ABSTRACT
Background: Parents of children with intellectual and neurodevelopmental disorders (IDD) often experience traumatic events in the care of their children. This leads to comparatively high numbers of mental health problems such as posttraumatic stress disorder (PTSD) in those parents. Intervention approaches for parents of children with IDD are scarce and many parents remain without support.
Objective: This study aims to test the feasibility and efficacy of online Narrative Exposure Therapy (eNET) with parents of children with IDD.
Methods: The study follows a randomized waitlist-control design. eNET is an exposure-based PTSD intervention and includes 8–12 90-minute sessions. All sessions will be conducted via video calls with trained paraprofessionals. We aim to include 50 parents, approximately 25 in the immediate intervention group and 25 in the waitlist group. Waitlist participants will receive the same intervention after a three-month wait period. All participants need to either fulfill full or subclinical PTSD symptoms according to DSM-5. Feasibility and efficacy of the intervention will be measured with pre, post, and 2 and 6 months follow-up surveys focusing on PTSD symptoms. Secondary outcomes include other health-related outcomes such as physical symptoms, depression symptoms, anxiety symptoms and functionality.
Conclusions: The proposed study allows us to test the feasibility and efficacy of eNET in a sample of parents of children with IDD. There are so far no published studies on the evidence of eNET; this study is one of the first randomized controlled trials investigating the feasibility and efficacy of eNET and therefore will have implications on further research and practice.
Clinical trial registration: NCT04385927
Date and version identifier: 22 July 2021
KEYWORDS: Parent, disability, PTSD, RCT, exposure, eNET, intervention, trauma
HIGHLIGHTS
Online Narrative Exposure Therapy (eNET) is a new approach to reduce PTSD symptoms in one-on-one video sessions.
This study examines the feasibility and efficacy of conducting eNET with parents of children with neurodevelopmental disorders in a randomized controlled trial.
Short abstract
Antecedentes: Los padres de niños con trastornos intelectuales y del neurodesarrollo (TIND) experimentan con frecuencia eventos traumáticos durante el cuidado de sus hijos. Esto lleva a cifras relativamente altas de problemas de salud mental, tales como el trastorno de estrés postraumático (TEPT), en estos padres. Los abordajes para intervenir a los padres de niños con TIND son escasos y muchos padres continúan sin recibir soporte.
Objetivo: El objetivo de este estudio es evaluar la viabilidad y la eficacia de la terapia de exposición narrativa en línea (eNET, por sus siglas en inglés) en padres de niños con TIND.
Métodos: El estudio sigue un diseño aleatorizado con el grupo de control asignado a una lista de espera. La eNET es una intervención para el TEPT basada en exposición que incluye 8 a 12 sesiones de 90 minutos cada una. Todas las sesiones se realizarán mediante videollamadas con paraprofesionales entrenados. El objetivo es incluir a 50 padres, aproximadamente 25 en el grupo de intervención inmediata y 25 en el grupo de lista de espera. Los participantes en la lista de espera recibirán la misma intervención luego de un periodo de tres meses de espera. Todos los participantes deben cumplir los criterios para el TEPT según el DSM-5, ya sea de manera completa o subclínica. La viabilidad y la eficacia de la intervención se medirán con encuestas enfocadas en los síntomas del TEPT tomadas antes de la intención, inmediatamente luego de concluirla y a los 2 y a los 6 meses de seguimiento. Los resultados secundarios incluyen a aquellos relacionados con otros factores de la salud tales como síntomas físicos, síntomas de depresión, síntomas de ansiedad y funcionalidad.
Conclusiones: El estudio propuesto nos permite evaluar la viabilidad y la eficacia del eNET en una muestra de padres de niños con TIND. Al momento, no existen estudios publicados sobre la evidencia de la eNET; este estudio es uno de los primeros ensayos aleatorizados que investigarán la viabilidad y la eficacia del eNET y, por tanto, tendrá implicancias para ulteriores investigaciones y para la práctica.
Registro de ensayo clínico: NCT04385927
Fecha e identificador de la versión: Julio 22 del 2021
PALABRAS CLAVE: Padrediscapacidad, TEPT, ensayo clínico aleatorizado, exposición, eNET, intervención, trauma
Short abstract
背景: 患有智力和神经发育障碍 (IDD) 儿童的父母在照顾他们孩子时经常会经历创伤性事件。这导致这些父母出现相对较多的心理健康问题,例如创伤后应激障碍 (PTSD)。对 IDD 儿童父母的干预方法很少,许多父母仍然得不到支持。
目的: 本研究旨在检验在线叙事暴露疗法 (eNET)对于IDD 儿童父母的可行性和有效性。
方法:本研究遵循随机候补名单对照设计。 eNET 是一种基于暴露的 PTSD 干预,包括 8-12 个 90 分钟的疗程。所有疗程都将通过与训练有素的辅助专业人员的视频通话进行。我们旨在招募 50 名父母,其中大约 25 名在立即干预组,25 名在等待名单组。等候名单组参与者将在三个月的等待期后接受相同的干预。所有参与者都需要满足全部或亚临床 DSM-5 PTSD 症状。干预的可行性和有效性将通过针对 PTSD 症状的前、后以及 2 个月和 6 个月的跟进调查来测量。次要结果包括其他健康相关结果,例如躯体症状、抑郁症状、焦虑症状和功能性。
结论: 本拟议研究使我们能够在 IDD 儿童的父母样本中检验 eNET 的可行性和有效性。到目前为止,还没有关于 eNET 证据的已发表研究;本研究是首批研究 eNET 可行性和有效性的随机对照试验之一,因此将对进一步的研究和实践有启发意义。
临床试验注册: NCT04385927
日期和版本标识符: 2021 年 7 月 22 日
关键词: 父母, 残疾, PTSD, RCT, 暴露eNET, 干预, 创伤
1. Introduction
Parents of children with intellectual and neurodevelopmental disorders (IDD) face considerable challenges in caring for their children. Their children’s health conditions can lead to life-threatening situations, causing harm to both the children and parents (Miodrag & Hodapp, 2010). Being repeatedly exposed to traumatic events in the care for their children can lead to higher rates of posttraumatic stress disorder (PTSD). Previous studies indicate high rates of PTSD of around 20–30% in these groups (Cabizuca, Marques-Portella, Mendlowicz, Coutinho, & Figueira, 2009; Craig et al., 2016; Goldberg, Morris, Simmons, Fowler, & Levison, 1990). Chronic courses of PTSD are common; up to 40% report symptoms 10 years after onset (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). In the long-term, PTSD can diminish physical health, impair functioning, and decrease quality of life (Erbes, Meis, Polusny, & Compton, 2011; Magruder et al., 2004; Shea, Vujanovic, Mansfield, Sevin, & Liu, 2010). A large number of parents with PTSD also experience comorbid disorders such as depression, anxiety, and substance abuse (Keane, Brief, Pratt, & Miller, 2007; Perkonigg, Kessler, Storz, & Wittchen, 2000).
Evidence-based interventions, such as exposure-based approaches, play a vital role in the remission of PTSD symptoms (Katzman et al., 2014). However, there are several barriers to access treatment within existing healthcare systems and interventions; for example, difficulties to afford services, limited access to care, shortage of services and health professionals, long wait lists, logistical challenges (e.g. travel, time off work), and stigmatization (Collins, Westra, Dozois, & Burns, 2004).
A trauma-focused intervention approach addressing repeated and continuous trauma exposure has been developed by Schauer et al. (2011): the Narrative Exposure Therapy (NET) aims to process multiple traumatic events chronologically throughout the client’s lifetime. NET has proven effective in a great variety of cultures (Lely et al., 2019; Siehl, Robjant, & Crombach, 2020). A reduction of PTSD symptoms as well as comorbid symptoms such as depression and physical symptoms were found in previous studies (Robjant & Fazel, 2010; Siehl et al., 2020). Furthermore, NET was developed to be pragmatic and easily learned by paraprofessionals. Several studies have shown that paraprofessionals can be effectively trained to administer NET (Jacob, Neuner, Maedl, Schaal, & Elbert, 2014; Köbach, Schaal, Hecker, & Elbert, 2017; Neuner et al., 2008). Most recently, recommendations have been published how to use NET via video calls (eNET; Kaltenbach et al., 2021). However, studies showing the efficacy of eNET still need to be conducted.
1.1. Objectives
To our knowledge there are so far no interventions focusing on addressing PTSD in parents of children with IDD. Studies examining the feasibility and efficacy of eNET are also still outstanding. The present study aims to test the feasibility and efficacy of eNET, an innovative distance-delivered, exposure-based intervention for PTSD that addresses the above-mentioned limitations. First, by offering the intervention online, it increases accessibility for those who live in remote regions or lack access to transportation and it reduces participants’ fear of stigma (Lingley-Pottie, McGrath, & Andreou, 2013). Meta-analyses show that distance-delivered interventions can reduce PTSD symptoms (Olthuis et al., 2016; Wozney et al., 2017). Second, the intervention has been especially adapted for parents of children with IDD. NET is an intervention that has been developed with the intention to be used and adapted to different populations. Finally, the intervention will be conducted by paraprofessionals under close supervision of a psychologist to address the extreme shortage of health professionals.
To achieve these objectives we intend to examine the following research questions:
Primary research question 1: Is eNET efficacious in reducing PTSD symptoms? The efficacy of eNET is measured through self-ratings of PTSD symptoms before, after, and 2 and 6 months after the intervention. Immediate and waitlist group are compared to investigate the efficacy of eNET.
Primary research question 2: Is eNET feasible in general as well as for parents of neurodiverse children experiencing PTSD symptoms? Feasibility is measured through dropout rate and reasons, symptom deteriorations, and adverse events.
Secondary research question: Does eNET reduce physical symptoms, depression symptoms, anxiety symptoms, and increase functionality in the participants? These secondary outcomes are measured through questionnaires before, after, and 2 and 6 months after the intervention.
2. Methods
2.1. Study design
Figure 1 illustrates the flow of participants through the study. At the beginning of the study, all participants take part in the initial survey ‘Survive and Thrive’. This survey was specifically designed for parents of children with IDD; parents with and without traumatic experiences and PTSD symptoms are asked to fill out this survey. It is a Canada wide cross-sectional survey that was developed by the researchers to get a better understanding about the traumatic experiences and mental health challenges parents of children with IDD face. It aims to have an approximately sample size of around 500–800 participants. It also functions as a screening survey for the eNET study. Researchers and parent partners advertise for this survey via social media channels, email lists, websites, support groups, or other venues where parents of children with IDD have a presence. Our parent partners are people with lived experience as caregivers for children with IDD. They provide valuable input at all stages of the project and help to ensure research is done in a manner that values and is of use for the unique experiences of this population.
Figure 1.
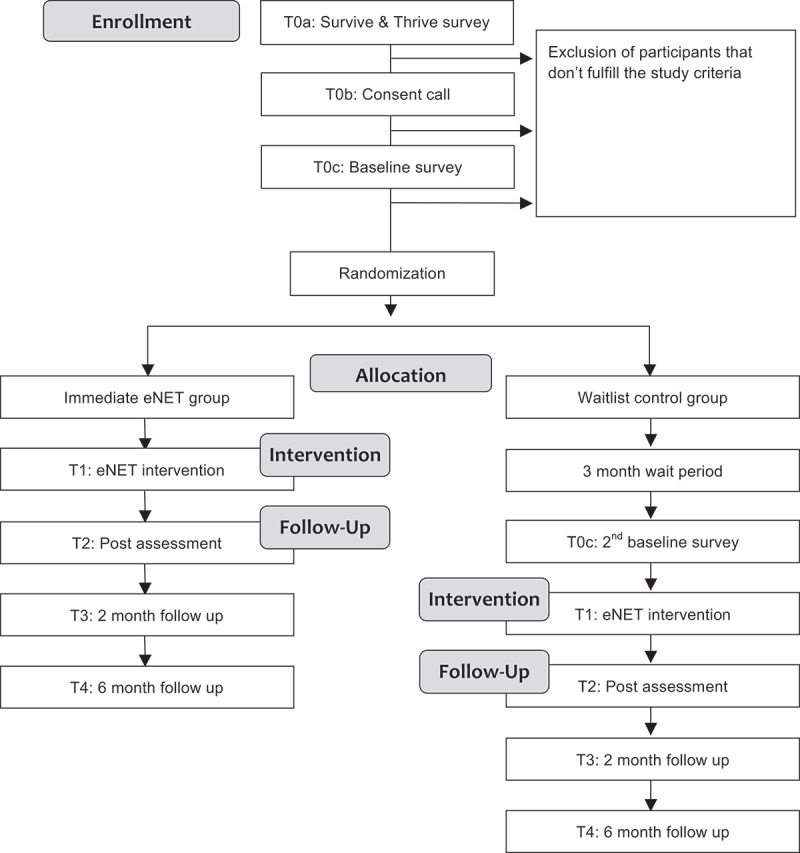
Study flow chart
Participants who completed the initial survey ‘Survive and Thrive’ and who agreed to be contacted for future studies are invited to get more information and check their eligibility for the eNET study. Interested parents are then invited to take part in a consent call where additional eligibility questions are asked. Trained paraprofessionals, explain in detail the purpose of this study, the risks and benefits, what their participation involves and their rights as a research participant. Participants give their approval for participation via recorded verbal consent. Parents of the same child are allowed in the study; in such a case those parents would be with different paraprofessionals. No exception would be made for the random allocation; both parents would be randomized as per protocol. Following consent, parents are asked to fill out another short baseline survey that finalizes their eligibility. After this, they are randomized into one of two groups following a waitlist control design. One group receives the intervention immediately after randomization, while the other group waits approximately three months before beginning the intervention. Block randomization with randomly varied blocks is used to ensure equal size of each group. Intervention allocation is 1:1, there is no stratification, and randomly varied blocks of 2 and 4 are used. The randomization process is conducted by an independent statistician through REDCap. Both groups complete assessments directly following the end of the intervention as well as two and six months after the end of the intervention. Additionally, waitlist participants are asked to fill out the initial questionnaire again after their 3-month wait period and before starting the intervention. Their eligibility is assessed again to ensure the intervention is still appropriate. For comparison, dropout participants are asked to fill out the follow-up surveys as well. In an effort to reduce dropout rates and accommodate the time restrictions parents face, we enable parents to stop during the survey and return at a later time (via email link). Furthermore, each question entails an answer category ‘prefer not to answer’. For their time commitment participants receive a $25 gift card for completing the surveys 2nd T1C, T3, T4, and T5.
2.2. Study setting
The research study is being conducted at the Centre for Research in Family Health at IWK Health in Halifax, Nova Scotia, Canada. The paraprofessionals conducting the intervention sessions do so offsite at their homes due to COVID-19. Paraprofessionals are defined as university graduates (in a relevant field such as psychology or social work) who have undergone extensive training in eNET and an understanding of the unique experiences and traumas that parents/caregivers of neurodiverse children may face. They are closely supervised by a psychologist throughout the intervention (regular group and individual supervision). In addition, randomly selected video recordings of the sessions are checked and rated for quality assurance throughout the study. All contact with study participants takes place virtually. The sessions are delivered via secure videoconferencing on Cisco Webex which is approved for the use in healthcare settings. All surveys as well as the randomization is done with REDCap. The study was approved by the Research Ethics Board at the IWK Health Centre in Canada (REB Ref. 1,025,577) and is registered on www.clinicaltrials.gov (identifier: NCT04385927).
2.3. Online narrative exposure therapy (eNET)
Table 1 outlines the major components of each intervention session. All participants receive the eNET intervention consisting of approx. 8–12 weekly 60–90 minute videoconference sessions between the participant and a paraprofessional. Those in the waitlist group receive the same intervention, except three months later. Depending on the amount of relevant traumatic experiences, the length of the intervention can vary slightly.
Table 1.
Content of the intervention
| Session | Main components |
|---|---|
| Session 1: Psychoeducation |
|
| Session 2: Lifeline |
|
| Sessions 3–11: Exposure |
|
| Session 12: Final Session |
|
NET is a well-established exposure-based intervention for PTSD (Schauer, Neuner, & Elbert, 2011). eNET is adapted for the use in a video call setting (Kaltenbach et al., 2021; Robjant, Meyer, Kaiser, Kaltenbach, & Schauer, 2020). Adaptations are mainly made in order to provide comparable content via video calls (e.g. conducting the interactive lifeline session with an online programme). Additional adjustments are made to fit the intervention to the target group of parents of children with IDD (mainly in the psychoeducation and final session). During the first session (i.e. psychoeducation), the participant and the paraprofessional look at the participants’ symptoms and discuss general information about PTSD symptoms and eNET. Topics such as suicidal ideation/behaviour, dissociation and an emergency plan are discussed. In the second session (i.e. lifeline), participants develop a lifeline together with the paraprofessional using an interactive web based application (https://yourlifeline.net). This tool helps to get an overview of the different life events of the participant. This includes giving a brief description of important events in their life including traumatic events (stones), positive events (flowers), sorrowful events (candles), and events where they harmed others (sticks). For each event, the name, place, and date of the event are named and written down. All events are placed in chronological order on a virtual timeline, with a rope that symbolizes their life.
The following sessions are exposure sessions. The participants’ most important traumatic events are exposed in chronological order. All exposure sessions follow the same structure. While the primary focus of the exposure sessions is on the reprocessing of a specific traumatic event, paraprofessionals will spend time before and after to discuss other events on the lifeline, ensuring to also emphasize participants’ positive experiences. Revisiting positive experiences can become a valuable resource for resilience. During exposure to a traumatic event, sensory, cognitive, emotional, physiological details, and meaning of the scene are repeatedly assessed to ensure a good exposure to the event. To ensure that the participant doesn’t become detached from the present, similar questions are asked about the present. The participant engages in reprocessing, meaning-making, and integrating challenging memories into a coherent narrative. The session ends with 5–10 minutes of checking in about the present. Subsequent to the session, the paraprofessional creates a written narrative of the exposed traumatic event. The narrative is read to the participant in the next session. The reading is interactive and considered a second exposure of the event; the participant adds missing aspects and the paraprofessional asks more questions to ensure that the participant is engaged in the event. After reading the event, the next event is exposed in the same manner as in the previous session.
The last session is spent reviewing the exposed events and looking towards the future. The lifeline programme is used to recapitulate the work and to add wishes for the future. Additionally, paraprofessional and participant discuss how to deal with traumatic events and PTSD symptoms in the future.
2.4. Measures
Measures are administered at five time points: T0a (survey ‘Survive and Thrive’; before start of the intervention), T0b (consent call; before the start of the intervention), T0c (baseline survey; before the start of the intervention, after consent), T1 (repeated surveys during the intervention), T2 (directly after the intervention), T3 (2 months follow-up), and T4 (6 months follow-up). T0c is completed twice for those in the waitlist group. In case of a time frame of less than two weeks in between T0a and T0c, the overlapping questionnaires are not be asked again. In this section, the information of the specific time points for each questionnaire is marked.
2.4.1. Demographics – T0a
Demographic information being collected consists of parent’s and children’s age and gender, family structure, time spent on caregiving, diagnoses of the child, marital and employment status, education, and family member involvement.
2.4.2. Life events checklist for DSM-5 (LEC-5; Weathers et al., 2013) – T0a
The LEC-5 is a self-rating measure to assess a broad range of traumatic experiences (Weathers et al., 2013). It was validated and utilized in a variety of populations, i.e. in a group of caregivers (Allen, 2015). It consists of 17 items with six response categories for each question; in our study, we changed the response categories to ‘yes’ and ‘no’ only. This response format has also been used and found to be feasible in other studies (Boughner, Thornley, Kharlas, & Frewen, 2016; Kaltenbach, Schauer, Hermenau, Elbert, & Schalinski, 2018).
2.4.3. Parenting trauma checklist (PTC; Xiong, McGrath, Yakovenko, Thomson, & Kaltenbach, 2021) – T0a
This questionnaire was created to assess the parents’ traumatic experiences related to caring for their children. The checklist was created by an extensive literature research and discussing the developed items with the parent advisors and other stakeholders. The checklist includes 17 items rated with ‘yes’ or ‘no’. Appendix 1 shows the content of the items.
2.4.4. PTSD checklist for DSM-5 (PCL-5; Weathers et al., 2013) – T0a, T0c, T2, T3 T4
The PCL-5 is a widely used and validated 20-item self-report scale that measures PTSD symptoms based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5; American Psychiatric Association, 2013). The items ask questions about the extent that participants were bothered by PTSD symptoms in the past month on a 5-point Likert scale ranging from 0 (not at all) to 4 (extremely) (Blevins, Weathers, Davis, Witte, & Domino, 2015). It shows strong reliability and validity (Blevins et al., 2015).
2.4.5. Patient health questionnaire (PHQ-9; Kroenke, Spitzer, & Williams, 2001) – T0c, T2, T3, T4
The PHQ-9 is a self-report measure that asks participants to report how often they have been bothered by a series of depression symptoms over the prior two weeks. Good psychometric properties were found in previous studies (Kroenke et al., 2001).
2.4.6. Generalized anxiety disorder (GAD-7; Spitzer, Kroenke, Williams, & Löwe, 2006) – T0c, T2, T3, T4
The GAD-7 is a 7-item self-report scale that asks participants to indicate how often in the past two weeks they have experienced a series of anxiety symptoms. The measure has good reliability and validity (Spitzer et al., 2006).
2.4.7. Patient health questionnaire physical symptoms (PHQ-15; Kroenke, Spitzer, & Williams, 2002) – T0c, T2, T3, T4
PHQ-15 is a 15-item self-report scale that asks participants to indicate how often in the past week they have been bothered by a series of physical symptoms.
2.4.8. Sheehan disability scale (SDS; Sheehan, 1983) – T0a, T0c, T2, T3, T4
The SDS is a five-item assessment about functional impairment (Leon, Olfson, Portera, Farber, & Sheehan, 1997). Participants rate to what extent their functioning is affected by their health on a scale from 0 (not at all) to 10 (extremely). The SDS asks for functionality regarding work, social life, and family life. It shows good validity and acceptable reliability (Leon et al., 1997).
2.4.9. Consent call eligibility questionnaire (self-constructed) – T0b
At the beginning of the consent call participants are asked several questions to screen for their eligibility. These questions screen for: presence of at least one traumatic event, PTSD intrusion symptoms, suicidal behaviour, dissociation, psychotic symptoms, participation in other exposure-based interventions for PTSD, use of alcohol, drugs or medication that could intervene with the intervention, access to a computer or tablet with Internet, and if necessary, child care during the sessions.
2.4.10. Adverse events and course of symptoms (self-constructed) – T1, T2
At the beginning of each session (T1), three questions are asked and further explored by the paraprofessional. One question is about symptom improvements, no change in symptoms or symptom deterioration; the other two ask for negative events related and unrelated to the intervention. Questions about adverse events and their persistence are also asked at the end of the intervention (T2). If adverse events are reported, lead researchers and supervisors will be immediately informed and the following procedure will be discussed.
2.4.11. Working alliance inventory – short form revised (WAI-SR; Hatcher & Gillaspy, 2006) – T2
Paraprofessional alliance is assessed using the Working Alliance Inventory – Short Form Revised, a 12-item self-report measure of alliance that asks participants about their perception of (a) agreement on goals of the intervention, (b) agreement on tasks of the intervention, and (c) paraprofessional-participant bond. The WAI-SR has good internal consistency and validity (Hatcher & Gillaspy, 2006).
2.4.12. The client satisfaction questionnaire (CSQ-8; Atkinson & Greenfield, 2004) – T2
The CSQ-8 has been implemented in primary care and mental health treatment to measure participant satisfaction with services received. Participants are asked to rate the quality of service they received as part of the eNET intervention on a four-point Likert scale. The CSQ-8 shows a good internal consistency (Atkinson & Greenfield, 2004). In addition to the CSQ-8, a question about the satisfaction with the intervention being conducted via videoconferencing are asked on the same scale as the CSQ-8. Three open-ended questions are asked additionally to see what participants experienced as helpful/not helpful and what they would like to see improved.
2.4.13. Other questionnaires
Additional questionnaires were used in the survey ‘Survive and Thrive’ as well as in the follow-up surveys. These are listed here for completeness reasons, as they are included in same surveys. They don’t form a major part regarding the results of the eNET and are therefore not detailed here. The questionnaires are: a) Help-seeking behaviour adapted from the Konstanz INDEX (KINDEX; Spyridou, Schauer, & Ruf-Leuschner, 2015) – T0a; Posttraumatic Growth Inventory – Short Form (PTGI; Tedeschi & Calhoun, 1996) – T0a, T2, T3, T4; The Parent and Family Adjustment Scales (PAFAS; Sanders, Morawska, Haslam, Filus, & Fletcher, 2014) – T0a, T2, T3, T4; The Multidimensional Scale of Perceived Social Support (MSPSS; Zimet, Dahlem, Zimet, & Farley, 1988) – T0a, T2, T3, T4; Health Service Use Questionnaire (self-constructed) – T0a, T0c, T2, T3, T4; Shutdown Dissociation Scale (Shut-D; Schalinski, Schauer, & Elbert, 2015) – T0c. During the intervention a short distress measure (self-constructed; 0–10) was asked at the beginning and end of each session. In addition to this, at the end of each session, the paraprofessional asked how helpful the participant found the session. These questions during the intervention were asked for therapeutic and not research purpose.
2.5. Participants
We plan to recruit 50 participants, with 25 cases in each arm. Inclusion criteria are the following: participants must be at least 18 years of age, and a parent or caregiver of a child (any age) with IDD. They must also be able to understand spoken and written English at a Grade 8 level. They must fulfil the criteria of full or subclinical PTSD symptoms according to DSM-5, measured with the LEC-5, the PTC, and the PCL-5. For this they have to report at least one traumatic event in the LEC-5 or the PTC. To fulfill the criteria of PTSD symptoms for this study, the participant additionally needs to respond with ‘moderately’ or higher in at least one item each for the criteria B and C and two items each for criteria D and E. Subclinical PTSD is fulfilled if the participant meets all but one criterion of B, C, D, or E. Participants must live in Canada and be able to participate in weekly video calls for approximately 12 weeks. They require access to a computer or laptop with high speed Internet in order to participate in these calls.
The following exclusion criteria apply: participants who have been in a comparable exposure intervention for PTSD symptoms for the same traumatic events will be excluded. Participants with the following symptoms will also be excluded: (1) participants with moderate to severe symptoms of dissociation (i.e. a score of ≥18.5 on the Shutdown Dissociation Scale; Schalinski et al., 2015), (2) acute psychotic symptoms, and (3) acute suicidal behaviour. Participants who cannot commit to 1.5 hour sessions weekly and are not able to have an uninterrupted space for themselves for this time (e.g. no child care available) cannot participate due to the nature of this intervention. Additionally, participants who have recently started or made changes to their medication will be asked to wait until they have been on this new medication/dose for at least two months. Participants will also be asked to refrain from taking any intoxicating substance (e.g. alcohol, cannabis, benzodiazepine) for at least two hours prior to and after a session; if this is not possible, participants will need to be excluded. If the paraprofessional has reason to believe a participant is in need of addiction treatment or is unable to refrain from substance use for the aforementioned amount of time, this will be discussed with a supervisor before allowing the individual into the study.
2.6. Safety assessment and reporting of adverse events
2.6.1. Safety protocol for study participants
A detailed and standardized safety protocol has been developed to minimize risk and harm for participants. The safety procedures include the following aspects:
Thorough eligibility process: A thorough process to determine the eligibility of the participants is deemed necessary to ensure that the intervention is safe and sound for those participating. If participants are screened ineligible and require immediate care (e.g. acute suicidal behaviour, high dissociation), the paraprofessional follows an emergency protocol to transfer them to appropriate services.
Continuous transparency, involvement and education of participants: Participants are informed and involved in decision making at each step. The consent form is conducted via video call to ensure understanding and encourage questions. Potential harms and benefits are addressed and discussed with each participant. The first intervention session completely focuses on psychoeducation to give the participants a thorough understanding, prepare them for the intervention, and to give them tools to handle potential risks (e.g. dissociation).
Regular check-ins on well-being: Before each session, the paraprofessional checks in with the participant on their well-being and readiness for the session. The preparation encompasses: (a) availability of time for a minimum of 1–1.5 hours, (b) a confidential and undisturbed setting/room, (c) water and an exposure tool kit to prevent and address dissociation (e.g. touch stimulator such as a massage ball, scent such as mint, and anti-dissociation exercises). Participants are also asked to answer a distress measure rating at the beginning as well as the end of each session. This way the readiness to start or end the session is determined.
Regular check-ins on adverse events and symptom deterioration: At the beginning of each session questions regarding adverse events and changes in the symptoms are asked by the paraprofessional. In case of an adverse event or major symptom deterioration, the paraprofessional will assess in more detail where these symptoms could stem from. In case of suppression of details of an event during exposure, the exposure will be repeated with focus on adding missing pieces. In case of new stressful or traumatic events, participant and paraprofessional will discuss how to deal with this new event and how the participant would like to proceed with the current intervention. The session can then either be used to continue with the intervention, to talk about how to deal with the new event, or the session will be rescheduled to allow the paraprofessional to discuss next steps with their supervisor. In case the paraprofessional and the participant cannot find the source of the symptom increase, the supervisor will be consulted immediately. In case of an adverse event, the supervisor as well as the Research Ethics Board will be informed immediately. If necessary, additional measures to ensure the safety and well-being of the participant will be taken.
Drop-out: In case a participant drops out of the study, the research team reaches out to ask for feedback about the reasons of drop-out and offer a conversation with one of the supervisors or principal investigators in case they were not satisfied with the programme or experienced a symptom deterioration or adverse event because of the intervention.
Contrasting between past and present during exposure: During the exposure sessions, participants’ memories of traumatic events are exposed in a structured and safe way. A structured procedure is followed during the exposure to ensure the assessment of all aspects of the events (sensations, emotions, physical reactions, cognitions, and meaning). Questions contrasting the past and the present prevent dissociative reactions and overwhelming emotions. Each exposure session ends at a safe spot in the story and paraprofessional and participant take some time to check in and prepare the participant for after the session.
Dealing with new upcoming traumatic events or memories: At the end of the intervention, a plan on how to deal with resurfacing memories and new traumatic events will be discussed and individualized for the participant.
Emergency procedures: An emergency protocol has been established to address situations of risk. On a standard basis, the protocol involves the collection of related information before the start of each session (e.g. address where the session is delivered, updated telephone number, telephone number of an emergency contact). The paraprofessionals are trained on how to react, refer and whom to inform in case of an emergency. The role of a paraprofessional in this case is to encourage and support the participant in seeking professional help and to refer the participant to according services. The supervisors and principal investigators of this project are informed immediately in case of an emergency.
Clear-set boundaries and responsibilities of the paraprofessionals: As this intervention is conducted by paraprofessionals, the boundaries of their work are clearly defined to not overstep their abilities and responsibilities. Paraprofessionals are trained to know their boundaries and how to transfer participants to appropriate services. Supervisors and the principal investigators will be contacted in such situations to confirm and discuss the procedure. Participants are informed that they work with paraprofessionals and that they need to contact other health services in case of emergencies or other mental health problems.
2.6.2. Safety protocol for paraprofessionals
Paraprofessionals constant exposure to others’ detailed narration of traumatic experiences can affect their personal life and their ability to continue working as a paraprofessional. Repeated exposure to details of traumatic experiences of others has also been linked to secondary traumatic stress (STS) and work-related mental health challenges in the literature (Gilroy, Carroll, & Murra, 2002; Hensel, Ruiz, Finney, & Dewa, 2015). The safety programme for the current study aims to prevent and treat STS and related mental health problems, to ensure participants’ safety, to ensure good quality in care, and to provide a good and long-lasting intervention environment.
Components used to lower the risk of harm for paraprofessionals encompass:
Safety culture: A constantly present safety culture at the workplace is key. Our safety culture recognizes and accepts challenges as an integral part. Support from within the team is available at any time and support outside the team can be arranged as well. Self-care and knowing your own limits will be encouraged and taken seriously in the daily work life. Exposure sessions demand a high level of concentration and emotional engagement. Former projects found that the number of sessions per day should be limited to guarantee that paraprofessionals can process the events and provide good work long-term. Sessions are limited to two exposure sessions a day.
Ongoing peer support system: Paraprofessionals form a peer support system. Pairs or triples are formed and frequent check-ins and exchange are part of the workday. A support chat and a weekly paraprofessionals meeting assists this peer support system.
Regular supervision: Group as well as individual supervision are provided on a regular basis. It focuses on challenges with participants as well as the paraprofessionals’ well-being.
Self-care and preventive exposure sessions: During the training, paraprofessionals are trained in participant and paraprofessional safety. They will learn how to detect signs of STS and mental health challenges in themselves as well as the other paraprofessionals. Reflection and assessment of their individual mental health is conducted in the training through self-rated questionnaires and through the voluntary offer to discuss this with one of the trainers or an independent person. Paraprofessionals also expose some of their own traumatic experiences. Sharing private information is encouraged but voluntary at each level. These elements support the paraprofessionals in forming a decision whether they feel ready to work as a paraprofessional. Self-reflection and exposure of own traumatic events are an important part in the work as a paraprofessional and it aims to prevent paraprofessionals from experiencing STS. Self-care is an integral part during the training and is also encouraged to practice by the paraprofessionals throughout their work as a paraprofessional. Paraprofessionals are further encouraged to do a post-session reflection about how they felt during and after the session and if there are any parts that affected them about the session.
2.7. Data analyses
A statistical power analysis was not conducted to estimate the required sample size due to the novelty of this study. Previous methodological studies (Julious, 2005; Sim & Lewis, 2012) suggest that a sample of 24–50 is recommended for a first trial assessing feasibility and efficacy. This is also in line with previous feasibility and pilot trials in the mental health domain, as reported in a review (Billingham, Whitehead, & Julious, 2013).
Data analyses will use Microsoft Excel, IBM SPSS, SAS (SAS Institute Inc., Cary, NC, USA) and R (R Core Team, Vienna, Austria). All participants, also those who might have dropped out during the intervention, will be included in the analyses. Dropouts will be compared with the group that completed the intervention on sociodemographic information, PTSD symptoms, physical symptoms, depression symptoms, anxiety symptoms, and trauma exposure. Missing data for the primary outcome data will be replaced through multiple imputation. Secondary outcome data will use data driven imputation. Baseline and follow-up data will be presented using descriptive statistics. Continuous data will be summarized by the mean/median, standard deviation (SD), and range. Categorical data will be presented by absolute and relative frequencies (n and %).
For the primary research question 1 (efficacy of eNET in reducing PTSD symptoms), we will run a t-test comparing the waitlist (time point T0a/T0c1st assessment and T0c2nd assessment) with the immediate group (time point T0a/T0c and T2). To see the PTSD course including the follow-up time points, we will then conduct a repeated measures linear regression.
To explore the primary research question 2 (feasibility of eNET), we will calculate different factors. We will look at the percentage of dropouts as well as describe their reasons for dropping out qualitatively. We will use descriptive statistics to describe symptom deteriorations and adverse events. The types of adverse events, their frequency, and their connection to the intervention will be described qualitatively through content analysis. In addition we will look at the participant satisfaction with the intervention as well as their paraprofessional. For this, sum scores as well as single item descriptions will be presented. Open questions will be analysed qualitatively through content analysis.
The secondary outcome measures (i.e. anxiety symptoms, depressive symptoms, physical health, functionality) will be explored descriptively and we will conduct t-tests between immediate intervention and waitlist group as described for the PTSD measure. To see the overall course over time we will conduct repeated measures linear regressions.
3. Discussion
In families with children with IDD, the focus often lies on the treatment of the children’s health challenges – parents’ health is often considered secondary. However, parents’ health and well-being is important for both the parent and the child as well as for the parent-child relationship and well-being. Experiencing traumatic events in parenting as well as in other parts of life can negatively influence parents’ mental and physical health. However, few parents are receiving help. The aim of this study is to provide an intervention that facilitates access to treatment and to test how feasible and effective this programme is for parents of children with IDD. The programme tackles the barrier of availability of treatment by providing this intervention online and thereby making it more feasible for parents to participate. It also addresses the current lack of health professionals by using an intervention approach that is feasible and efficient with paraprofessionals. Such an approach could run as an add-on to the existing health system. Furthermore, the programme is standardized but still adapts well to the circumstances of each parent. By testing the feasibility and efficacy of this approach for parents of children with IDD, we expect to get first answers that show whether this approach is promising in this population as well as if eNET is feasible and effective in general.
Online approaches have been on the rise in mental health care in the last years. However, there are few approaches that address PTSD symptoms in a one-on-one online setting. Transforming and adapting an established and efficient in-person approach like NET into an online intervention could reveal promising results. The principles of NET, amongst others, the activation of the different memory components during the exposure sessions, stay the same. The major challenge lies in ensuring a sound implementation of components that are different in video settings compared to in-person settings. For example, this study has stricter exclusion criteria for aspects that could cause safety issues in online settings such as high dissociation symptoms. Furthermore, paraprofessional and participant dedicate more time to explaining the procedure, making a plan as well as practicing certain exercises relating to how the participant can react in case they feel unsettled after a session, when the connection is interrupted, when they experience dissociation symptoms etc. Additionally to adaptations made for the online context, the last session includes information on how to deal with upcoming memories as well as new traumatic events after the intervention. This is particularly important for parents of children with IDD because they may continue to experience traumatic events with their children after the intervention. Activating available resources and being aware of potentially challenging situations might support dealing with new experiences. This may also include looking for help in a timely manner and reducing stigma about seeking help. Research assessing the feasibility and efficacy of interventions often focuses on positive outcomes, with a tendency to not assess adverse events and symptom deteriorations systematically. Our study aims to assess adverse events and changes in symptoms on a weekly basis. This will be important to react timely in case of adverse reactions as well as to shine light on whether online interventions and exposure-based PTSD interventions have the potential to lead to adverse reactions as feared by some therapists.
We expect that this intervention study will contribute to the knowledge about online interventions for PTSD and more specifically eNET. The challenges we will face by providing NET online will help us to improve the performance and efficacy of eNET. If eNET proves to be feasible and effective, we would suggest the continued use in research as well as in practice. eNET with paraprofessionals could be provided as an add-on to the general health care system and done in collaboration with mental health professionals. This could enable the health care system to provide treatment to more people and in a more timely fashion.
This study has some limitations: The aimed sample size allows implications on the feasibility and efficacy of the programme for parents of children with IDD. However, a large-scale RCT would be desirable to confirm the findings. Due to COVID-19 the results on the well-being of participants could be skewed, especially as some of the medical conditions of their children put them into the high risk group. Also, childcare and respite care is less or not available during COVID-19. Distress measures at the beginning and end of each session are conducted by the paraprofessionals which could lead to possible respondent bias because of social desirability. The results of this study will be limited in its generalizability due to the limited sample size and the very specific population studied.
This study is a promising approach to address PTSD symptoms in parents of children with IDD. By decreasing barriers to access support, this programme aims to reach parents who would normally not be able to receive or afford support. If feasible and effective, we hope that this intervention can be evaluated and implemented on a large-scale basis.
Acknowledgments
We are grateful for our research team, especially Maria McGrath, Michael Nash, and Karen Turner. We are thankful for our research collaborators, especially Janine Olthuis and Maggie Schauer. Furthermore, we thank all parent partners of this study: David Bell, Christine Kluczynski, Hannah McGee, Angela McNair, Jeanine Lebsack and our parent ambassadors.
Appendix 1: Parenting Trauma Checklist (PTC)
Instructions: Below you will find some difficult experiences parents sometimes experience while caring for their child or children. Please indicate which of these events you experienced.
| Yes | No | |
|---|---|---|
| (1) Witnessing a life-threatening situation of your child (e.g. severe bleeding, stop breathing, passing out, severe seizures) | ☐ | ☐ |
| (2) Witnessing a severe accident or injury of your child (e.g. car accident, falling, drowning) | ☐ | ☐ |
| (3) Experiencing a medical emergency of your child (ambulance rides, rushing to hospital, calling 911) | ☐ | ☐ |
| (4) Seeing your child undergoing a medical procedure (e.g. breathing treatments, child hooked up to machines, forced treatments, CPR) | ☐ | ☐ |
| (5) Your child undergoing a life-threating surgery (e.g. heart surgery, organ transplant, routine surgery that is life-threatening because of pre-existing conditions) | ☐ | ☐ |
| (6) Hearing of a life-threatening event of your child (e.g. that may have happened at school, in your absence) | ☐ | ☐ |
| (7) Fearing that your child would die while waiting for care (e.g. waiting for ambulance, waiting for transplant) | ☐ | ☐ |
| (8) Receiving diagnosis of life-threatening disability of your child | ☐ | ☐ |
| (9) Being in the ICU/NICU/PICU with your child | ☐ | ☐ |
| (10) Witnessing a child not in your care die or being critically ill | ☐ | ☐ |
| (11) Applying life-saving procedures to your child during crisis (e.g. performing CPR, give/inject rescue medication) | ☐ | ☐ |
| (12) Witnessing serious self-harming behaviour of your child (e.g. injuring themselves, suicide attempt) | ☐ | ☐ |
| (13) Birth was life-threatening for mother or child | ☐ | ☐ |
| (14) Miscarriage | ☐ | ☐ |
| (15) Death of your child | ☐ | ☐ |
| (16) A situation in which your child threatened the health or life of you or someone else | ☐ | ☐ |
| (17) Other situations that were extremely frightening when caring for your child. Please explain:_________ |
☐ | ☐ |
Funding Statement
This study is funded by the Canadian Institutes for Health Research, the Strategy for Patient Oriented Research (CHILD-BRIGHT Network) and the IWK Health Centre. The funders have no influence on the study design, collection, management, analysis, and interpretation of the data.
Authors’ contributions
EK, PM, DT and AC developed the study concept and design. EK, MC, and TX drafted the manuscript. PM and EK led the revision of the manuscript. All authors read and approved the final manuscript.
Data availability
This manuscript doesn’t include any data.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Allen, A. M. (2015). The impact of childhood trauma as moderated by ptsd, relationship with caregiver, and rumination. South Carolina: USC Aiken Psychology Theses. [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Atkinson, C. C., & Greenfield, T. K. (2004). The USCF client satisfaction scales: I. The client satisfaction questionnaire-8. In M.E. Maruish (Ed.) The use of psychological testing for treatment planning and outcomes assessment (3rd ED) (pp. 779–12). Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Billingham, S. A., Whitehead, A. L., & Julious, S. A. (2013). An audit of sample sizes for pilot and feasibility trials being undertaken in the UK registered in the UK clinical research network database. BMC Medical Research Methodology, 13(1), 1–6. doi: 10.1186/1471-2288-13-104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. doi: 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Boughner, E., Thornley, E., Kharlas, D., & Frewen, P. (2016). Mindfulness-related traits partially mediate the association between lifetime and childhood trauma exposure and PTSD and dissociative symptoms in a community sample assessed online. Mindfulness, 7(3), 672–679. doi: 10.1007/s12671-016-0502-3 [DOI] [Google Scholar]
- Cabizuca, M., Marques-Portella, C., Mendlowicz, M. V., Coutinho, E. S. F., & Figueira, I. (2009). Posttraumatic stress disorder in parents of children with chronic illnesses: A meta-analysis. Health Psychology : Official Journal of the Division of Health Psychology, American Psychological Association, 28(3), 379–388. doi: 10.1037/a0014512 [DOI] [PubMed] [Google Scholar]
- Collins, K. A., Westra, H. A., Dozois, D. J. A., & Burns, D. D. (2004). Gaps in accessing treatment for anxiety and depression: Challenges for the delivery of care. Clinical Psychology Review, 24(5), 583–616. doi: 10.1016/j.cpr.2004.06.001 [DOI] [PubMed] [Google Scholar]
- Craig, F., Operto, F. F., De Giacomo, A., Margari, L., Frolli, A., Conson, M., … Margari, F. (2016). Parenting stress among parents of children with Neurodevelopmental Disorders. Psychiatry Research, 242, 121–129. doi: 10.1016/j.psychres.2016.05.016 [DOI] [PubMed] [Google Scholar]
- Erbes, C. R., Meis, L. A., Polusny, M. A., & Compton, J. S. (2011). Couple adjustment and posttraumatic stress disorder symptoms in national guard veterans of the Iraq war. Journal of Family Psychology, 25(4), 479–487. doi: 10.1037/a0024007 [DOI] [PubMed] [Google Scholar]
- Gilroy, P. J., Carroll, L., & Murra, J. (2002). A preliminary survey of counseling psychologists’ personal experiences with depression and treatment. Professional Psychology: Research and Practice, 33(4), 402–407. doi: 10.1037/0735-7028.33.4.402 [DOI] [Google Scholar]
- Goldberg, S., Morris, P., Simmons, R. J., Fowler, R. S., & Levison, H. (1990). Chronic illness in infancy and parenting stress: A comparison of three groups of parents. Journal of Pediatric Psychology, 15(3), 347–358. doi: 10.1093/jpepsy/15.3.347 [DOI] [PubMed] [Google Scholar]
- Hatcher, R. L., & Gillaspy, J. A. (2006). Development and validation of a revised short version of the working alliance inventory. Psychotherapy Research, 16(1), 12–25. doi: 10.1080/10503300500352500 [DOI] [Google Scholar]
- Hensel, J. M., Ruiz, C., Finney, C., & Dewa, C. S. (2015) Meta-analysis of Risk Factors for Secondary Traumatic Stress in Therapeutic Work with Trauma Victims. Journal of traumatic stress, 28(2), 83–91. doi: 10.1002/jts.21998 [DOI] [PubMed] [Google Scholar]
- Jacob, N., Neuner, F., Maedl, A., Schaal, S., & Elbert, T. (2014). Dissemination of psychotherapy for trauma spectrum disorders in postconflict settings: A randomized controlled trial in Rwanda. Psychotherapy and Psychosomatics, 83(6), 354–363. doi: 10.1159/000365114 [DOI] [PubMed] [Google Scholar]
- Julious, S. A. (2005). Sample size of 12 per group rule of thumb for a pilot study. Pharmaceutical Statistics, 4(4), 287–291. doi: 10.1002/pst.185 [DOI] [Google Scholar]
- Kaltenbach, E., McGrath, P. J., Schauer, M., Kaiser, E., Crombach, A., & Robjant, K. (2021). Practical guidelines for online narrative exposure therapy (e-NET) – A short-term treatment for posttraumatic stress disorder adapted for remote delivery. European Journal of Psychotraumatology, 12(1), 1881728. doi: 10.1080/20008198.2021.1881728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaltenbach, E., Schauer, M., Hermenau, K., Elbert, T., & Schalinski, I. (2018). Course of mental health in refugees-a one year panel survey. Frontiers in Psychiatry, 9. doi: 10.3389/fpsyt.2018.00352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katzman, M. A., Bleau, P., Blier, P., Chokka, P., Kjernisted, K., & Ameringen, V. (2014). Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC Psychiatry, 14(1), 1–83. doi: 10.1186/1471-244X-14-S1-S1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keane, T. M., Brief, D. J., Pratt, E. M., & Miller, M. W. (2007). Assessment of PTSD and its comorbidities in adults. In M. J. Friedman, T. M. Keane, & P. A. Resick (Eds.), Handbook of PTSD: Science and practice (pp. 279–305). New York: The Guilford Press. [Google Scholar]
- Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry, 52(12), 1048–1060. doi: 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- Köbach, A., Schaal, S., Hecker, T., & Elbert, T. (2017). Psychotherapeutic Intervention in the demobilization process: Addressing combat-related mental injuries with narrative exposure in a first and second dissemination stage. Clinical Psychology and Psychotherapy, 24(4), 807–825. doi: 10.1002/cpp.1986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ‐9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613 doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2002). The PHQ-15: Validity of a new measure for evaluating the severity of somatic symptoms. Psychosomatic Medicine, 64(2), 258–266. doi: 10.1097/00006842-200203000-00008 [DOI] [PubMed] [Google Scholar]
- Lely, J. C. G., Knipscheer, J. W., Jongedijk, R. A., Smid, G. E., Smid, G. E., Jongedijk, R. A., … Smid, G. E. (2019). The effectiveness of narrative exposure therapy : A review, meta-analysis and meta-regression analysis meta-regression analysis. European Journal of Psychotraumatology, 10(1), 1550344. doi: 10.1080/20008198.2018.1550344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon, A. C., Olfson, M., Portera, L., Farber, L., & Sheehan, D. V. (1997). Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. International Journal of Psychiatry in Medicine, 27(2), 93–105. doi: 10.2190/T8EM-C8YH-373N-1UWD [DOI] [PubMed] [Google Scholar]
- Lingley-Pottie, P., McGrath, P. J., & Andreou, P. (2013). Barriers to mental health care: Perceived delivery system differences. Advances in Nursing Science, 36(1), 51–61. doi: 10.1097/ANS.0b013e31828077eb [DOI] [PubMed] [Google Scholar]
- Magruder, K. M., Frueh, B. C., Knapp, R. G., Johnson, M. R., Vaughan, J. A., Carson, T. C., … Hebert, R. (2004). PTSD symptoms, demographic characteristics, and functional status among veterans treated in VA primary care clinics. Journal of Traumatic Stress, 17(4), 293–301. doi: 10.1023/B:JOTS.0000038477.47249.c8 [DOI] [PubMed] [Google Scholar]
- Miodrag, N., & Hodapp, R. M. (2010). Chronic stress and health among parents of children with intellectual and developmental disabilities. Current Opinion in Psychiatry, 23(5), 407–411. doi: 10.1097/YCO.0b013e32833a8796 [DOI] [PubMed] [Google Scholar]
- Neuner, F., Onyut, P. L., Ertl, V., Odenwald, M., Schauer, E., & Elbert, T. (2008). Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 76(4), 686–694. doi: 10.1037/0022-006X.76.4.686 [DOI] [PubMed] [Google Scholar]
- Olthuis, J. V., Wozney, L., Asmundson, G. J. G., Cramm, H., Lingley-Pottie, P., & McGrath, P. J. (2016). Distance-delivered interventions for PTSD: A systematic review and meta-analysis. Journal of Anxiety Disorders, 44, 9–26. doi: 10.1016/j.janxdis.2016.09.010 [DOI] [PubMed] [Google Scholar]
- Perkonigg, A., Kessler, R. C., Storz, S., & Wittchen, H. U. (2000). Traumatic events and post-traumatic stress disorder in the community: Prevalence, risk factors and comorbidity. Acta Psychiatrica Scandinavica, 101(1), 46–59. doi: 10.1034/j.1600-0447.2000.101001046.x [DOI] [PubMed] [Google Scholar]
- Robjant, K., & Fazel, M. (2010). The emerging evidence for narrative exposure therapy: A review. Clinical Psychology Review, 30(8), 1030–1039. doi: 10.1016/j.cpr.2010.07.004 [DOI] [PubMed] [Google Scholar]
- Robjant, K., Meyer, D., Kaiser, E., Kaltenbach, E., & Schauer, M. (2020). e-NET: Narrative exposure therapy online - The challenges and opportunities of delivering trauma therapy remotely. Maltrattamento e Abuso All’Infanzia. doi: 10.3280/MAL2020-003002 [DOI] [Google Scholar]
- Sanders, M. R., Morawska, A., Haslam, D. M., Filus, A., & Fletcher, R. (2014). Parenting and family adjustment scales (PAFAS): Validation of a brief parent-report measure for use in assessment of parenting skills and family relationships. Child Psychiatry and Human Development, 45(3), 255–272. doi: 10.1007/s10578-013-0397-3 [DOI] [PubMed] [Google Scholar]
- Schalinski, I., Schauer, M., & Elbert, T. (2015). The shutdown dissociation scale (shut-D). European Journal of Psychotraumatology, 6(1), 25652. doi: 10.3402/ejpt.v6.25652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schauer, M., Neuner, F., & Elbert, T. (2011). Narrative exposure therapy: A short-term treatment for traumatic stress (2nd ed.). Göttingen: Hogrefe Publishing. [Google Scholar]
- Shea, M. T., Vujanovic, A. A., Mansfield, A. K., Sevin, E., & Liu, F. (2010). Posttraumatic stress disorder symptoms and functional impairment among OEF and OIF national guard and reserve veterans. Journal of Traumatic Stress, 23(1), 100–107. doi: 10.1002/jts [DOI] [PubMed] [Google Scholar]
- Sheehan, D. V. (1983). Sheehan disability scale. Handbook of Psychiatric Measures, 2, 100–102. [Google Scholar]
- Siehl, S., Robjant, K., & Crombach, A. (2020). Systematic review and meta-analyses of the long-term efficacy of narrative exposure therapy for adults, children and perpetrators. Psychotherapy Research, 1–16. doi: 10.1080/10503307.2020.1847345 [DOI] [PubMed] [Google Scholar]
- Sim, J., & Lewis, M. (2012). The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. Journal of Clinical Epidemiology, 65(3), 301–308. doi: 10.1016/j.jclinepi.2011.07.011 [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Spyridou, A., Schauer, M., & Ruf-Leuschner, M. (2015). Obstetric care providers are able to assess psyhosocial risks, identify and refer high-risk pregnant women: Validation of a short assessment tool - The KINDEX Greek version. BMC Pregnancy and Childbirth, 15(1). doi: 10.1186/s12884-015-0462-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tedeschi, R. G., & Calhoun, L. G. (1996). The posttraumatic growth inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9(3), 455–471. doi: 10.1002/jts.2490090305 [DOI] [PubMed] [Google Scholar]
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD Checklist for DSM-5 (PCL-5). National Center for PTSD. doi: 10.1037/t02622-000 [DOI] [Google Scholar]
- Wathers, F., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (2013). The Life Events Checklist for DSM-5 (LEC-5). National Center for PTSD. doi: 10.1177/1073191104269954 [DOI] [Google Scholar]
- Wozney, L., Huguet, A., Bennett, K., Radomski, A. D., Hartling, L., Dyson, M., … Newton, A. S. (2017). How do ehealth programs for adolescents with depression work? A realist review of persuasive system design components in internet-based psychological therapies. Journal of Medical Internet Research, 19(8), e266. doi: 10.2196/jmir.7573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong, T., McGrath, P. J., Yakovenko, I., Thomson, D., & Kaltenbach, E. (2021). Traumatic events from parenting children with neurodevelopmental disorders - development and validation of the parent trauma checklist. [DOI] [PubMed] [Google Scholar]
- Zimet, G. D., Dahlem, N. W., Zimet, S. G., & Farley, G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30–41. doi: 10.1207/s15327752jpa5201_ [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This manuscript doesn’t include any data.


