ABSTRACT
Background: Losing a loved one during the COVID-19 pandemic is a potentially traumatic loss that may result in symptoms of persistent complex bereavement disorder (PCBD), posttraumatic stress disorder (PTSD), and depression. To date, grief-specific cognitive-behavioural therapy (CBT) has mostly been delivered through individual face-to-face formats, while studies have shown that online treatment also yields promising results. Offering treatment online is now more than ever relevant during the pandemic and may offer important benefits compared with face-to-face CBT, such as lower costs and higher accessibility. Our expectation is that grief-specific online CBT is effective in reducing PCBD, PTSD, and depression symptoms.
Objective: Our aim is to evaluate the short-term and long-term effectiveness of grief-specific online CBT in reducing PCBD, PTSD, and depression symptom-levels for adults who lost a loved one during the COVID-19 pandemic.
Method: This study consists of two parts. In part 1, a two-armed (unguided online CBT versus waitlist controls) randomized controlled trial will be conducted. In part 2, a two-armed (guided online CBT versus unguided online CBT) controlled trial will be conducted. Symptoms of PCBD, PTSD, and depression will be assessed via telephone interviews at pre-treatment/pre-waiting period, post-treatment/post-waiting period, and six months post-treatment. Potential participants are people who lost a loved one at least three months earlier during the COVID-19 pandemic with clinically relevant levels of PCBD, PTSD, and/or depression. Analysis of covariance and multilevel modelling will be performed.
Discussion: This is one of the first studies examining the effectiveness of online grief-specific CBT. More research is needed before implementing online grief-specific CBT into clinical practice.
KEYWORDS: Coronavirus, grief, bereavement, posttraumatic stress, depression, online treatment, CBT
HIGHLIGHTS
This is the first study examining the effectiveness of online treatment in reducing psychopathology levels in people who lost loved ones during the COVID-19 pandemic.
Short abstract
Antecedentes: Perder a un ser querido durante la pandemia de COVID-19 es una pérdida potencialmente traumática que puede resultar en síntomas de trastorno de duelo complejo persistente (PCBD en su sigla en inglés), trastorno de estrés postraumático (TEPT) y depresión. Hasta la fecha, la terapia cognitivo-conductual (TCC) específica para el duelo se ha proporcionado principalmente a través de formatos individuales cara a cara, mientras que los estudios han demostrado que el tratamiento en línea también produce resultados prometedores. Ofrecer tratamiento en línea es ahora más relevante que nunca durante la pandemia y puede ofrecer importantes beneficios en comparación con la TCC presencial, como menores costos y mayor accesibilidad. Nuestra expectativa es que la TCC en línea específica para el duelo sea eficaz para reducir el PCBD, el TEPT y los síntomas de depresión.
Objetivo: Nuestro objetivo es evaluar la efectividad a corto y largo plazo de la TCC en línea específica para el duelo en la reducción de los niveles de PCBD, TEPT y síntomas de depresión en adultos que perdieron a un ser querido durante la pandemia de COVID-19.
Método: Este estudio consta de dos partes. En la parte 1, se llevará a cabo un ensayo controlado aleatorio de dos brazos (TCC en línea no guiado versus controles con la lista de espera). En la parte 2, se llevará a cabo un ensayo controlado de dos brazos (TCC en línea guiada versus TCC en línea no guiada). Los síntomas de PCBD, TEPT y depresión se evaluarán mediante entrevistas telefónicas en el período de pretratamiento/pre-espera, post-tratamiento/post-período de espera y seis meses post-tratamiento. Los participantes potenciales son personas que perdieron a un ser querido al menos tres meses antes durante la pandemia de COVID-19 con niveles clínicamente relevantes de PCBD, TEPT y/o depresión. Se realizarán análisis de covarianza y modelado multinivel.
Discusión: Este es uno de los primeros estudios que examinan la efectividad de la TCC en línea específica para el duelo. Se necesita más investigación antes de implementar la TCC en línea específica para el duelo en la práctica clínica.
PALABRAS CLAVES: Coronavirus, Luto, Duelo, Estrés post traumático, Depresión, Tratamiento online, TCC
Short abstract
背景: 在 COVID-19 疫情期间丧亲是一种潜在的创伤性损失, 可能导致持续性复杂丧亲症 (PCBD), 创伤后应激障碍 (PTSD) 和抑郁症状。迄今为止, 哀伤特定的认知行为疗法 (CBT) 主要通过个人面对面的形式提供, 而研究表明, 在线治疗也产生了有前景的结果。提供在线治疗在疫情期间比以往任何时候都更切题, 并且相较于面对面的 CBT, 可能提供重要的好处, 例如成本更低和易获得性更高。我们的期望是哀伤特定的在线 CBT 可有效减少 PCBD, PTSD 和抑郁症状。
目的: 我们旨在评估哀伤特定的在线 CBT 在减少 COVID-19 疫情期间成年丧亲者PCBD, PTSD 和抑郁症状水平方面的短期和长期有效性。
方法: 本研究由两部分组成。在第 1 部分中, 将进行一项双臂随机对照试验 (无指导的在线 CBT 与等候名单对照) 。在第 2 部分中, 将进行一项双臂对照试验 (指导性在线 CBT 与非指导性在线 CBT) 。
PCBD, PTSD 和抑郁症的症状将通过电话访谈在治疗前/等待期, 治疗后/等待期和治疗后六个月进行评估。潜在参与者是在 COVID-19 疫情期间至少三个月前丧亲且具有临床相关水平的 PCBD, PTSD 和/或抑郁的人。将进行协方差分析和多级建模。
讨论: 这是考查哀伤特定在线 CBT 有效性的首批研究之一。在将哀伤特定在线 CBT 应用于临床实践之前, 需要进行更多的研究。
关键词: 新冠病毒, 哀伤, 丧亲, 创伤后应激, 抑郁, 在线治疗, CBT
The first death due to coronavirus disease 2019 (COVID-19) in the Netherlands was registered in early March 2020. About one year later, over 16,500 Dutch people have died after being infected with COVID-19 (Coronadashboard Rijksoverheid, 2021). The death of a loved one is one of the most common potentially traumatic events that people may experience (Benjet et al., 2016). One out of ten people bereaved by a natural death (e.g. illness) develops persistent and severe grief symptoms, including persistent complex bereavement disorder1 (PCBD) (Lundorff, Holmgren, Zachariae, Farver-Vestergaard, & O’Connor, 2017). PCBD is entered in the fifth edition of the Diagnostic and Statistical Manual of mental disorders (DSM-5; American Psychiatric Association, 2013) in the section ‘Other specified trauma- and stressor-related disorders’. PCBD can be diagnosed if a person experiences persistent longing for the deceased, symptoms of reactive distress and social/identity disruption, after the death of a loved one at least 12 months earlier. Although PCBD is distinguishable from posttraumatic stress disorder (PTSD) and depression (Boelen, van de Schoot, van den Hout, de Keijser, & Van Den Bout, 2010; Djelantik, Smid, Kleber, & Boelen, 2017; Lenferink, de Keijser, Smid, Djelantik, & Boelen, 2017; Malgaroli, Maccallum, & Bonanno, 2018; O’Connor, Lasgaard, Shevlin, & Guldin, 2010), a meta-analysis shows that PCBD in an estimated 49% and 63% of the cases co-occurs with PTSD and depression, respectively (Komischke-Konnerup, Zachariae, Johannsen, Nielsen, & O’Connor, 2021). Losing a loved one due to an unnatural death, for instance an unexpected or violent death, increases the risk of developing clinically relevant PCBD up to nearly 50% (cf., Djelantik, Smid, Mroz, Kleber, & Boelen, 2020). This elevated risk of developing symptoms after a traumatic loss can be partially explained by the disruption of daily life and the violation of assumptions that the world is safe, benign, and predictable (Boelen, de Keijser, & Smid, 2015; Janoff-Bulman, 1989). The death of a loved one during the COVID-19 pandemic is a potentially traumatic loss, likely leading to higher rates of PCBD, PTSD, and depression compared with the natural death of a loved one (Eisma, Boelen, & Lenferink, 2020). A study by Eisma, Tamminga, Smid, and Boelen (2021) offers preliminary data supporting this claim. They found that COVID-19 bereavement resulted in higher acute grief levels compared to natural bereavement (but not compared to unnatural bereavement).
This elevated risk of psychopathology due to bereavement during the pandemic may be explained by at least five corona-related factors. First, because of the social distancing measures, it is difficult or even impossible to visit a loved one who is dying. Both grief rituals prior to death and grief rituals after death (e.g. attending a funeral) are, therefore, possibly hampered. Traditional grief rituals play an important role in processing the loss, e.g. by facilitating confrontation with the irreversibility of the death. Not being able to perform such rituals can block emotional processing (Boelen, van den Hout, & van den Bout, 2006). Second, physical social support is not or hardly possible because of social-distancing and self-quarantine measures. Limitations in engaging in social activities can lead to social isolation exacerbating grief symptoms (Lobb et al., 2010). Third, the COVID-19 pandemic leads to increased uncertainty (e.g. about losing one’s employment), anxiety (e.g. about getting sick), loneliness, and stress in the general population (Brooks et al., 2020; Cao et al., 2020). These secondary stressors may fuel distress following the death of a loved one. Fourth, deaths due to the coronavirus are likely to occur in social groups, e.g. within families and groups of friends. People bereaved due to COVID-19 are often part of the infection cycle and are therefore likely to experience multiple losses during the pandemic. Experiencing multiple deaths in a relatively short period of time elevates the risk of stagnating in the grieving process (Hengst, Smid, & Laban, 2018). Fifth, assumed (shared) responsibility for the death of a close person, for instance after a traffic accident of suicide, is a risk factor for elevated grief complaints (Erlangsen et al., 2017). Because prevention of contamination is such a focal point in the current pandemic, bereaved people may think that they are responsible for having contaminated the deceased, causing guilt and self-blame, impairing recovery from the loss. The interaction between the increase in number of deaths on the one hand and the corona-related factors on the other hand will likely lead to an increase in the number of people in need of bereavement care (Eisma et al., 2020; Kokou-Kpolou, Fernández-Alcántara, & Cénat, 2020). Based on reviews (Boelen & Smid, 2017a; Doering & Eisma, 2016), grief-specific cognitive-behavioural therapy (CBT) is considered the most effective treatment with PCBD (Boelen, Lenferink, & Spuij, 2021; Boelen & van den Bout, 2017; Rosner, Bartl, Pfoh, Kotoučová, & Hagl, 2015; Shear, Frank, Houck, & Reynolds, 2005). CBT addresses negative cognitions (e.g. about one’s life or the world) and avoidance behaviours with exposure, cognitive restructuring, and behavioural activation. During the pandemic, psychological interventions are often delivered remotely, such as through the Internet (Boelen, Eisma, Smid, de Keijser, & Lenferink, 2020). For instance, face-to-face interventions needed to switch to being delivered online. Consequently, it is likely that bereaved people searching for professional grief help look for support online. However, evidence-based online CBT for grief-related distress is not yet widely available. Therefore, it is crucial to enhance knowledge about the effectiveness of online grief-specific CBT in order to be able to offer bereaved people during the COVID-19 pandemic adequate mental health care.
Online grief-specific CBT could also address the care needs of bereaved people when the pandemic is over. It is likely that waiting lists for face-to-face interventions in general will increase, because providing care remotely is not feasible for all patients (e.g. people suffering from severe psychiatric conditions). In addition, people may have postponed using mental health care services during the pandemic, because of COVID-19 restrictions or fear of contamination. This may further lengthen the waitlists. As a result, it is likely that it will be very challenging to receive face-to-face grief-specific CBT for bereaved people in need of support during and after the pandemic. Therefore, online grief-specific CBT could be a solution. Furthermore, this approach may bring other benefits too. Offering CBT via the Internet might decrease the barrier for seeking treatment, because it is independent of geographical location. This could counteract barriers to care reported by bereaved people, including problems with finding help, transportation difficulties or problems with planning sessions (Lenferink, de Keijser, Eisma, Smid, & Boelen, 2020; Lichtenthal et al., 2015). Additionally, offering CBT online could lower treatment costs, thereby making treatment more easily accessible to people who need support (Boelen et al., 2020).
Several studies have shown that online treatment is effective in reducing PTSD and depression symptoms (Josephine, Josefine, Philipp, David, & Harald, 2017; Lewis, Roberts, Simon, Bethell, & Bisson, 2019). The effectiveness of online treatment depends on several factors, including the target group, content of treatment, and degree of therapeutic guidance (Andersson et al., 2009). The largest treatment effects have been found in online treatments that 1) are targeted at people with clinically relevant symptom-levels (vs. low or subclinical symptom-levels), 2) are extensive and comprehensive in the description of the content (instead of limited content), and 3) are guided by a therapist through email or telephone (compared to no or minimal guidance; Andersson et al., 2009). To our knowledge, online grief-specific CBT-based interventions have only been evaluated in four clinical trials (Eisma et al., 2015; Kersting et al., 2013; Litz et al., 2014; Wagner, Knaevelsrud, & Maercker, 2006). However, these trials had some limitations. Specifically, they were solely focused on recently (Litz et al., 2014) or perinatally bereaved people (Kersting et al., 2013), relied on relatively small samples (Eisma et al., 2015; Wagner et al., 2006), or had considerable dropout rates (Eisma et al., 2015). Furthermore, the comparability of the findings between the studies is restricted, because the content of the treatment varied greatly; different elements of CBT were offered, for instance exposure or behavioural activation only (Eisma et al., 2015) or the treatment only consisted of writing assignments (Kersting et al., 2013; Wagner et al., 2006). Taken together, more research is needed before online grief-specific CBT can be implemented in clinical practice.
The research introduced in the present study protocol consists of two parts. Our aim in part 1 is to evaluate the short-term and long-term effectiveness of unguided grief-specific online CBT (vs. waitlist controls) in reducing PCBD, PTSD, and depression symptom-levels for adults who lost a loved one during the COVID-19 pandemic. Our aim in part 2 is to evaluate the short-term and long-term effectiveness of guided grief-specific online CBT (vs. unguided online grief-specific CBT) in reducing PCBD, PTSD, and depression symptom-levels for adults who lost a loved one during the COVID-19 pandemic. In part 1 of the study, our first expectation is that people allocated to the unguided online CBT condition will show lower symptom-levels of PCBD, PTSD, and depression post-treatment compared with waitlist controls post-waiting period (Hypothesis 1). Our second expectation is that treatment effects on PCBD, PTSD, and depression symptom-levels will persist from pre-treatment through six months post-treatment (Hypothesis 2). In part 2 of the study, our first expectation is that both guided and unguided online CBT lead to a decrease in the severity of PCBD, PTSD, and depression symptom-levels immediately and six months after treatment (Hypothesis 3). Our second expectation is that participants allocated to the therapist-guided online CBT condition will show a stronger decrease in PCBD, PTSD, and depression symptom-levels post-treatment and at six months post-treatment than participants allocated to the unguided online CBT condition (Hypothesis 4).
1. Method
1.1. Design
In part 1, a mono-centre randomized controlled trial will be conducted examining the effectiveness of unguided online CBT in reducing PCBD, PTSD, and depression compared to a waitlist control condition. Participants in the unguided online CBT condition will receive treatment within one week after randomization. Participants allocated to the waitlist control condition will receive treatment after eight weeks of waiting. Inclusion of a waitlist control condition optimizes our recruitment efforts by making sure all participants will receive treatment. Furthermore, it enables a treatment vs. no treatment comparison, which provides knowledge about the effects of treatment relative to natural remission.
In part 2, a multi-centre controlled trial will be conducted evaluating the effectiveness of guided online CBT vs. unguided online CBT in reducing PCBD, PTSD, and depression symptoms. The guided online CBT will be carried out by therapists working at one of the five collaborating Dutch mental health care institutes (i.e. Reinier van Arkel, ARQ Centrum’45, GGZ Friesland, Expertisecentrum Trauma en Verlies and Prisma Psychologie). All participants from part 1 of the study (including the ones receiving immediate treatment and those receiving treatment after the waiting period) will serve as a control group for part 2 (i.e. the unguided online CBT group). After having recruited sufficient participants for part 1 of the study, people can only sign up for part 2 of the study. All participants who sign up for part 2 will receive treatment within one week after allocation.
The decision for a two-part design instead of a three-armed trial (guided online CBT vs. unguided online CBT vs. waitlist controls) was made because of pragmatic reasons. We started part 1 in July 2020. After we started data-collection of part 1 we received funding to start part 2. The study design was approved by the Medical Ethics Committee at the University Medical Center Utrecht (UMCU) in the Netherlands (NL74518.041.20). Both part 1 (NL8993) and part 2 of the study (NL9485) have been registered in the Netherlands Trial Register.
1.2. Participants
Dutch-speaking family members, spouses or friends of people who died at least three months earlier during the COVID-19 pandemic (i.e. from early March 2020 until present), either due to the coronavirus or other causes, are potentially eligible for participation. We chose to include people who lost their loved one(s) at least three months earlier, because prior research showed that delivering an early intervention for clinically relevant grief levels is effective (Litz et al., 2014). Additional inclusion criteria are being aged 18 years or older and experiencing clinically relevant levels of PCBD, PTSD, and/or depression. People will be excluded from the study if they 1) do not master the Dutch language, 2) do not have access to Internet, 3) suffer from a psychotic disorder, and/or 4) suffer from suicidality. Individuals who are not eligible to participate in the study will be referred to their general practitioner or to one of the collaborating mental health care institutes. We expect to recruit most participants through collaborating mental health care institutes Reinier van Arkel, ARQ Centrum’45, and GGZ Friesland. In addition, we expect to recruit participants by setting up an online campaign on social media, through media attention, and a website that has been developed for the current study (www.rouwencorona.nl). Recruitment of participants for part 1 started in October 2020 and ended the 1st of February 2021. Recruitment of participants for part 2 started in March 2021 and will continue until fall 2021.
1.3. Procedure
For part 1, after having received the signed consent form, a telephone interview will be planned and conducted to screen for eligibility in light of the inclusion and exclusion criteria. Symptom-levels of PCBD, PTSD, and depression of all participants will be assessed through telephone interviews at pre-treatment or pre-waiting, post-treatment or post-waiting, and six months post-treatment (see Figure 1). A trained master-level psychologist (LR) will conduct the interviews.
Figure 1.
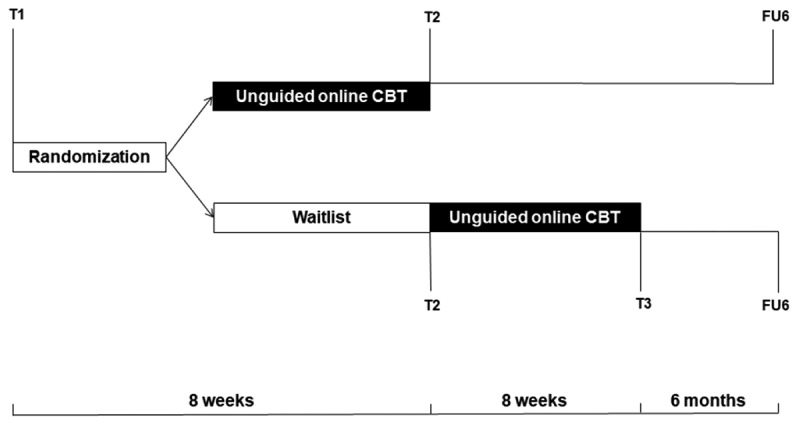
Design of the randomized controlled trial
Note. CBT = cognitive-behavioural therapy, T1 = pre-treatment/pre-waiting period assessment, T2 = post-treatment/post-waiting period assessment, T3 = post-treatment assessment (for the waitlist control group), FU6 = six months post-treatment assessment.
Eligible participants will be randomized to the unguided online CBT condition or to the waitlist control condition. A blocking randomization procedure will be carried out by LR. An allocation ratio of 1:1 will be implemented, ensuring that all participants are equally allocated across the two conditions. The results of the randomization procedure will be communicated to participants via email. There are no costs for participating in part 1 of the study.
For part 2, a telephone interview will be planned and conducted (the same interview will be used as in part 1 of the study) after receiving the signed consent form at 1) pre-treatment, 2) post-treatment and 3) six months post-treatment (see Figure 2). As mentioned earlier, all eligible participants will be allocated to the guided online CBT condition. For part 1 and part 2, participants voluntarily withdrawing from the study will not receive an invitation for the post-treatment assessments. The costs for participation consist of payment of the treatment costs that are not covered by the participants’ health insurance.
Figure 2.
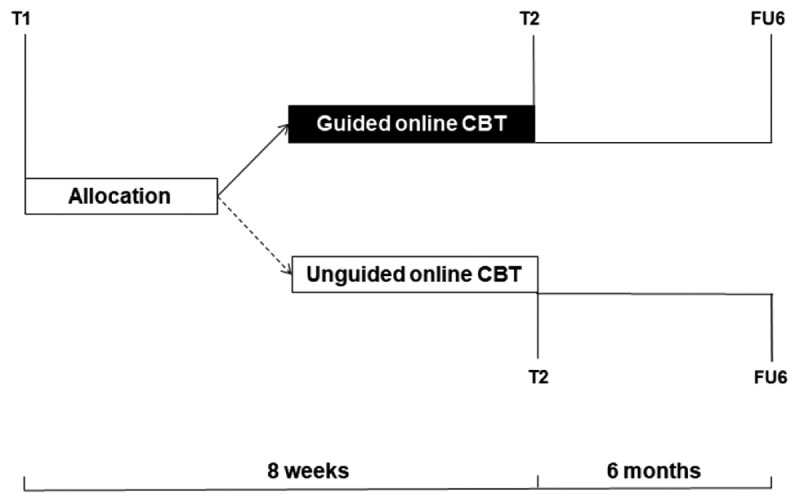
Design of the controlled trial
Note. CBT = cognitive-behavioural therapy, T1 = pre-treatment assessment, T2 = post-treatment assessment, FU6 = six months post-treatment assessment.
1.4. Materials
1.4.1. Outcome measures
PCBD symptoms are the primary outcome and will be assessed with 18 items from the Traumatic Grief Inventory – Clinician Administered2 (TGI-CA; Lenferink et al., in press). The TGI-CA is the interview version of the self-report questionnaire the Traumatic Grief Inventory – Self Report+ (TGI-SR+; Lenferink et al. 2022). The 22-item TGI-SR+ is an extension of the 18-item TGI-SR that has shown to be a valid and reliable instrument to assess PCBD symptoms (Boelen, Djelantik, de Keijser, Lenferink, & Smid, 2018; Boelen & Smid, 2017b; Lenferink, et al., 2022). The TGI-CA measures PCBD symptoms as included in the DSM-5 (American Psychiatric Association, 2013) and PGD symptoms as included in the ICD-11 (WHO, 2018) and DSM-5 text revision (American Psychiatric Association, 2020). The TGI-CA consists of 22 items, rated on a 5-point Likert scale ranging from 1 = never, through 5 = always. The instruction of the original questionnaire is altered from ‘the death of your loved one’ to ‘the death of your loved one(s) during the corona pandemic’.
Following the diagnostic scoring rule of the DSM-5 (American Psychiatric Association, 2013), participants are considered to have clinically relevant PCBD symptom-levels when scoring at least 3 (sometimes) on at least one of the B-cluster symptoms (representing separation distress; item 1, 2, 3, and item 14), six C-cluster symptoms (representing reactive distress and identity or social disruption; item 4–11 and item 15–18), and the D-cluster symptom (representing functional impairment; item 13) and/or report a total score of 54 or higher on items 1 through 18 (Boelen et al., 2018).
PTSD symptoms will be assessed with the 20-item PTSD Checklist for DSM-5 (PCL-5; Blevins, Weathers, Davis, Witte, & Domino, 2015; Boeschoten, Bakker, Jongedijk, & Olff, 2014). Participants rate how often they were bothered by each symptom (e.g. ‘In the past month, how much were you bothered by: Repeated, disturbing dreams of the stressful experience?’) on a 5-point Likert scale with anchors 0 = not at all, through 4 = extremely. The wording of the instruction and the items of the original questionnaire are altered from referring to the ‘stressful experience’ to the ‘the death of your loved one(s) during the corona pandemic’. Psychometric properties of the PCL-5 are adequate (Blevins et al., 2015). Each item rated as at least 2 (moderately) will be considered as a symptom endorsed. Following the DSM-5 diagnostic rule (American Psychiatric Association, 2013), participants are considered to report clinically relevant PTSD symptom-levels when endorsing at least one B item (item 1–5), one C item (item 6, 7), two D items (item 8–14), and two E items (item 15–20), and/or report a total score of 31 or higher (Weathers et al., 2013).
Depression symptoms will be assessed with the Patient Health Questionnaire (PHQ-9; Kroenke, Spitzer, & Williams, 2001). The PHQ-9 consists of nine items (e.g. ‘Over the last 2 weeks, how often have you been bothered by having little interest or pleasure in doing things?’). Participants select an answer option on a 4-point Likert scale (0 = not at all, through 3 = nearly every day) describing how often he/she was bothered by each symptom during the past two weeks. Psychometric properties of the PHQ-9 are adequate (Kroenke et al., 2001). According to Kroenke et al. (2001) a total score of 10 or higher reflects probable caseness for major depression and will therefore be used as cut-off score in the current study.
1.4.2. Other measures
Corona-related stressors will be assessed with the COVID-19 Stressful Events self-report questionnaire (Freedman, Greene, & Armour, 2020a) and with the COVID-19 Concerns self-report questionnaire (Freedman, Greene, & Armour, 2020b). The first includes 13 items and measures stressful events related to COVID-19 (e.g. ‘Have you been tested for coronavirus’). The second consists of nine items and assesses concerns and worries related to COVID-19 (e.g. ‘How worried are you being quarantined?’) on a 5-point Likert scale with 1 = not at all, through 5 = extremely.
Characteristics of participants (i.e. gender, age, educational level, country of birth), the deceased (i.e. age, date of death), the loss (i.e. kinship to deceased, time since loss, cause of loss), corona-related stressors (i.e. attendance at funeral, experiencing multiple losses), and prior and current use of psychological interventions will be registered.
1.5. Treatment
The online CBT treatment is targeted at people with clinically relevant levels of PCBD, PTSD and/or depression at least three months post-bereavement and could therefore be considered a secondary preventive intervention and not a primary preventive intervention (i.e. interventions targeted at all bereaved people; Schut & Stroebe, 2005). Moreover, studies show that elevated grief, PTSD, and depression levels in the first six months after a loss strongly predict elevated grief, PTSD, and depression levels later in time (Boelen & Lenferink, 2020, 2021). In both part 1 and part 2 of the study, the treatment encompasses eight weekly sessions delivered in a period of maximum 12 weeks. Eight sessions have shown to be sufficient to generate moderate to large treatment effects (Van Denderen, de Keijser, Stewart, & Boelen, 2018). For part 1 and part 2 of the study, the same online CBT treatment will be offered, in which the main target will be PCBD levels. The first session consists of psycho-education regarding possible emotional reactions to the death of a loved one during the COVID-19 pandemic and processes that might facilitate or impede recovery. Additionally, participants are encouraged to invite a close person to the online treatment for support. When a close person has been connected to the programme, (s)he will receive information on possible emotional reactions to losing a loved one and will receive information about how (s)he can support the participant. Sessions 2, 3, and 4 are spent on exposure, in which participants will focus on the story of the loss and its circumstances. Participants are encouraged to confront stimuli they tend to avoid, for instance by structured writing assignments drawn from Wagner, Knaevelsrud, and Maercker (2005) and Wagner and Maercker (2007). Sessions 5 and 6 contain cognitive restructuring assignments, in which participants are helped to identify and alter negative thought patterns about the self, life and the future by performing behavioural experiments and filling in thought diaries. Sessions 7 and 8 consist of behavioural activation assignments, focused on identifying valued activities and making plans to attain valued goals. Approximately two hours are spent on each session. During treatment, short pre-recorded video messages are shown in which a therapist provides information about treatment elements. These video messages can be read in text as well. At the beginning of the treatment, each participant can choose between either a male or female video therapist, presenting the same information. There is no communication with the video therapists.
In part 1 of the study, participants’ adherence to the treatment protocol will be monitored by one of the researchers (LR) through summarizing logdata of the participants, including total number of lessons completed. Treatment progress will be checked once a week. In case a participant is behind in treatment, LR will send an encouragement to the participant to continue treatment without providing therapeutic support. In part 2, a therapist will guide the online treatment through email contact. All therapists involved in the treatment are licenced clinical psychologists and will receive an 8-hour online training about the treatment protocol. Supervision of a participant consists of both providing feedback on the assignments and sending an encouragement once a week.
The online CBT treatment is specifically developed to be delivered online. The content of the treatment will be presented via a secured website, which is designed by the Dutch company Therapieland (www.therapieland.nl). Therapieland is not involved in formulation of the research questions, the design of the study or the content of the treatment, nor in analysing and reporting the results. During participation in the study, all participants are allowed to receive any other form of psychosocial, legal, and/or medical support. The use of co-intervention during participation in the study will be registered and considered in the analyses.
1.6. Analyses
To examine the short-term effects of unguided online CBT (vs. waitlist controls) in part 1 (Hypothesis 1), three separate analyses of covariance (ANCOVAs) will be conducted with mean symptom-levels of PCBD, PTSD, or depression at post-treatment (or post-waiting period) as dependent variables, condition (unguided online CBT vs. waitlist controls) as independent variable, and baseline symptom-levels of PCBD, PTSD, or depression and the use of psychological co-intervention as covariates. To examine the long-term effects of unguided online CBT at six months post-treatment on symptom-levels of PCBD, PTSD, or depression (Hypothesis 2), three multilevel models will be run with PCBD, PTSD, and depression as outcome variables, respectively, and time as fixed effect (dummy coded with the baseline measures (T1) as reference category). Data of all participants entering the study will be included in the analyses (i.e. intention-to-treat analysis).
In part 2 of the study, the effects of guided online CBT (vs. unguided online CBT) at post-treatment and at six months post-treatment on symptom-levels of PCBD, PTSD, and depression (Hypothesis 3 and Hypothesis 4) will be evaluated. To examine this, three multilevel models will be run with PCBD, PTSD, or depression as outcome variables and time (dummy coded with pre-treatment measures as reference category), condition, and time*condition as main effects. Data of all participants entering the study will be included in the analyses.
1.7. Sample size
For part 1, the sample size calculation is based on the analyses for testing Hypothesis 1. In order to find a difference between the two conditions (unguided online CBT vs. waitlist controls) of at least a large effect size (cf., Eisma et al., 2015; Litz et al., 2014), with a power of 80%, a sample size of 52 participants is sufficient. However, when considering a dropout rate of 19% (based on the mean dropout rate as reported in Currier, Holland, & Neimeyer, 2010), a total sample size of 62 (52 + 10) participants is needed. For part 2, our sample size calculation is based on testing Hypothesis 3 and Hypothesis 4. Considering prior research on therapist-guided vs. unguided online treatment for people with symptoms of depression and anxiety (Spek et al., 2007), we expect a medium effect size in favour of the therapist-guided online CBT. To find a difference between groups (guided vs. unguided online CBT) with a power of 80%, a medium effect size (f = 0.25), an α of 0.05 and a strong association (r = .50) between the pre-assessment, post-assessment and six months follow-up assessment, a total sample size of 86 participants is sufficient. Again, considering a dropout rate of 19%, a sample size of 102 (86 + 16) participants is needed. To test the hypotheses in part 2, multilevel analyses will be executed since our data are nested (i.e. repeated measures (level 1) within participants (level 2)). However, it is not feasible to perform a power calculation for multilevel analyses (Snijders & Bosker, 2012). For this reason, our power calculation is based on a repeated measures analysis of variance.
2. Discussion
Losing a loved one during the COVID-19 pandemic is a potentially traumatic loss, increasing the risk of developing PCBD, PTSD, and depression (Eisma et al., 2020). As far as we know, only four clinical trials examined the effectiveness of online grief-specific CBT-based interventions for reducing distress in bereaved people (Eisma et al., 2015; Kersting et al., 2013; Litz et al., 2014; Wagner et al., 2006). To our knowledge, the present study will be the first worldwide examining the effectiveness of an online CBT treatment that contains three interventions central to CBT for PCBD: exposure, cognitive restructuring, and behavioural activation (Boelen & van den Bout, 2017).
Strengths of the present study include: (1) the inclusion of both an intervention group and a waitlist control group in part 1, (2) a focus on three outcome measures (PCBD, PTSD, and depression), (3) PCBD, PTSD, and depression symptoms being assessed with clinical telephone interviews rather than by self-report and (4) the assessment of both short-term and long-term effects of the intervention.
Nevertheless, the present study has several potential limitations. First, it will be impossible to blind the participants as well as the researchers. Therefore, therapy expectancy could be a potential risk of bias. Secondly, in part 2 of the study, it will be impossible to carry out a randomization procedure due to pragmatic reasons. In addition, the waitlist control group in part 1 of the study starts with the unguided online CBT after eight weeks of waiting. Therefore, we can only compare the unguided online CBT group to the waitlist control group at the post-treatment assessment and not at the six months post-treatment assessment. Furthermore, potential mediators (e.g. changes in negative cognitions, avoidance behaviour) will not be examined which would have been valuable for examining potential mechanisms of change. Finally, we will actively look for methods to recruit participants, which could restrict the generalizability of our findings to bereaved people who seek treatment themselves.
To date, online evidence-based grief-specific CBT is not yet widely available. For this reason, our expectation is that the results of the current study will be of high value for clinical practice. Insights from this study will improve knowledge about the short-term and long-term effectiveness of online CBT for bereaved people during the COVID-19 pandemic. Results are expected to be highly relevant for future research as well, in which the effectiveness of online grief-specific CBT could be further examined, for instance by comparing the effects of guided online CBT (i.e. minimal therapeutic assistance) to guided online CBT with more extensive therapeutic assistance (i.e. therapeutic assistance via telephone or video calls).
Funding Statement
Part 1 was supported by the COVID-19 Fund of the Faculty of Social and Behavioural Sciences of Utrecht University and part 2 by Fonds Slachtofferhulp.
Notes
A diagnosis regarding severe and persistent grief-related distress has also been introduced as ‘prolonged grief disorder’ in the eleventh edition of the International Classification of Diseases (ICD-11; WHO, 2018) and the forthcoming text-revision of the DSM-5 (DSM-5-TR; American Psychiatric Association, 2020). However, in this study we will use the term PCBD, in accord with the DSM-5 (American Psychiatric Association, 2013), since the DSM-5 is widely used by mental health care practitioners in the Netherlands at the time of conducting this study.
Given the upcoming change in the DSM-5-TR replacing PCBD with PGD, we will repeat the analyses for the primary outcome using the PGD DSM-5-TR items in the TGI-CA.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data Availability Statement
Data sharing is not applicable for this article as data were not included.
References
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- American Psychiatric Association . (2020). View and comment on recently proposed changes to DSM–5. Arlington, VA: American Psychiatric Association. Accessed on 15 September 2021. Retrieved from https://www.psychiatry.org/psychiatrists/practice/dsm/proposed-changes [Google Scholar]
- Andersson, G., Carlbring, P., Berger, T., Almlöv, J., & Cuijpers, P. (2009). What makes internet therapy work? Cognitive Behaviour Therapy, 38(Sup1), 55–10. doi: 10.1080/16506070902916400 [DOI] [PubMed] [Google Scholar]
- Benjet, C., Medina-Mora, M. E., Bromet, E., Karam, E. G., Kessler, R. C., Shahly, V., … Koenen, K. C. (2016). The epidemiology of traumatic event exposure worldwide: Results from the world mental health survey consortium. Psychological Medicine, 46(2), 327–343. doi: 10.1017/S0033291715001981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. doi: 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Boelen, P. A., de Keijser, J., & Smid, G. E. (2015). Cognitive-behavioral variables mediate the impact of violent loss on post-loss psychopathology. Psychological Trauma: Theory, Research, Practice and Policy, 7(4), 382–390. doi: 10.1037/tra0000018 [DOI] [PubMed] [Google Scholar]
- Boelen, P. A., Djelantik, A. A. A. M. J., de Keijser, J., Lenferink, L. I. M., & Smid, G. E. (2018). Further validation of the traumatic grief inventory-self report (TGI-SR): A measure of persistent complex bereavement disorder and prolonged grief disorder. Death Studies. doi: 10.1080/07481187.2018.1480546 [DOI] [PubMed] [Google Scholar]
- Boelen, P. A., Eisma, M. C., Smid, G. E., de Keijser, J., & Lenferink, L. I. M. (2020). Remotely delivered cognitive behavior therapy for disturbed grief during the covid-19 crisis: Challenges and opportunities. Journal of Loss & Trauma doi: 10.1080/15325024.2020.1793547. [DOI] [Google Scholar]
- Boelen, P. A., Lenferink, L. I. M., & Spuij, M. (2021). CBT for prolonged grief in children and adolescents: A randomized clinical trial. The American Journal of Psychiatry, 178(4), 294–304. doi: 10.1176/appi.ajp.2020.20050548 [DOI] [PubMed] [Google Scholar]
- Boelen, P. A., & Lenferink, L. I. M. (2020). Symptoms of prolonged grief, posttraumatic stress, and depression in recently bereaved people: Symptom profiles, predictive value, and cognitive behavioural correlates. Social Psychiatry and Psychiatric Epidemiology: The International Journal for Research in Social and Genetic Epidemiology and Mental Health Services, 55(6), 765–777. doi: 10.1007/s00127-019-01776-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boelen, P. A., & Lenferink, L. I. (2021). Prolonged grief disorder in DSM-5-TR: Early predictors and longitudinal measurement invariance. The Australian and NewZealand Journal of Psychiatry, 48674211025728 doi: 10.1177/00048674211025728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boelen, P. A., & Smid, G. E. (2017a). Disturbed grief: Prolonged grief disorder and persistent complex bereavement disorder. BMJ, 357. doi: 10.1136/bmj.j2016 [DOI] [PubMed] [Google Scholar]
- Boelen, P. A., & Smid, G. E. (2017b). The Traumatic Grief Inventory Self Report version (TGI-SR): Introduction and preliminary psychometric evaluation. Journal of Loss & Trauma, 22(3), 196–212. doi: 10.1080/15325024.2017.1284488 [DOI] [Google Scholar]
- Boelen, P. A., van de Schoot, R., van den Hout, M. A., de Keijser, J., & van den Bout, J. (2010). Prolonged grief disorder, depression, and posttraumatic stress disorder are distinguishable syndromes. Journal of Affective Disorders, 125(1–3), 374–378. doi: 10.1016/j.jad.2010.01.076 [DOI] [PubMed] [Google Scholar]
- Boelen, P. A., & van den Bout, J. (2017). Protocollaire behandeling van persisterende complexe rouwstoornis [Protocolized treatment of persistent complex bereavement disorder]. In Keijsers G., van Minnen A., Verbraak M., Hoogduin K., and Emmelkamp P. (Eds.), Protocollaire behandelingen voor volwassenen met psychische klachten (pp. 125–173) (1st ed.). Amsterdam: Boom. [Google Scholar]
- Boelen, P. A., van den Hout, M. A., & van den Bout, J. (2006). A cognitive-behavioral conceptualization of complicated grief. Clinical Psychology: Science and Practice, 13(2), 109–128. doi: 10.1111/j.1468-2850.2006.00013.x [DOI] [Google Scholar]
- Boeschoten, M. A., Bakker, A., Jongedijk, R. A., & Olff, M. (2014). PTSS checklist voor de DSM-5 (PCL-5). Diemen: Arq Psychotrauma Expert Groep. [Google Scholar]
- Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. doi: 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao, W., Fang, Z., Hou, G., Han, M., Xu, X., Dong, J., & Zheng, J. (2020). The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research, 287, 112934. doi: 10.1016/j.psychres.2020.112934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coronadashboard Rijksoverheid .(2021). Totaal aantal overleden COVID-19 patiënten. The Hague: Rijksoverheid. Accessed on 30 March 2021. Retrieved from https://coronadashboard.rijksoverheid.nl/landelijk/sterfte [Google Scholar]
- Currier, J., Holland, J., & Neimeyer, R. (2010). Do CBT-based interventions alleviate distress following bereavement? a review of the current evidence. International Journal of Cognitive Therapy, 3(1), 77–93. doi: 10.1521/ijct.2010.3.1.77 [DOI] [Google Scholar]
- Djelantik, A. A. A. M. J., Smid, G. E., Kleber, R. J., & Boelen, P. A. (2017). Symptoms of prolonged grief, post-traumatic stress, and depression after loss in a Dutch community sample: A latent class analysis. Psychiatry Research, 247, 276–281. doi: 10.1016/j.psychres.2016.11.023 [DOI] [PubMed] [Google Scholar]
- Djelantik, A. A. A. M. J., Smid, G. E., Mroz, A., Kleber, R. J., & Boelen, P. A. (2020). The prevalence of prolonged grief disorder in bereaved individuals following unnatural losses: Systematic review and meta regression analysis. Journal of Affective Disorders, 265, 146–156. doi: 10.1016/j.jad.2020.01.034 [DOI] [PubMed] [Google Scholar]
- Doering, B. K., & Eisma, M. C. (2016). Treatment for complicated grief: State of the science and ways forward. Current Opinion in Psychiatry, 29(5), 286–291. doi: 10.1097/YCO.0000000000000263 [DOI] [PubMed] [Google Scholar]
- Eisma, M. C., Boelen, P. A., & Lenferink, L. I. M. (2020). Prolonged grief disorder following the coronavirus (covid-19) pandemic. Psychiatry Research, 288, 288, 113031. doi: 10.1016/j.psychres.2020.113031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisma, M. C., Boelen, P. A., Van den Bout, J., Stroebe, W., Schut, H., Lancee, J., & Stroebe, M. (2015). Internet-based exposure and behavioral activation for complicated grief and rumination: A randomized controlled trial. Behavior Therapy, 46(6), 729–748. doi: 10.1016/j.beth.2015.05.007 [DOI] [PubMed] [Google Scholar]
- Eisma, M. C., Tamminga, A., Smid, G. E., & Boelen, P. A. (2021). Acute grief after deaths due to COVID-19, natural causes and unnatural causes: An empirical comparison. Journal of Affective Disorders, 278, 54–56. doi: 10.1016/j.jad.2020.09.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erlangsen, A., Runeson, B., Bolton, J. M., Wilcox, H. C., Forman, J. L., Krogh, J., … Conwell, Y. (2017). Association between spousal suicide and mental, physical, and social health outcomes: A longitudinal and nationwide register-based study. JAMA Psychiatry, 74(5), 456–464. doi: 10.1001/jamapsychiatry.2017.0226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman, S., Greene, T., & Armour, C. (2020a). COVID-19 stressful events. doi: 10.17605/OSF.IO/YQR2D [DOI] [Google Scholar]
- Freedman, S., Greene, T., & Armour, C. (2020b). COVID-19 concerns. doi: 10.17605/OSF.IO/YQR2D [DOI] [Google Scholar]
- Hengst, S., Smid, G., & Laban, C. (2018). The effects of traumatic and multiple loss on psychopathology, disability, and quality of life in Iraqi asylum seekers in the Netherlands. The Journal of Nervous and Mental Disease, 206(1), 52–60. doi: 10.1097/NMD.0000000000000750 [DOI] [PubMed] [Google Scholar]
- Janoff-Bulman, R. (1989). Assumptive worlds and the stress of traumatic events: Applications of the schema construct. Social Cognition, 7(2), 113–136. doi: 10.1521/soco.1989.7.2.113 [DOI] [Google Scholar]
- Josephine, K., Josefine, L., Philipp, D., David, E., & Harald, B. (2017). Internet- and mobile-based depression interventions for people with diagnosed depression: A systematic review and meta-analysis. Journal of Affective Disorders, 223, 28–40. doi: 10.1016/j.jad.2017.07.021 [DOI] [PubMed] [Google Scholar]
- Kersting, A., Dölemeyer, R., Steinig, J., Walter, F., Kroker, K., Baust, K., & Wagner, B. (2013). Brief internet-based intervention reduces posttraumatic stress and prolonged grief in parents after the loss of a child during pregnancy: A randomized controlled trial. Psychotherapy and Psychosomatics, 82(6), 372–381. doi: 10.1159/000348713 [DOI] [PubMed] [Google Scholar]
- Kokou-Kpolou, C. K., Fernández-Alcántara, M., & Cénat, J. M. (2020). Prolonged grief related to covid-19 deaths: Do we have to fear a steep rise in traumatic and disenfranchised griefs? Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S94–S95. doi: 10.1037/tra0000798 [DOI] [PubMed] [Google Scholar]
- Komischke-Konnerup, K. B., Zachariae, R., Johannsen, M., Nielsen, L. D., & O’Connor, M. (2021). Co-occurrence of prolonged grief symptoms and symptoms of depression, anxiety, and posttraumatic stress in bereaved adults: A systematic review and meta-analysis. Journal of Affective Disorders Reports, 4, 100140. doi: 10.1016/j.jadr.2021.100140 [DOI] [Google Scholar]
- Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenferink, L. I. M., de Keijser, J., Eisma, M. C., Smid, G. E., & Boelen, P. A. (2020). Treatment gap in bereavement care: (Online) bereavement support needs and use after traumatic loss. Clinical Psychology & Psychotherapy. 10.1002/cpp.2544 [DOI] [PMC free article] [PubMed]
- Lenferink, L. I. M., de Keijser, J., Smid, G. E., Djelantik, A. A. A. M. J., & Boelen, P. A. (2017). Prolonged grief, depression, and posttraumatic stress in disaster-bereaved individuals: Latent class analysis. European Journal of Psychotraumatology, 8(1), 1. doi: 10.1080/20008198.2017.1298311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenferink, L. I. M., Eisma, M. C., Smid, G. E., de Keijser, J., & Boelen, P. A. (2022). Valid measurement of DSM-5 persistent complex bereavement disorder and DSM-5-TR and ICD-11 prolonged grief disorder: The Traumatic Grief Inventory-Self Report plus (TGI-SR+). Comprehensive Psychiatry, 112(152281) doi: 10.1016/j.comppsych.2021.152281 . [DOI] [PubMed] [Google Scholar]
- Lenferink, L. I. M., Franzen, F., Boelen, P. A., Knaevelsrud, C., & Heeke, C. (2022). A valid interview to assess prolonged grief disorder according to ICD-11 and new DSM-5 criteria: The traumatic grief inventory-clinician administered. [DOI] [PubMed]
- Lewis, C., Roberts, N. P., Simon, N., Bethell, A., & Bisson, J. I. (2019). Internet-delivered cognitive behavioural therapy for post-traumatic stress disorder: Systematic review and meta-analysis. Acta Psychiatrica Scandinavica, 140(6), 508–521. doi: 10.1111/acps.13079 [DOI] [PubMed] [Google Scholar]
- Lichtenthal, W. G., Corner, G. W., Sweeney, C. R., Wiener, L., Roberts, K. E., Baser, R. E., … Prigerson, H. (2015). Mental health services for parents who lost a child to cancer: If we build them, will they come? Journal of Clinical Oncology, 23(20), 2246–2254. doi: 10.1200/JCO.2014.59.0406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litz, B. T., Schorr, Y., Delaney, E., Au, T., Papa, A., Fox, A. B., … Prigerson, H. G. (2014). A randomized controlled trial of an internet-based therapist-assisted indicated preventive intervention for prolonged grief disorder. Behaviour Research and Therapy, 61, 23–34. doi: 10.1016/j.brat.2014.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobb, E., Kristjanson, L., Aoun, S., Monterosso, L., Halkett, G., & Davies, A. (2010). Predictors of complicated grief: A systematic review of empirical studies. Death Studies, 34(8), 673–698. doi: 10.1080/07481187.2010.496686 [DOI] [PubMed] [Google Scholar]
- Lundorff, M., Holmgren, H., Zachariae, R., Farver-Vestergaard, I., & O’Connor, M. (2017). Prevalence of prolonged grief disorder in adult bereavement: A systematic review and meta-analysis. Journal of Affective Disorders, 212, 138–149. doi: 10.1016/j.jad.2017.01.030 [DOI] [PubMed] [Google Scholar]
- Malgaroli, M., Maccallum, F., & Bonanno, G. A. (2018). Symptoms of persistent complex bereavement disorder, depression, and PTSD in a conjugally bereaved sample: A network analysis. Psychological Medicine, 48(14), 2439–2448. doi: 10.1017/S0033291718001769 [DOI] [PubMed] [Google Scholar]
- O’Connor, M., Lasgaard, M., Shevlin, M., & Guldin, M.-B. (2010). A confirmatory factor analysis of combined models of the Harvard Trauma Questionnaire and the inventory of complicated grief-revised: Are we measuring complicated grief or posttraumatic stress? Journal of Anxiety Disorders, 24(7), 672–679. doi: 10.1016/j.janxdis.2010.04.009 [DOI] [PubMed] [Google Scholar]
- Rosner, R., Bartl, H., Pfoh, G., Kotoučová, M., & Hagl, M. (2015). Efficacy of an integrative CBT for prolonged grief disorder: A long-term follow-up. Journal of Affective Disorders, 183, 106–112. doi: 10.1016/j.jad.2015.04.051 [DOI] [PubMed] [Google Scholar]
- Schut, H., & Stroebe, M. S. (2005). Interventions to enhance adaptation to bereavement. Journal of Palliative Medicine, 8(supplement 1), 147. doi: 10.1089/jpm.2005.8.s-140 [DOI] [PubMed] [Google Scholar]
- Shear, K., Frank, E., Houck, P. R., & Reynolds, C. F. (2005). Treatment of complicated grief: A randomized controlled trial. JAMA, 293(21), 2601–2608. doi: 10.1001/jama.293.21.2601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snijders, T. A. B., & Bosker, R. J. (2012). Multilevel analysis: An introduction to basic and advanced multilevel modeling (2nd ed.). Thousand Oaks, CA: SAGE Publications Ltd. [Google Scholar]
- Spek, V., Cuijpers, P., Nyklicek, I., Riper, H., Keyzer, J., & Pop, V. (2007). Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: A meta-analysis. Psychological Medicine, 37(3), 319–328. doi: 10.1017/S0033291706008944 [DOI] [PubMed] [Google Scholar]
- Van Denderen, M., de Keijser, J., Stewart, R., & Boelen, P. A. (2018). Treating complicated grief and posttraumatic stress in homicidally bereaved individuals: A randomized controlled trial. Clinical Psychology & Psychotherapy, 25(4), 497–508. doi: 10.1002/cpp.2183 [DOI] [PubMed] [Google Scholar]
- Wagner, B., Knaevelsrud, C., & Maercker, A. (2005). Internet-based treatment for complicated grief: Concepts and case study. Journal of Loss & Trauma, 10(5), 409–432. doi: 10.1080/15325020590956828 [DOI] [Google Scholar]
- Wagner, B., Knaevelsrud, C., & Maercker, A. (2006). Internet-based cognitive-behavioral therapy for complicated grief: A randomized controlled trial. Death Studies, 30(5), 429–453. doi: 10.1080/07481180600614385 [DOI] [PubMed] [Google Scholar]
- Wagner, B., & Maercker, A. (2007). A 1.5-year follow-up of an Internet-based intervention for complicated grief. Journal of Traumatic Stress, 20(4), 625–629. doi: 10.1002/jts.20230 [DOI] [PubMed] [Google Scholar]
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov Accessed on26 June 2020. Retrieved from https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp
- WHO . (2018). ICD-11. Prolonged Grief Disorder Criteria. Geneva: World Health Organization.Accessed on15 September 2021. Retrieved from https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/1183832314 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable for this article as data were not included.


