Abstract
Introduction
Transgender individuals are at risk for HIV. HIV risks are dynamic and there have been substantial changes in HIV prevention (e.g., pre-exposure prophylaxis [PrEP]). It is thus time to revisit HIV prevalence and burden among transgender individuals. The objective of this systematic review and meta-analysis was thus to examine worldwide prevalence and burden of HIV over the course of the epidemic among trans feminine and trans masculine individuals.
Methods
We conducted an updated systematic review by searching PsycINFO, PubMed, Web of Science, and Google Scholar, for studies of any research design published in in a peer-reviewed journal in any language that reported HIV prevalence among transgender individuals published between January 2000 and January 2019. Two independent reviewers extracted the data and assessed methodological quality. We then conducted a meta-analysis, using random-effects modelling, to ascertain standardized prevalence and the relative burden of HIV carried by transgender individuals by country and year of data collection, and then by geographic region. We additionally explored the impact of sampling methods and pre-exposure prophylaxis (PrEP).
Results
Based on 98 studies, overall standardized HIV prevalence over the course of the epidemic, based on weights from each country by year, was 19.9% (95% CI 14.7% - 25.1%) for trans feminine individuals (n = 48,604) and 2.56% (95% CI 0.0% - 5.9%) for trans masculine individuals (n = 6460). Overall OR for HIV infection, compared with individuals over age 15, was 66.0 (95% CI 51.4–84.8) for trans feminine individuals and 6.8 (95% CI 3.6–13.1) for trans masculine individuals. Prevalence varied by geographic region (13.5% - 29.9%) and sampling method (5.4% - 37.8%). Lastly, PrEP effects on prevalence could not be established.
Conclusion
Trans feminine and trans masculine individuals are disproportionately burdened by HIV. Their unique prevention and care needs should be comprehensively addressed. Future research should further investigate the impact of sampling methods on HIV prevalence, and monitor the potential impact of PrEP.
Introduction
Transgender individuals, defined as individuals who experience a misalignment between the sex they were assigned at birth and their gender identity or whose gender identity is incongruent with gender norms, [1, 2] are at significant risk for an HIV infection [3]. Individual level risk factors include condomless sex, particularly receptive anal sex, coinfection with other sexually transmitted infections, transactional sex, and the shared use of needles for hormone and/or silicon injections [4–8]. Individual level risk factors do not stand alone; they result from, and intersect with, other factors such as mental health difficulties, substance use, and many forms of marginalization and stigmatization that limit, among other things, educational and work opportunities, as well as legal recognition of one’s chosen gender [6, 9–14]. Given that HIV risk among transgender individuals is a dynamic phenomenon, it is important to regularly monitor and update our knowledge of HIV prevalence and burden, such that we can identify trends that can inform policy-making and interventions. Here, we present a comprehensive updated systematic review of HIV prevalence over the course of the epidemic and a meta-analyses of HIV burden among transgender individuals covering literature from 2000 until 2019.
Previous systematic reviews and meta-analyses
Since 2008, a series of systematic reviews and meta-analyses have been published [1, 4, 5, 11, 15–17]. The first, by Herbst and colleagues, [15] investigated HIV prevalence among trans individuals in the United States, covering literature from 1988 until early 2007, and included laboratory-confirmed and self-reported prevalence. Pooled HIV prevalence based upon studies reporting laboratory-confirmed HIV status was, for trans women, 27.7%. HIV prevalence among trans women based upon self-reported HIV status was 11.8%. Among trans men, only one study reported laboratory confirmed prevalence (2%) and self-reported prevalence rates ranged from 0% to 3%. The second systematic review and meta-analysis by Operario et al. [16] set out to assess whether transgender female sex workers (FSW) experienced higher HIV infection rates than cis-gender sex workers and transgender women who do not engage in sex work, using both laboratory-confirmed and self-reported HIV prevalence rates published between 1998 and 2006. HIV prevalence was 27.3% in transgender FSW and 14.7% in trans women who did not engage in sex work. Operario et al.’s meta-analysis further showed that transgender FSW are at significantly higher risk for HIV than cis-gender sex workers and trans women who do not engage in sex work [16]. In 2013, Baral and colleagues [4] published a systematic review and meta-analysis of HIV prevalence among transgender women, covering literature from 2000 to November 2011 and using only laboratory-confirmed HIV prevalence rates. Pooled prevalence was 19.1% and the meta-analytical findings showed that, compared to all adults of reproductive age, the odds ratio for HIV infection in trans women was 49 across the 15 countries included, thus demonstrating that transgender women carry a high burden of HIV [4]. Poteat and colleagues [5] followed up on Baral et al.’s work with a systematic review, but not a meta-analysis, of HIV prevalence literature published between 2012 and 2015, looking now at both trans feminine and trans masculine populations. Prevalence rates varied substantially based on locale but Poteat et al. [5] concluded, in line with the previous reviews, that HIV prevalence was high in trans feminine populations. They also concluded that data on HIV among trans masculine individuals is still very limited. Almost simultaneously, Reisner and Murchison [1] published a global research synthesis of HIV and STI risks in adult trans men, but not trans women, using 25 studies. They found HIV prevalence rates for trans men ranging from 0% to 4.3% for laboratory-confirmed HIV status and 0% to 10% for self-reported HIV, suggesting that trans masculine individuals may also be more vulnerable to HIV than cis-gender adults. Additionally, in 2017, MacCarthy and colleagues [11] published a global systematic review of HIV and sexually transmitted infections among transgender individuals. They reported HIV prevalence rates ranging from 0% to 17.6% for self-reported HIV status and 0.6% to 34.1% for laboratory-confirmed HIV status. However, given their focus on HIV and STI co-infection, the HIV prevalence rates reported in that review were derived only from studies that also reported STI prevalence rates. The reported prevalence rates were thus based on a mere 6 studies for self-reported HIV status and 13 studies for laboratory-confirmed HIV status. Recently, Becasen et al. [17] published a systematic review and meta-analysis of HIV prevalence among transgender individuals in the United States only using literature published in the United States between 2006 and May 2017. They established that laboratory-confirmed HIV prevalence was 14.1% for trans women and 3.2% for trans men; self-reported prevalence was 16.1% and 1.2% for trans women and trans men, respectively.
Current concerns
Overall, the various systematic reviews and meta-analyses demonstrate that transgender individuals, particularly trans feminine individuals, are disproportionately burdened with HIV but none of the more recent systematic reviews have comprehensively updated Baral et al.’s worldwide systematic review and meta-analysis with both transfeminine and transmasculine individuals. Furthermore, from a methodological perspective, more fine-grained analyses (e.g. by country and year of data collection) are being called for, rather than only pooled analyses by country or region, as has been the methodological approach in previous meta-analyses. Additionally, critique about reported prevalence rates has been levied, with the claim that many studies have relied on convenience samples of, often, transgender women who engage in sex work, which may inflate prevalence rates [18, 19]. Also, previous meta-analyses have not differentiated between various sampling strategies and this may impact meta-analytical findings. Further, there have been substantial and fundamental changes in HIV prevention in recent years. One is the emergence of pre-exposure prophylaxis (PrEP) as a powerful tool for HIV prevention for at risk groups like transgender individuals [5, 8, 20–23]. With these considerations in mind, we feel it is time to revisit worldwide HIV prevalence and burden among transgender individuals. We therefore systematically reviewed literature published between 2000 and 2019 on HIV prevalence among transgender individuals and then conducted a meta-analysis 1) to establish prevalence rates for both trans feminine and trans masculine individuals; and 2) to compare the burden of HIV infection among transgender individuals to individuals over 15 years of age in the countries and regions from which samples were derived, taking year of data collection into account. We then explored the possible impact of sampling methods and of PrEP on prevalence rates and the burden of HIV infection.
Methods
Search strategies and eligibility
We searched, in November 2017 and again in January 2019, PsycINFO, PubMed, Web of Science, and Google Scholar®, for studies in all languages published between January 1st, 2000 and January 28th, 2019. We selected this timeframe in order to gain a complete, comprehensive, and nuanced understanding of worldwide prevalence over and burden of HIV among transgender individuals. We also reviewed the studies included in Baral et al. [4] and in Poteat et al. [5] to ensure that they were covered in our analysis as well. We explicitly overlapped the timeframe in our meta-analysis with those of previous meta-analyses in order to generate comprehensive and robust meta-analytical findings. It also allowed us to explore the impact of applying more refined methodology (standardized vs. pooled prevalence rates) in the meta-analysis, and compare findings delivered by the different meta-analytical approaches. Articles and citations were downloaded and managed in the reference software Mendeley®.
We searched for articles on (the treatment of) HIV and transgender individuals using the following search terms: HIV OR AIDS OR “PrEP” OR “Pre-Exposure Prophylaxis” OR “TasP” OR “treatment as prevention” AND *transgender* OR “MTF” or “male to female transgender” OR “FTM” OR “female to male transgender” OR *transsexual* OR “travesty” OR “cross dresser” OR “koti” OR “hijra” OR “mahuvahine” OR “mahu” OR “waria” OR “katoey” OR “bantut” OR “nadleehi” OR “berdache” OR “xanith”. These terms are in line with the terms previously used by Baral et al. [4].
Studies of any research design published in peer-reviewed journals that reported laboratory- confirmed prevalence of HIV among transgender individuals were included. When prevalence rates were pooled across trans feminine and trans masculine individuals or when prevalence was pooled across trans feminine individuals and men who have sex with men (MSM), we contacted the authors and requested separate prevalence rates for the populations included.
Study selection and data extraction
Titles and abstracts were screened by two independent reviewers and articles that clearly did not include HIV prevalence data were excluded, as were duplicates. All articles that met the inclusion criteria and articles that needed further review to ascertain whether they met the criteria were subsequently downloaded. When one reviewer deemed the title and/or abstract potentially relevant and the other did not, the full-text for that article was nonetheless downloaded. Subsequently, the full texts were reviewed. When studies reported duplicate data, the study with the smallest sample size was excluded. If sample sizes were identical, the later publication was excluded. Any conflicts over study inclusion were resolved by project leads (KJ and SS) in conjunction with the researchers running the meta-analysis (MvD and HW). The PRISMA reporting checklist was used to guide the reporting of this study. No protocol was registered for this review.
Data were extracted by two trained coders using a standardized extraction form that included details about sample size, sampling method, sample description, recruitment location, time period of study, age range, transgender type (trans masculine/trans feminine/both), HIV measure (self-reported/laboratory testing), and HIV prevalence or incidence.
Methodological quality assessment
Given the lack of consensus on fitting quality assessment tools for epidemiological studies, [24] we developed criteria specifically for this systematic review and meta-analysis. In doing so, we used and adapted appropriate criteria from the JBI Critical Appraisal Checklist for Studies Reporting Prevalence Data [25]. Studies were deemed of sufficient quality if: 1) biological testing (rather than self-reported HIV status) was used to establish HIV diagnoses, as was done in Baral et al. [4]; 2) study participants were described in sufficient detail, meaning that prevalence was reported, or subsequently obtained directly from the authors, specifically for trans feminine and/or trans masculine individuals (rather than transgender individuals as a whole group); 3) if the study setting/location was sufficiently detailed; 4) if the data collection timeframe was reported; 5) if prevalence or frequency of HIV diagnosis within the total sample were reported; and 6) if sample size was at least 40 for trans feminine individuals. We did not apply a minimum sample size for studies reporting prevalence among trans masculine individuals as the majority of studies had small sample sizes, and a minimum sample size would have led to the exclusion of most studies reporting HIV prevalence among trans masculine individuals. Additionally, we did not exclude studies based on sampling method as investigating the impact of sampling methods was one of the objectives of this meta-analysis.
Data analyses
First, we used analogous methodology to prior meta-analyses [4, 26, 27]. We grouped studies by country, weighted by sample size. We calculated pooled HIV prevalence and 95% confidence intervals (CIs) per country. We did this separately for trans feminine and trans masculine samples. In line with previous meta-analyses, we then calculated odds ratios per country by dividing the HIV prevalence among transgender individuals (numerator) by the HIV prevalence rate among individuals over 15 years of age in the general population in the country from which the sample was derived (denominator), as reported by the 2017 UNAIDS reports (where prevalence estimates for adults are from 15 years of age onward) [28] and estimations of adult population size from the US Census Bureau International Division [29]. These results are reported in S1 Appendix.
Then, to achieve a more refined methodological analysis, we standardized rather than pooled prevalence rates, and ran the meta-analysis again, this time matching country-level prevalence rates to year(s) of data collection for the included studies. When data were collected over multiple years in the original studies, the median year of the year-span was chosen for the country by year analysis. If HIV prevalence in the sample was 0, we calculated confidence intervals using the Wilson interval [30]. Then, we grouped countries by geographic region (Africa, Latin America, Asia, and Global North) and calculated, per geographic region, the standardized HIV prevalence among trans feminine individuals as well as odds ratios based on weights from each country-year.
Subsequently, given recent discussions about the impact of sampling methods on findings pertaining to HIV prevalence among trans feminine individuals, [18] we grouped studies by sampling method, and calculated standardized HIV prevalence by sampling method. We delineated ten sampling methods, namely cluster sampling, convenience sampling, purposive sampling, respondent driven sampling, snowball sampling, sampling from database health plan, as well as sampling via STI clinic, via hospital, via NGO, and via surveillance. Overlap in categories may exist as some studies used multiple sampling methods. In such cases, we categorized the study under its primary sampling method.
Lastly, we explored possible effects of the introduction of PrEP on HIV prevalence among trans feminine individuals. We focused on US studies only as PrEP has been available in the US since 2012, which is longer than in any other country. We conducted subgroup analyses, with data being collected either prior to the introduction of PrEP (1997–2011), or after the introduction of PrEP (2012–2017).
The meta-analysis was conducted with the statistical software R [31] using the metafor package [32]. We used a random-effects model and the DerSimonian-Laird method to estimate the model. The DerSimonian-Laird Q test and I2 values were used to assess heterogeneity, with low, moderate, and high heterogeneity corresponding to I2 values of 25%, 50%, and 75%.[33] We investigated publication bias by inspecting funnel plots [34].
Results
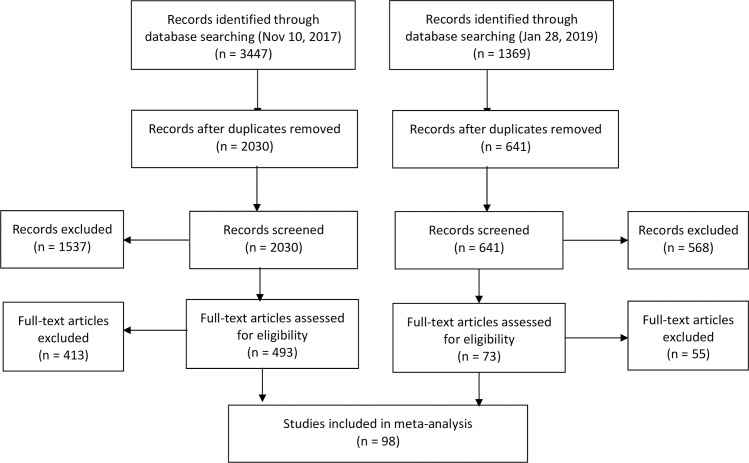
The study selection process is presented in Fig 1. We included 98 studies from a total of 34 countries, of which 78 studies described HIV prevalence in trans feminine individuals, 4 described prevalence in trans masculine individuals, and 16 described both. In total, we included 48,604 trans feminine individuals from 34 countries and 6460 trans masculine individuals from 5 countries. The included studies and relevant characteristics of those studies are reflected in Table 1.
Fig 1. PRISMA flow chart describing the study selection process.
Table 1. Studies included in review and meta-analysis.
| Authors | Year of publication | Year of data collection | Transgender sample | HIV prevalence (%) | HIV frequency (n) | Sample size | Country | Geographic region | Sampling method |
|---|---|---|---|---|---|---|---|---|---|
| Aguayo, Munoz, & Aguilar [35] | 2013 | 2011 | TF | 27.00% | 64 | 237 | Paraguay | Latin America | Cluster sampling |
| Akhtar, Badshah, Akhtar, et al. [36] | 2012 | 2009–2010 | TF (hijras) | 21.60% | 66 | 306 | Pakistan | Asia | Respondent driven sampling |
| Altaf [37] | 2009 | 2006–2007 | TF (hijras) | 4.70% | 38 | 810 | Pakistan | Asia | Surveillance |
| Altaf, Zahidie, & Agha [38] | 2012 | 2008 | TF (hijras) | 6.40% | 75 | 1181 | Pakistan | Asia | Surveillance |
| Baqi, Shah, Baig et al. [39] | 2006 | 1998 | TF (hijras) | 0.00% | 0 | 208 | Pakistan | Asia | Respondent driven sampling |
| Barrington, Weijnert, & Guardado et al. [40] | 2012 | 2008 | TF | 19.00% | 13 | 67 | El Salvador | Latin America | Respondent driven sampling |
| Bastos, Bastos, Coutinho et al. [41] | 2018 | 2016–2017 | TF | 29.62% | 843 | 2846 | Brazil | Latin America | Respondent driven sampling |
| Bellhouse, Walker, Fairley et al. [42] | 2016 | 2011–2014 | TM | 3.57% | 1 | 28 | Australia | Global North | STI clinic visit |
| TF | 10.39% | 8 | 77 | ||||||
| Brahmam, Kodavallaa, Rajkumar et al. [43] | 2008 | 2006–2007 | TF (hijras) | 18.10% | 104 | 575 | India | Asia | Cluster sampling |
| Carballo-Dieguez, Balan, Dolezal et al. [44] | 2012 | 2005–2006 | TF | 13.00% | 12 | 84 | Brazil | Latin America | Respondent driven sampling |
| Castel, Magnus, Peterson et al. [45] | 2012 | 2006 | TF & TM | 10.59% | 9 | 85 | US | Global North | STI clinic visit |
| Castillo, Konda, Leon et al. [46] | 2015 | 2008–2009 | TF | 16.82% | 35 | 208 | Peru | Latin America | Snowball |
| Chariyalersak, Kosachunhanan, Saokhieo et al. [47] | 2011 | 2008–2009 | TF | 9.30% | 13 | 140 | Thailand | Asia | STI clinic visit |
| Chen, McFarland, Tompson et al. [48] | 2011 | 2009 | TM | 0.00% | 0 | 59 | US | Global North | STI clinic visit |
| Chhim, Ngin, Chhoun et al. [49] | 2017 | 2015–2016 | TF | 5.90% | 81 | 1375 | Cambodia | Asia | Respondent driven sampling |
| Clements-Noelle, Wilkenson, Kitano et al. [50] | 2001 | 1997 | TM | 2.00% | 2 | 123 | US | Global North | Respondent driven sampling |
| TF | 35.00% | 137 | 392 | ||||||
| Colby, Nguyen, Le et al. [51] | 2016 | 2015 | TF | 18.00% | 37 | 205 | Vietnam | Asia | Snowball |
| Costa, Fontanari, Jacinto et al. [52] | 2015 | 1998–2014 | TM | 25.00% | 0 | 51 | Brazil | Latin America | Hospital |
| TF | 25.00% | 71 | 284 | ||||||
| Dasarathan & Kalaivani [53] | 2017 | 2011–2014 | TF | 13.40% | 11 | 82 | India | Asia | STI clinic visit |
| Diez, Bleda, Varela et al. [54] | 2014 | 2000–2009 | TF | 24.50% | 129 | 529 | Spain | Global North | STI clinic visit |
| Dos Ramos Farias, Garcia, Reynaga et al. [55] | 2011 | 2006–2009 | TF | 34.10% | 93 | 273 | Argentina | Latin America | Respondent driven sampling |
| Fernandes, Zanini, Rezende et al. [56] | 2015 | 2011–2013 | TF | 24.34% | 37 | 152 | Brazil | Latin America | Cluster sampling |
| Fernandez-Balbuena, Belza, Urdaneta et al. [57] | 2015 | 2008–2012 | TF & TM | 45.54% | 46 | 101 | Spain | Global North | NGO |
| Fernandez-Lopez, Reyes-Uruena, Agusti et al. [58] | 2018 | 2014–2016 | TF | 8.83% | 40 | 453 | Spain | Global North | STI clinic visit |
| Grandi, Goihman, Ueda et al. [59] | 2000 | 1992–1998 | TF | 40.00% | 174 | 434 | Brazil | Latin America | Respondent driven sampling |
| Green, Hoenigl, Morris et al. [60] | 2015 | 2008–2014 | TM | 3.00% | 1 | 30 | US | Global North | STI clinic visit |
| TF | 2.00% | 3 | 151 | ||||||
| Grinsztejn, Jalil, Monteiro et al. [61] | 2017 | 2015–2016 | TF | 31.20%/ 24.20% | 141 | 345 | Brazil | Latin America | Respondent driven sampling |
| Guadamuz, Wimonsate, Varangrat et al. [62] | 2011 | 2005 | TF | 14.00% | 64 | 474 | Thailand | Asia | Convenience sampling |
| Gutierrez, Tajada, Alvarez et al. [63] | 2004 | 1998–2003 | TF | 23.00% | 14 | 60 | Spain | Global North | Convenience sampling |
| Guy, Mustikawati, Wijaksono et al. [64] | 2011 | 2006–2008 | TF & TM | 31.60% | 151 | 477 | Indonesia | Asia | STI clinic visit |
| Habarta, Wang, Mulatu et al. [65] | 2015 | 2009–2011 | TM | 0.51% | 12 | 2364 | US | Global North | STI clinic visit |
| TF | 2.70% | 355 | 13154 | ||||||
| Hadikusumo, Utsumi, Amin et al. [66] | 2016 | 2012 | TF | 16.00% | 16 | 100 | Indonesia | Asia | STI clinic visit |
| Hakim, Coy, Patnaik et al. [67] | 2018 | 2014–2015 | TF | 22.42% | 37 | 165 | Mali | Africa | Respondent driven sampling |
| Hawkes, Collumbien, Platt et al. [68] | 2009 | 2007 | TF (khusra) | 2.00% | 6 | 269 | Pakistan | Asia | Respondent driven sampling |
| Hiransuthikul, Pattanachaiwit, Teeratakulpisarn et al. [69] | 2018 | 2012–2013 | TF | 4.26% | 2 | 47 | Thailand | Asia | STI clinic visit |
| Januraga, Wulandari, Muliawan et al. [70] | 2013 | 2009–2010 | TF (waria) | 36.87% | 80 | 217 | Indonesia | Asia | Respondent driven sampling |
| Jin, Restar, Biello et al. [71] | 2019 | 2012–2015 | TF | 24.71% | 65 | 263 | US | Global North | Convenience sampling |
| Kaplan, McGowan, & Wagner [72] | 2016 | 2012 | TF | 10.00% | 4 | 40 | Lebanon | Asia | Respondent driven sampling |
| Kellogg, Clements-Nolle, Dilley et al. [73] | 2001 | 1997–2000 | TF | 15.00% | 37 | 238 | US | Global North | STI clinic visit |
| Keshinro, Crowell, Nowak et al. [74] | 2016 | 2013–2016 | TF | 71.43% | 75 | 105 | Nigeria | Africa | Respondent driven sampling |
| Khan, Rehan, Qayyum et al. [75] | 2008 | 2004 | TF (hijras) | 1.00% | 5 | 409 | Pakistan | Asia | Cluster sampling |
| Kojima, Park, Konda et al. [76] | 2017 | 2013–2014 | TF | 30.10% / 27.60% | 30 | 89 | Peru | Latin America | STI clinic visit |
| Leinung, Urizar, Patel et al. [77] | 2013 | prior 2003 | TM | 0.00% | 0 | 50 | US | Global North | Hospital |
| TF | 8.33% | 16 | 192 | ||||||
| Lipsitz, Segura, Castro et al. [78] | 2014 | 2007–2009 | TF | 30.00% | 64 | 214 | Peru | Latin America | STI clinic visit |
| Lobato, Koff, Schestatsky et al. [79] | 2008 | 1998–2005 | TM | 0.00% | 0 | 16 | Brazil | Latin America | Hospital |
| TF | 19.67% | 24 | 122 | ||||||
| Logie, Lacombe-Duncan, Wang et al. [80] | 2016 | 2015 | TF | 25.20% | 26 | 103 | Jamaica | Latin America | Respondent driven sampling |
| Long, Montano, Cabello et al. [81] | 2017 | 2013–2015 | TF | 19.68% | 61 | 310 | Peru | Latin America | STI clinic visit |
| Luzzati, Zatta, Pavan et al. [82] | 2016 | 2000–2014 | TM | 0.00% | 0 | 20 | Italy | Global North | Hospital |
| TF | 12.10% | 21 | 173 | ||||||
| Manieri, Castellano, Crespi et al. [83] | 2014 | 2005–2011 | TM | 0.00% | 0 | 27 | Italy | Global North | Hospital |
| TF | 5.36% | 3 | 56 | ||||||
| McFarland, Wilson, Raymond et al. [84] | 2017 | 2014 | TM | 0.00% | 0 | 122 | US | Global North | Convenience sampling |
| Mimiaga, Hughto, Biello et al. [85] | 2019 | 2012–2015 | TF | 20.60% | 48 | 233 | US | Global North | Convenience sampling |
| Murrill, Liu, Guilin et al. [86] | 2008 | 2004 | TF & TM | 13.00% | 9 | 92 | US | Global North | Convenience sampling |
| Nemoto, Bödeker, Iwamoto et al. [87] | 2014 | 2000–2001 | TF | 29.93% | 161 | 538 | US | Global North | Purposive sampling |
| Nguyen, Nguyen, Le et al. [88] | 2008 | 2004 | TF ("male transvestites" "bong lo") | 7.00% | 5 | 75 | Vietnam | Asia | Convenience sampling |
| Nuttbrock, Bockting, Rosenblum et al. [89] | 2013 | 2004–2007 | TF | 2.80% | 9 | 230 | US | Global North | Convenience sampling |
| Nuttbrock, Hwahng, Bockting et al. [90] | 2009 | earlier than 2009 | TF | 35.98% | 186 | 517 | US | Global North | Convenience sampling |
| Ongwandee, Lertpiriyasuwat, Khawcharoenporn et al. [91] | 2018 | 2015–2016 | TF | 900.00% | 39 | 435 | Thailand | Asia | STI clinic visit |
| Pando, Gomez-Carrillo, Vignoles et al. [92] | 2011 | 2006–2008 | TF | 34.00% | 38 | 112 | Argentina | Latin America | NGO |
| Patrascioiu, Lopez, Porta et al. [93] | 2013 | 2006–2010 | TM | 2.20% | 2 | 92 | Spain | Global North | Convenience sampling |
| TF | 12.60% | 18 | 142 | ||||||
| Peitzmeier, Reisner, Harigopal et al. [94] | 2014 | 2006–2012 | TM | 0.86% | 2 | 233 | US | Global North | Hospital |
| Pell, Prone, Vlahakis et al. [95] | 2011 | 2004 | TM | 0.00% | 0 | 17 | Australia | Global North | STI clinic visit |
| TF | 4.26% | 6 | 141 | ||||||
| Pisani, Girault, Gultom et al. [96] | 2004 | 2002 | TF (waria) | 22.00% | 53 | 241 | Indonesia | Asia | Cluster sampling |
| Pitasi, Oraka, Clark et al. [97] | 2019 | 2010–2013 | TM | 8.30% | 10 | 120 | US | Global North | STI clinic visit |
| TF | 14.20% | 72 | 506 | ||||||
| Pizzicato, Vagenas, Gonzales et al. [98] | 2017 | 2011 | TF | 14.59% | 104 | 713 | Peru | Latin America | Respondent driven sampling |
| Poteat, Ackerman, Diouf et al. [99] | 2017 | 2011–2016 | TF | 2.78% | 3 | 108 | Burkina Faso | Africa | Respondent driven sampling |
| TF | 25.50% | 76 | 298 | Côte d’Ivoire | |||||
| TF | 59.15% | 42 | 71 | Lesotho | |||||
| TF | 16.00% | 12 | 75 | Malawi | |||||
| TF | 37.19% | 74 | 199 | Senegal | |||||
| TF | 14.17% | 17 | 120 | Swaziland | |||||
| TF | 17.65% | 9 | 51 | Togo | |||||
| Poteat, German, & Flynn [100] | 2016 | 2004–2005 | TF | 43.00% | 21 | 49 | US | Global North | Surveillance |
| Prabawanti, Bollen, Palupy et al. [101] | 2011 | 2007 | TF (waria) | 24.40% | 183 | 748 | Indonesia | Asia | Cluster sampling |
| Quinn, Nash, Hunkeler et al. [102] | 2017 | 2006–2014 | TM | 0.31% | 9 | 2892 | US | Global North | Database health plan |
| TF | 5.35% | 186 | 3475 | ||||||
| Rana, Reza, Alam et al. [103] | 2016 | 2012 | TF (hijras) | 0.80% | 7 | 889 | Bangladesh | Asia | STI clinic visit |
| Raymond, Wilson, Packer et al. [104] | 2019 | 2010 | TF | 39.17% | 123 | 314 | US | Global North | Respondent driven sampling |
| 2013 | TF | 36.05% | 84 | 233 | |||||
| 2016 | TF | 38.68% | 123 | 318 | |||||
| Reback, Lombardi, Simon et al. [105] | 2005 | 1998–1999 | TF | 22.10% | 54 | 244 | US | Global North | STI clinic visit |
| Reisner, White, Mayer et al. [106] | 2014 | 2007 | TM | 4.35% | 1 | 23 | US | Global North | STI clinic visit |
| Reisner, Vetters, White et al. [107] | 2015 | 2001–2010 | TF | 7.93% | 5 | 63 | US | Global North | STI clinic visit |
| TM | 2.40% | 2 | 82 | ||||||
| Rich, Scott, Johnston, et al. [108] | 2017 | 2012–2014 | TM | 0.00% | 0 | 11 | Canada | Global North | Respondent driven sampling |
| Rowe, Santos, McFarland et al. [109] | 2015 | 2012–2013 | TF | 4.00% | 13 | 292 | US | Global North | Snowball |
| Russi, Serra, Vinoles et al. [110] | 2003 | 1999 | TF ("male transvestites") | 21.50% | 49 | 200 | Uruguay | Latin America | Convenience sampling |
| Sahastrabuddhe, Gupta, Stuart et al. [111] | 2012 | 1993–2002 | TF (hijras) | 45.20% | 38 | 84 | India | Asia | STI clinic visit |
| Salas-Espinoza, Menchaca-Diaz, Patterson et al. [112] | 2017 | 2012 | TF | 22.00% | 22 | 100 | Mexico | Latin America | Cluster sampling |
| Saravanamurthy, Rajendran, Ramakrishnan et al. [113] | 2008 | 2007 | TF | 17.50% | 23 | 125 | India | Asia | Respondent driven sampling |
| Schulden, Song, Barros et al. [114] | 2008 | 2005–2006 | TM | 0.00% | 0 | 42 | US | Global North | Convenience sampling |
| TF | 12.00% | 67 | 559 | ||||||
| Seekaew, Pengnonyang, Jantarapakde et al. [115] | 2018 | 2015–2016 | TF | 8.80% | 69 | 786 | Thailand | Asia | Respondent driven sampling |
| Shan, Yu, Yang et al. [116] | 2018 | 2016 | TF | 7.60% | 38 | 498 | China | Asia | Snowball |
| Shaw, Lorway, Bhattacharjee et al. [117] | 2016 | 2011 | TF (kothi & hijras) | 15.30% | 27 | 176 | India | Asia | Cluster sampling |
| Shaw, Emmanuel, Adrien et al. [118] | 2011 | 2005–2006 | TF (hijras) | 1.00% | 10 | 1162 | Pakistan | Asia | Cluster sampling |
| Sherman, Park, Galai et al. [119] | 2019 | 2016–2017 | TF | 40.30% | 25 | 62 | US | Global North | Convenience sampling |
| Shinde, Setia, Row-Kavi et al. [120] | 2009 | earlier than 2009 | TF | 41.00% | 21 | 51 | India | Asia | STI clinic visit |
| Silva-Santisteban, Raymond, Salazar et al. [121] | 2012 | 2009 | TF | 30.00% | 130 | 420 | Peru | Latin America | Respondent driven sampling |
| Sotelo & Claudia [122] | 2011 | 2009 | TF | 34.00% | 152 | 441 | Argentina | Latin America | Unknown |
| Stephens, Bernstein, Philip et al. [123] | 2011 | 2006–2009 | TM | 2.90% | 7 | 69 | US | Global North | STI clinic visit |
| TF | 11.21% | 25 | 223 | ||||||
| Subramanian, Ramakrishnan, Aridoss et al. [124] | 2013 | 2005–2009 | TF | 12.00% | 48 | 404 | India | Asia | Cluster sampling |
| Toibaro, Ebensrtejin, Parlante et al. [125] | 2009 | 2002–2006 | TF | 27.60% | 29 | 105 | Argentina | Latin America | STI clinic visit |
| Van Veen, Götz, van Leeuwen et al. [126] | 2010 | 2002–2005 | TF | 19.00% | 13 | 69 | Netherlands | Global North | Cluster sampling |
| Waheed, Satti, Arshad et al. [127] | 2017 | 2015–2016 | TF | 16.40% | 22 | 134 | Pakistan | Asia | Convenience sampling |
| Wasantioopapokakorn, Manopaiboon, Phoorisri et al. [128] | 2018 | 2011–2016 | TF | 11.85% | 82 | 692 | Thailand | Asia | Convenience sampling |
| Weissman, Ngak, Srean et al. [129] | 2016 | 2012 | TF | 4.00% | 37 | 891 | Cambodia | Asia | Respondent driven sampling |
| World Health Organization [130] | 2016 | 2015–2016 | TF | 4.00% | 11 | 299 | Philippines | Asia | Surveillance |
| Wickersham, Gibson, Bazazi et al. [131] | 2017 | 2014 | TF | 12.00% | 24 | 193 | Malaysia | Asia | Respondent driven sampling |
| Zaccarelli, Spizzichino, Venezia et al. [132] | 2004 | 1993–2003 | TF | 31.50% | 149 | 473 | Italy | Global North | STI clinic visit |
| Zea, Reisen, del Rio-Gonzalez et al. [133] | 2015 | 2011 | TF | 13.79% | 8 | 58 | Colombia | Latin America | Respondent driven sampling |
TF = trans feminine; TM = trans masculine.
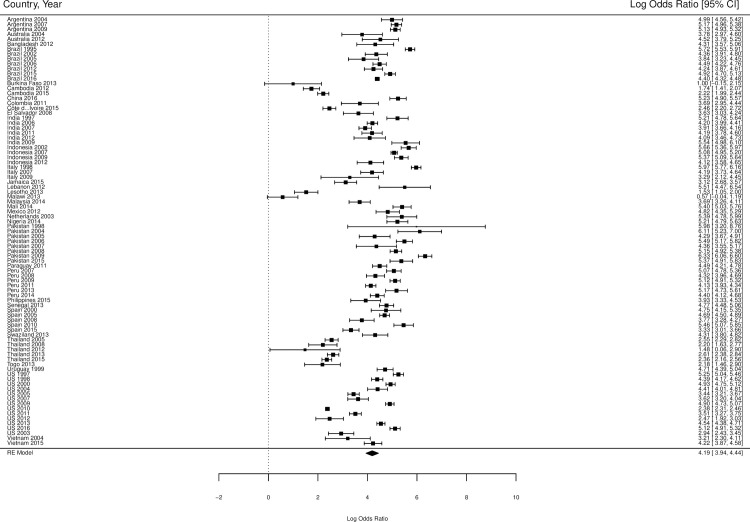
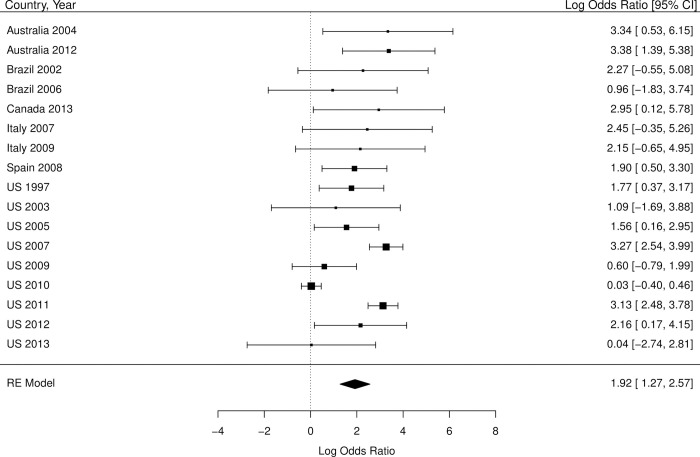
The overall standardized HIV prevalence over the course of the epidemic, based on weights from each country by year, was 19.9% (95% CI 14.7% - 25.1% Table 2) for trans feminine individuals and 2.56% (95% CI 0.0% - 5.9%; Table 3) for trans masculine individuals. The overall OR for HIV infection, compared with individuals over 15 years of age, was 66.0 (95% CI 51.4–84.8; Table 2 and Fig 2) for trans feminine individuals and 6.8 (95% CI 3.6–13.1, Table 3 and Fig 3) for trans masculine individuals. Tables 2 and 3 also show the overall standardized prevalence rates and overall odds ratios per country by year for trans feminine individuals and trans masculine individuals, respectively.
Table 2. Meta-analysis of HIV prevalence in trans feminine individuals compared to all adults (age 15+).
| Country | Year of data collection | Number of samples | Sample size | Frequency of HIV among TF in the samples | Prevalence (95% CI)* | Odds Ratio (95%CI) | HIV prevalence in adults (95% CI) |
|---|---|---|---|---|---|---|---|
| Argentina | 2004 | 1 | 105 | 29 | 27.6 (19.1–36.2) | 147.2 (96.0–225.9) | 0.258 (0.257–0.260) |
| Argentina | 2007 | 2 | 385 | 131 | 34 (29.3–38.8) | 176 (142.6–217.4) | 0.292 (0.290–0.294) |
| Argentina | 2009 | 1 | 441 | 152 | 34.5 (30–38.9) | 168.3 (138.3–204.8) | 0.312 (0.310–0.314) |
| Australia | 2004 | 1 | 141 | 6 | 4.3 (0.9–7.6) | 44 (19.4–99.7) | 0.101 (0.099–0.102) |
| Australia | 2012 | 1 | 77 | 8 | 10.4 (3.6–17.2) | 92.1 (44.3–191.5) | 0.126 (0.124–0.127) |
| Bangladesh | 2012 | 1 | 889 | 7 | 0.8 (0.2–1.4) | 74.7 (35.5–157.3) | 0.011 (0.010–0.011) |
| Brazil | 1995 | 1 | 434 | 174 | 40.1 (35.5–44.7) | 304.8 (251.6–369.3) | 0.219 (0.218–0.220) |
| Brazil | 2002 | 1 | 122 | 24 | 19.7 (12.6–26.7) | 78 (49.9–121.9) | 0.313 (0.312–0.314) |
| Brazil | 2005 | 1 | 84 | 12 | 14.3 (6.8–21.8) | 46.7 (25.3–86.0) | 0.356 (0.355–0.357) |
| Brazil | 2006 | 1 | 284 | 71 | 25.0 (20.0–30.0) | 89.3 (68.2–116.8) | 0.372 (0.371–0.373) |
| Brazil | 2012 | 1 | 152 | 37 | 24.3 (17.5–31.2) | 69.7 (48.1–100.9) | 0.460 (0.459–0.461) |
| Brazil | 2015 | 1 | 345 | 141 | 40.9 (35.7–46.1) | 136.4 (110.1–169.1) | 0.504 (0.503–0.505) |
| Brazil | 2016 | 1 | 2846 | 843 | 29.6 (27.9–31.3) | 81.1 (74.9–87.9) | 0.516 (0.515–0.517) |
| Burkina Faso | 2013 | 1 | 108 | 3 | 2.8 (-0.3–5.9) | 2.7 (0.9–8.5) | 1.043 (1.036–1.049) |
| Cambodia | 2012 | 1 | 891 | 37 | 4.2 (2.8–5.5) | 5.7 (4.1–7.9) | 0.756 (0.751–0.762) |
| Cambodia | 2015 | 1 | 1375 | 81 | 5.9 (4.6–7.1) | 9.2 (7.3–11.5) | 0.678 (0.673–0.683) |
| China | 2016 | 1 | 498 | 38 | 7.6 (5.3–10) | 187.7 (134.8–261.3) | 0.044 (0.044–0.044) |
| Colombia | 2011 | 1 | 58 | 8 | 13.8 (4.9–22.7) | 40.2 (19.1–84.8) | 0.397 (0.394–0.399) |
| Côte d’Ivoire | 2015 | 1 | 298 | 76 | 25.5 (20.6–30.5) | 11.7 (9.1–15.2) | 2.832 (2.823–2.841) |
| El Salvador | 2008 | 1 | 67 | 13 | 19.4 (9.9–28.9) | 37.9 (20.7–69.4) | 0.631 (0.623–0.639) |
| India | 1997 | 1 | 84 | 38 | 45.2 (34.6–55.9) | 183.8 (119.6–282.4) | 0.447 (0.447–0.448) |
| India | 2006 | 1 | 575 | 104 | 18.1 (14.9–21.2) | 66.7 (53.9–82.5) | 0.330 (0.330–0.330) |
| India | 2007 | 2 | 529 | 71 | 13.4 (10.5–16.3) | 49.8 (38.8–63.9) | 0.310 (0.310–0.311) |
| India | 2011 | 1 | 176 | 27 | 15.3 (10.0–20.7) | 65.7 (43.6–99.0) | 0.275 (0.275–0.275) |
| India | 2012 | 1 | 82 | 11 | 13.4 (6.0–20.8) | 59.9 (31.7–113.0) | 0.258 (0.258–0.258) |
| India | 2009 | 1 | 51 | 21 | 41.2 (27.7–54.7) | 255.3 (146.1–445.8) | 0.273 (0.273–0.274) |
| Indonesia | 2002 | 1 | 241 | 53 | 22 (16.8–27.2) | 288.5 (212.7–391.4) | 0.098 (0.097–0.098) |
| Indonesia | 2007 | 2 | 1225 | 334 | 27.3 (24.8–29.8) | 160.4 (141.5–181.9) | 0.233 (0.232–0.234) |
| Indonesia | 2009 | 1 | 217 | 80 | 36.9 (30.4–43.3) | 214.1 (162.5–282.1) | 0.272 (0.271–0.273) |
| Indonesia | 2012 | 1 | 100 | 16 | 16.0 (8.8–23.2) | 61.5 (36.0–105.0) | 0.309 (0.308–0.310) |
| Italy | 1998 | 1 | 473 | 149 | 31.5 (27.3–35.7) | 390.4 (321.5–474.1) | 0.118 (0.117–0.119) |
| Italy | 2007 | 1 | 173 | 21 | 12.1 (7.3–17) | 65.7 (41.7–103.8) | 0.210 (0.208–0.211) |
| Italy | 2009 | 1 | 56 | 3 | 5.4 (-0.5–11.3) | 26.8 (8.4–85.6) | 0.211 (0.210–0.212) |
| Jamaica | 2015 | 1 | 103 | 26 | 25.2 (16.9–33.6) | 22.7 (14.5–35.4) | 1.468 (1.451–1.484) |
| Lebanon | 2012 | 1 | 40 | 4 | 10.0 (0.7–19.3) | 246.1 (87.5–692.4) | 0.045 (0.043–0.047) |
| Lesotho | 2013 | 1 | 71 | 42 | 59.2 (47.7–70.6) | 4.6 (2.9–7.4) | 23.950 (23.876–24.023) |
| Malawi | 2013 | 1 | 75 | 12 | 16.0 (7.7–24.3) | 1.8 (1.0–3.3) | 9.683 (9.664–9.703) |
| Malaysia | 2014 | 1 | 193 | 24 | 12.4 (7.8–17.1) | 39.9 (26.0–61.1) | 0.355 (0.352–0.357) |
| Mali | 2014 | 1 | 165 | 37 | 22.4 (16.1–28.8) | 220.9 (153.1–318.6) | 0.131 (0.128–0.133) |
| Mexico | 2012 | 1 | 100 | 22 | 22 (13.9–30.1) | 123.9 (77.2–198.9) | 0.227 (0.226–0.228) |
| Netherlands | 2003 | 1 | 69 | 13 | 18.8 (9.6–28.1) | 218.8 (119.7–400.2) | 0.106 (0.104–0.108) |
| Nigeria | 2014 | 1 | 105 | 75 | 71.4 (62.8–80.1) | 183 (119.8–279.4) | 1.348 (1.346–1.350) |
| Pakistan | 1998 | 1 | 208 | 0 | 0 (0.0–0.0) | 395.9 (24.6–6359.6) | 0.001 (0.001–0.001) |
| Pakistan | 2004 | 1 | 409 | 5 | 1.2 (0.2–2.3) | 451.5 (186.8–1091.6) | 0.003 (0.003–0.003) |
| Pakistan | 2005 | 1 | 1162 | 10 | 0.9 (0.3–1.4) | 73.0 (39.2–136.1) | 0.012 (0.012–0.012) |
| Pakistan | 2006 | 1 | 810 | 38 | 4.7 (3.2–6.1) | 243.0 (175.4–336.6) | 0.020 (0.020–0.021) |
| Pakistan | 2007 | 1 | 269 | 6 | 2.2 (0.5–4) | 78.4 (34.9–176.1) | 0.029 (0.029–0.029) |
| Pakistan | 2008 | 1 | 1181 | 75 | 6.4 (5–7.7) | 172.4 (136.4–217.9) | 0.039 (0.039–0.040) |
| Pakistan | 2009 | 1 | 306 | 66 | 21.6 (17–26.2) | 560.5 (426.8–736.1) | 0.049 (0.049–0.049) |
| Pakistan | 2015 | 1 | 134 | 22 | 16.4 (10.1–22.7) | 214.8 (136.0–339.2) | 0.091 (0.091–0.092) |
| Paraguay | 2011 | 1 | 237 | 64 | 27 (21.4–32.7) | 89.5 (67.2–119.3) | 0.411 (0.406–0.417) |
| Peru | 2007 | 1 | 214 | 64 | 29.9 (23.8–36) | 158.9 (118.5–212.9) | 0.268 (0.266–0.270) |
| Peru | 2008 | 1 | 208 | 35 | 16.8 (11.7–21.9) | 75.3 (52.4–108.3) | 0.268 (0.266–0.270) |
| Peru | 2009 | 1 | 420 | 130 | 31 (26.5–35.4) | 166.9 (135.7–205.3) | 0.268 (0.266–0.270) |
| Peru | 2011 | 1 | 713 | 104 | 14.6 (12–17.2) | 62.5 (50.7–76.9) | 0.273 (0.270–0.275) |
| Peru | 2013 | 1 | 89 | 30 | 33.7 (23.9–43.5) | 176.6 (113.8–274.1) | 0.287 (0.285–0.289) |
| Peru | 2014 | 1 | 310 | 61 | 19.7 (15.3–24.1) | 81.1 (61.3–107.4) | 0.301 (0.299–0.303) |
| Philippines | 2015 | 1 | 299 | 11 | 3.7 (1.5–5.8) | 50.9 (27.9–92.9) | 0.075 (0.074–0.076) |
| Senegal | 2013 | 1 | 199 | 74 | 37.2 (30.5–43.9) | 118.1 (88.6–157.4) | 0.499 (0.494–0.504) |
| Spain | 2000 | 1 | 60 | 14 | 23.3 (12.6–34) | 115.6 (63.5–210.2) | 0.263 (0.261–0.264) |
| Spain | 2005 | 1 | 529 | 129 | 24.4 (20.7–28) | 109.3 (89.6–133.3) | 0.294 (0.293–0.296) |
| Spain | 2008 | 1 | 142 | 18 | 12.7 (7.2–18.1) | 43.6 (26.6–71.5) | 0.332 (0.330–0.334) |
| Spain | 2010 | 1 | 101 | 46 | 45.5 (35.8–55.3) | 235.3 (159.1–348.1) | 0.354 (0.352–0.356) |
| Spain | 2015 | 1 | 453 | 40 | 8.8 (6.2–11.4) | 28.1 (20.3–38.8) | 0.344 (0.342–0.346) |
| Swaziland | 2013 | 1 | 120 | 17 | 14.2 (7.9–20.4) | 74.5 (44.6–124.4) | 0.221 (0.218–0.225) |
| Thailand | 2005 | 1 | 474 | 64 | 13.5 (10.4–16.6) | 12.8 (9.9–16.7) | 1.202 (1.199–1.205) |
| Thailand | 2008 | 1 | 140 | 13 | 9.3 (4.5–14.1) | 9 (5.1–16) | 1.121 (1.119–1.124) |
| Thailand | 2012 | 1 | 47 | 2 | 4.3 (-1.5–10) | 4.4 (1.1–18.1) | 1.002 (1.000–1.005) |
| Thailand | 2013 | 1 | 692 | 82 | 11.8 (9.4–14.3) | 13.7 (10.8–17.2) | 0.975 (0.973–0.978) |
| Thailand | 2015 | 2 | 1221 | 108 | 8.8 (7.3–10.4) | 10.6 (8.7–12.9) | 0.908 (0.906–0.911) |
| Togo | 2013 | 1 | 51 | 9 | 17.6 (7.2–28.1) | 8.9 (4.3–18.2) | 2.359 (2.345–2.374) |
| Uruguay | 1999 | 1 | 200 | 49 | 24.5 (18.5–30.5) | 111.3 (80.6–153.8) | 0.291 (0.284–0.297) |
| US | 1997 | 1 | 392 | 137 | 34.9 (30.2–39.7) | 190.7 (154.9–234.7) | 0.281 (0.280–0.282) |
| US | 1998 | 2 | 482 | 91 | 18.9 (15.4–22.4) | 81.0 (64.5–101.7) | 0.287 (0.286–0.287) |
| US | 2000 | 1 | 538 | 161 | 29.9 (26.1–33.8) | 138.9 (115.5–167.1) | 0.306 (0.306–0.307) |
| US | 2004 | 2 | 141 | 30 | 21.3 (14.5–28) | 82.3 (55.0–123.2) | 0.327 (0.327–0.328) |
| US | 2005 | 3 | 852 | 81 | 9.5 (7.5–11.5) | 31.1 (24.8–39.2) | 0.336 (0.335–0.337) |
| US | 2007 | 1 | 223 | 25 | 11.2 (7.1–15.4) | 37.4 (24.7–56.7) | 0.337 (0.336–0.337) |
| US | 2009 | 2 | 602 | 195 | 32.4 (28.7–36.1) | 134.8 (113.7–159.9) | 0.354 (0.353–0.355) |
| US | 2010 | 3 | 16943 | 664 | 3.9 (3.6–4.2) | 10.8 (10–11.7) | 0.375 (0.374–0.376) |
| US | 2011 | 2 | 657 | 75 | 11.4 (9–13.8) | 33.5 (26.3–42.6) | 0.383 (0.383–0.384) |
| US | 2012 | 1 | 292 | 13 | 4.5 (2.1–6.8) | 11.8 (6.8–20.7) | 0.392 (0.391–0.392) |
| US | 2013 | 3 | 729 | 197 | 27 (23.8–30.2) | 94.1 (79.9–110.8) | 0.392 (0.391–0.393) |
| US | 2016 | 2 | 380 | 148 | 38.9 (34–43.9) | 166.6 (135.5–204.7) | 0.382 (0.381–0.382) |
| US | 2003 | 1 | 192 | 16 | 8.3 (4.4–12.2) | 18.9 (11.3–31.5) | 0.479 (0.478–0.480) |
| Vietnam | 2004 | 1 | 75 | 5 | 6.7 (1–12.3) | 24.7 (10–61.1) | 0.289 (0.287–0.290) |
| Vietnam | 2015 | 1 | 205 | 37 | 18 (12.8–23.3) | 68.4 (47.9–97.6) | 0.321 (0.320–0.322) |
| Overall | - | - | - | - | 19.9 (14.7–25.1)* | 66.0 (51.4–84.8) | - |
Note. Heterogeneity: Q = 6327.25, df = 86, p < .0001, I2 = 98.63%.
*Overall prevalence was calculated by direct standardization based on country-year weights used in meta-analysis.
Table 3. Meta-analysis of HIV prevalence in trans masculine individuals compared to all adults (age 15+).
| Country | Year of data collection | Number of samples | Sample size | Frequency of HIV among TM in the samples | Prevalence (95% CI)* | Odds Ratio (95% CI) | HIV prevalence in adults (95% CI) |
|---|---|---|---|---|---|---|---|
| Australia | 2004 | 1 | 17 | 0 | 0.0 (0.0–0.2) | 28.3 (1.7–470.5) | 0.101 (0.099–0.102) |
| Australia | 2012 | 1 | 28 | 1 | 3.6 (-3.3–10.4) | 29.4 (4–216.5) | 0.126 (0.124–0.127) |
| Brazil | 2002 | 1 | 16 | 0 | 0.0 (0.0–0.2) | 9.7 (0.6–160.9) | 0.313 (0.312–0.314) |
| Brazil | 2006 | 1 | 51 | 0 | 0.0 (0.0–0.1) | 2.6 (0.2–42.1) | 0.372 (0.371–0.373) |
| Canada | 2013 | 1 | 11 | 0 | 0.0 (0.0–0.3) | 19.1 (1.1–323.8) | 0.227 (0.226–0.229) |
| Italy | 2007 | 1 | 20 | 0 | 0.0 (0.0–0.2) | 11.6 (0.7–191.9) | 0.210 (0.208–0.211) |
| Italy | 2009 | 1 | 27 | 0 | 0.0 (0.0–0.1) | 8.6 (0.5–140.9) | 0.211 (0.210–0.212) |
| Spain | 2008 | 1 | 92 | 2 | 2.2 (-0.8–5.2) | 6.7 (1.6–27.1) | 0.332 (0.330–0.334) |
| US | 1997 | 1 | 123 | 2 | 1.6 (-0.6–3.9) | 5.9 (1.5–23.7) | 0.281 (0.280–0.282) |
| US | 2003 | 1 | 50 | 0 | 0.0 (0.0–0.1) | 3.0 (0.2–48.3) | 0.331 (0.330–0.332) |
| US | 2005 | 2 | 124 | 2 | 1.6 (-0.6–3.8) | 4.7 (1.2–19.2) | 0.345 (0.344–0.345) |
| US | 2007 | 2 | 92 | 8 | 8.7 (2.9–14.5) | 26.2 (12.7–54.2) | 0.362 (0.361–0.362) |
| US | 2009 | 2 | 292 | 2 | 0.7 (-0.3–1.6) | 1.8 (0.5–7.3) | 0.379 (0.378–0.379) |
| US | 2010 | 2 | 5256 | 21 | 0.4 (0.2–0.6) | 1.0 (0.7–1.6) | 0.387 (0.386–0.388) |
| US | 2011 | 1 | 120 | 10 | 8.3 (3.4–13.3) | 22.9 (12–43.8) | 0.395 (0.395–0.396) |
| US | 2012 | 1 | 30 | 1 | 3.3 (-3.1–9.8) | 8.7 (1.2–63.7) | 0.396 (0.395–0.396) |
| US | 2013 | 1 | 122 | 0 | 0.0 (0.0–2.8) | 1.0 (0.1–16.7) | 0.392 (0.391–0.393) |
| Overall | - | - | - | - | 2.56 (0.0–5.9)* | 6.8 (3.6–13.1) | - |
Note. Heterogeneity: Q = 13.06, df = 16, p<0.0001, I2 = 70.62%.
*Overall prevalence was calculated by direct standardization based on country-year weights used in meta-analysis.
Fig 2. Forest plot of HIV prevalence in trans feminine individuals compared to all adults (age 15+).
The scale on the x-axis is log odds ratio. The percentages indicate the weight of each country by year within the meta-analysis. The numbers in the right column are the log odds ratios including their confidence intervals. We converted these log odds ratios into odds ratios, as described in Table 2.
Fig 3. Forest plot of HIV prevalence in trans masculine individuals compared to all adults (age 15+).
The scale on the x-axis is log odds ratio. The percentages indicate the weight of each country by year within the meta-analysis. The numbers in the right column are the log odds ratios including their confidence intervals. We converted these log odds ratios into odds ratios, as described in Table 3.
Standardized prevalence rates and overall odd ratios (based on weights from each country by year) according to geographic region are presented in Table 4. In sub-Saharan Africa (n = 1192), standardized HIV prevalence among trans feminine individuals was 29.9% (95% CI 22.5% - 37.3%) and the overall OR for HIV infection, compared to individuals over 15 years of age in the countries from which we had prevalence data for trans feminine individuals, matched to year of data collection, was 21.5 (95% CI 6.3–73.7). In Latin America (n = 7917), standardized prevalence was 25.9% (95% CI 20.0% - 31.8%) and the overall OR for HIV infection, compared to individuals over 15 years of age, was 95.6 (95% CI 73.7–122.7). In Asia (n = 14,798), the standardized HIV prevalence was 13.5% (95% CI 2.3% - 17.7%) and the overall OR was 68.0 (95% CI 42.9–107.8). Lastly, in the Global North, thus in Australia, Europe, and North America (n = 24,697), the standardized HIV prevalence was 17.1% (95% CI 13.1% - 21.1%) and the overall OR for HIV infection was 48.4 (95% CI 28.2–83.9).
Table 4. HIV prevalence and odds ratios for trans feminine individuals compared to all adults (age 15+), separated by geographic region.
| Region | Number of countries | Number of Samples | Sample size | Prevalence (95% CI) * | Odds Ratio (95% CI) * | HIV prevalence in adults (95% CI)* |
|---|---|---|---|---|---|---|
| Africa | 9 | 9 | 1192 | 29.9 (22.5–37.3) | 21.5 (6.3–73.7) | 4.69 (4.67–4.71) |
| Asia | 11 | 35 | 14798 | 13.5 (2.3–17.7) | 68.0 (42.9–107.8) | 0.344 (0.343–0.345) |
| Global North | 5 | 35 | 24697 | 17.1 (13.1–21.1) | 48.4 (28.2–83.9) | 0.297 (0.296–0.298) |
| Latin America | 9 | 23 | 7917 | 25.9 (20.0–31.8) | 95.6 (73.7–122.7) | 0.391 (0.388–0.394) |
Note. The HIV prevalence in adults of the population (last column) is the weighted prevalence of the countries included in this meta-analysis, not overall prevalence in the region.
* Results were calculated by direct standardisation of country-year sample size instead of pooling.
The standardized HIV prevalence by sampling method is reported in Table 5. The standardized HIV prevalence among transgender individuals when respondent driven sampling was employed (33 studies) was 23.3% (95% CI 18.0% - 28.4%). When prevalence rates were ascertained via STI clinic visits (26 studies), standardized prevalence was 17.4% (95% CI 12.2% - 22.7%). When convenience sampling was employed (14 studies), standardized prevalence was 19.7% (95% CI 14.8% - 24.5%) and when cluster sampling was employed (11 studies), the standardized prevalence was 19.6% (95% CI 14.4% - 24.9%). The remaining sampling methods were relatively infrequently employed (i.e., employed in 5 or fewer studies).
Table 5. HIV prevalence in trans feminine individuals, separated by sampling method.
| Sampling method | Number of samples | Sample size | HIV prevalence (95% CI)* |
|---|---|---|---|
| Respondent driven sampling | 33 | 12202 | 23.3 (18.0–28.4) |
| STI clinic visit | 26 | 19360 | 17.4 (12.2–22.7) |
| Convenience sampling | 14 | 3733 | 19.7 (14.8–24.5) |
| Cluster sampling | 11 | 4273 | 19.6 (14.4–24.9) |
| Hospital | 5 | 827 | 15.0 (9.8–20.4) |
| Snowball | 4 | 1203 | 11.8 (8.0–15.6) |
| Surveillance | 4 | 2339 | 9.1 (6.1–12.0) |
| NGO | 2 | 213 | 37.8 (31.5–44.2) |
| Database health plan | 1 | 3475 | 5.4 (4.6–6.1) |
| Purposive sampling | 1 | 538 | 29.9 (26.1–33.8) |
Note. For one study, the sampling method was unknown and is not included in this table.
*: Results were calculated by direct standardisation of country-year sample size instead of pooling.
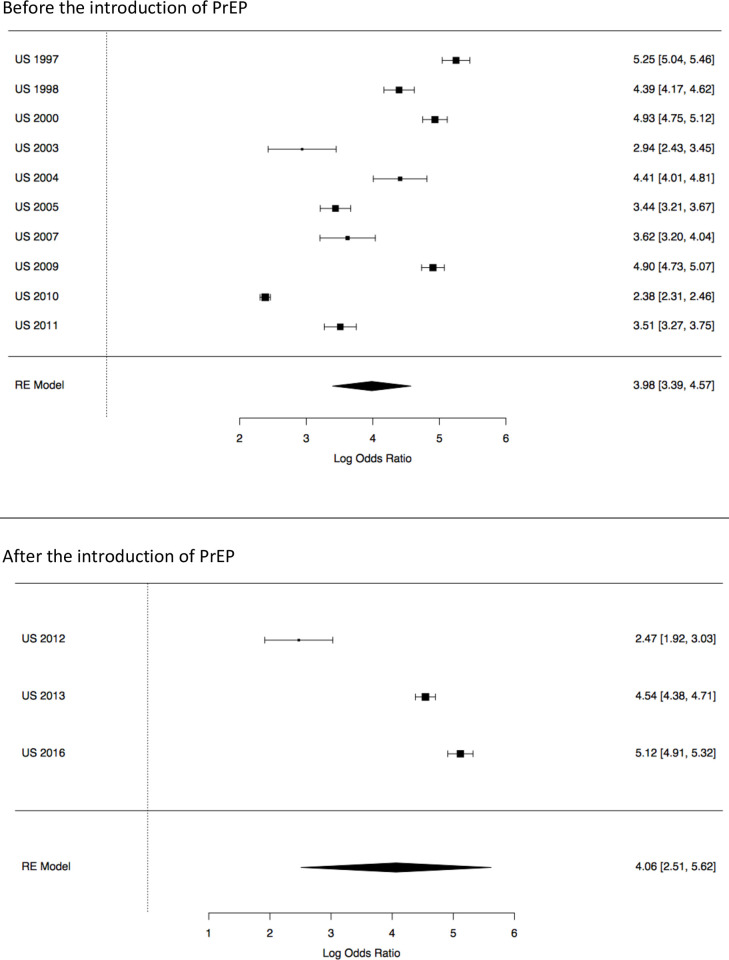
Next, we looked at the potential role of PrEP in reducing HIV prevalence among trans feminine individuals. Prior to the introduction of PrEP (1997–2011), the standardized HIV prevalence in US-based studies was 18.4% (95% CI 14.8% - 22.0%; Table 6) and the overall OR for HIV infection, compared to individuals over 15 years of age in the USA, was 53.5 (95% CI 29.7–96.5). After the introduction of PrEP (2012–2017), the standardized HIV prevalence in US-based studies was 23.7% (95% CI 20.2% - 27.2%) and the OR for HIV infection, compared to individuals over 15 years of age, was 58.0 (95% CI 12.3–275.9). The forest plot of this analysis is presented in Fig 4.
Table 6. HIV prevalence and odds ratios for trans feminine individuals compared to all adults (age 15+) in US-based studies, according to whether data was collected before or after the introduction of PrEP (2012).
| Number of studies | Sample size | Frequency of HIV among TF in the samples | Prevalence (95%CI)* | Odds Ratio (95%CI) | |
|---|---|---|---|---|---|
| Before PrEP | 18 | 21022 | 1475 | 18.4 (14.8–22.0) | 53.5 (29.7–96.5) |
| After PrEP | 6 | 1401 | 358 | 23.7 (20.2–27.2) | 58.0 (12.3–275.9) |
Note. *Overall prevalence was calculated by direct standardization based on country-year weights used in meta-analysis.
Fig 4. Forest plot of HIV prevalence in trans feminine individuals in the USA compared to all adults (age 15+) in the USA.
The 10 country-year including 18 studies above the line are studies where data were collected prior to the introduction of PrEP (2012). The 3 country-year including 6 studies below the line are studies where data were collected after the introduction of PrEP. The scale on the x-axis is log odds ratio. The percentages indicate the weight of each sample within the meta-analysis. The numbers in the right column are the log odds ratios including their confidence intervals.
Heterogeneity was high across the studies that included trans feminine individuals (Q = 6327.25, df = 86, p < .0001, I2 = 98.63%). This may be because the studies were conducted in different countries using different methodologies. Heterogeneity was moderate for the studies that included trans masculine individuals (Q = 102.06, df = 15, p<0.0001, I2 = 72.17%). The funnel plots showed an asymmetrical distribution of studies and may therefore indicate publication bias (S2 Appendix in Fig A2.1 and Fig A2.2).
Discussion
This systematic review and meta-analysis affirms that transgender individuals are disproportionately burdened by HIV, and that this is the case for not only trans feminine individuals, but also for trans masculine individuals. Using a larger pooled sample than ever compiled before, we ascertained that trans masculine individuals almost seven times more likely to have HIV, and trans feminine individuals are 66 times more likely to have HIV, than other individuals over 15 years of age. Additionally, based on data from 34 countries across major geographic regions, we found support for the contention that the disproportionate burden for HIV carried by transgender individuals is a worldwide phenomenon, and that some regions, such as Africa and Latin America, may be impacted more than others. Further, we established that sampling methods are likely to impact prevalence rates and that, to date, PrEP prevention effects on HIV prevalence cannot be established.
To our knowledge, no previous study has estimated the HIV burden carried by trans masculine individuals worldwide. Reisner and Murchinson [1] did conduct a research synthesis of HIV risks in trans masculine individuals where laboratory-confirmed prevalence ranged from 0% to 4.3% and Becasen and colleagues [17] established a laboratory-confirmed estimated prevalence rate of 3.2% but, in both studies, no odds ratios were calculated to ascertain the relative burden of HIV carried by trans masculine individuals. Our finding that trans masculine individuals are almost seven times more likely to have HIV than other individuals over 15 years of age indicates that many trans masculine individuals are indeed at risk for HIV. The presumption that trans masculine individuals almost exclusively have sex with cis-gender women and are therefore not at risk for HIV is thus incorrect [1]. As indicated by Reisner and Murchinson, there is a diverse range of bio-anatomies represented among trans masculine individuals and their partners in sexual encounters, and these should be considered in HIV prevention efforts [1].
Our finding that trans feminine individuals are 66 times more likely to have HIV than other individuals over 15 years of age is a higher estimate that the estimate generated in Baral and colleagues’ meta-analysis, [4] where the odds ratio for HIV infection among transgender women was 49.1. We believe that the odds ratio and prevalence rates established in our systematic review and meta-analysis are likely more realistic estimations for two reasons. First, our methodological approach used standardized rather than pooled prevalence and took into account not only country but also year of data collection. In a pooled estimate, the total study population and total HIV cases are summed, and then a crude proportion is calculated. This does not take heterogeneity and variation among the included studies into account. Our standardization approach entailed taking the weights from each country-year into account. Without the weighted standardization, a country-year combination that contains large or small study samples is likely to deliver misleading pooled results. The standardized approach thus delivers a more robust estimation than a pooled approach. Second, due to recent increases in the number of studies reporting HIV prevalence among transgender individuals, the total sample of transgender individuals in our meta-analysis was almost four and a half times larger than the pooled sample in Baral et al. [4] Third, the data reviewed in Baral et al. was derived from 15 countries, all of which have male-dominant epidemics, while the data in the meta-analysis reported here was derived from 34 countries, thus lending additional support to the contention that the high burden of HIV among transgender individuals is a worldwide phenomenon.
Our finding that HIV prevalence among transgender individuals appears to be, over the course of the epidemic, higher in African and Latin American regions may point to greater disapproval of gender fluidity and the accompanying marginalization that puts transgender individuals more at risk for HIV in these regions, although we recognize that overall prevalence rates for HIV are higher in Sub-Saharan Africa than in many other regions. Nonetheless, this was the first systematic review and meta-analysis to include samples from Sub-Saharan Africa, and the findings from Sub-Saharan Africa point to a significant burden of HIV among transgender individuals. However, given that, in our analyses, the sample sizes for African regions and Latin America were smaller than the sample sizes for other regions, more research is needed to confirm that transgender individuals in these regions do indeed have higher prevalence rates and carry an even greater burden of HIV. Additionally, future research should also seek to establish HIV prevalence rates and burdens in other understudied regions such as Eastern Europe.
This meta-analysis also demonstrated that sampling methods are likely to impact prevalence rates. This is in line with critiques of sampling methods that were levied in earlier commentaries on Baral et al. [4] and in other studies [11, 18, 134]. In our study, the various sampling methods generated very different prevalence rates for HIV in trans feminine individuals ranging from 5.4% to 37.8%. However, the four most frequently used sampling methods, namely respondent-driven sampling, sampling via STI clinics, convenience sampling, and cluster sampling had similar ranges (17.4% to 23.3%). We believe that the impact of sampling methods on prevalence rates is in need of further investigation. In our analyses, unambiguous classification was not always possible and the prevalence rates generated for less common sampling methods may be less reliable. We therefore recommend more comprehensive investigations of the impact of sampling methods in transgender studies.
In our meta-analyses, we also explored the potential role of PrEP availability by comparing studies conducted in the US where data was collected prior to and after the introduction of PrEP. No effect of PrEP could be established yet in our analyses. In fact, we found a higher HIV prevalence rate following the introduction of PrEP. This may be because there were only six studies done following the introduction of PrEP and the total sample after PrEP introduction was smaller and possibly less representative than the 18 studies conducted before PrEP was introduced. It is possible that no reduction in prevalence due to PrEP is the result of PrEP not yet reaching trans individuals. The inclusion of transgender individuals in PrEP trials has been low and access to PrEP for transgender individuals has been limited.[20, 21, 135] However, a qualitative study on PrEP acceptability among transgender women in San Francisco showed that interest was relatively high once participants were informed about the possibilities, thus suggesting that transgender individuals at high risk for HIV need to be informed about PrEP [20]. By the same bio-medical token, future meta-analytic studies should also include Treatment-as-prevention (TasP) effects in their analysis, once sufficiently robust primary data is available.
This systematic review and meta-analysis should be interpreted in light of possible limitations. One is potential sample size biases for studies originating from countries other than the USA, and those of trans masculine individuals. To be able to present a comprehensive, global picture, we set a lower bound for trans feminine individuals, excluding sample sizes of trans feminine individuals less than 40. Yet, we did not apply a minimum sample size for studies among trans masculine individuals as this would have resulted in the exclusion of most studies reporting HIV prevalence among trans masculine individuals. Further, we were not in a position to conduct city-level comparisons and thus acknowledge that our country-level analyses may provide a less precise estimation of the odds ratios, as these do not take into account that, in some countries, the HIV epidemic is more concentrated in certain areas. A third possible limitation is related to our classification of sampling methods. Unambiguous classification was not always feasible and it is possible that the prevalence rates generated for less common sampling methods were less reliable. Fourth, in our meta-analysis, the sample sizes for African regions and Latin America were smaller than the sample sizes for other regions, and this may have impacted the prevalence rates. Additionally, no prevalence rates from Eastern Europe were available. Fifth, our analysis did not account for sexual orientation or the presence or absence of gender reassignment surgery, both of which can impact HIV risk. It is also did not separately ascertain prevalence rates for trans feminine individuals who engage in sex work versus those who do not as primary level data on this is not available on a global scale. We recommend that future research take these potential shortcomings into consideration. Specifically, we recommend that future research explicitly investigate prevalence among sub-populations within the transgender community, and that new studies also take changes in HIV treatment (TasP) and sampling strategies, as well as their interactions, into account, as this will provide an even more comprehensive picture of HIV prevalence and burden among transgender individuals.
Summary and recommendations
That transgender individuals, both trans feminine and trans masculine, are, worldwide, disproportionately burdened by HIV points to the need to pay explicit attention to the unique HIV prevention and care needs of transgender individuals. HIV surveillance and research has traditionally grouped transgender individuals, particularly trans feminine individuals, with men who have sex with men (MSM), thus conflating gender with anatomy. This obscures the unique situation and vulnerabilities to HIV of transgender people [100]. It is therefore necessary to abandon the aggregation of data across MSM and trans feminine women [100, 136]. Additionally, and in line with MacCarthy et al., [11] we also propose disaggregating data across trans feminine and trans masculine individuals [106]. Although some individual and structural risk factors for HIV may be shared by transgender individuals, trans feminine and trans masculine individuals have unique needs [106].
Ascertaining that transgender individuals continue to be disproportionately burdened by HIV is important as it can serve as an impetus for efforts to change this burden. Although transgender individuals in certain regions may more affected by HIV and knowing that transgender processes are diverse across the world, we contend that it is important to, in all regions, target multiple levels of HIV risk, as well as their antecedents and their intersections, while being cognizant of the local context. Targeting individual level risk factors, such as unprotected sex, STI co-infection, and needle sharing, must occur alongside broader efforts to support transgender individuals and reduce stigmatization and marginalization [9, 137, 138].
Paramount to HIV risk reduction is gender affirmation, and in the context of HIV, gender affirmation is particularly important in health care [139–141]. Discrimination, judgment, insensitivity, and a lack of understanding from health care providers prevents many transgender individuals from accessing HIV prevention, testing, treatment, and care services [142]. Gender affirming care is not simply the provision of hormones and gender-affirming surgeries; it also includes using patients’ preferred names and pronouns, respecting diversity in gender identities and expressions, employing inclusive intake forms, displaying images that are welcoming to transgender individuals, and creating safe spaces where transgender individuals can be themselves [135, 143]. We recommend integrating HIV prevention and care services in broader gender-affirming care services [6, 135, 142]. This includes actively making PrEP available to transgender individuals [141, 144, 145].
Conclusion
In sum, this systematic review and meta-analyses have served to update our understanding of HIV prevalence over the course of the epidemic as well as HIV burden in both trans feminine and trans masculine individuals using a larger sample than ever before, and has shown that, worldwide, both carry a substantially higher burden of HIV than other individuals over 15 years of age. It has further demonstrated that a by country and year analysis is recommended, that prevalence rates are higher in African and Latin American regions, that sampling methods may impact prevalence rates, and that, at this point in time, the evidence does not suggest that PrEP has played a role in reducing HIV among transgender individuals.
Supporting information
(DOCX)
Fig A2.1. Funnel plot for the countries describing data from trans feminine individuals. Fig A2.2. Funnel plot for the countries describing data from trans masculine individuals.
(ZIP)
(DOC)
Acknowledgments
We thank Kristopher Banham (Cardiff University) and Ngoc Phuong Trinh Nguyen (Maastricht University) for their assistance with data extraction.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This systematic review and meta-analysis was funded by AIDSFonds (P-30805). See https://aidsfonds.nl. SS & KJ received the funding. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Reisner SL, Murchison GR. A global research synthesis of HIV and STI biobehavioural risks in female-to-male transgender adults. Glob Public Heal. 2016/01/21. 2016;11: 866–887. doi: 10.1080/17441692.2015.1134613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Melendez RM, Bonem LA, Sember R. On Bodies and Research: Transgender Issues in Health and HIV Research Articles. Sex Res Soc Policy A J NSRC. 2006;3: 21–38. doi: 10.1525/srsp.2006.3.4.21 [DOI] [Google Scholar]
- 3.World Health Organization W. Policy brief: Transgender people and HIV. Geneva, Switzerland; 2015. Available: https://www.who.int/hiv/pub/transgender/transgender-hiv-policy/en/.
- 4.Baral SD, Poteat T, Stromdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13: 214–222. doi: 10.1016/S1473-3099(12)70315-8 [DOI] [PubMed] [Google Scholar]
- 5.Poteat T, Scheim A, Xavier J, Reisner S, Baral S. Global Epidemiology of HIV Infection and Related Syndemics Affecting Transgender People. J Acquir Immune Defic Syndr. 2016/07/20. 2016;72 Suppl 3: S210–9. doi: 10.1097/QAI.0000000000001087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Santis JP. HIV infection risk factors among male-to-female transgender persons: A review of the literature. JANAC J Assoc Nurses AIDS Care. 2009;20: 362–372. doi: 10.1016/j.jana.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 7.Giami A, Le Bail J. HIV infection and STI in the trans population: A critical review. Rev D Epidemiol Sante Publique. 2011;59: 259–268. doi: 10.1016/j.respe.2011.02.102 [DOI] [PubMed] [Google Scholar]
- 8.Garofalo R, Kuhns LM, Reisner SL, Mimiaga MJ. Behavioral Interventions to Prevent HIV Transmission and Acquisition for Transgender Women: A Critical Review. Jaids-Journal Acquir Immune Defic Syndr. 2016;72: S220–S225. doi: 10.1097/QAI.0000000000001084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poteat T, Reisner SL, Radix A. HIV epidemics among transgender women. Curr Opin HIV AIDS. 2014;9: 168–173. doi: 10.1097/COH.0000000000000030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Poteat T, Wirtz AL, Radix A, Borquez A, Silva-Santisteban A, Deutsch MB, et al. HIV risk and preventive interventions in transgender women sex workers. Lancet. 2014/07/26. 2015;385: 274–286. doi: 10.1016/S0140-6736(14)60833-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.MacCarthy S, Poteat T, Xia ZY, Roque NL, Kim A, Baral S, et al. Current research gaps: a global systematic review of HIV and sexually transmissible infections among transgender populations. Sex Health. 2017;14: 456–468. doi: 10.1071/SH17096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Santos GM, Wilson EC, Rapues J, Macias O, Packer T, Raymond HF. HIV treatment cascade among transgender women in a San Francisco respondent driven sampling study. Sex Transm Infect. 2014;90: 430-+. doi: 10.1136/sextrans-2013-051342 [DOI] [PubMed] [Google Scholar]
- 13.Sevelius J. “There’s no pamphlet for the kind of sex I have”: HIV-related risk factors and protective behaviors among transgender men who have sex with nontransgender men. JANAC J Assoc Nurses AIDS Care. 2009;20: 398–410. doi: 10.1016/j.jana.2009.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hughto JMW, Reisner SL, Mimiaga MJ. Characteristics of transgender residents of Massachusetts cities with high HIV prevalence. Am J Public Health. 2015;105: e14–e18. doi: 10.2105/AJPH.2015.302877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: A systematic review. AIDS Behav. 2008;12: 1–17. doi: 10.1007/s10461-007-9299-3 [DOI] [PubMed] [Google Scholar]
- 16.Operario D, Soma T, Underhill K, Operario D, Soma T, Underhill K. Sex work and HIV status among transgender women: Systematic review and meta-analysis. JAIDS J Acquir Immune Defic Syndr. 2008;48: 97–103. doi: 10.1097/QAI.0b013e31816e3971 [DOI] [PubMed] [Google Scholar]
- 17.Becasen JS, Denard CL, Mullins MM, Higa DH, Sipe TA. Estimating the Prevalence of HIV and Sexual Behaviors Among the US Transgender Population: A Systematic Review and Meta-Analysis, 2006–2017. Am J Public Heal. 2019;109: E1–E8. doi: 10.2105/AJPH.2018.304727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bauer GR, Scheim AI. Sampling bias in transgender studies. Lancet Infect Dis. 2013;13: 832. doi: 10.1016/S1473-3099(13)70242-1 [DOI] [PubMed] [Google Scholar]
- 19.Stephenson R, Riley E, Rogers E, Suarez N, Metheny N, Senda J, et al. The Sexual Health of Transgender Men: A Scoping Review. J Sex Res. 2017;54: 424–445. doi: 10.1080/00224499.2016.1271863 [DOI] [PubMed] [Google Scholar]
- 20.Sevelius JM, Keatley J, Calma N, Arnold E. ‘I am not a man’: Trans-specific barriers and facilitators to PrEP acceptability among transgender women. Glob Public Health. 2016;11: 1060–1075. doi: 10.1080/17441692.2016.1154085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Escudero DJ, Kerr T, Operario D, Socias ME, Sued O, Marshall BD. Inclusion of trans women in pre-exposure prophylaxis trials: a review. AIDS Care. 2014/11/29. 2015;27: 637–641. doi: 10.1080/09540121.2014.986051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoornenborg E, Krakower DS, Prins M, Mayer KH. Preexposure prophylaxis for men who have sex with men and transgender persons in early adopting countries: a narrative review. AIDS. 2017. doi: 10.1097/QAD.0000000000001627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bekker LG, Rebe K, Venter F, Maartens G, Moorhouse M, Conradie F, et al. Southern African guidelines on the safe use of pre-exposure prophylaxis in persons at risk of acquiring HIV-1 infection. South Afr J HIV Med. 2016;17: 11. doi: 10.4102/sajhivmed.v17i1.455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Heal Policy Manag. 2014;3: 123–128. doi: 10.15171/ijhpm.2014.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Munn Z, MClinSc SM, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 2015;13: 147–153. doi: 10.1097/XEB.0000000000000054 [DOI] [PubMed] [Google Scholar]
- 26.Stahlman S, Liestman B, Ketende S, Kouanda S, Ky-Zerbo O, Lougue M, et al. Characterizing the HIV risks and potential pathways to HIV infection among transgender women in Cote d’Ivoire, Togo and Burkina Faso. J Int Aids Soc. 2016;19: 5–16. doi: 10.7448/IAS.19.3.20774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baral S, Sifakis F, Cleghorn F, Beyrer C. Elevated risk for HIV infection among men who have sex with men in low- and middle-income countries 2000–2006: A systematic review. PLoS Med. 2007;4: 1901–1911. doi: 10.1371/journal.pmed.0040339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.UNAIDS. AIDSinfo. 2017. Available: http://aidsinfo.unaids.org/.
- 29.U.S. Census Bureau. International Data Base. 2017. Available: https://www.census.gov/data-tools/demo/idb/informationGateway.php.
- 30.Brown LD, Cai TT, Das Gupta A. Interval estimation for a binomial proportion. Stat Sci. 2001;16: 101–117. doi: 10.1214/ss/1009213286 [DOI] [Google Scholar]
- 31.Institute for Statistics and Mathematics. The Comprehensive R Archive Network. Available: https://cran.r-project.org/.
- 32.Viechtbauer W. The metafor Package: A Meta-Analysis Package for R. Available: http://www.metafor-project.org/doku.php.
- 33.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327: 557–560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sterne JAC, Sutton AJ, Ioannidis JPA, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343: d4002. doi: 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
- 35.Aguayo N, Munoz SR, Aguilar G. P3.335 HIV and SYPHILIS Prevalence and Behaviour, Practises and Attitudes of the TRANS Population in Paraguay, 2011. Sex Transm Infect. 2013;89: A254.1-A254. doi: 10.1136/sextrans-2013-051184.0788 [DOI] [Google Scholar]
- 36.Akhtar H, Badshah Y, Akhtar S, Kanwal N, Akhtar MN, Zaidi N, et al. Prevalence of human immunodeficiency virus infection among transgender men in Rawalpindi (Pakistan). Virol J. 2012;9: 9. doi: 10.1186/1743-422X-9-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Altaf A. Explosive Expansion of HIV and associated risk factors among Male and Hijra Sex Workers in Sindh, Pakistan. Jaids-Journal Acquir Immune Defic Syndr. 2009;51: 158. doi: 10.1097/01.qai.0000351187.69035.d7 [DOI] [Google Scholar]
- 38.Altaf A, Zahidie A, Agha A. Comparing risk factors of HIV among hijra sex workers in Larkana and other cities of Pakistan: an analytical cross sectional study. BMC Public Health. 2012;12: 9. doi: 10.1186/1471-2458-12-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Baqi S, Shah SA, Baig MA, Mujeeb SA, Memon A. Seroprevalence of HIV, HBV and syphilis and associated risk behaviours in male transvestites (Hijras) in Karachi, Pakistan. J Pak Med Assoc. 2006;56: S17–21. [PubMed] [Google Scholar]
- 40.Barrington C, Wejnert C, Guardado ME, Nieto AI, Bailey GP. Social network characteristics and HIV vulnerability among transgender persons in San Salvador: Identifying opportunities for HIV prevention strategies. AIDS Behav. 2012;16: 214–224. doi: 10.1007/s10461-011-9959-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bastos FI, Bastos LS, Coutinho C, Toledo L, Mota JC, Velasco-de-Castro CA, et al. HIV, HCV, HBV, and syphilis among transgender women from Brazil: Assessing different methods to adjust infection rates of a hard-to-reach, sparse population. Medicine (Baltimore). 2018;97: S16–S24. doi: 10.1097/md.0000000000009447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bellhouse C, Walker S, Fairley CK, Vodstrcil LA, Bradshaw CS, Chen MY, et al. Patterns of sexual behaviour and sexual healthcare needs among transgender individuals in Melbourne, Australia, 2011–2014. Sex Transm Infect. 2016. doi: 10.1136/sextrans-2016-052710 [DOI] [PubMed] [Google Scholar]
- 43.Brahmam GN V, Kodavallaa V, Rajkumar H, Rachakulla HK, Kallam S, Myakala SP, et al. Sexual practices, HIV and sexually transmitted infections among self-identified men who have sex with men in four high HIV prevalence states of India. Aids. 2008;22: S45–S57. doi: 10.1097/01.aids.0000343763.54831.15 [DOI] [PubMed] [Google Scholar]
- 44.Carballo-Dieguez A, Balan I, Dolezal C, Mello MB, Carballo-Diéguez A, Balan I, et al. Recalled sexual experiences in childhood with older partners: A study of Brazilian men who have sex with men and male-to-female transgender persons. Arch Sex Behav. 2012;41: 363–376. doi: 10.1007/s10508-011-9748-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Castel AD, Magnus M, Peterson J, Anand K, Wu C, Martin M, et al. Implementing a Novel Citywide Rapid HIV Testing Campaign in Washington, DC: Findings and Lessons Learned. Public Health Rep. 2012;127: 422–431. doi: 10.1177/003335491212700410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Castillo R, Konda KA, Leon SR, Silva-Santisteban A, Salazar X, Klausner JD, et al. HIV and Sexually Transmitted Infection Incidence and Associated Risk Factors Among High-Risk MSM and Male-to-Female Transgender Women in Lima, Peru. Jaids-Journal Acquir Immune Defic Syndr. 2015;69: 567–575. doi: 10.1097/QAI.0000000000000667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chariyalertsak S, Kosachunhanan N, Saokhieo P, Songsupa R, Wongthanee A, Chariyalertsak C, et al. HIV Incidence, Risk Factors, and Motivation for Biomedical Intervention among Gay, Bisexual Men, and Transgender Persons in Northern Thailand. PLoS One. 2011;6: 8. doi: 10.1371/journal.pone.0024295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen SP, McFarland W, Thompson HM, Raymond HF. Transmen in San Francisco: What do we know from HIV test site data? AIDS Behav. 2011;15: 659–662. doi: 10.1007/s10461-010-9859-9 [DOI] [PubMed] [Google Scholar]
- 49.Chhim S, Ngin C, Chhoun P, Tuot S, Ly C, Mun P, et al. HIV prevalence and factors associated with HIV infection among transgender women in Cambodia: results from a national Integrated Biological and Behavioral Survey. BMJ Open. 2017;7: e015390. doi:ARTN e01539010.1136/bmjopen-2016-015390. doi: 10.1136/bmjopen-2016-015390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Clements-Nolle K, Wilkinson W, Kitano K, Marx R. HIV prevention and health service needs of the transgender community in San Francisco. In: Bockting W, Kirk S, Bockting (Ed) W, Kirk (Ed) S, editors. Transgender and HIV: Risks, prevention, and care. Clements-Nolle, Kristen, San Francisco Dept of Public Health, AIDS Office, 25 Van Ness Avenue, Suite #500, San Francisco, CA, US, 94102: Haworth Press; 2001. pp. 69–89. Available: http://login.ezproxy.ub.unimaas.nl/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2002-01046-005&site=ehost-live&scope=site.
- 51.Colby D, Nguyen NA, Le B, Toan T, Thien DD, Huyen HT, et al. HIV and Syphilis Prevalence Among Transgender Women in Ho Chi Minh City, Vietnam. AIDS Behav. 2016;20: S379–S385. doi: 10.1007/s10461-016-1485-8 [DOI] [PubMed] [Google Scholar]
- 52.Costa AB, Fontanari AM, Jacinto MM, da Silva DC, Lorencetti EK, da Rosa Filho HT, et al. Population-based HIV prevalence and associated factors in male-to-female transsexuals from Southern Brazil. Arch Sex Behav. 2014/09/24. 2015;44: 521–524. doi: 10.1007/s10508-014-0386-z [DOI] [PubMed] [Google Scholar]
- 53.Dasarathan S, Kalaivani S. Study of prevalence of sexually transmitted infections/human immunodeficiency virus and condom use among male-to-female transgender: A retrospective analysis from a tertiary care hospital in Chennai. Indian J Sex Transm Dis. 2017;38: 43–46. doi: 10.4103/0253-7184.196889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Diez M, Bleda MJ, Varela JA, Ordonana JR, Azpiri MA, Vall M, et al. Trends in HIV testing, prevalence among first-time testers, and incidence in most-at-risk populations in Spain: the EPI-VIH Study, 2000 to 2009. Eurosurveillance. 2014;19: 18–30. [DOI] [PubMed] [Google Scholar]
- 55.Dos Ramos Farias MS, Garcia MN, Reynaga E, Romero M, Vaulet MLG, Fermepin MR, et al. First report on sexually transmitted infections among trans (male to female transvestites, transsexuals, or transgender) and male sex workers in Argentina: high HIV, HPV, HBV, and syphilis prevalence. Int J Infect Dis. 2011;15: e635–40. doi: 10.1016/j.ijid.2011.05.007 [DOI] [PubMed] [Google Scholar]
- 56.Fernandes FRP, Zanini PB, Rezende GR, Castro LS, Bandeira LM, Puga MA, et al. Syphilis infection, sexual practices and bisexual behaviour among men who have sex with men and transgender women: a cross-sectional study. Sex Transm Infect. 2015;91: 142–149. doi: 10.1136/sextrans-2014-051589 [DOI] [PubMed] [Google Scholar]
- 57.Fernandez-Balbuena S, Belza MJ, Urdaneta E, Esteso R, Rosales-Statkus ME, de la Fuente L, et al. Serving the underserved: an HIV testing program for populations reluctant to attend conventional settings. Int J Public Health. 2015;60: 121–126. doi: 10.1007/s00038-014-0606-2 [DOI] [PubMed] [Google Scholar]
- 58.Fernandez-Lopez L, Reyes-Uruena J, Agusti C, Kustec T, Serdt M, Klavs I, et al. The COBATEST network: monitoring and evaluation of HIV community-based practices in Europe, 2014–2016. Hiv Med. 2018;19: 21–26. doi: 10.1111/hiv.12592 [DOI] [PubMed] [Google Scholar]
- 59.Grandi JL, Goihman S, Ueda M, Rutherford G. HIV and syphilis in Brazilian male sex workers. AIDS Behav. 2000;4: 129–135. Available: http://search.proquest.com/docview/39370745?accountid=14512%5Cnhttp://ucelinks.cdlib.org:8888/sfx_local?url_ver=Z39.88-2004&rft_val_fmt=info:ofi/fmt:kev:mtx:journal&genre=conference&sid=ProQ:ProQ%3Acpi&atitle=HIV+and+syphilis+in+Brazilian+male+sex+workers. [Google Scholar]
- 60.Green N, Hoenigl M, Morris S, Little SJ. Risk Behavior and Sexually Transmitted Infections Among Transgender Women and Men Undergoing Community-Based Screening for Acute and Early HIV Infection in San Diego. Medicine (Baltimore). 2015;94. doi:ARTN e183010.1097/MD.0000000000001830. doi: 10.1097/MD.0000000000001830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Grinsztejn B, Jalil EM, Monteiro L, Velasque L, Moreira RI, Garcia ACF, et al. Unveiling of HIV dynamics among transgender women: a respondent-driven sampling study in Rio de Janeiro, Brazil. Lancet HIV. 2017;4: E169–E176. doi: 10.1016/S2352-3018(17)30015-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Guadamuz TE, Wimonsate W, Varangrat A, Phanuphak P, Jommaroeng R, McNicholl JM, et al. HIV prevalence, risk behavior, hormone use and surgical history among transgender persons in Thailand. AIDS Behav. 2011;15: 650–658. doi: 10.1007/s10461-010-9850-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gutierrez M, Tajada P, Alvarez A, De Julian R, Baquero M, Soriano V, et al. Prevalence of HIV-1 non-B subtypes, syphilis, HTLV, and hepatitis B and C viruses among immigrant sex workers in Madrid, Spain. J Med Virol. 2004;74: 521–527. doi: 10.1002/jmv.20208 [DOI] [PubMed] [Google Scholar]
- 64.Guy R, Mustikawati DE, Wijaksono DB, Nugraihini N, Priohutomo S, Silitonga N, et al. Voluntary counselling and testing sites as a source of sentinel information on HIV prevalence in a concentrated epidemic: A pilot project from Indonesia. Int J STD AIDS. 2011;22: 505–511. doi: 10.1258/ijsa.2009.009445 [DOI] [PubMed] [Google Scholar]
- 65.Habarta N, Wang GS, Mulatu MS, Larish N. HIV Testing by Transgender Status at Centers for Disease Control and Prevention-Funded Sites in the United States, Puerto Rico, and US Virgin Islands, 2009–2011. Am J Public Health. 2015;105: 1917–1925. doi: 10.2105/AJPH.2015.302659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hadikusumo AA, Utsumi T, Amin M, Khairunisa SQ, Istimagfirah A, Wahyuni RM, et al. High Rates of Hepatitis B Virus (HBV), Hepatitis C Virus (HCV), and Human Immunodeficiency Virus Infections and Uncommon HBV Genotype/Subtype and HCV Subtype Distributions among Transgender Individuals in Surabaya, Indonesia. Jpn J Infect Dis. 2016;69: 493–499. doi: 10.7883/yoken.JJID.2015.384 [DOI] [PubMed] [Google Scholar]
- 67.Hakim AJ, Coy K, Patnaik P, Telly N, Ballo T, Traore B, et al. An urgent need for HIV testing among men who have sex with men and transgender women in Bamako, Mali: Low awareness of HIV infection and viral suppression among those living with HIV. PLoS One. 2018;13. doi: 10.1371/journal.pone.0207363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hawkes S, Collumbien M, Platt L, Lalji N, Rizvi N, Andreasen A, et al. HIV and other sexually transmitted infections among men, transgenders and women selling sex in two cities in Pakistan: a cross-sectional prevalence survey. Sex Transm Infect. 2009;85: 8–16. doi: 10.1136/sti.2008.033910 [DOI] [PubMed] [Google Scholar]
- 69.Hiransuthikul A, Pattanachaiwit S, Teeratakulpisarn N, Chamnan P, Pathipvanich P, Thongpaen S, et al. High subsequent and recurrent sexually transmitted infection prevalence among newly diagnosed HIV-positive Thai men who have sex with men and transgender women in the Test and Treat cohort. Int J STD AIDS. 2018; 956462418799213. doi: 10.1177/0956462418799213 [DOI] [PubMed] [Google Scholar]
- 70.Januraga PP, Wulandari LPL, Muliawan P, Sawitri S, Causer L, Wirawan DN, et al. Sharply rising prevalence of HIV infection in Bali: a critical assessment of the surveillance data. Int J Std Aids. 2013;24: 633–637. doi: 10.1177/0956462413477556 [DOI] [PubMed] [Google Scholar]
- 71.Jin H, Restar A, Biello K, Kuhns L, Reisner S, Garofalo R, et al. Burden of hiv among young transgender women: Factors associated with hiv infection and hiv treatment engagement. AIDS Care. 2019;31: 125–130. doi: 10.1080/09540121.2018.1539213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kaplan RL, McGowan J, Wagner GJ. HIV prevalence and demographic determinants of condomless receptive anal intercourse among trans feminine individuals in Beirut, Lebanon. J Int AIDS Soc. 2016;19: 17–25. doi:Artn 2078710.7448/Ias.19.3.20787. doi: 10.7448/IAS.19.3.20787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kellogg TA, Clements-Nolle K, Dilley J, Katz MH, McFarland W. Incidence of human immunodeficiency virus among male-to-female transgendered persons in San Francisco. J Acquir Immune Defic Syndr. 2001;28: 380–384. doi: 10.1097/00126334-200112010-00012 [DOI] [PubMed] [Google Scholar]
- 74.Keshinro B, Crowell TA, Nowak RG, Adebajo S, Peel S, Gaydos CA, et al. High prevalence of HIV, chlamydia and gonorrhoea among men who have sex with men and transgender women attending trusted community centres in Abuja and Lagos, Nigeria. J Int Aids Soc. 2016;19: 9. doi: 10.7448/IAS.19.1.21270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Khan AA, Rehan N, Qayyum K, Khan AA. Correlates and prevalence of HIV and sexually transmitted infections among Hijras (male transgenders) in Pakistan. Int J STD AIDS. 2008;19: 817–820. doi: 10.1258/ijsa.2008.008135 [DOI] [PubMed] [Google Scholar]
- 76.Kojima N, Park H, Konda KA, Davey DLJ, Bristow CC, Brown B, et al. The PICASSO Cohort: baseline characteristics of a cohort of men who have sex with men and male-to-female transgender women at high risk for syphilis infection in Lima, Peru. Bmc Infect Dis. 2017;17: 8. doi: 10.1186/s12879-016-2115-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Leinung M, Urizar M, Patel N, Sood S. Endocrine Treatment of Transsexual Persons: Extensive Personal Experience. Endocr Pract. 2013;19: 644–650. doi: 10.4158/EP12170.OR [DOI] [PubMed] [Google Scholar]
- 78.Lipsitz MC, Segura ER, Castro JL, Smith E, Medrano C, Clark JL, et al. Bringing testing to the people—benefits of mobile unit HIV/syphilis testing in Lima, Peru, 2007–2009. Int J Std Aids. 2014;25: 325–331. doi: 10.1177/0956462413507443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lobato MI, Koff WJ, Schestatsky SS, Chaves CP de V, Petry A, Crestana T, et al. Clinical characteristics, psychiatric comorbidities and sociodemographic profile of transsexual patients from an outpatient clinic in Brazil. Int J Transgenderism. 2008;10: 69–77. doi: 10.1080/15532730802175148 [DOI] [Google Scholar]
- 80.Logie CH, Lacombe-Duncan A, Wang Y, Jones N, Levermore K, Neil A, et al. Prevalence and Correlates of HIV Infection and HIV Testing Among Transgender Women in Jamaica. AIDS Patient Care STDS. 2016;30: 416–424. doi: 10.1089/apc.2016.0145 [DOI] [PubMed] [Google Scholar]
- 81.Long J, Montano M, Cabello R, Sanchez H, Lama JR, Duerr A. Comparing sexual risk behavior in a high-risk group of men who have sex with men and transgender women in Lima, Peru. J Acquir Immune Defic Syndr. 2019. doi: 10.1097/QAI.0000000000001966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Luzzati R, Zatta M, Pavan N, Serafin M, Maurel C, Trombetta C, et al. Prevalence of Human Immunodeficiency Virus, Hepatitis B Virus, and Hepatitis C Virus Infections Among Transgender Persons Referred to an Italian Center for Total Sex Reassignment Surgery. Sex Transm Dis. 2016;43: 407–411. doi: 10.1097/OLQ.0000000000000452 [DOI] [PubMed] [Google Scholar]
- 83.Manieri C, Castellano E, Crespi C, Di Bisceglie C, Dell’Aquila C, Gualerzi A, et al. Medical Treatment of Subjects with Gender Identity Disorder: The Experience in an Italian Public Health Center. Int J Transgenderism. 2014;15: 53–65. doi: 10.1080/15532739.2014.899174 [DOI] [Google Scholar]
- 84.McFarland W, Wilson EC, Raymond HF. HIV Prevalence, Sexual Partners, Sexual Behavior and HIV Acquisition Risk Among Trans Men, San Francisco, 2014. AIDS Behav. 2017;21: 3346–3352. doi: 10.1007/s10461-017-1735-4 [DOI] [PubMed] [Google Scholar]
- 85.Mimiaga M, Hughto JMW, Biello KB, Santostefano CM, Kuhns LM, Reisner SL, et al. Longitudinal Analysis of Syndemic Psychosocial Problems Predicting HIV Risk Behavior Among a Multicity Prospective Cohort of Sexually Active Young Transgender Women in the United States. Available SSRN 3249701. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Murrill CS, Liu KL, Guilin V, Colon ER, Dean L, Buckley LA, et al. HIV prevalence and associated risk behaviors in New York City’s house ball community. Am J Public Health. 2008;98: 1074–1080. doi: 10.2105/AJPH.2006.108936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nemoto T, Bödeker B, Iwamoto M, Sakata M, Bodeker B, Iwamoto M, et al. Practices of receptive and insertive anal sex among transgender women in relation to partner types, sociocultural factors, and background variables. AIDS Care. 2014;26: 434–440. doi: 10.1080/09540121.2013.841832 [DOI] [PubMed] [Google Scholar]
- 88.Nguyen TA, Nguyen HT, Le GT, Detels R. Prevalence and risk factors associated with HIV infection among men having sex with men in Ho Chi Minh City, Vietnam. AIDS Behav. 2008;12: 476–482. doi: 10.1007/s10461-007-9267-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nuttbrock L, Bockting W, Rosenblum A, Hwahng S, Mason M, Macri M, et al. “Gender abuse, depressive symptoms, and HIV and other sexually transmitted infections among male-to-female transgender persons: A three-year prospective study”: Erratum. Am J Public Health. 2013;103: 300–307. doi: 10.2105/AJPH.2011.300568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nuttbrock L, Hwahng S, Bockting W, Rosenblum A, Mason M, Macri M, et al. Lifetime risk factors for HIV/sexually transmitted infections among male-to-female transgender persons. JAIDS J Acquir Immune Defic Syndr. 2009;52: 417–421. doi: 10.1097/QAI.0b013e3181ab6ed8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ongwandee S, Lertpiriyasuwat C, Khawcharoenporn T, Chetchotisak P, Thiansukhon E, Leerattanapetch N, et al. Implementation of a Test, Treat, and Prevent HIV program among men who have sex with men and transgender women in Thailand, 2015–2016. PLoS One. 2018;13. doi: 10.1371/journal.pone.0201171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pando MA, Gomez-Carrillo M, Vignoles M, Rubio AE, Farias MSD, Vila M, et al. Incidence of HIV Type 1 Infection, Antiretroviral Drug Resistance, and Molecular Characterization in Newly Diagnosed Individuals in Argentina: A Global Fund Project. AIDS Res Hum Retroviruses. 2011;27: 17–23. doi: 10.1089/aid.2010.0013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Patrascioiu I, Lopez CQ, Porta MM, Velazquez GBA, Hanzu FA, Gomez-Gil E, et al. Characteristics of the HIV positive transgender population of Catalonia. Endocr Abstr. 2013;32. doi: 10.1530/endoabs.32.P341 [DOI] [Google Scholar]
- 94.Peitzmeier SM, Reisner SL, Harigopal P, Potter J. Female-to-male patients have high prevalence of unsatisfactory paps compared to non-transgender females: Implications for cervical cancer screening. J Gen Intern Med. 2014;29: 778–784. doi: 10.1007/s11606-013-2753-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Pell C, Prone I, Vlahakis E. A clinical audit of male to female (MTF) transgender patients attending taylor square private clinic in Sydney, Australia, aiming to improve quality of care. J Sex Med. 2011;8: 179. [Google Scholar]
- 96.Pisani E, Girault P, Gultom M, Sukartini N, Kumalawati J, Jazan S, et al. HIV, syphilis infection, and sexual practices among transgenders, male sex workers, and other men who have sex with men in Jakarta, Indonesia. Sex Transm Infect. 2004;80: 536–540. doi: 10.1136/sti.2003.007500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Pitasi MA, Oraka E, Clark H, Town M, DiNenno EA. HIV Testing Among Transgender Women and Men-27 States and Guam, 2014–2015. Mmwr-Morbidity Mortal Wkly Rep. 2017;66: 883–887. doi: 10.15585/mmwr.mm6633a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Pizzicato LN, Vagenas P, Gonzales P, Lama JR, Pun M, Sanchez J, et al. Active syphilis and its association with HIV and sexual risk behaviours in a multicity sample of men who have sex with men and transgender women in Peru. Sex Health. 2017;14: 304–312. doi: 10.1071/SH16149 [DOI] [PubMed] [Google Scholar]
- 99.Poteat T, Ackerman B, Diouf D, Ceesay N, Mothopeng T, Odette KZ, et al. HIV prevalence and behavioral and psychosocial factors among transgender women and cisgender men who have sex with men in 8 African countries: A cross-sectional analysis. PLoS Med. 2017;14. doi: 10.1371/journal.pmed.1002422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Poteat T, German D, Flynn C. The conflation of gender and sex: Gaps and opportunities in HIV data among transgender women and MSM. Glob Public Health. 2016;11: 835–848. doi: 10.1080/17441692.2015.1134615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Prabawanti C, Bollen L, Palupy R, Morineau G, Girault P, Mustikawati DE, et al. HIV, sexually transmitted infections, and sexual risk behavior among transgenders in Indonesia. AIDS Behav. 2011;15: 663–673. doi: 10.1007/s10461-010-9790-0 [DOI] [PubMed] [Google Scholar]
- 102.Quinn VP, Nash R, Hunkeler E, Contreras R, Cromwell L, Becerra-Culqui TA, et al. Cohort profile: Study of Transition, Outcomes and Gender (STRONG) to assess health status of transgender people. BMJ Open. 2017;7. doi: 10.1136/bmjopen-2017-018121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rana AKMM, Reza MM, Alam MS, Khatun M, Khan SI, Azim T. Effects of In-country and Cross-Border Mobility on Condom Use Among Transgender Women (hijras) in Bangladesh: A Cross-Sectional Study. AIDS Behav. 2016;20: 2165–2177. doi: 10.1007/s10461-015-1275-8 [DOI] [PubMed] [Google Scholar]
- 104.Raymond HF, Wilson EC, Packer T, Ick T, Lin J, McFarland W. High and Stable Human Immunodeficiency Virus Prevalence Among Transwomen With Low Income Recruited With Respondent-driven Sampling, San Francisco, 2010–2016. Sex Transm Dis. 2019;46: 118–124. doi: 10.1097/OLQ.0000000000000916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Reback CJ, Lombardi EL, Simon PA, Frye DM. HIV Seroprevalence and Risk Behaviors Among Transgendered Women Who Exchange Sex in Comparison with Those Who Do Not. J Psychol Human Sex. 2005;17: 5–22. doi: 10.1300/J056v17n01_02 [DOI] [Google Scholar]
- 106.Reisner SL, White JM, Mayer KH, Mimiaga MJ. Sexual risk behaviors and psychosocial health concerns of female-to-male transgender men screening for STD’S at an urban community health center. AIDS Care. 2014;26: 857–864. doi: 10.1080/09540121.2013.855701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Reisner SL, Vetters R, White JM, Cohen EL, LeClerc M, Zaslow S, et al. Laboratory-confirmed HIV and sexually transmitted infection seropositivity and risk behavior among sexually active transgender patients at an adolescent and young adult urban community health center. Aids Care-Psychological Socio-Medical Asp Aids/Hiv. 2015;27: 1031–1036. doi: 10.1080/09540121.2015.1020750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Rich A, Scott K, Johnston C, Blackwell E, Lachowsky N, Cui Z, et al. Sexual HIV risk among gay, bisexual and queer transgender men: findings from interviews in Vancouver, Canada. Cult Health Sex. 2017;19: 1197–1209. doi: 10.1080/13691058.2017.1299882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Rowe C, Santos GM, McFarland W, Wilson EC. Prevalence and correlates of substance use among trans*female youth ages 16–24 years in the San Francisco Bay Area. Drug Alcohol Depend. 2015;147: 160–166. doi: 10.1016/j.drugalcdep.2014.11.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Russi JC, Serra M, Vinoles J, Perez MT, Ruchansky D, Alonso G, et al. Sexual transmission of hepatitis B virus, hepatitis C virus, and human immunodeficiency virus type 1 infections among male transvestite comercial sex workers in Montevideo, Uruguay. Am J Trop Med Hyg. 2003;68: 716–720. [PubMed] [Google Scholar]
- 111.Sahastrabuddhe S, Gupta A, Stuart E, Godbole S, Ghate M, Sahay S, et al. Sexually transmitted infections and risk behaviors among transgender persons (Hijras) of Pune, India. JAIDS J Acquir Immune Defic Syndr. 2012;59: 72–78. doi: 10.1097/QAI.0b013e318236bd6f [DOI] [PubMed] [Google Scholar]
- 112.Salas-Espinoza KJ, Menchaca-Diaz R, Patterson TL, Urada LA, Smith D, Strathdee SA, et al. Hiv prevalence and risk behaviors in male to female (mtf) transgender persons in tijuana, mexico. AIDS Behav. 2017. doi: 10.1007/s10461-017-1931-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Saravanamurthy P, Rajendran P, Ramakrishnan Dr. L, Ashok G, Miranda PM, Raghavan SS, et al. STI and HIV prevalence in male-to-female transgender communities in Chennai, Southern India. XVII International AIDS Conference. 3–8 August 2008, Mexico City, Mexico. 2008.
- 114.Schulden JD, Song BW, Barros A, Mares-DelGrasso A, Martin CW, Ramirez R, et al. Rapid HIV Testing in Transgender Communities by Community-Based Organizations in Three Cities. Public Health Rep. 2008;123: 101–114. doi: 10.1177/00333549081230S313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Seekaew P, Pengnonyang S, Jantarapakde J, Sungsing T, Rodbumrung P, Trachunthong D, et al. Characteristics and HIV epidemiologic profiles of men who have sex with men and transgender women in key population-led test and treat cohorts in Thailand. PLoS One. 2018;13. doi: 10.1371/journal.pone.0203294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Shan D, Yu MH, Yang J, Zhuang MH, Ning Z, Liu H, et al. Correlates of HIV infection among transgender womenin two Chinese cities. Infect Dis Poverty. 2018;7. doi: 10.1186/s40249-018-0388-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Shaw SY, Lorway R, Bhattacharjee P, Reza-Paul S, du Plessis E, McKinnon L, et al. Descriptive epidemiology of factors associated with HIV infections among men and transgender women who have sex with men in South India. LGBT Heal. 2016;3: 292–299. doi: 10.1089/lgbt.2015.0023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Shaw SY, Emmanuel F, Adrien A, Holte-Mckenzie M, Archibald CP, Sandstrom P, et al. The descriptive epidemiology of male sex workers in Pakistan: a biological and behavioural examination. Sex Transm Infect. 2011;87: 73–80. doi: 10.1136/sti.2009.041335 [DOI] [PubMed] [Google Scholar]
- 119.Sherman SG, Park JN, Galai N, Allen ST, Huettner SS, Silberzahn BE, et al. Drivers of HIV infection among cisgender and transgender female sex worker populations in Baltimore city: Results from the SAPPHIRE study. J Acquir Immune Defic Syndr. 2019. doi: 10.1097/QAI.0000000000001959 [DOI] [PubMed] [Google Scholar]
- 120.Shinde S, Setia MS, Row-Kavi A, Anand V, Jerajani H. Male sex workers: Are we ignoring a risk group in Mumbai, India? Indian J Dermatology Venereol Leprol. 2009;75: 41–46. doi: 10.4103/0378-6323.45219 [DOI] [PubMed] [Google Scholar]
- 121.Silva-Santisteban A, Raymond HF, Salazar X, Villayzan J, Leon S, McFarland W, et al. Understanding the HIV/AIDS epidemic in transgender women of Lima, Peru: Results from a sero-epidemiologic study using respondent driven sampling. AIDS Behav. 2012;16: 872–881. doi: 10.1007/s10461-011-0053-5 [DOI] [PubMed] [Google Scholar]
- 122.Sotelo J, Claudia B. SEROPREVALENCE AND INCIDENCE STUDY OF HIV IN TRANSGENDER IN ARGENTINA-2009. J Epidemiol Community Health. 2011;65: A301–A301. doi: 10.1136/jech.2011.142976k.20 [DOI] [Google Scholar]
- 123.Stephens SC, Bernstein KT, Philip SS. Male to female and female to male transgender persons have different sexual risk behaviors yet similar rates of STDs and HIV. AIDS Behav. 2011;15: 683–686. doi: 10.1007/s10461-010-9773-1 [DOI] [PubMed] [Google Scholar]
- 124.Subramanian T, Ramakrishnan L, Aridoss S, Goswami P, Kanguswami B, Shajan M, et al. Increasing condom use and declining STI prevalence in high-risk MSM and TGs: evaluation of a large-scale prevention program in Tamil Nadu, India. BMC Public Health. 2013;13: 14. doi: 10.1186/1471-2458-13-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Toibaro JJ, Ebensrtejin JF, Parlante A, Burgoa P, Freyre A, Romero M, et al. Sexually transmitted infections among transgender individuals and other sexual identities. Med Aires. 2009;69: 327–330. [PubMed] [Google Scholar]
- 126.van Veen MG, Götz HM, van Leeuwen PA, Prins M, van de Laar MJW, Gotz HM, et al. HIV and sexual risk behavior among commercial sex workers in the Netherlands. Arch Sex Behav. 2010;39: 714–723. doi: 10.1007/s10508-008-9396-z [DOI] [PubMed] [Google Scholar]
- 127.Waheed U, Satti HS, Arshad M, Farooq A, Rauf A, Zaheer HA. Epidemiology of HIV/AIDS and Syphilis among High Risk Groups in Pakistan. Pak J Zool. 2017;49: 1829–1834. doi: 10.17582/journal.pjz/2017.49.5.1829.1834 [DOI] [Google Scholar]
- 128.Wasantioopapokakorn M, Manopaiboon C, Phoorisri T, Sukkul A, Lertpiriyasuwat C, Ongwandee S, et al. Implementation and assessment of a model to increase HIV testing among men who have sex with men and transgender women in Thailand, 2011–2016. Aids Care-Psychological Socio-Medical Asp Aids/Hiv. 2018;30: 1239–1245. doi: 10.1080/09540121.2018.1492697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Weissman A, Ngak S, Srean C, Sansothy N, Mills S, Ferradini L. HIV Prevalence and Risks Associated with HIV Infection among Transgender Individuals in Cambodia. PLoS One. 2016;11: 16. doi: 10.1371/journal.pone.0152906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.World Health Organization W. Policy brief: transgender health and HIV in the Philippines. Manila: WHO Regional Office for the Western Pacific; 2016.
- 131.Wickersham JA, Gibson BA, Bazazi AR, Pillai V, Pedersen CJ, Meyer JP, et al. Prevalence of Human Immunodeficiency Virus and Sexually Transmitted Infections Among Cisgender and Transgender Women Sex Workers in Greater Kuala Lumpur, Malaysia: Results From a Respondent-Driven Sampling Study. Sex Transm Dis. 2017;44: 663–670. doi: 10.1097/OLQ.0000000000000662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zaccarelli M, Spizzichino L, Venezia S, Antinori A, Gattari P. Changes in regular condom use among immigrant transsexuals attending a counselling and testing reference site in central Rome: a 12 year study. Sex Transm Infect. 2004;80: 541–545. doi: 10.1136/sti.2004.010769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zea MC, Reisen CA, del Rio-Gonzalez AM, Bianchi FT, Ramirez-Valles J, Poppen PJ. HIV Prevalence and Awareness of Positive Serostatus Among Men Who Have Sex With Men and Transgender Women in Bogota, Colombia. Am J Public Health. 2015;105: 1588–1595. doi: 10.2105/AJPH.2014.302307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Clark JL, Konda KA, Silva-Santisteban A, Peinado J, Lama JR, Kusunoki L, et al. Sampling methodologies for epidemiologic surveillance of men who have sex with men and transgender women in Latin America: An empiric comparison of convenience sampling, time space sampling, and respondent driven sampling. AIDS Behav. 2014;18: 2338–2348. doi: 10.1007/s10461-013-0680-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sevelius JM, Deutsch MB, Grant R. The future of PrEP among transgender women: the critical role of gender affirmation in research and clinical practices. J Int AIDS Soc. 2016;19. doi:Artn 21105 doi: 10.7448/IAS.19.7.21105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Bauermeister JA, Goldenberg T, Connochie D, Jadwin-Cakmak L, Stephenson R. Psychosocial Disparities Among Racial/Ethnic Minority Transgender Young Adults and Young Men Who Have Sex with Men Living in Detroit. Transgender Heal. 2016;1: 279–290. doi: 10.1089/trgh.2016.0027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Rood BA, Kochaver JJ, McConnell EA, Ott MQ, Pantalone DW. Minority Stressors Associated with Sexual Risk Behaviors and HIV Testing in a US Sample of Transgender Individuals. AIDS Behav. 2018;22: 3111–3116. doi: 10.1007/s10461-018-2054-0 [DOI] [PubMed] [Google Scholar]
- 138.Bos AER, Pryor JB, Reeder GD, Stutterheim SE. Stigma: Advances in Theory and Research. Basic Appl Soc Psych. 2013;35: 1–9. doi: 10.1080/01973533.2012.746147 [DOI] [Google Scholar]
- 139.Reisner SL, Poteat T, Keatley J, Cabral M, Mothopeng T, Dunham E, et al. Global health burden and needs of transgender populations: a review. Lancet. 2016/06/22. 2016;388: 412–436. doi: 10.1016/S0140-6736(16)00684-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Sevelius JM, Patouhas E, Keatley JG, Johnson MO. Barriers and Facilitators to Engagement and Retention in Care among Transgender Women Living with Human Immunodeficiency Virus. Ann Behav Med. 2014;47: 5–16. doi: 10.1007/s12160-013-9565-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Fontanari AM V, Costa AB, Zanella G, Feijo M, Schwarz K, Soll B, et al. AIDS RELATED CARE FOR TRANSGENDER PEOPLE: A SYSTEMATIC REVIEW. J Sex Med. 2018;15: S286–S286. [Google Scholar]
- 142.Bekker L-G, Alleyne G, Baral S, Cepeda J, Daskalakis D, Dowdy D, et al. Advancing global health and strengthening the HIV response in the era of the Sustainable Development Goals: the International AIDS Society—Lancet Commission. Lancet. 2018;392: 312–358. doi: 10.1016/S0140-6736(18)31070-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Valentine SE, Shipherd JC. A systematic review of social stress and mental health among transgender and gender non-conforming people in the United States. Clin Psychol Rev. 2018;66: 24–38. doi: 10.1016/j.cpr.2018.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Cairns G, McCormack S, Molina JM. The European preexposure prophylaxis revolution. Curr Opin Hiv Aids. 2016;11: 74–79. doi: 10.1097/COH.0000000000000223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Pacífico de Carvalho N, Mendicino CCP, Cândido RCF, Alecrim DJD, Menezes de Pádua CA. HIV pre-exposure prophylaxis (PrEP) awareness and acceptability among trans women: a review. AIDS Care. 2019; 1–7. doi: 10.1080/09540121.2019.1612014 [DOI] [PubMed] [Google Scholar]