Abstract
Objective:
To compare the anterior dentoalveolar and skeletal maxillary cephalometric factors involved in excessive upper incisor crown exposure (UICE) in subjects with skeletal open bite Class II (SOBCIIG) and Class III (SOBCIIIG) against an untreated control group (CG).
Materials and Methods:
Seventy pretreatment lateral cephalograms of orthodontic young adult patients (34 men, 36 women) were examined. The sample was divided into three groups according to both sagittal and vertical growth pattern and occlusion. The CG group (n = 25) included Class I, normodivergent cases with adequate overbite, and the SOBCIIG group (n = 25) and SOBCIIIG group (n = 20) included skeletal Class II or III malocclusions, respectively, with hyperdivergent pattern and negative overbite. Several cephalometric measurements were considered (skeletal and dental). Analysis of variance, multivariate analysis of covariance, and Tukey HSD post hoc tests were used. Principal component analysis (PCA) was used for reducing the number of cephalometric variables related to UICE. Finally, a multiple linear regression was calculated.
Results:
Significant differences in UICE were found between the groups (P < .05). UICE was 3.9 mm in SOBCIIG, 2.5 mm in SOBCIIIG, and 0.4 mm in CG. PCA showed that a nondental component—including vertical maxillary height (VMH) and upper lip height (ULH)—was the only component significantly associated with UICE. The regression model had a moderate prediction capability.
Conclusions:
Although the UICE was statistically different in SOBCIIG, the values were within the esthetic standards. The UICE was mainly influenced by VMH and ULH.
Keywords: Upper incisor crown exposure, Skeletal open bite, Cephalometry
INTRODUCTION
Upper incisor crown exposure (UICE) is directly influenced by hard and soft tissue structures that surround and support these teeth.1 Among the factors that affect UICE are vertical maxillary height, incisor extrusion, upper lip length, and maxillary incisor inclination.2 The amount of UICE has a direct impact on dentofacial esthetics.3
A vertical maxillary excess likely leads to gummy smile exposure.4–6 Depending on the maxillary vertical excess severity, an alternative treatment to maxillary impaction surgery is maxillary gingivectomy. Lately, (Temporary Anchorage Device) intrusion movements have been advocated, although their long-term stability has not been demonstrated.7 Another possibility is orthodontic camouflage,8–10 but their success is limited because true upper incisor (UI) intrusion mechanics are limited to 4 mm.11
The degree of UI inclination is also related to UICE, as teeth that are retroclined are usually more extruded. Maxillary incisor overeruption usually leads to a more coronal position of the gingival margins and excessive gingival display. Treatment of this condition may include orthodontic intrusion of the involved teeth with an associated movement of the gingival margin apically, surgical periodontal correction with or without adjunctive restorative therapy, or an interdisciplinary treatment plan.2,4 Also, the upper lip length may play an important role in UICE,2 as UIs that are well positioned may be overexposed when short upper lips are present. Short lips also decrease the possibility of a successful camouflage of the problem orthodontically when a surgical approach is not viable or declined.
There are only a couple of studies that had evaluated UICE in subjects with skeletal open bite conditions. Kucera et al.12 concluded that incisor eruption was significantly greater in dentally compensated skeletal open bite and that UIs were significantly more retroclined in in these subjects. They did not distinguish whether their cases were Class II or III, which likely could have unique camouflage compensations. Arriola-Guillén and Flores-Mir13 considered the sagittal malocclusion effect when analyzing skeletal open bite cases, but they analyzed the compensation mechanisms only at the molar level (posterior segment). The dental and skeletal compensations that could occur in the anterior segment of the occlusion were not considered.
The clinical challenge for the orthodontist is to resolve patients with open bite without increasing the exposure of the UIs with a consequent increase in gingival exposure. It is important to investigate whether UICE is altered in patients with open bite and take this into consideration during orthodontic treatment planning. It is also important to know which factors affect UICE and how they are presented in open bite cases with different growth patterns.
Therefore, the purpose of this study was to compare anterior dentoalveolar and skeletal maxillary cephalometric factors involved in excessive UICE in subjects with skeletal open bite Class II (SOBCIIG) and Class III (SOBCIIIG) compared with an untreated control group (CG). A better understanding of the factors involved in unesthetic UICE when an underlying skeletal open bite malocclusion is present should improve our diagnostic capability and treatment planning. Almost all articles14,15 regarding skeletal open bite are related to treatment protocols and their stability, but to our knowledge, none of these analyzed the individual contribution of different anterior dentoalveolar cephalometric factors on UICE.
MATERIALS AND METHODS
The study protocol was approved by the ethical committee of the School of Dentistry, Scientific University of the South, Lima, Perú. The sample included 70 pretreatment lateral cephalograms (34 men, 36 women) taken at maximum intercuspation. All of the cephalograms were taken with the lips at rest without forcing lip competency. Subjects with previous or under orthodontic treatment at the time acquisition were not considered. The age range of these patients varied from 16 to 40 years (all stage CV616).
Sample size was calculated considering a mean difference of 3 mm in UICE as a clinically relevant difference between groups with a standard deviation of 3.74 mm (obtained from a preliminary pilot study in which the mean of the UICE between open bite Class II and control were compared). With a one-sided significance level of .05 and a power of 80%, a minimum of 19 patients per skeletal group was required.
Imaging was performed with digital cephalometric panoramic equipment (ProMax, Planmeca, Finland). Device settings were set at 16 mA, 72 kV, and 9.9 seconds.
Group Classification
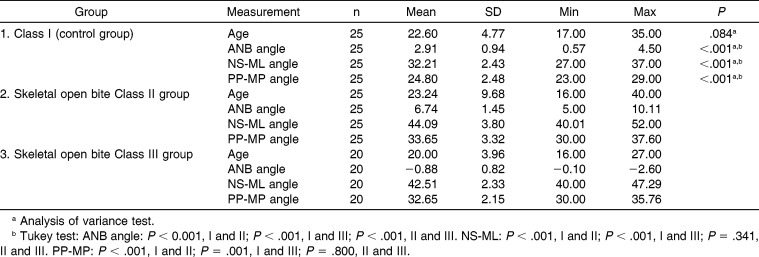
The study sample was composed of three groups categorized according to their skeletal facial growth pattern and overbite (Tables 1 and 2).
Table 1.
Characteristics of the Sample by Growth Pattern and Overbite
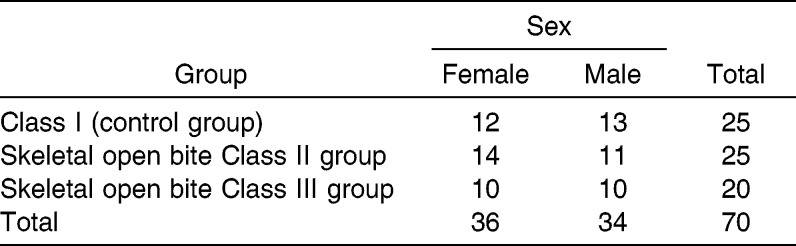
Table 2.
Distribution of the Sample by Skeletal Pattern and Sex
The CG (n = 25; mean age, 22.6 years) included subjects with ANB 2° ± 2°, Class I angle malocclusion, bilateral Class I molar relations, mandibular plane (MP) angle within the range of 33°± 6°, palatal plane (PP) to MP within the range of 26° ± 3°, overjet between 2 and 3 mm, overbite between 1 and 4 mm, and with complete permanent dentition.
The SOBCIIG group (n = 25; mean age, 23.4 years) included subjects with ANB >5°, Class II-1 angle malocclusion, bilateral Class II molar relations, overjet greater than 5 mm, MP angle greater than 40°, hyperdivergent PP (PP-MP >29°), and negative overbite greater than 0.5 mm.
The SOBCIIIG group (n = 20; mean age, 20 years) included subjects with ANB <0°, Class III angle malocclusion, bilateral Class III molar relations, overjet lower than −1 mm, MP angle greater than 40°, hyperdivergent PP (PP-MP >29°), and negative overbite greater than 0.5 mm.
Vertical Measurements
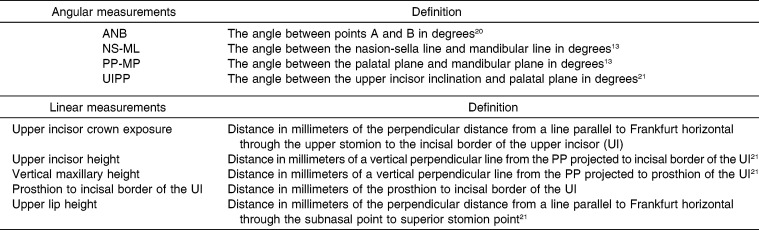
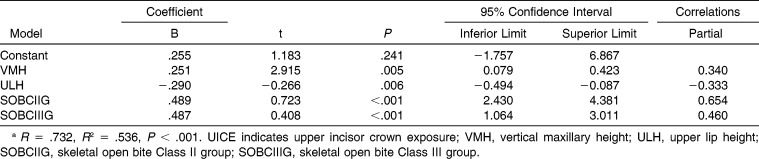
Vertical measurements are provided in millimeters (Figure 1). Cephalometric measurements were performed digitally by a trained expert researcher and calibrated with the MicroDicom viewer 0.8.1 software (Simeon Antonov Stoykov), without magnification, at a scale of 1∶1. The definitions of cephalometric points and angles used in this study are shown in Table 3.12,17
Figure 1.
Angular and linear measurements. UICE indicates upper incisor crown exposure; UIPP, upper incisor to palatal plane; UIH, upper incisor height; VMH, vertical maxillary height; UIPr, prosthion to incisal border of the UI; ULH, upper lip height.
Table 3.
Definitions of Cephalometric Points and Angles Used in This Study
UICE was measured as the perpendicular distance from a line parallel to Frankfurt horizontal through the upper stomion (lowermost point on the vermilion of the upper lip) to the incisal border of the UI.
Upper incisor height (UIH) was measured as the distance of a vertical perpendicular line from the PP projected to the incisal border of the UI.
Vertical maxillary height (VMH) was measured as the distance of a vertical perpendicular line from the PP projected to the prosthion of the UI.
Prosthion to incisal border of the UI (UIPr) was considered as a measurement of the clinical crown.
Upper lip height (ULH) was measured as the perpendicular distance from a line parallel to Frankfurt horizontal through the subnasal point to the superior stomion point.
Inclination measurements (in degrees) are presented in Figure 1.
Upper incisor inclination (UIPP) was evaluated considering the angle formed between the PP and the long axis of the upper central incisor.
Statistical Analysis
All statistical analyses were performed using SPSS versioin 20 for Windows (IBM SPSS, Chicago, Ill). The normality and homogeneity of variance assumptions were satisfied with Shapiro-Wilk tests. A multivariate analysis of covariance (MANCOVA) test was initially considered, with UICE as the dependent variable and considering age, sex, group, and their interactions as the independent variables. Neither sex nor age nor the interactions were significant.
One-way analysis of variance test with Tukey HSD post hoc tests were performed to determine whether there were differences between the three groups regarding UICE, UIH, VMH, UIPr, ULH, and UIPP measurements. In addition, principal component analysis (PCA) was used to reduce interrelated factors to increase the statistical power of the subsequent analysis. Based on the PCA results, a MANCOVA test was developed considering only the nondental component (VMH and ULH). Finally, a multiple linear regression was calculated. Statistical significance was set at P < .05 for all tests.
RESULTS
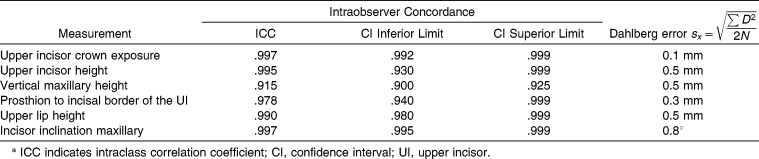
Reliability
The intraexaminer reliability (Table 4) was assessed with the intraclass correlation coefficient (ICC), which gave a result greater than .90 in all measurements. In addition, the Dahlberg error was less than 1 mm for linear measurements and 0.8° for angular measurements. All of the cephalometric tracings were drawn with a 2-month interval between them.
Table 4.
Intraobserver Concordance and Error Analysisa
Vertical Measurements
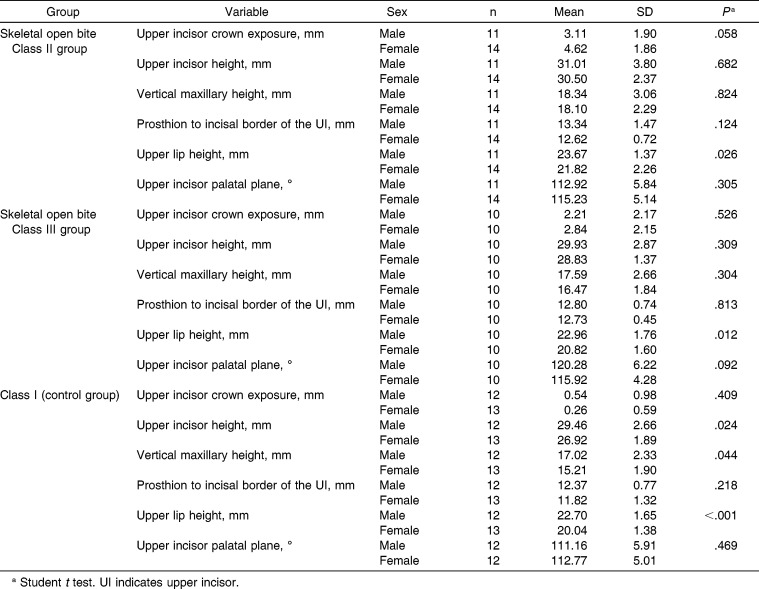
Descriptive statistics are shown in Table 5. When comparing all study variables grouped by sex and group, significant differences were observed for ULH (all P < .05).
Table 5.
Factors Involved in the Exposure of Upper Incisors by Malocclusion and Sex
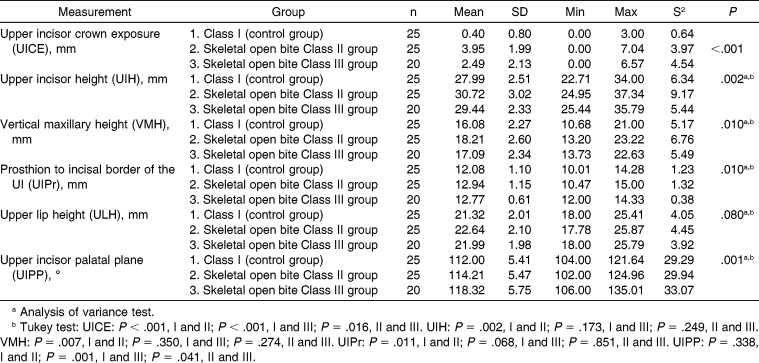
In Table 6, significant differences in the UICE among the vertical measurements (UIH, VMH, UIPr, UIPP) were found between the groups (P < .05). UICE was higher in SOBCIIG (4 mm) than in SOBCIIIG (2.5 mm) and CG (0.4 mm; P < .01). UIH was larger by approximately 2.8 mm in SOBCIIG and 1.5 mm in SOBCIIIG in comparison with CG, but was significant only for SOBCIIG when compared with CG (P = .002). The VMH for SOBCIIG was approximately 2 mm larger in comparison with CG (P = .007). SOBCIIIG was 1 mm greater than CG, but without significance. No difference was demonstrated between SOBGs. UIPr was significantly larger only for SOBCIIG compared with CG by approximately 1 mm (P = .011). For ULH, no difference was demonstrated between SOBGs and CG (P = .080). The UIPP was larger for SOBCIIIG by 6° and 4°, respectively, than for SOBCIIG (P = .041) and CG (P = .001).
Table 6.
Factors Involved in the Exposure of Upper Incisors in Subjects With Skeletal Open Bite Class II, Class III, and Control Group
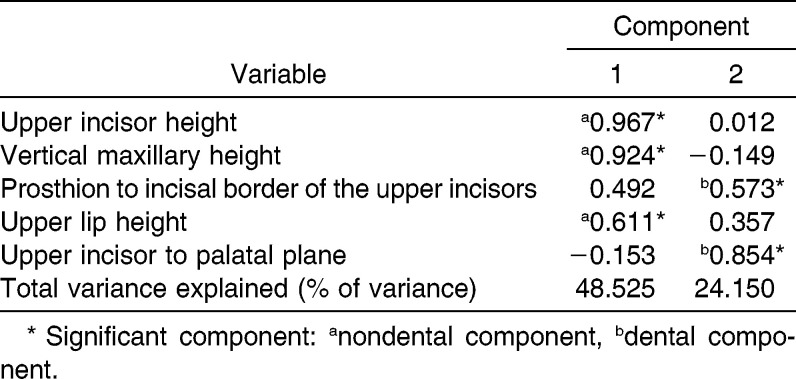
Principal Component Analysis
Two significantly factors were obtained after the reduction of the number of independent variables considered (Table 7). These factors were named the “nondental component” and the “dental component.”
Table 7.
Principal Component Analysis of the Factors Involved in the Crown Exposure of Upper Incisors
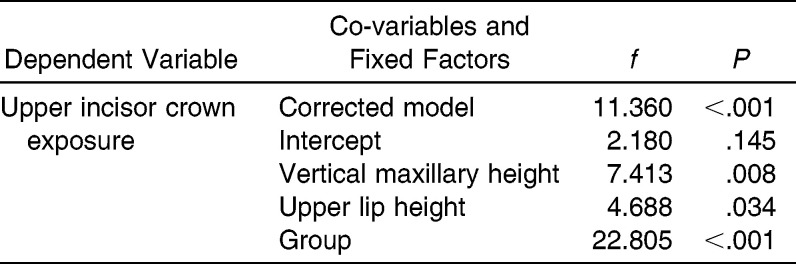
Final Statistical Analysis
A MANCOVA considered the only nondental component (VMH and ULH) because it was the only factor significantly involved in the UICE (Table 8). VMH, ULH, and groups were significant (P = .008, P = .034, and P < .001, respectively).
Table 8.
Multivariate Analysis of Covariance Considering Only the Dental Principal Component Analysis Factors Group, Sex, and the Interaction
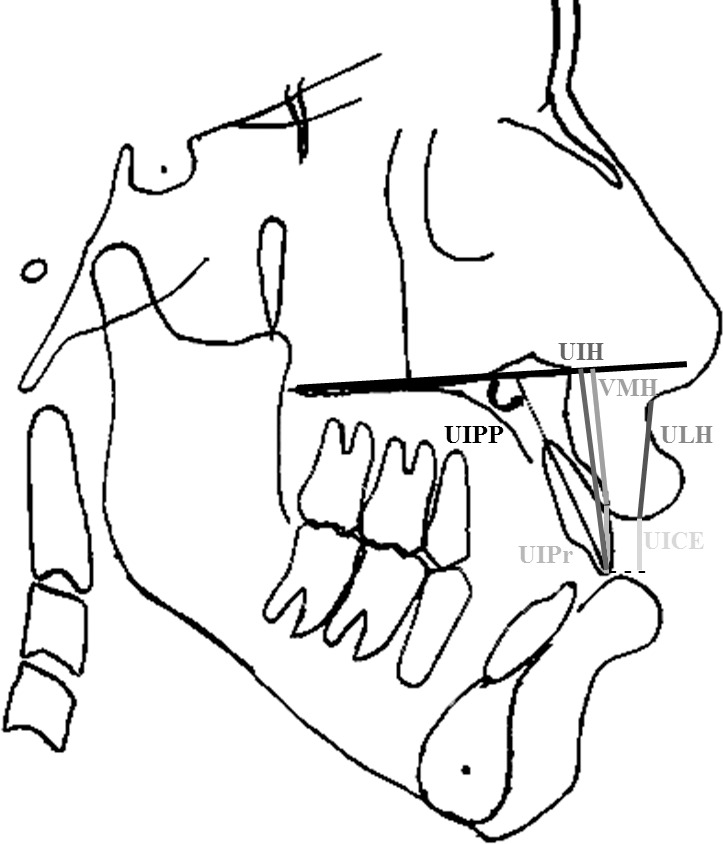
Finally, a multiple linear regression model (Table 9) was conducted with the variables that were significant in the last MANCOVA. The regression model had a moderate prediction capability of about 54% (P < .001, R2 = .536).
Table 9.
Multiple Linear Regression of the Influence of the Nondental Principal Component Analysis Factor Components and Groups Over UICEa
DISCUSSION
The purpose of this study was to consider anterior maxillary dentoalveolar and skeletal cephalometric factors associated with an excessive UICE in subjects with a Class II and III skeletal open bite malocclusion as contrasted with a CG with adequate occlusion and no major skeletal imbalances. The group's age and sex were initially balanced to diminish classification bias. SOBCIIG and SOBCIIIG groups met skeletal open bite requirements including a negative overbite, MP hyperdivergency, and upward inclination of the PP observed on the lateral cephalograms. Differences between the groups, some clearly clinically and statistically significant, were identified.
An increased UICE evaluated at rest and with smile has been previously associated with maxillary vertical excess, short upper lip, increased clinical crown, and/or more retroclined UIs.2 The authors of that study suggested that these features were related primarily to a genetic etiology; however, they may be favored if there is no anterior contact between the upper and lower incisors. This lack of contact is characteristic of a skeletal open bite and stimulates incisor extrusion and dentoalveolar process vertical development. In this study, the cephalograms were taken with the lips at rest without forcing lip competency. The amount and direction of upper lip movement during different smile movements (dynamic condition of UICE) is a difficult variable to control in this type of research.
In our study, the SOBCIIG had the highest values of UICE (4 mm), but this value does not exceed the ideal esthetic values proposed by Burstone et al.17 of 2 ± 2 mm in maximum exposure at rest. Because of the relatively small standard deviation (±2 mm), the treatment of most of these cases should focus primarily on maintaining or slightly decreasing the exposure, not necessarily implying major surgical procedures. Intrusion of the posterior teeth as the treatment of choice has been indicated by some studies,12,13 although the long-term stability of molar intrusion is still controversial. According to Baek et al.,18 relapse occurred on an average of 23% of the amount of molar intrusion facilitated by microscrews within 3 years of the postretention period.
The SOBCIIIG difference (2 mm) may be of questionable clinical importance. Furthermore, it seems that the most important factors involved with an increased UICE are related to a decrease of the length of the upper lip and an increase of the vertical maxillary height. Burstone et al.17 found that the distance of the upper incisor edge to the PP in males was 30.5 ± 2.1 mm and in females 27.5 ± 1.7 mm, where larger values were considered as overeruption and smaller values as infraeruption. Also, Kucera et al.12 found that in the skeletal open bite group, the incisor height was significantly elongated compared with CG by approximately 3 mm. Our results were consistent with those of previous studies,12–19 but they contradict those reported by Nahoum,20 who found smaller values for incisor height in patients with open bite with respect to CG. None of these studies took into account the sagittal skeletal pattern.
In orthodontic treatment of a skeletal open bite, careful consideration must be given to esthetic factors. In those cases, therapy could be directed primarily to the intrusion of molars instead of extruding the incisors, as it is very frequently the case that the incisors are already extruded. More extrusion could worsen the case esthetically, and the incisors may be more likely to relapse. In summary, excessive extrusion of incisors in open bite treatment may bring results that are neither stable nor esthetic.
The regression model had a moderate prediction capability of about 54%, which indicates that there are other uncontrolled variables in this study that significantly influence exposure incisors. Our study did focus only on the measurement of variables related only to the anterior part of the face. However, anterior open bite can also occur due to posterior dentoalveolar adaptations such as increased molar extrusion. Kucera et al.12 concluded that the increased molar height is a common finding in adults with skeletal open bite. In a study using the same sample, Arriola-Guillén and Flores-Mir13 concluded that the skeletal open bite groups had greater molar heights than did CG.
In addition, in open bite patients undergoing orthognathic surgery, it has been suggested that extrusion of the incisors is to be avoided in presurgical orthodontics to decrease the risk of dental relapse after surgery.21,22 The reasoning is that if upper teeth were to be extracted for decompensation purposes before surgery, the amount of incisor exposure at rest must be taken into account because it could easily worsen the case.
The UIPP determines the degree of upper incisor inclination with respect to its bony base. The measurement of the extrusion is strongly influenced by the angulation of incisors. In this research, the control of the UIPP as selection criteria was not made because all cases would be similar, and they will unlikely reflect the reality of compensation responses in the different malocclusions. Burstone et al.17 found that average value of inclination were 111° ± 4.7° in men and 112.5° ± 5.3° in women, where larger values indicate vestibular inclination. Our results showed that the upper incisor inclination on SOBCIIIG was 6° and 4° more proclined in SOBCIIIG than in SOBCIIG and CG groups, respectively. This inclination is typical for Class III patients, in whom tongue pressure and lack of upper lip resistance over the upper incisors allow for a greater vestibular inclination.13 No statistically significant differences were found on incisive inclination between SOBCIIG and CG. This is in agreement with other research, which found that the open bite group did not differ significantly from a CG in this regard.12,23,24 The ULH was not statistically significantly different between SOBGs and CG. This makes sense as the length of the upper lip is not influenced by the sagittal skeletal malocclusion.
In summary, our study evaluated which of the evaluated cephalometric factors was most significantly associated with UICE. PCA was used to reduce the number of evaluated variables during the statistical analysis, so that an increase in the statistical power was obtained. It was expected that among the evaluated cephalometric variables, several will be closely associated (some shared common cephalometric structures). Therefore, PCA allowed grouping them based on the strength of their interrelations. This automatically diminished the chances of false-positive results. After grouping the variables into two factors in relation to UICE, only the nondental component showed statistical significance regarding UICE. This component included the variables VMH and ULH. Therefore, we may assume that these are the variables that most influence UICE.
CONCLUSIONS
Although the UICE was statistically different in SOBCIIG, the values were within the esthetic standards.
UICE was mainly influenced by VMH and ULH.
REFERENCES
- 1.Robbins JW. Differential diagnosis and treatment of excess gingival display. Pract Periodont Aesthet Dent. 1999;11:265–272. [PubMed] [Google Scholar]
- 2.Silberberg N, Smidt A. Excessive gingival display: etiology, diagnosis, and treatment modalities. Quintessence Int. 2009;40:809–818. [PubMed] [Google Scholar]
- 3.Hunt O, Johnston C, Hepper P, Burden D, Stevenson M. The influence of maxillary gingival exposure on dental attractiveness ratings. Eur J Orthod. 2002;24:199–204. doi: 10.1093/ejo/24.2.199. [DOI] [PubMed] [Google Scholar]
- 4.Garber DA, Salama MA. The aesthetic smile: diagnosis and treatment. Periodontol 2000. 1996;11:18–28. doi: 10.1111/j.1600-0757.1996.tb00179.x. [DOI] [PubMed] [Google Scholar]
- 5.Polo M. Botulinum toxin type A in the treatment of excessive gingival display. Am J Orthod. 2005;127:214–218. doi: 10.1016/j.ajodo.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 6.Peck S, Peck L, Kataja M. Some vertical lineaments of lip position. Am J Orthod. 1992;101:519–524. doi: 10.1016/0889-5406(92)70126-U. [DOI] [PubMed] [Google Scholar]
- 7.Kaku M, Kojima S, Sumi H, et al. et al. Gummy smile and facial profile correction using miniscrew anchorage. Angle Orthod. 2012;82:170–177. doi: 10.2319/020711-86.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Redlich M, Mazor Z, Brezniak N. Severe high Angle Class II Division 1 malocclusion with vertical maxillary excess and gummy smile: a case report. Am J Orthod. 1999;116:317–320. doi: 10.1016/s0889-5406(99)70243-x. [DOI] [PubMed] [Google Scholar]
- 9.Conley RS, Legan HL. Correction of severe vertical maxillary excess with anterior open bite and transverse maxillary deficiency. Angle Orthod. 2002;72:265–274. doi: 10.1043/0003-3219(2002)072<0265:COSVME>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Bai D. Re: Gummy smile and facial profile correction using miniscrew anchorage by Masato Kaku, Shunichi Kojima, Hiromi Sumi, Hiroyuki Koseki, Sara Abedini, Masahide Motokawa, Tadashi Fujita, Junji Ohtani, Toshitsugu Kawata, and Kazuo Tanne. Angle Orthod. 2012;82:170–177. doi: 10.2319/020711-86.1. Angle Orthod. 2012;82:573–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Profitt WR, Turvey TA, Phillips C. Orthognathic surgery: a hierarchy of stability. Int J Adult Orthod Orthognath Surg. 1996;11:191–204. [PubMed] [Google Scholar]
- 12.Kucera J, Marek I, Tycova H, Baccetti T. Molar height and dentoalveolar compensation in adult subjects with skeletal open bite. Angle Orthod. 2011;81:564–569. doi: 10.2319/081910-488.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arriola-Guillén LE, Flores-Mir C. Molar height and incisor inclinations on adult subjects with skeletal open bite class II and III. Am J Orthod Dentofac Orthop. In press doi: 10.1016/j.ajodo.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 14.Sugawara J, Baik UB, Umemori M, et al. et al. Treatment and posttreatment dentoalveolar changes following intrusion of mandibular molars with application of a skeletal anchorage system (SAS) for open bite correction. Int J Adult Orthod Orthognath Surg. 2002;17:243–253. [PubMed] [Google Scholar]
- 15.Ribeiro GL, Regis S, Jr, da Cunha TM, Sabatoski MA, Guariza-Filho O, Tanaka OM. Multiloop edgewise archwire in the treatment of a patient with an anterior open bite and a long face. Am J Orthod Dentofacial Orthop. 2010;138:89–95. doi: 10.1016/j.ajodo.2008.03.036. [DOI] [PubMed] [Google Scholar]
- 16.Baccetti T, Franchi L, McNamara J. The cervical vertebral maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod. 2005;11:119–129. [Google Scholar]
- 17.Burstone CJ, James RB, Legan H, Murphy GA, Norton LA. Cephalometrics for orthognathic surgery. J Oral Surg. 1978;36:269–277. [PubMed] [Google Scholar]
- 18.Baek MS, Choi YJ, Yu HS, Lee KJ, Kwak J, Park YC. Long-term stability of anterior open-bite treatment by intrusion of maxillary posterior teeth. Am J Orthod Dentofacial Orthop. 2010;138:396.e1–9. doi: 10.1016/j.ajodo.2010.04.023. [DOI] [PubMed] [Google Scholar]
- 19.Schudy FF. Vertical growth versus anteroposterior growth as related to function and treatment. Angle Orthod. 1964;34:75–93. [Google Scholar]
- 20.Nahoum HI. Vertical proportions: a guide for prognosis and treatment in anterior open-bite. Am J Orthod. 1977;72:128–146. doi: 10.1016/0002-9416(77)90055-0. [DOI] [PubMed] [Google Scholar]
- 21.Arnett W, Bergman R. Facial keys to orthodontic diagnosis and treatment planning: part II. Am J Orthod Dentofacial Orthop. 1993;103:395–411. doi: 10.1016/s0889-5406(05)81791-3. [DOI] [PubMed] [Google Scholar]
- 22.Proffit WR, White PR, Sarver DM. Contemporary Treatment of Dentofacial Deformity. St Louis, Mo: Mosby Elsevier; 2003. [Google Scholar]
- 23.Beckmann SH, Kuitert RB, Prahl-Andersen B, Segner D, Tuinzing DB. Alveolar and skeletal dimensions associated with overbite. Am J Orthod Dentofacial Orthop. 1998;113:443–452. [PubMed] [Google Scholar]
- 24.Kuitert R, Beckmann S, van Loenen M, Tuinzing B, Zentnere A. Dentoalveolar compensation in subjects with vertical skeletal dysplasia. Am J Orthod Dentofacial Orthop. 2006;129:649–657. doi: 10.1016/j.ajodo.2004.09.032. [DOI] [PubMed] [Google Scholar]