Abstract
Objective:
Many breast cancer patients are vulnerable to poor nutritional status and may benefit from nutrition education, but existing materials are not generally tailored to the needs of low-literacy immigrant and minority patients.
Methods:
With nutritionist guidance, we developed a nutrition presentation for breast cancer patients. English- (n=29) and Spanish-speaking (n=19) patients were recruited from 5 safety-net hospitals, an academic cancer center, and a Latina cancer support organization. Materials were tested using multiple rounds of cognitive interviewing (with an adapted USDA interview guide), followed by study team reviews and modifications, until saturation.
Results:
Seven rounds of interviews per language were needed. Approximately 25% of interviewees had less than a high school education. Changes included adapting to regional lexicons and resolving vague/confusing phrasing. Specific food examples needed cultural tailoring. Text color coding (red/bad, green/good) was requested. Labeled images enhanced participants’ understanding of concepts. Spanish speakers expressed a desire to understand nutrition labelling, and this was emphasized in the Spanish slides.
Conclusion:
Cognitive interviews were an important tool for creating a nutrition curriculum tailored to the needs of low-literacy, mostly immigrant patients.
Practice Implications:
Cultural and linguistic factors should be considered for nutritional education materials in diverse patient populations.
1. INTRODUCTION
Breast cancer is the most common cancer to affect women in the US and throughout the world [1, 2]. Nutrition is a salient component of breast cancer treatment, recovery, and quality of life. Unfortunately, many cancer patients are vulnerable to poor nutritional status because of the disease and its treatment side-effects, such as nausea and vomiting [3, 4]. In the increasingly diverse populations of the US and many other Western countries [5–7], such as Canada, Australia, and European countries, and with the increasing costs of cancer treatment [8], nutrition education tailored to participants’ linguistic, cultural, and socioeconomic needs is vitally important.
Forty percent of US households are of a racial/ethnic minority background [6], and over five million (4.4%) are limited English proficient (LEP), meaning that they report speaking English less than “very well” [5]. Major metropolitan areas, such as New York, Los Angeles, and Miami account for 64% of the nation’s immigrant and 94% of the nation’s LEP population [9, 10].
In New York City, over six hundred languages are spoken [11] among the city’s 3 million immigrants [12], and 25% of households are LEP [12]. Minorities represent 95% of NYC’s safety net hospital system patients [13]. There are cultural and structural barriers to implementing healthy eating in low income immigrant communities. In a focus group study with 127 Somali, Mexican, Cambodian, and Sudanese immigrants, participants thought that time and financial constraints, and a desire to “Americanize,” promoted the prevalence of unhealthy eating practices, such as eating fast and processed foods [14].
Among NYC cancer patients treated in safety net clinics, 56% were found to have low/very low food security, lacking access to enough food to be active and healthy [15, 16]. To address food insecurity among cancer patients, we established FOOD (Food to Overcome Outcomes Disparities), a network of medically tailored food pantries and other food support programs that are co-located in NYC safety net and academic cancer centers [17]. Seventy-nine percent of FOOD pantry patients are immigrants, 41% are LEP, and 24% prefer speaking Spanish [17, 18]. Having less money for food since treatment began has been associated with food insecurity among underserved cancer patients [15], who are vulnerable to cancer-related job loss and may experience reduced income or income cessation coupled with high treatment-related expenses following a cancer diagnosis [8].
A lack of nutrition literacy, defined as the capacity to “obtain, process, and understand nutrition information” and the skill to make good nutrition decisions [19], can be a barrier to healthier eating among breast cancer survivors [20]. FOOD patients frequently request nutrition counselling, but we found that existing resources did not fit the needs of this diverse low-income patient population, suggesting a need for linguistically and culturally tailored nutrition education. While tailored approaches have proven to be effective in nutrition education interventions with immigrant and minority families [21, 22], there is a dearth of evidence-based culturally and linguistically responsive health education programs and materials [23].
Minimizing text and maximizing images helps with messaging and recall with nutrition education materials among people with low health literacy [24–27]. Shilts et al adapted the United States Department of Agriculture (USDA) MyPlate representations of dietary guidelines for low-income patients of multiple cultural backgrounds and with low health literacy [26]. Color photograph adaptations of MyPlate images with culturally relevant foods gave concrete representation to abstract MyPlate images [26]. Participants overwhelmingly reported successfully implementing and getting ideas from the adapted MyPlate representations [26].
Developing linguistically responsive interventions can be complicated by the language heterogeneity of participants. The Spanish language varies according to the speaker’s country and region of origin, which could be in the Caribbean, Central or South America, or Spain [28], and words for food items vary widely [29]. Similarly, many native and non-native English speakers use a dialect rather than standard American English, depending on their region of origin and post-migration linguistic influences [30].
Cancer patients often feel motivated to make dietary changes to improve their health, but many lack the knowledge to make sustained nutrition changes [3, 20]. To meet the needs of our diverse breast cancer patient community, we developed patient nutrition education materials in English and Spanish, to be used in an individual nutrition education session in the clinical setting. Cognitive interviews are an essential tool in evaluating and developing nutrition education materials with low income populations [31]. Cognitive interviewing was used with breast cancer patients to tailor the curriculum to their needs.
2. METHODS
To test the comprehensibility of nutrition education materials, cognitive interviews were conducted with breast cancer patients at a supportive care organization for Latinas with cancer, at 5 NYC safety-net hospitals, and at an academic cancer center, all of which participate in the Integrated Cancer Care Access Network (ICCAN) [15], which addresses non-medical needs of cancer patients, including emergency food assistance.
An English-language nutrition education slide deck was developed and translated into Spanish by our bilingual certified translator team.
The nutrition education materials consisted of approximately 47 slides that covered the following modules on nutrition during breast cancer treatment: nutrition recommendations, food groups, recommended portion sizes, healthy eating tips, managing treatment side-effects, healthy food resources, food safety, and stretching the food dollar. The materials were adapted from the USDA MyPlate recommendations for various food groups [33], the God’s Love We Deliver Guide on Nutrition Tips for Breast Cancer Patients [34], and USDA Tips on How to Stretch the Food Dollar [35], and were vetted by a nutritionist before being administered to patients for feedback.
Seven rounds of cognitive interviews were conducted for the English and Spanish materials. Interviews were conducted from November 2018 to April 2019, using a cognitive interview guide that we adapted from the USDA nutrition education interview guide (Appendix A) [32]. During the pre-interview introduction, participants were told the interview purpose, that all feedback was welcome, and that their feedback would not offend the researchers. To avoid interviewer bias, think-aloud techniques (e.g., “What thoughts came to mind while looking/reading…?”) were used to elicit open-ended responses, and verbal probing (e.g., “What do you think about the pictures we used?”, “What could be changed to make the material easier to understand?”) was used whenever the participant provided limited responses. During the interviews, researchers read the slides verbatim, and then asked for a teach back, to assess comprehension. Participants were asked to provide feedback on graphs, pictures, layout, language, and content. Participants were also encouraged to suggest alternative wording and were asked to define words from the slides to help address regional language. Additionally, comprehension/interpretation probing was conducted (e.g., “Any words you did not understand?”, “What word would you use instead?”, “Is there another word that would make more sense?”). Cognitive interviews were conducted in each participant’s preferred language (English or Spanish), using slides in their language. Interviews were conducted in rounds until we reached data saturation, and patient feedback informed modifications to the materials between rounds, in an iterative process.
In between interview rounds, the researchers compared respondents’ answers, identified recurrent themes to address problematic items, and then revised the items. Three to five patients participated in each round. Revised items were tested in the next interview round. English and Spanish materials were revised separately by bilingual certified translator staff. The final educational materials reflected the patients’ feedback.
3. RESULTS
Forty-eight women with breast cancer from 19 countries participated. Twenty-nine participated in English cognitive interviews and nineteen in Spanish.
Of the 29 patients who preferred using English in the healthcare setting, 3 were from the US, and the others were from 12 other countries, including Guyana (31%), Jamaica (15%), and Grenada (8%); the average length of time spent in the US was 18 years (16.6 SDs) (Table 1).Approximately one-fourth (24%) had not graduated from high school, including 2 (7% of the total) who had only some elementary school education and 2 (7% of the total) who had only some middle school education; less than one fifth (17%) were college graduates. About three-fourths (76%) were food insecure. Country of origin and education level are not reported for 2 and 3 English speakers, respectively.
Table 1.
Demographic characteristics for English and Spanish speakers
| Characteristics | Categories | Spanish Speakers n=19, no. (%) | English Speakers n=29, no. (%) |
|---|---|---|---|
|
| |||
| Food Insecurity | |||
| Food insecure | 11 (58) | 22 (76) | |
| Food secure | 5 (26) | 6 (21) | |
|
| |||
|
Education Level
a
|
|||
| Some elementary school | 1 (5) | 2 (7) | |
| Some middle school | 2 (11) | 2 (7) | |
| Some high school | 2 (11) | 3 (10) | |
| High school graduate or some college | 7 (37) | 14 (48) | |
| College graduate or more Missing | 4 (21) 3 (16) |
5 (17) 3 (10) |
|
|
| |||
| Born in US | |||
| Yes | 0 (0) | 3 (10) d | |
| No | 19 (100) c | 24 (83)e | |
|
| |||
| Time in US, y (mean, SD) b | |||
| 15 (11.5) | 18 (16.6) | ||
| Age, y (mean, SD) | |||
| 54 (8.3) | 55 (9.0) | ||
Missing data for 3 English speakers (10%) and for 3 Spanish speakers (16%)
Missing data for 5 English speakers (17%) and for 3 Spanish speakers (16%)
Birthplaces of Spanish speakers: Central America 6 (32%), Caribbean 9 (47%), South America 4 (21%)
Missing data for 2 English speakers (7%)
Birthplaces of foreign-born English speakers: Caribbean 12 (50%), South America 8 (33%), West Africa 2 (8%), Asia 1 (4%), Central America 1 (4%)
The 19 Spanish-preferring patients were from 8 countries, including the Dominican Republic (32%), Ecuador (16%), Puerto Rico (16%), El Salvador (11%), and Mexico (11%). The average time spent in the US was about 15 years (11.5 SDs). Slightly more than one fourth (26%) had not graduated from high school, including 1 who had finished only some elementary school, and 2 who had finished only some middle school; just over one fifth (21%) were college graduates. More than half (58%) were food insecure. Education level and time in the U.S. are not reported for 3 Spanish speakers.
Our interviews demonstrated the need to tailor the Spanish and English educational materials for the study population, including accounting for regional lexicon, vague/confusing phrasing, literacy/need for plain language, nutrition terminology, unfamiliar food items, layout, and visuals. These were grouped into three key themes in our analysis: language, food knowledge, and formatting.
Language
The language of the materials was not always appropriate for our English- and Spanish-speaking patients due to regional lexicon and vague/confusing phrasing (detailed examples are shown in the Appendix B).
Regional Lexicon
Our original text contained numerous words with which patients were unfamiliar or which were not understood as intended due to their regionalized use. For example, in the English presentation, patients were not familiar with the term “leftovers.” Patients recommended “food cooked yesterday” instead of “leftovers”. Similarly, the Spanish materials had to account for regional Spanish vocabulary, particularly in the domain of food items. For example, our Spanish materials initially employed the word “guisantes” (green peas), which is primarily used in Spain and was either unfamiliar to our Latin American patients or was understood to mean “meat” or “stew.” These patients preferred the regional words “alverjas.” and “chicharros,” so these words were also provided (revised text: “guisantes [alverjas, chicharros]”). We could not find a Spanish word for “snack” that did not cause confusion, so we retained the English word,“ which most Spanish speakers understood.
Vague/Confusing Phrasing
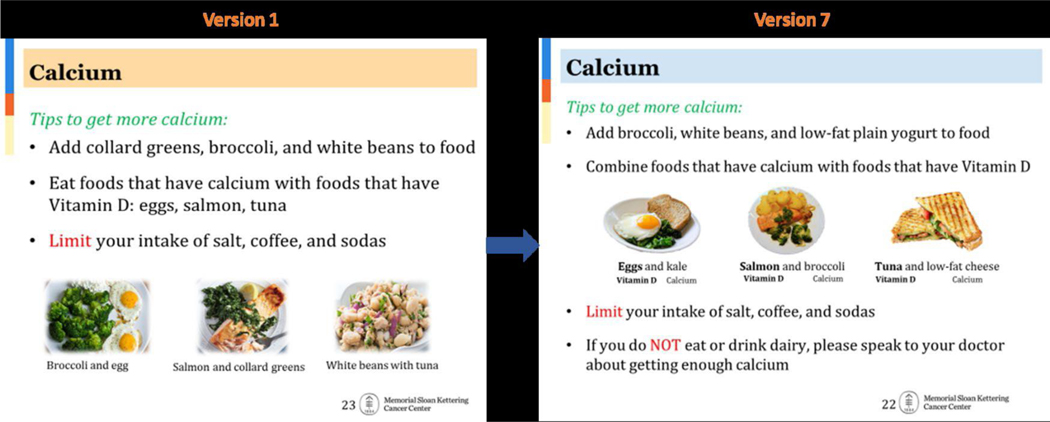
Patients found some information to be vague or unclear. In the English version, for example, patients had difficulty understanding the advice to consume vitamin D-rich foods to aid calcium absorption. Patients suggested rephrasing the text and adding illustrated examples for emphasis (Figure 1). In the Spanish version, patients also had difficulty understanding the phrasing of the text. For example, the iron slide initially read to eat iron-rich vegetables with vitamin C-rich foods (for example, spinach with orange juice). They suggested using the word “absorber” (absorb) and providing a more common food pairing (e.g., spinach with lemon juice or red bell pepper) as an example to clarify the concept, given patients did not think vegetables and fruits were ideal pairs.
Figure 1.
Original (A) versus modified (B) English calcium slides
Literacy/Need for Plain Language
We aimed to use accessible vocabulary for LEP patients and were largely successful. However, some terms caused confusion, such as “tolerate” and “found in.” To promote clarity, “tolerate treatment” was changed to “deal with cancer treatment.” Additionally, in the calcium slide, we originally wrote “Calcium is found in milk, yogurt, cheese,” but modified this to “Examples to choose from,” followed by a list.
Food Knowledge
Nutrition Terminology
Patients sometimes suggested replacing complex or unfamiliar terminology with simpler or more familiar terms and/or illustrations. For example, a few patients preferred the term “junk food” over “store-bought baked goods” and the term “low-fat meats” over “lean meat” in both the English and Spanish versions. Word replacements, examples, and labeled pictures were employed to increase comprehension in these instances. Spanish-speaking patients recommended adding “sal” (salt) next to sodium and explicitly writing “esto es sal” (this is salt)
Unfamiliarity with food items
Knowledge of specific foods also needed to be addressed in the nutrition materials. Patients were either not familiar with the food items or expressed not using the suggested foods. The unfamiliar items were replaced with items that patients suggested. Some previously unfamiliar healthy food options were preserved due to their nutrition value and our patients’ willingness to try new healthy food options.
In the Spanish version, the food items that were not found in patients’ countries of origin had no direct/universal translation, e.g., collard greens, kale, cracker, pretzel, and hummus. Per patients’ requests, pictures of unfamiliar food items were added to ease comprehension and allow patients to familiarize themselves with the items in case they wanted to use them in the future.
Formatting
Layout
We found that the layout of slide content could affect patients’ understanding. Consequently, several aspects of slide layout were adjusted, such as the flow of the information, the addition of emphasis, and placement/labeling of pictures. Patients found text challenging to read when there was a picture in the background, so clear backgrounds were used throughout.
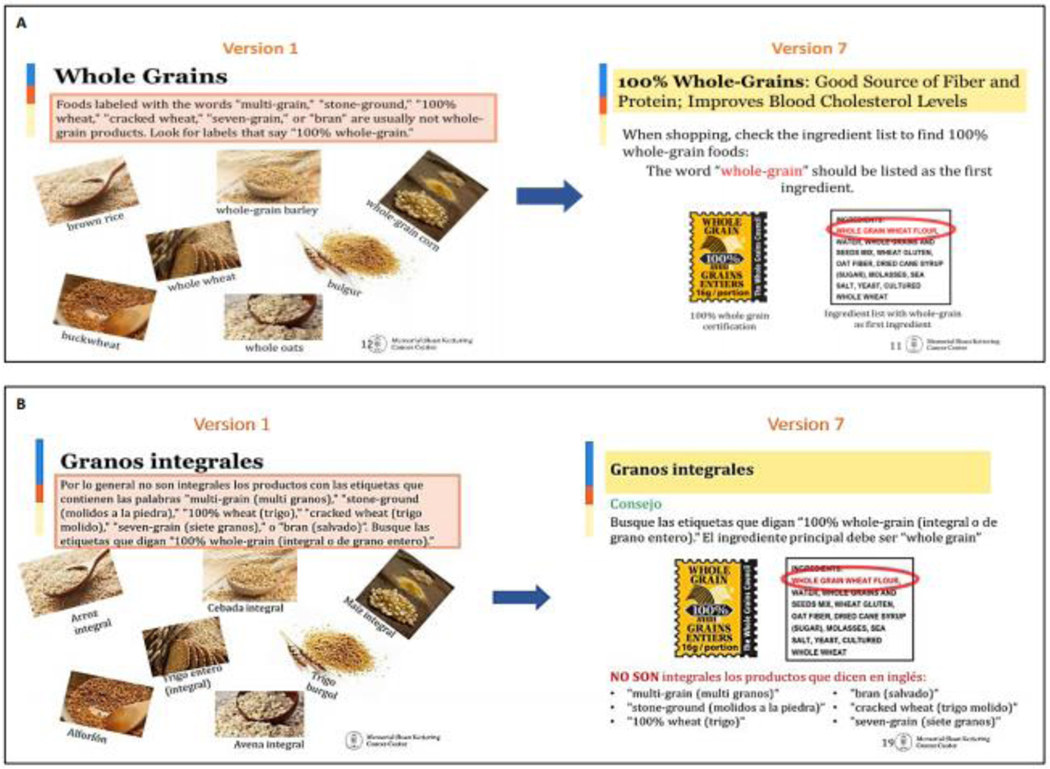
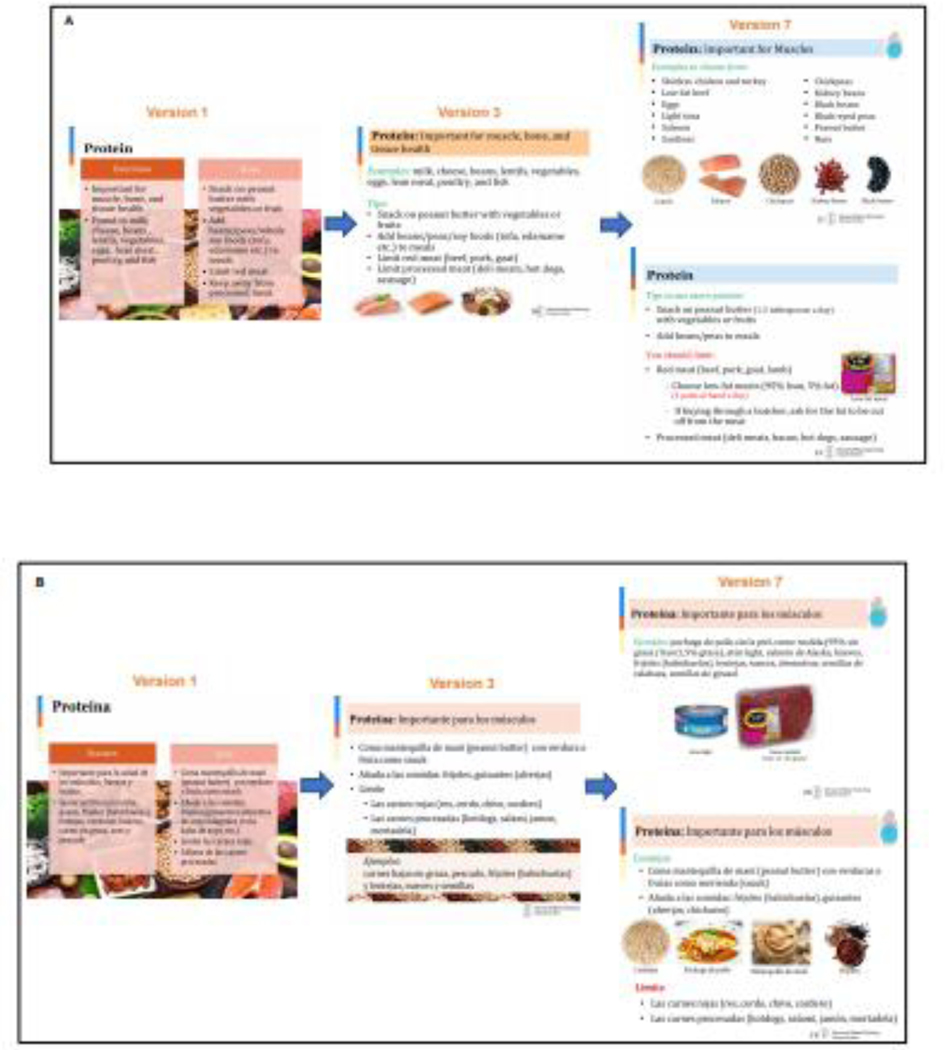
Patients were confused about what the pictures in Figures 2 demonstrated. They thought that the pictures exemplified grains to avoid rather than whole grains because nonwhole grains were referenced in the text. English- and Spanish-speaking patients wanted a clear visual distinction between “do’s and don’ts” or “good and bad.” Subsequently, they suggested positioning what to“do” at the top of the slide and what to “avoid” at the bottom. Patients also wanted important instructions, such as “limit” or “not,” to be highlighted, otherwise participants felt these terms got “lost in the page,” as one patient described it (Figure 3). Therefore, the layout of “do” at the top in green vs. “avoid” at the bottom in red was incorporated in both versions to provide structural and visual cues for the two types of tip.
Figure 2.
English (A) and Spanish (B) whole grains slides, showing modifications from version 1 to version 7
Figure 3.
English (A) and Spanish (B) protein slide modifications
Spanish-speaking patients requested instructions, and especially pictures, to help them recognize the recommended foods when shopping and to identify nutritional information (such as the nutrition labels) on food packaging. Both English- and Spanish-speaking patients advised labeling each picture because “people may not know” the terms corresponding to the pictured items. Patients also requested food group portion sizes in food group slides to serve as helpful reminders. Therefore, all pictures were labeled for recognition and included a portion size prompt.
In the Spanish version particularly, patients requested translation of English words found in the food pictures (e.g., nutrition label terms and food packaging labels). Spanish translations were therefore provided when pictures included English labels.
Visuals
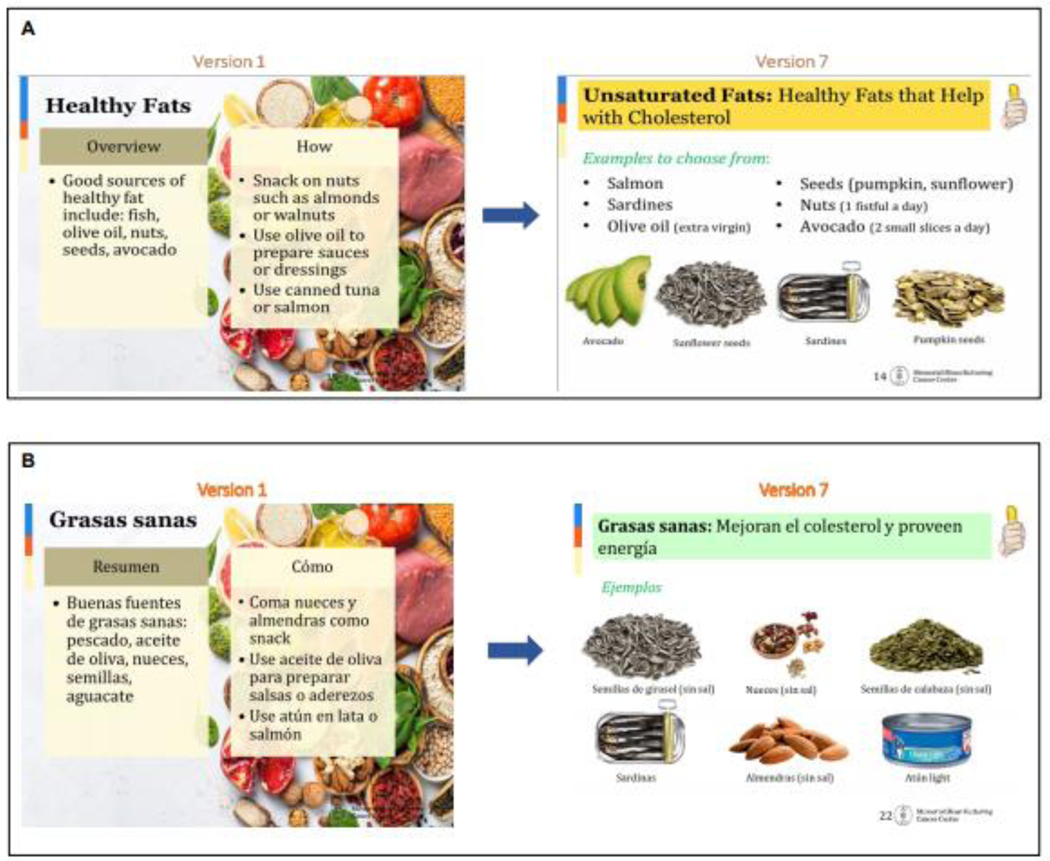
Through every iteration of the materials, patients frequently expressed appreciation of visual elements but requested the addition of more relevant and clear pictures. For example, in the initial version of the English and Spanish MyPlate slides, patients were unclear on which specific food items were illustrated and how much to consume of each (Figure 4). They requested better pictures that clearly outlined what type of food to eat, with portion distinction. A standard plate that demonstrated portion size was used, and each section of the plate and food group was labeled for clarity.
Figure 4.
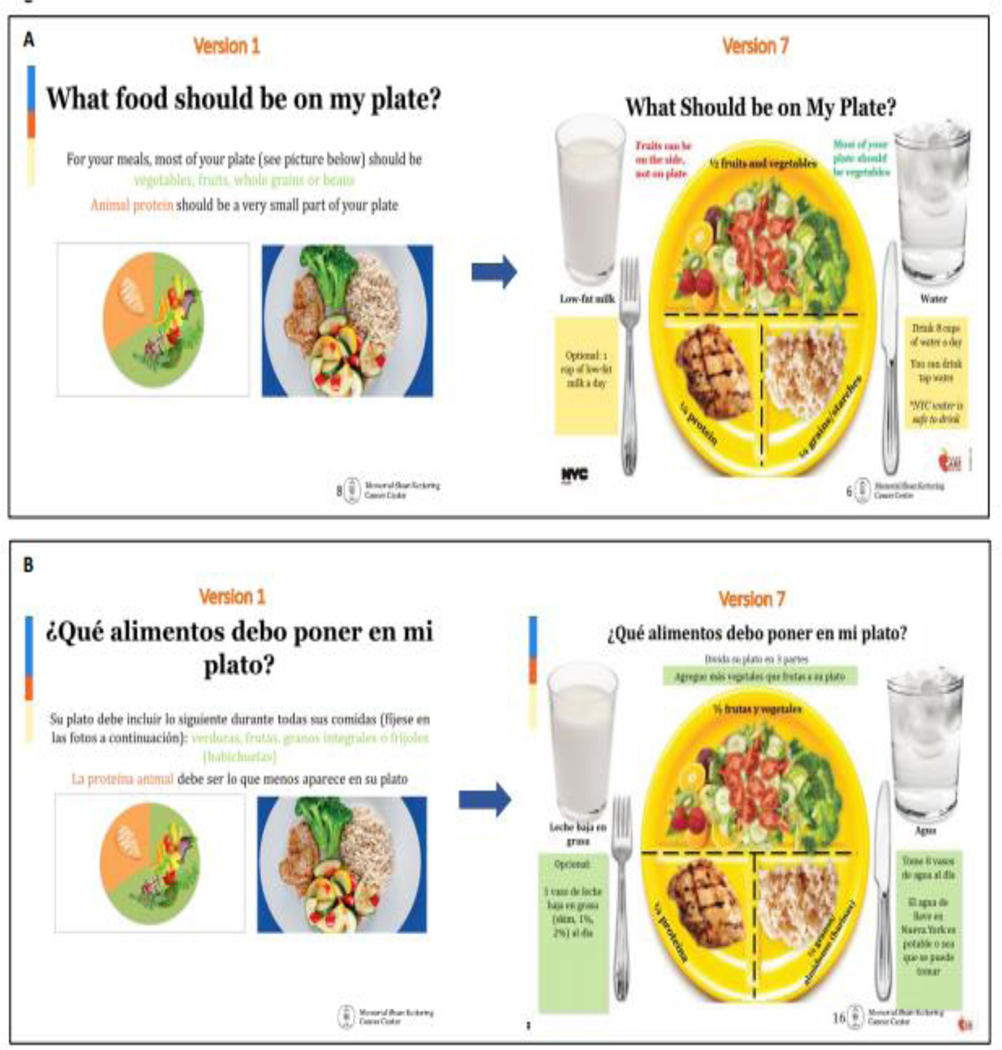
What should be on my plate slide modifications, English (A) and Spanish (B) versions
Overall, puzzling pictures were replaced, larger pictures were used, and more pictures of pertinent food examples were added and labeled while ensuring all were of high resolution (Figure 5).
Figure 5.
Unsaturated/healthy fats slide modifications for English (A) and Spanish (B) versions
4. DISCUSSION AND CONCLUSION
4.1. Discussion
Cognitive interviewing in English and Spanish provided valuable insight for the development of nutrition education materials for low-income, predominantly immigrant, Spanish- and English-preferring breast cancer patients and yielded recommendations for future development. These findings reinforce the importance of cognitive interviewing as a useful tool for improving comprehension of nutrition materials among immigrant populations [36, 37]. This study also highlights the importance of linguistic variation between countries/cultures that generally speak “the same language.” This is of particular interest in major metropolitan areas, such as NYC, Los Angeles, and Miami, and in other Western countries with large immigrant populations [9, 10].
When developing the materials, great care was taken to ensure that the content was culturally responsive. The English- and Spanish-speaking patients had varying countries of origin, and speakers often used different vocabulary to describe the same item. It is important to culturally and linguistically tailor health education interventions to English- and Spanish-speaking sub-groups, taking into account both their place of origin and their current geographic location [38]. To ensure inclusivity of a wide range of dialects, the materials were tailored to include regional vocabulary, offering alternate terms when needed. Furthermore, many Spanish speakers had lived in the US for over a decade and, possibly due to acculturation and lack of variation in equivalent Spanish terms, some preferred English words for certain terms, such as “snack.”
It was important to modify example foods to reflect those with which patients were familiar and may have preferred, a need that Shilts and colleagues also identified in their adaptation of MyPlate [26]. Both English- and Spanish-preferring patients were often unfamiliar with buckwheat and suggested quinoa instead. This tailoring can help ensure that education related to diet and nutrition is effectively adopted and can positively influence health outcomes [39].
Likewise, tailoring the layout of the English and Spanish slides to fit patient preferences facilitated comprehension. Color coding makes text more prominent and certain colors are associated with meaning and decision-making, with green having positive associations and red having negative associations [40]. Therefore, tips were coalesced in their respective color-coded categories. Furthermore, patient feedback led to a consistent slide layout, so that patients could easily discern good from bad foods by their placement on the slide. These features may have helped to relieve patients’ cognitive load, limiting the amount of working memory needed to comprehend the slides by tying into existing schemas (color coding, meaning of information placement), and freeing it up to process other aspects of the message [40, 41].
Both sets of patients interpreted what was shown in the images as having to be exactly followed. Also, patients looked to the images for instruction more commonly than the text. Subsequently, the materials were adapted to closely match the text. It has been recommended that graphics in nutrition education materials clarify and emphasize the written text by being clear, relevant, and realistic [42]. Patient feedback during the interviews supported this idea. The first slide deck included images that mainly served to enhance the aesthetic of the materials, not to enhance the written text. Patients shared that the images were not clear and did not help them understand the instruction, and they requested clear pictures to act as examples of textual descriptions.
Additionally, pictures, when strongly connected to text, are associated with more attention and recall of education information than text alone [43, 44]. Pictures that provide an emotional response can also help increase target behaviors and learning, suggesting that appealing pictures linked to simple text can be especially beneficial for patients [43, 44].Our findings reflect those of previous studies as the most requested recommendation across our English and Spanish speakers was the addition of labeled pictures (particularly for foods/items relevant to each slide). Patients also cared for the quality and recognizability of visual aids (e.g., common food pairings), and readily asked for more appealing, pertinent, or clear pictures.
Furthermore, the Spanish and English nutrition materials have some differences in content to reflect the communities’ feedback. To ensure fidelity when adapting nutrition education for a Spanish-speaking population, Willie recommended adding and rearranging the order of lessons and concepts [45]. Per patient request, our Spanish materials were adapted to contain an English Nutrition Facts label guide (including translations) and to include nutrition labels for each of the nutrients discussed (such as the “whole grain” label). It has been found that Spanish speakers of all income levels have a similar likelihood of using nutrition labels, and nutrition label use among English-speaking Latinos is significantly associated with reduced risk of poor diet, indicating potential feasibility and effectiveness of nutrition label education among Latinx people of all socioeconomic backgrounds [46]. The difference in demand for nutrition label information between the Spanish and English speakers in our study could have been due to the language barrier, as nutrition label usage among Latinx Spanish speakers is not associated with comprehension [47].Given the potential benefits of reading nutrition labels and the desire for nutrition literacy in our population, this could be a salient component of nutrition education interventions among Latinx Spanish speakers.
Notably, patients demonstrated an interest in nutrition information that went beyond the scope of the original intervention content. We considered their numerous requests for further information, which resulted in our inclusion of multiple additional topics, such as sugar, salt, and nutrition labels. However, to minimize the risk of overwhelming patients, all topics of interest could not be included in this one-time intervention.
Implications for Further Research
One topic of interest that was not incorporated in the nutrition education materials due to length and time limitations was recipes. Patients commented that they did not use certain healthy items because they did not know how to cook them. They requested recipes as a practical means of applying the tips and using the unfamiliar food items highlighted. While US women of all backgrounds and income levels may prepare homecooked meals, women with less education, like many of our patients, spend more time cooking [48, 49]. Increasing nutrition knowledge and cooking skills can influence food choice, increase cooking confidence, and promote fruit and vegetable consumption [48, 50]. This further demonstrates the demand for nutrition education among low-income immigrant cancer patients [51], and suggests that comprehensive intervention programs to enhance their health outcomes, education, and diet quality are needed.
Comprehensive and tailored nutrition education programs are important for diverse communities globally, to address health outcome inequities [52]. Ensuring comprehensible nutrition education materials for non-native speakers of the dominant language can be vital to decrease outcome disparities for low-income and immigrant breast cancer patients in a range of settings [53].
Further research should include the assessment of large-scale implementation of this study’s findings in a range of settings, including by the participating cancer clinics in NYC and other metropolitan areas whose clinics serve immigrant and minority populations, to further evaluate the study’s impact.
Limitations
These findings may not be representative of all breast cancer patients. Participants were from 6 NYC hospitals that participate in ICCAN and a Latina cancer support organization, potentially limiting generalizability. Nevertheless, participants recruited had all stages of cancer and represented varied backgrounds. The cognitive interviews were not audio recorded, and there is a risk that some of the responses were not recorded verbatim by the interviewers.
4.2. Conclusion
Our research demonstrates how a nutrition education curriculum for low-literacy, predominantly immigrant and minority, English- and Spanish-speaking breast cancer patients can be developed by using cognitive interviewing, nutritionist guidance, and a bilingual, culturally responsive study team. By working with patients in a structured process, we developed materials that addressed their desire for nutrition knowledge in ways that were tailored to their cultural and linguistic influences and were optimized to their learning needs.
4.3. Practice Implications
Several steps are needed to ensure nutrition education materials are comprehensively and clearly adapted for culturally and linguistically diverse audiences. Concepts that may not hew directly to the cultures of the intended audience can still be incorporated to reflect the patients’ expressed interest in learning new ideas. Instructions should be simple and well-defined, accounting for regional linguistic variations and post-migration influences and using examples, color cues, and images to clarify text. Patients value the use of textual and pictorial examples to clarify instruction. Finally, images should enhance text, not distract from it. This topic is of importance in many Western countries with large immigrant populations, and our methodology could be used with similar populations with breast and other cancer types.
Supplementary Material
Highlights.
Many immigrant breast cancer patients seen at safety net facilities are vulnerable to food insecurity
An English/Spanish nutrition presentation was developed for breast cancer patients.
Iterative development involved 7 rounds of cognitive interviews per language.
Changes included adapting to regional lexicons and tailoring layout and visuals.
Culturally/linguistically responsive food examples and labeled images were needed.
ACKNOWLEDGEMENTS
Funding: This work was supported by the National Cancer Institute [grant numbers R01 CA230446-01, U54 CA137788, and P30 CA008748] and the Laurie Tisch Illumination Fund.
Editorial Support: The authors thank Sonya J. Smyk, Memorial Sloan Kettering Cancer Center, for writing and editorial support.
Footnotes
CRediT author statement
Francesca Gany: conceptualization, methodology, formal analysis, investigation, writing (original draft, reviewing and editing), supervision, funding acquisition
Irina Melnic: methodology, formal analysis, investigation, writing (original draft, reviewing and editing), project administration
Angelica E. Alvarado: formal analysis, investigation, writing (original draft, reviewing and editing)
Maria Claros: formal analysis, investigation, writing (original draft, reviewing and editing)
Chanel I. Martinez: formal analysis, investigation, writing (original draft, reviewing and editing)
Javier Gonzalez: formal analysis, investigation, writing (reviewing and editing)
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- [1].Centers for Disease Control and Prevention, Breast Cancer Statistics, 2018. https://www.cdc.gov/cancer/breast/statistics/index.htm. (Accessed May 21, 2019.
- [2].Hochsmann C, Knaier R, Eymann J, Hintermann J, Infanger D, Schmidt-Trucksass A, Validity of activity trackers, smartphones, and phone applications to measure steps in various walking conditions, Scandinavian journal of medicine & science in sports 28(7) (2018) 1818–1827. [DOI] [PubMed] [Google Scholar]
- [3].Murphy JL, Girot EA, The importance of nutrition, diet and lifestyle advice for cancer survivors - the role of nursing staff and interprofessional workers, J Clin Nurs 22(11–12) (2013) 1539–49. [DOI] [PubMed] [Google Scholar]
- [4].Arends J, Baracos V, Bertz H, Bozzetti F, Calder PC, Deutz NEP, Erickson N, Laviano A, Lisanti MP, Lobo DN, McMillan DC, Muscaritoli M, Ockenga J, Pirlich M, Strasser F, de M. van Schueren der, Van Gossum A, Vaupel P, Weimann A, ESPEN expert group recommendations for action against cancer-related malnutrition, Clin Nutr 36(5) (2017) 1187–1196. [DOI] [PubMed] [Google Scholar]
- [5].United States Census Bureau, Limited English Speaking Households, 2018. https://data.census.gov/cedsci/table?q=languages%20spoken%20at%20home&hidePreview=false&table=C16001&tid=ACSST1Y2018.S1602&lastDisplayedRow=29&vintage=2018. (Accessed July 13 2020).
- [6].US Census Bureau, QuickFacts United States (V2019), 2019. https://www.census.gov/about.html. (Accessed June 26 2020).
- [7].Number of migrants now growing faster than world population, new UN figures show, 2019. https://news.un.org/en/story/2019/09/1046562. (Accessed April 5 2021).
- [8].Carrera PM, Kantarjian HM, Blinder VS, The financial burden and distress of patients with cancer: Understanding and stepping-up action on the financial toxicity of cancer treatment, CA: a cancer journal for clinicians 68(2) (2018) 153–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Budiman A, Key findings about U.S. immigrants, 2020. https://www.pewresearch.org/facttank/2020/08/20/key-findings-about-u-s-immigrants/. (Accessed April 5 2021).
- [10].Whatley M, Batalova J, Limited English Proficient Population of the United States in 2011, 2013. https://www.migrationpolicy.org/article/limited-english-proficient-population-united-states-2011#5. (Accessed April 5 2021).
- [11].Amaya N, How Many Languages Are Spoken in NYC?, 2018. https://www.worldatlas.com/articles/how-many-languages-are-spoken-in-nyc.html. (Accessed July 13 2020).
- [12].New York City, Language Access. https://www1.nyc.gov/site/planning/about/language-access.page. (Accessed July 13 2020).
- [13].NYC Health+Hospitals, Community Needs Health Assesssment, NYC Health+Hospitals, New York, NY, 2016. [Google Scholar]
- [14].Tiedje K, Wieland ML, Meiers SJ, Mohamed AA, Formea CM, Ridgeway JL, Asiedu GB, Boyum G, Weis JA, Nigon JA, Patten CA, Sia IG, A focus group study of healthy eating knowledge, practices, and barriers among adult and adolescent immigrants and refugees in the United States, Int J Behav Nutr Phys Act 11 (2014) 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Gany F, Lee T, Ramirez J, Massie D, Moran A, Crist M, McNish T, Winkel G, Leng JC, Do our patients have enough to eat?: Food insecurity among urban low-income cancer patients, Journal of health care for the poor and underserved 25(3) (2014) 1153–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].USDA Economic Research Service, Food Security in the U.S, 2019. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/. (Accessed July 10 2020).
- [17].Gany FM, Yorga S, Ramirez J, Paolantonio L, Development of a medically tailored hospital-based food pantry system, J Health Care Poor Underserved 31(2) (2020) 595–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Gany F, Lee T, Loeb R, Ramirez J, Moran A, Crist M, McNish T, Leng JC, Use of Hospital-Based Food Pantries Among Low-Income Urban Cancer Patients, J Community Health 40(6) (2015) 1193–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Silk KJ, Sherry J, Winn B, Keesecker N, Horodynski MA, Sayir A, Increasing nutrition literacy: testing the effectiveness of print, web site, and game modalities, J Nutr Educ Behav 40(1) (2008) 3–10. [DOI] [PubMed] [Google Scholar]
- [20].Parekh N, Jiang J, Buchan M, Meyers M, Gibbs H, Krebs P, Nutrition literacy among cancer survivors: feasibility results from the Healthy Eating and Living Against Breast Cancer (HEAL-BCa) Study: a pilot randomized controlled trial, J Cancer Educ 33(6) (2018) 1239–1249. [DOI] [PubMed] [Google Scholar]
- [21].Hammons AJ, Hannon BA, Teran-Garcia M, Barragan M, Villegas E, Wiley A, Fiese B, Effects of Culturally Tailored Nutrition Education on Dietary Quality of Hispanic Mothers: A Randomized Control Trial, Journal of nutrition education and behavior 51(10) (2019) 1168–1176. [DOI] [PubMed] [Google Scholar]
- [22].Ikeda JP, Pham L, Nguyen KP, Mitchell RA, Culturally relevant nutrition education improves dietary quality among WIC-eligible Vietnamese immigrants, Journal of nutrition education and behavior 34(3) (2002) 151–8. [DOI] [PubMed] [Google Scholar]
- [23].Fernandez-Gutierrez M, Bas-Sarmiento P, Albar-Marin MJ, Paloma-Castro O, Romero-Sanchez JM, Health literacy interventions for immigrant populations: a systematic review, International nursing review 65(1) (2018) 54–64. [DOI] [PubMed] [Google Scholar]
- [24].Katz MG, Kripalani S, Weiss BD, Use of pictorial aids in medication instructions: A review of the literature, 63(23) (2006) 2391–2397. [DOI] [PubMed] [Google Scholar]
- [25].Sansgiry SS, Cady PS, Adamcik BA, Consumer Comprehension of Information on Over-the-Counter Medication Labels: Effects of Picture Superiority and Individual Differences Based on Age, 11(3) (1997) 63–76. [Google Scholar]
- [26].Shilts MK, Johns MC, Lamp C, Schneider C, Townsend MS, A Picture Is Worth a Thousand Words: Customizing MyPlate for Low-Literate, Low-Income Families in 4 Steps, Journal of nutrition education and behavior 47(4) (2015) 394–6.e1. [DOI] [PubMed] [Google Scholar]
- [27].Winokur EJ, Rutledge DN, McGowan JJ, A Picture is Worth a Thousand Words: Pictographs to Improve Understanding of Discharge Instructions, Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association (2019). [DOI] [PubMed] [Google Scholar]
- [28].Costas-Muñiz R, Torres-Blasco N, Castro-Figueroa EM, González CJ, Breitbart W, Gany F, Meaning-Centered Psychotherapy for Latino Patients with Advanced Cancer: Cultural Adaptation Process, Journal of palliative medicine 23(4) (2020) 489–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Lowe E, Jamaican Food Words & Phrases: Fruits & Veggies Edition. https://cggmagazine.com/2019/11/12/jamaican-food-words-phrases-fruits-veggies-edition/#menuopen. (Accessed July 10 2020).
- [30].Nero S, Language, identity, and education of Caribbean English speakers, 25(34) (2006) 501–511. [Google Scholar]
- [31].Carbone ET, Campbell MK, Honess-Morreale L, Use of cognitive interview techniques in the development of nutrition surveys and interactive nutrition messages for low-income populations, 102(5) (2002) 690–6. [DOI] [PubMed] [Google Scholar]
- [32].Shafer K, Lohse B, How to Conduct a Cognitive Interview - A Nutrition Education Example, 2015. https://nifa.usda.gov/resource/how-conduct-cognitive-interview-nutrition-education-example. [Google Scholar]
- [33].United States Department of Agriculture, ChooseMyPlate.gov, 2018. https://www.choosemyplate.gov/MyPlate. (Accessed March 5, 2019.
- [34].God’s Love We Deliver, Every Bite Counts! Nutritional Tips for Breast Cancer Patients, 2017. https://www.glwd.org/wp-content/uploads/2018/09/Breast_Cancer_Patients.pdf.
- [35].United States Department of Agriculture, Save more at the grocery store: 10 MyPlate tips to stretch your food dollar, 2014. http://www.jumpinforhealthykids.org/userfiles/file/news/USDA-10TipsToStretchFoodDollar.pdf. (Accessed March 5, 2019.
- [36].McNeill E, Hashemi A, Ramirez J, Roberts-Eversley N, Gany F, Taxi Drivers at Risk: Tailoring Nutrition and Exercise Materials, Journal of community health (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Dickin KL, Larios F, Parra PA, Cognitive Interviewing to Enhance Comprehension and Accuracy of Responses to a Spanish-Language Nutrition Program Evaluation Tool, Journal of nutrition education and behavior 47(5) (2015) 465–71.e1. [DOI] [PubMed] [Google Scholar]
- [38].Rivera YM, Vélez H, Canales J, Jiménez JC, Moreno L, Torres J, Vadaparampil ST, Muñoz-Antonia T, Quinn GP, When a Common Language Is Not Enough: Transcreating Cancer 101 for Communities in Puerto Rico, 31(4) (2016) 776–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Hurt TR, Seawell AH, O’Connor MC, Developing Effective Diabetes Programming for Black Men, 2 (2015) 2333393615610576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Hieke S, Wilczynski P, Colour Me In--an empirical study on consumer responses to the traffic light signposting system in nutrition labelling, 15(5) (2012) 773–82. [DOI] [PubMed] [Google Scholar]
- [41].Sweller J, CHAPTER TWO - Cognitive Load Theory, in: Mestre JP, Ross BH (Eds.), Psychology of Learning and Motivation, Academic Press; 2011, pp. 37–76. [Google Scholar]
- [42].Clayton LH, Strategies for selecting effective patient nutrition education materials, 25(5) (2010) 436–42. [DOI] [PubMed] [Google Scholar]
- [43].Houts PS, Doak CC, Doak LG, Loscalzo MJ, The role of pictures in improving health communication: a review of research on attention, comprehension, recall, and adherence, 61(2) (2006) 173–90. [DOI] [PubMed] [Google Scholar]
- [44].Schneider S, Dyrna J, Meier L, Beege M, Rey GD, How affective charge and text–picture connectedness moderate the impact of decorative pictures on multimedia learning, American Psychological Association, US, 2018, pp. 233–249. [Google Scholar]
- [45].Wille CG, Creaciones en la Cocina: A Culturally Adapted Nutrition Education Curriculum for Spanish-Speaking Latinos, 52(7) (2020) 747–750. [DOI] [PubMed] [Google Scholar]
- [46].Wilson MD, Ramírez AS, Arsenault JE, Miller LMS, Nutrition Label Use and Its Association With Dietary Quality Among Latinos: The Roles of Poverty and Acculturation, 50(9) (2018) 876–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Sharif MZ, Rizzo S, Prelip ML, Glik DC, Belin TR, Langellier BA, Kuo AA, Garza JR, Ortega AN, The association between nutrition facts label utilization and comprehension among Latinos in two east Los Angeles neighborhoods, 114(12) (2014) 1915–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Winkler E, Turrell G, Confidence to cook vegetables and the buying habits of Australian households, 110(5 Suppl) (2010) S52–61. [DOI] [PubMed] [Google Scholar]
- [49].Taillie LS, Who’s cooking? Trends in US home food preparation by gender, education, and race/ethnicity from 2003 to 2016, 17(1) (2018) 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Chung LMY, Chung JWY, Chan APC, Building Healthy Eating Knowledge and Behavior: An Evaluation of Nutrition Education in a Skill Training Course for Construction Apprentices, 16(23) (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Maschke J, Kruk U, Kastrati K, Kleeberg J, Buchholz D, Erickson N, Huebner J, Nutritional care of cancer patients: a survey on patients’ needs and medical care in reality, 22(1) (2017) 200–206. [DOI] [PubMed] [Google Scholar]
- [52].Ledoux C, Pilot E, Diaz E, Krafft T, Migrants’ access to healthcare services within the European Union: a content analysis of policy documents in Ireland, Portugal and Spain, 14(1) (2018) 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Vahabi M, Lofters A, Kumar M, Glazier RH, Breast cancer screening disparities among urban immigrants: a population-based study in Ontario, Canada, 15(1) (2015) 679. [DOI] [PMC free article] [PubMed] [Google Scholar]; Trevena LJ, , Barratt A, Butow P. and Caldwell P. (2006), A systematic review on communicating with patients about evidence. Journal of Evaluation in Clinical Practice, 12: 13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.