ABSTRACT
Introduction and aims:
Guidelines for low back pain (LBP) management recommend patient education and exercises. GLA:D Back, a structured group-based patient-education exercise program for LBP, facilitates evidence-based care implementation. This study aimed to inform on the implementation processes, assessing clinician-related factors. Objectives were to describe profiles of implementers and nonimplementers by demographics, and responses to the tailored version of the Determinants of Implementation Behaviour Questionnaire (DIBQ-t) qualitatively explore clinician perspectives on implementation, and compare the results of the DIBQ-t with the interview data to evaluate their fit of integration for facilitators, barriers, and new insights.
Methods:
A mixed-methods parallel design study was conducted. Physiotherapists and chiropractors, educated in the GLA:D Back program, were asked to complete the DIBQ-t (measuring theoretical determinants of implementation) 6 months after their training. Implementers and nonimplementers of the program were selected for interviews. Qualitative data were used to understand clinicians’ viewpoints on implementation, providing a broader perspective on the quantitative data and exploring new aspects.
Results:
More physiotherapists than chiropractors implemented the program. Implementers responded more positively on most domains of the DIBQ-t. The interviews revealed three themes important for implementation: personal gain, practicalities, and buying-in on the program. Clinicians’ attitudes to the program appeared additionally as relevant to implementation.
Conclusion:
The profession of the clinician was associated with implementation behavior. Implementers and nonimplementers identified the same themes but perceived them as either positive or negative. Both groups reported high levels of knowledge and skills, indicating that training alone is insufficient for implementation.
Keywords: implementation, low back pain, mixed methods, primary care
What is known about the topic?
Guidelines for the management of people seeking care for LBP recommend patient education, advice to remain physically active and at work in addition to supervised exercise therapy.
A biopsychosocial approach to LBP is recommended, which requires clinicians to move away from a biomedical model of care; however, healthcare systems are fundamentally biomedically oriented.
Implementing guideline recommendations in primary care is challenging clinicians to change old routines in their clinical decision-making and practice.
What does this article add?
Profession was associated with implementation as there were more physiotherapists than chiropractors among the implementers; sex, age, and years of clinical experience were not associated with implementation.
Personal gain, practicalities, buying-in on the program, and clinicians’ attitudes toward the program were important for implementation.
High levels of knowledge and skills were reported by implementers and nonimplementers, indicating that training alone is insufficient for implementation.
Introduction
Implementation of clinical guidelines often involves a change in clinical practice, making clinicians an essential component of the implementation process.1,2 Moreover, the clinician's knowledge of, and attitudes toward, guidelines play a crucial role in successful implementation.3 Guidelines for managing people seeking care for low back pain (LBP) consistently recommend education about their condition, advice to remain physically active, stay at work, supervised exercise therapy, manual therapy, and cognitive behavioral therapy.
Moreover, a biopsychosocial approach to LBP is recommended, requiring clinicians to move away from the biomedical model of care.4–7 Implementing these guideline recommendations is challenging as healthcare systems are fundamentally oriented to a biomedical approach. Specifically, clinicians may recognize the importance of biopsychosocial factors but may perceive that screening for these is beyond their professional practice and skills.8–10 Moreover, clinicians tend to cling to established routines rather than integrating new recommendations into their clinical decision-making and practice.11–14
Therefore, to help implement guideline recommendations, a multidisciplinary group of clinicians and researchers developed GLA:D Back [GLA:D is a trademark owned by the University of Southern Denmark (SDU), Odense, Denmark], an evidence-based program for treating persistent or recurrent LBP.15–17 GLA:D Back was based on the same organizational frame as GLA:D for knee and hip patients, a successfully implemented program containing patient education and exercises18 and utilized the methodology for establishing best evidence of guideline implementation.19–21 In brief, GLA:D Back consists of three key elements: first, training of physiotherapists and chiropractors on a 2-day course to deliver structured, evidence-based patient education and exercises; second, delivery of the program at primary care clinics by these educated clinicians; and third, collecting data at clinician level and patient level in a registry.17
The Theoretical Domains Framework (TDF) has been used as the theoretical basis for identifying and assessing factors that may affect implementation.22 The TDF incorporates 33 psychological theories and 128 constructs that explore individual and organizational factors affecting the implementation of guidelines.23,24 Based on the TDF, the Determinants of Implementation Behaviour Questionnaire (DIBQ)25 was adapted into the tailored version of the DIBQ (DIBQ-t) to evaluate the implementation of GLA:D Back (accepted for publication).
However, more knowledge is needed about factors influencing implementation to inform how implementation might be improved by targeting clinician-related factors.
Methods
Aim
The overall aim was to assess clinician-related factors in implementing a structured program in primary health care. Specific objectives were: first, to describe profiles of the implementers, defined as those beginning to enroll patients in the GLA: D Back program within 6 months after participation in the GLA:D Back course, and nonimplementers by comparing their demographics and results of the DIBQ-t; second, to qualitatively explore clinician perspectives of the implementation process; and third, to compare the results of the DIBQ-t with the interview data to evaluate their fit of integration for facilitators, barriers as well as new insights.
Design
The current study used a mixed-methods parallel design, with independent analyses of a cross-sectional self-reported questionnaire and face-to-face and group interviews. The results were reported with a contiguous approach to integration.26 These analyses were preceded by an integrated discussion on the coherence of the quantitative and qualitative data. The Good Reporting of A Mixed Methods Study framework27 was used for this study.
Context and participants
Participants were physiotherapists and chiropractors working in primary care clinics in Denmark who had completed the 2-day GLA:D Back certification course. In this study, we only included clinicians who were the sole deliverer of GLA:D Back at their clinic. Identification numbers in the registry were connected to clinics and not the clinician. Therefore, clinicians could be miscategorized as implementer/nonimplementer at clinics with multiple GLA:D Back deliverers, as several clinicians could deliver the program using the same identification number. Clinicians were categorized as implementers based on whether they registered at least one patient within 6 months after they had attended a GLA:D Back course. Clinicians who did not register a single patient were categorized as nonimplementers.
For the interviews with the implementers, participants were selected from the 2017 cohort (described below). Inclusion criteria were as follows: started the GLA:D Back program by enrolling patients within 6 months after the course, either very positive or negative views as scored by the DIBQ-t, and able to participate in the interviews. Moreover, a diverse presentation of sexes, employment statuses (clinic owner, employed), and years of experience were anticipated. For the interviews with nonimplementers, participants of the 2018 cohort (described below) were selected with the criteria to present both sexes, different employment statuses (clinic owner, employed), and various years of experience.
The GLA:D Back intervention
GLA:D Back is targeting patients with persistent or recurrent LBP. The program consists of group-based patient education and supervised exercise sessions with the overall aim to improve the patients’ ability to self-manage.17 Clinicians can adapt GLA:D Back to their particular setting and the needs of the individual patient; however, specific elements cannot be altered: first, the program begins and ends with individual goal setting and physical tests; second, two patient education sessions followed by 8 weeks of supervised exercises, twice weekly; third, specified key messages, that is, stating that pain is not a sign of harm; fourth, a behavioral model of balancing demands and capacity rather than a biomedical model; fifth, the encouragement of patients to explore movements instead of clinician instruction to perform exercises in a ‘correct’ way; and sixth, entering data (patient demographics, test results, and patient-set goals) in the clinical register.
The implementation strategy
Reaching clinicians
In 2017, clinicians (chiropractors and physiotherapists) with a known interest in treating patients with persistent LBP were invited to participate in the feasibility study. All clinicians (n = 31, from nine clinics) accepted the invitation.15 In February 2018, course attendance was open to all clinicians in Denmark. The Danish Physiotherapy, the Danish Chiropractors’ associations, and some physiotherapy special interest groups posted course announcements. The GLA:D Back research team also promoted the course and registration form for the course on the GLA:D Back website, on Facebook, LinkedIn, and Twitter. Furthermore, clinicians who use the GLA:D register for knee/hip patients were notified when they logged on to the registry. The spread, reach, and adoption of GLA:D Back are studied and reported elsewhere (in review).
Education and certification of clinicians
Clinicians were trained during a 2-day course (7 h/day) by the program developers and experienced GLA:D Back clinicians.15 The course's primary aim was to give clinicians tools and competencies that support implementing the GLA:D Back program in their practice. The learning goals were obtained using different teaching elements, including lecturing, persuasion and modeling through examples and skills training. The course cost approximately 550€ (2018). Clinicians who completed the course and indicated their intent to deliver GLA:D Back at their clinic were listed as certified clinicians on the GLA:D Back website (http://gladryg.sdu.dk/). Because GLA:D is a registered trademark, only clinicians trained at SDU can use the brand.
Implementation facilitators
Clinicians were given access to ready-made patient educational materials, exercise programs, and written suggestions of language that could be used in the supervision of exercises to support implementation. To promote the program at their clinic, they received GLA:D Back t-shirts and two posters with key messages from the patient education and an overview of the exercises. To assist uniform marketing of the program, clinicians received patient information leaflets and flyers for general practitioners to advertise the program in their community. Their clinic names and logos could be added to these materials.15
Quantitative data
Data collection, variables
Demographic data [sex, age (25–35, 36–45, or ≥46 years), profession (physiotherapist or chiropractor), years of experience (0–5, 6–10, 11–15, 16–20, >20 years)] were collected electronically via Research Electronic Data Capture (REDCap), licensed by the Open Patient data Explorative Network (OPEN) from all clinicians signing up to a GLA:D Back course before they attended. The clinicians completed the DIBQ-t 6 months after the course. The original DIBQ was developed to evaluate the implementation processes of guideline recommendations based upon the TDF domains.28 The questionnaire was translated into Danish, tailored, and validated to GLA:D Back, resulting in the DIBQ-t (submitted). In short, first, the DIBQ was forward translated, then adapted into the DIBQ-t using qualitative face validity by the project team and quantitative content validity, tested by 16 experts using the content validity index.29 Finally, feasibility and construct validity were determined using confirmatory factor analyses based upon data from DIBQ-t collected from 598 clinicians. The final DIBQ-t included 28 items describing 10 of the original 18 DIBQ domains. Feasibility was considered acceptable as only 2‰ of the items were missing. The confirmatory factor analyses showed good fit after removing two items with the lowest domain loading. The DIBQ-t maintained linkage to all domains within the Behavioral Change Wheel. The items can be grouped into 10 domains: knowledge (two items), skills (one item), beliefs about capability (six items), beliefs about consequences (four items), innovation (four items), patients (two items), intentions (one item), organization (two items), social influences (three items), and behavioral regulation (three items). The domains are described in Table 1.30
Table 1.
Description of domains and constructs of tailored version Determinants of Implementation Behaviour Questionnaire to evaluate implementation of GLA:D Back
| Domain – construct(s) | Description | An example statement |
| Knowledge – knowledge, professional role | An awareness of the existence of GLA:D Back, knowledge of the procedures and tasks related to the delivery of GLA:D Back | I know how to deliver GLA:D Back following the program |
| Skills – skills | Ability or skills to deliver GLA:D Back acquired through practice | I have the skills to deliver GLA:D Back |
| Beliefs about capabilities – self-efficacy, perceived behavioral control | Acceptance of one's ability to deliver GLA:D Back, thus it can be used constructively | I am confident that I can deliver GLA:D Back |
| Beliefs about consequences – attitudes, outcome expectancies | Acceptance of outcomes of the use of GLA:D Back | GLA:D Back will help participants to be able to cope better with their back problems |
| Intentions – intentions, motivation | A conscious decision to use GLA:D Back | I intend to deliver GLA:D Back in the next 3 months |
| Innovation – resources | Adaptation of GLA:D Back toward the patient or context in which it is delivered | GLA:D Back is compatible with daily practice |
| Patients – outcome expectations | Patients’ perspectives toward the effect of GLA:D Back | Participants of GLA:D Back are motivated |
| Organization – resources | The circumstances of a person's situation or environment that discourages or encourages the use of skills and abilities to deliver GLA:D Back | In the organization I work, all necessary resources are available to deliver GLA:D Back |
| Social influences – social support, subjective norms | Interpersonal processes that can cause the change of thoughts, feelings, related to the implementation of GLA:D Back | Most people who are important to me think that I should deliver GLA:D Back following the program |
| Behavioral regulations – action planning | Anything aimed at managing or changing actions related to the implementation of GLA:D Back | I have a clear plan of how I will deliver GLA:D Back |
Quantitative analyses
Associations between demographics (sex, age, profession, years’ experience) and implementation were tested with independent t test (age) and Chi-squared (categorical demographic variables). For each item of the DIBQ, the response categories were dichotomized (strongly agree and agree versus neither, disagree and strongly disagree). For each domain, we tallied the number of positive items, meaning that for a clinician to be classified as positive for the domain, most of their responses had to be in agreement with the statement (i.e., strongly agree or agree). Likewise, to be classified as negative for the domain, the majority of their responses had to be in disagreement or be neutral in relation to the statement. The domains with an equal number of items (i.e., knowledge, capability, consequences, innovation, organization, and patient) could have an equal number of items in agreement and disagreement with the statements. When this occurred, the clinician was classified as being ‘tied’. If a clinician missed at least one item from a domain, their responses for that domain were excluded. All statistical analyses were carried out with the Statistical Package for Social Sciences (v. 25.0.0; IBM, New York, New York, USA).
Qualitative data
Data collection
The investigators developed a semistructured interview guide based upon the DIBQ-t domains used in the study combined with explorative questions (Table 2). A purposive, maximum variation sample was drawn based upon the results of the DIBQ-t to identify clinicians with strong positive or negative opinions.31 Eligible participants were then approached individually and informed by the research assistant about the interview's purpose and asked to participate. Informed written consent was obtained before the interview. Interviews with the four implementers were planned as semistructured interviews and, for practical reasons, conducted by a research assistant as two pair-wise interviews at the university (L.T.). These interviews were conducted in March 2018 and October 2018 and lasted approximately 1 h.
Table 2.
Interview guide for implementers and nonimplementers
| Theme | Questions | Constructs |
| Implementers | ||
| Introduction | We are going to talk about GLA:D Back. Do you have some general thoughts you would like to share with us? | Implementation in general |
| Implementation | Will you tell about your experiences with GLA:D Back? | Experiences |
| Implementation/motivation | What was the reason that you signed up for the GLA:D Back course? (What were your expectations attending the course?) | Expectations, motivation |
| Implementation intervention | Can you share your thoughts regarding the course? In which way do you use the knowledge and skills delivered at the GLA:D Back course? | Evaluation of the course Knowledge, skills |
| Implementation/internal factors | Which factors, at a personal level, have an influence on your capabilities of delivering GLA:DBack Can you tell how you perceived the GLA:D Back course to enable you to deliver GLA:D Back to the patients | Self-efficacy Knowledge, skills |
| Implementation/external factors | Which other factors at the clinic/patients/your colleagues’ influence make it harder/easier to delivery of GLA:D Back? Please expand on this | Context Organization Patients’ perspectives |
| Intentions | What are your plans for using GLA:D Back? Are there factors that influence your choice of future use of GLA:D Back? If you look one year ahead, which factors influence the fact that you still use GLA:D Back? Please expand your thoughts on this | Sustainability, continuing implementing Intentions |
| Attitudes | How is your view in general for the management of patients with nonspecific lumbar problems? Has GLA:D Back changed the way you treat back pain patients? In what way? Do you expect other consequences of using GLA:D Back than those related to patients? Can you describe the effects of GLA:D Back on patients? What do you think patients experience by attending in GLA:D Back? | A biomedical or behavioral approach Internal factors, Beliefs in consequences, Patients – expected perception |
| Norms | Have others (colleagues, patients, doctors, leads, etc.) opinions about you using GLA:D Back? Does this matter to you? | Social and professional norms from colleagues, patients and acknowledgement |
| Perceived behavioral control | What knowledge, tools, and capabilities do you need to deliver GLA:D Back? What are your thoughts about the tools presented at the GLA:D Back course? How do you find that you are capable of delivering GLA:D Back? | Knowledge and skills Beliefs about capability |
| Content course | What experiences (good, bad, others) do you have in: Selection of patients to enter the program Testing the patients Doing the patient education Training patients with the exercises Do the evaluation tests | Practical details of delivering GLA:D Back Innovation |
| Nonimplementers | ||
| Implementation/motivation | What was the reason that you signed up for the GLA:D Back course? (What were your expectations attending the course?) What was the reason that you intended to use GLA:D Back after the course? | Expectations, motivation |
| Implementation intervention Content course | Can you share your thoughts regarding the course? Did you feel capable to deliver GLA:D Back after the course? | Evaluation of the course Practical details of delivering GLA:D Back |
| Attitudes | What are your overall thoughts on the GLA:D Back program? | Beliefs about consequences, Patients’ perspectives Beliefs about capability |
| Implementation/external factors, internal factors, norms | What are the reasons that you did not implement GLA:D Back? Physical framework – Management's attitude – Colleagues’ attitude – Patients’ reaction – Resources | Context Organization Patients’ perspectives |
| Implementation intervention | What do you think is most effective: the existing program you have for your low back pain patients or GLA:D Back? Why? | Beliefs about consequences, Patients’ perspectives |
| Perceived behavioral control | Have you used parts of GLA:D Back in your daily practice? If so, which? | Knowledge and skills Beliefs about capability |
| Intentions | Do you plan to use GLA:D Back at some time? What is that decision depending on? | Intentions |
Semistructured interviews were conducted with five nonimplementers. The first six on a list with 20 names meeting these criteria were contacted; one declined for practical reasons. These interviews were conducted individually at the participants’ clinic during January and February 2019 and lasted approximately 30–50 min each. The semistructured interview guide was adapted to the nonimplementers, for example, added questions about not implementing the program.
Qualitative analyses
Two paired interviews with implementers, and five individual interviews with nonimplementers were analyzed for thematic emergence by two researchers (I.R. and a research assistant blinded to the DIBQ-t domains).32 Once recorded and transcribed verbatim, transcripts were read and re-read for familiarization. Each transcript was then coded using both inductive and deductive coding guided by the question: ‘How is this feedback relevant to the implementation process of GLA:D Back?’ and predefined codes related to the 10 DIBQ-t domains. A codebook was extracted from the first document and applied to the next transcript. As more codes emerged, the codebook was adjusted and then reapplied to prior documents. This iterative process was continued until all documents were with the final codebook. Once codified, the data were further abstracted into code families and eventually themed by reviewing associations within and between participants, using co-occurring codes and code families. The analysis process was managed using the Atlas.ti version 8 qualitative data analysis software program (ATLAS.ti, Berlin, Germany). Interview and questionnaire data were collected in Danish, and subsequently translated into English.
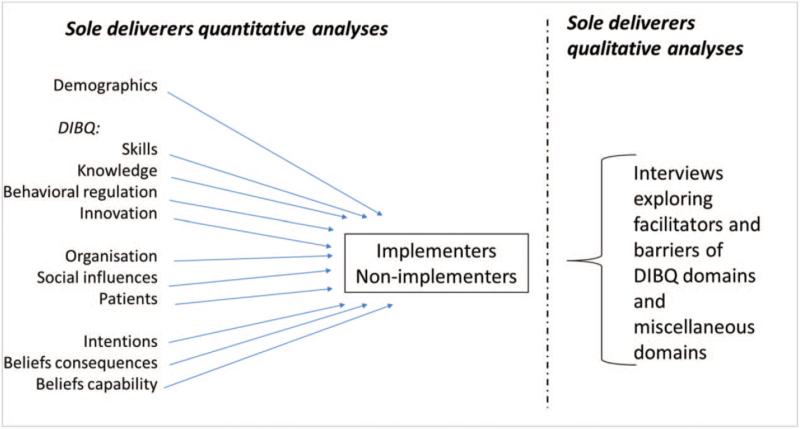
Integration of qualitative and quantitative data
The two datasets were compared and linked to assess the fit of integration (Fig. 1). First, possible facilitators or barriers of the implementation identified in the interviews were obtained by a discussion between the investigators. These were compared with the results of DIBQ-t assessing their fit of integration for facilitators and barriers. Second, possible expansions or insights through new aspects were looked for.26 The quantitative and qualitative datasets are presented in an overview to compare the results of both.
Figure 1.
Overview of the design.
Results
Demographics and the tailored version of the Determinants of Implementation Behaviour Questionnaire
In total, 131 sole deliverers (25% of the total cohort) completed the course. Of these, 63 implemented the program and 68 did not. The response rate at 6 months after the course for DIBQ-t was 73 and 60%, respectively, for the two groups. Comparing demographics, the most substantial difference between implementers and nonimplementers was profession. A larger proportion of implementers were physiotherapists (95%) compared with nonimplementers (72%) (Table 3).
Table 3.
Demographics of implementers and nonimplementers of GLA:D Back of sole deliverers
| Implementers, n = 63 | Nonimplementers, n = 68 | P value | |
| Male, n (%) | 18 (28.6) | 23 (33.8) | 0.52 |
| Profession physiotherapist/chiropractor, n (%) | 60 (95.2)/3 (4.8) | 49 (72.1)/19 (27.9) | <0.01 |
| Age group mean years/SD | 39.8 (11.1) | 40.8 (10.3) | 0.61 |
| 25–35 years, n (%) | 25 (39.7) | 24 (35.3) | |
| 36–45 years, n (%) | 18 (28.6) | 22 (32.4) | |
| 46–years, n (%) | 20 (31.7) | 22 (32.4) | |
| Years’ experience | 0.75 | ||
| 0–5, n (%) | 21 (33.3) | 20 (29.4) | |
| 6–10, n (%) | 10 (15.9) | 16 (23.5) | |
| 11–15, n (%) | 8 (12.7) | 10 (14.7) | |
| 16–20, n (%) | 9 (14.3) | 8 (11.8) | |
| 20+, n (%) | 15 (23.8) | 14 (20.6) |
Implementers were observed to be more positive across all domains as compared with nonimplementers (Table 4). Most implementers and nonimplementers had positive perceptions of the domains ‘Knowledge’ (89 versus 77%) and ‘Skills’ (96 versus 84%). The domains with most implementers with a neutral/negative perception of implementation were ‘Social influences’ (49% neutral/negative). The domain ‘Patients’ had most nonimplementers with neutral/negative responses (85%). For ‘Social influences’, positive and neutral/negative perception were observed with similar frequencies (51 versus 49%). The domain ‘Organization’ had the highest numbers of tied in both groups, with 24% of the implementers and 30% of the nonimplementers not identifying the domain as either positive or neutral/negative.
Table 4.
Implementers’/nonimplementers’ perception of domains being positive, negative, or tied
| Implementers, n = 46 | Nonimplementers, n = 43 | |||||||
| Domain (no. of items) | n Excluded from analyses | Positive, n (%) | Tied, n (%) | Neutral/negative, n (%) | n Excluded from analyses | Positive, n (%) | Tied, n (%) | Neutral/negative, n (%) |
| Knowledge (2) | 0 | 41 (89) | 3 (7) | 2 (4) | 0 | 33 (77) | 4 (9) | 6 (14) |
| Skills (1) | 0 | 44 (96) | 2 (4) | 0 | 36 (84) | 7 (16) | ||
| Beliefs about capability (6) | 0 | 34 (74) | 6 (13) | 6 (13) | 2 | 14 (34) | 4 (10) | 23 (56) |
| Beliefs about consequences (4) | 0 | 35 (76) | 4 (9) | 7 (15) | 1 | 13 (31) | 3 (7) | 26 (62) |
| Intentions (1) | 0 | 40 (87) | 6 (13) | 1 | 23 (55) | 19 (45) | ||
| Innovations (4) | 0 | 38 (83) | 4 (9) | 4 (9) | 1 | 20 (48) | 6 (14) | 16 (38) |
| Patients (2) | 0 | 36 (78) | 3 (7) | 7 (15) | 2 | 3 (7) | 1 (2) | 35 (85) |
| Organizations (2) | 0 | 33 (72) | 11 (24) | 2 (4) | 3 | 16 (40) | 12 (30) | 12 (30) |
| Social influences (3) | 1 | 23 (51) | 22 (49) | 3 | 18 (45) | 22 (55) | ||
| Behavioral regulation (3) | 2 | 32 (73) | 12 (27) | 2 | 19 (46) | 24 (59) | ||
Positive: the majority of the responses in agreement with the statements of the domain. Tied: an equal number of items in agreement and disagreement with the statements of the domain. Neutral/negative: the majority of the responses neutral or in disagreement with the statements of the domain. Grey cells: when tied not possible (impossible to have an equal number of positive and negative items for the domain, or single item domains).
Interviews
Four implementers, three females and one male aged 28–57 years, with 1–28 years experience, were interviewed. Two were chiropractors; two were physiotherapists, equally divided by employment as clinic owners or employees. Five nonimplementers, all physiotherapists, were interviewed, two males and three females, aged 29–61, with 3–36 years of experience; two were clinic owners, and three were employees.
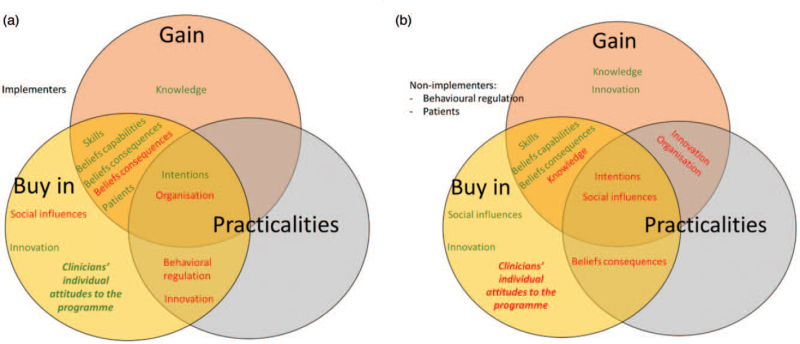
Three overall themes emerged from the interviews: ‘Gain’, ‘Practicalities’, and ‘Buying-in’. Quotes supporting the themes are provided in a later section. Both implementers and nonimplementers addressed all DIBQ-t domains except the domains ‘Patients’ and ‘Behavioral regulation’; those were commented on by the implementers only (Fig. 2). Some of the domains were identified as facilitators or barriers, some both. This was partly dependent on the respondent being an implementer or not. A new aspect of importance for the implementation process not covered by DIBQ-t domains was added: ‘Clinicians’ individual attitudes to the program’ on the program.
Figure 2.
Domains divided by themes, identified implementation-facilitators (green), or barriers (red) for implementers, nonimplementers.
Gain
Gain was the personal gain of implementing the program, that is, financial gain, success with patients or strengthened professional identity. Facilitators for implementation for both implementers and nonimplementers were personal gains such as enhanced skills, knowledge, and participating in a research project. The clinicians in both groups also gained personally from the program by experiencing positive feelings about their capability to deliver the program. Implementers expressed personal gains by getting positive emotions as patients benefited from the program. Loss of potential gain by using resources, mainly time, was mentioned as a barrier for implementation by both implementers and nonimplementers. Barriers for some implementers were also not achieving economic profit by implementing the program. Nonimplementers also noted the absence of new knowledge as part of the program as a lack of gain and the inability to adapt the program to their settings as they experienced the program being too rigid. They also mentioned that giving patients more responsibility in performing the exercises resulted in losing their professional identity. This related to an essential part of the program: clinicians encourage patients to explore the performance of the exercises at an individual level instead of being prescribed by a clinician.
Practicalities
Practicalities are any practical circumstance that influence implementation. Factors related to practicalities were nearly all identified as barriers. Several implementers and nonimplementers mentioned patient recruitment (lack of patients to participate in the program) and setting up the program in daily schedules (time) as barriers. Moreover, both groups felt uncertain as to what degree the program could be adapted to the individual patient. Implementers felt challenged in planning the different aspects of the delivery, that is, online registration of patient demographics and test results in the database. Another barrier was that general practitioners had little knowledge of the program and, therefore, did not refer patients.
Buying-in
Buying-in is defined as clinicians’ expressing reflections on determinants of implementation related to their acceptance and support of the program. Facilitators for implementation for both implementers and nonimplementers were their beliefs about being skilled and capable of delivering the program. The implementers also experienced the program's positive effects on participating patients as facilitating, which reinforced their buying-in on the program. Some implementers mentioned that the program was adaptable to patients’ needs and intended to continue using it. Nonimplementers mentioned the involvement with GLA:D Back as a brand as a facilitator. Barriers related to this theme for the implementation by implementers was their tendency to stick to habitual behaviors.
Clinicians’ individual attitudes to the program
The current new aspect, not covered by other DIBQ-t domains, included items concerning the novelty of the content of the program, aspects of the evidence-based foundation of the program, and alignment of the program with clinicians’ own perspectives on LBP.
In this regard, facilitators for implementation were clinicians wanting to deliver an evidence-based intervention, and alignment of the program's behavioral approach with their own attitudes and beliefs of patient self-management of LBP. ‘But the knowledge that this works, that the patients personally can do a great deal for their LBP. This is a good product we are trying to sell to the patient. We do this for the patients’ sake. We don’t do it, to make a lot of money.’ (D2:100). There were statements related to the program as a whole, and the exercises and patient education separately illustrated clinicians’ positive perspectives on the program. ‘It will be most optimal if everyone with unspecific LBP, of course not the acute, but everyone who has the recurring problems, or chronic would receive GLA:D Back to have the best treatment. They should all just exercise that way.’ (D2:157).
Barriers for nonimplementers were the opposite: the program was perceived to lack an evidence-based foundation ‘It simply must be a proper research project, this simply means that there are one, two, three interventions that you try to measure against each other. And that can be done. Then I would join in. I can promise you that.’ (D12:34). Moreover, the perception that the program was not different from their usual practice (lack of novelty) influenced implementation. ‘Because we already did these exercises, and we had a hard time seeing the exercises were better than what we did’. (D12:19). Some nonimplementers mentioned a different view on management of LBP. Consequently, their professional views did not agree with GLA:D Back. Finally, some nonimplementers (physiotherapists) considered being taught by chiropractors a barrier.
Integration of interviews with the tailored version of the Determinants of Implementation Behaviour Questionnaire
Comparing the interviews with the DIBQ-t domains (Table 5) illustrated that the implementers identified more potential facilitators in the interviews across the three interview themes than the nonimplementers. In contrast, nonimplementers identified more barriers than implementers did (Table 5).
Table 5.
Domains indicated by implementers/nonimplementers during interviews as facilitator (+) or barrier (−), distributed across themes
| Implementers | Nonimplementers | |||||
| Themes | Gain | Practicalities | Buying in | Gain | Practicalities | Buying in |
| DIBQ-t domains | ||||||
| Knowledge | + | +/− | − | |||
| Skills | + | + | + | + | ||
| Beliefs cap. | + | + | + | + | ||
| Beliefs cons. | +/– | +/− | + | − | +/− | |
| Intentions | + | + | +/− | − | − | − |
| Innovations | − | + | +/− | − | ||
| Patients | + | + | ||||
| Organization | − | − | − | − | ||
| Social infl. | − | − | − | +/− | ||
| Beh. Reg. | − | − | ||||
| New | ||||||
| Clinicians’ individual attitudes to the program | + | − | ||||
Beh. Reg, behavioral regulations; Beliefs cap, beliefs about capabilities; Beliefs cons., beliefs about consequences; DIBQ-t, tailored version of the Determinants of Implementation Behaviour Questionnaire; Social infl., social influences.
Knowledge
Between implementers and nonimplementers, 89 and 77% responded positively to DIBQ-t items in the domain ‘Knowledge’. The interviews confirmed the quantitative results indicating that the clinicians knew how to use the program. Knowledge derived from the course: ‘The material of the program and the patient education material, it makes you are ready to go’ (D2:45), but also former education and experience were mentioned to help implementation. GLA:D Back was developed to integrate patient education with exercises to help patients explore the exercises individually. However, a barrier for the nonimplementers in the knowledge domain was a misunderstanding that GLA:D Back was meant as an exercise program only, with standard exercises performed in ‘one correct manner’. ‘I think it's uninspiring. … They (the clinicians delivering GLA:D Back) become more or less programmed to do a standard routine’. (D10:37).
Skills
Results of DIBQ-t in the domain ‘Skills’ were that 96% of the implementers and 84% of the nonimplementers responded positively, resembling the positive views on the domain in the interviews. ‘The words and the examples in general (used in the patient education), I think were some of the best of the course’. (D2:54). Still, communication skills were seen as a challenge: ‘… it is not to dismiss (the patients’ back problem) by saying, ‘it's just a mental problem’, that's the tricky part, I think. How to communicate that’. (D2:193).
Beliefs about capability
In the DIBQ-t domain ‘Beliefs about capability’, 56% of nonimplementers had overall negative beliefs related to the domain. The interviews reflected the DIBQ-t results, illustrating contrasting results between implementers and nonimplementers. Implementers mentioned that GLA:D Back was not very different from usual practice. The materials of the program (e.g., slides for patient education and an exercise program) were easy to apply. ‘It is not because it's very different to what we’ve done in the past. But it is a great program to have for these (chronic low back pain patients) people. I don’t want to be without it’. (D2:34). In contrast, some nonimplementers mentioned uncertainty of how the program, both patient education and exercises, could be adapted to the individual patient: ‘So, I have doubts on how much one may change the exercises’ (D13:28).
Beliefs about consequences
‘Beliefs about consequences’ resulted in differences between the two groups: 76% of the implementers responded positive, versus 31% of the nonimplementers. This was exemplified in the interviews where implementers appreciated the thought of being part of a research project. ‘This is a project where we enter data, and it is used for research purposes. People like that too. I think it's a good thing to join’. (D2:117). Moreover, they stated that the exercises and patient education helped decrease fear of movement and improve understanding of coping with their LBP. ‘I think one of the most important things is that patients learn to move and exercise, and they can feel it is OK to do so. They are afraid to use their body. We can teach them that. That, I think is a big mission.’ (D3:50). Some implementers mentioned that they did not expect a financial benefit by using the program which hindered implementation. ‘So, don’t expect to make a big profit on this (GLA:D Back) because you don’t.’ (D2:67). Finally, there were some rather fierce statements of nonimplementers feeling dominated by chiropractors, which meant that they did not wish to be part of the program. ‘Well, it was about chiropractors versus physiotherapists. It was quite obvious that physiotherapists should be hired as their supporting staff.’ (D12:7).
Intentions
The DIBQ-t results showed that 55% of the nonimplementers had an overall positive perception with items related to intentions, although they had not implemented the program. The interviews revealed possible reasons for this. Time aspects was a barrier for some: ‘I have no doubts that it will probably work when we have started, but in a busy weekday, time is scarce.’ (D14:32). Competition at the clinic with the existing LBP group-exercises delivered by their colleagues could also weaken the intention to implement: ‘We are colleagues and competitors at the same time. So, if I ask everyone in the clinic to give me all their back patients because it is best for the patient, then, … So, we are having a bit of a problem that not one of us wants to talk about.’ (D14:28). Finally, the lack of patients influenced the intention to use GLA:D Back. ‘Well, there was no interest from patients coming to the clinic in compared with the expenses I used on marketing.’ (D10:86). The interviews disclosed that implementers who intended to continue using GLA:D Back in the future perceived the program as a high-quality treatment for LBP patients. ‘We continue to use GLA:D Back. It just is a vital part of good quality treatment, treatment of back patients’ (2:198).
Innovation
Among nonimplementers, 48% rated the DIBQ-t domain about innovation positive, and 38% negative. The interviews exemplified this as some nonimplementers believed clinicians should do specific corrections of the exercises. ‘We are very specific (in our dealing with exercises). This (GLA:D Back) is not specific at all, not at all. It's just: ‘What do you (the patient) feel?’ ‘Progress or regress the exercises as you like’ or, ‘What do YOU think is best for you?’ But when one is as specific and strict (in supervising exercises) as we are here, that simply makes a difference to our patients’. (D12:20). Other nonimplementers used the principles of the program to patients not enrolled in GLA:D Back. ‘I have it at the back of my mind; both exercises, at least elements of it, are included in my treatment of LBP patients. But also, the pain education, that it (low back pain) is not dangerous. And get them to understand that they can do exercises’. (D3:79). The possibility to adapt the program to the individual patient was perceived as a facilitator by the implementers - ‘We try fairly strictly to stick to the exercises. But we also have those where it does not fit. Maybe we then do it in a slightly different way, but still, l it is roughly the same exercise’ (D3:20) – and as a barrier by nonimplementers that understood the program to be rigid (quoted earlier). The intension of having the patients take ownership of their training program to enhance self-management was perceived both as a facilitator and a barrier.
Patients
Nonimplementers did not mention the domain ‘Patients’ during the interviews, which was expected because they had no experiences with patients’ responses to GLA:D Back. The domain had the highest number of neutral/negative responses (85%) among nonimplementers in the DIBQ-t, illustrating that they did not expect the program to have positive effects. Implementers observed positive results with the patients, both regarding their understanding of LBP and coping with LBP. ‘But it is also my impression that the information we give in patient education and along the way in dealing with their pain, that it changes them. Moreover, this is shown in their behavior’. (D2:186). They motivated their patients based upon the experiences with prior groups and by referring to the evidence when talking to patients: ‘There are studies that show this is what it takes to reduce relapses. We can see, in our former groups, that this is truly working, it's really good’. (D2:174). Clinicians were challenged when patients came to the program with a biomedical understanding of their back pain. ‘Once they have been told that the cartilage is gone, it is as if they hear nothing else, so they do not believe they can get better’. (D14:40). Finally, the out-of-pocket expense was mentioned as a patient factor potentially hindering participation in GLA:D Back.
Organization
Both groups mentioned ‘Organizational’ factors as negative for implementation in the interviews, but the DIBQ-t results reported most of the implementers responding positively on items related to organization. Both groups mentioned the perception of several organizational aspects as barriers for implementation, such as digital registration, staff change at the clinic, and recruitment of patients. Moreover, external collaborators such as general practitioners not being well informed about GLA:D Back was mentioned as a barrier. A positive organizational aspect for clinicians was the possibility to vary the workday, getting away from delivering passive treatments. ‘Great with some variety. I like to have a GLA:D Back group and then have patients, and then maybe you treat a baby. So, it provides variety, not just seeing six patients an hour, hour after hour for 37 h/week’. (D2:68).
Social influences
None of the groups had a strong tendency in either a positive or negative direction for this domain based upon DIBQ-t. The interviews also did not reveal that the influence of colleagues was important. Reimbursement by the Danish universal health care was mentioned as a possible factor for implementation if providing group-based exercises was required at a governmental level. Some clinicians were met with scepticism from external colleagues. ‘I have defended it occasionally. Someone has been more sceptical, …’ (D2:92). But none of the respondents mentioned this as an important barrier for implementation.
Behavioral regulation
The domain had a high number of neutral/negative responses (59%) among nonimplementers in the DIBQ-t but was not mentioned by the nonimplementers in the interviews. This was predictable, as they had no experiences with the planning of the program. Implementers mentioned different models of changing daily routines and planning the program in the clinics’ schedule. ‘So, we have simply drawn a schedule so that we write down in advance the dates and then people can go in and see if it fits their calendar.’ (D2:23).
Clinicians’ individual attitudes to the program
The new aspect covered items related to the novelty of the content of the program, aspects of the evidence-based foundation of the program, and alignment of the program with clinicians’ perspectives on LBP and expanded the insight on implementation processes. The qualitative data categorized in DIBQ-t domains and the reflections on potential facilitators or barriers are presented in detail below.
Discussion
Summary of the results
The current study was, to our knowledge, the first mixed-methods study conducted to investigate clinician-level factors related to implementing evidence-based care for LBP patients in primary care. There were significant differences between implementers and nonimplementers identified by the DIBQ-t, and qualitative data deepened our understanding of why some clinicians were more effective in implementing the GLA:D Back program than others.
Findings in relation to other studies
The overall facilitating role of most domains of the DIBQ-t was also reported in a Swedish study using the same questionnaire.33 The current study findings were also in concordance with a recent implementation study in the context of LBP, which identified knowledge, beliefs about capabilities, and beliefs about consequences as relevant to implementing an online training program with a cognitive behavioral approach for LBP.34 However, contrary to our investigation, social influences were identified as a relevant factor in two previous studies.34,35 Our data suggested clinicians rated ‘Social Influences’ low as a potential facilitator for implementation, supported by the interviews.
Organizational factors were documented as a key factor for the implementation of advanced musculoskeletal physiotherapy.36 This was in line with our results, as the domain was considered a barrier to implementation in both groups. Previous studies have also identified organizational factors such as time constraints and financial aspects as barriers to implementing physical activity programs in primary care in a Delphi study.35,37 More specifically, the Delphi study mentioned above reported that items related to knowledge, skills, and attitudes toward the intervention are important factors for implementation.37 Both implementers and nonimplementers reported high scores on items in the DIBQ-t domains ‘Knowledge’ and ‘Skills’, indicating that the perception of having sufficient knowledge and skills had little influence on implementation, which differs from the results of the Delphi study.
Clinicians’ attitudes to the program emerged from the interviews as either a barrier or a facilitator by implementers and nonimplementers, and therefore an important aspect of implementation and in line with the former study.37
‘Behavioral regulation’ was not identified as of high importance for implementation. This is perhaps somewhat surprising, as this is one of the most important predictors for completeness and high quality in using a physical activity program in physiotherapy practice38 and implementing evidence-based care for type 2 diabetes in primary care.39 This discrepancy may relate to the program being a ‘ready-to-go package’ and the delivery of the program described in detail. In contrast, other studies used less detailed programs. Therefore, the behavioral regulation and action planning of the program's delivery might not be an important issue in GLA:D Back. It is essential to bear in mind that we reported cross-sectional data, and no consideration was given to causal connections or predictions.
Strengths, limitations, and generalizability
The study presents new knowledge of implementing an evidence-based program in primary care using a mixed-methods approach, with interviews adding information to quantitative results. To minimize bias and encourage participants to speak freely, nonimplementers were not interviewed by a member of the GLA:D Back team. The nonimplementers were hard to recruit for the interviews. Therefore, they were interviewed individually at their work place to avoid unwillingness to participate, as they might be reluctant to use time on research related to a program they hadn’t implemented. The interviews with the nonimplementers were performed individually and with implementers in pairs, grouped by profession. Interviewing pairs can prompt the respondents to be more nuanced and gives them more autonomy.40 The reason for using pair interviews with implementers and individual interviews with nonimplementers was, therefore, pragmatic as nonimplementers were more unwilling to adapt their schedules for interviews. However, applying different interviews may give a broader understanding of the reasons for implementing.41
There are some study limitations to consider. First, the quantitative results build upon the records of sole deliverers only. Comparing sole deliverers’ demographics with deliverers from clinics with multiple GLA:D Back clinicians showed that they varied on two aspects. Profession: physiotherapist/chiropractors ratio for multideliverers clinics was 91/9% and for sole deliverers 84/16% (the overall ratio in Denmark is 87/13%). Moreover, more sole deliverers had less positive perceptions on the items of the domain of ‘Social influences’. Second, the interviews were conducted at two different time points, that is, all implementers had participated in the first GLA:D Back course, whereas nonimplementers had participated in later courses. However, the content of the courses was not changed substantially between the two. Third, we did not interview an equal number of respondents identified as implementers and nonimplementers The pragmatic constraints of the study restricted us to nine respondents (four implementers/five nonimplementers). We were, therefore, not able to reach respondence saturation through repeat interviews. However, given the thickness of the data obtained, it is unlikely that the unequal number of respondents affected our analysis negatively.
It is not clear if the results can be generalized to implementation of standardized care in primary care or practices with more than one GLA:D Back deliverer in a clinic, as context and organizational factors will probably be different. However, the study involved data from clinicians in both rural and urban areas. The interviews were done with both implementers and nonimplementers to have a better understanding of the quantitative data. Therefore, the results have good external validity toward sole deliverers of an evidence-based ready-to-go care package for LBP patients. More research on the implementation processes of evidence-based ready-to-go care package in clinics with multiple deliverers should be conducted.
Four of the authors (I.R., J.H., A.K., and L.T.) have been involved in the development of GLA:D Back. This could be a potential bias toward a positive interpretation of the results. The authors also hold strong opinions toward implementing the GLA:D Back program based upon their clinical experience and viewpoints that align with the GLA:D Back program's key elements. Interviews with nonimplementers were conducted by a person not connected to the GLA:D Back team (masters student in Health Science) to minimize this bias. Moreover, a person not part of the GLA:D Back team analyzed the interviews, but all authors took part in interpreting the results.
Implications of the results
The results indicate potential areas for improvement of the implementation strategy. Results related to the theme Gain indicate that a greater focus on possible gains for the clinicians could be beneficial, that is, the gain of receiving updated knowledge about the management of LBP patients and the program's adaptability toward patients’ and clinics’ context. Ways to handle clinicians’ changed role in handing over more responsibilities to the patient to self-manage their problems could be given more attention. Moreover, improvement of the reimbursement from the Danish health insurance with subsequent financial gains could be relevant.
Factors related to practicalities could be addressed by improving knowledge of the program by patients and general practitioners and improving the user-friendliness of the data register.
Aspects within the new theme Clinicians’ attitudes could be addressed with an increasing focus on the program's evidence-based foundation and the underlining of the cognitive approach in exercises as a new method of exercising LBP patients.
Conclusion and implications
Approximately half of the clinicians participating in GLA:D Back training courses implemented the program. Implementation was associated with the profession; physiotherapists more frequently implementing the program than chiropractors. The domains of the DIBQ-t were rated less positive by nonimplementers when compared with implementers. DIBQ-t is informing on implementation processes and could be considered in future research. Both implementers and nonimplementers reported high levels of knowledge and skills related to the program. Thus, clinician training alone appears not to be sufficient for implementation. The interviews confirmed this by revealing three themes with relevance for implementation: Gain, Practicalities, and Buying-in on the program. These themes covered all domains of DIBQ-t. Moreover, a new aspect emerged: clinicians’ attitudes to the program. Implementing evidence-based care for LBP, considering ways to address existing beliefs, improve incitements and overcome practical barriers should be considered.
Acknowledgements
We would like to acknowledge the Odense Patient data Explorative Network (OPEN) for access to REDCap for support with the electronic data collection, Bibi Heiberg for helping with the analyses, Lotte Trier for the interviews with the nonimplementers, Birgitta Öberg and Paul Enthoven from Linköping University, Sweden, for the development of the interview guide, and the involved clinicians for using resources to provide data to the study.
Authors’ contributions: I.R., E.B., C.M., J.H., L.T., and A.K. were involved in the study's design. I.R., L.T., and A.K. were involved in data collection. I.R., L.T., E.B. were responsible for data analyses. I.R., E.B., C.M., J.H., L.T., and A.K. were involved in developing the manuscript and have approved the final manuscript.
The study did not receive external funding.
Authors’ information: not applicable.
Ethics approval and consent to participate: The Regional Committees on Health Research Ethics for Southern Denmark decided that the study did not need ethical approval (file number S-20172000-93). The Danish data collection has obtained authorization from the Danish Data Protection Agency (DPA) as part of the University of Southern Denmark's institutional authorization (DPA no. 2015-57-0008 SDU no. 17/30591). According to Danish regulations, an observational study implementing a nonexperimental treatment that was offered to patients on the decision of the clinicians does not undergo research ethics evaluation [The National Committee on Health Research Ethics. Act on Research Ethics Review of Health Research Projects 2019 (updated 2019-02-21, accessed 02-12-2019)]. Written consent was secured when the clinicians entered the GLA:D Back project.
Consent for publication: not applicable.
Availability of data and material: The datasets and analyses used in the current study are available from the corresponding author on reasonable request.
Conflicts of interest
A.K.'s position at the University of Southern Denmark is financially supported by the Foundation for Chiropractic Research and Postgraduate Education. I.R.'s position is supported by income from the GLA:D Back clinician courses. GLA:D is a nonprofit initiative hosted at the University of Southern Denmark, and the GLA:D trademark is the property of the University of Southern Denmark. The GLA:D initiative is developed in close collaboration with the SDU Research & Innovation Organization, including legal reviews. The researchers do not have any personal financial benefits from working with the project.
References
- 1.Grol R, Wensing M. What drives change? Barriers to and incentives for achieving evidence-based practice. Med J Aust 2004; 180: (6 Suppl): S57–S60. [DOI] [PubMed] [Google Scholar]
- 2.Davy C, Bleasel J, Liu H, Tchan M, Ponniah S, Brown A. Factors influencing the implementation of chronic care models: a systematic literature review. BMC Fam Pract 2015; 16:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fischer F, Lange K, Klose K, Greiner W, Kraemer A. Barriers and strategies in guideline implementation – a scoping review. Healthcare (Basel, Switzerland) 2016; 4:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Savigny P, Watson P, Underwood M. Early management of persistent non-specific low back pain: summary of NICE guidance. BMJ 2009; 338:b1805. [DOI] [PubMed] [Google Scholar]
- 5.Foster NE, Anema JR, Cherkin D, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet 2018; 391:2368–2383. [DOI] [PubMed] [Google Scholar]
- 6.Sundhedsstyrelsen (Danish Health Authority). Recommendations for cross-sectoral interventions for people with chronic low back pain [in Danish]. Copenhagen: Sundhedsstyrelsen; 2017. [Google Scholar]
- 7.Whitehurst DG, Bryan S, Lewis M, Hay EM, Mullis R, Foster NE. Implementing stratified primary care management for low back pain: cost-utility analysis alongside a prospective, population-based, sequential comparison study. Spine 2015; 40:405–414. [DOI] [PubMed] [Google Scholar]
- 8.Gardner T, Refshauge K, Smith L, McAuley J, Hübscher M, Goodall S. Physiotherapists’ beliefs and attitudes influence clinical practice in chronic low back pain: a systematic review of quantitative and qualitative studies. J Physiother 2017; 63:132–143. [DOI] [PubMed] [Google Scholar]
- 9.Synnott A, O’Keeffe M, Bunzli S, Dankaerts W, O'Sullivan P, O'Sullivan K. Physiotherapists may stigmatise or feel unprepared to treat people with low back pain and psychosocial factors that influence recovery: a systematic review. J Physiother 2015; 61:68–76. [DOI] [PubMed] [Google Scholar]
- 10.Kent PM, Keating JL, Taylor NF. Primary care clinicians use variable methods to assess acute nonspecific low back pain and usually focus on impairments. Man Ther 2009; 14:88–100. [DOI] [PubMed] [Google Scholar]
- 11.Briggs AM, Jordan JE, Jennings M, et al. Supporting evaluation and implementation of musculoskeletal models of care: a globally-informed framework for judging ‘readiness’ and ‘success’. Arthritis Care Res (Hoboken) 2016; 69:567–577. [DOI] [PubMed] [Google Scholar]
- 12.Slade SC, Kent P, Patel S, Bucknall T, Buchbinder R. Barriers to primary care clinician adherence to clinical guidelines for the management of low back pain: a systematic review and metasynthesis of qualitative studies. Clin J Pain 2016; 32:800–816. [DOI] [PubMed] [Google Scholar]
- 13.Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet 2018; 391:2356–2367. [DOI] [PubMed] [Google Scholar]
- 14.Langridge N, Roberts L, Pope C. The clinical reasoning processes of extended scope physiotherapists assessing patients with low back pain. Man Ther 2015; 20:745–750. [DOI] [PubMed] [Google Scholar]
- 15.Kongsted A, Hartvigsen J, Boyle E, et al. GLA:D® Back: group-based patient education integrated with exercises to support self-management of persistent back pain – feasibility of implementing standardised care by a course for clinicians. Pilot Feasibility Stud 2019; 5:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kongsted A, Ris I, Kjaer P, Vach W, Morsø L, Hartvigsen J. GLA:D® Back: implementation of group-based patient education integrated with exercises to support self-management of back pain – protocol for a hybrid effectiveness-implementation study. BMC Musculoskelet Disord 2019; 20:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kjaer P, Kongsted A, Ris I, et al. GLA:D® Back group-based patient education integrated with exercises to support self-management of back pain – development, theories and scientific evidence. BMC Musculoskelet Disord 2018; 19:418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Skou ST, Roos EM. Good Life with osteoArthritis in Denmark (GLA:D): evidence-based education and supervised neuromuscular exercise delivered by certified physiotherapists nationwide. BMC Musculoskelet Disord 2017; 18:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zadro JR, O’Keeffe M, Allison JL, Lembke KA, Forbes JL, Maher CG. Effectiveness of implementation strategies to improve adherence of physical therapist treatment choices to clinical practice guidelines for musculoskeletal conditions: systematic review. Phys Ther 2020; 100:1516–1541. [DOI] [PubMed] [Google Scholar]
- 20.Al Zoubi FM, Menon A, Mayo NE, Bussieres AE. The effectiveness of interventions designed to increase the uptake of clinical practice guidelines and best practices among musculoskeletal professionals: a systematic review. BMC Health Serv Res 2018; 18:435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mesner SA, Foster NE, French SD. Implementation interventions to improve the management of non-specific low back pain: a systematic review. BMC Musculoskelet Disord 2016; 17:258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 2005; 14:26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012; 7:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mosavianpour M, Sarmast HH, Kissoon N, Collet JP. Theoretical domains framework to assess barriers to change for planning health care quality interventions: a systematic literature review. J Multidiscip Healthc 2016; 9:303–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huijg JM, Gebhardt WA, Dusseldorp E, et al. Measuring determinants of implementation behavior: psychometric properties of a questionnaire based on the theoretical domains framework. Implement Sci 2014; 9:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs – principles and practices. Health Serv Res 2013; 48 (6 Pt 2):2134–2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Cathain A, Murphy E, Nicholl J. The quality of mixed methods studies in health services research. J Health Serv Res Policy 2008; 13:92–98. [DOI] [PubMed] [Google Scholar]
- 28.Huijg JM, Gebhardt WA, Crone MR, Dusseldorp E, Presseau J. Discriminant content validity of a theoretical domains framework questionnaire for use in implementation research. Implement Sci 2014; 9:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Polit DF, Beck CT. The content validity index: are you sure you know what's being reported? Critique and recommendations. Res Nurs Health 2006; 29:489–497. [DOI] [PubMed] [Google Scholar]
- 30.Atkins L, Francis J, Islam R, et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement Sci 2017; 12:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Creswell JW, Plano Clark VL. Designing and conducting mixed methods. Thousand Oaks: SAGE; 2011. [Google Scholar]
- 32.Braun V, Clarke V. What can ‘thematic analysis’ offer health and wellbeing researchers? Int J Qual Stud Health Well-being 2014; 9:26152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schroder K, Oberg B, Enthoven P, Kongsted A, Abbott A. Confidence, attitudes, beliefs and determinants of implementation behaviours among physiotherapists towards clinical management of low back pain before and after implementation of the BetterBack model of care. BMC Health Serv Res 2020; 20:443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Richmond H, Hall AM, Hansen Z, Williamson E, Davies D, Lamb SE. Exploring physiotherapists’ experiences of implementing a cognitive behavioural approach for managing low back pain and identifying barriers to long-term implementation. Physiotherapy 2018; 104:107–115. [DOI] [PubMed] [Google Scholar]
- 35.Bernhardsson S, Johansson K, Nilsen P, Oberg B, Larsson ME. Determinants of guideline use in primary care physical therapy: a cross-sectional survey of attitudes, knowledge, and behavior. Phys Ther 2014; 94:343–354. [DOI] [PubMed] [Google Scholar]
- 36.Shaw BR, Heywood SE, Page CJ, et al. Advanced musculoskeletal physiotherapy: barriers and enablers to multi-site implementation. Musculoskeletal Care 2018; 16:440–449. [DOI] [PubMed] [Google Scholar]
- 37.Huijg JM, Crone MR, Verheijden MW, van der Zouwe N, Middelkoop BJ, Gebhardt WA. Factors influencing the adoption, implementation, and continuation of physical activity interventions in primary health care: a Delphi study. BMC Fam Pract 2013; 14:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huijg JM, Dusseldorp E, Gebhardt WA, et al. Factors associated with physical therapists’ implementation of physical activity interventions in The Netherlands. Phys Ther 2015; 95:539–557. [DOI] [PubMed] [Google Scholar]
- 39.Presseau J, Johnston M, Francis JJ, et al. Theory-based predictors of multiple clinician behaviors in the management of diabetes. J Behav Med 2014; 37:607–620. [DOI] [PubMed] [Google Scholar]
- 40.Lohm D, Kirpitchenko L. Interviewing pairs. Discussions on migration and identity. SAGE research methods cases. Thousand Oaks: SAGE; 2014. [Google Scholar]
- 41.Carter N, Bryant-Lukosius D, DiCenso A, Blythe J, Neville AJ. The use of triangulation in qualitative research. Oncol Nurs Forum 2014; 41:545–547. [DOI] [PubMed] [Google Scholar]