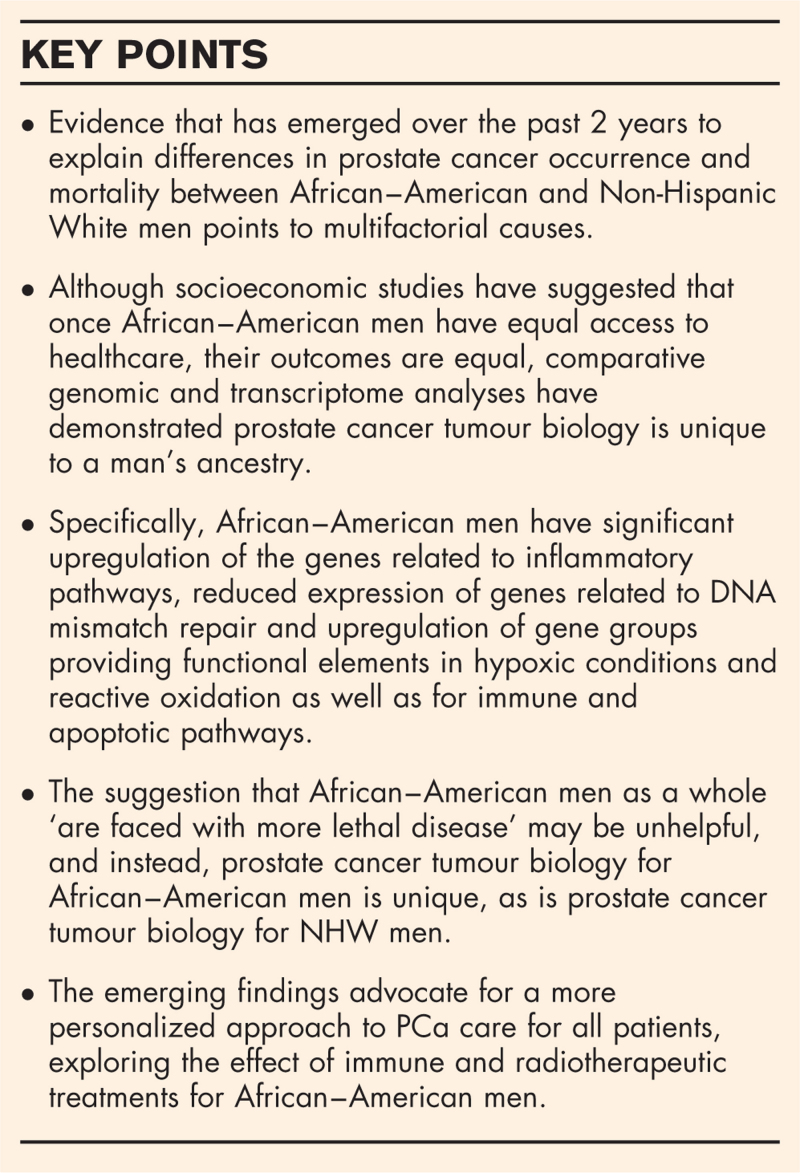
Purpose of review
African–American men in the USA have a higher incidence of and mortality from prostate cancer (PCa), with a longstanding debate about the cause for these worse outcomes. This review examines differences in tumour biology and socioeconomics for African–American and Non-Hispanic White (NHW) men to answer the question ‘why AA men face higher risks for lethal PCa’ and draw a management consensus to redress the imbalance.
Recent findings
Recent evidence from over the past 2 years suggests the reasons why African–American men face a higher risk of lethal PCa are multifactorial, with contributions from differences in tumour biology as well as socioeconomic and healthcare access factors. Regarding tumour biology, genomic and transcriptome profiling suggests African–American men have upregulated expression of genes related to inflammatory pathways with downregulation of DNA repair genes. In contrast, NHW men have higher DNA repair pathways and metabolic pathways involving glycolysis and cell cycle activity. In addition, epidemiological evidence suggests equal healthcare access ensures equal PCa specific outcomes, implying African–American men's disease is not inherently more lethal. However, differences in tumour biology remain, which may explain specific differences in PCa incidence and the clinical findings of African–American men's increased response to immunotherapy and radiotherapy in recent trials.
Summary
Regardless of racial differences in disease outcomes and the factors causing them, African–American and NHW men seem to have diseases unique to their ancestry. This supports the exploration of personalized PCa treatment approaches, leveraging translational basic science research to uncover these differences and devise specific individualized methods therapeutic regimes to address them.
Keywords: genomic and immunologic drivers, racial disparity, socioeconomics and healthcare access, tumour biology
INTRODUCTION
African–American men in the United States have a higher incidence of and mortality from prostate cancer (PCa) [1]. The risk of African–American men diagnosed with PCa in their lifetime is 1 in 6, compared with 1 in 8 for non-Hispanic white (NHW) men, and they are twice as likely to die of it once diagnosed [1]. There is a longstanding debate regarding the cause for these differences, ranging from healthcare access problems, socioeconomic differences resulting in comorbidities that may affect the tumour microenvironment, as well as fundamental differences in tumour biology [2▪▪]. The debate continues with recent evidence supporting the contributions of both socioeconomic issues and tumour biology [3▪▪–5▪▪]. Two recent epidemiological studies demonstrated that once equal healthcare access was provided to African–American populations, PCa outcomes were the same for African–American and NHW men. Dess et al.[4▪▪] examined data from Surveillance, Epidemiology and End Results (SEER), Radiation Therapy Oncology Group (RTOG) trials as well as the Veterans Affairs (VA) Health System in over 300 000 patients with PCa. They found equalized treatment resulted in equal PCa specific outcomes [4▪▪].
Box 1.
no caption available
Similarly, Riviere et al.[3▪▪], using a Veterans Affairs cohort for which all patients experienced equal healthcare access, demonstrated equality in stages of PCa presentation as well as no significant difference in PCa-specific survival outcomes [3▪▪]. By contrast, a recent multiinstitutional comparative study analysed 1152 patients (556 NHW men and 596 African–American men) with localized PCa who underwent surgical treatment. They found African–American men had more advanced disease at clinical presentation, with low and favourable intermediate-risk groups having higher risk genomic scores on examination of the surgical disease, as well as significant differences in tumour biology related to inflammatory and metabolic pathways [5▪▪]. The finding of differential expression in immune-related gene pathways has been supported by several recent similar studies assessing comparative genomics and transcriptome profiles in postsurgical tissues from cohorts of African–American and NHW men with localized PCa [6▪▪,7▪▪]. In addition, other studies have highlighted specific germline variants in those of African ancestry [8▪▪] and differences in mitochondrial metabolism and metabolic reprogramming pathways, which may also influence the aggressiveness of disease [8▪▪].
In light of the ongoing debate, this review examines the recent development in the field and literature that addresses the critical differences in tumour biology and socioeconomics for African–American and NHW men.
We expect the findings will answer as much as is possible the question ‘why AA men face higher risks for lethal PCa’ and draw a management consensus to improve African–American men's incidence and mortality from PCa and potentially help to redress this imbalance.
TUMOUR BIOLOGY
There is a breadth of literature investigating the genomics and molecular biology of PCa in African–American men, but despite this, an accurate understanding of how our knowledge of PCa molecular biology influences clinical outcomes remains elusive. This may, in part, result from the underrepresentation of African–American men in studies focused on genomic profiling, reflected in, for example, a relative paucity of African–American men overall in the PCa Genome Atlas Program (TCGA) [5▪▪]. However, several recent studies have examined the genomic and transcriptome profile of PCa patients allowing a more direct comparison of the racial differences in the molecular pathways underlying PCa oncogenesis and progression and potentially shedding light on future opportunities for screening and therapeutic intervention. Moreover, reviewing these studies together provides evidence of an emerging consensus on genuine differences in tumour biology.
One study has investigated a specific germline variant (rs72725854) at locus 8q24, as the most substantial risk factor for familial PCa associated with earlier diagnosis and higher-risk disease. This germline variant was found with high frequency in African–American men and absent in populations with European ancestry [8▪▪]. It was found in 32% of hereditary cases, and those with the homozygous allele carried a 33-fold increase in PCa risk compared to noncarriers (7.8% risk for homozygous carriers compared with 0.35% for controls). On the basis of this, it is reasonable to recommend that carriers be screened in a similar way to HOXB13 or BRCA2 mutations [8▪▪].
Yuan et al.[9▪▪] examined genetic and transcriptome changes from 61 African–American and 414 NHW men from the TCGA PCa cohort. For African–American men vs. NHW men, they demonstrated an increased frequency of SPOP mutations (20.3 vs. 10%), fewer TMPRSS2-ERG fusions (29.3 vs. 39.6%) and fewer PTEN deletions (11.5 vs. 30.2%) with increased differential expression of genes related to immune pathways in African–American men, and higher PTEN/PI3K signalling in NHW men [9▪▪]. The immune genes upregulated in African–American men were related to, for example B and T cell regulation and activation and interleukin signalling pathways, and support the findings of other recent genomic profiling studies suggesting differences in tumour immunobiology may play a role in the higher risk of lethal PCa that African–American men face [9▪▪,10,11].
Rayford et al.[5▪▪] performed a comparative analysis of 596 African–American men vs. 556 NHW men with localized PCa undergoing radical prostatectomy, examining their surgical specimens for many parameters related to tumour biology. They also found genomic differences in African–American men vs. NHW men with higher SPINK1 expression (22 vs. 10%), lower ERG expression (23 vs. 41%), significant upregulation of the genes CRYBB2, GSTM3, and those related to inflammatory pathways (e.g. CCL4, IFNG, CD3, IL33 and ICOSLG), as well as reduced expression of genes related to DNA mismatch repair (e.g. MSH6 and MSH2). Increased SPINK1 but reduced ERG expression has been found in prior recent studies [12▪▪,13], but its clinical and prognostic significance is not clear. Interestingly, Rayford et al.[5▪▪] also specifically studied expression within fundamental signalling pathways. African–American men had upregulation of gene groups providing functional elements in hypoxic conditions, reactive oxidation, and immune and apoptotic pathways (e.g. TNF alpha, NFKB, IFN alpha and gamma signalling). This was reflected in African–American men having an increased inflammatory response with increased gamma IFN and T cell activity at a prostate tissue level. By contrast, NHW men had higher DNA repair and metabolic pathways involving glycolysis and cell cycle activity (e.g. MYC and WNT-beta-catenin signalling) [5▪▪]. Two more recent similar studies investigated the comparative genomics and transcriptome landscape in surgical specimens for patients with localized PCa [6▪▪,7▪▪]. In a study of over 1300 African–American men who underwent radical prostatectomy, Weiner et al.[7▪▪] examined prostate specimens showing increased infiltrating lymphocytes with more plasma cells, elevated IFN gamma signalling, increased IgG expression and higher NK cell activity. Interestingly, higher plasma cell content was associated with improved disease-free survival, and as a result, may provide a biomarker for an immunotherapeutic response, as well as also offering a novel therapeutic approach to induce plasma cell function in the tumour microenvironment to maximize their antitumor effect [7▪▪]. These findings were confirmed in a similar study on radiation naive postradical prostatectomy specimens from the Decipher GRID registry [6▪▪]. The whole cohort in this study was split into discovery and validation cohorts with African–American men consisting of 127 out of 635 and 236 out 538 from each cohort, respectively.
Interestingly, NHW men were more likely to have an extracapsular extension (ECE) and lymph node invasion (LNI) on surgical disease in the discovery cohort as well as ECE in the validation cohort, suggesting, in contrast to study by Rayford et al.[5▪▪], NHW presented with more advanced disease. Further examining tissue for the transcriptome profile, they once again found significantly elevated immune-related gene expression for inflammatory cytokines such as IFN alpha and gamma, TNF, interleukins and markers for the process of epithelial to mesenchymal transition, one of the critical events in PCa oncogenesis. On the contrary, African–American men had higher expression of CD4 and CD8 markers, lower expression of DNA repair genes, and no difference in immune checkpoint markers (CTLA-4, PD-1, PD-L1 and L2 [6▪▪]. Concerning PCa being more lethal in African–American men, one of the overexpressed pro-inflammation genes, IFN-inducible transmembrane protein 3 (IFITM3) predicted biochemical recurrence in the African–American discovery and validation cohorts not for NHW patients [6▪▪]. As well as differences in inflammatory and DNA repair pathways, there is emerging research highlighting differences in tumour biology related to mitochondrial function and metabolic reprogramming [14]. There are a number of mitochondrial abnormalities at a genetic level in PCa, for example, in the mitochondrial ‘D-Loop’, consisting of two hypervariable regions and in nuclear-encoded mitochondrial proteins, some of which are nuclear-encoded proteins, which may be race-specific. More direct comparative analytic research is required, in line with the studies presented above, to elucidate how this may contribute mechanistically to any racial differences in PCa oncogenesis and progression. However, mitochondrial abnormalities can influence the roles of reactive oxidation, apoptotic signalling energy reprogramming, and glycolysis in cellular tumorigenesis [14].
CLINICAL SEQUELAE OF AFRICAN--AMERICAN GENOMIC DIFFERENCES – CAN THEY EXPLAIN WHY PROSTATE CANCER IS MORE LETHAL FOR AFRICAN--AMERICAN MEN?
The challenge for clinicians is to translate our growing understanding of these differences in tumour biology into biomarkers used for risk stratification at screening and diagnosis and novel therapeutic tools. In study by Rayford et al.[5▪▪], African–American men presented with more advanced disease. With regards to the clinical staging of patients in their cohort, at the time of presentation, African–American men had more elevated PSAs, increased incidence of locally advanced disease (defined as pT3b or T4 on histopathology postsurgery) and higher CAPRA-S scores (calculated from the PSA presurgery as well as Gleason score, staging, margin status and nodal involvement on postsurgical disease). These findings may support the concept that PCa in African–American men has a higher risk of tumour biology, and in this cohort, African–American men will be faced with lethal disease and a poorer prognosis at the time of diagnosis. However, advanced clinical staging at the time of presentation could potentially be explained by healthcare access issues alone, and in the study by Awasthi et al.[6▪▪], the reverse was true; NHW men had more adverse pathological features on their surgical pathology [5▪▪]. Looking at prognostic biomarkers in Rayford's cohort, Decipher scores were only higher in African–American men for low and favourable intermediate-risk Gleason grade groups (GGG) 1 and 2.
In contrast, for NHW men, the average genomic risk score (the average of 19 genomic signatures without decipher) was higher in Gleason grade groups (GGG) 4 and 5, suggesting that differences in tumour biology only affected the prognosis for African–American men with low and favourable intermediate-risk disease and NHW men with high-risk disease [5▪▪]. Nevertheless, the described differences in tumour immunobiology and metabolic processes remain, which further supports the emerging use of precision medicine for all patients and combinations of radiotherapy and immunotherapy in African–American men. In the PROCEED registry of over 1900 men (12% were African–American) with metastatic castrate-resistant prostate cancer (mCRPC) treated with Sipuleucel-T (autologous vaccine immunotherapy using patients’ ex vivo processed dendritic cells expressing key antigens), overall survival was significantly better for African–American men. This difference was especially marked for those patients with a lower baseline PSA, in whom the median overall survival for African–American vs. NHW men was 54.3 compared with 33.4 months [15▪▪].
Differences in tumour biology may influence responses to chemotherapeutic agents as well. For example, in assessing potential gene-based chemotherapeutic sensitivities in their cohort of 1152 patients, Rayford et al.[5▪▪] found that African–American men may respond more favourably to alkylating-based chemotherapeutic regimes NHW men would have better clinical responses to taxane-based chemotherapies. Taxane-based chemotherapy is the internationally established standard of care for advanced PCa. Although it would require clinical validation, this differential response may result from alkylating agents’ DNA damaging effect combined with the finding that PCa in African–American men has lower expression of DNA repair genes [5▪▪]. Moreover, reduced expression of DNA repair genes, itself negatively influenced by reduced androgen receptor signalling, may explain the findings of other studies that have demonstrated improved responses of African–American men to radiotherapy, which is by convention, combined with androgen receptor inhibiting hormone therapy [16▪,17,18].
Overall, these findings support the exploration of personalized approaches to PCa treatment, leveraging translational basic science research to uncover individual differences in PCa disease characteristics.
SOCIOECONOMICS, LIFESTYLE AND IMMUNOBIOLOGY
Counterbalancing these fundamental science discoveries is the epidemiological evidence that African–American men face genuine socioeconomic problems and healthcare access issues. Moreover, issues arise within African–American families and communities and from the physicians and institutions that care for them. For example, Freidlander et al.[19] examined 59 262 African–American men and 223 873 NHW men with localized PCa from the National Cancer Database in the USA managed between 2004 and 2013. Using multilevel logistic regression to predict the odds of receiving definitive therapy, they found that 39% of hospitals demonstrated significantly higher rates of definitive treatment (surgery or radiotherapy) for NHW men than African–American men [19]. Community education initiatives may help to encourage African–American men to improve their understanding of their health and invest in their healthcare, and interestingly, two recent epidemiological studies have shown that once healthcare access issues are overcome, survival outcomes for African–American men vs. NHS men are equalized [3▪▪,4▪▪]. These studies suggest that if African–American men were to engage in screening activities and present to healthcare institutions quickly, their PCa-specific survival outcomes would be the same. However, median follow-up was 5.89 years for NHW men and 5.79 years for African–American men in the study by Riviere et al.[5▪▪] and between 70 and 105 months in the study by Dess et al.[4▪▪], which may be too short to assess longer-term disease outcomes. Moreover, genomic risk scores are heterogeneous according to GGGs for African–American and NHW men, with higher decipher scores in African–American men with GGGs 1 and 2 and higher AGR scores for NHW men in GGGs 4 and 5 [5▪▪]. This would suggest that making generalizations about PCa outcomes for groups of African–American or NHW men as a whole is unhelpful.
There is evidence that diet, lifestyle and comorbidities, including obesity, hypertension and diabetes, create systemic inflammation, influencing PCa development and survival outcomes [20]. There are also several factors contributing to potential differences in lifestyle-induced systemic inflammation between African–American and NHW men, including genomic and socioeconomic [21,22]. Interestingly, markers of systemic inflammation such as neutrophil, platelet and mono-lymphocyte ratios may help show improved response to diet and lifestyle programs and may have prognostic value pretreatment for longer-term outcomes [20]. How lifestyle-induced systematic inflammation influences the tumour microenvironment and tumour immunobiology described above to affect PCa tumorigenesis is unclear and represents a controversial area. However, there are promising results from studies of anti-inflammatory diets improving survival in breast cancer patients, and it warrants further study.
CONCLUSION
Recent evidence from over the past two years suggests the reasons why African–American men face a higher risk of lethal PCa are multifactorial, with contributions from differences in tumour biology as well as socioeconomic and healthcare access factors. Regarding tumour biology, genomic and transcriptome profiling suggests African–American men have upregulated expression of genes related to inflammatory pathways, with downregulation of DNA repair genes. In contrast, NHW men have higher DNA repair pathways and metabolic pathways involving glycolysis and cell cycle activity. This may explain specific differences in PCa incidence rather than survival outcomes for African–American men and clinical findings of African–American men's increased response to immunotherapy and radiotherapy in recent trials. Regardless of racial differences and the factors causing them, overall, African–American and NHW men seem to have a disease that is unique to their ancestry. This supports the exploration of personalized approaches to PCa treatment, leveraging translational basic science research to uncover these differences and devise specific individualized therapeutic regimes.
Acknowledgements
We would like to thank all Department of Urology research team members for discussions related to the study.
Financial support and sponsorship
This work was supported by funding from the Deane Prostate Health, ISMMS and The Arthur M. Blank Family Foundation to A.K.T.
Conflicts of interest
Dr. Tewari has served as a site-PI on pharma/industry-sponsored clinical trials from Kite Pharma, Lumicell Inc, Dendreon and Oncovir Inc. He has received research funding (grants) to his institution from DOD, NIH, Axogen, Intuitive surgical, AMBFF and other philanthropy. Dr. Tewari has served as an unpaid consultant to Roivant Biosciences and advisor to Promaxo. He owns equity in Promaxo.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.DeSantis CE, Siegel RL, Sauer AG, et al. Cancer statistics for African Americans, 2016: progress and opportunities in reducing racial disparities. CA Cancer J Clin 2016; 66:290–308. [DOI] [PubMed] [Google Scholar]
- 2▪▪.Dovey ZS, Nair SS, Chakravarty D, Tewari AK. Racial disparity in prostate cancer in the African American population with actionable ideas and novel immunotherapies. Cancer Rep (Hoboken) 2021; 4:e1340. [DOI] [PMC free article] [PubMed] [Google Scholar]; The authors provide a comprehensive review of the significant research in recent years that has examined the molecular and genomic reasons for unequal cancer burden in African American and Caucasian American populations and acknowledge the challenges that lie ahead.
- 3▪▪.Riviere P, Luterstein E, Kumar A, et al. Survival of African American and non-Hispanic white men with prostate cancer in an equal-access healthcare system. Cancer 2020; 126:1683–1690. [DOI] [PubMed] [Google Scholar]; Authors suggest that access to care is an important determinant of racial disparity.
- 4▪▪.Dess RT, Hartman HE, Mahal BA, et al. Association of black race with prostate cancer-specific and other-cause mortality. JAMA Oncol 2019; 5:975–983. [DOI] [PMC free article] [PubMed] [Google Scholar]; Authors show that a large disparity exists in other-cause mortality (OCM) for African–American men with nonmetastatic PCa.
- 5▪▪.Rayford W, Beksac AT, Alger J, et al. Comparative analysis of 1152 African-American and European-American men with prostate cancer identifies distinct genomic and immunological differences. Commun Biol 2021; 4:670. [DOI] [PMC free article] [PubMed] [Google Scholar]; Authors have performed an in-depth analysis of prostate tumour biology, from a large cohort of patients and identified critical genomic and immunological differences to shed more light on its contribution to incidence and outcome disparities.
- 6▪▪.Awasthi S, Berglund A, Abraham-Miranda J, et al. Comparative genomics reveals distinct immune-oncologic pathways in African American men with prostate cancer. Clin Cancer Res 2021; 27:320–329. [DOI] [PMC free article] [PubMed] [Google Scholar]; Authors identify key immune oncological pathways of African–American men with PCa.
- 7▪▪.Weiner AB, Vidotto T, Liu Y, et al. Plasma cells are enriched in localized prostate cancer in Black men and are associated with improved outcomes. Nat Commun 2021; 12:935. [DOI] [PMC free article] [PubMed] [Google Scholar]; Authors demonstrate that tumours of African–American men have higher plasma and NK cell activity propose that plasma cells could be potential markers for immune responsiveness.
- 8▪▪.Darst BF, Wan P, Sheng X, et al. A germline variant at 8q24 contributes to familial clustering of prostate cancer in men of African ancestry. Eur Urol 2020; 78:316–320. [DOI] [PMC free article] [PubMed] [Google Scholar]; Authors identify an important germline variant that contributes to familial clustering of PCa in men of African Ancestry.
- 9▪▪.Yuan J, Kensler KH, Hu Z, et al. Integrative comparison of the genomic and transcriptomic landscape between prostate cancer patients of predominantly African or European genetic ancestry. PLoS Genet 2020; 16:e1008641. [DOI] [PMC free article] [PubMed] [Google Scholar]; Authors show that a significant heterogeneity exists in prostate tumours of African–American and European American men and nominate them as a potential contributor of racial disparity.
- 10.Tang W, Wallace TA, Yi M, et al. IFNL4-DeltaG allele is associated with an interferon signature in tumors and survival of African-American men with prostate cancer. Clin Cancer Res 2018; 24:5471–5481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaur HB, Guedes LB, Lu J, et al. Association of tumor-infiltrating T-cell density with molecular subtype, racial ancestry and clinical outcomes in prostate cancer. Mod Pathol 2018; 31:1539–1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12▪▪.Faisal FA, Kaur HB, Tosoian JJ, et al. SPINK1 expression is enriched in African American prostate cancer but is not associated with altered immune infiltration or oncologic outcomes postprostatectomy. Prostate Cancer Prostatic Dis 2019; 22:552–559. [DOI] [PubMed] [Google Scholar]; Authors investigate role of SPINK1 and oncologic outcome in tumours of African--American men with PCa.
- 13.Yamoah K, Johnson MH, Choeurng V, et al. Novel biomarker signature that may predict aggressive disease in African American men with prostate cancer. J Clin Oncol 2015; 33:2789–2796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xiao J, Cohen P, Stern MC, et al. Mitochondrial biology and prostate cancer ethnic disparity. Carcinogenesis 2018; 39:1311–1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15▪▪.Sartor O, Armstrong AJ, Ahaghotu C, et al. Survival of African-American and Caucasian men after sipuleucel-T immunotherapy: outcomes from the PROCEED registry. Prostate Cancer Prostatic Dis 2020; 23:517–526. [DOI] [PMC free article] [PubMed] [Google Scholar]; Authors present an exploratory analysis of PROCEED registry and show that in patients who received sipuleucel-T immunotherapy, the overall survival was significantly different between African--Americans and whites.
- 16▪.Spratt DE, Alshalalfa M, Fishbane N, et al. Transcriptomic heterogeneity of androgen receptor activity defines a de novo low AR-active subclass in treatment naive primary prostate cancer. Clin Cancer Res 2019; 25:6721–6730. [DOI] [PMC free article] [PubMed] [Google Scholar]; Integrating transcriptomic data, the authors have identified a subtype of treatment-naïve primary prostate cancer with molecular characteristics of aggressive metastatic castrate-resistant prostate cancer mCRPC.
- 17.Gandaglia G, Briganti A, Clarke N, et al. Adjuvant and salvage radiotherapy after radical prostatectomy in prostate cancer patients. Eur Urol 2017; 72:689–709. [DOI] [PubMed] [Google Scholar]
- 18.Spratt DE, Dess RT, Hartman HE, et al. Androgen receptor activity and radiotherapeutic sensitivity in African-American men with prostate cancer: a large scale gene expression analysis and meta-analysis of RTOG trials. Int J Radiat Oncol Biol Phys 2018; 102:S3. [Google Scholar]
- 19.Friedlander DF, Trinh QD, Krasnova A, et al. Racial disparity in delivering definitive therapy for intermediate/high-risk localized prostate cancer: the impact of facility features and socioeconomic characteristics. Eur Urol 2018; 73:445–451. [DOI] [PubMed] [Google Scholar]
- 20.Peng H, Luo X. Prognostic significance of elevated pretreatment systemic inflammatory markers for patients with prostate cancer: a meta-analysis. Cancer Cell Int 2019; 19:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bell CN, Kerr J, Young JL. Associations between obesity, obesogenic environments, and structural racism vary by county-level racial composition. Int J Environ Res Public Health 2019; 16:861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Powell IJ, Dyson G, Land S, et al. Genes associated with prostate cancer are differentially expressed in African American and European American men. Cancer Epidemiol Biomarkers Prev 2013; 22:891–897. [DOI] [PMC free article] [PubMed] [Google Scholar]