Abstract
Aims
Bi-unicondylar arthroplasty (Bi-UKA) is a bone and anterior cruciate ligament (ACL)-preserving alternative to total knee arthroplasty (TKA) when the patellofemoral joint is preserved. The aim of this study is to investigate the clinical outcomes and biomechanics of Bi-UKA.
Methods
Bi-UKA subjects (n = 22) were measured on an instrumented treadmill, using standard gait metrics, at top walking speeds. Age-, sex-, and BMI-matched healthy (n = 24) and primary TKA (n = 22) subjects formed control groups. TKA subjects with preoperative patellofemoral or tricompartmental arthritis or ACL dysfunction were excluded. The Oxford Knee Score (OKS) and EuroQol five-dimension questionnaire (EQ-5D) were compared. Bi-UKA, then TKA, were performed on eight fresh frozen cadaveric knees, to investigate knee extensor efficiency under controlled laboratory conditions, using a repeated measures study design.
Results
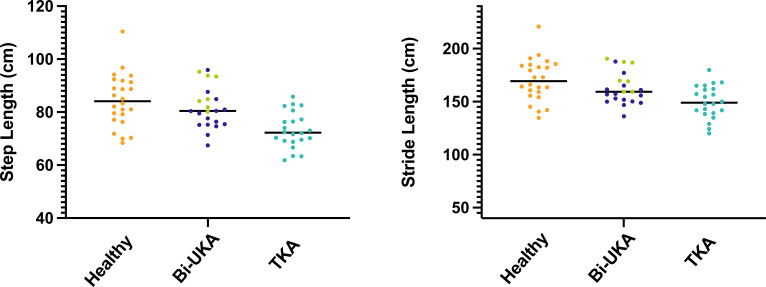
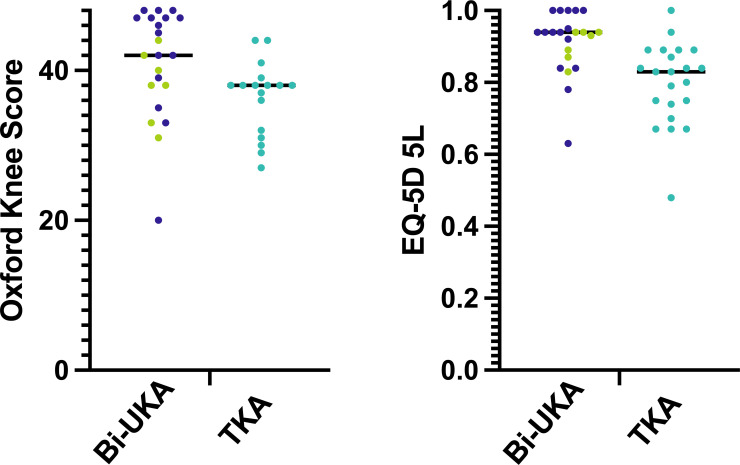
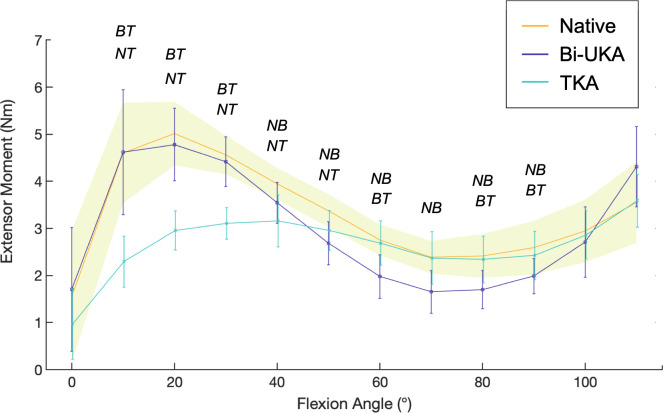
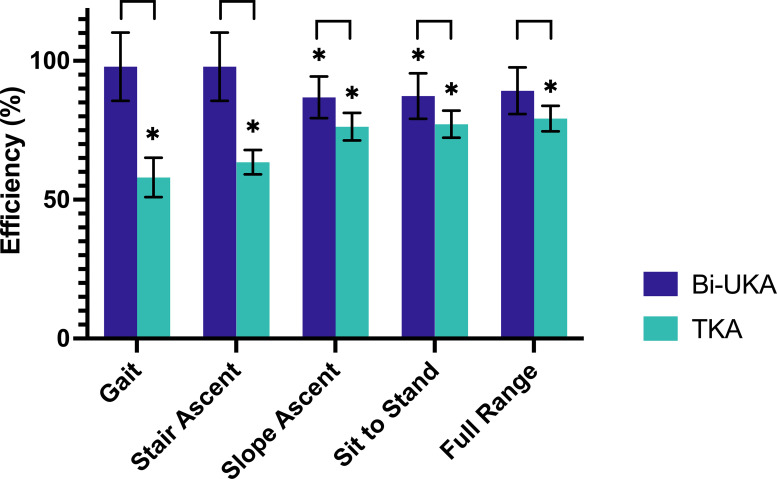
Bi-UKA walked 20% faster than TKA (Bi-UKA mean top walking speed 6.7 km/h (SD 0.9),TKA 5.6 km/h (SD 0.7), p < 0.001), exhibiting nearer-normal vertical ground reaction forces in maximum weight acceptance and mid-stance, with longer step and stride lengths compared to TKA (p < 0.048). Bi-UKA subjects reported higher OKS (p = 0.004) and EQ-5D (p < 0.001). In vitro, Bi-UKA generated the same extensor moment as native knees at low flexion angles, while reduced extensor moment was measured following TKA (p < 0.003). Conversely, at higher flexion angles, the extensor moment of TKA was normal. Over the full range, the extensor mechanism was more efficient following Bi-UKA than TKA (p < 0.028).
Conclusion
Bi-UKA had more normal gait characteristics and improved patient-reported outcomes, compared to matched TKA subjects. This can, in part, be explained by differences in extensor efficiency.
Cite this article: Bone Joint Res 2021;10(11):723–733.
Keywords: Knee extensor biomechanics, Bi-unicondylar compartmental arthroplasty, Gait and functional outcomes, arthroplasties, unicompartmental knee arthroplasty (UKA), total knee arthroplasty (TKA), knees, patient-reported outcomes, Oxford Knee Scores, EQ-5D scores, anterior cruciate ligament (ACL), patellofemoral joint, flexion angles
Article summary
What is the effect of bi-unicondylar arthroplasty (Bi-UKA) on gait, patient-reported outcomes, and extensor biomechanics compared to total knee arthroplasty (TKA).
Key messages
Bi-UKA restores a more normal gait than TKA.
Patients are highly satisfied and report excellent quality of life following Bi-UKA.
Bi-UKA preserves extensor efficiency of the knee, particularly during gait.
Strengths and limitations
Comprehensive investigation of Bi-UKA using a three pronged approach.
Repeated measures cadaveric study with minimal soft-tissue disruption and tendon-loading in anatomical directions.
Limited by lack of preoperative data.
Introduction
Total knee arthroplasty (TKA) remains the standard treatment for end-stage gonarthrosis with a well-documented record of safety and efficacy. 1 Smaller procedures including unicompartmental knee arthroplasty (UKA) are safer, 2 but can appear less successful, in part, owing to the paradoxical effect of differing thresholds for revision. 3 For patients with a well-functioning UKA, the addition of a second UKA for native compartment degeneration is a less invasive option than conversion to TKA. 4,5 The recently revised National Institute of Clinical Excellence (NICE) guidelines highlight this issue, suggesting that procedures following the primary arthroplasty be divided into major and minor revisions. 6 Less commonly, patients with concurrent medial and lateral tibiofemoral degeneration but a preserved patellofemoral joint and functional anterior cruciate ligament (ACL) may be offered primary bi-unicondylar arthroplasty (Bi-UKA), the combination of medial with ipsilateral lateral UKA (Figure 1), as an alternative to TKA, with excellent outcomes reported in medium- and long-term studies. 4,7-11
Fig. 1.
Anterior-posterior and lateral radiographs of the left knee with bi-unicondylar arthroplasty in situ.
Partial knee arthroplasty has been shown to offer improved function over TKA using objective metrics such as gait analysis, particularly in early stance, when the quadriceps are active. 12,13 This correlates with observed differences in extensor biomechanics, 14,15 including preserved efficiency, which may also influence activities such as stair ascent and sit-to-stand. 16 Similar benefits of Bi-UKA, whether a primary or staged procedure, have not been documented.
This study seeks to report the objective and subjective function of Bi-UKA, and determine whether any differences are substantiated by biomechanical investigation. The null hypotheses were thus that no difference will be demonstrable between Bi-UKA, TKA, and native knees in gait, patient-reported outcomes, or extensor biomechanics.
Methods
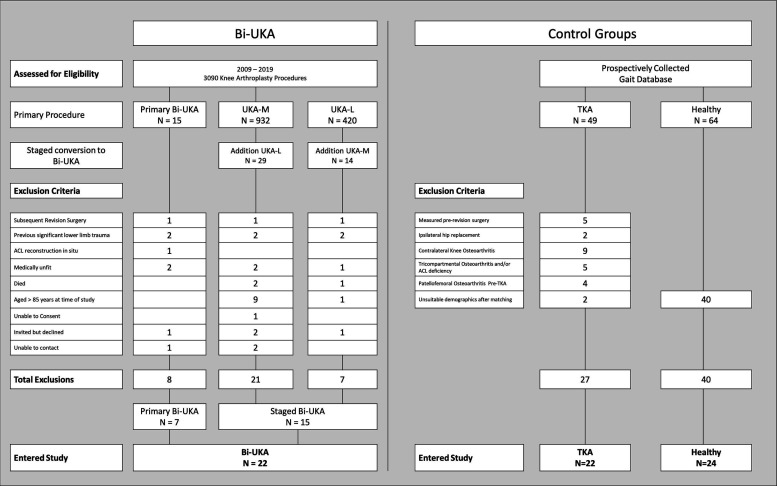
Gait analysis
Previously published differences in fast walking gait on the instrumented treadmill, comparing UKA-M to TKA, demonstrated the UKA-M to be 37% faster than TKAs (top walking speed UKA-M 7.9 km/h, TKA 5.76 km/h). 17 Assuming our TKA cohort would not differ significantly from the TKA subjects in the previous study, we anticipated that the Bi-UKA group may walk up to 15% faster. Thus, to adequately detect differences with 80% power and 95% confidence, 14 subjects per group were required. The senior author’s (JPC) operating lists (2009 to 2019) identified patients who had undergone primary (n = 15) or staged (n = 43) Bi-UKA. We sought to include every subject; however, of the primary Bi-UKA subjects, six were excluded: one of whom had undergone revision to tricompartmental arthroplasty (TCA) through the addition of a patellofemoral arthroplasty, one who had previously undergone ACL reconstruction, and two who had previously had significant lower limb trauma, resulting in post-traumatic OA and significant deformity (Figure 2). From the staged group, one subject had undergone revision of the tibial baseplate of the UKA-L from a mobile bearing design to a fixed-bearing design, for recurrent bearing dislocation. Another patient underwent conversion to Bi-UKA 15 years after primary UKA-M, through the addition of a UKA-L, but four years later sustained a fracture of the UKA-M mobile bearing while playing tennis. At the point of bearing replacement, the well-fixed UKA-M had been in situ for 19 years. Four patients had undergone Bi-UKA due to post-traumatic OA with significant deformity. All were excluded because it would be difficult to accurately interpret gait differences. Five subjects were excluded for medical conditions, including cardiac and neurological conditions and current treatment for cancer. In all, 36 subjects were excluded (Figure 2). Therefore, 22 Bi-UKA subjects (seven primary, 15 staged) were analyzed.
Fig. 2.
Pathway to entry into the clinical outcomes study. ACL, anterior cruciate ligament; Bi-UKA, bi-unicondylar arthroplasty; TKA, posterior cruciate-retaining total knee arthroplasty; UKA-L, lateral unicompartmental arthroplasty; UKA-M, medial unicompartmental arthroplasty.
Matching
For nine years, arthroplasty subjects have been prospectively measured on an instrumented treadmill (Kistler Gaitway, Kistler Instrument Corporation, USA), alongside healthy volunteers. Healthy controls (n = 24) were matched for age, sex, and BMI (Figure 2, Table I).
Table I.
Bi-unicondylar arthroplasty compared to matched healthy controls and total knee arthroplasty subjects: demographic details and gait characteristics at top walking speeds, Oxford Knee Score, and EuroQol five-level five-dimension questionnaire.
| Subject | Healthy | Bi-UKA | TKA |
|---|---|---|---|
| Number of knees | 24 | 22 | 22 |
| Sex, M:F | 14:10 | 14:8 | 12:10 |
| Mean age, yrs | 63 (8) | 68 (13) | 67 (10) |
| Mean BMI, kg/m2 (SD) | 27 (5) | 28 (5) | 27 (4) |
| Mean height, cm (SD) | 173 (10) | 174 (8) | 174 (11) |
| Mean months post-surgery (SD) | 23 (20)* | 52 (51)* | |
| Median months post-surgery (IQR) | 17 (8 to 33) | 24 (16 to 76) | |
| Mean top walking speed, km/h (SD) | 7.4 (0.7) | 6.7 (0.9)* † | 5.6 (0.7)* † |
| Mean Hof speed, H (SD) | 0.7 (0.1) | 0.7 (0.1)* † | 0.6 (0.1)* † |
| Mean weight acceptance rate, BW/s (SD) | 10.8 (3.5) | 10.5 (4.0) | 7.9 (3.8) |
| Mean maximum weight acceptance force, BW (SD) | 1.6 (0.2) | 1.4 (0.1)* † | 1.3 (0.2)* † |
| Mean mid-stance force, BW (SD) | 0.5 (0.1) | 0.6 (0.1)* † | 0.7 (0.1)* † |
| Mean push-off force, BW (SD) | 1.0 (0.2) | 1.0 (0.1) | 1.0 (0.1) |
| Mean push-off rate, BW/s (SD) | 4.3 (1.0) | 4.0 (0.8) | 3.8 (0.9) |
| Mean step length, cm (SD) | 85 (10) | 82 (8)* | 73 (7)* † |
| Mean stride length, cm (SD) | 170 (20) | 163 (15)* | 150 (16)* † |
| Mean step width, cm (SD) | 13 (3) | 14 (3) | 13 (3) |
| Mean cadence, step/min (SD) | 60 (5) | 57 (6)* | 52 (5)* † |
| Mean impulse, BW/s (SD) | 385 (21) | 377 (23) | 380 (29) |
| Mean double support time, s (SD) | 0.28 (0.1) | 0.29 (0.1)* | 0.34 (0.1)* † |
| Mean gait cycle time, s (SD) | 2.0 (0.2) | 2.1 (0.2)* | 2.3 (0.2)* † |
| Mean contact time, s (SD) | 1.3 (0.1) | 1.4 (0.1)* | 1.5 (0.1)* † |
| Mean OKS (SD) | 40.9 (7.1)* | 36.0 (5.3)* | |
| Median OKS (IQR) | 42 (38 to 47)* | 38 (31 to 39)* | |
| Mean EQ-5D (SD) | 0.91 (0.1)* | 0.80 (0.1) * | |
| Median EQ-5D (IQR) | 0.94 (0.88 to 0.95)* | 0.83 (0.74 to 0.89)* |
Significant difference between implant groups (Demographics: RMANOVA, Gait: Mann–Whitney U test, significance p < 0.05 with Bonferroni correction).
Significant difference implant versus healthy control (Mann-Whitney U test, significance p < 0.05 with Bonferroni correction).
Bi-UKA, bi-unicondylar arthroplasty; BW, normalized to body weight; EQ-5D, EuroQol five-dimension questionnaire; IQR, interquartile range; OKS, Oxford Knee Score; RMANOVA, repeated measures analysis of variance; SD, standard deviation; TKA, total knee arthroplasty.
All posterior cruciate-retaining TKA subjects (n = 49) were identified and screened for preoperative radiological evidence of ACL dysfunction and compartmental distribution of arthritis, according to Kellgren and Lawrence (KL) grade. Surgery had been performed by three senior surgeons (JPC, DN, RS). Subjects were excluded if they had anterior tibial translation > 7 mm, suggestive of ACL dysfunction; 18 tricompartmental OA or preoperative evidence of patellofemoral OA KL > 1, regardless of the pattern of wear in the tibiofemoral compartments. After exclusions (Figure 2), 22 TKA controls entered the study. Of these, six had KL grade ≥ 2 bi-tibiofemoral osteoarthritis pre-surgery, while 16 had OA confined to the medial (n = 12) or lateral (n = 4) compartment only.
Subgroup analysis was performed on the staged Bi-UKA subjects (n = 15), although in order to do this, three TKA subjects and four healthy subjects were excluded in order to match the Bi-UKA demographics. Of the 19 TKAs that remained, 12 had isolated medial OA, four had isolated lateral OA, while three had medial and lateral tibiofemoral OA (Supplementary Table i).
Gait analysis and reporting of patient outcomes
Subjects acclimatized to the treadmill during a two-minute 4 km/h warm-up. Speeds were increased in 0.5 km/h increments, with recordings at each speed, to their top walking speed: their fastest comfortable walking speed or highest achievable speed before running. No subjects used the safety rail. The vertical component of ground reaction force, and temporospatial measurements, were recorded by two tandem force plates beneath the belt.
Oxford Knee Scores (OKS) and EuroQol-5D 5L five-dimension five-level (EQ-5D-5L) scores were collected at the time of treadmill testing which, for Bi-UKA, were median 17 months (interquartile range (IQR) 8 to 33) following surgery, while for TKA were median 24 months (IQR 16 to 76) following surgery (p = 0.709, Pearson chi-squared test, Table I).
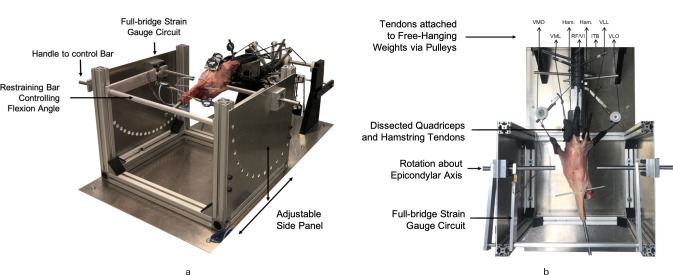
Cadaveric model
Extensor moment and efficiency were investigated, in vitro, using a repeated measures study design. Eight fresh-frozen knees (mid-femur to mid-tibia) from four Caucasian donors (two females, two males) aged between 61 and 66 years, mean BMI 24.5 kg/m2 (standard deviation (SD) 3.88) at death, were used. Specimens had no visible joint surface erosion, misalignment, trauma, or systemic disease known to impact on bone health. All underwent CT-based 3D operative planning (Embody Orthopaedic, UK) to match the Oxford Partial Knee System (Zimmer-Biomet, USA).
Dissected specimens were mounted into an extension rig in accordance with a previously published protocol. 14 In short: the iliotibial band, quadriceps, and hamstring tendons were loaded with a total of 225 N in physiological directions (Table II). 19 Resulting knee extension caused a tibial intramedullary rod to push against a restraining bar, equipped with a calibrated full-bridge strain gauge circuit (Figure 3). Three measurements were taken at each 10° increment of knee extension from 110° to 0°. Efficiency was defined as the ratio of energy output during extension after each arthroplasty to that of the native knee, calculated as the integral of the measured extensor moments over a chosen range. Five ranges of extension were examined that correspond to typical arcs of knee flexion for activities of daily living: 20 the full experimental range (110° to 0°), quadriceps active gait range (30° to 0°), 21 stair ascent (40° to 10°), 22 slope descent (80° to 10°), 23 and sit-to-stand (100° to 0°).
Table II.
Quadriceps, iliotibial band, and hamstring tendon loading weights and direction of pull relative to femoral shaft axis used for extensor moment testing.
| Tendon(s) | Direction of load relative to femoral shaft axis | Load, N | |
|---|---|---|---|
| Anteroposterior | Mediolateral | ||
| Rectus femoris and vastus intermedius | 0° Anterior | 0° Lateral | 61.25 |
| Vastus medialis longus | 0° Anterior | 15° Medial | 24.5 |
| Vastus medialis obliquus | 44° Posterior | 47° Medial | 15.75 |
| Vastus lateralis longus | 0° Anterior | 14° Lateral | 57.75 |
| Vastus lateralis obliquus | 33° Posterior | 35° Lateral | 15.75 |
| Iliotibial band | 6° Posterior | 0° Lateral | 30 |
| Semimembranosus and semitendinosus | 0° Posterior | 0° Medial | 10 |
| Long and short head of biceps femoris | 0° Posterior | 0° Lateral | 10 |
Fig. 3.
Knee extension rig with mounted cadaveric knee: a) front oblique view and b) aerial view, showing dissected tendons, from left to right. VMO, vastus medialis obliquus; VML, vastus medialis longus; Ham., semimembranosus and semitendinosus; RF/VI, rectus femoris with vastus intermedius; Ham., short and long head of biceps femoris; ITB, iliotibial band; VLL, vastus lateralis longus; VLO, vastus lateralis obliquus.
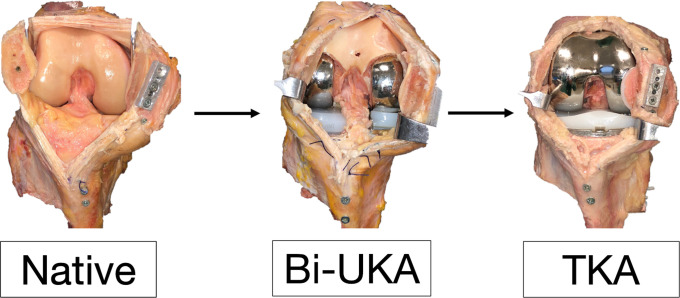
Specimens were tested in the native state; then following Bi-UKA, then again after conversion to TKA (Figure 4). Bi-UKA consisted of a mobile bearing medial UKA and a fixed-bearing lateral UKA (Oxford Partial Knee System, Zimmer-Biomet). Conversion to TKA involved careful removal of Bi-UKA implants, preserving bone stock. Bone cuts for posterior cruciate-retaining TKA (NexGen CR-Flex Zimmer-Biomet) were then performed. Testing order could not be randomized, due to progressive procedure invasiveness. We took steps to mitigate against bone loss, which may have influenced the TKA bone cuts following removal of the Bi-UKA implants. Previous studies from our group have demonstrated that only minimal cementing, without pressurization or bony penetration, is needed to fix the prosthesis to withstand the experimental loading and facilitate bone-sparing revision. 14,15,24 During removal, a fine saw blade was used at the cement-bone interface. The bone bed was visually inspected both after removal of the implants (Supplementary Figure a) and after the TKA bone cuts (Supplementary Figure b). The maximum thickness polyethylene bearing required to balance the TKA were 12 mm (n = 2) with the remaining six knees requiring a 10 mm bearing. Significant bone loss would have necessitated much thicker bearings. Finally, pilot tests were conducted, whereby three knees were tested first in the native state and then after TKA with no intermediate Bi-UKA step. The extension moment trajectories of these three ‘TKA-only’ knees fell within the 95% confidence interval of the whole sample. Further, repeated testing over 16 hours, including over-night refrigeration at 4°C, indicated that TKA was not disadvantaged by being last due to protocol length. Here, all subsequent TKA tests demonstrated similar extension moment and joint kinematic trajectories, in terms of both magnitude and shape, to those measured immediately after TKA. 25
Fig. 4.
Operative states for cadaveric testing. In the native and bi-unicondylar arthroplasty (Bi-UKA) states, the anterior cruciate ligament is intact and the patellofemoral joint is preserved; a transpatellar approach with longitudinal tendon split of rectus femoris, vastus intermedius, and the patellar tendon has been used to prevent disruption to the medial and lateral parapatellar tendons. TKA, total knee arthroplasty.
Statistical analysis
Gait data were normalized for body weight (BW) and leg length (Hof Scaling). 26 Repeated strides were averaged in MatLab (Mathworks, R2018, USA) and then analyzed in SPSS (Version 27, IBM, USA) using Kruskal-Wallis one-way analyses of variance with independent variable of implant state (three groups: healthy, Bi-UKA, and TKA). Post hoc Mann-Whitney U tests with Bonferroni correction (α = 0.05) were used when differences across tests were found.
OKS and EQ-5D for Bi-UKA and TKA were compared using the Mann-Whitney U test, according to overall score (α = 0.05). Descriptive analysis by individual question was undertaken to determine if there were specific areas where the arthroplasty types differed.
The three cadaveric intrastate repeats were averaged in MatLab then analyzed in SPSS. Data were verified normal (Shapiro-Wilk) and then analyzed with repeated measures analysis of variance (RMANOVA, α = 0.05): 1) two-way RMANOVA of extension moment with independent variables implant state (native, Bi-UKA, and TKA) and flexion angle (110° to 0° in 10° increments), and 2) one-way RMANOVAs of work done with independent variable implant state, for the full range of flexion angles (110° to 0°), and for the activity subset flexion angles.
Post hoc paired t-tests with Bonferroni correction were applied when differences across tests were found. Adjusted p-values, multiplied by the appropriate Bonferroni correction value in SPSS, were reported. A p-value < 0.05 was considered statistically significant.
Results
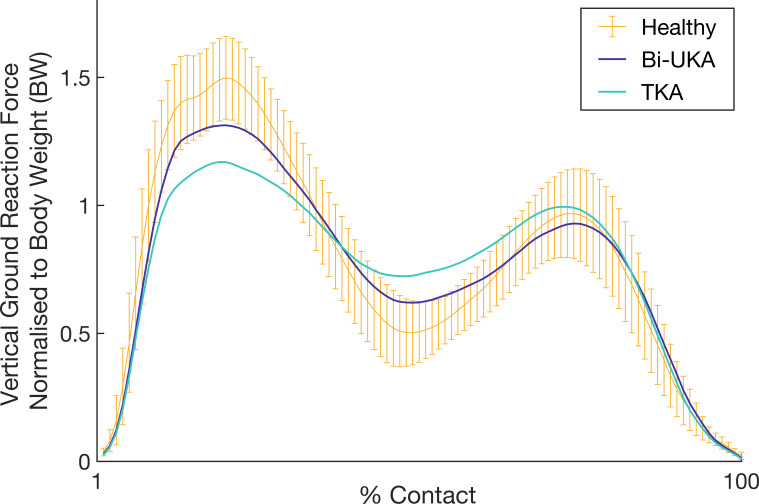
Gait analysis
The groups were well-matched (Table I) in terms of sex (p = 0.827, chi-squared test), age at time of treadmill assessment (p = 0.217, ANOVA), BMI (p = 0.786, ANOVA), height (p = 0.933, ANOVA), and median months between surgery and gait analysis (p = 0.289), although they differed in terms of mean months (p = 0.018, ANOVA). The same was true for the subgroup matching (Supplementary Table i). Healthy subjects walked at 7.4 km/h (SD 0.7), while the Bi-UKA and TKA groups were slower (Table I); however, Bi-UKA walked at 6.7 km/h (SD 0.9), 20% faster than TKA (5.6 km/h (SD 0.7), p < 0.001). Both arthroplasty groups had reduced maximum weight acceptance force compared to healthy subjects, but also differed from each other, with Bi-UKA closer to the healthy range (Table I, Figure 5, healthy vs Bi-UKA, p < 0.018; healthy vs TKA, p < 0.001; Bi-UKA vs TKA, p < 0.02). Similarly, Bi-UKA and TKA had higher mid-stance forces compared to healthy subjects (healthy vs Bi-UKA, p = 0.003, healthy vs TKA, p < 0.001), but Bi-UKA was again closer to the healthy range (Table I, Figure 5, Bi-UKA vs TKA, p < 0.009). Compared to TKA, Bi-UKA subjects had 9 cm (12%) longer step lengths (p = 0.003), 13 cm (9%) longer stride lengths (Figure 6, p = 0.048), and nearer-normal cadence, contact, double support, and gait cycle times (all p < 0.01). When analyzed by subgroup (Supplementary Table i), the staged Bi-UKA subjects, having undergone a minimum of two ipsilateral arthroplasty procedures, continue to be 18% faster (p = 0.006) and, compared to matched primary TKA subjects, preserve nearer-normal weight acceptance (p = 0.033), maximum weight-acceptance force (p = 0.021), mid-stance force (p = 0.048), cadence (p = 0.018), and double support, gait cycle, and contact times (all p < 0.018).
Fig. 5.
Vertical ground reaction force normalized for body weight during stance phase of gait for subjects with a bi-unicondylar arthroplasty (bi-UKA) compared to primary posterior cruciate-retaining total knee arthroplasty (TKA). Normal range for age-, sex-, and BMI-matched healthy subjects is shown with 95% confidence intervals.
Fig. 6.
Median step length and stride length for all bi-unicondylar arthroplasty (Bi-UKA) subjects compared to matched healthy subjects and posterior cruciate-retaining total knee arthroplasty (TKA) subjects. Black line represents the median score, with individual points for each subject shown. Bi-UKA group differentiates subjects by subgroup: primary Bi-UKA (green) and staged Bi-UKA (dark purple).
Patient-reported outcome measures
OKS and EQ-5D scores were analyzed for all arthroplasty subjects. Median OKS was four points higher for Bi-UKA (Bi-UKA 42 (IQR 38 to 47), TKA 38 (IQR 31 to 39), p = 0.004, Mann-Whitney U test, Table I, Figure 7). Bi-UKA scored equal to or higher than TKA for all questions (Table III), with differences noticed particularly in sit-to-stand movements (Q3 3.4 vs 2.8, p = 0.008), Q5 (3.3 vs 2.7, p = 0.027), kneeling (Q7 2.5 vs 1.7, p = 0.031), stability (Q10 3.6 vs 3.0, p = 0.008), and stair descent (Q12 3.5 vs 3.0, p = 0.011, Table III), although the OKS has not been validated for these individual questions.
Fig. 7.
Oxford Knee Score and EuroQol five-dimension five-level (EQ-5D-5L) scores for bi-unicondylar arthroplasty (Bi-UKA) and posterior cruciate-retaining total knee arthroplasty (TKA). Black line represents the median score, with individual points for each subject shown. Bi-UKA group differentiates subjects by subgroup: primary bi-UKA (green) and staged bi-UKA (dark purple).
Table III.
Oxford Knee Scores between bi-unicondylar arthroplasty and total knee arthroplasty groups by overall score, where 48 is the best possible outcome, and by individual question. Each question has a maximum score of 4 for best outcome, and all values are presented as means (standard deviations).
| Category | Bi-UKA | TKA | p-value* |
|---|---|---|---|
| Overall OKS | 40.9 (7.1) | 36 (5.3) | 0.004 |
| Q1. How would you describe the pain you usually have from your knee? | 2.9 (1.0) | 2.5 (1.2) | 0.380 |
| Q2. Have you had any trouble with washing and drying yourself (all over) because of your knee? | 3.8 (0.5) | 3.8 (0.4) | 0.494 |
| Q3. Have you had any trouble getting in or out of the car or using public transport because of your knee? | 3.4 (0.7) | 2.7 (0.9) | 0.008 |
| Q4. For how long have you been able to walk before pain from your knee becomes severe? | 3.6 (0.8) | 3.4 (0.8) | 0.165 |
| Q5. How painful has it been for you to stand up from a chair because of your knee? | 3.3 (0.8) | 2.7 (0.9) | 0.027 |
| Q6. Have you been limping when walking because of your knee? | 3.3 (0.9) | 2.9 (1.1) | 0.176 |
| Q7. Could you kneel down and get up again afterwards? | 2.5 (1.2) | 1.7 (1.0) | 0.031 |
| Q8. Have you been troubled by pain from your knee in bed at night? | 3.5 (0.8) | 3.0 (1.0) | 0.178 |
| Q9. How much has pain from your knee interfered with your usual work? | 3.6 (0.7) | 3.4 (0.9) | 0.401 |
| Q10. Have you felt that your knee may suddenly 'give way' or let you down? | 3.6 (0.8) | 3.1 (0.8) | 0.008 |
| Q11. Could you do the household shopping on your own? | 3.8 (0.6) | 3.6 (1.0) | 0.685 |
| Q12. Could you walk down one flight of stairs? | 3.5 (0.7) | 3.0 (0.8) | 0.011 |
Mann-Whitney U test.
Bi-UKA, bi-unicondylar arthroplasty; OKS, Oxford Knee Score; TKA, total knee arthroplasty.
Bi-UKA subjects reported a median EQ-5D score of 0.94 (IQR 0.88 to 0.95), compared with TKA 0.80 (IQR 0.74 to 0.89, p < 0.001, Table I, Figure 7). Bi-UKA scores were closer to 1 (highest quality of life) in all domains, compared to TKA (Table IV).
Table IV.
EuroQol five-dimension scores between bi-unicondylar arthroplasty and total knee arthroplasty groups by overall score and by individual domain. The best possible outcome for the overall score is 1. Each domain is graded 1 to 5 where 1 is the best overall outcome. Values are presented as means (standard deviations).
| Category | Bi-UKA | TKA | p-value* |
|---|---|---|---|
| Overall EQ-5D | 0.91 (0.1) | 0.80 (0.1) | < 0.001 |
| Mobility | 1.4 (0.7) | 2.2 (0.8) | 0.001 |
| Self-care | 1.2 (0.5) | 1.4 (0.6) | 0.177 |
| Usual activities | 1.4 (0.6) | 2.1 (0.9) | 0.004 |
| Pain | 1.9 (0.7) | 2.5 (0.6) | 0.007 |
| Anxiety | 1.2 (0.5) | 1.4 (0.7) | 0.460 |
Mann-Whitney U test.
Bi-UKA, bi-unicondylar arthroplasty; EQ-5D, EuroQol five-dimension questionnaire; TKA, total knee arthroplasty.
Cadaveric model
In vitro, mean extension moment for the native knees (n = 8) peaked at 20°, at 5.0 Nm (SD 0.3) (Figure 8) notably decreasing toward terminal extension (1.5 Nm (SD 0.6)) and towards a minimum of 2.4 Nm (SD 0.1) at 70° flexion before increasing once again in deep flexion 3.6 Nm (SD 0.4) at 110°. The effects of implant state on extensor moment depended on knee flexion angle (p < 0.001, two-way RMANOVA, Figure 8).
Fig. 8.
Static flexion angles against mean extension moment (Nm) for native knees, bi-unicondylar arthroplasty (Bi-UKA) and total knee arthroplasty (TKA); 95% confidence intervals with a shaded yellow area for the native knee and bars for implanted knees. Italicized letters indicate pairwise statistical differences (p < 0.05). BT, Bi-UKA versus TKA; NB, native versus Bi-UKA; NT, native versus TKA.
The addition of Bi-UKA made little difference at terminal extension 1.7 Nm (SD 0.6; two-way RMANOVA p = 1.000) or 20° 4.8 Nm (SD 0.6; p = 0.356). Between 40° and 100°, Bi-UKA extensor moments were lower than native (two-way RMANOVA, all p < 0.05), with minimum moment of 1.65 Nm (SD 0.2) at 70° (Bi-UKA vs native 31% reduction, p = 0.024, two-way RMANOVA). Bi-UKA extensor moments were within the normal range at 100° (native 2.9 Nm (SD 0.3), Bi-UKA 2.7 Nm (SD 0.3); p = 1.000, two-way RMANOVA) and 110° flexion (Bi-UKA 4.3 Nm (SD 0.4), 19% increase vs native p = 0.080, two-way RMANOVA).
TKA had a highly significant impact on extensor moment at 10° (2.3 Nm (SD 0.2), vs native, two-way RMANOVA p < 0.001, vs Bi-UKA p = 0.002), 20° (3.0 Nm (SD 0.2) 40% reduction vs native two-way RMANOVA p < 0.001, 38% reduction vs Bi-UKA, p < 0.001), and 30° (3.1 Nm (SD 0.1) vs native two-way RMANOVA p < 0.001, vs Bi-UKA p < 0.001). At 40° both Bi-UKA and TKA were reduced compared to the normal range (TKA 3.2 Nm (SD 0.2) vs native two-way RMANOVA p < 0.001, vs Bi-UKA p = 0.063). From 50° to 110°, TKA extensor moments were within the native range (two-way RMANOVA, all p > 0.05) recording a minimum moment of 2.34 Nm (SD 0.2) at 70° and a near native moment at 110° (3.6 (SD 0.2), p = 1.000, two-way RMANOVA).
Extensor efficiency
Over the full flexion range (Figure 9), TKA were less efficient than Bi-UKA (one-way RMANOVA all p < 0.03) and native knees (21% reduction, p < 0.001, one-way RMANOVA). Bi-UKA demonstrated near-normal efficiency in the gait range (30° to 0°, 2% reduction, p = 1.000), while TKA was less efficient than native (42% reduction, p = 0.001, one-way RMANOVA) and Bi-UKA (p = 0.001, one-way RMANOVA). In the stair ascent range (40° to 10°) Bi-UKA was near native (4% reduction, p = 0.402, one-way RMANOVA) while TKA lost 37% efficiency (p < 0.001, one-way RMANOVA). Both arthroplasty states were less efficient than native for the slope ascent (80° to 10°, p < 0.007, one-way RMANOVA) and sit-to-stand (100° to 0°) ranges (p < 0.0026, one-way RMANOVA); however, TKA was least efficient (p < 0.032 vs Bi-UKA, one-way RMANOVA Figure 9).
Fig. 9.
Mean with 95% confidence interval work output by the extending knee over different ranges of motion for bi-unicondylar arthroplasty (Bi-UKA) and total knee arthroplasty (TKA) as a percentage of the native knee work output. Data for gait (30° to 0°), stair ascent (40° to 10°), uphill slope walking (80° to 10°), sit-to-stand (100° to 0°), and full (110° to 0°) ranges of knee flexion are shown. The asterisks (*) indicate data statistically different from the native knee, and brackets indicate differences between the arthroplasties (paired t-tests p < 0.05).
Discussion
Improved function following Bi-UKA compared to TKA was measured across three domains: gait, patient-reported outcomes, and in vitro, overturning the null hypotheses. In vivo, Bi-UKA restored nearer-normal weight-acceptance and mid-stance forces, when the quadriceps are active. 12 This may be explained by differences observed in extensor function in vitro: extensor efficiency was greatly reduced following TKA over the quadriceps active gait range compared to both Bi-UKA and the native knee. Although important for all activities, extensor efficiency is particularly relevant for daily activities with a high number of cycles, including stair ascent and fast walking, 12,14 where Bi-UKA presently outperformed TKA. This study suggests that TKA patients may expend significantly more energy to achieve the same function during these activities, corroborating findings of others, who have shown abnormal flexion-extension moments following TKA, attributing this to reduced quadriceps effectiveness. 12,23 This finding was supported by the patient-reported outcomes.
Arthroplasty performance can be measured reliably on the instrumented treadmill, particularly during fast walking. 13,17,27 With every 0.1 m/s increase in top walking speed, life expectancy improves significantly, 17 making the reported difference in top walking speed meaningful. During flexion, TKA demonstrates paradoxical anterior-posterior translation, limiting mid-swing flexion, and reducing stride length and walking speed. 26 Bi-UKA is more anterior-posterior stable, which may explain observed differences in step and stride length. 24 This study supports the findings of Banks et al 28 regarding the gait and kinematics of four Bi-UKA subjects, and one subject with a TKA femoral component but medial and lateral tibial unicompartmental components, compared to contralateral healthy knees, UKA, and TKA. Bi-UKA patients demonstrated higher knee flexion from heel-strike to mid-stance than TKA patients, but similar flexion in late stance through swing phase. 28
Bi-UKA patients reported higher OKS and EQ-5D scores than TKA. The OKS is said to have a minimal important difference (MID) of five points. 29 The present study found a mean difference in OKS of 4.9, hence conclusions beyond noninferiority compared to TKA are limited except to say that both arthroplasty groups were satisfied, but there appears to be a stiatistical advantage of Bi-UKA over TKA, which warrants an adequately powered study to determine if clinically relevant. The TKA patient-reported outcomes in this study reflected those of larger studies, including TOPKAT. 30-33 Confalonieri et al 34 reported higher satisfaction and functional scores with Bi-UKA compared to TKA, aligning with present findings. Although the OKS is not validated according to individual questions, the differences in relation to alighting a vehicle, rising from a chair, stair ascent, and kneeling are noteworthy, and support the concept that Bi-UKA preserves isokinetic quadriceps strength, 12 further reinforced by the cadaveric data. ACL preservation in Bi-UKA may, in part, explain differences in stability.
The ability to independently orientate each UKA to the native compartmental anatomy is a strength of Bi-UKA. However, this freedom increases technical difficulty and opportunity for error, which may limit widespread adoption. Patients in the gait study underwent surgery with standard instrumentation, performed by JPC, an expert knee arthroplasty surgeon with a highly specialized partial knee arthroplasty practice. In vitro, procedures were performed by AJG, a skilled but not expert surgeon, again with conventional instumentation. Compared to TKA, Bi-UKA, implanted with robotic assistance, better maintains native kinematics while restoring coronal joint line obliquity and constitutional alignment. 35 It is conceivable that robotics might reduce the technical demands of Bi-UKA, improve alignment accuracy, and support surgeons willing to use the procedure in appropriate patients. 36-38
This study has limitations: the clinical element is small, patients were not randomized, and there is a lack of preoperative data. TKA subjects were drawn retrospectively from a database, meaning that the timing of measurement on the instrumented treadmill varied, with some subjects measured relatively early in their recovery phase, while others had undergone surgery much longer ago. The TKA group were further from surgery, meaning that they likely had had more opportunity to recover and rehabilitate. 30,39 If so, the effect would favour the TKA group, meaning that false positives are less likely, strengthening the conclusions of this work. This study used the OKS and EQ-5D since these are broad and capture trends across a wide spectrum of joint pathologies. However, a ceiling effect is visible in the Bi-UKA dataset (Figure 5), suggesting that future research may benefit from other scores less susceptible to ceiling effects.
The arthroplasty subjects were not propensity matched, nor were their patterns of disease. However, only TKA subjects with one- or two-compartment arthritis, without evidence of ACL dysfunction on preoperative radiographs, were included, while those with tricompartmental disease or anterior tibial translation > 7 mm were excluded, in an attempt to exclude TKA subjects who may have been ineligible for Bi-UKA. All TKA subjects included in this study would have been considered appropriate for isolated medial/lateral UKA, or Bi-UKA by JPC, the senior surgical author. Out of 22 TKA patients, 16 (73%) had only single tibiofemoral compartment arthritis pre-arthroplasty. The inclusion of single-compartment OA patients in the TKA group was necessary to power the study, but perhaps disadvantaged the Bi-UKA group, since all had bi-tibiofemoral arthritis. Further, all TKA subjects had undergone only one procedure, whereas 15 of 22 (68%) Bi-UKA patients had undergone two separate arthroplasty procedures, which many would consider another disadvantage for the Bi-UKA group.
The subgroup analysis demonstrates objective benefits of staged Bi-UKA compared to primary TKA, preserving the well-functioning primary PKA, rather than removing it and converting to TKA. This second procedure would be classified a PR2a revision, according to the Revision Partial Knee Classification (RPKC) system, 40 making it a minor revision, in line with the recommendations made by NICE. 6
The gait and cadaveric methodologies complement each other. The cadaveric model allowed within-specimen repeated measures analyses, eliminating confounding factors including anatomical variance or quadriceps deficiency, only varying implant state. However, this model cannot account for postoperative rehabilitation, nor does it replicate true in vivo loading or kinematics, which are inherently captured by gait measurements. In vivo, muscle forces vary dynamically, an order of magnitude higher than in the cadaveric experiment. Loading in physiological directions was prioritized over magnitude, so efficiency data were normalized to the native knee, accounting for load reduction. Increasing procedure invasiveness made randomization of testing order impossible. However, pilot data found no difference in extensor moment trend, or any deleterious effect of repeated testing. Analysis of kneeling and other complex knee movement was not possible during the current study, but may be advantageous in order to determine differences between Bi-UKA and TKA among higher-functioning patients.
In summary, benefits for Bi-UKA are reported in gait and patient-reported outcomes, substantiated by advantageous in vitro biomechanics. These data support the concept that staged Bi-UKA is an acceptable alternative to conversion to TKA, or rarely, as a primary procedure.
Author contributions
A. J. Garner: Conceptualization, Methodology, Investigation, Formal analysis, Writing – original draft.
O. Dandridge: Investigation, Formal analysis, Writing – review & editing.
A. A. Amis: Methodology, Writing – review & editing.
J. Cobb: Conceptualization, Formal analysis, Writing – review & editing.
R. J. van Arkel: Methodology, Writing – review & editing.
Funding statement
This work was funded by the Sir Michael Uren Foundation; The Royal College of Surgeons of England and the Dunhill Medical Trust Clinical Research Fellowship. Infrastructure support was provided by the National Institute for Health Research (NIHR) Imperial Biomedical Research Centre (BRC). Human samples used in this research project were obtained from the Imperial College Healthcare Tissue Bank (ICHTB). ICHTB is supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Imperial College Healthcare NHS Trust and Imperial College London. ICHTB is approved by Wales REC3 to release human material for research (17/WA/0161). Surgical instruments and implants for the in vitro study were supplied by Zimmer Biomet (Warsaw, USA). The instrumented treadmill was provided by The Centre of Excellence in Medical Engineering funded by the Wellcome Trust and EPSRC under grant number WT 088844/Z/09/Z. The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement
R. J. van Arkel reports a research support grant from DePuy Synthes. O. Dandridge and A. Garner report provision of surgical instruments and implants for this study from Zimmer Biomet. A. Garner also reports research grants from Dunhill Medical Trust, RCS England, and the Sir Michael Uren Foundation for this study. J. Cobb reports an institutional grant from Zimmer Biomet for this study, and board membership on Orthonika, consultancy payments from JRI, an institutional grant from DePuy Synthes, payment for lectures from Ceramtex, a patent and stocks from Embody, and royalties from Matortho, all unrelated to this study.
Acknowledgements
The authors would like to thank Mr Dinesh Nathwani and Mr Robyn Strachan for their contribution of Total Knee Arthroplasty patients to the Gait Analysis Database. Thanks also go to Dr Amy Maslivec and Miss Rhiannon Jones for their contribution toward data collection in the gait laboratory, and to Miss Jennifer Stoddart for her contribution toward data collection in the cadaveric laboratory.
Ethical review statement
This study was conducted with full ethical approval. Data were collected in the gait laboratory with Institutional Review Board approval from NRES Committee South Central - Oxford B, Study title: 3D and 2D Motion Capture Gait Analysis of Lower Limb Orthopaedic Patients. REC reference: 14/SC/1243. IRAS project ID: 136430 and from the Academic Health Science Centre, Imperial College London and Imperial College Healthcare NHS Trust. Project Title: Gait Analysis Using An Instrumented Treadmill. Joint Research Office Reference number: JROHH0208. Ethics Reference number: 10/H0807/101. The cadaveric work was conducted with approval from Imperial College Healthcare Tissue Bank. ICHTB HTA licence: 12275, REC Wales approval: 12/WA/0196, Project title: Physiological load transfer in hip and knee replacement, Tissue Bank application number R15022-5A.
Open access funding
The authors report that they received open access funding for their manuscript from the Sir Michael Uren Foundation, through Imperial College, London, UK.
Follow A. J. Garner @dramygarner
Follow O. W. Dandridge @OliDandridge
Follow J. P. Cobb @orthorobodoc
Follow R. J. van Arkel @ICBiomechanics
Supplementary material
Subgroup analysis of gait data for staged bi-unicondylar arthroplasty compared to a matched cohort of primary posterior cruciate-retaining total knee arthroplasty subjects and healthy controls.
Contributor Information
Amy J. Garner, Email: a.garner@imperial.ac.uk.
Oliver W. Dandridge, Email: o.dandridge18@imperial.ac.uk.
Andrew A. Amis, Email: a.amis@imperial.ac.uk.
Justin P. Cobb, Email: j.cobb@imperial.ac.uk.
Richard J. van Arkel, Email: r.vanarkel@imperial.ac.uk.
References
- 1. No authors listed . 16th Annual report 2019. National Joint Registry. 2019. https://reports.njrcentre.org.uk/portals/0/pdfdownloads/njr%2016th%20annual%20report%202019.pdf (date last accessed 25 October 2021).
- 2. Liddle AD, Judge A, Pandit H, Murray DW. Adverse Outcomes after Total and Unicompartmental Knee Replacement in 101,330 Matched Patients: A Study of Data from the National Joint Registry for England and Wales. Lancet. 2014;384(9952):1437–1445. [DOI] [PubMed] [Google Scholar]
- 3. Goodfellow JW, O’Connor JJ, Murray DW. A critique of revision rate as an outcome measure: re-interpretation of knee joint registry data. J Bone Joint Surg Br. 2010;92-B(12):1628–1631. [DOI] [PubMed] [Google Scholar]
- 4. Stoddart JC, Dandridge O, Garner A, Cobb J, van Arkel RJ. The compartmental distribution of knee osteoarthritis - a systematic review and meta-analysis. Osteoarthr Cartil. 2021;29(4):445–455. [DOI] [PubMed] [Google Scholar]
- 5. Pandit H, Mancuso F, Jenkins C, et al. Lateral unicompartmental knee replacement for the treatment of arthritis progression after medial unicompartmental replacement. Knee Surg Sports Traumatol Arthrosc. 2017;25(3):669–674. [DOI] [PubMed] [Google Scholar]
- 6. No authors listed . Joint replacement (primary): hip, knee and shoulder: NICE guideline [NG157]. National Institute for Health and Care Excellence (NICE). 2020. https://www.nice.org.uk/guidance/ng157 (date last accessed 12 October 2021). [PubMed]
- 7. Garner A, van Arkel RJ, Cobb J. Classification of combined partial knee arthroplasty. Bone Joint J. 2019;101-B(8):922–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Engelbrecht E, Siegel A, Rottger J, Buchholz HW. Statistics of total knee replacement: Partial and total knee replacement, design st. Georg: A review of a 4-year observation. Clin Orthop Relat Res. 1976;120:54–64. [PubMed] [Google Scholar]
- 9. Parratte S, Ollivier M, Lunebourg A, Abdel MP, Argenson JN. Long-term results of compartmental arthroplasties of the knee: Long term results of partial knee arthroplasty. Bone Joint J. 2015;97-B(10 Suppl A):9–15. [DOI] [PubMed] [Google Scholar]
- 10. Romagnoli S, Zacchetti S, Perazzo P, Verde F, Banfi G, Viganò M. Onsets of complications and revisions are not increased after simultaneous bilateral unicompartmental knee arthroplasty in comparison with unilateral procedures. Int Orthop. 2015;39(5):871–877. [DOI] [PubMed] [Google Scholar]
- 11. Biazzo A, Manzotti A, Confalonieri N. Bi-unicompartmental versus total knee arthroplasty: Long term results. Acta Orthop Belg. 2018;84(3):237–244. [PubMed] [Google Scholar]
- 12. Lundberg HJ, Rojas IL, Foucher KC, Wimmer MA. Comparison of antagonist muscle activity during walking between total knee replacement and control subjects using unnormalized electromyography. J Arthroplasty. 2016;31(6):1331–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wiik AV, Manning V, Strachan RK, Amis AA, Cobb JP. Unicompartmental knee arthroplasty enables near normal gait at higher speeds, unlike total knee arthroplasty. J Arthroplasty. 2013;28(9 Suppl):176–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Garner A, Dandridge O, Amis AA, Cobb JP, van Arkel RJ. The extensor efficiency of unicompartmental, bicompartmental, and total knee arthroplasty. Bone Joint Res. 2021;10(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Joseph MN, Carmont MR, Tailor H, Stephen JM, Amis AA. Total knee arthroplasty reduces knee extension torque in-vitro and patellofemoral arthroplasty does not. J Biomech. 2020;104:109739. [DOI] [PubMed] [Google Scholar]
- 16. Mizner RL, Snyder-Mackler L. Altered loading during walking and sit-to-stand is affected by quadriceps weakness after total knee arthroplasty. J Orthop Res. 2005;23(5):1083–1090. [DOI] [PubMed] [Google Scholar]
- 17. Jones GG, Kotti M, Wiik AV, et al. Gait comparison of unicompartmental and total knee arthroplasties with healthy controls. Bone Joint J. 2016;98-B(10_Supple_B):16–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chiu SS. The anterior tibial translocation sign. Radiology. 2006;239(3):914–915. [DOI] [PubMed] [Google Scholar]
- 19. Bull AM, Andersen HN, Basso O, Targett J, Amis AA. Incidence and mechanism of the pivot shift. An in vitro study. Clin Orthop Relat Res. 1999;363:219–231. [PubMed] [Google Scholar]
- 20. Ellis MI, Seedhom BB, Wright V. Forces in the knee joint whilst rising from a seated position. J Biomed Eng. 1984;6(2):113–120. [DOI] [PubMed] [Google Scholar]
- 21. Winter D. The Biomechanics and Motor Control of Human Gait. Waterloo, Canada: University of Waterloo Press. 1988. [Google Scholar]
- 22. Adiputra LS, Parasuraman S, khan MKAA, Elamvazuthi I. Bio mechanics of desending and ascending walk. Procedia Computer Science. 2015;76:264–269. [Google Scholar]
- 23. Montgomery JR, Grabowski AM. The contributions of ankle, knee and hip joint work to individual leg work change during uphill and downhill walking over a range of speeds. R Soc Open Sci. 2018;5(8):180550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Garner AJ, Dandridge OW, Amis AA, Cobb JP, van Arkel RJ. Partial and combined partial knee arthroplasty: greater anterior-posterior stability than posterior cruciate-retaining total knee arthroplasty. J Arthroplasty. 2021;36(11):3765–3772.e4. [DOI] [PubMed] [Google Scholar]
- 25. Dandridge O, Garner A, Jeffers JRT, Amis AA, Cobb JP, van Arkel RJ. Validity of repeated-measures analyses of in vitro arthroplasty kinematics and kinetics. J Biomech. 2021;129:110669. [DOI] [PubMed] [Google Scholar]
- 26. Hof AL. Scaling gait data to body size. Gait & Posture. 1996;4(3):222–223. [Google Scholar]
- 27. Garner AJ, Dandridge OW, van Arkel RJ, Cobb JP. The compartmental approach to revision of partial knee arthroplasty results in nearer-normal gait and improved patient reported outcomes compared to total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2021; Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Banks SA, Fregly BJ, Boniforti F, Reinschmidt C, Romagnoli S. Comparing in vivo kinematics of unicondylar and bi-unicondylar knee replacements. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):551–556. [DOI] [PubMed] [Google Scholar]
- 29. Beard DJ, Harris K, Dawson J, et al. Meaningful changes for the Oxford hip and knee scores after joint replacement surgery. J Clin Epidemiol. 2015;68(1):73–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Williams DP, Blakey CM, Hadfield SG, Murray DW, Price AJ, Field RE. Long-term trends in the Oxford knee score following total knee replacement. Bone Joint J. 2013;95-B(1):45–51. [DOI] [PubMed] [Google Scholar]
- 31. Burn E, Sanchez-Santos MT, Pandit HG, et al. Ten-year patient-reported outcomes following total and minimally invasive unicompartmental knee arthroplasty: A propensity score-matched cohort analysis. Knee Surg Sports Traumatol Arthrosc. 2018;26(5):1455–1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Liddle AD, Pandit H, Judge A, Murray DW. Patient-reported outcomes after total and unicompartmental knee arthroplasty: A study of 14,076 matched patients from the national joint registry for England and Wales. Bone Joint J. 2015;97-B(6):793–801. [DOI] [PubMed] [Google Scholar]
- 33. Beard DJ, Davies LJ, Cook JA, MacLennan G, Price A, Kent S, et al. The Clinical and Cost-Effectiveness of Total versus Partial Knee Replacement in Patients with Medial Compartment Osteoarthritis (TOPKAT): 5-Year Outcomes of a Randomised Controlled Trial. Lancet. 2019;394(10200):746–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Confalonieri N, Manzotti A, Cerveri P, De Momi E. Bi-unicompartmental versus total knee arthroplasty: A matched paired study with early clinical results. Arch Orthop Trauma Surg. 2009;129(9):1157–1163. [DOI] [PubMed] [Google Scholar]
- 35. Banger MS, Johnston WD, Razii N, et al. Robotic arm-assisted bi-unicompartmental knee arthroplasty maintains natural knee joint anatomy compared with total knee arthroplasty: A prospective randomized controlled trial. Bone Joint J. 2020;102-B(11):1511–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jones GG, Clarke S, Jaere M, Cobb J. 3d printing and unicompartmental knee arthroplasty. EFORT Open Rev. 2018;3(5):248–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kayani B, Haddad FS. Robotic unicompartmental knee arthroplasty: Current challenges and future perspectives. Bone Joint Res. 2019;8(6):228–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Clement ND, Bell A, Simpson P, Macpherson G, Patton JT, Hamilton DF. Robotic-assisted unicompartmental knee arthroplasty has a greater early functional outcome when compared to manual total knee arthroplasty for isolated medial compartment arthritis. Bone Joint Res. 2020;9(1):15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Scott CEH, Bell KR, Ng RT, MacDonald DJ, Patton JT, Burnett R. Excellent 10-year patient-reported outcomes and survival in a single-radius, cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1106–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Garner AJ, Edwards TC, Liddle AD, Jones GG, Cobb JP. The revision partial knee classification system: understanding the causative pathology and magnitude of further surgery following partial knee arthroplasty. Bone Jt Open. 2021;2(8):638–645. [DOI] [PMC free article] [PubMed] [Google Scholar]