Abstract
Exposure to community violence is an epidemic problem that causes debilitating effects on youth mental health. However, the relationships between violence exposure and youth mental health remain unclear when examining co-occurring socioecological risk and protective factors. The purpose of this study is to clarify the observed gaps in knowledge by utilizing structural equation modeling (SEM) to examine the mediating role of community violence exposure on the relationship between perceived neighborhood risk factors, parental behaviors, and peers on depressive symptoms in a sample of urban youth in low-income public housing communities (n = 320). Results indicate that community violence exposure and exposure to delinquent peers mediates the effects of perceived neighborhood risk and parenting behaviors on depressive symptoms. These findings suggest that while interventions that limit exposure to community violence and delinquent peers could reduce depressive symptoms, interventions that reduce community violence are essential to improve youth mental health.
Keywords: Exposure to community violence, Youth mental health, Public housing, Urban neighborhoods
1. Introduction
Exposure to violence is an epidemic problem that causes devastating health consequences (Frazer et al., 2018; Slutkin et al., 2018). According to national data, youth are particularly vulnerable and 60% of all youth in the United States report being exposed to violence over the past year either through witnessing or direct victimization (Finkelhor et al., 2015). Place is a salient feature of community violence exposure. Youth living in U.S. urban neighborhoods are at higher risk of violence exposure in their communities (Aizer, 2008; Browning et al., 2017; Schwab-Stone et al., 1999; Seal et al., 2014; Stein et al., 2003; Zona and Milan, 2011). In community samples, an astounding 85% of youth in U.S. urban neighborhoods report exposure to community violence in their lifetimes (McDonald and Richmond, 2008). Largely due to living in neighborhoods characterized by hyper-segregation and concentrated poverty, Black and Latinx youth are much more likely to witness violence and be victimized compared to White youth (Stein et al., 2003; Thomas et al., 2011; Zimmerman and Messner, 2013).
Exposure to community violence has adverse effects on social, behavioral, and health outcomes (Kennedy and Ceballo, 2014; Margolin, 2005; Ozer et al., 2017; Woods-Jaeger et al., 2019). The mental health effects of community violence exposure are particularly damaging. Youth that experience community violence are at increased risk of developing elevated depressive symptoms and the behavioral and emotional problems it leaves in its wake (Moffitt, 2013; Slutkin et al., 2018; Turner et al., 2013). The purpose of this paper is to contribute to literature on violence and mental health by exploring how exposure to community violence operates in conjunction with other co-occurring contextual factors to influence depressive symptoms.
2. Review of the literature
2.1. Exposure to community violence and depressive symptoms
Evidence suggests that exposure to community violence is not equally distributed among youth or across space (Peterson and Krivo, 2009; Rojas-Gaona et al., 2016; Voisin and Berringer, 2014). Indeed, a consistent findings in the violence literature is the enduring relationship among race, place, and violence (Friedson and Sharkey, 2015; Graif and Matthews, 2017; Griffiths, 2013; Morenoff et al., 2001). A large proportion of neighborhood studies historically emphasize the role of concentrated poverty and racial segregation on the differential rate of violence exposure among Black and Latinx youth as larger shares of these children and youth live in high poverty neighborhoods compared to the poorest of their white peers (Gibson et al., 2009; McArdle and Acevedo-Garcia, 2017; Sampson, 1993). Living in urban neighborhoods that are inundated with poverty, racial segregation, and high population turn over have been found to have significantly higher rates of violent crimes, which places youth living in these neighborhoods at an increased risk of violence exposure (Aizer, 2008; Browning et al., 2017; Eron et al., 1997; Seal et al., 2014; Zona and Milan, 2011). This is especially true for Black and Latinx youth who are particularly vulnerable to community violence exposure, and are much more likely to witness violence and be victimized compared to white youth (Thomas et al., 2011; Zimmerman and Messner, 2013).
Moreover, evidence points to the negative consequences of violence exposure on youth mental health (Fowler et al., 2009; Kelly, 2010; Ozer et al., 2017). Much of this evidence, however, often fails to highlight socioecological factors known to affect health, such as aspects of neighborhood context (Huang et al., 2018). The limited research on this demonstrates an association between exposure to community violence and internalizing symptoms. This association, however, has not always been consistent (Fowler et al., 2009; McDonald and Richmond, 2008; Shukla and Wiesner, 2015). For example, exposure to community violence has been associated with increased depressive symptoms among youth (Salzinger et al., 2002). Others have found no associations between exposure to community violence and depressive symptoms (Ahmad et al., 2017) and differential effects based on exposure levels (Gaylord-Harden et al., 2011). Direct victimization tends to have larger effects on depressive symptoms whereas witnessing or hearing about violence has smaller or no effects (McDonald and Richmond, 2008). The diverse and inconsistent findings in the literature suggest a need for additional research.
2.2. Family and peer influences on depressive symptoms
Family factors, such as effective family functioning, effective parenting, and parental monitoring and support are thought to be protective against the harmful consequences of community violence exposure (Copeland-Linder et al., 2010). Although, several studies indicate that effective family functioning and parenting practices buffer the harmful effects of violence exposure on youth mental health (Bacchini et al., 2011; Ceballo et al., 2003; Low and Espelage, 2014; Voisin et al., 2012), the direction and magnitude of the effects has been inconsistent (Copeland-Linder et al., 2010). A recent review of studies found no consistent association between parental monitoring and youth violence exposure on mental health outcomes (Ozer et al., 2017).
Fewer studies have examined whether parenting behaviors may protect against community violence exposure and provide contradicting conclusions (Gorman-Smith and Tolan, 1998; Sheidow et al., 2001; Gorman-Smith, Henry and Tolan, 2004; Lambert et al., 2015; Moed, Gershoff and Bringewatt, 2017). Gorman-Smith, Henry, and Tolan (2004) and Sheidow, Gorman-Smith, Tolan, and Henry (2001) found that poor family functioning was a risk factor for African-American and Latinx children’s exposure to violence, but only within communities facing extreme social and economic problems. Extreme social and economic problems disproportionately faced by African American and Latinx families are exacerbated by residential segregation, predatory lending, and housing discrimination that cluster families in neighborhoods characterized by concentrated poverty (Chiteji, 2016; Desmond, 2014). These conditions have been found to disrupt a family’s capacity to respond to and function optimally under the weight of stressors caused by racism, classism, and sexism at systemic levels (Friedline et al., 2020). Lambert et al. (2015) found that positive parenting behaviors limited youth exposure to perceived neighborhood risks and mitigated adverse mental health outcomes.
In contrast, Gorman-Smith and Tolan (1998) found nonsignificant relationships between parenting practices, family characteristics, and youth exposure to violence among African American and Latinx adolescents and their caregivers living in economically disadvantaged neighborhoods. Similarly, Turner et al. (2013) found that family social support was not protective of youth adverse life events or exposure to violence victimization but did mediate the relationship between neighborhood disorder and psychological distress among a national sample of youth. In a sample of youth in Chicago neighborhoods, Zimmerman and Messner (2013) found that parenting behaviors such as warmth, lack of hostility, and supervision were not protective of community violence exposure among youth. Moed, Gershoff, and Bingewatt (2017) found that higher levels of parental control were associated with lower levels of witnessing community violence among African American, Latinx, and white youth living in low-income neighborhoods, but did not significantly affect direct violence victimization.
Research also shows that peers influence youth behavior patterns during adolescence and impact youth mental health (Lombe and Nebbitt, 2015). Exposure to peers that engage in deviant and delinquent behaviors (e.g., theft, property damage, etc.) increases youth problem behaviors due to peer expectations and pressures to engage in conforming behaviors including violent acts (e.g., assault) (Lambert et al., 2011; Lambert et al., 2015). Additionally, youth who affiliate with delinquent peers are at increased risk of violence exposure due to peer social networks (Lambert et al., 2011; Slutkin et al., 2018), and report more depressive symptoms compared to youth who affiliate with nondelinquent peers (Lombe and Nebbitt, 2015). Peer social networks may also facilitate the spread of values, norms, and behavioral expectations (e.g., social contagion) (Fagan et al., 2007). The complex interaction between family and peer effects on youth community violence exposure and inconclusive evidence on mental health effects suggests a clear need for further research.
2.3. Neighborhoods, exposure to community violence, and depressive symptoms
Neighborhood environments, including objective conditions and subjective appraisals, influence individual behaviors and mental health outcomes (Butcher et al., 2015; Curry et al., 2008; Giurgescu et al., 2015; D. Kim, 2008; Lambert et al., 2011; Latkin et al., 2007; Ross and Mirowsky, 2009; Schaefer-McDaniel, 2009; Stiffman et al., 1999; Turner et al., 2013). Neighborhood stressors such as crime, violence, drug sales, deteriorating infrastructure, and poor housing quality have all been linked to psychological distress among youth (Nebbitt, 2015), as well as increased risks of depressive symptoms (Duncan, 1996; D. Kim, 2008; Latkin and Curry, 2003; Snedker and Herting, 2016). Adverse neighborhood conditions increase levels of daily stress, heighten vulnerability for experiencing negative events, and may disrupt the formation of social networks that are protective of community violence exposure (Casciano and Massey, 2012; Cutrona et al., 2006). These stressors are often chronic and characterized by imperceptible onset, unavoidability, and open-ended recurrence (Matheson et al., 2006). Thus, living in distressed neighborhoods can produce unpleasant emotional states and produce feelings of demoralization and hopelessness (Ross and Mirowsky, 2009).
Stiffman et al. (1999) found that youths’ perceptions of their neighborhood environment had direct effects on mental health outcomes including suicidality, posttraumatic stress, conduct disorder, and depressive symptoms. Additionally, they found that exposure to violence had direct adverse effects on youth mental health, and indirect effects which were mediated through youths’ perceived neighborhood environment (Stiffman et al., 1999). Curry, Latkin and Davey-Rothwell (2008) found direct effects of perceptions of neighborhood disorder and experiences of violent crime on youth depressive symptoms. Similarly, Butcher, Galanek, Kretschmar and Flannery (2015) found that neighborhood disorganization was associated with higher levels of exposure to violence, which was associated with increased trauma symptoms among youth. Turner et al. (2013) found that youth living in neighborhoods with higher levels of disorder experienced significantly higher levels of psychological distress, but this relationship was fully mediated by family support, violence victimization, and adverse life events.
2.4. The context of public housing
Housing policy, land use zoning, and intentional government neglect have led to an enduring legacy of residential segregation in the U.S. (Nebbitt, 2015; Rothstein, 2017). African American youth are disproportionately over-represented in extremely poor and hyper-segregated neighborhoods (Nebbitt, 2015), which resulted from decades of U.S. government policy that allowed and encouraged housing discrimination towards African American families through practices such as predatory lending and redlining in Black neighborhoods, restrictive housing covenants, and blockbusting (Rothstein, 2017). Additionally, refusal to insure mortgages in or near African American neighborhoods while subsidizing housing for white families in the suburbs contributed significantly to race and class segregation in the U.S. and perpetuated a cycle of severe disinvestment in African American neighborhoods (Gordon, 2008; Rothstein, 2017). Such policies also prevented African American families from building wealth through homeownership which limited opportunities for socioeconomic mobility (Gordon and Bruch, 2020). These policies, which segregated Black families and prevented wealth accumulation, had devastating effects in the past as well as the present (Andrews et al., 2017; Gordon and Bruch, 2020).
Federal housing policy, particularly through the citing and development of public housing, is unheralded in its success in forcing African American families into urban public housing developments often characterized by crime, violence, and disorder (Goetz, 2013; Rothstein, 2017). These adverse community conditions originated and were reproduced through social (e.g., concentrated poverty, residential instability, limited public services) and physical mechanisms (e.g., land use, physical distress) (Lens, 2013), and exacerbated by the criminalization of Black families and communities (Hinton and Cook, 2021). Residents of public housing communities in the U.S. often identify violence and safety as major concerns in their communities (Goering and Feins, 2003), and evidence suggests that living in urban public housing is associated with increased exposure to community violence (Garbarino et al., 1991; Goering and Feins, 2003). The co-occurring contextual factors associated with community violence exposure have significant consequences on the health and well-being of African American youth (Nebbitt, 2015).
Notwithstanding these facts, theorists argue that urban neighborhoods like public housing communities may be simultaneously promotive and inhibitive (Coll et al., 1996). For example, in such environments, parents may adapt to adverse neighborhood conditions by creating promotive social networks to protect their children (Coll et al., 1996). As a result, African American youth in public housing experience multifinality whereby youth share similar life experiences but divergent socio-behavioral outcomes (Cicchetti and Rogosch, 1996; McDonald et al., 2011). Accordingly, abundant research makes clear that many public housing youth successfully navigate these tough neighborhoods, avoid life-compromising experiences, and become well-functioning adults (Furstenberg et al., 2000; McDonald et al., 2011; C. Smith et al., 1995).
This study is premised on the assumption that U.S. public housing policy has created a unique social context (i.e., public housing) for African American families that is, primarily, unshared by other ethnic groups. This paper adds to existing literature on violence and depressive symptoms by examining these factors in an understudied population that is disproportionately over-represented in our nation’s only publicly owned neighborhood.
Research on community violence and mental health tends to focus narrowly on isolated effects of community, family, or peer influences to explain differential effects on youth mental health. This paper represents a unique contribution to research by testing a comprehensive mediation model that examines the associations between the proximal and distal co-occurring socioecological factors influencing youth mental health vis-a-vis depressive symptoms. Specifically, the current study examines the relationship between youth perceptions of neighborhood risk, community violence exposure, parental behaviors, exposure to delinquent peers, and depressive symptoms to further understand the processes by which such factors may compete or converge to influence adolescent mental health.
2.5. Theoretical framework, research questions, and hypotheses
We draw upon the Social Ecological Model adapted from Bronfenbrenner and Ceci’s (1994) bioecological framework to understand the complex relationship between exposure to violence and depressive symptoms considering potential mediating effects of neighborhoods, parents, and peers. The theory highlights the importance of youths’ socioecological context, which includes the interpersonal (microsystem), community (exosystem), organizational (mesosystem), and macro or policy/enabling environment (Bronfenbrenner and Ceci, 1994). Additionally, the theory acknowledges that youth are shaped by processes that occur at multiple levels in the proximal and distal environment. In this regard, it provides a useful framework for understanding how environmental stressors, such as community violence, impact youth depressive symptoms within the context of their social worlds (Copeland-Linder et al., 2010).
While prevailing scholarship focuses on specific elements of a youth’s microsystem (i.e., parental behaviors, peer influences) and to a lesser extent youths’ exosystem (e.g., neighborhood, community), we examine these elements as an integrated system to understand the direct and indirect contributions to youth mental health vis-a-vis depressive symptoms. Specifically, we include these relevant contextual components in a single empirical model which allows us to examine proximal and distal relationships within youth environments. Our approach allows us to examine which factors embedded in youths’ socioecological context have greater or lesser effects on depressive symptoms when considering them as an interconnected system. The primary interests of this study are on the direct and indirect effects of perceived neighborhood risks, parenting behaviors, and exposure to delinquent peers on depressive symptoms among youth and young adults in public housing. Our secondary interests are on the direct effects of community violence exposure on depressive symptoms, and the risk and protective factors for community violence exposure.
Based upon the theoretical model and literature review, we advance the following research question: (1) To what extent is the impact of perceived neighborhood risk factors, parental behaviors, and exposure to delinquent peers on depressive symptoms mediated by victimization by, or witnessing, community violence? We predict that perceived neighborhood risks, parenting behaviors, and exposure to delinquent peers will affect youth mental health via depressive symptoms (Fig. 1, Path A). We also predict that witnessing and victimization by community violence will have direct effects on youth depressive symptoms, and will partially mediate the effects of perceived neighborhood risk, parenting behaviors, and exposure to delinquent peers on depressive symptoms (Fig. 1, Path B). We also expect that perceived neighborhood risk and exposure to delinquent peers will be risk factors for community violence exposure, while parenting behaviors will be protective.
Fig. 1.
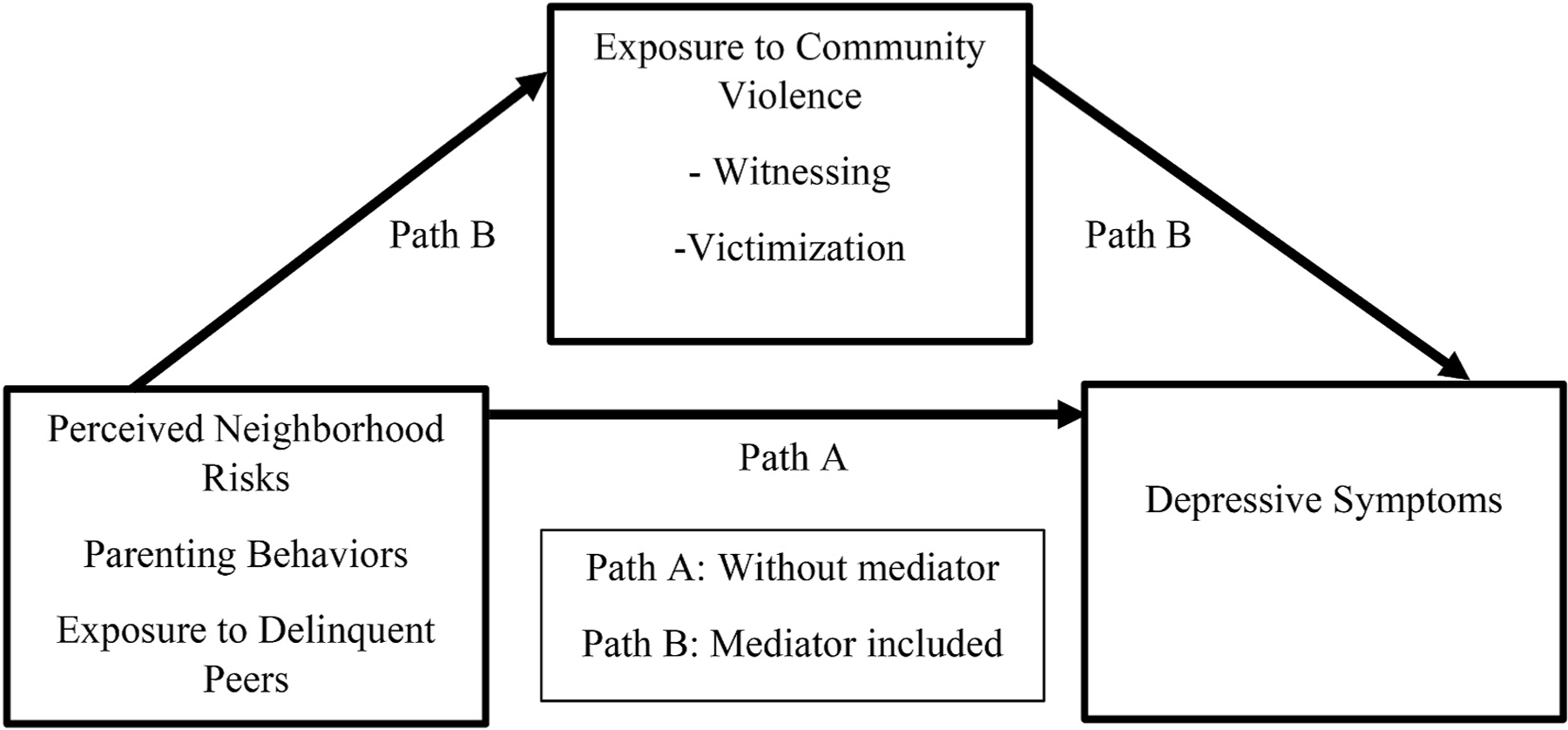
Conceptual model of the socioecological correlates of depressive symptoms.
3. Methods
3.1. Participants and research setting
Data were collected from 320 African American youth and young adults between the ages of 13 and 21 who lived in two public housing developments and one private low-income apartment complex; all three locations had similar socioeconomic status (SES). The recruitment sites were all located in a large Northeastern city.
3.2. Data collection and recruitment
Recruitment material for the study included flyers and an information sheet which described the study and the research team. The research team gave flyers to social service agencies and community partners to post in the targeted housing developments and neighborhoods. Data collection took place at community centers within each research setting. Parental permission and youth assent were obtained from all participants prior to survey completion. The research team utilized the Capacity-to-Consent Screen to assess youths’ capacity to give informed consent prior to completing the survey (Zayas et al., 2005).
After youth ages 17 and younger met eligibility criteria they were given parental permission and youth assent forms to obtain a parent/guardian’s signature. Prior to completing the survey, parental permission and youth assent were obtained from youth ages 17 and younger. After young adults 18 years of age and older met inclusion criteria they were given informed consent forms to review and sign. Youth and young adults who met inclusion criteria were instructed to stay in the community centers to complete the survey.
Youth ages 17 and younger who demonstrated the capacity to give informed consent and provide parental permission met in groups of 8–10 youth to complete the paper survey. Key research personnel (i.e., licensed clinical social workers) read the survey questions and possible responses aloud to the group and youth circled their responses. Young adults ages 18 and older who demonstrated the capacity to give informed consent and provided informed consent met in small groups of 5–7 people to complete the paper survey on their own. This data collection protocol was employed across all research sites and during all data collection sessions.
After completing the survey, participants were provided a bag of chips and bottled water as a licensed clinical social work debriefed participation in the study. After their debriefing they were given a resource guide to mental and behavioral health services available in their community and a $40.00 Visa gift card for their participation. The Institutional Review Board at the University of Illinois – Chicago approved the research protocol, which was supported by a Certificate of Confidentiality issued by the National Institutes of Health.
3.3. Measures
Demographic Characteristics.
Three items were utilized to assess youth sex, age, and racial/ethnic identity. Sex was assessed with the following item: “What is your sex?”. Response options included male and female. Age was assessed with the following item: “How old are you?”. Response options were open-ended such that youth could report their age in years. Racial/ethnic identity was assessed with the following item: “I consider myself to be (Please select only one answer)?”. Response options included (1) African American (Black), (2) White (European, Caucasian, non-Hispanic), (3) Non-white Hispanic or Latino/Latina, (4) Native American, (5) Asian, Asian American, (6) Mixed, parents from two different groups, (7) Other (Specify).
Exposure to Community Violence.
Exposure to direct and indirect community violence was assessed using the 26-item Survey of Exposure to Community Violence: Self-Report Version (Richters and Martinez, 1993). Example items included: “How many times have you seen someone else being threatened with serious physical harm?” and “How many times have you yourself actually been beaten up or mugged?” Likert-scale responses ranged from “never = 1” to “many = 4”. Items were summed so that higher scores represented increased exposure to violence. The victimization (α = 0.84) and witnessing (α = 0.85) subscales demonstrated acceptable internal consistency among a sample of African American youth recruited from public housing (Nebbitt, 2015). Both subscales demonstrated acceptable internal consistency with this sample (victimization α = 0.89, witnessing α = 0.90).
Perceived Neighborhood Risk.
Perceived neighborhood risk was measured using the 11-item ambient hazards subscale from the Subjective Neighborhood Scale (SNS) (Aneshensel and Sucoff, 1996). The ambient hazard subscale assessed perceived neighborhood risk such as neighborhood safety, crime and violence, police harassment, and drug dealing. Examples of items include: “Property gets damaged or destroyed here” and “Violent crimes happen here.” Likert-scale responses ranged from “strongly disagree 1” to “strongly agree 4”. The ambient hazard subscale demonstrated acceptable reliability in a sample of African American youth in public housing (α = 0.64) (Nebbitt, 2015). The scale demonstrated acceptable reliability with this sample (α = 0.79).
Exposure to Delinquent Peers.
Exposure to Delinquent Peers was measured using an adapted version of the delinquency subscale from the AddHealth National Longitudinal Survey of Adolescent to Adult Health (Harris et al., 2009). Youth were asked to respond to 13 items based on the following prompt: “How many of your friends in the Apartment Complex/Housing Development where your family lives now, have done the following:” Example items included: “Get into a serious physical fight” and “Threaten to use a weapon to get something from someone.” Likert-scale responses ranged from “none” (0) to “all my friends” (4). The subscale demonstrated acceptable reliability among the study sample (α = 0.90).
Parenting Behaviors.
Parenting behaviors were assessed using an adapted version of the Parental Attitude Measure (PAM) (Jordan, 2003; Lamborn et al., 1991). We modified the 12-item parental supervision and encouragement scale to create two different 12-item scales to assess maternal and paternal parenting practices. An original item in the paternal supervision subscale read, for example, “How much does your father/mother, stepfather/stepmother or the adult who takes care of you really knows who your friends are?” We replaced the phrase, “father/mother, stepfather/stepmother or the adult” with the phrase “mother, stepmother or the female adult” for the maternal modification and “father, stepfather or the male adult” for the paternal modification, on all items of the PAM. These revisions were made to be inclusive of varied family composition. The PAM has demonstrated acceptable reliability (α = 0.69) in a sample of African American youth (Nebbitt, 2015). The modified subscales demonstrated acceptable reliability in the present sample (Table 1).
Table 1.
Sample characteristics and descriptive statistics for study variables (n = 320).
| |
Total Sample |
Housing Type, Percents & Means (SD) |
Test Statistics |
||||
|---|---|---|---|---|---|---|---|
| N | M(SD) | Public | Private | t-test | α | χ 2 | |
| Demographics | |||||||
| Gender | 320 | – | – | – | – | – | N.S.(0.050) |
| Male | 123 | 38.4% | 45.4% | 34.2% | – | – | – |
| Female | 197 | 61.6% | 54.6% | 65.8% | – | – | – |
| Age | 317 | 16.59 (2.47) | 16.52 (2.57) | 16.62 (2.40) | N.S. (0.718) | – | – |
| Parenting Behaviors | |||||||
| Maternal Encouragement | 311 | 22.14 (5.62) | 21.50 (5.82) | 22.75 (5.36) | N.S. (0.058) | .892 | – |
| Maternal Monitoring/Supervision | 311 | 15.03 (4.02) | 14.71 (4.04) | 15.36 (3.91) | N.S. (0.160) | .848 | – |
| Paternal Encouragement | 310 | 18.19 (7.36) | 18.51 (6.76) | 18.09 (7.69) | N.S. (.624) | .952 | – |
| Paternal Monitoring/Supervision | 307 | 11.90 (5.22) | 12.40 (4.96) | 11.63 (5.38) | N.S. (0.220) | .930 | – |
| Peers | |||||||
| Exp. to Delinquent Peers | 307 | 22.55 (10.61) | 21.51 (9.38) | 23.27 (11.39) | N.S. (0.151) | .926 | – |
| Perceived Neighborhood Risk | |||||||
| Ambient Hazards | 286 | 24.55 (6.01) | 25.56 (5.90) | 23.97 (6.05) | Sig (0.034) | .781 | – |
| Community Violence Exposure | |||||||
| Community Violence Victimization | 304 | 15.17 (5.85) | 15.27 (6.08) | 15.10 (5.72) | N.S. (0.807) | .885 | – |
| Community Violence Witnessing | 295 | 25.93 (9.08) | 25.54 (9.14) | 26.23 (9.08) | N.S. (0.536) | .899 | – |
| Mental Health (Depressive Symptoms) | |||||||
| Center for Epi Studies – Depression (CES-D) | 279 | 33.67 (11.19) | 35.07 (12.8) | 32.67 (9.72) | N.S. (0.104) | .90 | – |
Data Source: DCFAM (2012).
Depressive Symptoms.
Depressive symptoms were measured using the 20-item Center for Epidemiologic Studies Depression Scale (CES-D). Participants were asked the following prompt: “Below is a list of some of the ways you may have felt or behaved. Please indicate how often you have felt this way during the past WEEK by circling the appropriate response.” Example items included: “I am bothered by the things that usually don’t bother me” and “I felt hopeless about the future.” Likertscale responses included “less than 1 day” (0), “1–2 days” (1), “3–4 days” (2), and “5–7 days” (3). The CES-D has been widely used and demonstrated adequate reliability with public housing youth (α 0.80 to 0.90) (Nebbitt and Lombe, 2007; Lu et al., 2017; Estreet et al., 2018) and among the present sample (α = 0.90).
3.4. Analysis plan
A two-step structural equation modeling (SEM) procedure was used to test hypotheses about relationships between perceived neighborhood risk, parenting practices, exposure to delinquent peers, and exposure to community violence and post-traumatic stress. The first step involved construction of a model to validate latent variables used in the structural model. Given validation of these constructs in other studies, these models were congeneric, thus each observed variable loaded on only one factor. We used the WLSMV estimator in Mplus due to the combination of categorical and continuous observed variables. Commonly used fit indices were utilized to determine the best fitting model for both measurement and structural models. Chi-square values that were not statistically significant, RMSEA <0.05, CFI and TLI >0.95, and WRMR <0.90 were considered evidence of good fit (Bowen and Guo, 2012; Browne and Cudeck, 1993; Hu and Bentler, 1999). Given the sensitivity of chi-square to sample size as well as the experimental nature of WRMR, we relied on RMSEA, CFI, and TLI to determine the best-fitting measurement models (Muthén, & Muthén, n.d.; Schumacker and Lomax, 2004). After validation of our measurement models, structural models were specified for theorized paths between latent variables. Standardized coefficients and p-values for regression terms including the latent variables were examined to determine the effect and magnitude of each theorized relationship. Indirect effects and statistical significance were calculated for each mediating relationship of interest between latent variables using the Sobel test computed manually and in the powerMediation R package (Qiu, 2018; Sobel, 1986). Power analyses were conducted for each model to determine adequate power for both close and not-close fit. As our missing data were completely random, we used listwise deletion to handle the missing data, similar to other studies (Kang, 2013). When missing are completely random, listwise deletion does not include any biases in parameter estimates (Allison, 2001). This procedure yielded a sample size of n = 226 for the victimization model and n = 222 for the witnessing model.
4. Results
4.1. Sample characteristics
Data were collected from 320 youth who lived in public housing (37.2%), privately-owned multi-family housing complexes (59.4%), and foreclosed housing in the study area (3.4%) (Table 1). All recruitment sites shared similarity on key study variables. The age of the sample ranged from 13 to 21 years of age (M = 16.6 years, SD = 2.5 years). The sample was primarily African American (97%) males (61.6%). Community violence exposure was high with roughly 67% of youth having been directly victimized, 79% having witnessed community violence, and 66% having been victims and witnesses of community violence.
4.2. Measurement models
Following examination of descriptive statistics and bivariate correlations, we estimated measurement models to determine the best fitting model. The latent construct correlations for the full structural models are presented in Table 2.
Table 2.
Correlation matrices for latent variables (n = 320)a.
| Perceived Neighborhood Risk | Parenting Behaviors | Delinquent Peers | Violence (Victim) | Depressive Symptoms | |
|---|---|---|---|---|---|
| Perceived Neighborhood Risk | 1.00 | – | – | – | – |
| Parenting Behaviors | −0.22** | 1.00 | – | – | – |
| Delinquent Peers | 0.31*** | −0.22** | 1.00 | – | – |
| Violence (Victim) | 0.41*** | −0.31** | 0.59*** | 1.00 | – |
| Depressive Symptoms | 0.20** | −0.27** | 0.41*** | 0.42*** | 1.00 |
| Perceived Neighborhood Risk | Parenting Behaviors | Delinquent Peers | Violence (Witness) | Depressive Symptoms | |
|
| |||||
| Perceived Neighborhood Risk | 1.00 | - | - | - | - |
| Parenting Behaviors | −0.23** | 1.00 | - | - | - |
| Delinquent Peers | 0.31*** | −0.25** | 1.00 | - | - |
| Violence (Witness) | 0.44*** | −0.33*** | 0.58*** | 1.00 | - |
| Depressive Symptoms | 0.24** | −0.26** | 0.44*** | 0.42*** | 1.00 |
p<.05,
p<.01,
p<.001
Calculated in Mplus. Data Source: DCFAM (2012).
Results indicated that depressive symptoms had a significant positive correlation with community violence victimization, witnessing community violence, perceived neighborhood risk, exposure to delinquent peers, and parenting behaviors (e.g., supervision and encouragement). Next, modification indices were examined to improve model fit, and 6 correlated measurement errors were determined to be theoretically and statistically appropriate for specification in both the violence victimization and violence witnessing models. After specifying these correlated measurement errors, fit indices for the measurement models indicated good fit to the data, χ2(1579) = 1922.635, RMSEA = 0.032(0.026, 0.037), CFI = 0.974, TLI = 0.973, WRMR = 1.06 for the victimization model and χ2 (1936) = 2417.253, RMSEA = 0.034(0.030, 0.038), CFI = 0.963, TLI = 0.962, WRMR = 1.14 for the violence witnessing model.
4.3. Structural models
We then added structural paths to the measurement models for the full models. Because we theorized relationships between all latent variables, the fit indices were identical to the measurement models which indicated good fit to the data. However, there were multiple nonsignificant paths between hypothesized relationships between latent variables which suggested partial support for the theoretical model. For example, the structural models indicated that perceived neighborhood risk and parenting behaviors did not have a direct effect on depressive symptoms, though both of these were shown to be mediated by exposure to community violence in both victim and witness models. Nonsignificant paths were removed individually and robust chi-square difference testing was used to determine whether trimmed models should be preferred over the full models. All results for the robust chi-square difference testing were non-significant indicating that the more parsimonious model should be accepted. The final trimmed models also had a good fit to the data, χ2(1581) = 1893.565, RMSEA = 0.030(0.025, 0.035), CFI = 0.976, TLI = 0.975, WRMR = 1.07 being a victim of community violence, and χ2(1938) 2385.247, RMSEA 0.033(0.028, 0.037), CFI = 0.966, TLI = 0.965, WRMR = 1.15 for witnessing community violence.
Results suggested that community violence victimization and witnessing community violence operated similarly in its effect on youth depressive symptoms. The final models indicated that both exposure to delinquent peers and witnessing or being a victim of community violence had significant and positive direct effects on depressive symptoms. Witnessing or being a victim of community violence positively mediated the effects of perceived neighborhood risk, parenting behaviors, and exposure to delinquent behaviors on depressive symptoms. Exposure to delinquent peers positively mediated the effects of perceived neighborhood risk and parenting behaviors on depressive symptoms. The final models are displayed in Figs. 2 and 3, respectively. Squared multiple correlation coefficients for the final models indicated that perceived neighborhood risk, parenting behaviors, and exposure to delinquent peers explained 44.1% of the variation in being a victim of community violence and 43.8% of variation in witnessing community violence. Exposure to delinquent peers and being a victim of or witnessing community violence, on the other hand, explained 22.4% and 24.1% of variation in depressive symptoms, respectively.
Fig. 2.
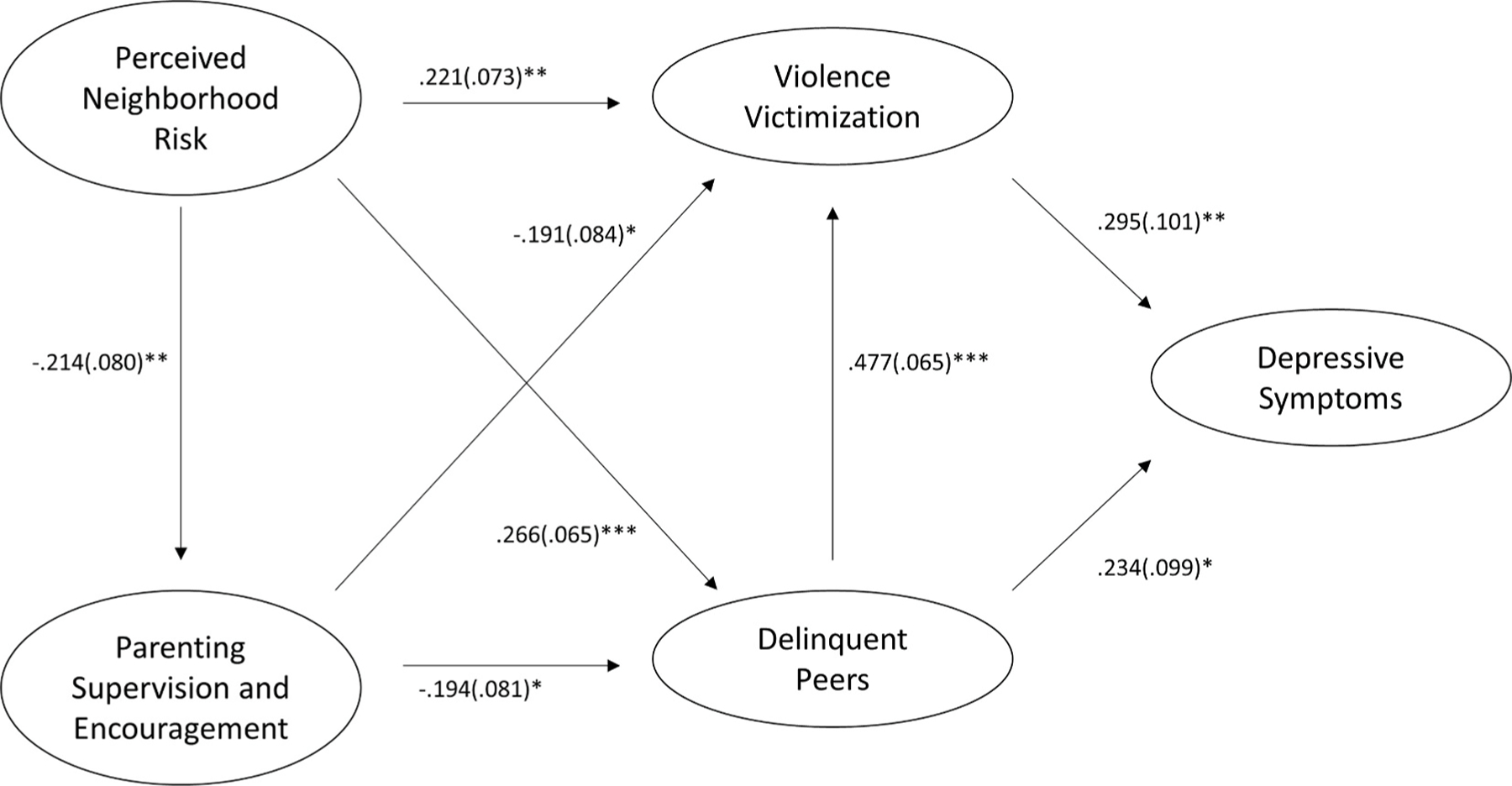
Final Structural Model for Violence Victimization (Standardized coefficients) (n = 226). *p < 0.05, **p < 0.01, **p < .001. Indirect Effects (DS = Depressive Symptoms). Perceived Neighborhood Risk - > DS = 0.066. Delinquent Peers - > DS = 0.143. Parenting Behaviors (Supervision and Encouragement) - > DS = 0.057. Data Source: DCFAM (2012).
Fig. 3.
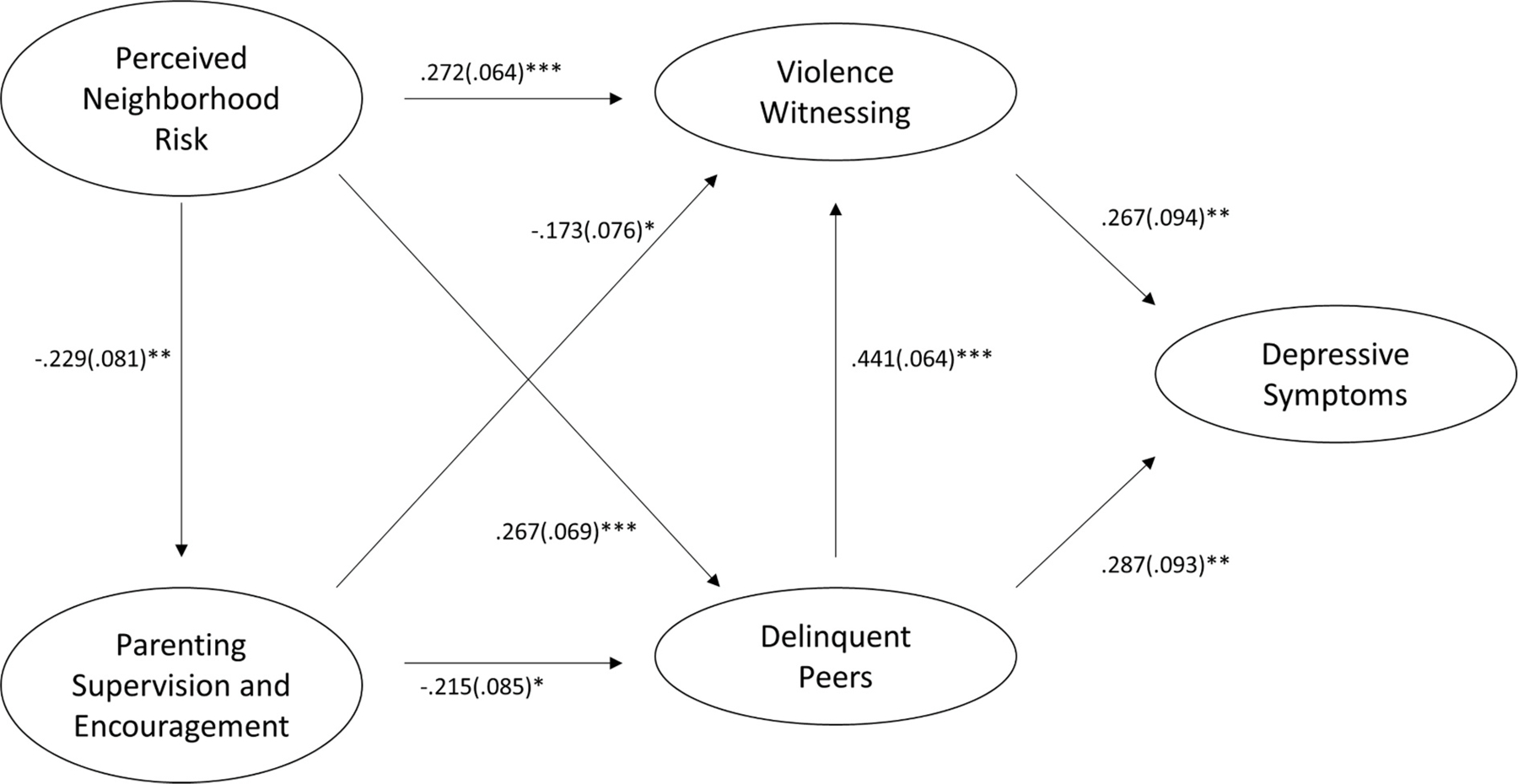
Final Structural Model for Violence Witnessing (Standardized coefficients) (n = 222). *p < 0.05, **p < 0.01, ***p < .001. Indirect Effects (DS = Depressive Symptoms) Perceived Neighborhood Risk - > DS = 0.073. Delinquent Peers - > DS = 0.118. Parenting Behaviors (Supervision and Encouragement) - > DS = 0.046. Data Source: DCFAM (2012).
4.4. Indirect and total effects
Indirect effects and total effects were calculated for the mediating associations between perceived neighborhood risk, parenting behaviors, and exposure to delinquent peers and depressive symptoms through either being a victim of or witnessing community violence. Indirect and total effects are presented in Table 3. For the violence victimization model, the indirect effect of perceived neighborhood risk on depressive symptoms through being a victim of community violence was significant (B = 0.065, p = 0.036). This relationship was fully mediated by being a victim of community violence, as evidenced by the lack of a significant direct effect. The indirect effect of exposure to delinquent peers on depressive symptoms mediated by being a victim of community violence was also significant (B = 0.141, p = 0.007). Given the direct effect of exposure to delinquent peers on depressive symptoms, this relationship was only partially mediated by being a victim of community violence with a total effect of B = 0.375. While parenting behavior also had a fully mediated, indirect effect on depressive symptoms via being a victim of community violence, this effect was only trending toward significance (B = −0.056, p = 0.073).
Table 3.
| Violence (Victim) Model (n = 226) | Direct Effect | Indirect Effect | Total Effect |
|---|---|---|---|
| Perceived Neighborhood Risk - > Depressive Symptoms | – | 0.065* | – |
| Parenting Behaviors - > Depressive Symptoms | – | −0.056 | – |
| Delinquent Peers - > Depressive Symptoms | 0.234* | 0.141** | 0.375 |
| Violence (Witness) Model (n = 222) | |||
| Perceived Neighborhood Risk - > Depressive Symptoms | – | 0.073* | – |
| Parenting Behaviors - > Depressive Symptoms | – | −0.046 | – |
| Delinquent Peers - > Depressive Symptoms | 0.287** | 0.118** | 0.405 |
Notes.
p<.05,
p<.01,
p<.001
Calculated manually using the Sobel Test (Sobel, 1986). Data Source: DCFAM (2012).
P values calculated using powerMediation package in R (Qui, 2018).
For the violence witnessing model, the indirect effect of perceived neighborhood risk on depressive symptoms, which was fully mediated by witnessing community violence, was also significant (B = 0.073, p = 0.018). Similar to the victimization model, exposure to delinquent peers had a partially mediated, significant indirect effect on depressive symptoms as well (B = 0.118, p = 0.009). The total effect of exposure to delinquent peers on depressive symptoms is B = 0.405. Lastly, parenting behavior also had a fully mediated, non-significant effect on depressive symptoms, though it was approaching significance (B = −0.046, p = 0.076).
6. Discussion
This study examined the influence of perceived neighborhood risks, parental behaviors, and peers on the relationship between community violence exposure and depressive symptoms in a sample of African American youth and young adults in urban public housing communities. We believe that findings reported in this study make a unique contribution to the state of knowledge by examining co-occurring socioecological risk and protective factors associated with community violence exposure and youth mental health. Whereas prior research has examined the effects of family, peer, and community factors independently, we examined them as a co-occurring system in the lives of a vulnerable group of youth living in U.S. public housing. Below we explain these findings within the context of the existing body of knowledge with respect to racially segregated and poor communities and the myriad distal (i.e., structural) and proximal (i.e., social interactions) problems that such communities experience.
First, we found that exposure to delinquent peers and community violence had direct adverse consequences for youth depression, adding to the uncertain literature on associations between community violence exposure and depressive symptoms. However, whereas prior literature suggests differential mental health effects for youth that experience direct victimization compared to those who witness community violence (Fowler et al., 2009) our findings reveal that both witnessing and direct victimization by community violence have devastating effects on youth depressive symptoms. These findings suggest that exposure to community violence has pernicious effects even for youth who are not directly victimized.
Findings of this study also highlighted the effects of witnessing violence (e.g., indirect victimization) on adolescents’ depressive symptoms. Although beyond the scope of the current study, it is very likely that the effects of witnessing violence on depressive symptoms may be attributed to a legacy of violence (e.g., urban war stories shared within families and among peers), the constant threat of violence (e.g., hearing gunshots), and/or due to the constant presence of violent reminders (e. g., makeshift memorials in the community) (Goering and Feins, 2003). These observations are in line with premises of social learning theory suggesting that the effects of community violence on adolescents’ depressive symptoms may be due to the vicarious effects of witnessing violence (Dubow et al., 2009; A. J. Smith et al., 2017).
Our findings also highlight the salience of peer effects on youth mental health and exposure to community violence; largely supporting existing literature that elucidate the direct and indirect effects of exposure to delinquent peers on youth mental health. This finding may be best explained by social contagion theory (Fagan et al., 2007) and may also lend additional empirical support to this theory. Although not directly related to violence and depressive symptoms, previous research has identified contagion effects in alcohol and drug use (Rowe and Rodgers, 1994) delinquency (Jones, 1997), and suicidal behaviors (Gould and Lake, 2013). Indeed, it is likely that pervasive violence experienced by youth and young adults in public housing communities has created a hopeless or depressive script that is shared among youth within these communities (Fagan et al., 2007). In addition to pervasive violence, many of these communities are ground zero for the War of Drugs and the police hostility that it leaves in its wake (Alexander, 2012). Furthermore, although not assessed in our data, the heavy presence of law enforcement is probably perceived as additional acts of violence by youth and young adults contributing to their shared script of hopelessness.
Our findings also offer new insights into the co-occurring socioecological factors that affect youth mental health. For youth and young adults in our study, parenting behaviors such as supervision and encouragement were associated with reduced exposure to community violence and delinquent peers, adding a unique contribution to the uncertain literature on the protective effects of positive parenting behaviors on youth exposure to violence. Prior literature suggests both protective effects (e.g., reduced exposure) (Copeland-Linder et al., 2010) as well as null effects (Salzinger et al., 2011) of parenting behaviors on youth community violence exposure. Thus, our findings that positive parenting behaviors reduced youth exposure to community violence and delinquent peers adds a unique contribution to the uncertain literature in this area. While this finding is promising for youth in our study, the socioecological context of violence exposure in many communities indicates that violence may be community-wide, frequent, and unavoidable (Sheidow et al., 2001; Voisin et al., 2016) and therefore minimize the theorized protective effects of parenting behaviors on community violence exposure (Salzinger et al., 2011). For example, pervasive community violence may not only impact youth mental health but also impair parents’ capacity to protect their children (Hurd et al.,2013).
Prior research has also shown that perceptions of neighborhood conditions directly influence youth mental health (Aneshensel and Sucoff, 1996; D. Kim, 2008; J. Kim and Ross, 2009; Kruger et al., 2007). However, we found that perceived neighborhood risks were indirectly associated with youth mental health and were fully mediated by exposure to community violence. These findings suggest that interventions designed to improve the community environment or strengthen positive parenting behaviors without directly reducing community violence may be minimally effective at reducing youth depressive symptoms.
Taken together, our findings highlight the need for comprehensive and targeted interventions that address the co-occurring socioecological factors influencing youth mental health in public housing communities. Such interventions must incorporate strategies at multiple socioecological levels and involve cross-sector partnerships to address the complex relationship between neighborhood conditions, community violence, and youth development.
7. Limitations
Study findings must be considered alongside study limitations. We utilized a cross-sectional design which precludes our ability to establish causal relationships. Additionally, results are based on a narrow sample of African American youth (i.e., urban and living in public housing neighborhoods). Thus, a different set of mediators may emerge among African American youth from different social contexts. There may also be other salient factors (e.g., parent-child relationship dynamics, length of residence, mental health status prior to violence exposure, police violence and over-policing) that are associated with violence exposure and youth mental health, but which are beyond the scope of our data. It is also likely that risk and protective factors associated with violence exposure and youth mental health function differently for youth of different social identities. For instance, evidence suggests that there may be moderating effects by gender (Fowler et al., 2009; Javdani et al., 2014; Wamser-Nanney and Cherry, 2018). Additionally, we believe there could potentially be moderation by housing type (i.e. private vs. public subsidized housing). However, due to inadequate statistical power, we were unable to test these proposed moderating effects. Despite these limitations, this study advances our understanding of community violence experienced by urban African American youth that live in public housing and under resourced neighborhoods, an important area of inquiry given the high rates violence and effects on the mental health of this vulnerable population of youth.
8. Conclusion and implications
Taken together, our findings highlight the need for comprehensive and targeted interventions that address the co-occurring socioecological factors influencing the mental health of youth and young adults living in public housing communities. Such interventions may need to incorporate strategies at multiple socioecological levels and involve cross-sector partnerships to address the complex relationship between neighborhood conditions, community violence, and youth development. Drawing upon these findings, we present recommendations for interventions to prevent and treat community violence exposure and interrupt the predictable pattern of community violence in inadequately resourced urban neighborhoods.
First, interventions that treat the effects of youth community violence exposure are vital to healthy youth development. Traumainformed interventions, many of which are based on cognitivebehavioral therapy (CBT), appear generally effective at reducing internalizing symptoms, preventing revictimization, and reducing future perpetration (Abt, 2017; Darawshy et al., 2020). Stable and positive social support systems and positive school environments are also important resources that help youth cope with exposure to violence (Cooley-Stricland et al., 2011; Cooley and Lambert, 2006; Darawshy et al., 2020; Dulmus, 2003; Morrison, 2000). Therefore, school-based CBT interventions that target the mental health consequences of community violence exposure are clearly needed.
Interventions to reduce exposure to community violence are also needed to support youth and young adults. However, there exists relatively few preventative interventions to reduce youth community violence exposure (Fowler and Braciszewski, 2009; Voisin and Berringer, 2014). Most interventions toward reducing community violence exposure involve strengthening family dynamics and peer relationships (Thomas et al., 2011). While interventions to strengthen parent capacity to protect children from exposure to violence and promote positive peer relationships may be necessary, they are unlikely to be effective if implemented apart from interventions designed to address the multiple interacting socioecological factors that affect the etiology of community violence and its reproduction. Therefore, interventions that target youth social support, peer relationships, and provide opportunities to address community violence in cooperation with community stakeholders seem necessary and promising (Thomas et al., 2011).
Our findings reinforce the notion that targeting individual and family risk factors, or proximal socioecological factors, may be necessary but not sufficient for preventing youth exposure to violence and disrupting detrimental mental health effects. Although such interventions are important, they are unlikely to make significant headway towards population-level health effects for African American youth and young adults in urban environments given the frequency and universality of community violence exposure (Voisin et al., 2016) and failure to adequately address underlying community-level factors that influence the epidemiology of violence (Massetti and David-Ferdon, 2016). This observation underscores the need for interventions implemented as part of multilevel strategies to address community violence exposure and reduce community violence itself.
A consistent approach to reduce community violence has been to invest in policing and law enforcement to reduce crime. Yet, community violence exposure often includes exposure to police violence and is a key source of trauma for youth (Nordberg et al., 2016; Woods-Jaeger et al., 2019). Indeed, youth experiences with law enforcement as a unique form of community violence, and the extent to which these experiences influence mental health, represents a key area for future research. Additionally, policing interventions to reduce violence have demonstrated mixed effects (Braga et al., 2014, 2018; Gill et al., 2014), and community-police relationships are often tenuous due to racial biases and undue abuses of power toward racial subordination. Therefore, investments in law enforcement must be balanced with investments to address structural and systemic factors that give rise to violence and its spatial distribution. The evidence is clear that heightened surveillance, punishment, and apprehension are not effective crime prevention strategies (Abt, 2017; Braga et al., 2018). Such strategies must be incorporated into more effective crime reduction strategies such as problem-oriented policing, focused deterrence, and community-based crime prevention approaches (Abt, 2017; Braga et al., 2014; 2018; Gill et al., 2014).
Our findings suggest that a comprehensive multilevel community-based intervention agenda is needed. The best strategies to prevent community violence start early and involve systems that directly serve youth and their families. These strategies must be comprehensive, sustained, and target changing community conditions at multiple levels (Cohen et al., 2016). Access to high quality schools, living wage jobs, affordable housing, and quality public services are vital in the fight to reduce community violence (Boyd-Swan et al., 2016; Branas et al., 2018; Brotman et al., 2016; Cohen et al., 2016; Kondo et al., 2016; Reeves et al., 2017). Additionally, interventions that are community-based and target youth along with the social and structural systems that affect their lives are needed above and beyond person-centered approaches (Farahmand et al., 2012). These types of structural interventions are also integral towards addressing youth mental health. For example, Reeves et al. (2017) found that livable minimum wage policies reduced poverty and depressive symptoms among low-wage workers. Living wage policies represent a structural intervention that provide vital resources for families and their children. Similarly, programs such as the Earned Income Tax Credit (EITC) has also been shown to reduce depressive symptoms among adults, particularly mothers with children, and should be expanded (Boyd-Swan et al., 2016). Implementing greening interventions on vacant and abandoned properties also seems promising towards crime reduction as a mechanism for reducing risks of community violence exposure among youth and young adults (Branas et al., 2018; Kondo et al., 2016). Once violence occurs, programs and services that treat and reduce exposure are vital to healthy youth development. Such interventions must increase access to culturally relevant mental health services embedded in trusted community institutions, increase investments in neighborhood infrastructure, and include mechanisms for public accountability for addressing community violence (Woods-Jaeger et al., 2019). These interventions should also target individual and family risk factors alongside structural and systems change efforts at larger socioecological levels (Massetti and David-Ferdon, 2016). Within severely distressed neighborhoods such as those often emblematic of U.S. public housing, targeted and comprehensive interventions are sorely needed and represent promising approaches to community violence prevention.
Acknowledgements
We would like to acknowledge our research team for their diligence at building rapport with our community partners, which established a solid foundation for our data collection. They were also critical in debriefing our community partners on the importance of their participation. We acknowledge Drs. Sharon Alston and Ajita Robinson for their leadership and for their unwavering commitment to this study. We would also like to acknowledge the faculty at the Jane Addams College of Social Work at the University of Illinois Chicago for their assistance in developing the research protocol and their support throughout the IRB process. Finally, we would like to acknowledge the John D. and Katherine T. MacArthur Foundation for sponsoring this exploration. This research was presented at the Society for Social Work and Research (SSWR) 23rd Annual Conference, San Francisco, California, January 16–20, 2019.
Funding
This work was made possible by the John D. and Katherine T. MacArthur Foundation, 40 S. Dearborn Street, Chicago, IL 60603–5285; grant numbers 2010–0297; 2010–2013.
Footnotes
Declaration of competing interest
None.
References
- Abt TP, 2017. Towards a framework for preventing community violence among youth. Psychol. Health Med. Taylor & Francis 22, 266–285. 10.1080/13548506.2016.1257815. [DOI] [PubMed] [Google Scholar]
- Ahmad F, et al. , 2017. Mental health problems due to community violence exposure in a small urban setting. Fam. Med. & Commun. Health 5 (3), 170–178. 10.15212/FMCH.2017.0128. [DOI] [Google Scholar]
- Aizer A, 2008. Neighborhood violence and urban youth 13773. Cambridge, MA. Available at: http://www.nber.org/papers/w13773.pdf. [Google Scholar]
- Alexander M, 2012. The New Jim Crow: Mass Incarceration in the Age of Colorblindness The New Press, New York, NY. [Google Scholar]
- Allison PD, 2001. Missing data. In: Sage University Papers Series on Quantitative Applications in the Social Sciences, vol. 136. SAGE Publications, Inc. https://us.sagepub.com/en-us/nam/missing-data/book9419#contents. [Google Scholar]
- Andrews R, Casey M, Hardy BL, Logan TD, 2017. Location matters: historical racial segregation and intergenerational mobility. Econ. Lett 158, 67–72. 10.1016/j.econlet.2017.06.018. [DOI] [Google Scholar]
- Aneshensel CS, Sucoff CA, 1996. The neighborhood context of adolescent mental health. J. Health Soc. Behav 37 (4), 293–310. [PubMed] [Google Scholar]
- Bacchini D, Miranda MC, Affuso G, 2011. Effects of parental monitoring and exposure to community violence on antisocial behavior and anxiety/depression among adolescents. J. Interpers Violence 26 (2), 269–292. 10.1177/0886260510362879. [DOI] [PubMed] [Google Scholar]
- Bowen NK, Guo S, 2012. Structural Equation Modeling Oxford University Press, New York, NY. [Google Scholar]
- Boyd-Swan C, Herbst CM, Ifcher J, Zarghamee H, 2016. The earned income tax credit, mental health, and happiness. J. Econ. Behav. Organ 126, 18–38. 10.1016/j.jebo.2015.11.004. [DOI] [Google Scholar]
- Braga AA, Papachristos AV, Hureau DM, 2014. ‘The effects of hot spots policing on crime: an updated systematic review and meta-analysis. Justice Quart 31 (4), 633–663. 10.1080/07418825.2012.673632. Routledge. [DOI] [Google Scholar]
- Braga AA, Weisburd D, Turchan B, 2018. Focused deterrence strategies and crime control: an updated systematic review and meta-analysis of the empirical evidence. Criminol. Publ. Pol 17 (1), 205–250. 10.1111/1745-9133.12353. [DOI] [Google Scholar]
- Branas CC, South E, Kondo MC, Hohl BC, Bourgois P, Wiebe DJ, MacDonald JM, 2018. Citywide cluster randomized trial to restore blighted vacant land and its effects on violence, crime, and fear. PNAS Proc. Nat. Acad. Sci. U. S. A 115 (12), 2946–2951. 10.1073/pnas.1718503115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U, Ceci SJ, 1994. ‘Nature-nurture reconceptualized in developmental perspective : a bioecological model’. Psychol. Rev 101 (4), 568–586. [DOI] [PubMed] [Google Scholar]
- Brotman LM, Dawson-McClure S, Kamboukos D, Huang K-Y, Calzada EJ, Goldfeld K, Petkova E, 2016. Effects of ParentCorps in prekindergarten on child mental health and academic performance: follow-up of a randomized clinical trial through 8 years of age. JAMA Pediatr 170 (12), 1149–1155. 10.1001/jamapediatrics.2016.1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, Cudeck R, 1993. Alternative ways of assessing model fit. In: Bollen KA, Long JS (Eds.), Testing Structural Equation Models SAGE Publications, Inc., Newbury Park, CA, pp. 136–162. [Google Scholar]
- Browning CR, et al. , 2017. Understanding racial differences in exposure to violent areas: integrating survey, smartphone, and administrative data sources. Ann. Am. Acad. Polit. Soc. Sci 669 (1), 41–62. 10.1177/0002716216678167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butcher F, et al. , 2015. The impact of neighborhood disorganization on neighborhood exposure to violence, trauma symptoms, and social relationships among at-risk youth. In: Social Science & Medicine, 146. Elsevier Ltd, pp. 300–306. 10.1016/j.socscimed.2015.10.013. [DOI] [PubMed] [Google Scholar]
- Casciano R, Massey DS, 2012. Neighborhood disorder and anxiety symptoms: new evidence from a quasi-experimental study. Health & Place 18 (2), 180–190. 10.1016/j.healthplace.2011.09.002. Elsevier. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceballo R, et al. , 2003. ‘Community violence and children’s psychological well-being: does parental monitoring matter?’. J. Clin. Child Adolesc. Psychol 32 (4), 586–592. 10.1207/S15374424JCCP3204. [DOI] [PubMed] [Google Scholar]
- Chiteji N, 2016. The connection between segregation, predatory lending, and black wealth. The Dream Revisited: Contemporary Debates about Housing, Segregaton, and Opportunity https://furmancenter.org/research/iri/essay/the-connection-between-segregation-predatory-lending-and-black-wealth.
- Cicchetti D, Rogosch FA, 1996. Equifinality and multifinality in developmental psychopathology. Dev. Psychopathol 8, 597–600. [Google Scholar]
- Cohen L, Davis R, Realini A, 2016. Violence affecting youth: pervasive and preventable. In: Korin MR (Ed.), Health Promotion for Children and Adolescents Springer, New York, NY, pp. 235–262. 10.1007/978-1-4899-7711-3. [DOI] [Google Scholar]
- Coll CG, et al. , 1996. An integrative model for the study of developmental competencies in minority children. Child Dev 67 (5), 1891–1914. [PubMed] [Google Scholar]
- Cooley MR, Lambert SF, 2006. School-based interventions for children exposed to community violence. In: Lieberman AF, DeMartino R (Eds.), Interventions for Children Exposed to Violence Johnson & Johnson Pediatric Institute, LLC, New Brunswick, NJ, pp. 187–208. [Google Scholar]
- Cooley-Stricland MR, et al. , 2011. Urban African American youth exposed to community violence: a school-based anxiety preventive intervention efficacy study. J. Prevent. Intern. Comm 39 (2), 149–166. 10.1080/10852352.2011.556573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland-Linder N, Lambert SF, Ialongo NS, 2010. Community violence, protective factors, and adolescent mental health: a profile analysis. J. Clin. Child Adolesc. Psychol 39 (2), 176–186. 10.1080/15374410903532601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry A, Latkin C, Davey-Rothwell M, 2008. Pathways to depression: the impact of neighborhood violent crime on inner-city residents in Baltimore, Maryland, USA. Soc. Sci. Med 67, 23–30. 10.1016/j.socscimed.2008.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutrona CE, Wallace G, Wesner KA, 2006. Neighborhood characteristics and depression: an examination of stress processes. Curr. Dir. Psychol. Sci 15 (4), 188–192. 10.1111/j.1467-8721.2006.00433.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darawshy NA-S, Gewirtz A, Marsalis S, 2020. Psychological intervention and prevention programs for child and adolescent exposure to community violence: a systematic review. Clin. Child Fam. Psychol. Rev, 0123456789 10.1007/s10567-020-00315-3. [DOI] [PubMed] [Google Scholar]
- Desmond M, 2014. Poor black women are evicted at alarming rates, setting off a chain of hardship https://www.macfound.org/media/files/hhm_research_brief_-_poor_black_women_are_evicted_at_alarming_rates.pdf.
- Dubow EF, Huesmann LR, Boxer P, 2009. ‘A social-cognitive-ecological framework for understanding the impact of exposure to persistent ethnic-political violence on children’s psychosocial adjustment’. Clin. Child Fam. Psychol. Rev 12 (2), 113–126. 10.1007/s10567-009-0050-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dulmus CN, 2003. Approaches to preventing the psychological impact of community violence exposure on children. Crisis Intervent. Time Limited Treatment 6 (3), 185–202. 10.1080/713638933. [DOI] [Google Scholar]
- Duncan DF, 1996. Growing up under the gun: children and adolescents coping with violent neighborhoods. J. Prim. Prev 16 (4), 343–356. 10.1007/BF02411740. [DOI] [PubMed] [Google Scholar]
- Eron LD, Guerra N, Huesmann LR, 1997. Poverty and violence. In: Feshbach S, Zagrodzka J (Eds.), Aggression: Biological, Developmental, and Social Perspectives, first ed. Springer Science + Business Media, LLC, New York, NY, pp. 139–154 10.1007/978-1-4615-5883-5. [DOI] [Google Scholar]
- Estreet AT, et al. , 2018. ‘Examining the role of parental factors on depression among urban African American youth living in public housing. J. Human Behav. Soc. Environ 28 (4), 494–508. 10.1080/10911359.2018.1430647. Routledge. [DOI] [Google Scholar]
- Fagan J, Wilkinson DL, Davies G, 2007. Social contagion of violence. In: Flannery DJ, Vazsony AT, Waldman ID (Eds.), The Cambridge Handbook of Violent Behavior and Aggression Cambride University Press, New York, NY. [Google Scholar]
- Farahmand FK, Duffy SN, Tailor MA, Dubois DL, Lyon AL, Grant KE, Zarlinski JC, Masini O, Zander KJ, Nathanson AM, 2012. Community-based mental health and behavioral programs for low-income urban youth: a meta-analytic review. Clin. Psychol. Sci. Pract 19 (2), 195–215. 10.1111/j.1468-2850.2012.01283.x. [DOI] [Google Scholar]
- Finkelhor D, et al. , 2015. Children’s exposure to violence, crime, and abuse: an update, Juvenile Justice Bulletin Laural, MD. Available at: http://www.ojjdp.gov/Publications/PubResults.asp?sei=94%5Cnhttp://www.ojjdp.gov/pubs/248547.pdf. [Google Scholar]
- Fowler PJ, Braciszewski JM, 2009. Community violence prevention and intervention strategies for children and adolescents: the need for multilevel approaches. J. Prev. Interv. Community 37 (4), 255–259. 10.1080/10852350903196258. [DOI] [PubMed] [Google Scholar]
- Fowler PJ, et al. , 2009. Community violence: a meta-analysis on the effect of exposure and mental health outcomes of children and adolescents. Dev. Psychopathol 21 (1), 227–259. 10.1017/S0954579409000145. [DOI] [PubMed] [Google Scholar]
- Frazer E, et al. , 2018. The violence epidemic in the African American community: a call by the National Medical Association for comprehensive reform. J. Nat. Med. Assoc 110 (1), 4–15. 10.1016/j.jnma.2017.08.009. Elsevier Inc. [DOI] [PubMed] [Google Scholar]
- Friedline T, Chen Z, Morrow SP, 2020. ‘Families’ financial stress & well-being: the importance of the economy and economic environments’. J. Fam. Econ. Issues 10.1007/s10834-020-09694-9 (online first). [DOI] [PMC free article] [PubMed]
- Friedson M, Sharkey P, 2015. Violence and neighborhood disadvantage after the crime decline. Ann. Am. Acad. Polit. Soc. Sci 660 (1), 341–358. 10.1177/0002716215579825. [DOI] [Google Scholar]
- Furstenberg FF, et al. , 2000. Managing to Make it: Urban Families and Adolescent Success University of Chicago Press, Chicago, IL. [Google Scholar]
- Garbarino J, Kosteny K, Dubrow N, 1991. What children can tell us about living in danger. Am. Psychol 46 (4), 376–383. 10.1037//0003066x.46.4.376. [DOI] [PubMed] [Google Scholar]
- Gaylord-Harden NK, Cunningham JA, Zelencik B, 2011. Effects of exposure to community violence on internalizing symptoms: does desensitization to violence occur in African American youth? J. Abnorm. Child Psychol 39 (5), 711–719. 10.1007/s10802-011-9510-x. [DOI] [PubMed] [Google Scholar]
- Gibson CL, Morris SZ, Beaver KM, 2009. Secondary exposure to violence during childhood and adolescence: does neighborhood context matter. Justice Q. JQ 26 (1), 30–57. 10.1080/07418820802119968. [DOI] [Google Scholar]
- Gill C, et al. , 2014. Community-oriented policing to reduce crime, disorder and fear and increase satisfaction and legitimacy among citizens: a systematic review. J. Exp. Criminol 10 (4), 399–428. 10.1007/s11292-014-9210-y. [DOI] [Google Scholar]
- Giurgescu C, et al. , 2015. The impact of neighborhood quality, perceived stress, and social support on depressive symptoms during pregnancy in African American women. In: Social Science and Medicine, 130. Elsevier Ltd, pp. 172–180. 10.1016/j.socscimed.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goering J, Feins JD, 2003. Choosing a Better Life?: Evaluating the Moving to Opportunity Social Experiment Rowman & Littlefield Publishers; Urban Institute Press, Washington, D.C. [Google Scholar]
- Goetz EG, 2013. New Deal Ruins: Race, Economic Justice, & Public Housing Policy Cornell University Press, Ithaca, NY. [Google Scholar]
- Gordon C, 2008. Mapping Decline: St. Louis and the Fate of the American City University of Pennsylvania Press, Philadelphis, PA. [Google Scholar]
- Gordon C, Bruch SK, 2020. Home inequity: race, wealth, and housing in St. Louis since 1940. Hous. Stud 35 (7), 1285–1308. 10.1080/02673037.2019.1657073. [DOI] [Google Scholar]
- Gorman-Smith D, Tolan P, 1998. The role of exposure to community violence and developmental problems among inner-city youth. Dev. Psychopathol 10, 101–116. [DOI] [PubMed] [Google Scholar]
- Gorman-Smith D, Henry D, Tolan P, 2004. ‘Relation of adolescent mothers’ history of antisocial behavior to child conduct problems and social competence’. J. Clin. Child Adolesc. Psychol 33 (3), 463–476. 10.1207/s15374424jccp3303. [DOI] [PubMed] [Google Scholar]
- Gould MS, Lake AM, 2013. The contagion of suicidal behavior. In: Forum on Global Violence Prevention et al. (eds) Contagion of. Violence: Workshop Summary. National Academies Press (US), Washington, D.C., pp. 68–72. 10.17226/13489 [DOI] [Google Scholar]
- Graif C, Matthews SA, 2017. ‘The long arm of poverty: extended and relational geographies of child victimization and neighborhood violence exposures. Justice Quart 34 (6), 1096–1125. 10.1080/07418825.2016.1276951. Routledge. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths E, 2013. Race, space, and the spread of violence across the city. Soc. Probl 60 (4), 491–512. 10.1525/sp.2013.60.4.491. [DOI] [Google Scholar]
- Harris KM, et al. , 2009. The National Longitudinal Study of Adolescent to Adult Health: Add Health Codebook Explorer (ACE)
- Hinton E, Cook D, 2021. The mass criminalization of black Americans: a historical overview. Annu. Rev. Criminol 4 (1), 261–286. 10.1146/annurevcriminol-060520-033306. [DOI] [Google Scholar]
- Hu L, Bentler PM, 1999. ‘Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equat. Model 6 (1), 1–55. 10.1080/10705519909540118. [DOI] [Google Scholar]
- Huang X, King C, McAtee J, 2018. Exposure to violence, neighborhood context, and health-related outcomes in low-income urban mothers. In: Health & Place, 54. Elsevier Ltd, pp. 138–148. 10.1016/j.healthplace.2018.09.008. August 2017. [DOI] [PubMed] [Google Scholar]
- Hurd NM, Stoddard SA, Zimmerman MA, 2013. ‘Neighborhoods, social support, and African American adolescents’ mental health outcomes: a multilevel path analysis’. Child Dev 84 (3), 858–874. 10.1111/cdev.12018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Javdani S, et al. , 2014. Gender differences in the effects of community violence on mental health outcomes in a sample of low-income youth receiving psychiatric care. Am. J. Community Psychol 53 (3–4), 235–248. 10.1007/s10464-014-9638-2. [DOI] [PubMed] [Google Scholar]
- Jones MB, 1997. Behavioral contagion and official delinquency: epidemic course in adolescence. Soc. Biol 45 (1–2), 134–142. 10.1080/19485565.1998.9988968. [DOI] [PubMed] [Google Scholar]
- Jordan M, 2003. ‘Buffers of, and Risks for, Children’s Exposure to Community Violence and Negative Emotional Adjustment’ Loyola University Chicago, Chicago, IL. [Google Scholar]
- Kang H, 2013. The prevention and handling of the missing data. Kor. J. Anesthesiol 64 (5), 402–406. 10.4097/kjae.2013.64.5.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly S, 2010. The psychological consequences to adolescents of exposure to gang violence in the community: an integrated review of the literature. J. Child Adolesc. Psychiatr. Nurs 23 (2), 61–73. 10.1111/j.1744-6171.2010.00225.x. [DOI] [PubMed] [Google Scholar]
- Kennedy TM, Ceballo R, 2014. Who, what, when, and where? Toward a dimensional conceptualization of community violence exposure. Rev. Gen. Psychol 18 (2), 69–81. 10.1037/gpr0000005. [DOI] [Google Scholar]
- Kim D, 2008. Blues from the neighborhood? Neighborhood characteristics and depression. Epidemiol. Rev 30 (1), 101–117. 10.1093/epirev/mxn009. [DOI] [PubMed] [Google Scholar]
- Kim J, Ross CE, 2009. Neighborhood-specific and general social support: which buffers the effect of neighborhood disorder on depression? J. Community Psychol 37 (6), 725–736. 10.1002/jcop.20327. [DOI] [Google Scholar]
- Kondo M, Hohl B, Han S, Branas C, 2016. Effects of greening and community reuse of vacant lots on crime. Urban Stud 53 (15), 3279–3295. 10.0.4.153/0042098015608058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruger DJ, Reischl TM, Gee GC, 2007. Neighborhood social conditions mediate the association between physical deterioration and mental health. Am. J. Community Psychol 40 (3–4), 261–271. 10.1007/s10464-007-9139-7. [DOI] [PubMed] [Google Scholar]
- Lambert SF, et al. , 2011. Examining the developmental process of risk for exposure to community violence among urban youth. J. Prev. Interv. Community 39 (2), 98–113. 10.1080/10852352.2011.556558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert SF, Barksdale CL, Nebbitt VE, 2015. The relationship between neighborhood risk and adolescent health-risk behaviors: A focus on adolescent depressive symptoms. In: Adolescents in Public Housing: Addressing Psychological and Behavioral Health Columbia University Press, pp. 109–139. [Google Scholar]
- Lamborn SD, et al. , 1991. Patterns of competence and adjustment among adolescents from authoritative, authoritarian, indulgent, and neglectful families. Child Dev 62 (5), 1049–1065. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Curry AD, 2003. Stressful neighborhoods and depression: a prospective study of the impact of neighborhood disorder. J. Health Soc. Behav 44 (1), 34–44. https://www.jstor.org/stable/1519814. [PubMed] [Google Scholar]
- Latkin CA, et al. , 2007. Direct and indirect associations of neighborhood disorder with drug use and high-risk sexual partners. Am. J. Prev. Med 32 (6 Suppl. L), 234–241. 10.1016/j.amepre.2007.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lens MC, 2013. Subsidized housing and crime: theory, mechanisms, and evidence. J. Plann. Lit 28 (4), 352–363. 10.1177/0885412213500992. [DOI] [Google Scholar]
- Lombe M, Nebbitt VE, 2015. Risk and protective factors of depressive symptoms. In: Adolescents in public housing: Addressing psychological and behavioral health Columbia University Press, pp. 123–139. [Google Scholar]
- Low S, Espelage D, 2014. Conduits from community violence exposure to peer aggression and victimization: contributions of parental monitoring, impulsivity, and deviancy. J. Counsel. Psychol 61 (2), 221–231. 10.1037/a0035207. [DOI] [PubMed] [Google Scholar]
- Lu W, et al. , 2017. Psychometric properties of the CES-D among black adolescents in public housing. J. Soc. Soc. Work. Res 8 (4), 595–619. 10.1086/694791. [DOI] [Google Scholar]
- Margolin G, 2005. ‘Children’s exposure to violence: exploring developmental pathways to diverse outcomes’. J. Interpers Violence 20 (1), 72–81. 10.1177/0886260504268371. [DOI] [PubMed] [Google Scholar]
- Massetti GM, David-Ferdon C, 2016. Preventing violence among high-risk youth and communities with economic, policy, and structural strategies. MMWR Suppl 65 (1), 57–60. 10.15585/mmwr.su6501a9. [DOI] [PubMed] [Google Scholar]
- Matheson FI, Moineddin R, Dunn JR, Creatore MI, Gozdyra P, Glazier RH, 2006. Urban neighborhoods, chronic stress, gender and depression. Soc. Sci. Med 63 (10), 2604–2616. 10.1016/j.socscimed.2006.07.001. [DOI] [PubMed] [Google Scholar]
- McArdle N, Acevedo-Garcia D, 2017. ‘Consequences of segregation for children’s opportunity and wellbeing’. In: A Shared Future: Fostering Communities of Inclusion in an Era of Inequality https://www.jchs.harvard.edu/sites/default/files/media/imp/a_shared_future_consequences_of_segregation_for_children.pdf.
- McDonald CC, Richmond TR, 2008. The relationship between community violence exposure and mental health symptoms in urban adolescents. J. Psychiatr. Ment. Health Nurs 15 (10), 833–849. 10.1111/j.1365-2850.2008.01321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald CC, et al. , 2011. Community violence exposure and positive youth development in urban youth. J. Community Health 36 (6), 925–932. 10.1007/s10900-011-9391-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moed A, Gershoff ET, Bringewatt EH, 2017. Violence exposure as a mediator between parenting and adolescent mental health. Child Psychiatr. Human Dev 48 (2), 235–247. 10.1007/s10578-016-0636-5. Springer US. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, the Klaus-Grawe 2012 Think Tank, 2013. ‘Childhood exposure to violence and lifelong health: clinical intervention science and stress biology research join forces. Dev. Psychopathol 25 (402), 1–27. 10.1017/S0954579413000801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morenoff JD, Sampson RJ, Raudenbush SW, 2001. Neighborhood inequality, collective efficacy, and the spatial dynamics of urban violence. Criminology 39 (3), 517–558. 10.1111/j.1745-9125.2001.tb00932.x. [DOI] [Google Scholar]
- Morrison JA, 2000. ‘Protective factors associated with children’s emotional responses to chronic community violence exposure’. Trauma Violence Abuse 1 (4), 299–320. [Google Scholar]
- Muthén LK, & Muthén BO (no date) Mplus User’s Guide eighth ed. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nebbitt VE, 2015. Adolescents in public housing: Addressing psychological and behavioral health Columbia University Press. [Google Scholar]
- Nebbitt VE, Lombe M, 2007. Environmental correlates of depressive symptoms among African American adolescents living in public housing. Journal of Human Behavior in the Social Environment 15 (2–3), 435–454. 10.1300/J137v15n02_24. [DOI] [Google Scholar]
- Nordberg A, et al. , 2016. ‘Exploring minority youths’ police encounters: a qualitative interpretive meta-synthesis’. Child Adolesc. Soc. Work J 33 (2), 137–149. 10.1007/s10560-015-0415-3. Springer US. [DOI] [Google Scholar]
- Ozer EJ, et al. , 2017. Protective factors for youth exposed to violence in their communities: a review of family, school, and community moderators. J. Clin. Child Adolesc. Psychol 46 (3), 353–378. 10.1080/15374416.2015.1046178,2015. [DOI] [PubMed] [Google Scholar]
- Peterson RD, Krivo LJ, 2009. Segregated spatial locations, race-ethnic composition, and neighborhood violent crime. Ann. Am. Acad. Polit. Soc. Sci 623 (1), 93–107. 10.1177/0002716208330490. [DOI] [Google Scholar]
- Qiu W, 2018. ‘Package “powerMediation”: power/sample size calculation for mediation analysis. powerMediation: power/sample size calculation for mediation analysis. R package version 0.2.9. The Comprehensive R Archive Network (CRAN-R) 1–57.
- Reeves A, McKee M, Mackenbach J, Whitehead M, Stuckler D, 2017. Introduction of a national minimum wage reduced depressive symptoms in low-wage workers: a quasi-natural experiment in the UK. Health Econ 26 (5), 639–655. 10.1002/hec.3336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richters JE, Martinez P, 1993. The NIMH community violence project I: children as victims of and witnesses to violence. Psychiatry 56 (1), 7–21. [DOI] [PubMed] [Google Scholar]
- Rojas-Gaona CE, Hong JS, Peguero AA, 2016. The significance of race/ethnicity in adolescent violence: a decade of review, 2005–2015. J. Crim. Justice Educ. JCJE 46, 137–147. 10.1016/j.jcrimjus.2016.05.001. [DOI] [Google Scholar]
- Ross CE, Mirowsky J, 2009. Neighborhood disorder, subjective alienation, and distress. J. Health Soc. Behav 50 (1), 49–64. 10.1177/002214650905000104. [DOI] [PubMed] [Google Scholar]
- Rothstein R, 2017. The Color of Law: A Forgotten History of How Our Government Segregated America Liveright Publishing Corporation, New York, NY. [Google Scholar]
- Rowe DC, Rodgers JL, 1994. A social contagion model of adolescent sexual behavior: explaining race differences. Soc. Biol 41 (1–2), 1–18. 10.1080/19485565.1994.9988856. [DOI] [PubMed] [Google Scholar]
- Salzinger S, et al. , 2002. An ecological framework for understanding risk for exposure to community violence and the effects of exposure on children and adolescents. Aggress. Violent Behav 7 (5), 423–451. 10.1016/S1359-1789(01)00078-7. [DOI] [Google Scholar]
- Salzinger S, et al. , 2011. ‘Role of parent and peer relationships and individual characteristics in middle school children’s behavioral outcomes in the face of community violence’. J. Res. Adolesc 21 (2), 395–407. 10.1111/j.1532-7795.2010.00677.x.Role. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson RJ, 1993. The community context of violent crime. In: Wilson WJ (Ed.), Sociology and the Public Agenda SAGE Publications, Inc, pp. 259–286. 10.4135/9781483325484.n13. [DOI] [Google Scholar]
- Schaefer-McDaniel N, 2009. Neighborhood stressors, perceived neighborhood quality, and child mental health in New York City. Health Place 15 (1), 148–155. 10.1016/j.healthplace.2008.03.007. [DOI] [PubMed] [Google Scholar]
- Schumacker RE, Lomax RG, 2004. A Beginner’s Guide to Structural Equation Modeling, second ed. Lawrence Erlbaum, Mahwah, NJ. [Google Scholar]
- Schwab-Stone M, et al. , 1999. ‘No safe haven II: the effects of violence exposure on urban youth. J. Am. Acad. Child Adolesc. Psychiatr 38 (4), 359–367. 10.1097/00004583-199904000-00007. [DOI] [PubMed] [Google Scholar]
- Seal D, Nguyen A, Beyer K, 2014. Youth exposure to violence in an urban setting. Urbn. Stud. Res 1–11. 10.1155/2014/368047. [DOI]
- Sheidow AJ, et al. , 2001. Family and community characteristics: risk factors for inner-city youth. J. Community Psychol 29 (3), 345–360. [Google Scholar]
- Shukla KD, Wiesner M, 2015. Direct and indirect violence exposure: relations to depression for economically disadvantaged ethnic minority mid-adolescents. Violence Vict 30 (1), 120–135. 10.1891/0886-6708.VV-D-12-00042. [DOI] [PubMed] [Google Scholar]
- Slutkin G, Ransford C, Zvetina D, 2018. How the health sector can reduce violence by treating it as a contagion. AMA J. Ethics 20 (1), 47–55. 10.1001/journalofethics.2018.20.1.nlit1-1801. [DOI] [PubMed] [Google Scholar]
- Smith C, et al. , 1995. Resilient youth: identifying factors that prevent high-risk youth from engaging in delinquency and drug use. In: Hagan J (Ed.), Delinquency and Disrepute in the Life Course JAI Press, Greenwich, CT, pp. 217–247. [Google Scholar]
- Smith AJ, et al. , 2017. Protective factors, coping appraisals, and social barriers predict mental health following community violence: a prospective test of social cognitive theory. J. Trauma Stress 30, 245–253. 10.1002/jts.22197. [DOI] [PubMed] [Google Scholar]
- Snedker KA, Herting JR, 2016. Adolescent mental health: neighborhood stress and emotional distress. Youth Soc 48 (5), 695–719. 10.1177/0044118X13512335. [DOI] [Google Scholar]
- Sobel ME, 1986. Some new results on indirect effects and their standard errors in covariance structure models. Socio. Methodol 16, 159–186. [Google Scholar]
- Stein BD, et al. , 2003. Prevalence of child and adolescent exposure to community violence. Clin. Child Fam. Psychol. Rev 6 (4), 247–264. 10.1023/B:CCFP.0000006292.61072.d2. [DOI] [PubMed] [Google Scholar]
- Stiffman AR, et al. , 1999. Impact of environment on adolescent mental health and behavior: structural equation modeling. Am. J. Orthopsychiatry 69 (1), 73–86. [DOI] [PubMed] [Google Scholar]
- Thomas DE, et al. , 2011. Contemporary interventions to prevent and reduce community violence among African American youth. In: Lemelle A, Reed W, Taylor S (Eds.), Handbook of African American Health: Social and Behavioral Interventions Springer, New York, NY, pp. 113–128. 10.1007/978-1-4419-9616-9. [DOI] [Google Scholar]
- Turner HA, et al. , 2013. Community disorder, victimization exposure, and mental health in a national sample of youth. J. Health Soc. Behav 54 (2), 258–275. 10.1177/0022146513479384. [DOI] [PubMed] [Google Scholar]
- Voisin DR, Berringer KR, 2014. Interventions targeting exposure to community violence sequelae among youth: a commentary. Clin. Soc. Work. J 43 (1), 98–108. 10.1007/s10615-014-0506-1. [DOI] [Google Scholar]
- Voisin DR, et al. , 2012. Examining parental monitoring as a pathway from community violence exposure to drug use, risky sex, and recidivism among detained youth. J. Soc. Serv. Res 38 (5), 699–711. 10.1080/01488376.2012.716020. [DOI] [Google Scholar]
- Voisin D, et al. , 2016. No safe havens: protective parenting strategies for African American youth living in violent communities. Violence Vict 31 (3), 523–536. 10.1891/0886-6708.VV-D-14-00056. [DOI] [PubMed] [Google Scholar]
- Wamser-Nanney R, Cherry KE, 2018. Children’s trauma-related symptoms following complex trauma exposure: evidence of gender differences. In: Child Abuse and Neglect, 77. Elsevier, pp. 188–197. 10.1016/j.chiabu.2018.01.009. June 2017. [DOI] [PubMed] [Google Scholar]
- Woods-Jaeger B, et al. , 2019. Mitigating negative consequences of community violence exposure: perspectives from African American youth. Health Aff 38 (10), 1679–1686. 10.1377/hlthaff.2019.00607. [DOI] [PubMed] [Google Scholar]
- Zayas LH, Cabassa LJ, Perez MC, 2005. Capacity-to-consent in psychiatric research: development and preliminary testing of a screening tool. Res. Soc. Work. Pract 15 (6), 545–556. 10.1177/1049731505275867. [DOI] [Google Scholar]
- Zimmerman GM, Messner SF, 2013. ‘Individual, family background, and contextual explanations of racial and ethnic disparities in youths’ exposure to violence’. Am. J. Publ. Health 103 (3), 435–442. 10.2105/AJPH.2012.300931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zona K, Milan S, 2011. Gender differences in the longitudinal impact of exposure to violence on mental health in urban youth. J. Youth Adolesc 40 (12), 1674–1690. 10.1007/s10964-011-9649-3. [DOI] [PubMed] [Google Scholar]


