Abstract
Objectives
This study aimed to compare and evaluate the porosity and pore size distribution of high-viscosity glass ionomer cements (HVGICs) and conventional glass ionomer cements (GICs) using micro-computed tomography (micro-CT).
Materials and Methods
Forty cylindrical specimens (n = 10) were produced in standardized molds using HVGICs and conventional GICs (Ketac Molar Easymix, Vitro Molar, MaxxionR, and Riva Self-Cure). The specimens were prepared according to ISO 9917-1 standards, scanned in a high-energy micro-CT device, and reconstructed using specific parameters. After reconstruction, segmentation procedures, and image analysis, total porosity and pore size distribution were obtained for specimens in each group. After checking the normality of the data distribution, the Kruskal-Wallis test followed by the Student-Newman-Keuls test was used to detect differences in porosity among the experimental groups with a 5% significance level.
Results
Ketac Molar Easymix showed statistically significantly lower total porosity (0.15%) than MaxxionR (0.62%), Riva (0.42%), and Vitro Molar (0.57%). The pore size in all experimental cements was within the small-size range (< 0.01 mm3), but Vitro Molar showed statistically significantly more pores/defects with a larger size (> 0.01 mm3).
Conclusions
Major differences in porosity and pore size were identified among the evaluated GICs. Among these, the Ketac Molar Easymix HVGIC showed the lowest porosity and void size.
Keywords: Glass ionomer cements, Porosity, X-ray microtomography
INTRODUCTION
In recent years, glass-ionomer cements (GICs) have gained a prominent role in restorative dentistry due to their broad clinical indications and relatively simple clinical technique. They can be successfully used as restorative materials and fissure sealants, as well as bonding agents for orthodontic appliances, luting agents for indirect restorations, cavity liners, and bases [1]. These materials have become appealing in operative dentistry due to properties such as easy handling, chemical bonding to enamel and dentin, a coefficient of thermal expansion similar to that of tooth structure, and potential bioactive properties, such as the release of biologically active ions, including fluoride [2,3]. Among polyalkenoate-based cements, many brands of GICs are presently available on the market with indications as temporary or relatively long-term restorative materials [4,5]. The limitations of these cements are related to their relative lack of strength and low resistance to abrasion and wear [6].
A systematic review found that GICs had better survival rates than composites when used to restore cervical carious lesions both in permanent and primary teeth; however, they were not indicated for load-bearing areas in both dentitions [7]. These relatively disappointing results were associated with the physical and mechanical properties of conventional GICs, which could reduce their clinical use as long-term restoratives compared with composite resins for load-bearing areas [8]. However, the mechanical properties of GICs have improved subsequently and the relatively new category of high-viscosity GICs (HVGICs) are currently showing better success and/or survival rates, especially for single-surface atraumatic restorative treatment (ART) restorations [9,10,11].
Indeed, the physical, chemical, and mechanical properties of GICs may be influenced by several factors; in particular, the presence of voids after mixing procedures and setting may reduce the mechanical strength of the material [12]. HVGICs were proposed as materials with an improved powder-to-liquid ratio and reduced particle size, but whether this change in composition affects material porosity is unknown.
There are common misconceptions related to the definition of material porosity. Pores can be defined as parts of the material volume that are not occupied by the solid material [13], and must be differentiated from material defects, including bubbles or air-voids [14]. It has been recently demonstrated that porosity in GICs could be related to a slow maturation reaction [15]. In fact, a volumetric pore analysis confirmed that the pore distribution in GICs is complex and highly variable, but decreases with time immediately after setting [16].
Various techniques have been used to evaluate porosity in GICs, such as transmitted light with a stereomicroscope [14], scanning electron microscope (SEM) [16,17,18] and micro-computed tomography (micro-CT) [19,20]. Micro-CT has the clear advantage of allowing non-destructive 3-dimensional (3D) visualization and quantification of pores in the internal structure, both qualitatively and quantitatively [21]. However, to the best of our knowledge, no study has yet compared the porosity of conventional and HVGICs used in dental clinical practice. This raises the question of whether the improvements in the powder-to-liquid ratio and reduction in particle size have resulted in less porous cements.
Therefore, the purpose of the present study was to compare the degree of porosity and pore size distribution of 2 commercially available conventional GICs with 2 HVGICs using a non-destructive micro-CT technique. The null hypotheses were that all tested GICs would have similar degree of porosity and there would be no difference in pore size distribution among the tested materials.
MATERIALS AND METHODS
Two commercially available conventional restorative GICs (MaxxionR, FGM, Joinville, Brazil and Riva Self-Cure, SDI, Victoria, Australia) and 2 HVGICs (Vitro Molar, Nova DFL, Rio de Janeiro, Brazil and Ketac Molar Easymix, 3M ESPE, Seefeld, Germany), were used in the present study. The details of GICs used in the present study are depicted in Table 1. The cements were of the self-cured type and were hand-mixed according to each manufacturers' instructions. The test specimens were prepared according to ISO 9917-1 standards for water-based cements, as described below.
Table 1. Details of glass ionomer cements used in the present study.
| Type of GIC | Material | Manufacturer | Batch number | Composition | Powder/liquid ratio by weight (g/g) | Mean particle size (µm) |
|---|---|---|---|---|---|---|
| Conventional | Maxxion R | FGM (Joinville, SC, Brazil) | 150915 | Liquid: tartar acid, water | 1.38:1 | 15.78 |
| Powder: fluoroaluminium silicate, polycarboxylic acid, calcium fluoride | ||||||
| Riva Self-Cure | SDI (Melbourne, Australia) | 621141V | Liquid: 25% polyacrylic acid, 10% tartaric glass | 2.65:1 | 24 | |
| Powder: 90% fluoroaluminium silicate, 10% polyacrylic acid | ||||||
| High-viscosity | Vitro Molar | DFL (Rio de Janeiro, Brazil) | 15111766 | Liquid: polyacrylic and tartaric acid, distilled water | 3.00:1 | 5.14 |
| Powder: barium and aluminum silicate, polyacrylic acid, iron oxide | ||||||
| Ketac Molar Easy Mix | 3M ESPE (Seefeld, Germany) | 56633 | Liquid: 25%–35% polycarbonic acid, 5%–10% tartaric acid and 55%–65% water | 4.50:1 | 2.18 | |
| Powder: 85%–95% fluorosilicate glass, strontium and lanthanum, 5%–15% polyacrylic acid |
GIC, glass ionomer cement.
Sample size calculation
The sample size calculation was based on standard deviations and mean differences obtained from the only 2 available previous studies employing a micro-CT methodology to study the porosity of non-resin GICs [19,20]. G*Power [22] was used for sample size calculation for 4 groups, using an estimated standard deviation of 0.30 and a mean minimum difference of 0.5 to be detected among the groups, resulting in 10 samples per group (40 specimens).
Preparation of specimens
Standardized cylindrical specimens were fabricated in metallic molds with a 4.0 ± 0.1 mm diameter and 6.0 ± 0.1 mm height (100.5 mm3). All specimens were prepared by a single operator using the proprietary dispensers provided by each manufacturer and following the specific instructions regarding proportions, preparation, mixing technique, and handling. Cement manipulation was carried out at room temperature (25 ± 1°C) and while relative humidity could not be completely controlled, it was kept around 50 ± 5%.
The molds were lubricated with petroleum jelly, and the GICs were mixed with a plastic spatula on paper blocks until a glossy and homogeneous cement was obtained. The material was immediately placed in the molds with the aid of a syringe (Centrix Accudose low-viscosity tube, Centrix Dental, Shelton, CT, USA) and excess cement was removed. Then, 1 operator applied a slight digital pressure on the mold for final material adaptation, as would be performed during clinical procedures for ART. Ten minutes later, after initial sample hardening, the specimens were removed from the molds and a thin layer of petroleum jelly was painted around the specimens to prevent syneresis. The samples were then stored in distilled water for 24 hours at 37°C [23].
Micro-computed tomography scanning and reconstruction procedures
The samples were scanned in a high energy micro-CT device (Skyscan 1173, Bruker, Kontich, Belgium) with the following acquisition parameters: 70 kV, 114 µA, 2,240 × 2,240 pixel matrix, 12.11 µm pixel size, 1 mm thick Al filter, 800 ms exposure time, 0.5° rotation step over 360°, frame averaging of 5, and a random-movement setting of 30. Scanning time was approximately 70 minutes for each specimen. Projections were saved as 16-bit grayscale TIFF format images. After image acquisition, reconstruction was accomplished using proprietary software (NRecon, v.1.6.9, Bruker) with standardized parameters for artifact minimization, including a ring artifact correction of 1, a beam hardening correction of 25%, and input of contrast limits (0–0.15). Images were reconstructed in 8-bit *.BMP format.
Porosity analysis
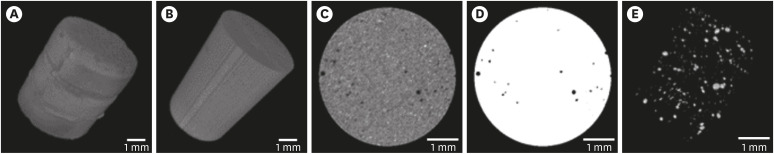
The cross-sectional volumes of each specimen were digitally cropped to fit a 150 pixel (1.82 mm) radius and 5 mm height cylinder (77.8 mm3), in order to exclude outer and possibly non-homogeneous surface areas of the cements and standardize readings (Figure 1A and 1B). A 3D median filter with a 1-pixel radius was applied to each cropped volume to reduce noise, and the histograms of all images were then normalized according to mean gray values for each cement group (Figure 1C). The threshold for pores was fixed at a gray value of 40 after an iterative user-based analysis of representative specimens in each cement group (Figure 1D). Total porosity and the distribution of pore sizes were obtained for each experimental cement group samples after pore segmentation (Figure 1E). Pores were considered small if their individual volume was ≤ 0.01 mm3 and large if it was > 0.01 mm3. All image processing and analysis steps were undertaken within the Fiji/ImageJ interface [24].
Figure 1. Glass ionomer cement specimens and porosity. (A) Original specimen. (B) Specimen after definition of the volume of interest. (C) Cross-sectional slice of the specimen after normalization and filtering. (D) Application of the iterative threshold. (E) Three-dimensional renderization of pore segmentation.
Statistical analysis
The normality of data distribution was checked with Shapiro-Wilk test. As the null hypothesis of normality was rejected, the Kruskal-Wallis test followed by the Student-Newman-Keuls test was used to detect differences in porosity among the experimental groups using the BioEstat 5.3 statistical package (Instituto Mamirauá, Tefé, AM, Brazil).
RESULTS
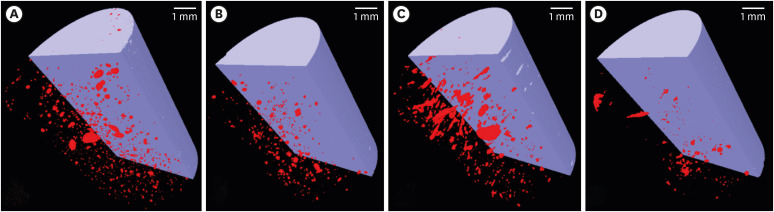
Table 2 shows the total porosity values for the tested cements. Ketac Molar Easymix showed statistically significantly lower porosity (0.15%) than MaxxionR (0.62%), Riva Self-Cure (0.42%), and Vitro Molar (0.57%). As presented in Table 3, most pore sizes in all tested cements were within the small size range (≤ 0.01 mm3), but Vitro Molar showed a statistically significantly higher percentage of larger pores (> 0.01 mm3). Figure 2 shows 3D volume renderings obtained after image acquisition and reconstruction of 1 representative specimen from each group.
Table 2. Mean percentage of the total porosity for each experimental glass ionomer cement.
| Glass ionomer cement | Total porosity (%) |
|---|---|
| MaxxionR | 0.62 ± 0.63a |
| Riva Self-Cure | 0.42 ± 0.40a |
| Vitro Molar | 0.57 ± 0.41a |
| Ketac Molar EasyMix | 0.15 ± 0.14b |
Different lowercase superscript letters indicate statistically significant differences (Kruskal-Wallis followed by Student-Newman-Keuls test, p < 0.05).
Table 3. Percentage (%) distribution of pore size among the experimental groups.
| Pore size | Maxxion R | Riva Self-cure | Vitro Molar | Ketac Molar Easy Mix |
|---|---|---|---|---|
| Small pores (< 0.01 mm3) | 99.81 ± 0.09a | 99.95 ± 0.07a | 99.50 ± 0.22b | 99.89 ± 0.23a |
| Large pores (> 0.01 mm3) | 0.08 ± 0.09a | 0.05 ± 0.07a | 0.50 ± 0.22b | 0.11 ± 0.23a |
Different lowercase superscript letters in each row indicate statistically significant differences (Kruskal-Wallis followed by Student-Newman-Keuls test, p < 0.05).
Figure 2. Three-dimensional volume rendering obtained after image acquisition and reconstruction of a representative specimen of each studied material. (A) MaxxionR; (B) Riva Self-Cure; (C) Vitro Molar; (D) Ketac Molar Easymix.
DISCUSSION
GICs are composed of a polyalkenoic acid aqueous solution that reacts with a basic powdered glass component [1]. After setting, however, these cements may present voids or defects, which can reduce their clinical performance [12]. In view of the improved HVGICs, the present study analyzed the porosity of commercially available hand-mixed conventional GIC and HVGICs used in restorative dentistry using a non-destructive 3D technique. The materials used in the present study have been previously evaluated in randomized clinical trials, showing encouraging results, with cumulative survival rates ranging from 45% to 68% after 18 months in multiple surface restorations in primary molars [10,25,26], and for this reason, they were chosen for the present evaluation.
Pore volume determination within a material is highly dependent on the type and resolution of the experimental technique used. For this reason, the results should be compared with caution. Higher porosity values have been recently found for self-cured GICs (2.7-3.5%) after 24 hours of setting using gas adsorption measurements [27], which is an understandable result if the resolution used by the authors (2 nm) is compared to the resolution used in the present study (12 µm). The same probably happens with the higher total porosity values for HVGICs found by a bidimensional SEM analysis, ranging from around 2%–3% for Ketac Molar Easymix [17,18] to 8% for Fuji IX [16]. Specifically, regarding 3D porosity analysis in micro-CT, the threshold method used to define voids also plays an important role in the total measurements. Previous micro-CT studies did not disclose how the threshold for pores was established [19,20]. In the present study, an iterative method based on the mean histogram distribution for all the specimens was chosen for all specimens.
In the present study, only hand-mixed cements were used; still, the total porosity was low for all cements (< 1%). This may be due to general improvements in the formulation of hand-mixed GICs, including addition of polyacrylic acid into the powder and its finer grain size distribution [6]. However, the null hypotheses of the present study were rejected, as the degree of porosity and pore size distribution of the tested GICs were not similar, with Ketac Molar Easymix presenting the lowest total porosity and Vitro Molar showing a higher proportion of large pores. We attribute the favorable results regarding total porosity obtained in the present study by Ketac Molar Easymix to the high wettability of the powder [28]. Vitro Molar, despite being classified as a HVGIC with a purported high powder-to-liquid ratio and small particle size distribution, showed porosity values comparable to those of conventional GICs and a higher proportion of large voids than the other materials. As “large” pores are frequently regarded as “defects” created inside the material structure, these poor porosity results for this HVGIC could be attributed to problems or incompatibility between the powder particles and the liquid mixture.
The threshold for voids in GICs has been set as > 0.01 mm3, as described earlier [13], but the measurements reported by these authors were bidimensional, measured in terms of the surface area. Others have reported void measurements in diameters [16,20,27], while some did not report pore size distribution [17,19]. In the present study, the threshold of 0.01 mm3 was chosen to allow a distinction between pores and defects (large pores).
A mean porosity value of 0.1% in hand-mixed Ketac Molar samples was previously found by micro-CT [20], corroborating the results of the present study (0.15%). In that study, however, the authors found much fewer voids than in the present study (on average 32 voids per sample compared to on average 700 voids found in the present study). This may be due to the lower resolution used (26 µm compared to 12 µm used in the present study), allowing the detection of larger voids (> 0.01 mm3). The present study detected pores within a small size range, corroborating the results obtained by others [16].
It has been also previously demonstrated that the hand-mixed manipulation method was favored for conventional GICs and for HVGICs, since it resulted in only minor effects on compressive strength and porosity [20]. In fact, porosity seems to be lower in hand-mixed GICs than in those manipulated using automated machines [14]. With the goal of minimizing the incorporation of larger pores or bubbles and the “operator effect,” a syringe was used in the present study to insert the cement into the molds. Previous studies have failed to identify differences in mechanical properties [29] caused by variation in the method of insertion, while other studies have shown that the syringe method favors particle agglutination, reduces air bubble incorporation, and improves mechanical properties [12,17].
Although many studies have evaluated the porosity of different types, mixing methods, and brands of GICs [14,16,17,27,28], very few have used the nondestructive micro-CT technique [18,19]. Micro-CT allows evaluation of the bulk of the entire specimen, the visualization of its internal structure, and volumetric analysis [30]. In the present study, a statistically significant difference in total porosity was observed between the 2 HVGICs, with Vitro Molar showing lower porosity results than the conventional GICs. This underperformance is corroborated by the results of previous mechanical tests, which have shown differences in flexural/compressive strength and hardness among the GICs indicated for ART treatment, with Ketac Molar Easymix showing superior results to Vitro Molar, Riva Self-Cure, and Maxxion R [31].
Finally, it is important to acknowledge that some degree of porosity may be expected in cement-like materials. Specifically for GICs, porosity is a mechanism in which fluoride release is involved [32]. However, the pores involved in fluoride diffusion through GICs are on the submicron scale [27].
As a limitation of the present study, one may argue that evaluations of the porosity of a material may differ depending on the technique used [33], but micro-CT has the advantage of a nondestructive nature, making it possible for future studies to correlate the porosity with mechanical properties within the same specimens to predict clinical performance. In this regard, the present study can be used as a methodological protocol to obtain, in a systematic and reproducible way, porosity data on dental cements from micro-CT data.
CONCLUSIONS
Major differences in porosity and pore size are present among the evaluated GICs. Among these, Ketac Molar Easymix showed the lowest porosity and size of voids. Conventional GICs and HVGICs may not be differentiated on the basis of porosity.
Footnotes
Funding: This study was supported by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) Finance code 001, Conselho Nacional de Pesquisa Científica (CNPq) and Fundação Carlos Chagas de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ) grant number E-26/203.185/2016.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- Conceptualization: Neves AB, Neves AA.
- Data curation: Neves AB, Neves AA.
- Formal analysis: Silva ASS, Lopes RT.
- Funding acquisition: Neves AB, Neves AA.
- Investigation: Neves AB, Lopes LIG, Bergstrom TG.
- Methodology: Neves AA, Lopes RT.
- Project administration: Neves AA.
- Resources: Neves AB, Neves AA.
- Software: Neves AB, Silva ASS, Lopes RT, Neves AA.
- Supervision: Neves AA.
- Validation: Neves AA.
- Visualization: Neves AB, Lopes LIG, Bergstrom TG, Silva ASS, Lopes RT, Neves AA.
- Writing - original draft: Neves AB, Neves AA.
- Writing - review & editing: Neves AB, Lopes LIG, Bergstrom TG, Silva ASS, Lopes RT, Neves AA.
References
- 1.Sidhu SK, Nicholson JW. A review of glass-ionomer cements for clinical dentistry. J Funct Biomater. 2016;7:16. doi: 10.3390/jfb7030016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coutinho E, Cardoso MV, De Munck J, Neves AA, Van Landuyt KL, Poitevin A, Peumans M, Lambrechts P, Van Meerbeek B. Bonding effectiveness and interfacial characterization of a nano-filled resin-modified glass-ionomer. Dent Mater. 2009;25:1347–1357. doi: 10.1016/j.dental.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 3.Berg JH, Croll TP. Glass ionomer restorative cement systems: an update. Pediatr Dent. 2015;37:116–124. [PubMed] [Google Scholar]
- 4.Hesse D, Bonifácio CC, Bönecker M, Guglielmi Cde A, da Franca C, van Amerongen WE, Colares V, Raggio DP. Survival rate of Atraumatic Restorative Treatment (ART) restorations using a glass ionomer bilayer technique with a nanofilled coating: a Bi-center randomized clinical trial. Pediatr Dent. 2016;38:18–24. [PubMed] [Google Scholar]
- 5.Burke FJT, Lucarotti PSK. The ultimate guide to restoration longevity in England and Wales. Part 3: glass ionomer restorations - time to next intervention and to extraction of the restored tooth. Br Dent J. 2018;224:865–874. doi: 10.1038/sj.bdj.2018.436. [DOI] [PubMed] [Google Scholar]
- 6.Frankenberger R, Sindel J, Krämer N. Viscous glass-ionomer cements: a new alternative to amalgam in the primary dentition? Quintessence Int. 1997;28:667–676. [PubMed] [Google Scholar]
- 7.Schwendicke F, Göstemeyer G, Blunck U, Paris S, Hsu LY, Tu YK. Directly placed restorative materials: Review and network meta-analysis. J Dent Res. 2016;95:613–622. doi: 10.1177/0022034516631285. [DOI] [PubMed] [Google Scholar]
- 8.van Dijken JW, Pallesen U. Fracture frequency and longevity of fractured resin composite, polyacid-modified resin composite, and resin-modified glass ionomer cement class IV restorations: an up to 14 years of follow-up. Clin Oral Investig. 2010;14:217–222. doi: 10.1007/s00784-009-0287-z. [DOI] [PubMed] [Google Scholar]
- 9.Leal S, Bonifacio C, Raggio D, Frencken J. Atraumatic restorative treatment: restorative component. Monogr Oral Sci. 2018;27:92–102. doi: 10.1159/000487836. [DOI] [PubMed] [Google Scholar]
- 10.Hilgert LA, de Amorim RG, Leal SC, Mulder J, Creugers NH, Frencken JE. Is high-viscosity glass-ionomer-cement a successor to amalgam for treating primary molars? Dent Mater. 2014;30:1172–1178. doi: 10.1016/j.dental.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 11.de Amorim RG, Frencken JE, Raggio DP, Chen X, Hu X, Leal SC. Survival percentages of atraumatic restorative treatment (ART) restorations and sealants in posterior teeth: an updated systematic review and meta-analysis. Clin Oral Investig. 2018;22:2703–2725. doi: 10.1007/s00784-018-2625-5. [DOI] [PubMed] [Google Scholar]
- 12.Nomoto R, McCabe JF. Effect of mixing methods on the compressive strength of glass ionomer cements. J Dent. 2001;29:205–210. doi: 10.1016/s0300-5712(01)00010-0. [DOI] [PubMed] [Google Scholar]
- 13.Nimmo JR. Porosity and pore size distribution. Reference module in earth systems and environmental sciences. Amsterdam: Elsevier; 2013. [Google Scholar]
- 14.Mitchell CA, Douglas WH. Comparison of the porosity of hand-mixed and capsulated glass-ionomer luting cements. Biomaterials. 1997;18:1127–1131. doi: 10.1016/s0142-9612(97)00038-0. [DOI] [PubMed] [Google Scholar]
- 15.Nicholson JW. Maturation processes in glass-ionomer dental cements. Acta Biomater Odontol Scand. 2018;4:63–71. doi: 10.1080/23337931.2018.1497492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Geirsson J, Thompson JY, Bayne SC. Porosity evaluation and pore size distribution of a novel directly placed ceramic restorative material. Dent Mater. 2004;20:987–995. doi: 10.1016/j.dental.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 17.Coldebella CR, Santos-Pinto L, Zuanon AC. Effect of ultrasonic excitation on the porosity of glass ionomer cement: a scanning electron microscope evaluation. Microsc Res Tech. 2011;74:54–57. doi: 10.1002/jemt.20873. [DOI] [PubMed] [Google Scholar]
- 18.Covey DA, Ewoldsen NO. Porosity in manually and machine mixed resin-modified glass ionomer cements. Oper Dent. 2001;26:617–623. [PubMed] [Google Scholar]
- 19.Malkoç MA, Sevimay M, Tatar İ, Çelik HH. Micro-CT detection and characterization of porosity in luting cements. J Prosthodont. 2015;24:553–561. doi: 10.1111/jopr.12251. [DOI] [PubMed] [Google Scholar]
- 20.Nomoto R, Komoriyama M, McCabe JF, Hirano S. Effect of mixing method on the porosity of encapsulated glass ionomer cement. Dent Mater. 2004;20:972–978. doi: 10.1016/j.dental.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 21.De Souza ET, Nunes Tameirão MD, Roter JM, De Assis JT, De Almeida Neves A, De-Deus GA. Tridimensional quantitative porosity characterization of three set calcium silicate-based repair cements for endodontic use. Microsc Res Tech. 2013;76:1093–1098. doi: 10.1002/jemt.22270. [DOI] [PubMed] [Google Scholar]
- 22.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 23.Calvo AF, Kicuti A, Tedesco TK, Braga MM, Raggio DP. Evaluation of the relationship between the cost and properties of glass ionomer cements indicated for atraumatic restorative treatment. Braz Oral Res. 2016;30:S1806-83242016000100201. doi: 10.1590/1807-3107BOR-2016.vol30.0008. [DOI] [PubMed] [Google Scholar]
- 24.Schmid B, Schindelin J, Cardona A, Longair M, Heisenberg M. A high-level 3D visualization API for Java and ImageJ. BMC Bioinformatics. 2010;11:274. doi: 10.1186/1471-2105-11-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anna Luisa de Brito P, Isabel Cristina O, Clarissa Calil B, Ana Flávia Bissoto C, José Carlos Pettorossi I, Daniela Prócida R. One year survival rate of Ketac Molar versus Vitro Molar for occlusoproximal ART restorations: a RCT. Braz Oral Res. 2017;31:e88. doi: 10.1590/1807-3107BOR-2017.vol31.0088. [DOI] [PubMed] [Google Scholar]
- 26.Bonifácio CC, Hesse D, Raggio DP, Bönecker M, van Loveren C, van Amerongen WE. The effect of GIC-brand on the survival rate of proximal-ART restorations. Int J Paediatr Dent. 2013;23:251–258. doi: 10.1111/j.1365-263X.2012.01259.x. [DOI] [PubMed] [Google Scholar]
- 27.Benetti AR, Jacobsen J, Lehnhoff B, Momsen NC, Okhrimenko DV, Telling MT, Kardjilov N, Strobl M, Seydel T, Manke I, Bordallo HN. How mobile are protons in the structure of dental glass ionomer cements? Sci Rep. 2015;5:8972. doi: 10.1038/srep08972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peez R, Frank S. The physical-mechanical performance of the new Ketac Molar Easymix compared to commercially available glass ionomer restoratives. J Dent. 2006;34:582–587. doi: 10.1016/j.jdent.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 29.Raggio DP, Bonifácio CC, Bönecker M, Imparato JC, Gee AJ, Amerongen WE. Effect of insertion method on Knoop hardness of high viscous glass ionomer cements. Braz Dent J. 2010;21:439–445. doi: 10.1590/s0103-64402010000500011. [DOI] [PubMed] [Google Scholar]
- 30.Neves AB, Bergstrom TG, Fonseca-Gonçalves A, Dos Santos TMP, Lopes RT, de Almeida Neves A. Mineral density changes in bovine carious dentin after treatment with bioactive dental cements: a comparative micro-CT study. Clin Oral Investig. 2019;23:1865–1870. doi: 10.1007/s00784-018-2644-2. [DOI] [PubMed] [Google Scholar]
- 31.Bonifácio CC, Kleverlaan CJ, Raggio DP, Werner A, de Carvalho RC, van Amerongen WE. Physical-mechanical properties of glass ionomer cements indicated for atraumatic restorative treatment. Aust Dent J. 2009;54:233–237. doi: 10.1111/j.1834-7819.2009.01125.x. [DOI] [PubMed] [Google Scholar]
- 32.Nicholson J, Czarnecka B. In: Materials for the direct restoration of teeth. Nicholson J, Czarnecka B, editors. Amsterdam: Elsevier; 2016. Conventional glass-ionomer cements; pp. 107–136. [Google Scholar]
- 33.Santa G, Bentz D, Weiss J. Capillary porosity depercolation in cement-based materials: Measurement techniques and factors which influence their interpretation. Cement Concr Res. 2011;41:854–864. [Google Scholar]