Abstract
Study Objectives:
The aim of this study was to estimate the association between insufficient sleep and prescription opioid misuse among US high school students.
Methods:
Participants were 6,884 high school students who self-reported on sleep duration and prescription opioid misuse in the 2019 Youth Risk Behavior Survey. Sleep duration was categorized by the Youth Risk Behavior Survey according to the American Academy of Sleep Medicine guidelines as follows: recommended sleep duration (8–9 hours) vs insufficient sleep (< 8 hours). Participants also reported whether they had any prescription opioid misuse during their lifetime and whether they had prescription opioid misuse within the past 30 days.
Results:
Most (79.4%) participants reported sleeping less than 8 hours per night. Among all youth, 12.9% reported lifetime prescription opioid misuse and 6.2% reported current prescription opioid misuse. Prevalence of both lifetime and current opioid medication misuse was higher among those also reporting insufficient sleep compared to those reporting recommended sleep duration (14.3% vs 7.7%, P < .0001 for lifetime misuse and 6.6% vs 4.3%, P = .0091 for current misuse). In multivariate models, insufficient sleep was associated with an increased odds of lifetime prescription opioid misuse (adjusted odds ratios = 1.4; 95% confidence interval, 1.1–1.2; P = .006); however, we did not find an association between sleep duration and current prescription opioid misuse in multivariate analysis.
Conclusions:
Sleep duration is associated with lifetime opioid misuse among US youth. Longitudinal studies are needed to test whether causal relationships exist, and to understand biobehavioral mechanisms that underlie associations between sleep deficiency and opioid misuse in adolescents.
Citation:
Groenewald CB, Rabbitts JA, Tham SW, Law EF, Palermo TM. Associations between insufficient sleep and prescription opioid misuse among high school students in the United States. J Clin Sleep Med. 2021;17(11):2205–2214.
Keywords: insufficient sleep, adolescent, opioid misuse, high school students
BRIEF SUMMARY
Current Knowledge/Study Rationale: Insufficient sleep and the opioid epidemic are 2 public health concerns affecting adolescents in the United States, yet associations between these 2 health concerns remain poorly described. This study was performed to determine whether insufficient sleep is associated with lifetime and current prescription opioid misuse using data from a large, nationally representative study designed to measure health behaviors affecting high school students in the US.
Study Impact: Compared to students who obtained the recommended sleep duration (8–9 hours per weeknight), those with insufficient sleep (< 8 hours per weeknight) had increased rates of both lifetime (14.3% vs 7.7%, P < .0001) and past 30 days’ prescription opioid misuse (6.6% vs 4.3%, P = .0091 for current misuse).
INTRODUCTION
Obtaining adequate sleep is important for the overall health and well-being of adolescents,1 including their physical, social, and psychological health. However, up to 75% of adolescents do not obtain recommended sleep duration,2 defined as 8–10 hours of sleep per night by the American Academy of Sleep Medicine and National Sleep Foundation.3,4 Furthermore, there has been a progressive reduction in nighttime sleep duration for adolescents over the past 3 decades.5 According to the Youth Risk Behavior Survey (YRBS), the proportion of high school students who reported adequate sleep decreased from 31.1% to 25.4% from 2007 to 2017.6
Prescription opioid misuse is defined as using prescribed opioids such as oxycodone, hydrocodone, or codeine in a manner other than directed by a health care provider. This includes using opioids in greater amounts, for longer than prescribed, or from someone else’s prescription.7 The National Survey on Drug Use and Health documented 2.3% of adolescents (12–17 years) with prescription opioid misuse in 2019, a decrease from 2017 when 3.8% of adolescents reported prescription opioid misuse.8,9 Regardless of this decrease, prescription opioid misuse remains a primary driver of opioid overdose and development of opioid use disorder, contributing to an unprecedented opioid crisis currently facing adolescents in the United States.10,11 Indeed, of those adolescents who initiate heroin use, > 90% started with prescription opioid misuse.12,13
There is increasing evidence that sleep disturbance is linked to prescription opioid misuse across the lifespan, likely due to multiple biobehavioral mechanisms. Tang et al14 found higher rates of current (past month) prescription opioid misuse among a community sample of Chinese adolescents with poor sleep quality, while we recently found increased lifetime rates of prescription opioid misuse among adults who reported sleep disturbance during adolescence.15 However, no study has examined the associations between sleep duration and current and lifetime prescription opioid misuse in a nationally representative sample of adolescents from the United States. This represents an important gap in knowledge: A clearer understanding of the link between sleep and opioid misuse may lead to population-based public health interventions in the adolescent population.
Therefore, the primary aim of this study was to determine whether insufficient sleep is associated with prescription opioid misuse among high school students in a large nationally representative dataset in the United States. We hypothesized that insufficient sleep would be associated with increased prevalence rates of both lifetime prescription opioid misuse and current prescription opioid misuse (past 30 days). Further, we expected that these associations would remain significant after controlling for other known risk factors, including sociodemographic factors (age, sex, race, and ethnicity), depressive symptoms, experiencing violence, and other substance use behaviors, which have all been shown previously to affect both sleep and opioid misuse behaviors. A secondary aim of this study was to determine whether a dose-dependent relationship exists between sleep duration (hours of sleep per night) and the prevalence of opioid misuse in adolescents. Previous studies have found that the odds of other substance use behaviors (tobacco, alcohol, and marijuana) increase for each hour decrease in sleep duration; however, this relationship has not been described in the context of opioid misuse.16 With respect to youth in our sample, we hypothesized that each hour decrease in sleep duration on school nights would be associated with an incremental increase in rates of current and lifetime prescription opioid misuse in both univariate and multivariate analyses.
METHODS
Participants and procedure
For this analysis we used cross-sectional data from the 2019 YRBS. The YRBS is conducted every 2 years by the Centers for Disease Control and Prevention and is the largest public health surveillance system of adolescent health behavior risk factors in the United States. The YRBS uses a 3-stage cluster sampling design to produce nationally representative estimates of health behaviors (including self-reported sleep duration and prescription opioid misuse) of US public and private school students in grades 9–12 (high school in the US). Surveys are school-based: Parents give permission, and surveys are self-administered by participating youth at their schools during a single class period (time to complete is approximately 45 minutes). The overall response rate for 2019 YRBS was 60.3%. Additional information about YRBS is available at https://www.cdc.gov/healthyyouth/data/yrbs/index.htm.17 As data were de-identified and are publicly available, our IRB deemed this study as exempt from review.
Measures
Insufficient sleep
Our primary predictor variable of interest was insufficient sleep defined as adolescent self-report of hours of sleep on an average school night. Participants were asked, “On an average school night, how many hours of sleep do you get?” The response options were “4 or less hours,” “5 hours,” “6 hours,” “7 hours,” “8 hours,” “9 hours,” and “10 or more hours.” The YRBS then dichotomized responses, with those obtaining < 8 hours of sleep per night categorized as having insufficient sleep vs those obtaining 8 or more hours of sleep per night as having sufficient sleep. For this analysis we excluded participants who reported 10 or more hours of sleep from analyses (n = 186).17 Consequently, we defined those reporting 8–9 hours of sleep as obtaining “recommended sleep duration” vs those reporting < 8 hours of sleep as obtaining “insufficient sleep.” This categorization is based on guidelines from the American Academy of Sleep Medicine.
Prescription opioid misuse
Current prescription opioid misuse was defined as any prescription opioid medication misuse during the past 30 days.18 Adolescents were asked, “During the past 30 days, how many times have you taken prescription pain medicine without a doctor’s prescription or differently than how a doctor told you to use it?” with response options: “0 times,” “1 or 2 times,” “3 to 9 times,” “10 to 19 times,” “20 to 39 times,” and “40 or more times.” Participants were asked to include drugs such as codeine, Vicodin, OxyContin, hydrocodone, and Percocet. The YRBS then categorized those participants reporting “1 or 2 times” or more as current prescription opioid misusers.
Lifetime prescription opioid misuse was defined as any prescription opioid misuse during the teen’s lifetime. Participants were asked, “During your lifetime have you taken prescription pain medication without a doctor’s prescription or differently than how a doctor told you to use it?” with response options: “0 times,” “1 or 2 times,” “3 to 9 times,” “10 to 19 times,” “20 to 39 times,” and “40 or more times.” Participants were again asked to count drugs such as codeine, Vicodin, OxyContin, hydrocodone, and Percocet. The YRBS categorized those participants reporting “1 or 2 times” or more as lifetime prescription opioid misusers.
Covariates
We included covariates previously shown to be associated with both insufficient sleep and prescription opioid misuse, including sociodemographic factors (age, sex, race, and ethnicity),19 other substance use behaviors (tobacco, marijuana, alcohol),9 depressive symptoms,20 and a history of exposure to violence (sexual violence and/or violence at school).21
Sociodemographics
Students were asked to self-report their age, sex, race, and ethnicity (White, non-Hispanic; Black, non-Hispanic; Hispanic; Asian, non-Hispanic; American Indian/Alaska Native; Native Hawaiian/Other Pacific Islander; and multiple race).
Alcohol, tobacco, and marijuana use
Participants who reported 1 or more episodes of alcohol use over the past 30 days were coded as having current alcohol use; those who reported 1 day or more of tobacco use were coded as having current tobacco use; those reporting marijuana use more than once over the past 30 days were coded as having current marijuana use. All 3 variables were coded as binary (0 = no; 1 = yes).
Depressive symptoms
Depressive symptoms were captured as a binary (0 = no; 1 = yes) variable in response to the question “During the past 12 months, did you ever feel so sad or hopeless almost every day for 2 weeks or more in a row that you stopped doing some usual activities?”
History of violence
Participants who responded “yes” to the question “Have you ever been forced to have sexual intercourse when you did not want to?” were categorized as having a history of sexual violence. Responses of “1 time” or more to the question “During the past 12 months, how many times has someone threatened or injured you with a weapon such as a gun, knife, or club on school property?” were categorized as having a history of experiencing violence at school. Both variables were coded as binary (0 = no; 1 = yes).
Statistical analysis plan
Analyses were conducted using Stata version 14.2 (StataCorp, College Station, TX); α was set at .05, and hypothesis testing was 2-tailed. Missing data were not imputed. We adjusted for the complex sample design of YRBS by using sampling weights, regional stratification, and primary sampling unit information to provide nationally representative estimates of high school students in the United States.
We first conducted descriptive analysis to analyze the distribution of variables in the sample.
To address our primary aim, we used Pearson chi-square analysis to compare prevalence rates of both current and lifetime prescription opioid misuse between participants with recommended sleep duration (8–9 hours) relative to those with insufficient sleep (< 8 hours). For multivariate analyses, we performed multivariate logistic regression to determine the association between insufficient sleep and current and lifetime prescription opioid misuse. Our multivariate models controlled for sociodemographics (age, sex, race, and ethnicity), depressive symptoms, other substance use behaviors (tobacco, alcohol, and marijuana use), and experience of violence (history of sexual violence and violence at school).
To address our secondary aim, we first conducted univariate analyses to compare rates of both current and lifetime prescription opioid misuse by sleep duration using Pearson chi-square analysis. Then we performed multivariate logistic regression analysis to determine whether incremental sleep loss (each hour under the recommended sleep duration of 8–9 hours) was associated with increased odds of lifetime or current prescription opioid misuse after controlling for the same covariates as listed for our primary analyses.
RESULTS
Sample characteristics
Our sample included 6,884 participants. Of these, 1,414 (weighted percentage: 20.6%) reported sleeping 8 or more hours per school night, while 5,470 (79.4%) reported insufficient sleep (< 8 hours of sleep on school nights) (Table 1). Overall, 901 (weighted 12.9%) reported 1 or more episodes of prescription opioid misuse during their lifetime, while 450 (6.2%) reported 1 or more episodes of prescription opioid misuse during the past 30 days. Most adolescents self-identified as being White, non-Hispanic (54.7%), followed by 22.1% who self-identified as being multiracial; fewer identified as being Black, non-Hispanic (8.4%); Hispanic (8.9%); and Asian (5.2%). In our sample, 33.9% reported current tobacco use, 21.3% reported current marijuana use, and 29.8% reported current alcohol use. More than one-third (37.1%) reported past-year depressive symptoms. Less than 10% reported a history of sexual violence (6.8%) or physical violence (6.3%).
Table 1.
Baseline characteristics of participants in the 2019 Youth Risk Behavior Surveillance Survey with completed data on all variables.
| Total Sample (n = 6,884) | Weighted % | 95% CI | |
|---|---|---|---|
| Sleep | |||
| Sleep 8–9 h per night | 1,414 | 20.6 | (18.9–22.5) |
| Sleep < 8 h per night | 5,470 | 79.4 | (77.5–81.1) |
| Lifetime prescription opioid misuse | |||
| No | 5,983 | 87.1 | (85.2–88.7) |
| Yes | 901 | 12.9 | (11.3–14.8) |
| Current (past 30 d) prescription opioid misuse | |||
| No | 6,434 | 93.9 | (92.8–94.7) |
| Yes | 450 | 6.2 | (5.3–7.2) |
| Age (mean/standard deviation) | 6,884 | 16.0 | 1.25 |
| Sex | |||
| Male | 3,326 | 49.7 | (47.6–51.8) |
| Female | 3,558 | 50.3 | (48.2–52.4) |
| Race and ethnicity | |||
| White, non-Hispanic | 3,560 | 54.7 | (48.8–60.4) |
| Black, non-Hispanic | 769 | 8.4 | (6.3–11.1) |
| Hispanic | 572 | 8.9 | (7.0–11.4) |
| Asian | 375 | 5.2 | (2.6–10.1) |
| American Indian/Alaska Native | 47 | 0.4 | (0.3–0.7) |
| Native Hawaiian/other Pacific Islander | 25 | 0.3 | (0.2–0.5) |
| Multiple | 1,536 | 22.1 | (18.6–26.1) |
| Current tobacco use | |||
| No | 4,651 | 66.1 | (63.4–68.7) |
| Yes | 2,233 | 33.9 | (31.3–36.6) |
| Current marijuana use | |||
| No | 5,471 | 78.7 | (76.2–81.0) |
| Yes | 1,413 | 21.3 | (19.0–23.8) |
| Current alcohol use | |||
| No | 4,891 | 70.2 | (67.8–72.4) |
| Yes | 1,993 | 29.8 | (27.6–32.2) |
| Felt sad or hopeless | |||
| No | 4,295 | 62.9 | (60.9–64.8) |
| Yes | 2,589 | 37.1 | (35.2–39.1) |
| Sexual assault history | |||
| No | 6,420 | 93.2 | (92.3–94.1) |
| Yes | 464 | 6.8 | (5.9–7.7) |
| Threatened or injured with a weapon on school property | |||
| No | 6,447 | 93.7 | (92.6–94.6) |
| Yes | 437 | 6.3 | (5.4–7.4) |
CI = confidence interval.
Associations between insufficient sleep with lifetime and current prescription opioid misuse
Rates of lifetime and current prescription opioid misuse by average sleep duration on school nights are presented in Table 2. In univariate analyses, the rate of lifetime prescription opioid misuse was almost double (14.3%) among students reporting insufficient sleep on school nights as compared to those receiving the recommended sleep duration on school nights (7.7%, P < .0001). The rate of current prescription opioid misuse was 6.6% among students reporting insufficient sleep, while the rate of current opioid misuse was significantly lower (4.3%, P = .0091) among those reporting recommended sleep duration on school nights.
Table 2.
Univariate analyses comparing rates of lifetime and current prescription opioid misuse between high school students reporting insufficient sleep to those who reported 8–9 hours of sleep per night.
| Opioid Measure | Insufficient Sleep (< 8 h per night) | Recommended Sleep Duration (8–9 h per night) | P | ||
|---|---|---|---|---|---|
| Weighted % | 95% CI | Weighted % | 95% CI | ||
| Current opioid misuse | 6.6 | (5.7–7.7) | 4.3 | (3.1–6.0) | .0091 |
| Lifetime opioid misuse | 14.3 | (12.5–16.3) | 7.7 | (5.9–9.9) | < .0001 |
CI = confidence interval.
Results of multivariate analyses examining associations between current and lifetime prescription opioid misuse and average sleep duration on school nights are presented in Table 3. Similar to univariate findings, insufficient sleep was significantly associated with lifetime prescription opioid misuse (adjusted odds ratio [aOR] = 1.4; 95% confidence interval [CI], 1.1–1.2; P = .006), after controlling for covariates. In contrast to univariate findings, however, insufficient sleep was not associated with an increased risk of current prescription opioid misuse (aOR = 1.0; 95% CI, 0.7–1.4; P = .85), after controlling for covariates. Age and sex were not associated with prescription opioid misuse in either model. High school students who self-reported their race and ethnicity as Black/non-Hispanic, Hispanic, or multiracial were at increased risk for current prescription opioid misuse relative to those who self-reported as White/non-Hispanic and these associations held in multivariate analysis. In both models, current alcohol use was associated with significantly increased odds of both current and lifetime prescription opioid misuse, while current tobacco use was associated with increased odds of current use only and marijuana use was associated with lifetime use only. Those with a past-year history of depressive symptoms and of experiencing sexual assault or violence at school had increased odds for both current and lifetime prescription opioid misuse.
Table 3.
Multivariate logistic regression analysis determining associations between insufficient sleep and both lifetime and current prescription opioid misuse.
| Variables | Lifetime Prescription Opioid Misuse | Current Prescription Opioid Misuse | ||||
|---|---|---|---|---|---|---|
| aOR | 95% CI | P | aOR | 95% CI | P | |
| Sleep | ||||||
| Sleeps 8–9 h per night | Ref | Ref | ||||
| Sleeps < 8 h per night | 1.4 | (1.1–1.2) | .006 | 1.0 | (0.7–1.4) | .850 |
| Age | 1.0 | (0.9–1) | .36 | 0.9 | (0.8–1.1) | .238 |
| Sex | ||||||
| Male | Ref | Ref | ||||
| Female | 1.0 | (0.8–1.3) | .971 | 1.0 | (0.8–1.2) | .878 |
| Race and ethnicity | ||||||
| White, non-Hispanic | Ref | Ref | ||||
| Black, non-Hispanic | 1.4 | (0.9–2.0) | .116 | 1.8 | (1–3.2) | .035 |
| Hispanic | 1.0 | (0.7–1.6) | .856 | 1.9 | (1.2–3.1) | .013 |
| Asian | 1.0 | (0.6–1.5) | .928 | 1.3 | (0.8–2.3) | .322 |
| American Indian/Alaska Native | 1.5 | (0.4–5.8) | .58 | 0.6 | (0.2–2.4) | .495 |
| Native Hawaiian/other Pacific Islander | 0.6 | (0.1–3.4) | .597 | 1.7 | (0.3–9.9) | .539 |
| Multiple race | 1.3 | (0.9–1.9) | .103 | 1.8 | (1.2–2.8) | .006 |
| Current tobacco use | ||||||
| No | Ref | Ref | ||||
| Yes | 1.2 | (1–1.6) | .066 | 1.6 | (1.2–2.1) | .002 |
| Current marijuana use | ||||||
| No | Ref | Ref | ||||
| Yes | 1.9 | (1.5–2.4) | <.0001 | 1.3 | (1–1.7) | .059 |
| Current alcohol use | ||||||
| No | Ref | Ref | ||||
| Yes | 1.7 | (1.4–2.1) | <.0001 | 2.3 | (1.7–3.1) | <.0001 |
| Felt sad or hopeless | ||||||
| No | Ref | Ref | ||||
| Yes | 2.3 | (2–2.7) | <.0001 | 2.4 | (1.8–3.2) | <.0001 |
| Sexual assault history | ||||||
| No | Ref | Ref | ||||
| Yes | 2.0 | (1.4–2.9) | <.0001 | 2.0 | (1.5–2.8) | <.0001 |
| Threatened or injured with a weapon on school property | ||||||
| No | Ref | Ref | ||||
| Yes | 2.0 | (1.5–2.7) | < .0001 | 1.9 | (1.3–2.9) | .002 |
aOR = adjusted odds ratio, CI = confidence interval, Ref = reference.
Rates of lifetime and current prescription opioid misuse by hours slept
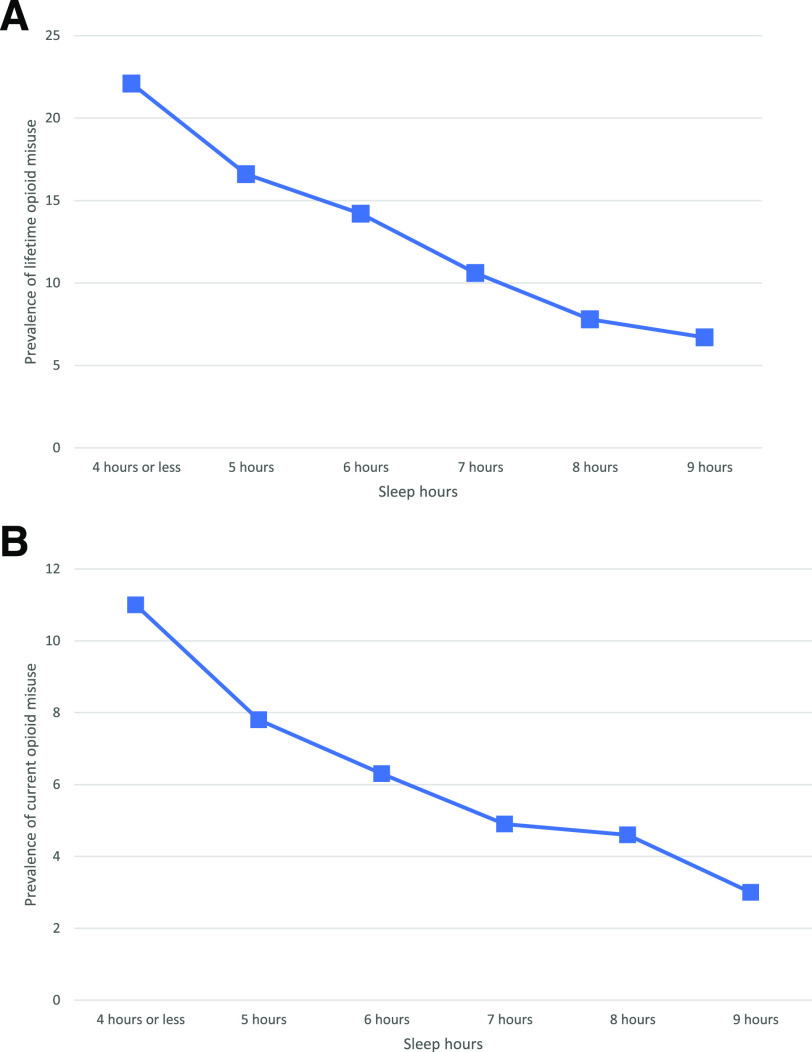
In univariate analyses, the prevalence of lifetime prescription opioid misuse varied according to sleep duration in a dose-dependent fashion (Figure 1A). Among adolescents who reported sleeping 9 hours/night on school nights, the prevalence of lifetime prescription opioid misuse was 6.7%, and this increased to 14.2% among adolescents who reported sleeping 6 hours/night on school nights, and to 22.1% among those reporting 4 or fewer hours of sleep (P < .0001). This pattern held in multivariate analysis. Specifically, the odds of lifetime prescription opioid misuse was 1.5 times greater among those sleeping 6 hours compared to those sleeping the recommended 8–9 hours (aOR = 1.5; 95% CI, 1.1–1.9; P = .008), while the odds for lifetime prescription opioid misuse was 1.8 times greater among those sleeping 4 or less hours per night relative to those reporting 8–9 hours of sleep (aOR = 1.8; 95% CI, 1.2–2.6; P = .002) (Table 4).
Figure 1. Prescription opioid misuse by reported hours slept.
(A) Prevalence of lifetime prescription opioid misuse by reported hours slept. (B) Prevalence of current prescription opioid misuse by reported hours slept.
Table 4.
Multivariate logistic regression analysis determining associations between insufficient sleep (number of hours sleep reported) and both lifetime and current prescription opioid misuse.
| Sleep Reported | Lifetime Prescription Opioid Misuse | Current Prescription Opioid Misuse | ||||
|---|---|---|---|---|---|---|
| aOR* | 95% CI | P | aOR* | 95% CI | P | |
| 8–9 h (reference) | Ref | Ref | ||||
| 7 h | 1.2 | (0.9–1.7) | .208 | 0.9 | (0.7–1.3) | .656 |
| 6 h | 1.5 | (1.1–1.9) | .008 | 1.0 | (0.7–1.5) | .966 |
| 5 h | 1.5 | (1.1–2.1) | .016 | 1.1 | (0.7–1.5) | .787 |
| 4 h or less | 1.8 | (1.2–2.6) | .002 | 1.3 | (0.8–2.3) | .301 |
*Adjusted for age, sex, race, and ethnicity; current tobacco use; current marijuana use; current alcohol use; depressive symptoms; sexual assault; and being threatened with a weapon. aOR = adjusted odds ratio, CI = confidence interval.
The prevalence of current prescription opioid misuse in univariate analyses also increased as sleep hours decreased (Figure 1B). The prevalence of current prescription opioid misuse was 3% among students reporting 9 hours of sleep and increased to 11% among those reporting 4 or less hours of sleep (P = .002). However, in multivariate analysis this association was not observed; incremental sleep loss was not associated with an increased odds of current opioid misuse after controlling for covariates.
DISCUSSION
Using a nationally representative sample of high school students in the United States, we found that high school students with insufficient sleep on school nights (less than 8 hours of sleep per night) reported higher rates of both lifetime prescription opioid misuse and current prescription opioid misuse, relative to those who obtained the recommended 8–9 hours of sleep duration per school night. In partial support of our hypothesis, the association between insufficient sleep and lifetime prescription opioid misuse remained significant after controlling for demographic, behavioral, and psychological covariates in multivariate analyses. However, in contrast to our expectation, we did not detect a significant association between insufficient sleep and current prescription opioid misuse in our multivariate model. We also examined whether there was a dose-response relationship between sleep duration and rates of opioid misuse. As expected, we found that a sequential reduction in average hours slept on school nights was associated with an incremental increase in the rates of both current and lifetime prescription opioid misuse in univariate analyses, and this association remained significant when we examined lifetime opioid misuse in multivariate analyses. However, contrary to our hypothesis, we did not detect significant associations between sleep duration and current prescription opioid misuse after controlling for relevant covariates in multivariate analysis. These findings add to our limited understanding of associations between sleep deficiency and prescription opioid misuse in young people.
Indeed, in a previous study we found that adolescent sleep disturbances (including chronic insufficient sleep, chronic unrestful sleep, and insomnia symptoms), but not self-reported sleep duration, were prospectively associated with the development of prescription opioid misuse in young adulthood using a sample from the National Longitudinal Study of Adolescent to Adult Health.15 Tang et al14 found increased rates of prescription opioid misuse use among a community sample of Chinese adolescents with poor sleep quality (as measured using the Chinese Pittsburgh Sleep Quality Index) in a cross-sectional analysis. Our study extends these findings to show associations between sleep duration and prescription opioid misuse in a large, nationally representative sample of high school students. Given our findings and the existing literature, it appears that multiple aspects of sleep disturbance, including quantity and quality of sleep, may be associated with prescription opioid misuse in adolescence.
Adolescence has been identified as “the perfect storm” for the development and maintenance of sleep disturbances due to developmental changes in biological circadian rhythms (ie, sleep timing shifting to later in the evening) as well as behavioral and environmental factors unique to this age group that decrease opportunity for nighttime sleep (eg, homework load, evening activities for sports/clubs, early school start times, use of electronics and social media after bedtime, and decreased monitoring and supervision from adults at night).22 Adolescence is also a high-risk period for initiating prescription opioid misuse23 and contributors to this risk are multifactorial. For example, adolescent brain development is characterized by unequal maturation, with brain reward and pleasure-seeking centers maturing rapidly, while the prefrontal cortex, involved in executive function, only matures in adulthood.24,25 This unequal maturation can increase propensity for risk-taking behaviors as well as vulnerability to the positive reinforcing effects of opioids and other substances.26 There are also behavioral risk factors that are shared between sleep disturbances and opioid misuse that arise or are already established during adolescence, including mental health conditions,20,27 history of adverse childhood experiences,21,28 and other substance use.9,29 Given the known negative outcomes associated with sleep disturbances and opioid misuse for adolescents, understanding these associations may help inform policy and clinical practice targeting improved individual health and public health.
To date, potential mechanisms underlying the sleep-opioid relationship in youth have been largely unexplored. Research on the sleep-opioid relationship in adults has focused on long-term opioid therapy among individuals with chronic pain conditions. Sleep disturbances are known to reduce pain thresholds,30 and self-treatment of pain is the most commonly reported motivating factor for adolescent prescription opioid misuse.19 Adolescents may also misuse prescription opioids in order to facilitate sleep.31,32 A bidirectional, cyclical association is also possible, where opioid use causes sleep disturbance that subsequently triggers ongoing or increased opioid use in order to facilitate sleep and prevent withdrawal.33 While research in adolescents is scarce, long-term opioid therapy is known to disrupt sleep architecture, reduce sleep efficiency, decrease sleep quality, and increase daytime sleepiness among adults with chronic pain.34,35 Opioid use can also cause respiratory depression and contribute to the onset or exacerbation of sleep-related breathing disorders.36 Recently, the American Academy of Sleep Medicine released a position statement highlighting the potential adverse effects of opioid therapy on sleep in adults.37 However, similar guidance does not exist for adolescents.
Among covariates examined, we found that Black, non-Hispanic high school students reported increased rates of current prescription opioid misuse relative to White, non-Hispanic students. Historically, White, non-Hispanic adolescents have reported increased rates of opioid misuse relative to minority populations; however, other studies have found that this trend has reversed over the past few years.8 Our findings are consistent with recent data from the National Survey on Drug Use and Health and the Monitoring the Future survey, both of which now show that Black, non-Hispanic youth are at increased risk of prescription opioid misuse relative to other population groups.19,38 We also found a strong association between depressive symptoms (feeling sad or hopeless) and both lifetime and current prescription opioid misuse. Depressive symptoms are strongly correlated with both sleep disturbance and opioid misuse39 among youth, reflecting overlapping neurobiology between these conditions.40 We therefore included depressive symptoms as a covariate in multivariate analysis. However, we found that insufficient sleep is associated with lifetime prescription opioid misuse independently of depressive symptoms.
Our study also found a dose-response relationship between lifetime opioid misuse and hours of sleep on school nights, where the prevalence of lifetime opioid misuse increased as sleep duration decreased. This pattern was not replicated when we examined current opioid misuse. A prior study also found increased odds of substance use (tobacco, alcohol, and marijuana) for each hour of sleep lost in a community sample of adolescents from Fairfax County, VA.16 To our knowledge, this study is the first to demonstrate a similar dose-response relationship for lifetime opioid misuse.
It is important to point out that we did not find an association between insufficient sleep and current prescription opioid misuse in multivariate analysis. This negative finding should not necessarily be interpreted as a lack of association: It is possible that no association exists; however, it is also possible that the sample size was not large enough to detect an association (lack of power). One possible reason for finding no association between sleep and current opioid misuse is related to changes in prescription opioid misuse rates among youth in the United States over time. Rates of prescription opioid misuse declined between 2010–20198,9 in response to greater awareness of the opioid crisis and reduced opioid prescribing to youth.41 This decline in opioid misuse may have resulted in weaker associations between sleep and current opioid use in our sample due to lack of power. We should also keep in mind that 2019 was the first year during which YRBS surveyed youth about current prescription opioid misuse behaviors. It is possible that associations between sleep duration and current opioid misuse will emerge once larger samples sizes from future years of YRBS are combined (eg, combining 2019 and 2021 data). Although reductions in prescription opioid misuse among adolescents are promising, it is still very important to clarify the association between sleep and opioid misuse, as rates of opioid-related overdose deaths among adolescents have continued to escalate significantly over time.10
This study has several limitations that should be considered. First, the cross-sectional design limited our ability to draw a cause-effect relationship between sleep and opioid misuse. Longitudinal data are needed to understand the potential causal relationships to better understand how sleep deprivation leads to subsequent opioid misuse. Second, both sleep and opioid misuse were measured using single items. Sleep is a complex phenomenon that includes other dimensions, such as sleep quality, efficiency, architecture, and disturbance. Future studies should include assessment of multiple aspects of sleep, in addition to duration, and consider objective measurements using actigraphy or polysomnography. Third, when interpreting results from our study, it is important to recognize that the rates of prescription opioid misuse reported in our sample are not directly comparable to other, large nationally representative surveys (eg, the National Survey on Drug Use and Health and the Monitoring the Future study9,42) due to differences in sampling procedures and survey methodology. The YRBS asked about prescription pain medication misuse, which could consist of both opioids and nonopioids (acetaminophen, nonsteroidal anti-inflammatory medications, and the gabapentinoids). However, the question provides examples of opioid or opioid-combination prescription medications only.18 Although unlikely in this community sample, it is possible that some participants reported on misuse of nonopioid pain medication, which could have inflated rates of prescription opioid misuse and led to differences between the rates of opioid misuse identified in our study compared to published data from other nationally representative surveys. Finally, the YRBS does not assess chronic pain or chronic health conditions, and therefore it is unknown if the survey participants were using opioid medication for chronic pain.
Despite these limitations, our study has several strengths that should also be considered when interpreting the data. Specific to the US adolescent population, the YRBS is the largest risk surveillance system in the United States to survey both sleep and current prescription opioid misuse. Other large databases, such as the National Survey on Drug Use and Health and Monitoring the Future, do not ask participants about sleep duration. Furthermore, using the YRBS allowed us to control for other risk factors in our analysis, allowing us to isolate the specific risk associated with insufficient sleep.
From a population health perspective, our findings, although speculative, suggest that targeting sleep has a role in reducing the impact of the opioid epidemic on adolescents. Furthermore, our findings confirm that during health care visits all adolescents, especially those with sleep disturbance, should be for screened for prescription opioid misuse using validated screening tools such as the Brief Screener for Tobacco, Alcohol, and other Drugs.43 Adolescent sleep disturbances may be targeted via community and/or school-based strategies, or at the individual level. Efforts to delay school start times of adolescents have been ongoing for the last decade, and education on the importance of sleep also has been promoted to a broader audience.22
From a research perspective, there is a clear need to consider insufficient sleep in future studies aimed at understanding the development of prescription opioid misuse behaviors. Longitudinal research is needed to test whether causal relationships exist, and to understand potential mechanisms linking sleep deficiency and opioid misuse in adolescents. Ideally, studies should follow youth after a first opioid prescription, for example after surgery, and assess multiple aspects of sleep, including objective measurements of sleep using actigraphy and polysomnography.
In conclusion, we found that insufficient sleep was independently associated with prescription opioid misuse in a nationally representative sample participating in the Youth Risk Behavior Survey. Insufficient sleep and the opioid epidemic are major public health concerns that have affected the adolescent population over the past 20 years. Given the significant impact of the opioid epidemic on public health in the United States, it is urgent that the role of sleep be elucidated.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. Dr. Groenewald was supported by grant K23HL138155 from the National Heart, Lung, and Blood Institute. Dr. Tham was supported by grant K23DK118111 from the National Institute of Diabetes and Digestive and Kidney Diseases. Dr. Law was supported by grant K23NS089966 from the National Institute of Neurologic Disorders and Stroke. This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by, the NIH. The authors report no conflicts of interest.
ABBREVIATIONS
- aOR,
adjusted odds ratio
- CI,
confidence interval
- YRBS,
Youth Risk Behavior Survey
REFERENCES
- 1. Smaldone A, Honig JC, Byrne MW . Sleepless in America: inadequate sleep and relationships to health and well-being of our nation’s children . Pediatrics. 2007. ; 119 ( Suppl 1 ): S29 – S37. [DOI] [PubMed] [Google Scholar]
- 2. Baiden P, Tadeo SK, Peters KE . The association between excessive screen-time behaviors and insufficient sleep among adolescents: findings from the 2017 youth risk behavior surveillance system . Psychiatry Res. 2019. ; 281 : 112586. [DOI] [PubMed] [Google Scholar]
- 3. Paruthi S, Brooks LJ, D’Ambrosio C, et al . Consensus statement of the American Academy of Sleep Medicine on the recommended amount of sleep for healthy children: methodology and discussion . J Clin Sleep Med. 2016. ; 12 ( 11 ): 1549 – 1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hirshkowitz M, Whiton K, Albert SM, et al . National Sleep Foundation’s sleep time duration recommendations: methodology and results summary . Sleep Health. 2015. ; 1 ( 1 ): 40 – 43. [DOI] [PubMed] [Google Scholar]
- 5. Keyes KM, Maslowsky J, Hamilton A, Schulenberg J . The great sleep recession: changes in sleep duration among US adolescents, 1991-2012 . Pediatrics. 2015. ; 135 ( 3 ): 460 – 468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kann L, McManus T, Harris WA, et al . Youth risk behavior surveillance—United States, 2017 . MMWR Surveill Summ. 2018. ; 67 ( 8 ): 1 – 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Centers for Disease Control and Prevention . Opioid basics. Commonly used terms. https://www.cdc.gov/drugoverdose/opioids/terms.html . Accessed December 17, 2020.
- 8. Vaughn MG, Nelson EJ, Salas-Wright CP, Qian Z, Schootman M . Racial and ethnic trends and correlates of non-medical use of prescription opioids among adolescents in the United States 2004-2013 . J Psychiatr Res. 2016. ; 73 : 17 – 24. [DOI] [PubMed] [Google Scholar]
- 9. McCabe SE, Wilens TE, Boyd CJ, Chua KP, Voepel-Lewis T, Schepis TS . Age-specific risk of substance use disorders associated with controlled medication use and misuse subtypes in the United States . Addict Behav. 2019. ; 90 : 285 – 293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gaither JR, Shabanova V, Leventhal JM . US national trends in pediatric deaths from prescription and illicit opioids, 1999-2016 . JAMA Netw Open. 2018. ; 1 ( 8 ): e186558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. McCabe SE, Veliz P, Schulenberg JE . Adolescent context of exposure to prescription opioids and substance use disorder symptoms at age 35: a national longitudinal study . Pain. 2016. ; 157 ( 10 ): 2173 – 2178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McCabe SE, Boyd CJ, Evans-Polce RJ, McCabe VV, Schulenberg JE, Veliz PT . Pills to powder: a 17-year transition from prescription opioids to heroin among US adolescents followed into adulthood . J Addict Med. 2020. ; 15 ( 3 ): 241 – 244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kelley-Quon LI, Cho J, Strong DR, et al . Association of nonmedical prescription opioid use with subsequent heroin use initiation in adolescents . JAMA Pediatr. 2019. ; 173 ( 9 ): e191750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tang D, Li P, Guo L, et al . The prevalences of and association between nonmedical prescription opioid use and poor sleep among Chinese high school students . Sci Rep. 2016. ; 6 ( 1 ): 30411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Groenewald CB, Law EF, Rabbitts JA, Palermo TM . Associations between adolescent sleep deficiency and prescription opioid misuse in adulthood . Sleep. 2020. ; 44 ( 3 ): zsaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Winsler A, Deutsch A, Vorona RD, Payne PA, Szklo-Coxe M . Sleepless in Fairfax: the difference one more hour of sleep can make for teen hopelessness, suicidal ideation, and substance use . J Youth Adolesc. 2015. ; 44 : 362 – 378. [DOI] [PubMed] [Google Scholar]
- 17. Centers for Disease Control and Prevention . Youth Risk Behavior Surveillance System (YRBSS). 2019 YRBS Results and Data Available Now. https://www.cdc.gov/healthyyouth/data/yrbs/index.htm. Accessed June 24, 2021.
- 18. Jones CM, Clayton HB, Deputy NP, et al . Prescription opioid misuse and use of alcohol and other substances among high school students—Youth Risk Behavior Survey, United States, 2019 . MMWR Suppl. 2020. ; 69 ( 1 ): 38 – 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Groenewald CB, Patel KV, Rabbitts JA, Palermo TM . Correlates and motivations of prescription opioid use among adolescents 12 to 17 years of age in the United States . Pain. 2020. ; 161 ( 4 ): 742 – 748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Quinn PD, Hur K, Chang Z, et al . Association of mental health conditions and treatments with long-term opioid analgesic receipt among adolescents . JAMA Pediatr. 2018. ; 172 ( 5 ): 423 – 430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Quinn K, Boone L, Scheidell JD, et al . The relationships of childhood trauma and adulthood prescription pain reliever misuse and injection drug use . Drug Alcohol Depend. 2016. ; 169 : 190 – 198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Adolescent Sleep Working Group , Committee on Adolescence, and Council on School Health . School start times for adolescents . Pediatrics. 2014. ; 134 ( 3 ): 642 – 649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Groenewald CB, Law EF, Fisher E, Beals-Erickson SE, Palermo TM . Associations between adolescent chronic pain and prescription opioid misuse in adulthood . J Pain. 2019. ; 20 ( 1 ): 28 – 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Spear LP . The adolescent brain and age-related behavioral manifestations . Neurosci Biobehav Rev. 2000. ; 24 ( 4 ): 417 – 463. [DOI] [PubMed] [Google Scholar]
- 25. Gogtay N, Giedd JN, Lusk L, et al . Dynamic mapping of human cortical development during childhood through early adulthood . Proc Natl Acad Sci USA. 2004. ; 101 ( 21 ): 8174 – 8179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Steinberg L . Risk taking in adolescence: new perspectives from brain and behavioral science . Curr Dir Psychol Sci. 2007. ; 16 ( 2 ): 55 – 59. [Google Scholar]
- 27. Alfano CA, Zakem AH, Costa NM, Taylor LK, Weems CF . Sleep problems and their relation to cognitive factors, anxiety, and depressive symptoms in children and adolescents . Depress Anxiety. 2009. ; 26 ( 6 ): 503 – 512 . [DOI] [PubMed] [Google Scholar]
- 28. Rojo-Wissar DM, Davidson RD, Beck CJ, Kobayashi US, VanBlargan AC, Haynes PL . Sleep quality and perceived health in college undergraduates with adverse childhood experiences . Sleep Health. 2019. ; 5 ( 2 ): 187 – 192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Logan RW, Hasler BP, Forbes EE, et al . Impact of sleep and circadian rhythms on addiction vulnerability in adolescents . Biol Psychiatry. 2018. ; 83 ( 12 ): 987 – 996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Finan PH, Goodin BR, Smith MT . The association of sleep and pain: an update and a path forward . J Pain. 2013. ; 14 ( 12 ): 1539 – 1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. McCabe SE, West BT, Boyd CJ . Motives for medical misuse of prescription opioids among adolescents . J Pain. 2013. ; 14 ( 10 ): 1208 – 1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. McCabe SE, Cranford JA, Boyd CJ, Teter CJ . Motives, diversion and routes of administration associated with nonmedical use of prescription opioids . Addict Behav. 2007. ; 32 ( 3 ): 562 – 575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Eacret D, Veasey SC, Blendy JA . Bidirectional relationship between opioids and disrupted sleep: putative mechanisms . Mol Pharmacol. 2020. ; 98 ( 4 ): 445 – 453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Xiao L, Tang YL, Smith AK, et al . Nocturnal sleep architecture disturbances in early methadone treatment patients . Psychiatry Res. 2010. ; 179 ( 1 ): 91 – 95. [DOI] [PubMed] [Google Scholar]
- 35. Cao M, Javaheri S . Effects of chronic opioid use on sleep and wake . Sleep Med Clin. 2018. ; 13 ( 2 ): 271 – 281. [DOI] [PubMed] [Google Scholar]
- 36. Teichtahl H, Prodromidis A, Miller B, Cherry G, Kronborg I . Sleep-disordered breathing in stable methadone programme patients: a pilot study . Addiction. 2001. ; 96 ( 3 ): 395 – 403. [DOI] [PubMed] [Google Scholar]
- 37. Rosen IM, Aurora RN, Kirsch DB, et al. ; American Academy of Sleep Medicine Board of Directors . Chronic opioid therapy and sleep: an American Academy of Sleep Medicine position statement . J Clin Sleep Med. 2019. ; 15 ( 11 ): 1671 – 1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. McCabe SE, West BT, Veliz P, McCabe VV, Stoddard SA, Boyd CJ . Trends in medical and nonmedical use of prescription opioids among US adolescents: 1976–2015 . Pediatrics. 2017. ; 139 ( 4 ): e20162387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Edlund MJ, Forman-Hoffman VL, Winder CR, et al . Opioid abuse and depression in adolescents: results from the National Survey on Drug Use and Health . Drug Alcohol Depend. 2015. ; 152 : 131 – 138. [DOI] [PubMed] [Google Scholar]
- 40. Benca RM, Peterson MJ . Insomnia and depression . Sleep Med. 2008. ; 9 ( Suppl 1 ): S3 – S9. [DOI] [PubMed] [Google Scholar]
- 41. Gagne JJ, He M, Bateman BT . Trends in opioid prescription in children and adolescents in a commercially insured population in the United States, 2004–2017 . JAMA Pediatr. 2019. ; 173 ( 1 ): 98 – 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. McCabe SE, Schulenberg J, McCabe VV, Veliz PT . Medical use and misuse of prescription opioids in US 12th-grade youth: school-level correlates . Pediatrics. 2020. ; 146 ( 4 ): e20200387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. National Institute on Drug Abuse . Screening tools for adolescent substance use. https://www.drugabuse.gov/nidamed-medical-health-professionals/screening-tools-resources/screening-tools-for-adolescent-substance-use . Accessed March 5, 2021.