ABSTRACT
Background: Most refugees are less than 18 years and at heightened risk of common mental disorders (CMDs) relative to other youth. Limited evidence exists for psychosocial programsfor youth in low-resource settings. Early Adolescent Skills for Emotions (EASE) was developed by the World Health Organization to address this gap.
Objectives: This study tested the safety, feasibility, and trial procedures of the EASE intervention among Syrian refugee youth in preparation for a definitive randomized controlled trial (RCT).
Methods: A feasibility RCT was conducted in Amman, Jordan with Syrian children aged 10–14 years who reported psychological distress. Following community screening, youth and their caregivers were randomized to receive either the EASE intervention or enhanced treatment as usual (ETAU). EASE comprised seven group sessions teaching children coping skills, and caregivers received three group sessions to augment the youth sessions. Assessments were conducted at baseline and 1 week following the last EASE session (8 weeks following baseline). Following the trial, a qualitative process evaluation with staff and beneficiaries took place. Primary outcomes were safety and feasibility indicators, and distress was measured by the Paediatric Symptom Checklist.
Results: In November 2018, 179 children were screened; 61 (33%) met criteria for distress (34.1%), two were excluded for suicidal risk, and 59 were randomized (EASE = 33, ETAU = 26). Of those who received EASE, 26 children (79%) completed the intervention. Group attendance was high and no adverse events were reported in either arm. Psychological distress did not show signs of abating in either group over time.
Conclusion: This feasibility trial demonstrated the safety and acceptability of the intervention. Important lessons were learnt regarding entry criteria into the study and engagement of caregivers in the intervention. A fully powered randomized controlled trial will be conducted to evaluate the efficacy of EASE.
KEYWORDS: psychological intervention, adolescent, trial, mental health, psychosocial support
HIGHLIGHTS
Feasibility trial of group psychological intervention (GroupPM+) in a Syrian refugee camp in Jordan.
Sixty-four participants randomized; safety and cultural acceptance was observed.
Positive results support the readiness for a definitive RCT to test effectiveness and cost-effectiveness.
Short abstract
Antecedentes: La mayoría de los refugiados tienen menos de 18 años y corren un mayor riesgo de padecer trastornos mentales comunes (TMC) en comparación con otros jóvenes. Existe limitada evidencia de programs psicosociales para jóvenes en entornos de bajos recursos. El program denominado Early Adolescent Skills for Emotions (EASE, por sus siglas en inglés) fue desarrollado por la Organización Mundial de la Salud con el objetivo de abordar esta brecha.
Objetivos: Este estudio probó la seguridad, viabilidad y los procedimientos de la intervención EASE entre los jóvenes refugiados sirios en preparación para un ensayo controlado aleatorizado (RCT) definitivo.
Métodos: Se realizó un RCT de viabilidad en Amman, Jordania, con niños sirios de 10 a 14 años que reportaron angustia psicológica. Después de la evaluación comunitaria, los jóvenes y sus cuidadores fueron asignados al azar para recibir la intervención EASE o el tratamiento como de costumbre mejorado (ETAU por sus siglas en ingles). EASE comprendió siete sesiones grupales para enseñar a los niños habilidades de afrontamiento, y los cuidadores recibieron tres sesiones grupales para potenciar las sesiones para jóvenes. Las evaluaciones se realizaron al inicio y una semana después de la última sesión de EASE (8 semanas después del inicio). Después del ensayo, se llevó a cabo una evaluación cualitativa del proceso con el personal y los beneficiarios. Los resultados principales fueron los indicadores de seguridad y viabilidad, y la angustia se midió mediante la lista de verificación de síntomas pediátricos.
Resultados: En noviembre de 2018, se examinaron 179 niños; 61 (33%) cumplieron los criterios de angustia (34,1%), dos fueron excluidos por riesgo de suicidio y 59 fueron aleatorizados (EASE = 33, ETAU = 26). De los que recibieron EASE, 26 niños (79%) completaron la intervención. La asistencia al grupo fue alta y no se informaron eventos adversos en ninguno de los brazos. La angustia psicológica no mostró signos de disminuir a lo largo del tiempo en ninguno de los grupos.
Conclusión: Este ensayo de viabilidad demostró seguridad y aceptabilidad de la intervención. Se aprendieron importantes lecciones con respecto a los criterios de ingreso al estudio y la participación de los cuidadores en la intervención. Se llevará a cabo un ensayo controlado aleatorizado totalmente potenciado para evaluar la eficacia de EASE.
PALABRAS CLAVE: intervención psicológica, adolescente, ensayo, salud mental, apoyo psicosocial
Short abstract
背景: 大多数难民不足18岁, 并且较其他年轻人有更高风险罹患常见精神障碍 (CMD) 。对于资源匮乏环境中青少年的社会心理计划证据有限。世界卫生组织开发了旨在填补这一不足的青少年早期情感技巧 (EASE) 。
目的: 本研究考查了叙利亚青年难民进行EASE干预的安全性, 可行性和试验程序, 以准备最终随机对照试验 (RCT) 。
方法: 在约旦安曼进行了一项对有心理困扰的10至14岁叙利亚儿童的可行性RCT。在社区筛查之后, 青年及其看护人被随机分配接受EASE干预或常规强化治疗 (ETAU) 。 EASE包括七个教孩子们应对技巧的团体课程, 看护者则参加三个团体课程以加强青年人疗效。评估在基线和最后一次EASE治疗后一周 (基线后8周) 进行。试验之后, 对工作人员和受益人进行了定性过程评估。主要结果是安全性和可行性指标, 以及由儿科症状检查表测量的痛苦。
结果: 2018年11月筛查了179名儿童; 61名 (33%) 符合患病标准 (34.1%), 2名因有自杀风险被排除, 59名被随机分组 (EASE = 33, ETAU = 26) 。在接受EASE治疗的患者中, 26名儿童 (79%) 完成了干预。小组出勤率很高, 两组均未报告不良事件。两组的心理困扰都没有随时间减弱的迹象。
结论: 该可行性试验展示了干预措施的安全性和可接受性。从研究的纳入标准和护理人员参与干预方面学到了重要的经验。将进行一项强有力的随机对照试验, 以评估EASE的疗效。
关键词: 心理干预, 青少年, 试验, 心理健康, 社会心理支持
1. Introduction
There are currently more than 70 million people forcibly displaced globally, almost 30 million of whom are registered refugees (UNHCR, 2020a). More than half are under the age of 18 years and have experienced a disproportionately high number of adverse events, such as war, and acculturation difficulties (UNICEF, 2016). Unsurprisingly, this population is significantly at risk of developing common mental disorders (Charlson et al., 2019). Syrians who fled the 2011 civil war currently make up the largest population of refugees (UNHCR, 2019). More than 90% of The Syrian refugees have resettled in low- and middle-income countries (LMIC) directly bordering Syria, including Jordan, Turkey, Lebanon, and Iraq. They commonly experience poverty, unemployment, inadequate shelter, and discrimination, potentially impacting on mental health (Catani, 2018). Additionally, health systems in LMICs are commonly under-resourced to manage the mental health needs of vulnerable populations, meaning many refugees do not receive adequate treatment (World Health Organization [WHO], 2013).
A recent meta-analysis reported the prevalence of mental disorders in conflict-affected populations was greater than 20% (Charlson et al., 2019) and UNHCR reported 15–20% of Syrians will experience a mental disorder (Hassan, Ventevogel, Jefee-Bahloul, Barkil-Oteo, & Kirmayer, 2016). This highlights that effective psychological interventions are important in these contexts. There are a number of evidence-based interventions that are shown to be effective in adult refugee populations (Barbui et al., 2020). Despite efficacy, a number of these programs are difficult to implement in humanitarian contexts and have not been adequately scaled-up. Reasons for this include: (a) programtargeting a single diagnosis, (b) intensive resource requirements, (c) requirement of specialized staff, and potential mismatch with cultural norms in local settings (Eaton et al., 2011). To circumvent these barriers, efforts have led to the development of interventions allowing for task-shifting which involves training non-specialized staff to implement mental health programs under the supervision of professionals. A meta-analysis of task-shifting programs reported they have a moderate effect in the reduction of psychological distress in adults (Singla et al., 2017).
Despite advances in addressing the mental health needs of adults in LMICs, there has been a relative lack of development in evidence-based programs to address child mental health (Uppendahl, Alozkan-Sever, Cuijpers, De Vries, & Sijbrandij, 2020). The evidence for the use of psychological therapies for children in LMICs is sparse and of low quality. An individual participant data meta-analysis showed the effectiveness of psychosocial interventions for some outcomes, but the strengths of these effects were reduced in younger samples (Purgato et al., 2018). This is a particularly urgent issue as approximately 50% of The Syrian refugees are children (UNHCR, 2020b). Further, studies have reported rates of depression and PTSD symptoms in Syrian children were between 44% and 45% (Rogers-Sirin & Sirin, 2015), and almost 50% displayed clinical anxiety (Cartwright, El-Khani, Subryan, & Calam, 2015).
In recognition of the gap in good quality evidence for children and limited availability of scalable psychological interventions in adverse settings, the World Health Organization (WHO) developed Early Adolescent Skills for Emotions (EASE) targeting youth aged 10–14 years displaying symptoms of internalizing disorders (e.g. anxiety and depression) (Dawson et al., 2019). To maximize scale-up potential, resource intensiveness is diminished through the design of a group-based low-intensity, a brief psychological intervention that utilizes a task-shifting approach. Rather than focusing on specific disorders, EASE addresses symptoms across common mental disorders. Caregiver groups were incorporated into EASE, as research has shown parenting and psychological wellbeing of caregivers can influence refugee children’s mental health (Bryant et al., 2018), and caregiver sessions have shown to improve the efficacy of child-focused interventions (Fawley-King, Haine-Schlagel, Trask, Zhang, & Garland, 2013). Similar efforts to evaluate adult WHO psychological interventions, such as Problem Management Plus (PM+), have proven fruitful (Dawson et al., 2015). Three independent randomized controlled trials (RCT) have shown the efficacy of PM+ in reducing psychological distress and symptoms of common mental disorders in both individual and group formats (Bryant et al., 2017; Rahman et al., 2019, 2016).
This study presents a feasibility trial and process evaluation in preparation of a large-scale controlled trial to evaluate EASE conducted with Syrian refugee youth residing in Amman, Jordan. The aims of this trial were to (a) determine the safety and feasibility (e.g. session attendance, recruitment rate) of the EASE program in this population, (b) to test and assess trial procedures (e.g. responses to assessments), and (c) identify factors to be considered in the preparation of a definitive controlled trial (e.g. recruitment strategy, assessments) (Brown et al., 2019).
2. Methods
2.1. Setting
There are currently more than 650,000 formally registered Syrian refugees in Jordan, however, including unregistered refugees, the total estimate approximates 1.4 million (Jordan Ministry of Planning and International Cooperation, 2018). This study was conducted in two urban districts of Amman that have a high proportion of Syrians. Study approval was obtained through the Ministry of Planning and International Cooperation in Jordan, and the University of New South Wales (UNSW). The trial was registered on 26 November 2018 on the Australia New Zealand Clinical Trials Registry (ACTRN12618001917224). This study was conducted by UNSW in cooperation with the Institute for Family Health (IFH), a Jordanian non-governmental organization.
2.2. Participants
Community screening was conducted by trained assessors hired by IFH and took place in November 2018. Potential participants were identified through door-to-door visits. Families were invited to complete screening assessments if they met the following criteria: (1) Syrian refugee (regardless of registration status), (2) aged between 10 and 14 years, and (3) reside with a related caregiver who can provide legal consent. Following the screening, participants were invited to the study if they scored >5 on the Child Psychosocial Distress Screener (CPDS) (Jordans, Komproe, Ventevogel, Tol, & De Jong, 2008). The cut-off score for the CPDS was determined through a validation study conducted in Lebanon with Syrian children (not yet published). Exclusion criteria were the following: (1) unaccompanied minor; (2) minors with an unrelated caregiver; (3) significant developmental, cognitive, or neurological impairments as determined by four items from an adapted version of the 10 Questions instrument (Durkin, Hasan, & Hasan, 1995); or (4) imminent risk of suicide. Only one child, selected by the caregiver, per household was invited to participate to minimize the burden on the family and reduce the likelihood of contamination of the intervention between youth. Additionally, only one caregiver was nominated to attend caregiver sessions. Participants who met the exclusion criteria following screening were referred to specialized services within IFH or another organization according to Inter-Agency Standard Operating Procedures (Inter-Agency Working Group, 2014).
No power calculations were conducted because this study was not intended to detect significant differences between conditions. A sample of 60 children was targeted based on two arms with approximately 30 participants each. EASE groups were designed for 6–12 participants which allowed for four groups, two groups of girls (n ≈ 15), and two groups of boys (n ≈ 15).
2.3. Procedure
Assessors provided a brief explanation to the family about the study prior to taking consent from caregivers and assent from children. Following consent, participants completed screening assessments which included socio-demographic questions for both child and caregiver, the CPDS, and the WHO mhGAP imminent risk of suicide tool (WHO, 2010).
Participants who screened negative on the CPDS were contacted and provided feedback that their child was coping well. Referral options and services were provided for families expressing further concern. Those eligible, who screened positive, were invited to participate in the study. Assent/consent of child and caregiver was obtained prior to pre-assessments. Following pre-assessments, children were randomized to receive EASE or Enhanced Treatment as Usual (ETAU).
Randomization was conducted by an independent individual from the University of New South Wales using computerized software for random number generation. Participants randomized into the EASE intervention were contacted and provided session details while those in the ETAU arm were contacted to arrange a meeting.
Post-intervention assessments were completed eight-weeks following pre-assessment (1-week following the EASE intervention). To ensure blinding, assessors instructed families not to indicate whether they received EASE or ETAU.
2.4. Measures
Participants were assessed at three time points: screening, baseline, and post-intervention. Assessments were administered in Arabic using an interview format. Assessors were national staff who had previous experience conducting large-scale screening programs and interviews within Syrian communities. Prior to the trial, they received training on the psychological assessments, interviewing techniques, informed consent, data management, methods of managing participant distress and reporting adverse events. To examine the effectiveness of blinding procedures, assessors registered their guess of what condition participants were allocated.
2.4.1. Trial procedures and acceptability measures
To assess the feasibility of conducting a definitive trial, we observed recruitment and retention rates as well as the proportion of missing data. Acceptability of the EASE intervention was determined by the number of participants completing the intervention, defined as children attending at least five sessions. Lastly, safety was inferred by the number of adverse and serious adverse events.
2.4.2. Screening
The CPDS was used to assess psychological distress at screening (Jordans et al., 2008). The screener consists of seven items, five child-reported and two-caregiver reported. Responses are scored on a 3-point Likert scale (0 = never, 2 = often/a lot). To account for children not attending school, an additional option was included in one of the caregiver reported items. Scores are calculated by taking the sum of seven items, and the cut-off ≥5 was used based on feasibility work conducted in a sample of young adolescent Syrian refugees in Lebanon (not yet published). In addition to the CPDS, socio-demographics, a suicide screener (WHO, 2010), and a screener for neurological and developmental disorders were administered (Durkin et al., 1995).
2.4.3. Child reported outcomes
2.4.3.1. Primary outcome
The Paediatric Symptom Checklist (PSC-35) was used to assess child reported psychological distress at baseline and post-assessment (Jellinek et al., 1999). The PSC-35 is a 35-item instrument measuring the frequency of internalizing, externalizing, somatic, social, and academic difficulties. Scores are measured on a 3-point Likert scale (0 = never, 2 = often) and total scores are calculated by adding individual items (range: 0–70).
2.4.3.2. Secondary outcomes
The Patient Health Questionnaire, adolescent version (PHQ-A) was used to assess symptoms of depression (Johnson, Harris, Spitzer, & Williams, 2002). The PHQ-A is a 9-item symptom checklist corresponding to symptoms of depression experienced in the past week and scored on a 4-point scale (0 = not at all, 3 = nearly every day). Scores are computed by summing all items, with a maximum score of 27; higher scores indicate worse symptom severity.
The Children’s Revised Impact of Events Scale (CRIES-13) was used to assess levels of traumatic stress (Children and War Foundation, 2005). The scale consists of 13-items measuring the impact of traumatic events on three domains: intrusion (4 items), avoidance (4 items) and arousal (5 items). Items are scored on a 4-point scale (0 = not at all, 1 = rarely, 3 = sometimes, 5 = often) and the sum is taken to compute the total score (range 0–65).
Wellbeing was measured using the Warwick Edinburgh Mental Wellbeing Scale (WEBWBS), which consists of 14 statements on the child’s thoughts and feelings in the past week (Stewart-Brown et al., 2011). Scores are recorded on a 5-point scale (1 = none of the time, 5 = all of the time). Items are summed to provide a total score, ranging from 14 to 70, with higher scores indicating greater wellbeing.
For children who attended school, their perception of belonging and psychological engagement in school (psychological membership) was measured using the Psychological Sense of School Membership (PSSM) scale (Goodenow, 1993). Scores for the 18 items exploring relationships, acceptance, and rejection in school are measured on a 5-point scale (1 = not at all true, 5 = completely true). Scores were calculated by taking the mean of the items, with higher scores indicating a greater sense of belonging.
Daily functioning was measured using a scale specifically developed for the EASE study, utilizing methods outlined by Bolton (Bolton & Tang, 2002). In total, nine items were selected to be representative of daily activities that a well-functioning child would undertake. Children rated items on a 4-point scale (1 = none, 4 = often), with total higher scores correlating with greater levels of impairment.
2.4.4. Caregiver reported outcomes
The caregiver version of the PSC-35 was used to assess caregiver perceived psychological distress of their child (Jellinek et al., 1999). The number of items and scoring of the PSC-35 caregiver report is the same as the child version.
The caregiver level of psychological distress was measured using the Kessler Distress Scale (K6) (Kessler et al., 2003). The K6 has six-items relating to symptoms experienced in the past week. Levels of distress are reported on a 5-point scale (1 = all of the time, 5 = none of the time). Items are summed and higher scores indicate more distress.
Parenting behaviours were assessed using the Alabama Parenting Questionnaire (APQ-42) (Maguin, Nochajski, De Wit, & Safyer, 2016). Five parenting constructs were measured: involvement, supervision and monitoring, positive parenting, consistent discipline, and corporal punishment. Items are scored on a 5-point scale (1 = never, 5 = always) and scores are reported for each construct by summing relevant items.
2.4.5. Child traumatic events
Caregivers were asked about potentially traumatic events children might have been exposed to through a 27-item traumatic events checklist. The items were adapted in collaboration with local mental health professionals from commonly used trauma checklists (Foa, Johnson, Feeny, & Treadwell, 2001; Mollica et al., 1992; Nickerson et al., 2015; Steinberg, Brymer, Decker, & Pynoos, 2004). Items were scored dichotomously.
2.5. Interventions
2.5.1. EASE
Details of the development of EASE have been previously reported (Dawson et al., 2019). EASE was developed by the WHO based on evidence-supported strategies for the management of internalizing emotional disorders in young adolescents (aged 10–14 years). EASE was developed through a formative process consisting of a narrative review, identification of empirically supported strategies for child-mental health interventions, and extensive expert consultation. Both the child and caregiver are engaged throughout EASE with the child receiving seven 90-min group sessions and caregivers receiving three 120-min group sessions. EASE was initially adapted for Syrians residing in Lebanon and further adapted for use in Jordan. Following adaptation, focus groups were conducted with stakeholders and EASE facilitators to ensure the manual was contextually appropriate for Syrian refugees. Child sessions involve the following strategies: psychoeducation, problem-solving, stress management (diaphragmatic breathing), behavioural activation, and relapse prevention. Caregiver sessions involve psychoeducation, active listening, quality time, praise, self-care, and relapse prevention. Caregiver sessions are scheduled so that the first occurs before the third child session, the second occurs before the fifth, and the third occurs before the last child session. We considered completers of EASE to be children who attended at least five sessions.
Ten EASE facilitators were trained and were non-specialized male and female staff recruited by IFH with a range of qualifications, including MHPSS experience to tertiary qualifications in a variety of disciplines. All facilitators received 8 days of training on the EASE manual, basic counselling and group facilitation skills, and were required to complete two supervised practice cycles following the classroom-based learning. Training and weekly clinical supervision were conducted by a local supervisor (MG) who had a BSc degree, over 10 years of mental health and psychosocial counselling experience, had attended the EASE training of trainers, and received specific training on supervision and was supported by a Master supervisor; the Master supervisor (AM) was an author of EASE and provided remote supervision of the supervisor on a weekly basis during the trial. Each EASE session was conducted by two facilitators in pre-determined locations, chosen for ease of accessibility in the two urban areas. Participants received reimbursement for travel costs. To ensure treatment fidelity, the supervisor attended 10% of the sessions to assess facilitator competency and to ensure the manual was being followed accurately using a standardized checklist.
2.5.2. ETAU
Treatment as usual for Syrians experiencing psychological distress in urban communities usually consists of no intervention. For this study, the control group received ETAU, a one-on-one psychoeducation session conducted in the participant’s home. Two community health workers were recruited as ETAU facilitators. A script was drafted to standardize sessions and both caregiver and child were invited to attend. Sessions were approximately 30 minutes in duration. The primary purpose of ETAU was to provide the family with self-care strategies and nearby referral options.
2.6. Process evaluation
Following the collection of post-intervention data, a process evaluation was conducted to understand the acceptability of the intervention and to learn practical lessons for improvement in the upcoming RCT. The evaluation consisted of semi-structured individual and focus group discussions with key-informants and participants of the EASE program. Process evaluations were conducted by IFH monitoring and evaluation staff who had previous experience in conducting similar focus groups and interviews for other programs. Children and caregivers were divided by whether they completed the intervention or not, and were selected at random across genders. Both completers and non-completers of EASE were interviewed as part of the process evaluation. Two focus groups were conducted with completers; (1) children (n = 6), (2) caregivers (n = 5) and seven interviews with non-completers (children = 3, caregivers = 4). Open-ended questions regarding their experience with EASE (e.g. what were your positive/negative experiences with EASE), helpfulness (e.g. what did you think was good/bad about the materials and information you received) and impact and suggestions for improvements were asked (e.g. if you wanted to improve the program for other children/caregivers, are there any things that you would change). For non-completers, an additional open-ended question regarding the reasons they ceased EASE participation was asked. Key informants included EASE facilitators (n = 9), assessors (n = 5), and ETAU facilitators (n = 2). Responses were analysed by Arabic-speaking interpreters in association with two English-speaking investigators by summarizing the responses of each focus group. Interpretation of responses was guided by the grounded theory that proposes that a theory can be generated from qualitative responses (Corbin & Strauss, 2014). Major themes pertinent to the intervention and trial were identified during the examination of responses rather than being pre-determined or being quantified. Central to the premise of grounded theory is the potential influence of raters’ perceptions of qualitative information. To that end, interpretation of responses was conducted jointly by (a) one female adult Jordanian health workers with much experience in working with Syrian adolescents and families, (b) an adult male Arabic-speaking interpreter experienced with Syrian youth expressions, and (c) one adult, English-speaking co-author of the original EASE manual.
2.7. Statistical analysis
This feasibility study was not intended to detect significant differences between conditions. An exploratory completer analysis of variance (ANOVA) of outcome measures was conducted to observe differences between EASE and ETAU. Results of within- and between-subject F-scores were reported. The process evaluations were transcribed by IFH staff and major themes were identified throughout the focus groups and key-informant interviews. All analyses were conducted using SAS 9.4 (SAS Institute Inc, ed, 2013).
3. Results
One hundred and seventy-nine children were screened to participate, 61 of whom indicated elevated levels of psychological distress (34.1%) (Figure 1). The average CPDS score was 4.22 (SD = 2.51) for all children and 6.48 (SD = 1.74) for study participants. Two children were excluded from the study due to suicide risk and were referred to the child protection department for appropriate care. Fifty-nine children were invited to participate in the trial, all of which completed the pre-assessment and were randomized into the study. Characteristics of study participants are in Table 1. The average age of children in the study was 11.73 years (SD = 1.35), with slightly more than half being boys (n = 33, 55.93%). Children, on average, had more than three siblings and those selected to participate were among the youngest children of the caregiver. Almost all children were currently enrolled in school (93.22%). Children were exposed to more than six traumatic events on average prior to the study (SD = 3.05), with most common events being: having lived in a war zone, a serious accident, fire, or explosion, lack of food or water and danger during displacement (Table 2). No child had directly participated in armed conflict or been forced to destroy someone else’s property.
Figure 1.
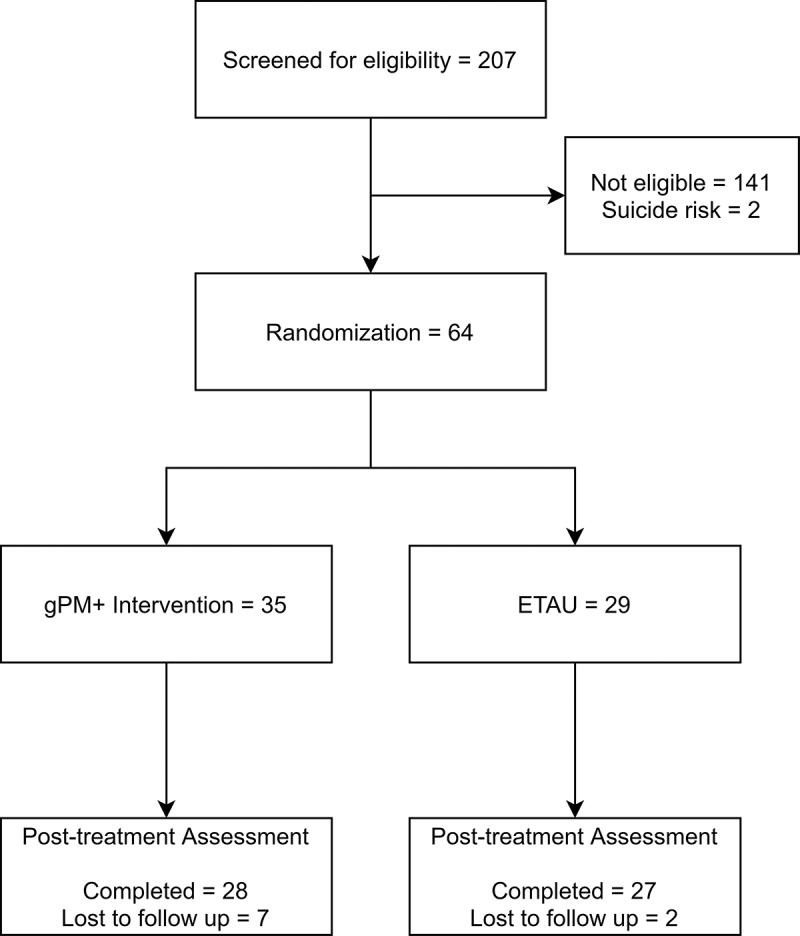
Study flowchart
Table 1.
Participant characteristics
| EASE (n = 33) | ETAU (n = 26) | Total (n = 59) | |
|---|---|---|---|
| Children | |||
| Age (mean, SD) | 11.52 (1.35) | 12.00 (1.33) | 11.73 (1.35) |
| Gender (N = Boys, %) | 18 (54.55) | 15 (57.69) | 33 (55.93) |
| Number of children (mean, SD) | 4.08 (1.67) | 4.06 (1.30) | 4.07 (1.46) |
| Birth order (mean, SD) | 2.36 (1.48) | 3.04 (2.95) | 2.66 (2.25) |
| Currently in school (N, %) | 30 (90.91) | 25 (96.15) | 55 (93.22) |
| Number of school years complete | |||
| ≤ 3 years (N, %) | 0 (0%) | 3 (11.54%) | 3 (5.08%) |
| 4 years (N, %) | 4 (12.12%) | 1 (3.85%) | 5 (8.47%) |
| 5 years (N, %) | 15 (45.45%) | 8 (30.77%) | 23 (38.98%) |
| 6 years (N, %) | 6 (18.18%) | 8 (30.77%) | 14 (23.73%) |
| 7 years (N, %) | 5 (15.15%) | 4 (15.38%) | 9 (15.25%) |
| ≥8 years (N, %) | 2 (6.06%) | 2 (7.69%) | 4 (6.78%) |
| Baseline CPDS Score (mean, SD) | 6.53 (1.54) | 6.42 (2.00) | 6.48 (1.74) |
| Suicidal thoughts (past month) (N,%) | 2 (6.1%) | 1 (3.85%) | 3 (5.1%) |
| Year arrived to Jordan | |||
| <2011 | 2 (6.06%) | 0 (0%) | 2 (3.39%) |
| 2011 | 1 (3.03%) | 0 (0%) | 1 (1.69%) |
| 2012 | 2 (6.06%) | 6 (23.08%) | 8 (13.56%) |
| 2013 | 21 (63.64%) | 17 (65.38%) | 38 (64.41%) |
| 2014 | 7 (21.21%) | 3 (11.54%) | 10 (16.95%) |
| Attended 5 EASE sessions (N, %) |
26 (78.78%) |
- |
- |
| Caregiver | |||
| Caregiver Type (N, %) | |||
| Mother | 31 (93.94) | 25 (96.15) | 56 (94.92) |
| Father | 2 (6.06) | 1 (3.85) | 3 (5.08) |
| Age (Mean, SD) | 36.94 (5.84) | 37.77 (8.27) | 37.31 (6.96) |
| Both parents living at home? (N, %) | 27 (81.82) | 21 (80.77) | 48 (81.36) |
| Mother Education (N, %) | |||
| No schooling complete | 0 (0) | 2 (7.69) | 2 (3.39) |
| Primary school | 4 (12.12) | 8 (30.77) | 12 (20.34) |
| Middle school | 22 (66.67) | 14 (53.85) | 36 (61.02) |
| High school | 6 (18.18) | 1 (3.85) | 7 (11.86) |
| Technical institute | 0 (0) | 0 (0) | 0 (0) |
| Higher education | 1(3.03) | 1 (3.85) | 2 (3.39) |
| Father Education (N, %) | |||
| No schooling complete | 2 (7.41) | 0 (0) | 2 (4.17) |
| Primary school | 8 (29.63) | 6 (28.57) | 14 (29.17) |
| Middle school | 14 (51.85) | 11 (52.38) | 25 (52.08) |
| High school | 1 (3.70) | 4 (19.05) | 5 (10.42) |
| Technical institute | 1 (3.70) | 0 (0) | 1 (2.08) |
| Higher education | 1 (3.70) | 0 (0) | 1 (2.08) |
| Housing Type (N, %) | |||
| Rented house/apartment | 32 (96.97) | 26 (100) | 58 (98.31) |
| Owned property | 1 (3.03) | 0 (0) | 1 (1.69) |
| Mother Employment (N, %) | |||
| Daily worker | 1 (3.03) | 1 (3.85) | 2 (3.39) |
| Self-employed | 0 (0) | 1 (3.85) | 1 (1.69) |
| Looking for work | 4 (12.12) | 1 (3.85) | 5 (8.47) |
| Homemaker | 28 (84.85) | 23 (88.46) | 51 (86.44) |
| Father Employment (N, %) | |||
| Full-time | 2 (7.41) | 1 (4.76) | 3 (6.25) |
| Daily worker | 17 (62.96) | 15 (71.43) | 32 (66.67) |
| Looking for work | 2 (7.41) | 3 (14.29) | 5 (10.42) |
| Not looking for work | 1 (3.70) | 1 (4.76) | 2 (4.17) |
| Homemaker | 1 (3.70) | 0 (0) | 1 (2.08) |
| Unable to work | 4 (14.81) | 1 (4.76) | 5 (10.42) |
| Household Income (N, %) | |||
| 0–299 JOD | 28 (84.85) | 25 (96.15) | 53 (89.83) |
| 300–599 JOD | 4 (12.12) | 1 (3.85) | 5 (8.47) |
| Unable to Answer | 1 (3.03) | 0 (0) | 1 (1.69) |
| Recent NGO use (N, %) | 1 (3.85) | 1 (3.03) | 2 (3.39) |
Table 2.
Children’s traumatic events
| EASE (n = 33) | ETAU (n = 26) | Total (n = 59) | |
|---|---|---|---|
| Number of Traumatic Events (Mean, SD) | 6.76 (3.16) | 5.96 (2.90) | 6.41 (3.05) |
| Number of Traumatic Events (Median, IQR) | 7 (4, 9) | 6 (4, 8) | 7 (4, 9) |
|
28 (84.8%) | 21 (80.7%) | 49 (83.1%) |
|
26 (78.8%) | 16 (61.5%) | 42 (71.2%) |
|
26 (78.8%) | 15 (57.7%) | 41 (69.5%) |
|
22 (66.7%) | 19 (73.1%) | 41 (69.5%) |
|
19 (57.6%) | 16 (61.5%) | 35 (59.3%) |
|
20 (60.6%) | 10 (38.5%) | 30 (50.8%) |
|
18 (54.5%) | 12 (46.2%) | 30 (50.8%) |
|
12 (36.4%) | 12 (46.2%) | 24 (40.7%) |
|
13 (39.4%) | 6 (23.1%) | 19 (32.2%) |
|
8 (24.2%) | 6 (23.1%) | 14 (23.7%) |
|
5 (15.2%) | 4 (15.4%) | 9 (15.3%) |
|
5 (15.2%) | 2 (7.7%) | 7 (11.9%) |
|
3 (9.1%) | 3 (11.5%) | 6 (10.1%) |
|
3 (9.1%) | 1 (3.8%) | 4 (6.8%) |
|
1 (3.0%) | 3 (11.5%) | 4 (6.8%) |
|
2 (6.1%) | 2 (7.7%) | 4 (6.8%) |
|
1 (3.0%) | 3 (11.5%) | 4 (6.8%) |
|
3 (9.4%) | 1 (3.8%) | 4 (6.8%) |
|
2 (6.1%) | 1 (3.8%) | 3 (5.1%) |
|
6 (18.1%) | 2 (7.7%) | 8 (13.6%) |
Most of the accompanying caregivers were mothers (n = 56, 94.92%), with a mean age of 37.31 years (SD = 6.96). The majority of families had both mother and father living together (81.36%). The average highest level of education for mothers (61%) and fathers (52%) was middle school. Most families resided in rental accommodation (98.31%) and households earned less than 299 USD JOD (~$420 USD) per month (89.83%). Very few individuals reported recently accessing NGO services (3.39%).
Participants were allocated into one of the five EASE groups (5–8 participants per group). Children attended an average of 5.39 sessions (out of 7) and caregivers attended an average of 1.78 sessions (out of 3). There were four children (12.12%) and nine caregivers (27.27%) who did not attend any sessions. Of the children who attended at least one EASE session (n = 29), 89.66% completed at least five sessions and were considered completers. All 26 participants randomized into ETAU were provided with a psychoeducation session. No adverse events were reported. Table 3 contains the mean pre- and post-treatment assessment scores for child and caregivers.
Table 3.
Psychological measures
| EASE (N = 33) |
ETAU (N = 26) |
Repeated Measures ANOVA |
|||||
|---|---|---|---|---|---|---|---|
| Pre-Assessment (N = 33) Mean (SD) |
Post-Assessment (N = 32) Mean (SD) |
Pre-Assessment (N = 26) Mean (SD) |
Post-Assessment (N = 25) Mean (SD) |
Time (F, p) | Randomization (F, p) | Interaction (F, p) | |
| Child | |||||||
| PSC-35 | 21.12 (10.04) | 19.56 (7.35) | 18.92 (8.39) | 16.60 (6.69) | 2.18 (0.1452) | 2.80 (0.0997) | 0.00 (0.9664) |
| Attention | 4.58 (2.06) | 5.00 (2.00) | 5.00 (2.01) | 4.08 (1.85) | 0.20 (0.6531) | 0.54 (0.4638) | 3.64 (0.0618) |
| Internalizing | 3.52 (2.46) | 2.59 (1.62) | 3.58 (2.37) | 2.84 (2.01) | 5.97 (0.0178) | 0.02 (0.8861) | 0.29 (0.5939) |
| Externalizing | 3.48 (2.66) | 3.63 (1.96) | 2.92 (1.72) | 2.80 (1.35) | 0.01 (0.9224) | 2.57 (0.1141) | 0.10 (0.7573) |
| PHQ | 6.30 (6.28) | 3.09 (3.98) | 4.38 (4.13) | 3.16 (4.40) | 6.45 (0.0139) | 1.60 (0.2110) | 2.36 (0.1305) |
| CRIES | 23.27 (18.48) | 19.97 (18.29) | 21.00 (19.04) | 16.36 (17.44) | 1.33 (0.2531) | 1.13 (0.2916) | 0.00 (0.9518) |
| Intrusion | 7.55 (6.81) | 5.59 (6.39) | 7.50 (7.81) | 5.28 (6.64) | 3.07 (0.0855) | 0.13 (0.7241) | 0.03 (0.8655) |
| Avoidance | 6.36 (5.55) | 7.47 (6.76) | 6.73 (6.69) | 5.48 (6.21) | 0.01 (0.9287) | 0.66 (0.4186) | 0.73 (0.3980) |
| Arousal | 9.36 (7.74) | 6.91 (6.18) | 6.77 (6.48) | 5.60 (5.80) | 1.93 (0.1707) | 3.45 (0.0686) | 0.69 (0.4086) |
| Daily Functioning | 6.09 (5.28) | 4.13 (2.42) | 4.77 (3.83) | 3.6 (5.05) | 2.79 (0.1006) | 1.69 (0.1991) | 0.41 (0.5241) |
| Wellbeing | 46.39 (12.28) | 49.75 (9.27) | 48.19 (11.60) | 51.48 (9.39) | 3.26 (0.0763) | 1.26 (0.2667) | 0.20 (0.6569) |
| PSSMa |
3.26 (0.58) |
2.97 (0.53) |
3.36 (0.49) |
3.34 (0.51) |
5.48 (0.0231) |
1.92 (0.1718) |
0.13 (0.7242) |
| Caregiver | |||||||
| PSC-35 | 24.24 (11.56) | 23.56 (8.66) | 20.92 (11.51) | 20.12 (7.87) | 0.06 (0.8093) | 3.88 (0.0539) | 0.31 (0.5818) |
| Attention | 5.21 (2.85) | 5.63 (2.14) | 4.77 (2.34) | 4.28 (1.88) | 0.01 (0.9294) | 4.21 (0.0449) | 0.76 (0.3878) |
| Internalizing | 3.64 (2.38) | 3.75 (2.30) | 3.69 (2.33) | 3.08 (2.06) | 0.27 (0.6022) | 0.90 (0.3457) | 0.37 (0.5480) |
| Externalizing | 4.58 (2.97) | 4.59 (2.30) | 3.46 (2.72) | 3.60 (1.91) | 0.32 (0.5736) | 5.34 (0.0246) | 0.32 (0.5736) |
| K6 | 18.21 (5.77) | 18.78 (5.34) | 17.92 (6.27) | 16.88 (5.09) | 0.08 (0.7755) | 0.57 (0.4534) | 1.12 (0.2937) |
| Alabama | |||||||
| Parental Involvement | 31.30 (7.59) | 32.91 (5.23) | 34 (7.07) | 33.15 (5.88) | 0.07 (0.7862) | 1.34 (0.2524) | 2.16 (0.1470) |
| Positive Parenting | 21.27 (5.48) | 23.38 (2.84) | 23.62 (3.31) | 23.12 (3.56) | 1.86 (0.1781) | 1.47 (0.2305) | 4.98 (0.0298) |
| Poor Monitoring | 16.18 (5.91) | 15.94 (4.48) | 14.81 (5.61) | 15.4 (3.43) | 0.03 (0.8653) | 1.45 (0.2329) | 0.40 (0.5293) |
| Inconsistent Discipline | 15.27 (3.69) | 15.97 (3.29) | 16.04 (5.45) | 15.40 (2.60) | 0.02 (0.8891) | 0.02 (0.8819) | 0.41 (0.5261) |
| Corporal Punishment | 6.00 (2.89) | 5.31 (2.09) | 7.15 (3.07) | 4.92 (2.00) | 9.39 (0.0034) | 0.23 (0.6319) | 1.87 (0.1772) |
aOnly completed by children who were currently attending school (n = 55).
The repeated-measures ANOVA found significant improvements for both groups from pre- to post-treatment on Child reported PSC-35 (internalizing domain), PHQ, PSSM, and caregiver reported APQ-42 (corporal punishment domain). There were significant between-group main effects for treatment condition for caregiver reported PSC-35 (attention and externalizing domains), such that those in the EASE arm reported lower average attention and externalizing scores. There was also a significant interaction effect in the APQ-42 (positive-parenting domain) between time and treatment, indicating that caregivers who received EASE reported greater improvement in positive parenting relative to those in the ETAU arm.
3.1. Process evaluation
Those who completed a minimum of five EASE sessions indicated they very much enjoyed sessions and learned new skills throughout the program. Caregivers of children who completed the program expressed that they noticed visible improvements in their children’s mood and ability to cope with emotions. Both children and caregivers indicated they would have preferred additional sessions of EASE for children. A similar sentiment was shared by EASE facilitators who echoed these comments based on feedback received during sessions. Additionally, EASE facilitators noted observing positive changes in the mood of children who completed the intervention. Caregivers indicated they were initially wary of the program but following the first caregiver session were much more willing for their child to attend. This sentiment was reinforced by feedback from facilitators who indicated that caregivers seemed excited following their first EASE session. Lastly, caregivers expressed they expected the intervention would be related to their child’s education and were upset to discover otherwise. ETAU facilitators reported that families responded positively to their visit and that a number of participants asked for further help in contacting resources for additional assistance. In addition, they indicated that the length of the session was adequate to go through materials and answer any questions. Non-completers indicated the greatest barriers to attendance were: (1) having multiple children at home who would be unsupervised if their child went to the EASE program as the caregiver or child attending EASE were primary caretakers and (2) financial concerns related to initial cost of transport to EASE locations. There were frustration and confusion expressed in the focus groups and interviews regarding repeated assessments; specifically, participants reported annoyance that many questions in the assessment appeared to be similar, and they felt burdened in answering these questions both before and after the program.
4. Discussion
The aims of this trial were two-fold. Firstly, to assess the safety and acceptability of the newly designed EASE program among Syrian refugees, and secondly to learn lessons on how to implement a larger definitive RCT evaluating EASE in this context.
In EASE, high attendance rates for youth were observed suggesting acceptability of the intervention. Moderate caregiver engagement was achieved. Following the intervention, caregivers provided feedback indicating that following the first caregiver session, they were more willing to allow their children to attend EASE groups. Considering this is an early feasibility study of the WHOs new EASE program, it is encouraging that so many youths remained in groups and indicated a willingness to engage in the program. The attendance by caregivers, however, suggests that caregiver engagement needs to be addressed. The obstacle caregiver attendance can be multiple in LMICs, including transport difficulties and competing demands. Caregiver and family engagement is often seen as an obstacle that needs to be addressed in child mental health treatments (Semrau et al., 2016). Based on these finding, it is recommended that the first caregiver session precedes the first child session and be adapted to enhance adherence. Additionally, the community engagement phase needs to highlight the benefits for the child and family and clarify potential misunderstandings (e.g. education).
There were no adverse events reported for children or caregivers throughout the trial, including during the screening and assessment phases. This is an important finding for the safety of the intervention in Jordan as the ‘do no harm’ principle is a core foundation of mental health interventions and humanitarian work alike (Wessells, 2009). During the screening, two children were found to be at-risk of suicide and were immediately referred to child protection services for appropriate support. Without screening, these children likely would have remained unidentified. As psychological interventions for Syrian refugee children are often scarce, it is essential that any programming attempts guarantee the safety of child participants and adequately identify the most vulnerable. Trial protocols in this instance appear to show appropriate safeguarding of children and identification of those most-at-risk. Little is known about the profile of Syrian refugees living in urban settings in Jordan, and data that is available often captures only the experiences of registered refugees. The demographic data present an interesting snapshot of the lives of Syrian youth in Jordan, irrespective of registration status. The vast majority of children participating in this trial were attending some form of school. Greater than 85% of the caregivers did not have a high-school education. Despite data suggesting high average household sizes (minimum of 6 persons in most households was reported), monthly income was considerably below the poverty line (UNICEF, 2020). Additionally, children had experienced a large number of traumas in their journeys from Syria to Jordan. Interestingly, few individuals reported recent contact with services available to them in the community which suggests that refugees in urban communities were not help-seeking.
Although the feasibility trial was not powered to detect between-group differences, it is interesting that there was no trend for the remission of distress in either EASE or ETAU conditions. This is an unusual pattern in trials to reduce psychological distress. Several possibilities exist for this observation. First, it is possible that neither EASE nor ETAU were sufficient to reduce youth distress. Second, the stressors that exist for refugee youth in Jordan may limit their capacity to experience reductions in distress; this possibility is underscored by the high prevalence of prior traumatic events and ongoing stressors regarding poverty and academic pressures. Third, it is possible that the level of distress that was used as an entry criterion to the study was too low, which resulted in 34% of the screened youth being eligible; enrolment of youth who are not significantly distressed may limit the capacity for distress to reduce over time.
4.1. Lessons learned
Numerous lessons learned can be extrapolated from the current findings. Firstly, a considerable number of persons was screened within a relatively short period of time, suggesting that the recruitment of refugees can be achieved if areas targeted have a high density of refugees. Secondly, between the screening and pre-assessment phase, no drop-outs were observed, and only two participants were lost to follow-up. Although preliminary, this trend demonstrates promising feasibility in conducting a larger definitive controlled trial and in implementing a program, such as EASE after conducting community screening. This is particularly important in settings where people are not treatment-seeking. We note that the level of acceptability in this pilot trial may be influenced by the apparent proportion of youth who were not extremely distressed; however, we also note that there was a significant proportion of the sample that did have psychological distress, which attests to the protocol being acceptable for these youths.
A third lesson learned relates to the selection of cut-off scores used during screening. Despite screening positive for distress on the CPDS, the primary outcome measure of psychological distress (PSC-35) showed mean pre-assessment scores of participants included in the EASE intervention and ETAU (21.12 and 18.92, respectively) were considerably lower than globally recognized cut-offs in both child and caregiver reported versions, consequently generating a floor-effect for observing exploratory changes in outcomes (Jellinek et al., 1999; Pagano, Cassidy, Little, Murphy, & Jellinek, 2000). This suggests the population screening for inclusion was possibly not representative of a population of youth experiencing psychological distress, which was the target group the intervention was developed for. Further, it speaks to the resilience of many Syrian refugee populations that despite the number of traumatic events reported, two-thirds of the screened population did not meet the criteria for distress. Based on the finding in this feasibility study, the screening criteria are to be adjusted for the subsequent definitive RCT study to ensure a truly distressed cohort is recruited (Brown et al., 2019). More specifically, the CPDS, which is a generic measure of distress in children, will be replaced with a more clinical measure of distress (PSC-17) as the primary screening measure (Jellinek et al., 1999).
Lastly, more clear scripts will be produced for assessment staff to guide initial interactions with families during the screening and baseline assessments. Although there were minimal dropouts during the follow-up assessments, caregivers expressed frustration as the length and repetition. During the focus groups when the purpose and reasons for repeated assessments were provided, caregivers were more understanding of the procedure. This would afford the research team to more appropriately inform participants on the program as well as addressing known misunderstandings identified during the feasibility trial (e.g. education).
4.2. Limitations
Due to the low numbers of recruited persons, we did not have sufficient power to elucidate the effects of the EASE intervention. As this was a feasibility trial, the potential to learn lessons was the primary priority. Secondly, the true effect of the EASE intervention may have been less apparent due to the low-level of psychological distress exhibited by the recruited sample as noticed by baseline assessment scores. Thirdly, the primary endpoint of the definitive RCT will be a three-month follow-up assessment. As we only examined post-intervention assessments in the feasibility trial, it was not possible to determine retention rates in the full trial.
Lastly, not all measures used in this study have been previously validated in this population. Further investigation into the validity and reliability of these measures should be undertaken.
5. Conclusion
In summary, this feasibility trial indicates that the new EASE intervention developed by the WHO appears to be safe and acceptable to both refugee children and their caregivers. Importantly, attendance at the groups was encouraging, which can be a major barrier in LMICs. The observation that youth and caregivers maintained their attendance over the course of the EASE program, with 79% of participants completing the program, reflects a high level of motivation and engagement. These factors point to the need for a fully powered controlled trial to evaluate the benefits of EASE for youth affected by psychological distress. The current findings highlighted that the initially planned screening instrument was not optimal for this setting, and so the RCT required a more stringent measure to identify youth who are distressed. This study indicates that pilot research is useful before full trials to determine optimal procedures for the identification of participants and assessment of outcomes.
Funding Statement
This work was supported by the Research for Health in Humanitarian Crises (R2HC) Programme [26889].
Consent for publication
Not applicable.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The de-identified data of this study are available at https://doi.org/10.6084/m9.figshare.13488810.
Ethics approval and consent to participate
The project has been approved by the Ministry of Planning and International Cooperation in Amman, Jordan and the University of New South Wales Human Research Ethics Committee. Informed consent/assent involved two-steps: 1) consent/assent to conduct the screening and 2) consent/assent for taking part in the EASE feasibility trial. The latter was only required for participants meeting inclusion criteria following the screening. For each step, participating respondents were asked to complete a written consent form. For illiterate participants, witnessed oral consent was collected in line with recommendations from WHO.
References
- Barbui, C., Purgato, M., Abdulmalik, J., Acarturk, C., Eaton, J., Gastaldon, C., … Thornicroft, G. (2020). Efficacy of psychosocial interventions for mental health outcomes in low-income and middle-income countries: An umbrella review. The Lancet Psychiatry, 7(2), 162–13. doi: 10.1016/S2215-0366(19)30511-5 [DOI] [PubMed] [Google Scholar]
- Bolton, P., & Tang, A. M. (2002). An alternative approach to cross-cultural function assessment. Social Psychiatry and Psychiatric Epidemiology, 37(11), 537–543. doi: 10.1007/s00127-002-0580-5 [DOI] [PubMed] [Google Scholar]
- Brown, F. L., Steen, F., Taha, K., Aoun, M., Bryant, R. A., Jordans, M. J. D., … Akhtar, A. (2019). Early Adolescent Skills for Emotions (EASE) intervention for the treatment of psychological distress in adolescents: Study protocol for randomised controlled trials in Lebanon and Jordan. Trials, 20(1), 545. doi: 10.1186/s13063-019-3654-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant, R. A., Edwards, B., Creamer, M., O’Donnell, M., Forbes, D., Felmingham, K. L., … Hadzi-Pavlovic, D. (2018). The effect of post-traumatic stress disorder on refugees’ parenting and their children’s mental health: A cohort study. Lancet Public Health, 3(5), e249–e258. doi: 10.1016/S2468-2667(18)30051-3 [DOI] [PubMed] [Google Scholar]
- Bryant, R. A., Schafer, A., Dawson, K. S., Anjuri, D., Mulili, C., Ndogoni, L., & Tsai, A. C. (2017). Effectiveness of a brief behavioural intervention on psychological distress among women with a history of gender-based violence in urban Kenya: A randomised clinical trial. PLoS Medicine, 14(8), e1002371. doi: 10.1371/journal.pmed.1002371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cartwright, K., El-Khani, A., Subryan, A., & Calam, R. (2015). Establishing the feasibility of assessing the mental health of children displaced by the Syrian conflict. Global Mental Health, 2, e8. doi: 10.1017/gmh.2015.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catani, C. (2018). Mental health of children living in war zones: A risk and protection perspective. World Psychiatry, 17(1), 104–105. doi: 10.1002/wps.20496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson, F., Van Ommeren, M., Flaxman, A., Cornett, J., Whiteford, H., & Saxena, S. (2019). New WHO prevalence estimates of mental disorders in conflict settings: A systematic review and meta-analysis. The Lancet, 394(10194), 240–248. doi: 10.1016/S0140-6736(19)30934-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Children and War Foundation . (2005). Children and War Foundation children’s revised impact of event scale (CRIES-13). Bergen: Child and War Foundation. [Google Scholar]
- Corbin, J., & Strauss, A. (2014). Basics of qualitative research: Techniques and procedures for developing grounded theory. New York: Sage publications. [Google Scholar]
- Dawson, K. S., Bryant, R. A., Harper, M., Kuowei Tay, A., Rahman, A., Schafer, A., & Van Ommeren, M. (2015). Problem Management Plus (PM+): A WHO transdiagnostic psychological intervention for common mental health problems. World Psychiatry, 14(3), 354–357. doi: 10.1002/wps.20255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson, K. S., Watts, S., Carswell, K., Shehadeh, M. H., Jordans, M. J. D., Bryant, R. A., … Van Ommeren, M. (2019). Improving access to evidence-based interventions for young adolescents: Early Adolescent Skills for Emotions (EASE). World Psychiatry, 18(1), 105–107. doi: 10.1002/wps.20594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkin, M. S., Hasan, Z. M., & Hasan, K. Z. (1995). The ten questions screen for childhood disabilities: Its uses and limitations in Pakistan. Journal of Epidemiology & Community Health, 49(4), 431–436. doi: 10.1136/jech.49.4.431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton, J., McCay, L., Semrau, M., Chatterjee, S., Baingana, F., Araya, R., … Saxena, S. (2011). Scale up of services for mental health in low-income and middle-income countries. The Lancet, 378(9802), 1592–1603. doi: 10.1016/S0140-6736(11)60891-X [DOI] [PubMed] [Google Scholar]
- Fawley-King, K., Haine-Schlagel, R., Trask, E. V., Zhang, J., & Garland, A. F. (2013). Caregiver participation in community-based mental health services for children receiving outpatient care. The Journal of Behavioral Health Services & Research, 40(2), 180–190. doi: 10.1007/s11414-012-9311-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa, E. B., Johnson, K. M., Feeny, N. C., & Treadwell, K. R. H. (2001). The child PTSD symptom scale: A preliminary examination of its psychometric properties. Journal of Clinical Child & Adolescent Psychology, 30(3), 376–384. doi: 10.1207/S15374424JCCP3003_9 [DOI] [PubMed] [Google Scholar]
- Goodenow, C. (1993). The psychological sense of school membership among adolescents: Scale development and educational correlates. Psychology in the Schools, 30(1), 79–90. doi: [DOI] [Google Scholar]
- Hassan, G., Ventevogel, P., Jefee-Bahloul, H., Barkil-Oteo, A., & Kirmayer, L. J. (2016). Mental health and psychosocial wellbeing of Syrians affected by armed conflict. Epidemiology and Psychiatric Sciences, 25(2), 129–141. doi: 10.1017/S2045796016000044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inter-Agency Working Group . (2014). Inter-agency emergency standard operating procedures for prevention of and response to gender-based violence and violence, abuse, neglect and exploitation of children in Jordan. Amman: Inter-Agency Working Group. [Google Scholar]
- Jellinek, M. S., Murphy, J. M., Little, M., Pagano, M. E., Comer, D. M., & Kelleher, K. J. (1999). Use of the pediatric symptom checklist to screen for psychosocial problems in pediatric primary care: A national feasibility study. Archives of Pediatrics & Adolescent Medicine, 153(3), 254–260. doi: 10.1001/archpedi.153.3.254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, J. G., Harris, E. S., Spitzer, R. L., & Williams, J. B. W. (2002). The patient health questionnaire for adolescents: Validation of an instrument for the assessment of mental disorders among adolescent primary care patients. Journal of Adolescent Health, 30(3), 196–204. doi: 10.1016/S1054-139X(01)00333-0 [DOI] [PubMed] [Google Scholar]
- Jordan Ministry of Planning and International Cooperation . (2018). Jordan response plan for the Syria crises, 2018-2020. Amman: Jordan Ministry of Planning and International Cooperation. [Google Scholar]
- Jordans, M. J. D., Komproe, I. H., Ventevogel, P., Tol, W. A., & De Jong, J. T. V. M. (2008). Development and validation of the child psychosocial distress screener in Burundi. American Journal of Orthopsychiatry, 78(3), 290–299. doi: 10.1037/a0014216 [DOI] [PubMed] [Google Scholar]
- Kessler, R. C., Barker, P. R., Colpe, L. J., Epstein, J. F., Gfroerer, J. C., Hiripi, E., & Zaslavsky, A. M. (2003). Screening for serious mental illness in the general population. Archives of General Psychiatry, 60(2), 184–189. doi: 10.1001/archpsyc.60.2.184 [DOI] [PubMed] [Google Scholar]
- Maguin, E., Nochajski, T. H., De Wit, D. J., & Safyer, A. (2016). Examining the validity of the adapted Alabama parenting questionnaire-parent global report version. Psychological Assessment, 28(5), 613–625. doi: 10.1037/pas0000214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollica, R. F., Caspi-yavin, Y., Bollini, P., Truong, T., Tor, S., & Lavelle, J. (1992). The Harvard trauma questionnaire. Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. The Journal of Nervous and Mental Disease, 180(2), 111–116. doi: 10.1097/00005053-199202000-00008 [DOI] [PubMed] [Google Scholar]
- Nickerson, A., Bryant, R. A., Schnyder, U., Schick, M., Mueller, J., & Morina, N. (2015). Emotion dysregulation mediates the relationship between trauma exposure, post-migration living difficulties and psychological outcomes in traumatized refugees. Journal of Affective Disorders, 173, 185–192. doi: 10.1016/j.jad.2014.10.043 [DOI] [PubMed] [Google Scholar]
- Pagano, M. E., Cassidy, L. J., Little, M., Murphy, J. M., & Jellinek, A. M. S. (2000). Identifying psychosocial dysfunction in school-age children: The pediatric symptom checklist as a self-report measure. Psychology in the Schools, 37(2), 91–106. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purgato, M., Gross, A. L., Betancourt, T., Bolton, P., Bonetto, C., Gastaldon, C., … Barbui, C. (2018). Focused psychosocial interventions for children in low-resource humanitarian settings: A systematic review and individual participant data meta-analysis. The Lancet Global Health, 6(4), e390–e400. doi: 10.1016/S2214-109X(18)30046-9 [DOI] [PubMed] [Google Scholar]
- Rahman, A., Hamdani, S. U., Awan, N. R., Bryant, R. A., Dawson, K. S., Khan, M. F., …Van Ommeren, M. (2016). Effect of a multicomponent behavioral intervention in adults impaired by psychological distress in a conflict-affected area of Pakistan: A randomized clinical trial. JAMA, 316(24), 2609–2617. doi: 10.1001/jama.2016.17165 [DOI] [PubMed] [Google Scholar]
- Rahman, A., Khan, M. N., Hamdani, S. U., Chiumento, A., Akhtar, P., Nazir, H., …and van Ommeren, M. (2019). Effectiveness of a brief group psychological intervention for women in a post-conflict setting in Pakistan: A cluster randomized controlled trial. Lancet, 393, 1733–1744. doi: 10.1016/S0140-6736(18)32343-2 [DOI] [PubMed] [Google Scholar]
- Rogers-Sirin, L., & Sirin, S. R. (2015). The educational and mental health needs of Syrian refugee children. Washington, DC: Migration Policy Institute. [Google Scholar]
- SAS Institute Inc (Ed). (2013). The SAS system for windows. Release 9.2. (Ed). Cary, NC: SAS Institute Inc. [Google Scholar]
- Semrau, M., Lempp, H., Keynejad, R., Evans-Lacko, S., Mugisha, J., Raja, S., … Hanlon, C. (2016). Service user and caregiver involvement in mental health system strengthening in low- and middle-income countries: Systematic review. BMC Health Services Research, 16(1), 79. doi: 10.1186/s12913-016-1323-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singla, D. R., Kohrt, B., Murray, L. K., Anand, A., Chorpita, B. F., & Patel, V. (2017). Psychological treatments for the world: Lessons from low- and middle-income countries. Annual Review of Clinical Psychology, 13(1), 149–181. doi: 10.1146/annurev-clinpsy-032816-045217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg, A. M., Brymer, M. J., Decker, K. B., & Pynoos, R. S. (2004). The University of California at Los Angeles post-traumatic stress disorder reaction index. Current Psychiatry Reports, 6(2), 96–100. doi: 10.1007/s11920-004-0048-2 [DOI] [PubMed] [Google Scholar]
- Stewart-Brown, S., Platt, S., Tennant, A., Maheswaran, H., Parkinson, J., Weich, S., … Clarke, A. (2011). The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): A valid and reliable tool for measuring mental well-being in diverse populations and projects. Journal of Epidemiology & Community Health, 65(Suppl 2), A38–A39. doi: 10.1136/jech.2011.143586.86 [DOI] [Google Scholar]
- UNHCR . (2019). Global trends: Forced displacement in 2018. Retrieved from https://www.unhcr.org/5d08d7ee7.pdf
- UNHCR . (2020a, April 9). Figures at a glance. Retrieved from http://www.unhcr.org/uk/figures-at-a-glance.html
- UNHCR . (2020b, August 10). Situation Syria regional refugee response. Retrieved from http://data.unhcr.org/syrianrefugees/syria.php
- UNICEF . (2016). Uprooted: The growing crisis for refugee and migrant children. Retrieved from https://www.unicef.org/reports/uprooted-growing-crisis-refugee-and-migrant-children
- UNICEF . (2020). Geographic multidimensional vulnerability analysis - Jordan. Retrieved from https://www.unicef.org/jordan/Geographic-Multidimensional-Vulnerability-Analysis
- Uppendahl, J. R., Alozkan-Sever, C., Cuijpers, P., De Vries, R., & Sijbrandij, M. (2020). Psychological and psychosocial interventions for PTSD, depression and anxiety among children and adolescents in low- and middle-income countries: A meta-analysis. Frontiers in Psychiatry, 10(933). doi: 10.3389/fpsyt.2019.00933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wessells, M. G. (2009). Do no harm: Toward contextually appropriate psychosocial support in international emergencies. American Psychologist, 64(8), 842–854. doi: 10.1037/0003-066X.64.8.842 [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) . (2010). mhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings. Geneva: Author. [PubMed] [Google Scholar]
- World Health Organization (WHO) . (2013). Building back better: Sustainable mental health care after emergencies. Geneva: WHO. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The de-identified data of this study are available at https://doi.org/10.6084/m9.figshare.13488810.


