Abstract
Both COVID-19 and unrest are posing a significant threat to population mental health across the globe. This study examined trends of probable depression and anxiety during a time of civil unrest and concurrent COVID-19 in Hong Kong. Four random digit dialing telephone surveys were conducted in July 2019 (n = 1112), February–March 2020 (n = 2003), April–May 2020 (n = 2008), and July–August 2020 (n = 2034). The prevalence of probable depression increased from 25.7% (95% CI: 23.2–28.3) in July 2019 to 28.2% (95% CI: 26.2–30.1) in February–March 2020, and then decreased to 15.3% (95% CI: 14.0–17.0) in April–May 2020 and 13.7% (95% CI: 12.2–15.2) in July–August 2020. The prevalence of probable anxiety was 19.2% (95% CI: 17.5–20.9) in February–March 2020 and then stabilized in April–May 2020 and July–August 2020 (14.1%, 95% CI: 12.0–15.8). Probable depression and anxiety were more prevalent among persons with high relative to low daily routine disruptions. Combined high unrest-COVID-19 stress was associated with probable depression and anxiety across all persons; high unrest stress alone was associated with probable mental disorders at high daily routine disruptions. Civil unrest and COVID-19 are jointly associated with depression and anxiety among Hong Kong citizens. While population mental health improved, daily routine disruptions is a risk factor of mental disorders at every time-point.
Keywords: Depression, Anxiety, Daily routines, Civil unrest, COVID-19
1. Introduction
With an estimated 1–2 million of the 7.5 million Hong Kong people reportedly participating in some forms of civil protest, the anti-extradition bill protests of 2019–2020 have become the largest scale social/political movement in Greater China since the pro-democracy Umbrella Movement/Occupy Central in Hong Kong in 2014 and the Tiananmen Square protests in Beijing, China, in 1989. In October 2019, four months after the introduction of an extradition bill that would have allowed Hong Kong people to be transferred to China to stand trial, the Hong Kong SAR Government definitively withdrew the bill. However, by that time, several large-scale relatively peaceful demonstrations and protests had transformed into regular pro-democracy protests and violent clashes between protestors and police or other citizens on the streets, in shopping malls, and in university campuses across districts in Hong Kong (Choi, 2020). Compounding the particular set of challenges brought about by the civil unrest, coronavirus disease 2019 (COVID-19) emerged in Hong Kong in late January 2020, along with increased incidence and mortality over time (Supplementary Material 1). COVID-19 has evolved into a pandemic affecting more than 200 countries or territories worldwide and instigated widespread infection control measures of lockdown, quarantine, and social distancing. The prevalences of probable depression and anxiety were 1.7%–2.1% (Nan et al., 2013; Yu et al., 2012) and 5.3%–6.3% (Yang et al., 2019; Yu et al., 2018), respectively, among Hong Kong Chinese during non-unrest and pre-COVID-19 period. It has been well documented that COVID-19 is associated with a burden of poor population mental health (Holmes et al., 2020). However, no studies to date have reported the changing prevalence of depression and anxiety over time during a period of multiple other population-wide stressors. In addition to the importance of documenting these trends, a clearer understanding of the forces that mitigate the population mental health burden during moments of multiple co-occurring traumas may point the way to efforts to mitigate these harms. A central determinant of mental health may be the ability to maintain routine daily activities which has been associated with resilience in the face of mass trauma (Hou et al., 2018; Miller and Rasmussen, 2010). The ability to maintain regular daily activities has been evident among survivors of various natural disasters (Fukuda et al., 1999; Parks et al., 2018), and evidence shows that restoration of pre-disaster daily routines relates to lower psychological distress over time (Goodwin et al., 2020). Among international forced migrants who have been exposed to continuous sociopolitical unrest in their home countries, disruptions of personal, social, and materialistic dimensions of daily routines in host countries relate to higher levels of different psychiatric symptoms over and beyond the adverse mental health impact of pre-migration trauma exposure (Hou et al., 2020).
Therefore, building on the existing literature, we assessed the changing prevalence of probable depression and probable anxiety through 2019–2020, and how disruptions to daily routines and stressors due to the civil unrest and COVID-19 affected these trends. We expected that the prevalence of probable depression and probable anxiety will change across surveys according to different intensity of civil unrest and COVID-19 over time. The prevalence of probable depression and probable anxiety will be the highest among persons with high daily routine disruptions relative to those with low daily routine disruptions across surveys. While high unrest stress and high COVID-19 stress alone will be positively associated with higher odds of probable depression and probable anxiety over time, combined high unrest stress and high COVID-19 stress will demonstrate the strongest positive associations with the odds of probable mental disorders. Controlling for the effects of sociodemographics, the positive associations of unrest stress and COVID-19 stress with probable mental disorders will be stronger among persons with high daily routine disruptions relative to those with low daily routine disruptions.
2. Material and methods
2.1. Respondents and procedure
This study was approved by the Ethics Committee of The Education University of Hong Kong, and the investigation was carried out in accordance with the latest version of the Declaration of Helsinki. Four population-based samples were recruited by random digit dialing using a Computer-Assisted Telephone Interview system in July 2019 (survey 1), February–March 2020 (survey 2), April–May 2020 (survey 3), and July–August 2020 (survey 4). Centre for Communication and Public Opinion Survey and Hong Kong Public Opinion Research Institute were contracted to conduct the surveys. Telephone numbers were drawn from the databases of Hong Kong Communication Authority with a dual-frame sampling approach (50% landline and 50% mobile phone numbers). Each telephone number was used once to prevent repeated participation across the four surveys. The sample frame for these four surveys were being 1. a Hong Kong Chinese resident, 2.15 years of age or older, and 3. Cantonese-speaking. For landline phone calls, if multiple eligible persons were found in a successfully contacted household, the one with the closest birthday to the interview date was selected. Computer-Assisted Telephone Interview system conducted attempts for numbers that were “no answer,” “busy,” or “eligible respondent not at home.” All interviews were conducted during both working and non-working hours from 2pm to 10pm on weekdays and weekends. Oral informed consent was obtained before each interview started. The response rates (i.e., Completed/[Eligibles + Unknown x Eligibles/(Eligibles + Ineligibles)]) were 43% in survey 1, 42.1% in survey 2, 33.8% in survey 3, and 32% in survey 4, according to Response Rate 3 in American Association for Public Opinion Research (AAPOR). The cooperation rates (i.e., sum of completed interviews divided by the eligible numbers) were 72.0% in survey 1, 67.3% in survey 2, 73.5% in survey 3, and 72.8% in survey 4. Data of survey 1–3 was also reported in other previous investigations (Hou et al., 2021a, 2021b). Detailed sampling information for all four surveys were summarized in Supplementary Material 2.
In survey 4, a total of 74,476 telephone numbers were attempted, 29,971 (40.2%) of them were ineligible for interview (i.e., invalid, non-resident/business telephone, fax numbers, no eligible respondent) and 41,712 (56%) were unconfirmed eligible. Among the 2793 (3.8%) eligible numbers, interviews were completed for 2034 (72.8%), 485 (17.4%) refused and 274 (9.8%) eligible respondents did not complete the interviews. A total of 2034 respondents were recruited with a response rate of 32% and a cooperation rate of 72.8% (error = ±1.6%, 95% CI).
The participation and nonparticipation rates were acceptable and comparable with population-representative samples in prior studies in Hong Kong (Galea and Tracy, 2007; Hou et al., 2015; Leung et al., 2005). All samples were weighted according to population demographic characteristics (Census Statistics Department, 2020) to minimize potential selection biases and ensure the generalizability of the findings to the general population.
2.2. Measurements
Unrest stress. Respondents rated to what extent they felt distressed over: 1. government's handling of unrest, 2. widespread and continuous demonstrations and protests, and 3. confrontation between the police and the protestors, and the use of riot control measures including physical assault, tear gas, and rubber bullets, on a 4-point scale (0 = not at all, 1 = some, 2 = quite, 3 = very much). Scores of each item were recoded into low (not at all/some = 0) and high (quite/very much = 1). High unrest stress referred to perceived high stress (i.e., quite/very much) on at least one of the three dimensions of government's handling of the unrest, widespread protests, and the police's confrontation with the protestors and riot control measures. The items are listed in Supplementary Material 3.
COVID-19 stress. Respondents rated to what extent they worried about being infected with COVID-19 on the same 4-point scale as in unrest stress items or perceived threat of 1. life, 2. long-term ill health, and 3. treatment side-effect if they were infected with COVID-19 on a 4-point scale (1 = strongly disagree, 2 = disagree, 3 = agree, 4 = strongly agree) (Supplementary Material 3). Scores for worry item were recoded into low (0 = not at all/some = 0) and high (quite/very much = 1). Items on health-related threat were summed (Cronbach's alpha = 0.82) and recoded into low and high by median split. High COVID-19 stress referred to high scores on worry (quite/very much = 1) or high health/life threat (≥median).
Daily routine disruptions. Respondents rated to what extent daily routines of healthy eating and sleep (1 item) and socializing and leisure activities (1 item) were disrupted in the previous two weeks on an 11-point scale ranging from 0 (no disruption) to 10 (high level of disruptions) (Hou et al., 2019; Lai et al., 2020). These two items were written in line with the categorization of everyday activities into primary and secondary routines (Hou et al., 2018, 2019). Scores on these two items were summed to indicate overall daily routine disruptions and recoded into high disruptions (≥median) and low disruptions (<median).
Probable depression. The Chinese version of the 9-item Patient Health Questionnaire (PHQ-9) (Yu et al., 2012) was used to assess depressive symptoms in the past two weeks (0 = not at all, 1 = on several days, 2 = on more than half of the days, 3 = nearly every day) in survey 1–4. High summed scores indicated higher depressive symptoms (range = 0–27). Chinese version of PHQ-9 has shown high internal consistency among Chinese in the prior studies (α > 0.80) (Yu et al., 2012). Cronbach's alphas in this study were 0.84 in survey 1, 0.86 in survey 2, 0.86 in survey 3, and 0.82 in survey 4. Scores of 10 or above were used to indicate probable depression based on previous population-based studies among Chinese (Hou et al., 2015; Yu et al., 2012). Due to possible overlaps between items in PHQ-9 and daily routine disruptions, we replicated all analyses with the first two items in PHQ-9 (i.e., PHQ-2): “Little interest or pleasure in doing things;” “Feeling down, depressed, or hopeless” with a validated cutoff score of 3 as a sensitivity analysis.
Probable anxiety. The Chinese version of the 7-item Generalized Anxiety Disorder (GAD-7) was used to assess anxiety symptoms on the same 4-point scale as PHQ-9 in previous 2 weeks (Spitzer et al., 2006) from survey 2 to 4. Higher scores indicated higher anxiety symptoms (range 0–21). The scale was shown to be reliable (α = 0.92) and inversely correlated with different dimensions of self-rated health status of the measure was shown across different populations (Spitzer et al., 2006). Cronbach's alpha in this study were 0.93 in survey 2, 0.93 in survey 3, and 0.92 in survey 4. Scores at or exceeding 10 were used to indicate probable anxiety (Plummer et al., 2016).
Demographics. We asked demographic characteristics including age in years, gender (female vs. male), education level (primary or below and secondary vs. tertiary or above), monthly household income (≤HK$19,999, HK$20,000–$39,999, HK$40,000–$59,999, and HK$60,000–$79,999 vs. ≥HK$80,000), employment status (dependent/unemployed vs. employed), home ownership (no vs. yes), savings (<HK$200,000 vs. ≥HK$200,000), income change and saving change since the COVID-19 outbreak (loss vs. gain/no change).
2.3. Analytic plan
First, we calculated the percentage of respondents by demographic characteristics and exposure to daily disruptions, weighted to the Hong Kong Census. Second, we estimated the prevalence of probable depression and probable anxiety with corresponding 95% confidence intervals (CI) stratified by high/low daily routine disruptions across the four surveys from July 2019 to August 2020. Third, we estimated trends of probable depression and probable anxiety from surveys 2 to 4 for four stress groups: 1. low unrest stress and low COVID-19 stress, 2. high unrest stress and low COVID-19 stress, 3. low unrest stress and high COVID-19 stress, and 4. high unrest stress and high COVID-19 stress (Table 1 ). Fourth, we used multiple logistic regression to assess the adjusted associations of stress groups with probable depression and probable anxiety controlling for sociodemographic characteristics in survey 4. In separate models we also analyzed the associations of individual unrest and COVID-19 stressors with probable depression and probable anxiety. All analyses were stratified by high/low daily routine disruptions. Multiple imputation replaced missing data (<6%).
Table 1.
Sample size and percentage of stress groups.
| T2 (n = 2003) |
T3 (n = 2008) |
T4 (n = 2034) |
||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Group | ||||||
| Low unrest stress & low COVID-19 stress | 372 | 18.6 | 289 | 14.4 | 411 | 20.2 |
| High unrest stress & low COVID-19 stress | 627 | 31.3 | 526 | 26.2 | 716 | 35.2 |
| Low unrest stress & high COVID-19 stress | 101 | 5 | 202 | 10 | 118 | 5.8 |
| High unrest stress & high COVID-19 stress | 903 | 45.1 | 991 | 49.3 | 789 | 38.8 |
3. Results
3.1. Sample
We analyzed results on 1112 respondents in survey 1, 2003 respondents in survey 2, 2008 respondents in survey 3, and 2034 respondents in survey 4 in this study. The current samples were weighted by Hong Kong population demographics. Demographic characteristics of the respondents in four surveys, namely age, gender, education level, and monthly household income were reflective of data in 2020 Hong Kong Census (Census Statistics Department, 2020). Supplementary Material 4 illustrates the comparison of survey 4 sample characteristics in July–August 2020 with the population demographic characteristics during the 2020 Hong Kong Census.
3.2. Descriptive results
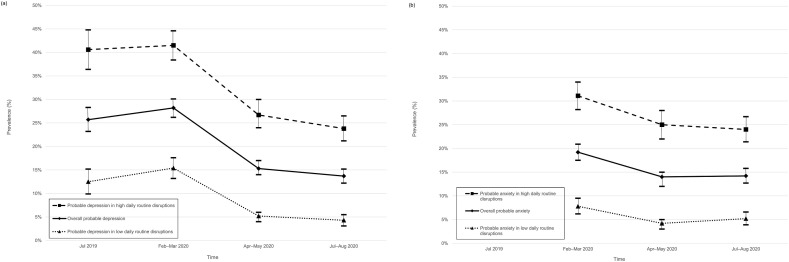
The prevalence of probable depression was 25.7% in July 2019, 28.2% in February–March 2020, 15.3% in April–May 2020, and 13.7% in July–August 2020; the prevalence of probable anxiety was 19.2% in February–March 2020, 14% in April–May 2020, and 14.2% in July–August 2020 (Table 2 ). Overall, the prevalence of probable depression and the prevalence of probable anxiety were lower in the Hong Kong population in April–May 2020 and July–August 2020 than in July 2019 or February–March 2020. The prevalences of probable depression and probable anxiety were higher across surveys among respondents with high daily routine disruptions relative to those with low daily routine disruptions.
Table 2.
Prevalence of probable depression and anxiety among Hong Kong respondents from July 2019 to August 2020.
| Overall |
High daily routine disruptions |
Low daily routine disruptions |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Depressiona |
Anxietyb |
Depressiona |
Anxietyb |
Depressiona |
Anxietyb |
|||||||
| Prevalence (n) | 95% confidence interval | Prevalence (n) | 95% confidence interval | Prevalence (n) | 95% confidence interval | Prevalence (n) | 95% confidence interval | Prevalence (n) | 95% confidence interval | Prevalence (n) | 95% confidence interval | |
| Time | ||||||||||||
| Survey 1 (July 2019) | 25.7% (286) | 23.2, 28.3 | 40.6% (212) | 36.4, 44.8 | 12.5% (74) | 9.9, 15.2 | ||||||
| Survey 2 (February–March 2020) | 28.2% (564) | 26.2, 30.1 | 19.2% (384) | 17.5, 20.9 | 41.5% (406) | 38.4, 44.6 | 31.1% (304) | 28.2, 34.0 | 15.4% (158) | 13.2, 17.6 | 7.8% (80) | 6.2, 9.5 |
| Survey 3 (April–May 2020) | 15.3% (307) | 14.0, 17.0 | 14.0% (281) | 12.0, 15.0 | 26.7% (252) | 24.0, 30.0 | 25.0% (236) | 22.0, 28.0 | 5.2% (55) | 4.0, 6.0 | 4.2% (45) | 3.0, 5.0 |
| Survey 4 (July–August 2020) | 13.7% (278) | 12.2, 15.2 | 14.2% (290) | 12.7, 15.8 | 23.8% (232) | 21.2, 26.5 | 24.0% (234) | 21.4, 26.7 | 4.3% (46) | 3.1, 5.5 | 5.2% (55) | 3.9, 6.6 |
PHQ-9 scores ≥10 were used to define probable depression.
GAD-7 scores ≥10 were used to define probable anxiety, GAD-7 asked in surveys 2–4.
Fig. 1 shows the prevalence of probable depression and probable anxiety stratified by high and low daily routine disruptions across surveys. Probable depression and probable anxiety were higher among persons with high daily routine disruptions than persons with low daily routine disruptions across surveys. The trends of the prevalence of probable depression and probable anxiety from July 2019/February–March 2020 to July–August 2020 were highly consistent.
Fig. 1.
Prevalence of probable (a) depression and (b) anxiety among Hong Kong respondents stratified by high/low daily routine disruptions from July 2019/February–March 2020 to July–August 2020.
Supplementary Material 5 shows the trends of probable depression and probable anxiety for the four stress groups from February–March 2020 to July–August 2020. The trends were highly similar between probable depression and probable anxiety. Overall, the trends of probable depression and probable anxiety were the highest among respondents with high unrest stress and high COVID-19 stress and the lowest among those with low unrest stress and low COVID-19 stress. Among high unrest and low COVID-19 stress group, the trends of probable depression dropped from high to low levels whereas the trends of probable anxiety remained consistently low between February 2020 and May 2020; both trends stabilized between May 2020 and August 2020. Among low unrest and high COVID-19 stress group, the trends of probable depression remained stable and probable anxiety dropped sharply between February 2020 and May 2020 and then became stable between May 2020 and August 2020. Overall, the trends of probable depression started high in February 2020 among low unrest stress and high COVID-19 stress group and high unrest stress and low COVID-19 stress group, but the trends for the two groups reduced and remained stable to a similar level between May 2020 and August 2020. Probable anxiety started higher in February 2020 among lower unrest stress and high COVID-19 stress group relative to high unrest stress and low COVID-19 stress group, but the trends for the two groups converged to a similar level in July–August 2020. Each increase or decrease described above was outside the 95% confidence limit of the estimate at the previous time-point.
Table 3 shows the relations of sociodemographic characteristics with probable depression and probable anxiety. Table 4 shows the associations of unrest stress and COVID-19 stress exposure with probable depression and probable anxiety, controlling for sociodemographic characteristics. Combined high unrest stress and high COVID-19 stress, relative to combined low unrest stress and low COVID-19 stress, were associated with higher probable depression and probable anxiety at both low daily routine disruptions (adjusted odds ratio (aOR) = 7.99–8.50, 95% CI: 2.34–2.82, 25.67–27.30) and high daily routine disruptions (aOR = 2.63–4.99, 95% CI: 1.50–2.55, 4.61–9.77). At high daily routine disruptions, high unrest stress and low COVID-19 stress was also associated with increased likelihood of probable anxiety (aOR = 2.17, 95% CI: 1.06–4.42) relative to combined low unrest stress and low COVID-19 stress.
Table 3.
Multivariable logistic regression examining the associations of socio-demographics with probable depression and anxiety among Hong Kong respondents by high/low daily routine disruptions in July–August 2020.
| High daily routine disruptions (n = 975) |
Low daily routine disruptions (n = 1059) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Depression (n = 232)a |
Anxiety (n = 234)b |
Depression (n = 46)a |
Anxiety (n = 55)b |
|||||
| aOR (95% CI) | p | aOR (95% CI) | p | aOR (95% CI) | p | aOR (95% CI) | p | |
| Gender | ||||||||
| Male | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Female | 1.34 (0.97–1.85) | 0.07 | 1.31 (0.95–1.81) | 0.10 | 0.93 (0.49–1.76) | 0.82 | 1.34 (0.75–2.40) | 0.32 |
| Age | ||||||||
| 15–24 | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| 25–34 | 0.82 (0.48–1.39) | 0.45 | 1.04 (0.61–1.75) | 0.89 | 0.27 (0.07–0.98) | 0.05 | 0.40 (0.14–1.16) | 0.09 |
| 35–44 | 0.44 (0.25–0.80) | 0.01 | 0.42 (0.23–0.76) | 0.004 | 0.66 (0.21–2.10) | 0.49 | 0.39 (0.13–1.17) | 0.09 |
| 45–54 | 0.46 (0.25–0.84) | 0.01 | 0.60 (0.33–1.08) | 0.09 | 0.49 (0.15–1.59) | 0.23 | 0.55 (0.20–1.49) | 0.24 |
| 55–64 | 0.35 (0.19–0.66) | 0.001 | 0.31 (0.16–0.58) | <0.001 | 0.46 (0.13–1.60) | 0.22 | 0.42 (0.14–1.25) | 0.12 |
| 65 or above | 0.68 (0.36–1.29) | 0.24 | 0.33 (0.16–0.65) | 0.002 | 1.03 (0.33–3.19) | 0.95 | 0.29 (0.09–0.97) | 0.04 |
| Education level | ||||||||
| Tertiary education or above | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Secondary education | 0.90 (0.62–1.32) | 0.61 | 0.83 (0.57–1.21) | 0.33 | 0.69 (0.32–1.49) | 0.35 | 0.53 (0.27–1.03) | 0.06 |
| Primary education or below | 0.47 (0.24–0.91) | 0.03 | 0.68 (0.35–1.32) | 0.25 | 0.57 (0.17–1.93) | 0.37 | 0.84 (0.26–2.70) | 0.77 |
| Employment | ||||||||
| Employed | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Dependent/Unemployed | 0.99 (0.68–1.45) | 0.96 | 1.11 (0.76–1.63) | 0.58 | 0.93 (0.44–1.97) | 0.85 | 1.27 (0.65–2.46) | 0.48 |
| Monthly household income (HK$)c | ||||||||
| $80,000 or above | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| $60,000–$79,999 | 1.01 (0.49–2.08) | 0.97 | 1.19 (0.58–2.44) | 0.63 | 2.46 (0.71–8.45) | 0.15 | 0.92 (0.31–2.70) | 0.88 |
| $40,000–$59,999 | 0.96 (0.54–1.73) | 0.90 | 1.26 (0.70–2.27) | 0.43 | 0.73 (0.21–2.47) | 0.61 | 0.87 (0.37–2.09) | 0.76 |
| $20,000–$39,999 | 0.67 (0.37–1.20) | 0.18 | 1.09 (0.61–1.94) | 0.77 | 0.72 (0.23–2.29) | 0.58 | 0.41 (0.16–1.07) | 0.07 |
| $19,999 or below | 1.02 (0.54–1.90) | 0.96 | 1.21 (0.64–2.28) | 0.56 | 0.83 (0.25–2.76) | 0.76 | 0.60 (0.22–1.63) | 0.32 |
| Home ownership | ||||||||
| Yes | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| No | 1.57 (1.03–2.40) | 0.04 | 1.14 (0.76–1.71) | 0.54 | 3.35 (1.29–8.73) | 0.01 | 1.35 (0.66–2.77) | 0.41 |
| Savings | ||||||||
| High | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Low | 1.01 (0.70–1.48) | 0.94 | 0.77 (0.53–1.12) | 0.17 | 1.66 (0.76–3.64) | 0.21 | 1.01 (0.50–2.02) | 0.99 |
| Income change | ||||||||
| Gain/no change | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Loss | 1.22 (0.85–1.74) | 0.29 | 1.38 (0.96–1.98) | 0.08 | 1.72 (0.84–3.50) | 0.14 | 2.02 (1.05–3.90) | 0.04 |
| Savings change | ||||||||
| Gain/no change | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| Loss | 1.35 (0.95–1.94) | 0.10 | 1.29 (0.90–1.85) | 0.16 | 0.91 (0.44–1.90) | 0.80 | 0.99 (0.51–1.93) | 0.97 |
Note: p values are 2 sided.
Abbreviation: aOR, adjusted odds ratio; CI, confidence interval.
PHQ-9 scores ≥10 were used to define probable depression.
GAD-7 scores ≥10 were used to define probable anxiety.
US$1 ≈ HK$7.80.
Table 4.
Adjusted multivariable logistic regression examining the associations of stress groups with probable depression and anxiety among Hong Kong respondents by high/low daily routine disruptions in July–August 2020.
| High daily routine disruptions (n = 975) |
Low daily routine disruptions (n = 1059) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Depression (n = 232)a |
Anxiety (n = 234)b |
Depression (n = 46)a |
Anxiety (n = 55)b |
|||||
| aOR (95% CI) | P | aOR (95% CI) | p | aOR (95% CI) | p | aOR (95% CI) | p | |
| Stress Group | ||||||||
| Low unrest stress and low COVID-19 stress | 1.0 | 1.0 | 1.0 | 1.0 | ||||
| High unrest stress and low COVID-19 stress | 1.63 (0.90–2.96) | 0.11 | 2.17 (1.06–4.42) | 0.03 | 2.91 (0.82–10.28) | 0.10 | 1.39 (0.41–4.77) | 0.60 |
| Low unrest stress and high COVID-19 stress | 1.17 (0.50–2.74) | 0.72 | 1.59 (0.59–4.25) | 0.36 | 2.76 (0.43–17.74) | 0.28 | 2.59 (0.47–14.20) | 0.27 |
| High unrest stress and high COVID-19 stress | 2.63 (1.50–4.61) | 0.001 | 4.99 (2.55–9.77) | <0.001 | 7.99 (2.34–27.30) | 0.001 | 8.50 (2.82–25.67) | <0.001 |
Note: p values are 2 sided.
Abbreviation: aOR, adjusted odds ratio; CI, confidence interval.
PHQ-9 scores ≥10 were used to define probable depression.
GAD-7 scores ≥10 were used to define probable anxiety.
Additional analysis showed that (Supplementary Material 6) high stress towards government's handling of unrest (vs. low stress) was positively associated with probable depression (aOR = 2.10, 95% CI: 1.41–3.14) and probable anxiety (aOR = 2.25, 95% CI: 1.49–3.40) among persons with high daily routine disruptions. Probable anxiety was also positively associated with high stress towards confrontation between the police and the protestors (vs. low stress) and high worry about being infected with COVID-19 (vs. low worry) (aOR = 1.85–1.89, 95% CI: 1.19–1.32, 2.73–2.87) among persons with high daily routine disruptions. Among persons with low daily routine disruptions, high worry about being infected with COVID-19 (vs. low worry) was positively associated with probable depression (aOR = 2.54, 95% CI: 1.29–5.02) and probable anxiety (aOR = 4.77, 95% CI: 2.40–9.48).
All descriptive and inferential statistical analyses were replicated with probable depression defined by PHQ-2 (≥3) (Supplementary Material 7–10) and co-morbid disorders defined by PHQ-9 (≥10) and GAD-7 (≥10) (Palgi et al., 2020) (Supplementary Material 11–14), and found highly consistent findings.
4. Discussion
Using data from four, serial cross-sectional population-representative surveys over 2019 and 2020 in Hong Kong, we found an overall decline in probable depression and anxiety as the civil unrest abated in the first half of 2020. We also found that overall prevalence of probable depression and anxiety were higher among persons with high daily routine disruptions than among persons with low daily routine disruptions. One year after the start of the anti-extradition bill protest (i.e., July 2020), high unrest and combined high unrest-COVID-19 stress—in particular stress about the government's handling of unrest, about confrontations between the police and the protestors and riot control measures, and worry about COVID-19 infection—were associated with probable depression and anxiety among persons with high daily routine disruptions. Among persons with low daily routine disruptions, combined high unrest-COVID-19 stress—in particular worry about COVID-19 infection—was associated with higher risk of probable depression and anxiety.
We found a prevalence of probable depression of 25.7% in the second half of 2019 in current study; this is much higher than the ordinary time and also 11.2% probable depression documented in face-to-face interviews during a similar time point in Hong Kong (Ni et al., 2020). Non-face-to-face assessments can encourage reporting of psychological distress (Benard et al., 2020) and our anonymous telephone surveys might have elicited reports of depression symptoms that might not be reflected in face-to-face interviews, particularly in an area like Hong Kong where mental health remains stigmatized. Other studies during mass traumatic events suggest, consistent with our study, that the prevalence of mental disorders, including depression, anxiety, post-traumatic stress disorder, bipolar disorder, and schizophrenia, can be as high as 22.1% at any point in time in conflict-affected populations across the globe (Charlson et al., 2019). Prevalence of mental disorders could be even higher in regions with more intense conflicts and casualties. For example, the prevalence of depression was 38.5% among a random sample of households in Dogo Nahawa, North-Central Nigeria, where citizens were undergoing frequent and intense violent conflicts and massacre in the past decades (Taru et al., 2018). Prevalences of depression and anxiety were estimated to be 41% and 26% among people in the Kashmir Valley, a region with restricted economic development, political instability including elimination of semi-autonomy provisions by India in 2019, and ongoing armed conflicts (Housen et al., 2017). Further work will be needed to reconcile the different prevalence of probable depression under civil unrest in Hong Kong reported by different studies.
We showed high prevalences of probable depression and anxiety over time among persons with high daily routine disruptions relative to those with low disruptions; these findings were consistent with previous evidence in different populations (Fukuda et al., 1999; Goodwin et al., 2020; Lai et al., 2020; Parks et al., 2018). Although we are not aware that this has been demonstrated in population-based studies after multiple traumas, other work suggests that this is consistent with our growing understanding of how stress affects mental health. Among conflict-affected refugees and forced migrants, previous studies have identified the protective role of stable everyday life experiences against symptoms of depression, anxiety, and post-traumatic stress disorder (Hou et al., 2020; Riza et al., 2020). Clinically, the onset and severity of bipolar spectrum symptoms have been suggested to be dependent upon the regularity of daily routines – irregular routines disrupt circadian rhythms, which predispose to more onsets of mental illnesses and more severe symptomatology (Goodwin and Jamison, 2007). A large body of literature has reported an inverse association between regularity of routines and episode onset in people with bipolar spectrum disorders (Alloy et al., 2015).
We found that the effect of COVID-19 stress compounded the effect of unrest stress, contributing to diminished population mental health. These findings are both consistent with stress sensitization (McLaughlin et al., 2010) and proliferation (Pearlin et al., 1997) hypotheses on the cumulative nature of stressors and provide some of the first data about the relative importance of unrest stress and COVID-19 stress on population mental health. COVID-19 stress was associated with higher prevalence of probable depression and anxiety relative to unrest stress in the beginning of the pandemic (February–March 2020), but then the prevalences converged towards July–August 2020. More importantly, high unrest stress alone and combined high unrest-COVID-19 stress were both associated with probable depression and anxiety among persons with high daily routine disruptions, who already had substantially higher burden of depression and anxiety. Probable depression and anxiety were associated only with combined high unrest-COVID-19 stress among persons with low daily disruptions, suggesting that this group is protected against lower levels of stressors. This suggests that groups with disruptions to daily routines are more vulnerable to the adverse mental health impact of large-scale stressors (Goodwin et al., 2020; Parks et al., 2018).
Some limitations suggest cautions in interpreting the current findings. First, we used self-report instruments (i.e., PHQ-9 and GAD-7) instead of clinical diagnoses to determine probable depression and anxiety. PHQ-9 and GAD-7 are the most extensively psychometrically tested reliable tools across populations (Dear et al., 2011; El-Den et al., 2018; Martin-Subero et al., 2017; Plummer et al., 2016) including Chinese (Chen et al., 2020; Wang et al., 2014, Yu et al., 2012; Zeng et al., 2013). There could be concerns around inflated rates of depression and anxiety using self-report scores (Levis et al., 2020). But high sensitivity of PHQ-9 and GAD-7 for detecting probable depression and anxiety is nonetheless considered suitable for initial population screening and early detection (Dear et al., 2011, El-Den et al., 2018), when clinical interview is not feasible during the pandemic. Second, the response rates ranged between 32% and 43%. Because we did not obtain data on the demographics of people who did not respond to the survey, we were not able to analyze whether non-response was related to demographic factors. Nonetheless, there is no clear link between response rates and validity of data (Ben-Ezra et al., 2021; Galea and Tracy, 2007; Morton et al., 2012), with ample evidence that there may be no systematic difference in validity of surveys with lower or higher response rates as long as surveys are representative and do not embed differential enrolment biases related to the questions of interest (Kohut et al., 2012). Third, the interval between survey 1 and 2 (i.e., 7–8 months) was different from those between other surveys (2–3 months). The intensity of protests and confrontation stayed at high levels starting June 2019 until the outbreak of COVID-19 (Hartley and Jarvis, 2020). Critically, the prevalence of probable depression was higher in survey 2 relative to survey 1, suggesting that our data do capture plausible changes in mental health in the Hong Kong population. Fourth, only generic, health-related COVID-19 stress was assessed in the current study. There existed specific stressors such as the loss of a loved one from COVID-19 that were closely related to probable depression and anxiety. Fifth, cross-sectional design limited causal inference in this study. Directions of the associations between trends of probable depression/anxiety and daily routine disruptions should be interpreted with cautions.
This study is one of the first to describe the trends of mental disorders during simultaneous stressors from unrest and the COVID-19 pandemic. Remission of the current pandemic is yet to come even as civil unrest has been rising in other parts of the world, from the U.S. to Belarus and Lebanon. Our serial data suggest that the effect of COVID-19 stress combines with stress due to unrest to shape population mental health and that the latter may linger longer if civil unrest continues past the COVID-19 era. Exploring policies that help residents safely return to their routines such as eating and sleeping, leisure activities, and socializing with friends may be a ripe area for future research to consider. Disadvantaged persons experiencing disruptions of daily living (Lai et al., 2020, Lai et al., 2021) during COVID-19 are particularly vulnerable to these stressors and require particular attention to mitigate the consequences of the multiple population-based traumas of the moment.
Funding
This work was supported by the Policy Innovation and Co-ordination Office, Hong Kong SAR Government [grant number SR2020.A5.019 to W.K.H.]; Research Grants Council, University Grants Committee, Hong Kong SAR, China [grant number C7069-19 GF, 18600320 to W.K.H and T.M.C.L.]. The funding source had no role in any process of our study.
Author statement
Wai-Kai Hou: Conceptualization, Methodology, Formal analysis, Supervision, Writing - Original Draft, Writing - Review & Editing, Funding acquisition Tsz Wai Li: Methodology, Investigation, Formal analysis, Data Curation, Writing - Review & Editing Li Liang: Investigation, Data Curation, Writing - Review & Editing Huinan Liu: Investigation, Data Curation, Writing - Review & Editing Catherine K. Ettman: Writing - Review & Editing Stevan E. Hobfoll: Writing - Review & Editing Tatia Mei-Chun Lee: Conceptualization, Writing - Review & Editing, Funding acquisition Sandro Galea: Conceptualization, Writing - Original Draft, Writing - Review & Editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2021.11.037.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Alloy L.B., Boland E., Ng T.H., Whitehouse W.G., Abramson L.Y. Low social rhythm regularity predicts first onset of bipolar spectrum disorders among at-risk individuals with reward hypersensitivity. J. Abnorm. Psychol. 2015;124:944–952. doi: 10.1037/abn0000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Ezra M., Hamama-Raz Y., Goodwin R., Leshem E., Levin Y. Association between mental health trajectories and somatic symptoms following a second lockdown in Israel: a longitudinal study. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2021-050480. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benard V., Pignon B., Geoffroy P.A., Benradia I., Roelandt J., Rolland B., Fovet T., D'Hondt F., Thomas P., Vaiva G., Amad A. Depression with and without a history of psychotic symptoms in the general population: sociodemographic and clinical characteristics. J. Affect. Disord. 2020;273:247–251. doi: 10.1016/j.jad.2020.04.048. [DOI] [PubMed] [Google Scholar]
- Census Statistics Department . 2020. Hong Kong Statistics.https://www.censtatd.gov.hk/hkstat/index.jsp [Google Scholar]
- Charlson F., Van Ommeren M., Flaxman A., Cornett J., Whiteford H., Saxena S. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet. 2019;394:240–248. doi: 10.1016/S0140-6736(19)30934-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X., Wang S.B., Li X.L., Huang Z., Tan W., Lin H., Hou C., Jia F. Relationship between sleep duration and sociodemographic characteristics, mental health and chronic diseases in individuals aged from 18 to 85 years old in Guangdong province in China: a population-based cross-sectional study. BMC Psychiatr. 2020;20:455. doi: 10.1186/s12888-020-02866-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi S.Y. When protests and daily life converge: the spaces and people of Hong Kong's anti-extradition movement. Critiq. Anthropol. 2020;40:277–282. doi: 10.1177/0308275X20908322. [DOI] [Google Scholar]
- Dear B.F., Titov N., Sunderland M., McMillan D., Anderson T., Lorian C., Robinson E. Psychometric comparison of the generalized anxiety disorder scale-7 and the penn state worry Questionnaire for measuring response during treatment of generalised anxiety disorder. Cognit. Behav. Ther. 2011;40:216–227. doi: 10.1080/16506073.2011.582138. [DOI] [PubMed] [Google Scholar]
- El-Den S., Chen T., Gan Y., Wong E., O'Reilly C.L. The psychometric properties of depression screening tools in primary healthcare settings: a systematic review. J. Affect. Disord. 2018;225:503–522. doi: 10.1016/j.jad.2017.08.060. [DOI] [PubMed] [Google Scholar]
- Fukuda S., Morimoto K., Mure K., Maruyama S. Posttraumatic stress and change in lifestyle among the hanshin-awaji earthquake victims. Prev. Med. 1999;29:147–151. doi: 10.1006/pmed.1999.0528. [DOI] [PubMed] [Google Scholar]
- Galea S., Tracy M. Participation rates in epidemiologic studies. Ann. Epidemiol. 2007;17:643–653. doi: 10.1016/j.annepidem.2007.03.013. [DOI] [PubMed] [Google Scholar]
- Goodwin F., Jamison K. second ed. Oxford University Press; New York: 2007. Manic-Depressive Illness: Bipolar Disorders and Recurrent Depression. [Google Scholar]
- Goodwin R., Sugiyama K., Sun S., Aida J., Ben-Ezra M. Psychological distress after the Great East Japan Earthquake: two multilevel 6-year prospective analyses. Br. J. Psychiatry. 2020;216:144–150. doi: 10.1192/bjp.2019.251. [DOI] [PubMed] [Google Scholar]
- Hartley K., Jarvis D.S.L. Policymaking in a low-trust state: legitimacy, state capacity, and responses to COVID-19 in Hong Kong. Polic. Soc. 2020;38:403–423. doi: 10.1080/14494035.2020.1783791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Silver R.C., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A.…Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatr. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou W.K., Hall B.J., Canetti D., Lau K.M., Ng S.M., Hobfoll S.E. Threat to democracy: physical and mental health impact of democracy movement in Hong Kong. J. Affect. Disord. 2015;186:74–82. doi: 10.1016/j.jad.2015.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou W.K., Hall B.J., Hobfoll S.E. In: Mental Health of Refugee and Conflict-Affected Populations: Theory, Research and Clinical Practice. Morina N., Nickerson A., editors. Springer; New York: 2018. Drive to thrive: a theory of resilience following loss; pp. 111–133. [Google Scholar]
- Hou W.K., Lai F.T.T., Hougen C., Hall B.J., Hobfoll S.E. Measuring everyday processes and mechanisms of stress resilience: development and initial validation of the Sustainability of Living Inventory (SOLI) 2019. Psychol. Assess. 31. 715-729. [DOI] [PubMed]
- Hou W.K., Liu H., Liang L., Ho J., Kim H., Seong E., Bonanno G.A., Hobfoll S.E., Hall B.J. Everyday life experiences and mental health among conflict-affected forced migrants: a meta-analysis. J. Affect. Disord. 2020;264:50–68. doi: 10.1016/j.jad.2019.11.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou W.K., Hall B., Liang L., Li T.W., Liu H., Galea S. Probable depression and suicidal ideation in Hong Kong amid massive civil unrest. Ann. Epidemiol. 2021;54:45–51. doi: 10.1016/j.annepidem.2020.09.006. [DOI] [PubMed] [Google Scholar]
- Hou W.K., Lee T.M.C., Liang L., Li T.W., Liu H., Ettman C.K., Galea S. Civil unrest, COVID-19 stressors, anxiety, and depression in the acute phase of the pandemic: a population-based study in Hong Kong. Soc. Psychiatr. Psychiatr. Epidemiol. 2021;56:1499–1508. doi: 10.1007/s00127-021-02037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Housen T., Lenglet A., Ariti C., Shah S., Shah H., Ara S., Viney K., Janes S., Pintaldi G. Prevalence of anxiety, depression and post-traumatic stress disorder in the Kashmir Valley. BMJ Glob. Health. 2017;2 doi: 10.1136/bmjgh-2017-000419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohut A., Keeter S., Doherty C., Dimock M., Christian L. 2012. Assessing the Representativeness of Public Opinion Surveys.https://assets.pewresearch.org/wp-content/uploads/sites/5/legacy- pdf/Assessing%20the%20Representativeness%20of%20Public%20Opinion%20Surveys.pdf [Google Scholar]
- Lai F.T.T., Chan V.K.Y., Li T.W., Li X., Hobfoll S.E., Lee T.M.C., Hou W.K. Disrupted daily routines mediate the socioeconomic gradient of depression amid public health crises: A repeated cross-sectional study. Aust. N. Z. J. Psychiatr. 2021 doi: 10.1177/00048674211051271. In press. [DOI] [PubMed] [Google Scholar]
- Lai F.T.T., Hall B.J., Liang L., Galea S., Hou W.K. Socioeconomic determinants of depression amid the anti-extradition bill protests in Hong Kong: the mediating role of daily routine disruptions. J. Epidemiol. Community Health. 2020;74:988–994. doi: 10.1136/jech-2019-213693. [DOI] [PubMed] [Google Scholar]
- Leung G.M., Ho L.M., Chan S.K., Ho S., Bacon-Shone J., Choy R.Y.L., Hedley A.J., Lam T.H., Fielding R. Longitudinal assessment of community psychobehavioral responses during and after the 2003 outbreak of severe acute respiratory syndrome in Hong Kong. Clin. Infect. Dis. 2005;40:1713–1720. doi: 10.1086/429923. [DOI] [PubMed] [Google Scholar]
- Levis B., Benedetti A., Ioannidis J., Sun Y., Negeri Z., He C., Wu Y., Krishnan A., Bhandari P.M., Neupane D., Imaran M., Rice D.B., Riehm K.E., Saadat N., Azar M., Boruff J., Cuijpers P., Gilbody S., Kloda L.A., Thombs B.D. Patient Health Questionnaire-9 scores do not accurately estimate depression prevalence: individual participant data meta-analysis. J. Clin. Epidemiol. 2020;122:115–128.e1. doi: 10.1016/j.jclinepi.2020.02.002. [DOI] [PubMed] [Google Scholar]
- Martin-Subero M., Kroenke K., Diez-Quevedo C., Rangil T., De Antonio M., Morillas R.M., Lorán M.E., Mateu C., Lupon J., Planas R., Navarro R. Depression as measured by PHQ-9 versus clinical diagnosis as an independent predictor of long-term mortality in a prospective cohort of medical inpatients. Psychosom. Med. 2017;79:273–282. doi: 10.1097/PSY.0000000000000390. [DOI] [PubMed] [Google Scholar]
- McLaughlin K.A., Conron K.J., Koenen K.C., Gilman S.E. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychol. Med. 2010;40:1647–1658. doi: 10.1017/S0033291709992121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller K., Rasmussen A. War exposure, daily stressors, and mental health in conflict and post-conflict settings: bridging the divide between trauma-focused and psychosocial frameworks. Soc. Sci. Med. 2010;70:7–16. doi: 10.1016/j.socscimed.2009.09.029. [DOI] [PubMed] [Google Scholar]
- Morton S., Bandara D., Robinson E., Carr P. In the 21stCentury, what is an acceptable response rate? Aust. N. Z. J. Publ. Health. 2012;36:106–108. doi: 10.1111/j.1753-6405.2012.00854.x. [DOI] [PubMed] [Google Scholar]
- Nan H., Lee P., Ni M., Chan B., Lam T. Effects of depressive symptoms and family satisfaction on health related quality of life: the Hong Kong FAMILY study. PLoS One. 2013;8 doi: 10.1111/10.1371/journal.pone.0058436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni M.Y., Yao X.I., Leung K.S.M., Yau C., Leung C.M.C., Lun P., Flores F.P., Chang W.C., Cowling B.J., Leung G.M. Depression and post-traumatic stress during major social unrest in Hong Kong: a 10-year prospective cohort study. Lancet. 2020;395:273–284. doi: 10.1016/S0140-6736(19)33160-5. [DOI] [PubMed] [Google Scholar]
- Palgi Y., Shrira A., Ring L., Bodner E., Avidor S., Bergman Y., Cohen-Fridel S., Keisari S., Hoffman Y. The loneliness pandemic: loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 2020;275:109–111. doi: 10.1016/j.jad.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks V., Drakeford L., Cope M.R., Slack T. Disruption of routine behaviors following the deepwater horizon oil spill. Soc. Nat. Resour. 2018;31:277–290. doi: 10.1080/08941920.2017.1377794. [DOI] [Google Scholar]
- Pearlin L.I., Aneshensel C.S., LeBlanc A.J. The forms and mechanisms of stress proliferation: the case of AIDS caregivers. J. Health Soc. Behav. 1997;38:223–236. doi: 10.2307/2955368. [DOI] [PubMed] [Google Scholar]
- Plummer F., Manea L., Trepel D., McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatr. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- Riza E., Karnaki P., Gil-Salmerón A., Zota K., Ho M., Petropoulou M., Katsas K., Garcés-Ferrer J., Linos A. Determinants of refugee and migrant health status in 10 European countries: the mig-HealthCare project. Int. J. Environ. Res. Publ. Health. 2020;17:6353. doi: 10.3390/ijerph17176353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Taru M.Y., Audu M.D., Philip T.F., John D.F., Yushau A.A., Nnaemeka C.N., Bamidele L.I. Armed conflict and depression among heads of households in dogonahawa, North-Central Nigeria: prevalence and correlates. Open J. Depress. 2018;7:17–30. doi: 10.4236/ojd.2018.72002. [DOI] [Google Scholar]
- Wang W., Bian Q., Zhao Y., Li X., Wang W., Du J., Zhang G., Zhou Q., Zhao M. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatr. 2014;36:539–544. doi: 10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- Yang Y., Song Y., Lu Y., Xu Y., Liu L., Liu X. Associations between erectile dysfunction and psychological disorders (depression and anxiety): a cross‐sectional study in a Chinese population. Andrologia. 2019;51 doi: 10.1111/and.13395. [DOI] [PubMed] [Google Scholar]
- Yu X., Tam W.W., Wong P.T., Lam T.H., Stewart S.M. The Patient Health Questionnaire-9 for measuring depressive symptoms among the general population in Hong Kong. Compr. Psychiatr. 2012;53:95–102. doi: 10.1016/j.comppsych.2010.11.002. [DOI] [PubMed] [Google Scholar]
- Yu W., Singh S., Calhoun S., Zhang H., Zhao X., Yang F. Generalized anxiety disorder in urban China: prevalence, awareness, and disease burden. J. Affect. Disord. 2018;234:89–96. doi: 10.1016/j.jad.2018.02.012. [DOI] [PubMed] [Google Scholar]
- Zeng Q.Z., He Y.L., Liu H., Miao J.M., Chen J.X., Xu H.N., Wang J.Y. Reliability and validity of Chinese version of the Generalized Anxiety Disorder 7-item (GAD-7) scale in screening anxiety disorders in outpatients from traditional Chinese internal department. Chin. Ment. Health J. 2013;27:163–168. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.