ABSTRACT
Describe the epidemiology of tuberculosis in the last two decades (2000–2019) in the East region of Tunisia (city of Sousse). This was a descriptive retrospective analysis of notified incident cases of tuberculosis from 2000 to 2019 in Sousse Governorate, Tunisia. The data collection was done via the regional registry of tuberculosis. Stata software was used to characterize the socio-demographic and clinical profile of tuberculosis, to calculate its incidence, mortality and fatality rates and to determine predictive factors of mortality. R software was used to analyze the chronological trend of tuberculosis incidence and mortality. A total of 2606 incident cases of tuberculosis were declared from 2000 to 2019 in Sousse. The mean age was 39 ± 19 years with a sex ratio (male/female) of 1.19. Only one case was HIV positive among the total 2606 incident cases. Extra-pulmonary tuberculosis was the most recorded (1,534 cases, 58.9%). The mean annual case notification and deaths were 130 and four respectively. After adjusting for confounders, individuals with pulmonary tuberculosis were 1.9 significantly more likely to die from tuberculosis compared to those suffering from extra-pulmonary tuberculosis. There was a trend of increasing mortality with increasing age. The association was statistically significant only for those above 60 years’ old who had 12.5 times higher odds of dying compared to those below 60 years. After adjusting for age and gender, with every year there was an increase in the total incidence rate (+0.35 per 100,000) with p = 0.005 and in the extra-pulmonary incidence (+0.27 per 100,000), with p = 0.001. This study demonstrated the increasing trend of tuberculosis in Sousse, Tunisia from 2000 to 2019. The national program against tuberculosis should enhance community knowledge and centralize the national and regional epidemiological information for better epidemiological surveillance.
KEYWORDS: Tuberculosis, epidemiology, incidence, mortality, Tunisia
1. Introduction
Tuberculosis is an infectious disease caused by the bacillus Mycobacterium tuberculosis [1]. It affects the lungs usually, but it might affect other organs and sites (urinary tract, ganglionic, cutaneous, etc.) [1]. The transmission of pulmonary tuberculosis is facilitated by expelling bacteria into the air [2]. Tuberculosis has existed for centuries and remains a public health problem globally. In 2015, it was one of the leading causes of death in the world, beating HIV-AIDS as one of the leading causes of death from infectious diseases with 1.4 million deaths. In the same year, there were 10.4 million new cases and 480,000 multidrug resistance tuberculosis cases [3]. As a global response, the World Health Organization (WHO) has led global initiatives to fight tuberculosis with the recent one being the End Tuberculosis Strategy to reduce deaths by 95% and new infections by 90% between 2015 and 2035 [4].
Tunisia is no exception in terms of tuberculosis infection as the country has intermediate endemicity [5]. The efforts to fight tuberculosis started since the independence in 1956, with screening campaigns in certain areas. Then in 1978, the National Tuberculosis Control Program was created and it integrated three main interventions: mandatory BCG vaccine for school-aged children, systematic screening for those consulting Primary Healthcare Centers (PHCs) with suspected symptomatology, and finally free treatment in PHCs for all confirmed cases till complete healing [5]. From 1978 to 2018, the tuberculosis incidence rate dropped from 48.8/100 000 to 35/100 000 population [6] with the goal to ultimately achieve the WHO’s recommendations and to obtain an incidence of one case per one million populations by 2050 [5].
Despite the implementation of the national program, the burden of tuberculosis is inequitable across the country. A recent analysis of tuberculosis disease burden in Southern Tunisia revealed a recent increase in incidence in this region and suggested regional heterogeneity in infection burden [7]. The data on tuberculosis burden and other epidemiological indicators had not been analyzed for the other regions of Tunisia. Therefore, to assess the performance of control strategies, the description of the epidemiological trend and profile of the disease over time and in other geographical areas is fundamental. This research project aimed to understand the epidemiology of tuberculosis in the last two decades (2000–2019) in the city of Sousse, Tunisia.
2. Methodology
This study is an epidemiological description of tuberculosis incidence in the city of Sousse. It was based on a descriptive retrospective analysis of all notified cases of tuberculosis from 2000 to 2019 in Sousse, Tunisia. The data collection was done via the regional registry of tuberculosis which included cases notified from both private and public institutions. The regional registry of tuberculosis is an epidemiological surveillance support and it is maintained by the Regional Healthcare Service. Proper agreement for accessing and using the data from the regional registry of tuberculosis was made with the Regional Directorate of Health and the Basic Health Group of Sousse (ethical approval number 7047). For the purposes of the study, we included notified new tuberculosis cases (incident cases) independently of the site (pulmonary, extra-pulmonary). According to the National tuberculosis guidelines and in alignment with the WHO diagnosis criteria [8], the confirmation of cases was done via bacteriological or histological evidence, or alternatively, via clinical and radiological evidence and amelioration under treatment [5]. Relapsed cases were not included, to be able to calculate the incidence rate. A relapsed case of tuberculosis was defined as the occurrence of a new episode of tuberculosis in an already treated and cured patient [9]. Statistical analysis was done using STATA, except for the trend analysis, which was done in RStudio software.
We used Pearson’s Chi-Square test and the independent t-test to compare the socio-demographic and clinical profile of cases (pulmonary and extra-pulmonary). We also calculated for every year from 2000 to 2019 using the corresponding formulas. The total population size of the city of Sousse in each year was extracted from the Tunisian National Institute of Statistics [10]. We then analyzed predictors of mortality using logistic regression controlling for all variables statistically associated with the outcome at the bivariate level at p < 0.2. Finally, we analyzed the chronological trends of tuberculosis incidence and mortality rates through R software using simple and multiple linear regression adjusting for gender (expressed as the % male in each year) and age (expressed as the average age each year), adding the R-squared (R2) ranging from 0 to 1 which indicates how much of the variation of the incidence is explained by the chronological trend. Significance was set at p < 0.05 at 95% confidence interval.
3. Results
From 2000 to 2019, there were 2,606 incident cases of tuberculosis in all sites combined in Sousse Governorate. The mean age was 39 years ± 19 years with a sex ratio (male/female) of 1.19. Extra-pulmonary tuberculosis was the most recorded with 1,534 cases (58.9%). Table 1 compares basic demographic characteristics, management of cases, and patient outcome between pulmonary and extra-pulmonary tuberculosis. Table 2 showcased the mean incidence of tuberculosis in the different areas within Sousse.
Table 1.
Comparison of basic characteristics between pulmonary and extra-pulmonary tuberculosis cases in Sousse, Tunisia, 2000–2019, n (%)
| Pulmonary tuberculosis N = 1072 |
Extra-pulmonary tuberculosis N = 1534 |
Total cases N = 2606 |
p | |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Gender | ||||
| Male | 799 (74.5) | 619 (40.4) | 1,418 (54.4) | <10−3 |
| Female | 273 (25.5) | 915 (59.6) | 1,188 (45.6) | |
| Age groups | ||||
| <60 | 885 (82.6) | 1293 (84.3) | 2178 (83.6) | 0.24 |
| ≥60 | 186 (17.4) | 240 (15.7) | 426 (16.4) | |
| Management | ||||
| Patient transferred from | ||||
| Not mentioned | 670 (62.5) | 816 (53.2) | 1,486 (57.0) | <0.001 |
| Public institution | 355 (33.1) | 587 (38.3) | 942 (36.2) | |
| Private institution | 47 (4.4) | 131 (8.5) | 178 (6.8) | |
| HIV Test | ||||
| Not done | 929 (86.7) | 1,267 (82.6) | 2,196 (84.3) | – |
| Negative | 143 (13.3) | 266 (17.3) | 409 (15.7) | |
| Positive | 0 (0.0) | 1 (0.1) | 1 (0.0) | |
| Antibiotics | ||||
| Bi therapy | 34 (3.4) | 84 (6.1) | 118 (5.0) | |
| Tri therapy | 20 (2.0) | 50 (3.6) | 70 (2.9%) | 0.01 |
| Quadric therapy | 937 (94.6) | 1253 (90.3) | 2,190 (92.1) | |
| Outcome | ||||
| Loss of follow-up | 53 (5.0) | 65 (4.3) | 118 (4.6) | 0.001 |
| Cured | 964 (90.4) | 1,416 (93.7) | 2,380 (92.3) | |
| Deceased | 49 (4.6) | 31 (2.1) | 80 (3.1) | |
Table 2.
Mean incidence rate of Tuberculosis per delegation, in Sousse, Tunisia, from 2000 to 2019
| Delegation | Population in 2009 | Frequency N | Incidence/ 1000 | 95% Confidence Interval |
|---|---|---|---|---|
| Prison | 1178 | 29 | 246.18 | [243.24, 249.12] |
| Sousse medina | 29,271 | 541 | 184.82 | [182.16, 187.48] |
| Hamam sousse | 38,474 | 207 | 53.80 | [52.36, 55.24] |
| Sousse Riadh | 79,206 | 421 | 53.15 | [51.72, 54.58] |
| Hergla | 8309 | 43 | 51.75 | [50.35, 53.15] |
| Kalaa sghira | 31,342 | 131 | 41.80 | [40.53, 43.07] |
| Enfidha | 45,607 | 158 | 34.64 | [33.49, 35.79] |
| Sidi abdelhamid | 53,783 | 174 | 32.35 | [31.24, 33.46] |
| Jawhra | 73,286 | 235 | 32.07 | [30.96, 33.18] |
| Kalaa kbira | 53,692 | 172 | 32.03 | [30.92, 33.14] |
| Sidi bou ali | 18,596 | 58 | 31.19 | [30.10, 32.28] |
| Kondar | 12,245 | 35 | 28.58 | [27.54, 29.62] |
| Akouda | 28,244 | 78 | 27.62 | [26.59, 28.65] |
| Msaken | 90,168 | 229 | 25.40 | [24.41, 26.39] |
| Bouficha | 25,161 | 51 | 20.27 | [19.39, 21.15] |
| Sidi el heni | 11,871 | 21 | 17.69 | [16.87, 18.51] |
| Others | 23 |
Over the study period, a mean number of 130.2 tuberculosis cases and 4 deaths were reported per year (Table 3) with a mean tuberculosis incidence rate equal to 21.23, 95%CI [20.33, 22.14] (per 100,000 population). A total of 80 tuberculosis death cases were reported over the 20 years of the study in Sousse governorate (Table 4). After adjusting for confounders, individuals with pulmonary tuberculosis were 1.9 significantly more likely to die from tuberculosis compared to those suffering from extra-pulmonary tuberculosis. There was a trend of increasing mortality with older age group. The association was statistically significant for those above 60 years’ old who had 12.5 times higher odds of dying compared to those below 60 years old (95%CI [7.5, 21.0]) (Table 4).
Table 3.
Tuberculosis incidence and mortality rates in Sousse Governorate by year from 2000 to 2019
| Year | Total population | Incident cases | Death cases | Fatality rate (%) |
Incidence rate / 100,000 |
Mortality rate /100,000 |
|---|---|---|---|---|---|---|
| 2000 | 492,500 | 99 | 2 | 2 [1.72, 2.28] | 20.10 [19.22, 20.98] | 0.41 [0.28, 0.53] |
| 2001 | 501,200 | 87 | 3 | 3 [2.66, 3.34] | 17.36 [16.54, 18.17] | 0.60 [0.45, 0.75] |
| 2002 | 510,100 | 87 | 3 | 3 [2.66, 3.34] | 17.06 [16.25, 17.86] | 0.59 [0.44, 0.74] |
| 2003 | 536,300 | 96 | 9 | 9 [8.41, 9.59] | 17.90 [17.07, 18.73] | 1.68 [1.42, 1.93] |
| 2004 | 545,800 | 82 | 3 | 4 [3.61, 4.39] | 15.02 [14.26, 15.78] | 0.55 [0.40, 0.69] |
| 2005 | 557,100 | 131 | 8 | 6 [5.52, 6.48] | 23.51 [22.57, 24.46] | 1.44 [1.20, 1.67] |
| 2006 | 568,200 | 110 | 5 | 5 [4.56, 5.44] | 19.36 [18.50, 20.22] | 0.88 [0.70, 1.06] |
| 2007 | 579,000 | 114 | 7 | 6 [5.52, 6.48] | 19.69 [18.82, 20.56] | 1.21 [0.99, 1.42] |
| 2008 | 590,100 | 146 | 4 | 3 [2.66, 3.34] | 24.74 [23.77, 25.72] | 0.68 [0.52, 0.84] |
| 2009 | 608,624 | 138 | 6 | 4 [3.61, 4.39] | 22.67 [21.74, 23.61] | 0.99 [0.79, 1.18] |
| 2010 | 621,778 | 159 | 4 | 3 [2.66, 3.34] | 25.57 [24.58, 26.56] | 0.64 [0.49, 0.80] |
| 2011 | 600,382 | 124 | 3 | 2 [1.72, 2.28] | 20.65 [19.76, 21.54] | 0.50 [0.36, 0.64] |
| 2012 | 648,706 | 120 | 2 | 2 [1.72, 2.28] | 18.50 [17.66, 19.34] | 0.31 [0.20, 0.42] |
| 2013 | 662,487 | 154 | 4 | 3 [2.66, 3.34] | 23.25 [22.30, 24.19] | 0.60 [0.45, 0.76] |
| 2014 | 677,501 | 140 | 3 | 2 [1.72, 2.28] | 20.66 [19.77, 21.55] | 0.44 [0.31, 0.57] |
| 2015 | 690,715 | 155 | 3 | 2 [1.72, 2.28] | 22.44 [21.51, 23.37] | 0.43 [0.31, 0.56] |
| 2016 | 703,646 | 187 | 5 | 3 [2.66, 3.34] | 26.58 [25.57, 27.59] | 0.71 [0.55, 0.88] |
| 2017 | 715,744 | 143 | 1 | 1 [0.80, 1.20] | 19.98 [19.10, 20.85] | 0.14 [0.07, 0.21] |
| 2018 | 726,867 | 161 | 3 | 2 [1.72, 2.28] | 22.15 [21.23, 23.07] | 0.41 [0.29, 0.54] |
| 2019 | 737,027 | 173 | 2 | 1 [0.80, 1.20] | 23.47 [22.52, 24.42] | 0.27 [0.17, 0.37] |
| 2000–2019 | 2606 | 80 | 3 [2.66, 3.34] | 20.03 [20.14, 21.93] | 0.67 [0.52, 0.83] |
Table 4.
Predictive factors of Tuberculosis deaths, in Sousse Governorate, Tunisia, from 2000 to 2019, n (%)
| Cured N = 2380 |
Dead N = 80 |
p | Crude OR 95%CI | Adjusted OR 95%CI | |
|---|---|---|---|---|---|
| Gender | |||||
| female | 1,105 (97.4) | 29 (2.6) | - | - | |
| Male | 1,275 (96.2) | 51 (3.8) | 0.07 | 1.5 [0.4, 1.] | 1.5 [0.9, 2.4] |
| Age groups | |||||
| <60 | 2029 (98.7) | 26 (1.3) | |||
| ≥60 | 349 (86.6) | 54 (13.4) | <0.001 | 12.1 [7.5, 19.5] | 12.5 [7.5, 21.0] |
| Tuberculosis site | |||||
| Extra-pulmonary | 1,416 (97.9) | 31 (2.1) | - | - | |
| Pulmonary | 964 (95.2) | 49 (4.8) | <0.001 | 2.3 [1.5, 3.7] | 1.9 [1.1, 3.3] |
| Antibiotherapy | |||||
| Two antibiotics | 103 (96.3) | 4 (3.7) | - | - | |
| Three antibiotics | 63 (92.6) | 5 (7.3) | 0.30 | 2.0 [0.5, 7.9] | 2.9 [0.7, 12.4] |
| Four antibiotics | 2,004 (97.0) | 62 (3.0) | 0.67 | 0.8 [0.3, 2.2] | 0.8 [0.3, 2.4] |
The trend of the total tuberculosis incidence (all sites combined) from 2000 to 2019 was increasing (Figure 1A). Each year, there was an increase in the total tuberculosis incidence rate by 0.27 per 100,000, and it was significant with p = 0.01, and in extra-pulmonary incidence rate by +0.25 per 100,000 with p < 0.001 (Figure 1B). The increase in pulmonary tuberculosis incidence was much smaller and not significant (Figure 1C) (+0.02 per 100,000, p = 0.7).
Figure 1.
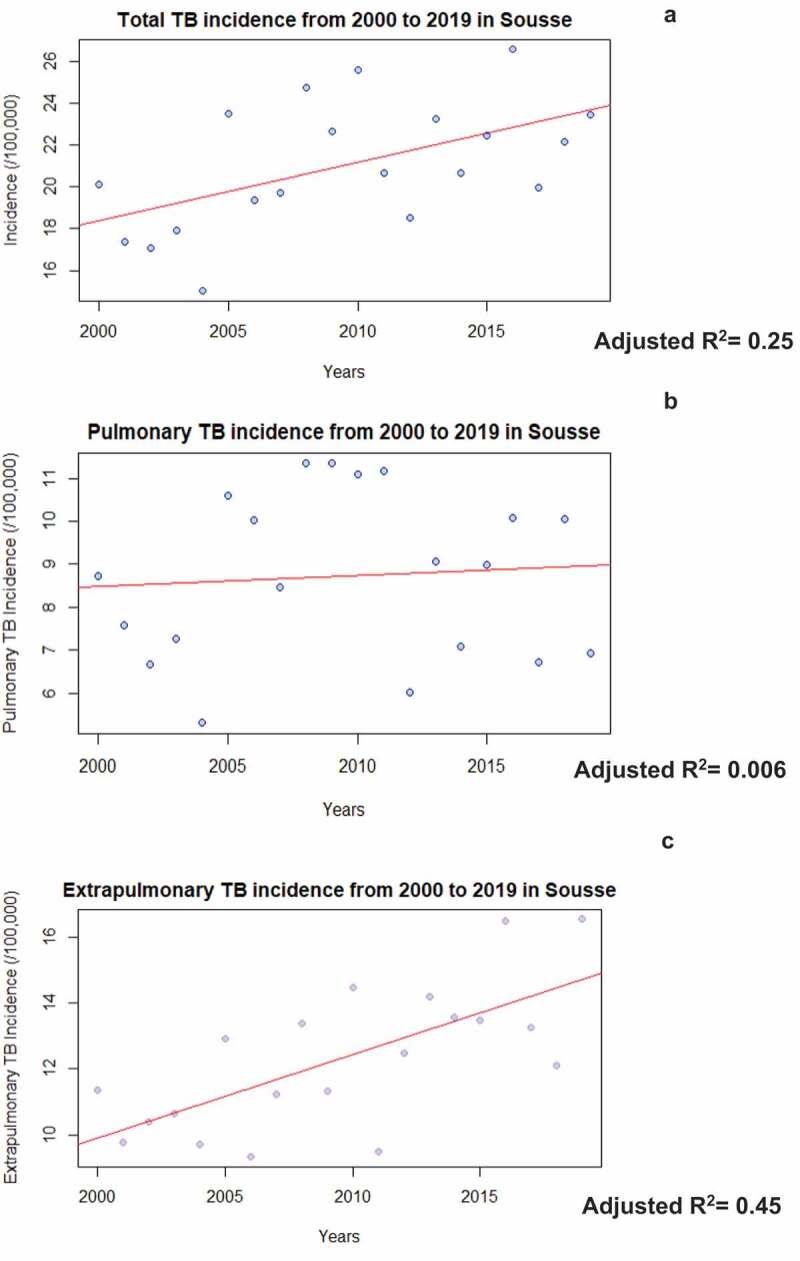
Incidence Trend of tuberculosis (TB) from 2000 to 2019 in Sousse Governorate, Tunisia
When adjusting for age and gender, every year there was an increase in the total incidence rate by +0.35 per 100,000 and it was significant (p = 0.005, and adjusted R2 = 0.29) and the increase in the extra-pulmonary incidence (+0.27 per 100,000) remained significant (p = 0.001 and adjusted R2 = 0.40).
There was a decreasing mortality rate trend (−0.03 per 100,000 each year), and it was statistically significant with p = 0.02 (Figure 2). However, it was not significant when adjusting for age and gender (p = 0.08).
Figure 2.
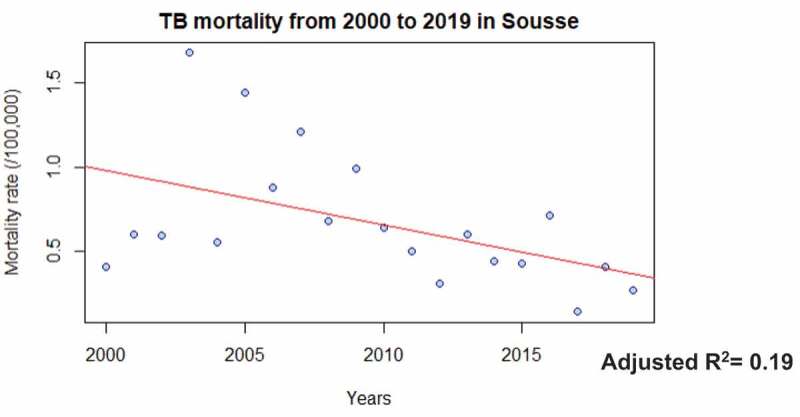
Mortality rate trend of tuberculosis (TB) from 2000 to 2019, in Sousse governorate, Tunisia
4. Discussion
In the early 90s, the WHO declared tuberculosis as a global health emergency, and since then, prominent efforts to address it have been put in place. Currently ending tuberculosis is a target under the Sustainable Development Goals (target 3.3). The global incidence of tuberculosis is decreasing globally by 2% per year with a cumulative reduction of 9% between 2015 and 2019 [11]. The End Tuberculosis Strategy defines targets for reduction in tuberculosis cases (80% reduction in the tuberculosis incidence rate) and deaths (90% reduction in the number of tuberculosis deaths) [11]. In Tunisia, efforts to fight tuberculosis started more than 60 years ago and the incidence has decreased from 48.8 to 22.5 per 100,000 habitants from 1978 to 2007 [12] and then increased to 35 per 100,000 in 2018 [6].
5. Increasing trend of Tuberculosis
Our study showcased a linear increasing trend of tuberculosis incidence over the past 20 years (from 2000 till 2019) with a slope equal to +0.35 per year when adjusting for age and gender. This incidence found in our study, even though below the national rate, remains above the threshold set by the office of the WHO Eastern Mediterranean to classify countries of low incidence which is 20/100,000 population [12]. The increasing trend of tuberculosis can be the result of socio-economic deprivation, which may lead to poor living conditions, overcrowding, and malnutrition especially in prisons where there is a higher incidence of tuberculosis compared to the general population [13–16] which was objective also in our study. These factors increase tuberculosis exposure risk, and individual vulnerability. According to the literature, unhealthy lifestyle habits are also implicated in the genesis of tuberculosis, for example, active or passive tobacco smoking are risk factors for latent tuberculosis cases and enhance the progression to active disease, same for alcohol use [17,18]. Moreover, the lack of social support can lead to non-compliance and poor treatment outcomes [19]. Also, demographic factors characterized by aging can lead to an increase in tuberculosis incidence. A study in China found that tuberculosis incidence increased for those above 45 years old [20]. Other studies have associated this increase to the degradation of the immune system over time due to other comorbidities or drugs [21–23]. Among these comorbidities, diabetes has been linked to increased risks and adverse tuberculosis treatment outcomes [18,24,25]. Environmental factors have been also incriminated in the tuberculosis genesis such as air pollution [26] and seasonality [14,15,27]. In Sousse, Tunisia, the tuberculosis incidence increasing trend can also be explained by the above-described factors, as the population is aging [28], and there is a quite high prevalence of smoking and diabetes [17,29–31]. Other studies done in Tunisia, have also have objectified this rise in incidence whether in the South of Tunisia [7] and Monastir governorate [32].
6. Rise of Extra pulmonary cases
Our results showed a much higher proportion of extra-pulmonary tuberculosis with 58.9% of the total tuberculosis cases from 2000 to 2019 of which the majority was females (59.6%) and with a younger age compared to pulmonary cases. The predominant extra-pulmonary sites were lymph nodes, pleura, and digestive system. This increase in extra-pulmonary cases could be the results of a multitude and complex risk factors such as immunological factors (HIV infection), socio-demographic factors (female sex, younger age, and non-white race) comorbidities, and lifestyle behaviors (diabetes, liver diseases, and consumption of unpasteurized raw milk) and genetic factors [33–38] and also the evolution and amelioration of diagnostic tools [39]. Worldwide, out of the 6.3 million new cases of tuberculosis recognized in 2017, 16% were extra-pulmonary with an incidence rate ranging from 8% in the Western Pacific Region to 24% in the Eastern Mediterranean Region [24]. Extra-pulmonary cases represented 20% of all tuberculosis cases in Korea [40], 33% in China [24], 49% in both Morocco and Ethiopia [37,39] and reached 51% in India [41]. In the European Union and the European Economic Area, more than 150,000 cases of extra-pulmonary tuberculosis were declared in the 30 member states from 2002 to 2011 which accounted for 19.3% of all cases [42]. In Tunisia, the proportion of extra-pulmonary tuberculosis exceeded 50%, both in Monastir governorate (51%) [43] and in the south region of Tunisia (68%) [7]. This increase in tuberculosis incidence in Tunisia may be partially due to sociodemographic factors, comorbidities, and especially lifestyle factors dominated by the consumption of unpasteurized milk [5,44,45]. However, it can be the result of progress made in screening-diagnosis tools and the improvement of surveillance, policy, and programming of tuberculosis management.
The Tunisian efforts to fight tuberculosis started after the independence, and the latest version of the National Guide was published in 2018 [46]. This edition is, still, more oriented toward pulmonary tuberculosis which may be due to the contagious nature of pulmonary tuberculosis compared to the extra-pulmonary form. Currently, there is a need to be more, or at least, equally focused on both pulmonary and extra-pulmonary tuberculosis. Incidence of tuberculosis were found to be much higher in prison settings which need to be addressed by the public health authorities. Moreover, there is a national necessity to enhance the community’s knowledge about tuberculosis and especially about the extra-pulmonary form. Ben Salah et al. [47] highlighted the knowledge disparity and heterogeneity. They stated that coughing was the main alarming symptom for people, with a variety between regions, educational status, and gender. They highlighted the importance of mass media such as televisions and radios as they were the main two sources of information stated by the population of the study [47]. Also, it is time to digitalize and computerize the regional and national registry of tuberculosis. This will allow the centralization of both national and regional epidemiological information at the ministerial level, thus, better knowledge about the distribution of important epidemiological parameters using geographical information systems and per consequence identifying high-risk zones and intervene effectively and efficiently.
Supplementary Material
Acknowledgments
This study was done as part of my Master of Public Health in the Faculty of Health Science, American University of Beirut. This Master was sponsored by the World Health Organization under the TDR scholarship. I would like to thank My Advisor Dr. Ghina Mumtaz and my Second Reader Dr. Rima Nakkash for their multiple corrections, reviews and inputs.
Funding Statement
The author(s) reported there is no funding associated with the work featured in this article.
Supplemental data
Supplemental data for this article can be accessed here.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- [1].Pai M, Behr MA, Dowdy D, et al. Tuberculosis. Nat Rev Dis Primers. 2016;27(2):16076. [DOI] [PubMed] [Google Scholar]
- [2].Churchyard G, Kim P, Shah NS, et al. What We Know About Tuberculosis Transmission: an Overview. J Infect Dis. 2017;03(216(suppl_6)):S629–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].WHO . Global tuberculosis report 2016 [Internet]. 2016. Available from: https://apps.who.int/iris/handle/10665/191102
- [4].WHO . WHO End TB Strategy [Internet]. WHO. World Health Organization; 2015. [cited 2020 Oct 26]. Available from: http://www.who.int/tb/post2015_strategy/en/
- [5].MOH . Plan stratégique National. 2008;28.
- [6].World Bank . Incidence of tuberculosis (per 100,000 people), Tunisia [Internet]. the World Bank Data. 2018. [cited 2020 Oct 23]. Available from: https://data.worldbank.org/indicator/SH.TBS.INCD?locations=TN
- [7].Ben Ayed H, Koubaa M, Gargouri L, et al. Epidemiology and disease burden of tuberculosis in south of Tunisia over a 22-year period: current trends and future projections. PLoS One [Internet]. 2019 Jul 24 [cited 2020. Oct 11];14(7). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6656341/ e0212853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].WHO . WHO | implementing tuberculosis diagnostics: a policy framework [Internet]. WHO. World Health Organization; 2015. [cited 2021 Mar 31]. Available from: http://www.who.int/tb/publications/implementing_TB_diagnostics/en/
- [9].Mjid M, Hedhli A, Zakhma M, et al. Profil clinique et microbiologique des patients en situation de rechute tuberculeuse en Tunisie. Rev Pneumol Clin. 2018 Apr 1 74(2):76–80. [DOI] [PubMed] [Google Scholar]
- [10].Statistiques Tunisie . Tunisia Data Portal, Data Analysis [Internet]. 2020. [cited 2021 Feb 14]. Available from: http://dataportal.ins.tn/en/DataAnalysis?6KCQ6cWoYkmJzTvjiuTsg
- [11].WHO . Tuberculosis [Internet]. 2021. [cited 2021 Apr 20]. Available from: https://www.who.int/news-room/fact-sheets/detail/tuberculosis
- [12].Mohamed KC, Hédia B, Sassia D, et al. Evaluation de l’efficacite´ du programme tunisien de lutte antituberculeuse. Sante. 2010. Apr 1;20(2):87–92. [DOI] [PubMed] [Google Scholar]
- [13].Bhatti N, Law MR, Morris JK, et al. Increasing incidence of tuberculosis in England and Wales: a study of the likely causes. BMJ. 1995. Apr 15;310(6985):967–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Bonell A, Contamin L, Thai PQ, et al. Does sunlight drive seasonality of TB in Vietnam? A retrospective environmental ecological study of tuberculosis seasonality in Vietnam from 2010 to 2015. BMC Infect Dis. 2020. Feb 28;20(1):184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Butt MF, Younis S, Wu Z, et al. The relationship between seasonality, latitude and tuberculosis notifications in Pakistan. BMC Infect Dis. 2021. Feb 25;21(1):210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Velen K, Charalambous S.. Tuberculosis in prisons: an unintended sentence? Lancet Public Health. 2021. May 1;6(5):e263–4. [DOI] [PubMed] [Google Scholar]
- [17].Bates MN. Risk of Tuberculosis From Exposure to Tobacco Smoke: a Systematic Review and Meta-analysis. Arch Intern Med. 2007. Feb 26;167(4):335. [DOI] [PubMed] [Google Scholar]
- [18].Millet J-P, Moreno A, Fina L, et al. Factors that influence current tuberculosis epidemiology. Eur Spine J. 2013. Jun;22(Suppl 4):539–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Duarte R, Lönnroth K, Carvalho C, et al. Tuberculosis, social determinants and co-morbidities (including HIV). Pulmonol. 2018. Mar 1;24(2):115–119. [DOI] [PubMed] [Google Scholar]
- [20].Zhu M, Han G, Takiff HE, et al. Times series analysis of age-specific tuberculosis at a rapid developing region in China, 2011–2016. Sci Rep. 2018. Jun 7;8(1):8727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ku -C-C, Dodd PJ, Tizzoni M. Forecasting the impact of population ageing on tuberculosis incidence. PLOS ONE. 2019. Sep 24;14(9):e0222937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Negin J, Abimbola S, Marais BJ. Tuberculosis among older adults – time to take notice. Inter J Infect Dis. 2015. Mar;1(32):135–137. [DOI] [PubMed] [Google Scholar]
- [23].Thomas TY, Rajagopalan S. Tuberculosis and Aging: a Global Health Problem. Clinl Infect Dis. 2001. Oct 1;33(7):1034–1039. [DOI] [PubMed] [Google Scholar]
- [24].Pang Y, An J, Shu W, et al. Epidemiology of Extrapulmonary Tuberculosis among Inpatients, China, 2008–2017. Emerg Infect Dis. 2019. Mar;25(3):457–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Silva DR, Muñoz-Torrico M, Duarte R, et al. Risk factors for tuberculosis: diabetes, smoking, alcohol use, and the use of other drugs. J Bras Pneumol. 2018. Apr;44(2):145–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Yang J, Zhang M, Chen Y, et al. A study on the relationship between air pollution and pulmonary tuberculosis based on the general additive model in Wulumuqi, China. Inter J Infect Dis. 2020. Jul;1(96):42–47. [DOI] [PubMed] [Google Scholar]
- [27].Parrinello CM, Crossa A, Harris TG. Seasonality of tuberculosis in New York City, 1990-2007. Int J Tuberc Lung Dis. 2012. Jan;16(1):32–37. [DOI] [PubMed] [Google Scholar]
- [28].Ben Salem K, Ben Abdelaziz A. The Maghreb demographic transition: Tunisia case study. Tunis Med. 2018. Nov;96(10–11):754–759. [PubMed] [Google Scholar]
- [29].Ben Romdhane H, Ali SB, Aissi W, et al. Prevalence of diabetes in Northern African countries: the case of Tunisia. BMC Public Health. 2014. Jan;28(14):86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Maoui A, Bouzid K, Ben Abdelaziz A, et al. Epidemiology of Type 2 Diabetes in the Greater Maghreb. Example of Tunisia. Systematic review of the literature. Tunis Med. 2019. Feb;97(2):286–295. [PubMed] [Google Scholar]
- [31].Sriha Belguith A, Bouanene I, Elmhamdi S, et al. [Nicotine dependance and carbon monoxide intoxication among adult smokers]. Tunis Med. 2015. Apr;93(4):231–236. [PubMed] [Google Scholar]
- [32].Bennasrallah C, Kacem M, Dhouib W, et al. BCG vaccination and tuberculosis prevention: a forty years cohort study, Monastir, Tunisia. PLOS ONE. 2019;14(8):e0219991. août. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Al-Ghafli H, Varghese B, Enani M, et al. Demographic risk factors for extra-pulmonary tuberculosis among adolescents and adults in Saudi Arabia. PLOS ONE. 2019. Mar 27;14(3):e0213846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Ayed HB. Extrapulmonary Tuberculosis: update on the Epidemiology, Risk Factors and Prevention Strategies. 2018; 6.
- [35].Ben-Selma W, Ben-Abderrahmen Y, Boukadida J, et al. IL-10R1 S138G loss-of-function polymorphism is associated with extrapulmonary tuberculosis risk development in Tunisia. Mol Biol Rep. 2012. Jan 1;39(1):51–56. [DOI] [PubMed] [Google Scholar]
- [36].Qian X, Nguyen DT, Lyu J, et al. Risk factors for extrapulmonary dissemination of tuberculosis and associated mortality during treatment for extrapulmonary tuberculosis. Emerg Microbes Infect [Internet]. 2018. Jun 6 [cited 2021 Apr 21];7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5988830/ 1 1–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Sbayi A, Arfaoui A, Janah H, et al. Epidemiological characteristics and some risk factors of extrapulmonary tuberculosis in Larache, Morocco. Pan Afr Med J [Internet]. 2020. Aug 31 [cited 2021 Apr 20];36(381). Available from: https://www.panafrican-med-journal.com/content/article/36/381/full [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Yang Z, Kong Y, Wilson F, et al. Identification of Risk Factors for Extrapulmonary Tuberculosis. Clinl Infect Dis. 2004. Jan 15;38(2):199–205. [DOI] [PubMed] [Google Scholar]
- [39].Arega B, Mersha A, Minda A, et al. Epidemiology and the diagnostic challenge of extra-pulmonary tuberculosis in a teaching hospital in Ethiopia. PLOS ONE. 2020;15(12):e0243945. déc [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Lee JY. Diagnosis and Treatment of Extrapulmonary Tuberculosis. Tuberc Respir Dis (Seoul). 2015. Apr;78(2):47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Prakasha SR, Suresh G, D’sa IP, et al. Mapping the Pattern and Trends of Extrapulmonary Tuberculosis. J Glob Infect Dis. 2013;5(2):54–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Kulchavenya E. Extrapulmonary tuberculosis: are statistical reports accurate? Therapeutic Advances in Infection. 2014; Apr,;1 2(2):61–70. doi [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Ben Nasrallah C, Kacem M, Grira S, et al. Extra-pulmonary tuberculosis incidence, trends and predictions in Monastir, Tunisia (2000-2030). Eur J Public HealthInternet]. 2020. Sep 1 [cited 2021 Apr 20];30(ckaa166.1342). Available from 10.1093/eurpub/ckaa166.1342 [DOI] [Google Scholar]
- [44].Dejoui N. Lait cru: le ministère de la Santé met en garde [Internet]. L’Economiste Maghrébin. 2015. [cited 2021 May 7]. Available from: https://www.leconomistemaghrebin.com/2015/06/19/lait-cru-le-ministere-de-la-sante-met-en-garde/
- [45].Tritar-Cherif F, Daghfous H. [Lymph node tuberculosis management]. Tunis Med. 2014. Jan;92(1):111–113. [PubMed] [Google Scholar]
- [46].CCM . Le programme National de Lutte contre la Tuberculose [Internet]. CCM TUNISIE. 2018. [cited 2020 Oct 4]. Available from: https://www.ccmtunisie.org.tn/programmes-nationaux/le-programme-national-de-lutte-contre-la-tuberculose
- [47].Ben-Salah N, Snene H, Bejar D, et al. Évaluation des connaissances attitudes et pratiques par rapport à la tuberculose selon les caractéristiques sociodémographiques en Tunisie. Rev Mal Respir. 2018. Jan 1;35:A229. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


