Musculoskeletal infections are common and often difficult to treat. 1,2 Their diagnostics and treatment are an integral part of the daily clinical routine of every orthopaedic and trauma surgeon. Diagnostics and first treatment approaches are often initiated prior to referrals to a specialized centre. Treatment algorithms in the field of musculoskeletal infections, based on clinical and experimental empiricism, promise successful treatment courses in many cases, 3-5 although a considerable proportion of bone and joint infections are characterized by treatment failure, for a variety of reasons. 6
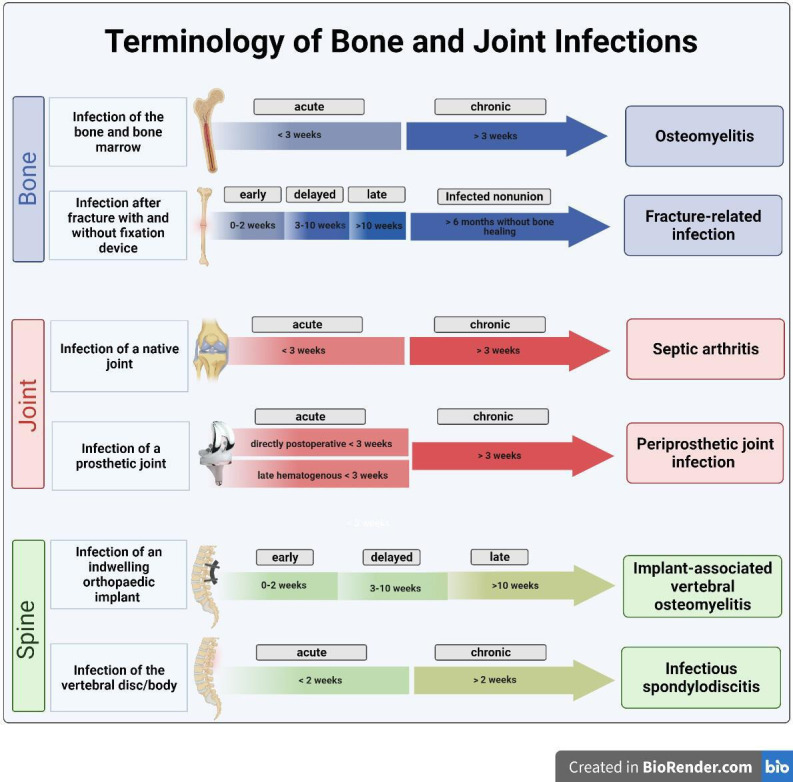
The basic prerequisite for the initiation of correct diagnostics, and thus consecutive best possible therapy, is the correct terminology of individual bone and joint infections. A variety of terms exists to describe bone and joint infections. Osteomyelitis, implant-associated infection, fracture-related infection (FRI), and infected nonunion denote bone infections. Joint infections are described by periprosthetic joint infection (PJI) and septic arthritis, with its synonyms of supportive and infectious arthritis. In the spine, a distinction can be made between implant-associated vertebral osteomyelitis and hematogenous spondylodiscitis according to the aetiology. Even among experts in the field, terms are interchanged and used synonymously. It often appears to be difficult to arrive at exact definitions, which naturally limits the understanding of optimal treatment. For FRI and PJI, diagnostic criteria have been developed, and in the case of PJI those criteria have been continuously improved and are still the subject of scientific discussion. 7-9
To lay the foundation for optimal therapy using the correct terminology of the underlying condition, this infographic presents the hallmarks of bone and joint infections and diagnostic criteria.
Author contributions
M. Rupp: Conceptualization, Methodology, Project administration, Writing – original draft, Writing – review & editing, Visualization.
N. Walter: Formal analysis, Methodology, Software, Writing – review & editing, Visualization.
S. Baertl: Formal analysis, Methodology, Software, Writing – review & editing, Visualization.
S. Lang: Formal analysis, Methodology, Software, Writing – review & editing.
V. Alt: Conceptualization, Project administration, Resources, Validation, Writing – review & editing, Supervision.
D. W. Lowenberg: Conceptualization, Supervision, Validation, Writing – review & editing.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement
D. W. Lowenberg reports consultancy payments from Nuvasive Orthopaedics, and sits on the board for Genae Corp, unrelated to the article.
Contributor Information
Markus Rupp, Email: Markus.rupp@ukr.de.
Nike Walter, Email: nike.walter@ukr.de.
Susanne Baertl, Email: susanne.baertl@ukr.de.
Siegmund Lang, Email: siegmund.lang@ukr.de.
Volker Alt, Email: volker.alt@ukr.de.
References
- 1. Kurtz SM, Lau EC, Son MS, Chang ET, Zimmerli W, Parvizi J. Are We Winning or Losing the Battle With Periprosthetic Joint Infection: Trends in Periprosthetic Joint Infection and Mortality Risk for the Medicare Population. J Arthroplasty. 2018;33(10):3238–3245. [DOI] [PubMed] [Google Scholar]
- 2. Walter N, Rupp M, Lang S, Alt V. The epidemiology of fracture-related infections in Germany. Sci Rep. 2021;11(1):10443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Walter N, Rupp M, Hierl K, et al. Long-term patient-related quality of life after fracture-related infections of the long bones. Bone Joint Res. 2021;10(5):321–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Petis SM, Abdel MP, Perry KI, Mabry TM, Hanssen AD, Berry DJ. Long-Term Results of a 2-Stage Exchange Protocol for Periprosthetic Joint Infection Following Total Hip Arthroplasty in 164 Hips. J Bone Joint Surg Am. 2019;101-A(1):74–84. [DOI] [PubMed] [Google Scholar]
- 5. Slullitel PA, Oñativia JI, Cima I, et al. Patients with no recurrence of infection five years after two-stage revision hip arthroplasty may be classified as periprosthetic infection ’in remission. Bone Joint J. 2021;103-B(1):79–86. [DOI] [PubMed] [Google Scholar]
- 6. Morgenstern M, Kuehl R, Zalavras CG, et al. The influence of duration of infection on outcome of debridement and implant retention in fracture-related infection. Bone Joint J. 2021;103-B(2):213–221. [DOI] [PubMed] [Google Scholar]
- 7. Parvizi J, Tan TL, Goswami K, et al. The 2018 definition of periprosthetic hip and knee infection: An evidence-based and validated criteria. J Arthroplasty. 2018;33(5):1309–1314. [DOI] [PubMed] [Google Scholar]
- 8. Baertl S, Metsemakers WJ, Morgenstern M, et al. Fracture-related infection. Bone Joint Res. 2021;10(6):351–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McNally M, Sousa R, Wouthuyzen-Bakker M, et al. The EBJIS definition of periprosthetic joint infection. Bone Joint J. 2021;103-B(1):18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]


