Abstract
Background Due to limited sensitivity of radiographs for scaphotrapeziotrapezoid (STT) arthritis and the high rate of concurrence between thumb carpometacarpal (CMC) and STT arthritis, intraoperative visualization of the STT joint is recommended during CMC arthroplasty.
Purpose We quantified the percentage of trapezoid facet of the scaphotrapezoid (ST) joint that could be visualized during this approach, and compared it to the degree of preoperative radiographic STT arthritis.
Methods We performed dorsal surgical approach to the thumb CMC joint after obtaining fluoroscopic anteroposterior, lateral, and oblique wrist radiographs of 11 cadaver wrists. After trapeziectomy, the ST joint was inspected and the visualized portion of the trapezoid articulation marked with an electrocautery. The trapezoid was removed, photographed, and the marked articular surface area and total surface area were independently measured by two authors using an image analysis software. The radiographs were analyzed for the presence of STT arthritis.
Results The mean visualized trapezoid surface area during standard approach for CMC arthroplasty was 60.3% (standard deviation: 24.6%). The visualized percentage ranged widely from 16.7 to 96.5%. There was no significant correlation between degree of radiographic arthritis and visualized percentage of the joint ( p = 0.77).
Conclusions: On average, 60% of the trapezoid joint surface was visualized during routine approach to the thumb CMC joint, but with very large variability. Direct visualization of the joint did not correlate with the degree of radiographic STT arthritis.
Clinical Relevance A combination of clinical examination, pre- and intraoperative radiographs, and intraoperative visualization should be utilized to assess for STT osteoarthritis and determine the need for surgical treatment.
Level of Evidence This is a Cadaveric Research Article.
Keywords: scaphotrapezoid, scaphotrapeziotrapezoid arthritis, carpometacarpal arthritis, STT, CMC, intraoperative visualization
Thumb carpometacarpal (CMC) arthritis, also known as basilar joint arthritis, is a prevalent and progressive pathology. 1 Population-based studies put the prevalence of radiographic CMC osteoarthritis at >10% for men and >15% for women aged 55 to 64 years, and >25 and >35% respectively for those more than 75 years old. 2 Basal joint arthritis is often accompanied by concurrent scaphotrapeziotrapezoid (STT) arthritis, estimated to be radiographically present in 8% of the population or approximately one-third of patients with CMC arthritis. 3 Patients are twice as likely to be symptomatic from their STT arthritis when both joints are involved. 3 However, while radiographic evaluation of the STT joint has a reported specificity of 86% for arthritis, its reported sensitivity is only 44%. 4
Following CMC arthroplasty for basal joint arthritis, up to 30% of patients have continued pain. Multiple etiologies have been proposed for this, including metacarpal (MC) proximal subsidence, concomitant thumb metacarpophalangeal joint laxity, and scaphotrapezoid (ST) joint arthritis. 5 6 7 8 Because of the limited sensitivity of radiographs for STT arthritis and the high rate of concurrence between thumb CMC and STT arthritis, intraoperative visualization of the STT joint is recommended during surgery for CMC arthroplasty. No previous study has evaluated the quality of ST joint visualization during CMC arthroplasty. We therefore assessed the percentage of the ST joint that could be visualized during this approach. We compared this to the preoperative radiographic degree of STT arthritis. We hypothesized that the visualized area of the trapezoid articular surface is limited during this approach, and that worsening radiographic arthritis would correlate with decreasing visualization.
Materials and Methods
The investigation was performed using 11 fresh-frozen cadaver upper extremities. Cadaver demographics included eight males (ages 55, 71, 71, 77, 77, 80, 90, and 90 years) and three females (ages 65, 91, and 91 years). Predissection posteroanterior (PA), lateral, and oblique wrist fluoroscopic images were obtained. Routine dorsal surgical approach to the thumb CMC was performed as follows. A longitudinal skin incision was made over the dorsoradial thumb trapeziometacarpal joint. Blunt dissection was used to access to the first extensor compartment tendons. The interval between the abductor pollicis longus and extensor pollicis brevis was used to access the dorsal CMC capsule, which was sharply divided and elevated to reveal the trapezium and base of the first MC. The trapezium was removed with an elevator, sharp dissection and a rongeur, revealing the ST joint. Particular attention was paid to make sure there was no injury to the trapezoid and its ligaments. Traction was applied by one operator, who placed one hand around the distal forearm to stabilize the wrist and used the other to pull manual distraction on the index finger to distract the ST joint. A second operator then introduced a Freer elevator to separate the joint. The visualized portion of the scaphoid facet of the trapezoid articulation was marked with fine-needle electrocautery. The trapezoid was then removed in its entirety. The cauterized portion was colored with a purple pen to improve image contrast. The trapezoid was then digitally photographed, and the marked surface area and total surface area of the scaphoid facet of the trapezoid were measured using ImageJ image analysis software as follows (ImageJ 1.x, National Institutes of Health, LOCI, University of Wisconsin) ( Fig. 1 ). 9 All images included a ruler, which was used to calibrate prior to analysis. Next, using the free-hand drawing function, the marked area was outlined and calculated in squared centimeters. The same technique was repeated to outline and measure the entire scaphoid facet. These values were used to calculate the percentage of the joint surface that had been marked.
Fig. 1.
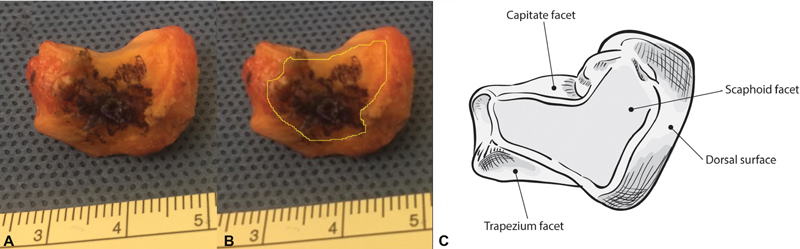
Cadaver trapezoid and anatomic illustration. ( A ) Photograph of cadaver trapezoid for surface area measurement. After surgical approach to the carpometacarpal was used to visualize the scaphotrapezoid joint and marked visible articular surface with electrocautery, scaphoids were excised. To improve contrast for image analysis, electrocauterized areas were colored over with a surgical marker ( purple ink ). Photographs were taken with a ruler in frame. ( B ) Example of surface area measurement of the scaphoid articulation of the trapezoid. The marked area was outlined in the same way to allow calculation of percentage visualized. Measurement was performed by two authors independently using ImageJ software with calibration based on ruler length. ( C ) Illustration of the trapezoid.
Two authors independently took two separate measurements each of each trapezoid in ImageJ, and these four values were averaged. The PA and lateral radiographs were analyzed for the presence of STT arthritis using the system described by White et al ( Fig. 2 ). In brief, this classification consists of stage 1, with narrowing of the joint space compared with the capitolunate joint, with or without periarticular sclerosis; stage 2, with narrowing of the joint space with one or more of periarticular sclerosis, cyst-like lucencies or osteophytes; and stage 3, with complete narrowing of the joint. 10 While their system used a modifier for involvement of the scaphotrapezial joint, scaphotrapezoidal joint, or both, for our purposes only the scaphotrapezial joint was evaluated. One-way ANOVA (analysis of variance) was used to determine if there was a significant association between radiographic degree of arthritis and percentage of the joint visualized during surgery.
Fig. 2.

Lateral and anteroposterior radiographs showing the scaphotrapezoid and scaphotrapezium joint in a cadaver wrist. Radiographs were evaluated using White et al's classification system. While their system used a modifier for involvement of the scaphotrapezial joint, scaphotrapezoidal joint, or both, for our purposes only the scaphotrapezial joint was evaluated.
Results
Surface Area Measurements
The mean surface area of the trapezoid portion of the ST joint visualized during the standard approach for CMC arthroplasty was 60.3% (standard deviation: 24.6%). There was a wide range of surface area visualized, from 16.7 to 96.5% ( Fig. 3 ). Surface area measurements between raters differed by an average of only 4.4%, and had a Pearson's correlation coefficient of R = 0.9278, representing a strong positive correlation.
Fig. 3.

Box and whiskers plot of distribution of measured percentage scaphotrapezoid joint surface. The bottom of the box represents the first quartile and the top of the box represents the third quartile. The horizontal line within the box represents the median. The vertical lines represent the minimum and maximum values.
Radiographic Classification
By White et al's classification of STT arthritis, 3 cadavers had stage 0 ST arthritis, 4 cadavers had stage 1 ST arthritis, and 4 cadavers had stage 2 ST arthritis. There was no correlation between degree of radiographic arthritis of the ST joint and the percentage of the joint that was visualized ( p = 0.77).
Discussion
Using a fresh-frozen cadaver model, we found that on average 60% of the trapezoid joint surface was visualized during routine dorsoradial approach to the thumb CMC joint. There was large variability in the proportion of visualized articular surface. The percentage visualized did not correlate with radiographic degree of ST arthritis.
STT arthritis is the second most common site of carpal degenerative arthritis, reported at 14% in a radiographic series by Watson and Ballet. 11 It occurs with increased incidence and severity in wrists with severe concurrent CMC arthritis, with rates of 40 to 44% for the scaphotrapezoidal joint. 6 12 The correlation of radiographic stage of arthritis with the gross pathologic grade of arthritis is poor, reported at 29% for the scaphotrapezoidal joint specifically. 6 Further, the gross pathologic incidence of STT arthritis may be far higher than is felt to be clinically symptomatic. Bhatia et al reported on 73 cadavers (mean age: 84 years), with 83% showing STT arthritis and increased incidence (72.6%) and severity (55% high grade) in the ST joint compared with the scaphotrapezial joint (65.7% incidence, 34% high grade). 13
While the radiographic and pathologic incidence of STT arthritis does vary in published cadaveric studies, possibly due to differences in the definitions of arthritis or in the demographic characteristics of the studied cadavers, it is clear that STT arthritis is present far more often than we, as clinicians, attribute symptoms to it. 10 14 When we do, the combination of the above factors (high frequency of ST arthritis in the general population, high concurrence with CMC arthritis, and poor correlation between radiographic and pathologic arthritis) makes diagnosing clinically relevant disease complex. Before performing STT arthrodesis or excision of the distal pole of the scaphoid, a diagnostic injection or further advanced imaging could be considered in patients with persistent mechanical postoperative pain after CMC arthroplasty when STT arthritis is the suspected cause. 1 13 15
This study has several weaknesses. As it was a cadaver study, we were unable to correlate clinical symptoms with radiographic degree of arthritis or percentage of the joint visualized. Further, cadavers lack dynamic stabilizing forces, and the tension of the soft tissues may differ from that in living patients, altering our ability to access the ST joint. We did note inherent variability in the laxity of the cadaver tissues, which may represent a spectrum of ligamentous laxity within the general population and could in part explain the range in percentage ST joint visualized. Our technique of ST joint distraction, manual distraction by one operator while another operator marked the visible joint, could also have contributed to variability. We could have used a force gauge to generate a consistent force in each specimen. However, the method we used is probably the most likely to be used intraoperatively in real-world clinical practice. As a further limitation, we only utilized the dorsoradial approach to the CMC. It is possible the ST joint might be better visualized via the Wagner approach to the CMC. Finally, our study was performed on only 11 cadavers, which is likely not representative of all clinical scenarios.
In conclusion, only a portion of the ST joint was typically visualized intraoperatively following trapeziectomy via the dorsal approach for CMC arthroplasty. The degree of radiographic ST arthritis did not correlate with the percentage of the joint visualized. However, because of ability to evaluate clinical arthritis intraoperatively, even if for a portion of the joint, we do feel routine visualization provides useful clinical information when used in concert with other modalities. We therefore recommend a combination of clinical examination, pre- and intraoperative radiographs, and intraoperative visualization to assess for ST arthritis and determine the need for surgical treatment.
Acknowledgments
The authors thank Olivia George for her skills in creating the trapezoid illustration in Fig. 1 .
Conflict of Interest None declared.
Note
The work was performed at The Rothman Orthopaedic Institute, 925 Chestnut St, 5th Floor, Philadelphia PA 19107.
Ethical Approval
This study was deemed exempt from review by our institution.
References
- 1.Haugen I K, Englund M, Aliabadi P. Prevalence, incidence and progression of hand osteoarthritis in the general population: the Framingham Osteoarthritis Study. Ann Rheum Dis. 2011;70(09):1581–1586. doi: 10.1136/ard.2011.150078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haara M M, Heliövaara M, Kröger H. Osteoarthritis in the carpometacarpal joint of the thumb. Prevalence and associations with disability and mortality. J Bone Joint Surg Am. 2004;86(07):1452–1457. doi: 10.2106/00004623-200407000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Armstrong A L, Hunter J B, Davis T R. The prevalence of degenerative arthritis of the base of the thumb in post-menopausal women. J Hand Surg [Br] 1994;19(03):340–341. doi: 10.1016/0266-7681(94)90085-x. [DOI] [PubMed] [Google Scholar]
- 4.Tomaino M M, Vogt M, Weiser R. Scaphotrapezoid arthritis: prevalence in thumbs undergoing trapezium excision arthroplasty and efficacy of proximal trapezoid excision. J Hand Surg Am. 1999;24(06):1220–1224. doi: 10.1053/jhsu.1999.1220. [DOI] [PubMed] [Google Scholar]
- 5.Bhatia A, Pisoh T, Touam C, Oberlin C. Incidence and distribution of scaphotrapezotrapezoidal arthritis in 73 fresh cadaveric wrists. Ann Chir Main Memb Super. 1996;15(04):220–225. doi: 10.1016/s0753-9053(96)80030-5. [DOI] [PubMed] [Google Scholar]
- 6.Brown G D, III, Roh M S, Strauch R J, Rosenwasser M P, Ateshian G A, Mow V C. Radiography and visual pathology of the osteoarthritic scaphotrapezio-trapezoidal joint, and its relationship to trapeziometacarpal osteoarthritis. J Hand Surg Am. 2003;28(05):739–743. doi: 10.1016/s0363-5023(03)00258-2. [DOI] [PubMed] [Google Scholar]
- 7.Papatheodorou L K, Winston J D, Bielicka D L, Rogozinski B J, Lourie G M, Sotereanos D G. Revision of the failed thumb carpometacarpal arthroplasty. J Hand Surg Am. 2017;42(12):10320–1.032E10. doi: 10.1016/j.jhsa.2017.07.015. [DOI] [PubMed] [Google Scholar]
- 8.Wolf J M.Treatment of scaphotrapezio-trapezoid arthritis Hand Clin 20082403301–306., vii [DOI] [PubMed] [Google Scholar]
- 9.Schneider C A, Rasband W S, Eliceiri K W. NIH Image to ImageJ: 25 years of image analysis. Nat Methods. 2012;9(07):671–675. doi: 10.1038/nmeth.2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.White L, Clavijo J, Gilula L A, Wollstein R. Classification system for isolated arthritis of the scaphotrapeziotrapezoidal joint. Scand J Plast Reconstr Surg Hand Surg. 2010;44(02):112–117. doi: 10.3109/02844311003675388. [DOI] [PubMed] [Google Scholar]
- 11.Watson H K, Ballet F L. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984;9(03):358–365. doi: 10.1016/s0363-5023(84)80223-3. [DOI] [PubMed] [Google Scholar]
- 12.Bade H, Koebke J. Arthrosis in the peritrapezial joints of the hand. Surg Radiol Anat. 1996;18(03):209–214. doi: 10.1007/BF02346129. [DOI] [PubMed] [Google Scholar]
- 13.Crosby E B, Linscheid R L, Dobyns J H. Scaphotrapezial trapezoidal arthrosis. J Hand Surg Am. 1978;3(03):223–234. doi: 10.1016/s0363-5023(78)80086-0. [DOI] [PubMed] [Google Scholar]
- 14.Moritomo H, Viegas S F, Nakamura K, Dasilva M F, Patterson R M. The scaphotrapezio-trapezoidal joint. Part 1: an anatomic and radiographic study. J Hand Surg Am. 2000;25(05):899–910. doi: 10.1053/jhsu.2000.4582. [DOI] [PubMed] [Google Scholar]
- 15.Martini K, Becker A S, Guggenberger R, Andreisek G, Frauenfelder T. Value of tomosynthesis for lesion evaluation of small joints in osteoarthritic hands using the OARSI score. Osteoarthritis Cartilage. 2016;24(07):1167–1171. doi: 10.1016/j.joca.2016.01.982. [DOI] [PubMed] [Google Scholar]


