Abstract
Objective
This study aims to characterize changes in the total operative cases logged by general surgery residents across three residency programs.
Design
Retrospective cohort study. De-identified case logs, divided by institution and post graduate year (PGY) level, were obtained from the general surgery training programs at three academic hospitals. Total cases logged were calculated over the pandemic period (start: beginning of residency, end: May 31st, 2020) and the control period (start: beginning of residency, end: May 31st, 2019).
Setting
Three academic tertiary hospitals (Mayo Clinic – Arizona, Mayo Clinic – Florida, and Mayo Clinic – Rochester)
Participants
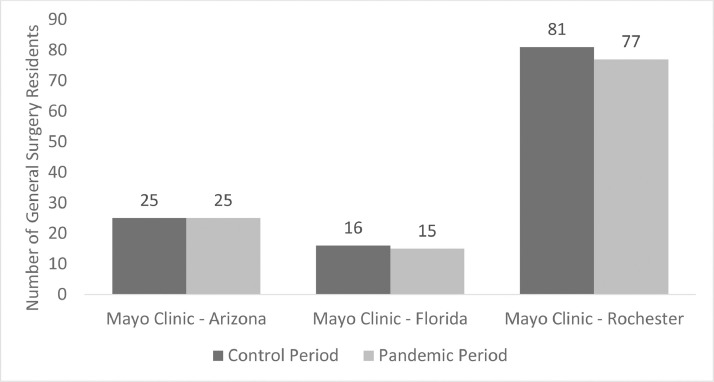
All general surgery residents at these three hospitals, including 25 residents at Mayo Clinic – Arizona in both the pandemic and control period, 16 and 15 residents at Mayo Clinic – Florida in the control and pandemic period, respectively, and 81 and 77 residents at Mayo Clinic – Rochester in the control and pandemic period, respectively.
Results
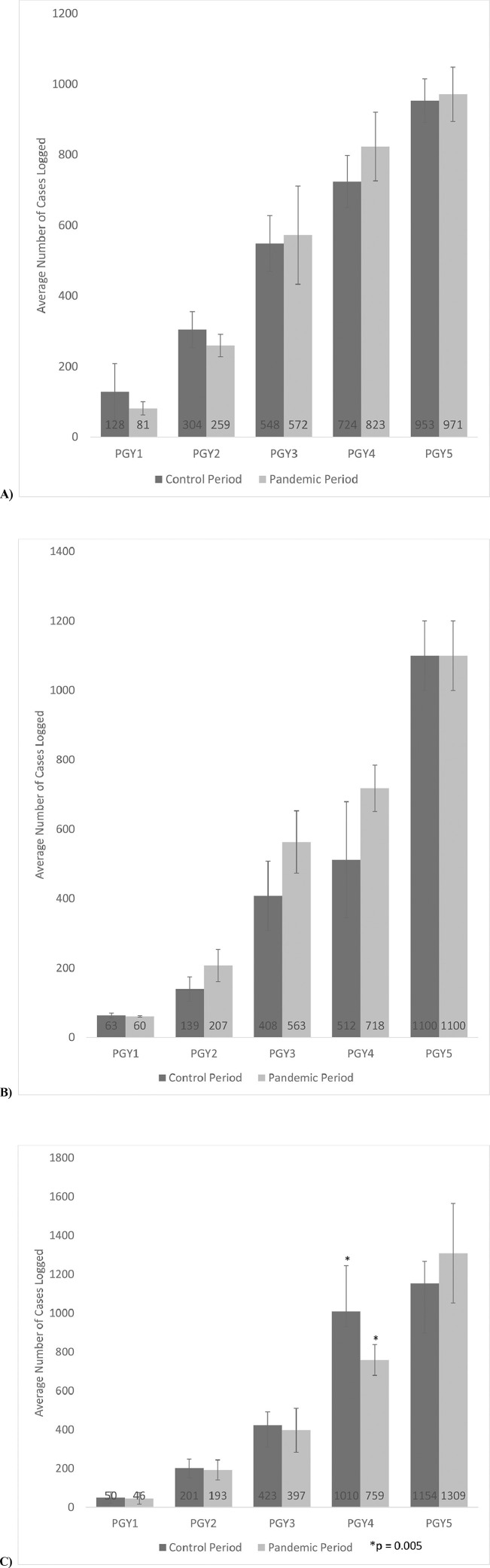
Only PGY 4 general surgery residents at Mayo Clinic – Rochester had a decrease in operative cases logged in the pandemic period (759 cases on average compared to 1010 cases, p = 0.005), with no other changes in operative cases logged noted.
Conclusions
While elective cases were postponed secondary to the COVID-19 pandemic for around 1 month in the spring of 2020, the decrease in elective cases did not greatly impact overall resident operative cases logged for residents in three general surgery residency programs.
Key Words: operative experience, COVID-19, general surgery residency, operative case log
Introduction
In the spring of 2020, governmental restrictions secondary to the novel coronavirus (COVID-19) pandemic in several regions of the United States required postponement of elective surgical operations. During this time, as described by a scoping review of the impact of COVID-19 on resident education, many residency programs across the United States restructured their call and rotation schedules, rotating a group of residents in “reserve” at home with another group of residents working clinical hours.1 This restructuring in resident rotations has been evident across the literature, with the majority of the impact reported in surgical specialties (such as orthopedic surgery, otolaryngology, neurosurgery, general surgery, cardiothoracic surgery, vascular surgery, plastic surgery, urology, and oral and maxillofacial surgery) all reporting similar restructuring across the United States. 2, 3, 4, 5, 6, 7, 8, 9, 10
Several editorials within surgical fields have hypothesized that postponement of elective cases and rotation restructuring will cause surgical residents’ operative case counts overall to decrease. Within general surgery, a nationwide survey demonstrated a subjective decrease in resident operative cases secondary to the pandemic.11 Other similar surveys in surgical specialties, including separate surveys of urology, oral and maxillofacial surgery (OMFS), neurosurgery, and thoracic surgery residents and program directors, reported a subjective decrease in trainee surgical volumes ranging from 67-83%.3 , 4 , 6 , 12 Furthermore, surgical residents, when surveyed, have associated this subjective, not objective, decrease in operating experience with a negative impact on their training.12 A systematic review reported from numerous articles that shortages in personal protective equipment, postponement of elective cases, and need for shorter operating time to reduce risk of infection has theoretically decreased the operating experience of surgical residents.13
Little is known about the objective effect of COVID-19 governmental restrictions and postponement of elective surgical cases on surgical trainees’ objective overall operative experience. The studies published to date have focused on the subjective experience of surgical trainees and program directors, in the form of survey research. This study aims to determine if there was an objective change in the total operative cases logged by general surgery residents across three general surgery residency programs after the time period affected by pandemic governmental restrictions compared to the previous year. We hypothesize that general surgery residents would have significantly decreased operative cases logged after the pandemic governmental restrictions.
MATERIAL AND METHODS
De-identified case log information was collected for all general surgery trainees at three general surgery training programs (Mayo Clinic – Arizona, Mayo Clinic – Florida, and Mayo Clinic – Rochester). Total number of cases were calculated for two periods: from the beginning of residency (July 1st) to May 31st, 2020 (pandemic period) and from the beginning of residency (July 1st) to May 31st, 2019 (control period). May 31st was selected as the period end date as this study is assessing the effects of the COVI-19 governmental restrictions on elective cases on resident cases logged and these governmental restrictions lasted until May. The start date for the “beginning of residency” was in July for each resident, but the date varied based on the resident. Average total cases logged with these two periods were calculated based on campus and post graduate year (PGY) (PGY1 to PGY5).
Quantitative variables were reported as means and standard deviations and were compared between the control and pandemic periods. Univariate analysis was performed with Student's t-test for quantitative variables. Significance was determined with α < 0.05 and all hypothesis tests were 2-sided. This study was approved by an institutional COVID-19 Research Task Force and deemed exempt by the Institutional Review Board.
RESULTS
At Mayo Clinic – Arizona, a total of 25 residents were compared in both the control period to the pandemic period. At Mayo Clinic – Florida, a total of 16 residents in the control period and 15 surgical residents in the pandemic period were compared. At Mayo Clinic – Rochester, a total of 81 residents in the control period and 77 residents in the pandemic period were compared (Fig. 1 ).
FIGURE 1.
Number of general surgery residents at each hospital during the control (2018-2019) and pandemic (2019-2020) period.
Each state had a unique timeline with respect to pandemic governmental restrictions, which mandated postponement of elective surgical cases. In Arizona, elective surgeries were postponed from March 19th until May 1st, 2020. In Florida, postponement of elective surgeries was in effect from April 1st to May 1st, 2020. In Minnesota, elective surgeries were postponed from March 19th, 2020 to May 11th, 2020. All three hospitals postponed elective surgeries pursuant to state executive order, resuming elective surgeries in a progressive, iterative fashion after executive orders were lifted.
When comparing total cases logged by general surgery residents at these three campuses between the pandemic and control periods, no difference in operative cases logged was seen when grouped by PGY level at Mayo Clinic – Arizona or Mayo Clinic – Florida (Fig. 2 ). At Mayo Clinic – Rochester, PGY 4 general surgery residents had a significant decrease in total cases logged with 759 total cases logged on average by May 2020 compared to 1010 total cases logged on average by May 2019 (p = 0.005) (Fig. 2).
FIGURE 2.
Total operative cases performed by general surgery residents. Compared total cases logged during residency for each PGY level with an end date of May 2019 to an end date of May 2020. Significant differences (p < 0.05) denoted with a *. A) Mayo Clinic – Arizona B) Mayo Clinic – Florida C) Mayo Clinic – Rochester
PGY 4 and PGY 5 general surgery residents at Mayo Clinic – Rochester were pulled from the same pool of residents to cover similar call and rotation schedules during the time affected by pandemic governmental restrictions. Based on this fact and the finding of a significant decrease in cases logged in PGY 4 and not PGY 5 residents, a post hoc analysis was performed comparing the types of cases, based on ACGME case requirements, logged during the pandemic period to the control period in PGY 4 and PGY 5 general surgery residents at Mayo Clinic – Rochester. A significant decrease in three types of cases for Mayo Clinic – Rochester PGY 4 general surgery residents was seen when comparing cases logged by May of 2020 compared to May of 2019: Alimentary Tract – Stomach, Alimentary Tract – Large Bowel, and Vascular. For stomach operations, in the pandemic period PGY 4 Mayo Clinic – Rochester residents had only logged 13 stomach cases on average (standard deviation 3.9) compared to 40 cases on average (standard deviation 7.8) for the control period (p = 0.04). For large bowel operations, in the pandemic period PGY 4 Mayo Clinic – Rochester residents had only logged 28 large bowel cases on average (standard deviation 15.2) compared to 90 cases on average (standard deviation 18.4) for the control period (p = 0.001). For vascular cases, in the pandemic period PGY 4 Mayo Clinic – Rochester residents had only logged 64 vascular cases on average (standard deviation 11.0) compared to 103 cases on average (standard deviation 28) for the control period (p = 0.0005). When comparing volumes by type of cases, there was no significant difference between the pandemic period and the control period for PGY 5 Mayo Clinic – Rochester general surgery residents.
Based on this information, we then performed a post hoc analysis comparing the number of days the PGY 4 Mayo Clinic – Rochester general surgery residents spent covering different surgical services compared to the PGY 5 residents during the months affected by the pandemic governmental restrictions. The PGY 4 and 5 residents covered surgical oncology services, emergency general surgery services, trauma surgery services, colon and rectal surgery services, the surgical intensive care unit, and “flex” coverage during this time period. PGY 4 and 5 residents covered these services fairly evenly, only the “flex” coverage differing significantly between PGY 4 and 5 residents. PGY 4 residents spent more days (5.5 days on average, standard deviation 5.7) on a flexible service coverage schedule, functioning as back-up coverage for operative cases, than PGY 5 residents (1.2 days on average, standard deviation 1.8) (p = 0.04).
DISCUSSION
A nationwide survey of general surgery residents conducted in the summer of 2020 reported that general surgery residents felt they operated significantly less, from > 4 cases a week on average to < 4 cases a week on average.11 In the same study, 42% of general surgery residents worried that they would not meet the minimum case requirements based on restructured rotations and decreased operative volume secondary to the pandemic.11 These results led to this study's hypothesis that general surgery trainee's operative cases logged would be significantly decreased after the pandemic period compared to the previous year. However, when examining three general surgery residency programs in the United States, overall operative case logs for general surgery residents remained unaffected with a significant decrease only seen in PGY 4 residents at Mayo Clinic – Rochester. That decrease in cases was only seen in vascular and alimentary tract cases. Interestingly, the PGY 4 residents had a similar call schedule and covered similar rotations to the PGY 5 residents at Mayo Clinic – Rochester, but the PGY 5 residents saw no similar pandemic-related decrease in case volume. Several possible explanations exist for this finding. As PGY 5 case volume did not change as PGY 4 case volume decreased, operative cases may have been shunted to the PGY 5 residents during the period affected by elective case cancellations. Furthermore, PGY 5 residents may have been pulled to cover more surgical oncology cases, as they are more complex, during the pandemic period, thus explaining the decrease in Alimentary Tract cases logged for PGY 4 residents. Additionally, Mayo Clinic – Rochester general surgery residents were taken off of the vascular surgery services during the period affected by governmental restrictions. Since Mayo Clinic – Rochester residents typically complete their vascular surgery rotations by the end of PGY 4 year, some PGY 4 residents may have lost the opportunity to complete their second or third vascular surgery rotation during the pandemic period, thus causing the evident decrease in vascular cases logged.
Several possible explanations exist for a lack of overwhelming decrease in operative cases logged at all three hospitals. The authors’ feel the most likely explanation is that elective surgeries were only postponed for approximately a month in all three states, therefore the lost operative opportunities in this month were not significant. Additionally, the change in resident staffing shifted surgical residents toward the emergency general surgery and trauma services. We do not expect that the operative volume on these services, which deal in surgical emergencies, would be greatly affected by the postponement of elective cases. Furthermore, services which typically perform elective cases did continue to operate on urgent patients, albeit at a lower volume, therefore allowing residents staffing those services to obtain continued operative experiences. Also, as has been subjectively reported by faculty surgeons at these hospitals, a “catch-up” effect likely existed after elective procedures restarted such that residents were operating more than they typically would when the governmental restrictions ended. Our findings may help alleviate concerns present in the literature that residents’ operative experience and competency will suffer significantly because of the COVID-19 pandemic, however further research is needed to see if no difference in operative case load is found within other surgical specialties. Further qualitative work should be done to identify why some operative case volume for some residents were affected and others were not.
This study has several limitations. This is a multi-center study, reviewing operative case logs at three separate residency programs, but the resident experience at these three programs may not be representative of all general surgery residents across the United States. Second, the individual sizes of the general surgery programs reported here, while at or above average for the nation, are still relatively small and may, therefore, be underpowered for finding a difference in cases logged within PGY level.
CONCLUSIONS
In conclusion, only PGY 4 residents at Mayo Clinic – Rochester had a significant decrease in operative cases during the pandemic, with all other general surgery residents in three residency programs unaffected. Understanding the impact of postponing elective operations secondary to COVID-19 on general surgery residents’ operative experience will be essential in anticipating any deficiencies in experience prior to resident graduation.
Footnotes
None of these authors have published, posted, or submitted any papers from the same study. This work was not and will not be presented at a conference. All authors are have approved of this manuscript and agreed to submit our findings to the Journal of Surgical Education
REFERENCES
- 1.Tolu LB, Feyissa GT, Ezeh A, Gudu W. Managing resident workforce and residency training during COVID-19 pandemic: scoping review of adaptive approaches. Adv Med Educ Pract. 2020;11:527–535. doi: 10.2147/AMEP.S262369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.An TW, Henry JK, Igboechi O, Wang P, Yerrapragada A, Lin CA, et al. How are orthopaedic surgery residencies responding to the Covid-19 pandemic? AN assessment of resident experiences in cities of major virus outbreak. J Am Acad Orthop Surg. 2020 doi: 10.5435/JAAOS-D-20-00397. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huntley RE, Ludwig DC, Dillon JK. Early effects of COVID-19 on oral and maxillofacial surgery residency training – results from a national survey. J Oral Maxillofac Surg. 2020;78:1257–1267. doi: 10.1016/j.joms.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pelargos PE, Chakraborty A, Zhao YD, Smith ZA, Dunn AI, Bauer AM. An evaluation of neurosurgical resident education and sentiment during the coronavirus disease 2019 pandemic: a north American survey. World Neurosurg. 2020;140:381–386. doi: 10.1016/j.wneu.2020.05.263. 0.1016/j.wneu.2020.05.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Latz CA, Boitano LT, Png CYM, Tanious A, Kibrik P, Conrad M, et al. Early vascular surgery response to the COVID-19 pandemic: results of a nationwide survey. J Vasc Surg. 2020 doi: 10.1016/j.jvs.2020.05.032. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coyan GN, Aranda-Michel E, Kilic A, Luketich JD, Okusanya O, Chu D, et al. The impact of COVID-19 on thoracic surgery residency programs in the US: a program director survey. J Card Surg. 2020 doi: 10.1111/jocs.14954. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marchioni D, Bisi N, Molteni G, Rubini Covid-19 and ENT practice: Our experience: ENT outpatient department, ward and operating room management during the SARS-CoV-2 pandemic. Am J Otolaryngol. 2020;41 doi: 10.1016/j.amjoto.2020.102676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.White EM, Shaughnessy MP, Esposito AC, Slade MD, Korah M, Yoo PS. Surgical Education in the time of COVID: Understanding the early response of surgical training programs to the novel coronavirus pandemic. J Surg Educ. 2020 doi: 10.1016/j.jsurg.2020.07.036. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cho DY, Yu JL, Ulm GT, Beck CM, Vedder NB, Friedrich JB. The early effects of COVID-19 on plastic surgery residency training: the University of Washington experience. Plast Reconstr Surg. 2020;146:447–454. doi: 10.1097/PRS.0000000000007072. [DOI] [PubMed] [Google Scholar]
- 10.Rosen GH, Murray KS, Greene KL, Pruthi RS, Richstone L, Mizra M. Effect of COVID-19 on urology residency training: a nationwide survey of program directors by the society of academic urologists. J Urol. 2020 doi: 10.1097/JU.0000000000001155. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 11.Aziz H, James T, Remulla D, Sher L, Genyk Y, Sullivan ME, et al. Effect of COVID-19 on surgical training across the United States: a national survey of general surgery residents. J Surg Educ. 2020 doi: 10.1016/j.jsurg.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fero KE, Weinberger JM, Lerman S, Bergman J. Perceived impact of urologic surgery training program modifications due to COVID-19 in the United States. Urology. 2020;143:62–67. doi: 10.1016/j.urology.2020.05.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dedeilia A, Sotiropoulos MG, Hanrahan JG, Janga D, Dedeilias P, Sideris M. Medical and surgical education challenges and innovations in the COVID-19 era: a systematic review. In Vivo. 2020;34(3 Suppl):1603–1611. doi: 10.21873/invivo.11950. [DOI] [PMC free article] [PubMed] [Google Scholar]