 2021, which is higher than previous estimates of one in five U.S. adults living with anxiety or depression in 2019 (Symptoms of Generalized Anxiety Disorder Among Adults: United States, 2019; Symptoms of Depression Among Adults: United States, 2019). The current estimate is higher than previously reported prior to and early in the pandemic, demonstrating the cumulative impact of the pandemic on the population's mental health (Ettman et al., 2020; Twenge and Joiner, 2020). In addition to their increased risk for infection and related morbidity and mortality, people with symptoms of anxiety or depression were less likely to receive COVID-19 vaccination but were more likely to report that they would be vaccinated in the future, compared with those without these symptoms, suggesting that vaccination coverage among this population after the COVID-19 vaccine became available to everyone in April 2021 may be higher than reported in this study Only 40% of people with anxiety or depression had received ≥1 dose of the COVID-19 vaccine, compared to 53% among those without symptoms. In addition, females with mental health symptoms were less likely to receive a COVID-19 vaccination, but more likely to intend to be vaccinated, suggesting the need to further understand reasons for the disparities in coverage by sex. The differences could be due to access issues such as childcaring, inability to take time off work to get a vaccine, or hesitancy toward vaccines. However, females with mental health symptoms were more likely to intend to be vaccinated, suggesting that the lower overall rate of vaccination in this population may be a result of logistical issues/barriers to care. Reported reasons for not getting vaccinated (i.e., lack of trust in the government, lack of trust in vaccines, dislike of vaccines, concerns about vaccine side effects and efficacy, and concerns about cost) were higher among those with symptoms of anxiety or depression than those without symptoms. These results are consistent with other studies that have found similar percentages of adults who are hesitant toward COVID-19 vaccinations and have similar reasons for not being vaccinated (Nguyen et al., 2021; Nguyen et al., 2020). Previous studies have also found that uptake of similar vaccines, such as influenza, was as low as 25% among people with severe mental illness (Lorenz et al., 2013). Efforts are needed to increase vaccination uptake and confidence among this population by removing barriers to access and addressing concerns about the vaccine. Other strategies include offering specific discussions from mental health professionals, tailored vaccine education and awareness to highlight the importance of vaccines and address misinformation, vaccination programs within mental health services that provides reminders and access to vaccines, and focused outreach and monitoring uptake among groups who are still hesitant (Warren et al., 2020).
People with anxiety were more likely to have prior diagnosis of COVID-19 compared to those without symptoms. It is unclear from our cross-sectional data whether people with psychiatric disorders were more likely to get COVID-19, or whether those with COVID-19 were more likely to produce symptoms of psychiatric disorders. Both of these possible explanations are consistent with other studies that have found a bidirectional association between COVID-19 and psychiatric disorders (Taquet et al., 2021). Given the potential importance of these findings for medical and public health practice, it will be essential that future research examines the temporal relationship of these variables and develop strategies to address the implications of these results.
People with anxiety or depression were more likely to lack medical care, counseling, or therapy during the pandemic, which may be due to similar access barriers that may have contributed to lower COVID-19 vaccination receipt among this population. This population is also more likely to have lower levels of income, lack health insurance and report concerns about the cost of the COVID-19 vaccine despite the fact that the vaccine is provided free of charge to all people in the United States (CDC, 2019). These concerns underscore the need to minimize access and logistic barriers to vaccination, which may be accomplished by recommending and directing vaccines to people with mental health conditions, increasing confidence in vaccines among this vulnerable group, and working with healthcare providers and communities to strengthen the message that the vaccine is effective, safe, and available without charge to recipients, regardless of insurance status.
The findings in this study are subject to several limitations. First, vaccination status was self-reported and is subject to social desirability bias. Second, although symptoms of anxiety and depression were derived from a validated scale (Census Bureau, 2020), this questionnaire asks about symptoms within the previous 7 days instead of the usual 14 days, and these conditions are self-reported and have not been confirmed by physician diagnosis. Third, the HPS has a low response rate (<10%); however, non-response bias assessment conducted by the Census Bureau found that the survey weights adjusted for most of this bias, even though some bias may remain (Warren et al., 2020). Finally, the HPS is a cross-sectional survey and therefore cannot reveal temporal relationships. For example, the results only provide associations rather than causal relationships; furthermore, respondents' mental health status, which was derived from questions asking about symptoms in the past 7 days, could have changed after vaccination.
Lower vaccination receipt and intent among people with psychiatric disorders underscore the need for continued efforts to reach these vulnerable and underserved populations, many of which are experiencing a disproportionate burden of COVID-19 infections and deaths. These efforts include outreach to those with mental illness (e,g., peer educators), educating mental health professionals about the need to promote vaccines, providing vaccines in mental health centers, and providing vouchers for transportation. Despite the vaccine being available for free, many people are still hesitant about getting vaccinated, and have cited the cost of the vaccine as a barrier to getting vaccinated. Since the vaccine is currently available to everyone nationally, directing vaccines to vulnerable populations and tailoring messages to boost confidence in vaccines are needed to achieve the goal of herd immunity. Sharing clear and accurate messages about COVID-19 vaccines, ensuring that healthcare/mental healthcare providers are recommending (or having discussions about the importance of) vaccination, and engaging communities that experience a disproportionate burden of the disease can bolster public confidence in COVID-19 vaccines and brings the world closer to the end of the pandemic.
Funding/support
No funding was secured for this study. Jennifer D. Allen was supported by the Tufts University Office of the Vice Provost for Research (OVPR) and Scholarship Strategic Plan.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Afifi M. Gender differences in mental health. Singap. Med. J. 2007;48(5):385. [PubMed] [Google Scholar]
- Anxiety and Depression Centers for Disease Control and Prevention. 2021. https://www.cdc.gov/nchs/covid19/pulse/mental-health.htm
- Arroll B., Goodyear-Smith F., Crengle S., Gunn J., Kerse N., Fishman T., Falloon K., Hatcher S. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann. Family Med. 2010;8(4):348–353. doi: 10.1370/afm.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bieler G.S., Brown G.G., Williams R.L., Brogan D.J. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am. J. Epidemiol. 2010;171(5):618–623. doi: 10.1093/aje/kwp440. [DOI] [PubMed] [Google Scholar]
- Cai C., Woolhandler S., Himmelstein D.U., Gaffney A. Trends in anxiety and depression symptoms during the COVID-19 pandemic: results from the US Census Bureau’s Household Pulse Survey. J. Gen. Intern. Med. 2021;36(6):1841–1843. doi: 10.1007/s11606-021-06759-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC Frequently Asked Questions about COVID-19 Vaccination. 2019. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/faq.html Available at:
- Census Bureau Nonresponse Bias Report for the 2020 Household Pulse Survey. 2020. https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/2020_HPS_NR_Bias_Report-final.pdf Available at:
- Cipriani A., Smith K., Macdonald O. Covid-19 vaccination programme: where do people with mental health difficulties lie within the order of priority? BMJ Opin. 2021 https://blogs.bmj.com/bmj/2021/02/16/covid-19-vaccination-programme-where-do-people-with-mental-health-difficulties-lie-within-the-order-of-priority/ (Assessed September 4, 2021) [Google Scholar]
- Dooling K., McClung N., Chamberland M., et al. The advisory committee on immunization Practices’ interim recommendation for allocating initial supplies of COVID-19 vaccine—United States, 2020. MMWR Morb. Mortal. Wkly Rep. 2020;69:1857–1859. doi: 10.15585/mmwr.mm6949e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dooling K., Marin M., Wallace M., et al. The Advisory Committee on Immunization Practices’ updated interim recommendation for allocation of COVID-19 vaccine—United States, December 2020. MMWR Morb. Mortal. Wkly Rep. 2021;69:1657–1660. doi: 10.15585/mmwr.mm695152e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druss B.G. Addressing the COVID-19 pandemic in populations with serious mental illness. JAMA Psychiatry. 2020 doi: 10.1001/jamapsychiatry.2020.0894. [DOI] [PubMed] [Google Scholar]
- Estimates of Mental Health Symptomatology, by Month of Interview: United States National Health Interview Survey. 2019. https://www.cdc.gov/nchs/data/nhis/mental-health-monthly-508.pdf (Assessed June 2, 2021)
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw. Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fields J.F., Hunter-Childs J., Tersine A., Sisson J., Parker E., Velkoff V., Logan C., Shin H. U.S. Census Bureau; 2020. Design and Operation of the 2020 Household Pulse Survey, 2020.https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/2020_HPS_Background.pdf Updated July 31, 2020. Assessed September 9, 2021. [Google Scholar]
- https://www.who.int/news/item/03-05-2021-expanding-reach-addressing-gender-barriers-in-covid-19-vaccine-rollout
- https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/Phase%203%20Questionnaire_02.25.21_English.pdf
- Kahl K.G., Correll C.U. Management of patients with severe mental illness during the coronavirus disease 2019 pandemic. JAMA Psychiatry. 2020;77(9):977–978. doi: 10.1001/jamapsychiatry.2020.1701. [DOI] [PubMed] [Google Scholar]
- Lorenz R.A., Norris M.M., Norton L.C., et al. Factors associated with influenza vaccination decisions among patients with mental illness. Int. J. Psychiatry Med. 2013;46:1–13. doi: 10.2190/PM.46.1.a. [DOI] [PubMed] [Google Scholar]
- Mazereel V., Van Assche K., Detraux J., De Hert M. COVID-19 vaccination for people with severe mental illness: why, what, and how? Lancet Psychiatry. 2021;8(5):444–450. doi: 10.1016/S2215-0366(20)30564-2. (Epub 2021 Feb 3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemani K., Li C., Olfson M., Blessing E.M., Razavian N., Chen J., Petkova E., Goff D.C. Association of psychiatric disorders with mortality among patients with COVID-19. JAMA Psychiatry. 2021;78(4):380–386. doi: 10.1001/jamapsychiatry.2020.4442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen K.H., Srivastav A., Razzaghi H., Williams W., Lindley M.C., Jorgensen C., Abad N., Singleton J.A. 2020. COVID-19 Vaccination Intent, Perceptions, and Reasons for Not Vaccinating Among Groups Prioritized for Early Vaccination—United States, September and December 2020. [Google Scholar]
- Nguyen K.H., Nguyen K., Corlin L., Allen J.D., Chung M. Changes in COVID-19 vaccination receipt and intention to vaccinate by socioeconomic characteristics and geographic area, United States, January 6–March 29, 2021. Ann. Med. 2021;53(1):1419–1428. doi: 10.1080/07853890.2021.1957998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Plummer F., Manea L., Trepel D., McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatry. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: a review of the existing literature. Asian J. Psychiatr. 2020;52 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roca M., Gili M., Garcia-Garcia M., Salva J., Vives M., Campayo J.G., Comas A. Prevalence and comorbidity of common mental disorders in primary care. J. Affect. Disord. 2009;119(1–3):52–58. doi: 10.1016/j.jad.2009.03.014. [DOI] [PubMed] [Google Scholar]
- Rosenfield S., Mouzon D. Handbook of the Sociology of Mental Health. Springer; Dordrecht: 2013. Gender and mental health; pp. 277–296. [Google Scholar]
- Sartorious N. Comorbidity of mental and physical diseases: a main challenge for medicine of the 21st century. Shanghai Arch. Psychiatry. 2013;25(2):68. doi: 10.3969/j.issn.1002-0829.2013.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siva N. Severe mental illness: reassessing COVID-19 vaccine priorities. Lancet. 2021;397(10275):657. doi: 10.1016/S0140-6736(21)00429-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Source of the Data and Accuracy of the Estimates for the Household Pulse Survey – Phase 3 Census Bureau. 2021. https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/Phase3_Source_and_Accuracy_Week_27.pdf Available at:
- Steele L., Dewa C., Lee K. Socioeconomic status and self-reported barriers to mental health service use. Can. J. Psychiatry. 2007;52(3):201–206. doi: 10.1177/070674370705200312. [DOI] [PubMed] [Google Scholar]
- Stip E., Javaid S., Amiri L. People with mental illness should be included in COVID-19 vaccination. Lancet Psychiatry. 2021;8(4):275–276. doi: 10.1016/S2215-0366(21)00068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Symptoms of Depression Among Adults: United States Centers for Disease Control and Prevention. 2019. https://www.cdc.gov/nchs/products/databriefs/db379.htm (September 28, 2021)
- Symptoms of Generalized Anxiety Disorder Among Adults: United States Centers for Disease Control and Prevention. 2019. https://www.cdc.gov/nchs/products/databriefs/db378.htm (August 21, 2021)
- Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8(2):130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge J.M., Joiner T.E. US Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress. Anxiety. 2020;37(10):954–956. doi: 10.1002/da.23077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahratian A., Blumberg S.J., Terlizzi E.P., Schiller J.S. Symptoms of anxiety or depressive disorder and use of mental health care among adults during the COVID-19 pandemic — United States, August 2020–February 2021. MMWR Morb. Mortal. Wkly Rep. 2021;70:490–494. doi: 10.15585/mmwr.mm7013e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Xu R., Volkow N.D. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry. 2021;20(1):124–130. doi: 10.1002/wps.20806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren N., Kisely S., Siskind D. Maximizing the uptake of a COVID-19 vaccine in people with severe mental illness: a public health priority. JAMA Psychiatry. 2020 doi: 10.1001/jamapsychiatry.2020.4396. http://www.ncbi.nlm.nih.gov/pubmed/33320243 [Epub ahead of print: 15 Dec 2020].pmid: [DOI] [PubMed] [Google Scholar]
- World Health Organization . 2002. Gender and Mental Health. [Google Scholar]
- Yao H., Chen J.H., Xu Y.F. Patients with mental health disorders in the COVID-19 epidemic. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]