Abstract
Objective:
Meditation practice and meditation-based psychotherapies have become increasingly popular. Although psychological benefits associated with meditation are well-documented, potential risks are unclear.
Method:
We conducted a population-based survey to evaluate the occurrence of a broad range of meditation-related adverse effects (MRAE).
Results:
953 participants completed our screening survey, 470 endorsed lifetime exposure to meditation practice, and 434 completed a follow-up survey assessing MRAE (92.3% response rate). A higher proportion than hypothesized reported occurrence of MRAE (general item = 32.3%, 1+ specific item = 50.0%) and MRAE duration ≥1 month (10.4%). Anxiety, traumatic re-experiencing, and emotional sensitivity were the most common MRAE. Some degree of functional impairment was reported by 10.6% of participants, with impairment lasting ≥1 month for 1.2%. Childhood adversity was associated with elevated risk for MRAE. Participants reporting MRAE were equally glad to have practiced meditation as those not reporting MRAE. Additional correlates of MRAE were identified in exploratory analyses.
Conclusion:
MRAE are common, even in a sample with relatively modest amounts of experience. Identifying individuals at elevated risk for MRAE, being transparent and realistic about the possible range of effects, and increasing trauma-sensitivity are warranted to maximize benefits and minimize risks of meditation.
Keywords: adverse effects, meditation, mindfulness, harm, mindfulness-based interventions
In the past several decades, meditation practice and evidence-based interventions centered on meditation practice such as mindfulness-based stress reduction (MBSR; Kabat-Zinn, 2013) and mindfulness-based cognitive therapy (MBCT; Segal et al., 2013) have entered into the mainstream of popular culture and medicine. Meditation apps are far and away the most widely used mental health apps (Wasil et al., 2020), mindfulness training is being used as primary prevention in elementary school settings (e.g., van de Weijer-Bergsma et al., 2014), and past year utilization of meditation tripled between 2012 and 2017 (Clarke et al., 2018). Although some media claims regarding meditation are inaccurate (Van Dam et al., 2018), the results of hundreds of randomized trials testing standardized mindfulness-based interventions suggest these approaches generally confer benefits superior to waitlist controls and on par or superior to other active therapies across a wide range of populations, clinical conditions, and outcome types (Dunning et al., 2019; Goldberg et al., 2021; Goldberg et al., 2018).
In parallel to rising popularity, there has been growing concern regarding the possibility that meditation practice may also cause harm (Baer et al., 2019). The notion of side effects is well-known in medicine. In psychopharmacology, for example, clinical potency is commonly coupled with elevated risk for adverse effects, with many of the most effective psychopharmacological agents (e.g., antipsychotic medications) also carrying the highest side effect burden (Haddad & Sharma, 2007). It has likewise long been recognized that psychological interventions can produce both benefit and harm (Bergin, 1966; Lilienfeld, 2007). Despite the acknowledgement of potential harm in other mental health interventions, investigation of adverse effects in meditation-based interventions has been comparatively minimal and primarily occurred only the past 10 years (Farias et al., 2020). This coupling of increased utilization with inadequate acknowledgment of potential risks highlights the need to more fully characterize the range of effects that meditation training can produce.
Meditation-related adverse effects (MRAE)
The World Health Organization (WHO, 2010) International Classification for Patient Safety defines a side effect as “a known effect, other than that primarily intended, related to a medicine’s pharmacological properties” (p. 17). Adverse effects are defined as negatively valenced (i.e., subjectively unpleasant) side effects which vary in degree of severity. Although WHO (2010) guidelines were not originally written with reference to psychological interventions, psychotherapy researchers have applied similar notions of side effects and adverse effects in psychotherapy. Adverse effects can occur as a result of incorrect treatment (malpractice reaction) or correct treatment (adverse treatment reaction; Linden, 2013) and range in severity from mild (e.g., crying in session) to extremely severe or life threatening (e.g., suicide; Linden & Schermuly-Haupt, 2014). Adverse effects also vary in duration, from transient to sustained (Duggan et al., 2014), although even short duration adverse effects may be clinically important (e.g., acute suicidality). Adverse effects and treatment benefits can co-occur and may occur in one domain (e.g., target problem) and not another (i.e., non-target problem; Dimidjian & Hollon, 2010). Thus, a broad, multi-dimensional approach that avoids arbitrarily defining certain experiences as “harm” (and others as “not harm”) and captures the full range of severity can be helpful for a thorough evaluation of adverse effects in psychosocial interventions.
There is no reasonable doubt that meditation can cause challenging experiences. Discussion of a wide variety of distressing consequences of meditation practice appear in both traditional contemplative sources (e.g., Sayadaw, 2016) and are now widely documented in the scientific literature (Anderson et al., 2019; Britton et al., in press; Dobkin, Irving, & Amar, 2012; Farias et al., 2020; Lindahl et al., 2017). However, several open questions remain, questions whose answers are important for efforts to increase the safety, acceptability, and efficacy of meditation-based interventions and provide accurate information to consumers. Key questions include the population-level prevalence and types of adverse effects occurring in meditation (i.e., meditation-related adverse effects [MRAE]); the subjective appraisal of MRAE; and participant-, provider-, and intervention-related factors associated with elevated risk for MRAE (Baer et al., 2019).
Frequency estimates of MRAE vary widely, and depend heavily on study design, sample, and how MRAE are defined and measured. A systematic review of meditation studies found an overall rate of 8.3% that varied by study design: 3.7% for experimental studies (e.g., randomized controlled trials [RCT]) and 33.2% for observational studies (Farias et al. 2020). Cross-sectional online survey studies (Cebolla et al., 2017; Schlosser et al., 2019; Vieten et al., 2018) which variously queried “unwanted or adverse reactions with potential harm to your health” (Cebolla et al 2017) and particularly unpleasant experiences (e.g., anxiety, fear, distorted emotions or thoughts, altered sense of self or the world; Schlosser et al., 2019; Vieten et al., 2018) have produced MRAE prevalence rates between 25.4–32%.
Three studies have systematically examined MRAEs in the context of standardized 8-week mindfulness-based interventions (MBSR/MBCT). In two samples (ns < 100), Baer et al. (2020) reported rates of 67–73% for “unpleasant experiences” and rates of 2 to 7% for “harm,” which was defined as being “worse off, in any way, after the course, than you would have been if you hadn’t done the course.” In a sample MBSR participants (n = 2,311), Hirshberg et al. (2020) reported rates of 15.2– 43.7% for increased symptoms, 6.8–32.3% for >35% symptom increase and 3.6– 4.4% for “clinically significant harm” which was defined as psychological distress worsening from functional to clinical levels. Rates across all three indices were similar to or lower than rates in a waitlist group. In three variants of MBCT (n = 96), Britton et al. (in press) found rates of 58% for negatively valenced experiences, and 6% for negative impacts on functioning lasting more than 1 month.
Both RCTs and observational studies provide worthwhile perspectives for clarifying prevalence of MRAE. In theory, RCTs can be used to establish causality (i.e., whether meditation training caused a particular adverse effect), although the existing literature is limited in important ways. In two meta-analyses of RCTs of mindfulness-based interventions, Kuyken et al. (2016) and Wong et al., (2018) reported serious (i.e., life threatening) adverse events occurring for ≤2% of participants and at similar rates across meditation and non-meditation control conditions. However, similar to psychotherapy generally (Jonsson et al., 2014), both meta-analyses note that adverse events were not consistency reported; more than 80% of RCTs do not provide any adverse effects statements (Wong et al., 2018), and less severe adverse effects whose assessment may not be required by regulatory bodies are almost never reported. Moreover, if assignment to the non-meditation control condition itself causes adverse effects (e.g., nocebo effects when using waitlist controls, although this possibility is debated; Furukawa et al., 2014; Munder et al., 2019), comparative rates of adverse effects may under-estimate their occurrence within meditation-based interventions. Randomized controlled trials also often lack the statistical power for examining other key questions such as factors correlated with occurrence of adverse effects.
Cross-sectional observational studies, such as those included in Farias et al.’s (2020) review, have been important for characterizing MRAE in the general population and can capture effects associated with varying degrees of meditation exposure. At once, the available studies also have important limitations, especially in regard to sampling procedures. The most important limitation is that none of the three recent cross-sectional studies were population-based surveys (see Supplemental Materials Table 1). Cebolla et al. (2017) specifically recruited individuals who reported having had MRAE and both Vieten et al. (2018) and Schlosser et al. (2019) recruited convenience samples through various online platforms (e.g., social media, academic and meditation center listservs). To our knowledge, no study has examined the prevalence of MRAE starting with a population-based sampling method in which efforts are made to recruit a demographically representative sample. Lacking such a design, it is unclear the degree to which previous results may be influenced by self-selection bias. A second limitation is that previous studies were primarily composed of individuals who were currently practicing meditation (Vieten et al., 2018) and/or who had practiced at least two months (Cebolla et al., 2017; Schlosser et al., 2019). These samples may omit a vital piece of the picture – individuals exposed to meditation who did not continue precisely due to adverse effects. Third, none of the three previous surveys applied the definitional boundaries of meditation that have been used in the largest representative survey of meditation practice – the National Health Interview Survey (NHIS; Centers for Disease Control and Prevention, n. d.). Sampling conducted using standardized definitions of what constitutes meditation should aid in comparability across studies. Finally, all three studies focused on MRAE broadly and did not query specific symptoms or assess the degree to which these experiences caused functional impairment.
Two additional dimensions that, to our knowledge, have not been previously investigated include the occurrence of adverse effects in relation to meditation training delivered through mobile health (mHealth) technology (e.g., smartphone apps) and the degree to which those experiencing MRAE feel glad to have practiced meditation. Meditation apps are widely used (Wasil et al., 2020) and the predominantly unguided format may contribute to the frequency of MRAE (given these experiences are more likely to occur when practicing alone; Schlosser et al., 2019). Moreover, those experiencing MRAE from mHealth may lack support from a qualified teacher, which could in turn cause greater impairment and persistence of difficulties, should MRAE occur. It is also important to evaluate whether MRAE are associated with whether or not an individual feels glad to have practiced meditation, as studies suggest that similar experiences may be experienced as helpful or harmful by different participants or even by the same participant at different times (e.g., Lindahl et al., 2020).
The Current Study
We aimed to evaluate the prevalence and correlates of a broad range of adverse effects associated with meditation practice in a population-based sample. To do so, we conducted an online survey using the Prolific platform which allows recruitment of participants in proportion with their representation in the United States (US) population based on age, gender, and race. Participants who indicated lifetime exposure to meditation using NHIS descriptions were invited to complete a follow-up survey assessing their meditation practice background, MRAE, and whether they felt glad to have practiced meditation. In order to capture a wide range of MRAE occurring naturalistically, we intentionally did not restrict our assessment to certain degrees of severity or duration (i.e., in contrast to only assessing serious / life-threatening adverse effects). We also assessed demographic and psychological characteristics theoretically and/or previously linked to increased risk for MRAE (e.g., childhood adversity, psychiatric symptoms; Lindahl et al., 2017; Schlosser et al., 2019; Treleaven, 2018). We made four a priori hypotheses which were preregistered through the Open Science Framework (https://osf.io/sjmpu). First, we hypothesized that MRAE would occur for a minority of participants (e.g., ~25%; Schlosser et al., 2019) and would generally be mild in nature (i.e., not impairing) and not persistent (e.g., ~5% persist beyond one month). Second, we hypothesized that the most common MRAE will be anxiety (Cebolla et al., 2017). Third, we hypothesized that MRAE will be more common for participants who report early childhood adversity (Treleaven, 2018). Fourth, we hypothesized that even those reporting MRAE will generally indicate that they were glad to have practiced meditation. We conducted several exploratory analyses examining correlates of MRAE.
Method
Participants
US residents were recruited through Prolific (www.Prolific.co) using their representative sampling procedure (see Supplemental Materials Table 2 for recruitment materials). Prolific is an online participant recruitment platform with functionality similar to Amazon’s Mechanical Turk. In contrast to Mechanical Turk, Prolific participants are on average more diverse, less dishonest, and more naïve to commonly used measures (Peer et al., 2017). In addition, Prolific offers demographically representative sampling in which participants are recruited in proportion to their representation in the population (Prolific.co, n. d.). Sampling is stratified based on age, gender, and race, currently using 2015 data from the US Census Bureau.
A total of 993 participants initiated the screening survey which assessed basic demographics and lifetime exposure to meditation practice, as defined using the NHIS criteria (see Measures). Of these, 953 passed the attention check item and completed screening. As shown in Supplemental Materials Table 3, relative to the US population (US Census Bureau, 2019), the overall sample was older (median age = 44 vs. 38.1), higher income (median income = $40,000 vs. $34,103), and more educated (50.6% with a bachelor’s degree or higher vs. 32.1%). Although several racial/ethnic groups appeared at rates similar to the population (Black, multiracial, Asian), non-Hispanic White participants were overrepresented (70.6%) and Hispanic participants were underrepresented (6.0%), likely due to Prolific matching on race but not ethnicity. Participants were paid $0.50 to $0.55 for completing the screening survey and $3.67 to $4.59 for completing the follow-up survey. Study procedures were approved by the Institutional Review Board at the University of Wisconsin - Madison.
Almost half of participants (n = 470; 49.3%) endorsed having lifetime exposure to at least one of the three NHIS meditation types and were invited to complete a follow-up survey regarding their experience with meditation. Most of those invited (n = 434; 92.3%) completed the follow-up survey and passed the attention check item. Those completing follow-up did not differ from those invited but not completing the follow-up survey on most demographic characteristics (age, gender, education, income; rs = −.05 to .05, ps > .284). However, non-Hispanic White participants were more likely to complete follow-up (r = .15, p = .001).
Measures
Demographics.
Participants provided their age, gender identity, race/ethnicity, educational background (i.e., highest degree), and annual income. For use as covariates in analyses, demographic variables (except age) were dichotomized: gender (not male as reference group), race/ethnicity (racial/ethnic minority as reference group), education (not college graduate as reference group), and income (income below US population per capita median [$34,103] as reference group; US Census Bureau, 2019).
Meditation practice background.
Several items assessed participants’ meditation practice background. To assess lifetime exposure to meditation, we included an item from the NHIS (Centers for Disease Control and Prevention, n. d.) in the screening survey. Participants were asked, “Have you ever tried any of the following types of meditation, even just once?” and were provided with NHIS descriptions of mantra meditation, mindfulness meditation, and spiritual meditation (Supplemental Materials Table 4). Participants reporting lifetime exposure to meditation were asked additional questions about their meditation practice in the follow-up survey (Supplemental Materials Table 5). This included when the participant was first introduced to meditation (in years), how the participant was first introduced (e.g., through smartphone app), and how the participant has ever been exposed to meditation (e.g., through smartphone app). Although multiple types of exposure were assessed, this variable was dichotomized as first and lifetime exposure through smartphone apps, given the rising popularity of this approach (Wasil et al., 2020). Participants also indicated their average days of meditation practice per week in the past 30 days (response options 0 to 7) and their lifetime hours of practice (response options 1–10, 11–100, 101–500, 501–1000, 1001–5000, 5000+). Participants indicated whether they have ever been exposed to various styles of practice. As concentration and insight practices have been previously linked to MRAE (Lindahl et al., 2017; Schlosser et al., 2019), two dichotomous variables (yes/no) were created reflecting lifetime exposure to concentration or insight practice. Participants also indicated whether they have attended a multiday meditation retreat, as intensive meditation retreats have previously been linked to MRAE (Lindahl et al., 2017).
Depression and anxiety symptoms.
Two widely used measures assessed symptoms of depression and anxiety in the past 7 days. These measures were included based on the notion that individuals more prone to common psychiatric symptoms may also be more at risk for MRAE (Schlosser et al., 2019). To assess depression and anxiety symptoms, four-item versions of the Patient-Reported Outcome Measurement Information System (PROMIS) Depression (4a) and Anxiety (4a) were used (Pilkonis et al., 2011). Items index symptoms of depression (e.g., “I felt worthless”) and anxiety (e.g., “I felt fearful) in the past 7 days. Responses are made on a 5-point Likert-type scale ranging from 1 (never) to 5 (always). A total score was computed by summing across times. Internal consistency was adequate in the current sample (αs = .93 and .90, for PROMIS Depression and Anxiety, respectively).
Loneliness.
We used the 5-item National Institutes of Health Loneliness scale (Cyranowski et al., 2013) to assess loneliness. This was based on the rationale that individuals more prone to experience loneliness may be at increased risk for MRAE. Participants rated their experience in the past 7 days (e.g., “I feel alone”) on a 5-point Likert-type scale ranging from 1 (never) to 5 (always). Internal consistency was adequate (α = .94).
Adverse childhood experiences.
Childhood adversity was measured using the 11-item Adverse Childhood Experience (ACE) module from the Behavioral Risk Factor Surveillance System (Ford et al., 2014). This measure assesses the occurrence of eleven adverse experiences including household dysfunction and occurrence of physical, emotional, and sexual abuse. Response options are dichotomous (i.e., yes/no, never/one or more times). A total score was computed by summing across all items (Ford et al., 2014). Internal consistency was adequate (Kuder-Richardson = .75).
Social desirability.
Social desirability was measured based on the possibility that it influenced participants’ willingness to disclose adverse experiences. The Socially Desirable Response Set (Hays et al., 1989) is a widely used measure where participants indicate the degree to which each of five items is true or false for them. Items include common but socially desirable or undesirable behavior (e.g., “I sometimes feel resentful when I don’t get my way”). Ratings are made on a 5-point Likert-type scale (definitely true to definitely false). Responses are dichotomized, with 1 being assigned when a respondent indicates the maximally socially desirable response option (e.g., definitely false for a socially undesirable item). A total score is computed across all items. Internal consistency was adequate (Kuder-Richardson = .71)
MRAE and feeling glad to have practiced meditation.
Items were included to assess the prevalence of a broad range of MRAE and whether participants feel glad to have practiced meditation (Tables 1 and 2, Supplemental Materials Table 5). In order to most fully capture these experiences, we included three items assessing MRAE that referred to “challenging, difficult, or distressing experiences,” an 11-item questionnaire (Britton, Lindahl, & Cooper, 2018) that assessed the occurrence of specific MRAE previously found to occur in the context of mindfulness-based programs (Lindahl et al., 2017), and a single item assessing whether participants felt glad to have practiced meditation, given potential challenging experiences.
Table 1.
Follow-up survey sample descriptive statistics (n = 434)
| Variables | Mean | SD | % | n | Min | Max | Skew | Kurtosis |
|---|---|---|---|---|---|---|---|---|
| Age | 43.77 | 15.53 | 19 | 78 | 0.16 | −1.17 | ||
| Male | 43.55 | 189 | 0 | 1 | 0.26 | −1.94 | ||
| non-Hispanic White | 72.58 | 315 | 0 | 1 | −1.01 | −0.98 | ||
| Bachelor’s degree | 56.91 | 247 | 0 | 1 | −0.28 | −1.93 | ||
| Low income | 43.09 | 187 | 0 | 1 | 0.28 | −1.93 | ||
| Any adverse effect | 32.26 | 140 | 0 | 1 | 0.76 | −1.43 | ||
| Mantra meditation | 29.26 | 127 | 0 | 1 | 0.91 | −1.18 | ||
| Mindfulness meditation | 70.97 | 308 | 0 | 1 | −0.92 | −1.15 | ||
| Spiritual meditation | 53.23 | 231 | 0 | 1 | −0.13 | −1.99 | ||
| 1+ MRAES-MBP | 50.00 | 217 | 0 | 1 | 0.00 | −2.00 | ||
| MRAES-MBP total | 1.90 | 2.73 | 0 | 10 | 1.47 | 1.09 | ||
| Any impairment | 10.60 | 46 | 0 | 1 | 2.55 | 4.52 | ||
| Impairment >1 day | 5.99 | 26 | 0 | 1 | 3.70 | 11.69 | ||
| Impairment ≥1 month | 1.15 | 5 | 0 | 1 | 9.12 | 81.42 | ||
| Years since first exposure | 14.28 | 13.77 | 0 | 59 | 1.18 | 0.49 | ||
| App first exposure | 3.92 | 17 | 0 | 1 | 4.73 | 20.46 | ||
| App ever exposure | 45.85 | 199 | 0 | 1 | 0.17 | −1.98 | ||
| Any meditation in the past 30 days | 65.21 | 283 | 0 | 1 | −0.64 | −1.60 | ||
| Weekly days of meditation in the past 30 days | 2.21 | 2.38 | 0 | 7 | 0.84 | −0.61 | ||
| Lifetime meditation hours category | ||||||||
| 0–10 | 18.89 | 82 | 0 | 1 | 1.58 | 0.51 | ||
| 11–100 | 41.24 | 179 | 0 | 1 | 0.35 | −1.88 | ||
| 101–500 | 16.36 | 71 | 0 | 1 | 1.81 | 1.29 | ||
| 501–1000 | 8.99 | 39 | 0 | 1 | 2.86 | 6.18 | ||
| 1001–5000 | 7.14 | 31 | 0 | 1 | 3.32 | 9.02 | ||
| 5001+ | 7.37 | 32 | 0 | 1 | 3.25 | 8.59 | ||
| Lifetime meditation hours continuous | 2.21 | 0.74 | 1 | 3 | −0.35 | −1.11 | ||
| Concentration practice | 84.33 | 366 | 0 | 1 | −1.88 | 1.55 | ||
| Insight practice | 25.81 | 112 | 0 | 1 | 1.10 | −0.79 | ||
| Residential retreat | 6.91 | 30 | 0 | 1 | 3.39 | 9.48 | ||
| PROMIS Depression in the past week | 8.53 | 4.26 | 4 | 20 | 0.7 | −0.5 | ||
| PROMIS Anxiety in the past week | 9.24 | 4.01 | 4 | 20 | 0.48 | −0.61 | ||
| NIH Toolbox Loneliness in the past week | 2.39 | 1.09 | 1 | 5 | 0.42 | −0.79 | ||
| Adverse Childhood Experiences | 14.04 | 2.43 | 11 | 22 | 0.71 | −0.02 | ||
| Socially Desirable Response Set | 0.21 | 0.68 | 0 | 5 | 4.61 | 25.14 | ||
| Glad to have practiced meditation | 4.99 | 1.12 | 1 | 6 | −0.94 | 0.25 | ||
| Glad to have practiced meditation dichotomous | 88.71 | 385 | 0 | 1 | −2.44 | 3.95 |
Note: MRAES-MBP = Meditation-Related Adverse Effects Scale – Mindfulness-Based Program; 1+ MRAES-MBP = whether any MRAES-MBP item was endorsed (i.e., response other than “Never”); App first exposure = first exposure to meditation through a smartphone app; App ever exposure = ever having been exposed to meditation through a smartphone app; Weekly days of meditation = average days of meditation per week in the past 30 days; Lifetime meditation hours continuous = 0 to 10 (1), 11–100 (2), 101+ (3); PROMIS = Patient-Reported Outcome Measurement Information System; NIH = National Institutes of Health; Glad to have practiced meditation dichotomous = dichotomized with responses 1 to 3 coded as 0 and 4 to 6 coded as 1
Table 2.
Frequency and duration of specific meditation-related adverse effects
| MRAES-MBP Item | Any | Never | Days to 1 week | 1 week to 1 month | 1 month to 1 year | 1 year+ |
|---|---|---|---|---|---|---|
| 1 | 12.44 | 87.56 | 9.45 | 1.84 | 0.46 | 0.69 |
| 2 | 26.96 | 73.04 | 21.89 | 2.30 | 1.61 | 1.15 |
| 3 | 25.81 | 74.19 | 18.66 | 3.92 | 1.61 | 1.61 |
| 4 | 22.81 | 77.19 | 15.67 | 4.15 | 1.38 | 1.61 |
| 5 | 16.13 | 83.87 | 9.22 | 3.46 | 1.61 | 1.84 |
| 6 | 17.97 | 82.03 | 11.29 | 3.46 | 1.84 | 1.38 |
| 7 | 19.35 | 80.65 | 11.52 | 3.23 | 1.38 | 3.23 |
| 8 | 15.21 | 84.79 | 10.14 | 1.84 | 1.38 | 1.84 |
| 9 | 13.82 | 86.18 | 7.14 | 3.00 | 1.84 | 1.84 |
| 10 | 19.59 | 80.41 | 13.36 | 2.76 | 2.30 | 1.15 |
| 11 | 5.76 | 94.24 | 3.00 | 1.15 | 0.23 | 1.38 |
Note: MRAES-MBP = Meditation-Related Adverse Effects Scale – Mindfulness-Based Program (Britton et al., 2018). MRAES-MBP items assess trouble thinking clearly (Item 1), anxiety (Item 2), traumatic re-experiencing (Item 3), emotional sensitivity (Item 4), trouble enjoying things (Item 5), feeling distant or cut off from others (Item 6), difficulty sleeping (Item 7), experiencing headaches and/or body pain (Item 8), sensitive hearing (Item 9), feeling disconnected from everything (Item 10), and other (Item 11). Values represent percentage of sample. n = 434.
The first item of the three-item scale examined occurrence (“I personally have had challenging, difficult, or distressing experiences as a result of my meditation practice”) with participants indicating frequency (never, rarely, occasionally, regularly, frequently, other). The subsequent two items assessed impairment (“My meditation-related challenging, difficult, or distressing experiences impaired my ability to function,” not at all, somewhat, moderately, severely, other) and duration of impairment (“How long did your impairment last?,” 1 day or less, for a few days to 1 week, 1 week to 1 month, 1 month to 1 year, 1 year or longer, other).
The 11-item Meditation-Related Adverse Effects Scale – Mindfulness-Based Program version (MRAES-MBP; Britton, Lindahl, & Cooper, 2018) was used to assess the occurrence and duration of specific MRAE. This measure was derived from more than 150 qualitative interviews with Buddhist meditators, meditation teachers, and mindfulness-based program participants about distressing and/or impairing meditation-related experiences (Britton et al., in press; Lindahl et al., 2017). Items represented the ten meditation-related experiences that were most highly associated with negative impact in functioning in the context of a mindfulness-based program (e.g., hyperarousal, dissociation, “I felt anxious,” “I had difficulty sleeping,” “I felt distant or cut off from other people”). Specific items were drawn from validated clinical symptom measures (e.g., PROMIS; Cella et al., 2007). Participants were asked, “Have you ever had any of the following occur as a result of meditation?” with response options: never, for a few days to 1 week, 1 week to 1 month, 1 month to 1 year, 1 year or longer. The eleventh item queried the experience of “other significant symptoms” which participants could describe. The frequency of most response options was low (<5%; Table 2), therefore, items were dichotomized for use in analyses. A total score was computed across the 10 specific items. Internal consistency reliability was adequate (Kuder-Richardson = .88).
A final item assessed whether participants’ felt glad to have practiced meditation. Participants were asked to “consider the various experiences you have had through meditation, including any challenging, difficult, or distressing experiences” and then indicate their agreement with the statement “I am glad I have practiced meditation” (response options ranging from strongly disagree to strongly agree on a 6-point Likert-type scale). Responses of 4 or greater (i.e., above midpoint) were interpreted as indicating feeling glad to have practiced meditation.
Data Analysis
Data used in this study are part of a two-part project assessing utilization of meditation practice and MRAE in a population-based sample. Both parts were preregistered separately through the Open Science Framework (https://osf.io/sjmpu, https://osf.io/4h86s/?view_only=0e5d7ad85f87468ea40e047b3cf7c795). Data related to utilization will be published elsewhere. Some response options were simplified for use in the current study. Specifically, we reduced the types of meditation exposure to focus on exposure through smartphone apps, reduced the types of meditation practice to focus on concentration or insight, reduced the types of meditation classes attended to focus on meditation retreats, and restricted the sample to those endorsing at least one of the three NHIS meditation items.
Planned analyses were specified in our preregistration. However, we made three deviations. First, as the three MRAE items assessing occurrence, impairment severity, and duration of impairment showed low frequency of most response options (<5%; Table 2), these items were dichotomized for use in analyses (i.e., yes/no). The responses were simplified to any occurrence of MRAE, any impairment, and duration of impairment lasting longer than one day. Second, we used correlations and partial correlations (controlling for demographics) for characterizing the association between MRAE and other study variables rather than regression models. This was done to aid in interpretation of effect size magnitude. Correlations with dichotomous variables (i.e., point biserial or phi) are simplified cases of Pearson’s product moment correlation (Cohen et al., 2003). Third, we used two-proportions z-tests rather than one sample t-tests for testing the proportion of participants who indicated experiencing MRAE.
In terms of our four a priori hypotheses, we examined whether the proportion of participants reporting MRAE as assessed via the single occurrence item and the MRAES-MBP was higher than 25% using a two-proportions z-test. We also used this test to assess whether the duration of participants’ longest lasting MRAE was one month or longer and whether impairment was reported for more than 5% of participants. We used McNemar’s test for paired nominal data to examine whether anxiety was reported more frequently than other MRAE on the MRAES-MBP. We used correlations and partial correlations that controlled for demographic variables (age, gender, race/ethnicity, education, income) to examine the association between MRAE with early childhood adversity and participants’ ratings of whether they felt glad to have practiced meditation. Separate models were run for each of the four MRAE variables (i.e., single-item any unwanted experiences, MRAES-MBP total score, single-item any impairment, single-item duration of impairment >1 day).
In addition to these a priori hypotheses, we examined the association between several variables with occurrence of MRAE. These included five demographic variables, eight meditation practice-related variables, three psychological constructs (depression, anxiety, loneliness), and social desirability. These analyses were primarily intended to be descriptive. Nonetheless, we controlled for false discovery rate (FDR) using Benjamini and Hochberg’s method given the number of tests conducted. FDR adjustment was applied based on the number of tests for each of the four MRAE variables. Lifetime meditation practice hours had some low frequency response options (<10% for each of the three highest hour amounts), so categories were collapsed for use in correlations (i.e., recoded responses to be 0–10, 11–100, and 101 or more). Lastly, in keeping with our preregistration, models were re-estimated without outliers (i.e., values three standard deviations from the mean).1
Results
Sample descriptive statistics are presented in Table 1. With the exception of social desirability, skewness (range = −0.94 to 1.47) and kurtosis (range = −1.17 to 1.09) for all continuous variables were below the cut-offs for substantial departure from normality (skewness < 2.0, kurtosis < 7.0; Curran et al., 1996).2 Most participants reported lifetime exposure to mindfulness meditation (71.0%) and/or spiritual meditation (53.2%), with 29.2% reporting exposure to mantra meditation. A plurality (41.2%) of participants reported 11–100 hours of meditation practice, with 18.9% reporting 0–10, 16.4% reporting 101–500, 9.0% reporting 501–1000, 7.1% reporting 1001–5000, and 7.4% reporting ≥ 5001 hours. A minority (6.9%) had attended a multiday residential retreat and 65.2% had meditated in the past 30 days.
The percentage of participants reporting MRAE are displayed for the overall sample and separated by lifetime meditation hours in Table 1, Figure 1, and Supplemental Materials Tables 6 and 7. Rates of endorsing either the single occurrence item (32.3%) or at least one items on the MRAES-MBP (50.0%) were higher than our a priori hypothesis of 25% (ps < .001). On the single occurrence item, 19.8% reported MRAE occurred rarely, 8.7% occasionally, 1.8% regularly, and 0.7% frequently. On the MRAES-MBP, participants’ longest-lasting adverse effect lasted for a few days to a week (30.0%), 1 week to 1 month (9.4%), 1 month to 1 year (3.5%), and 1 year or longer (6.5%). The rate of symptom duration lasting one month or longer (10.4%) was higher than our a priori hypothesis of 5% (p < .001).
Figure 1.
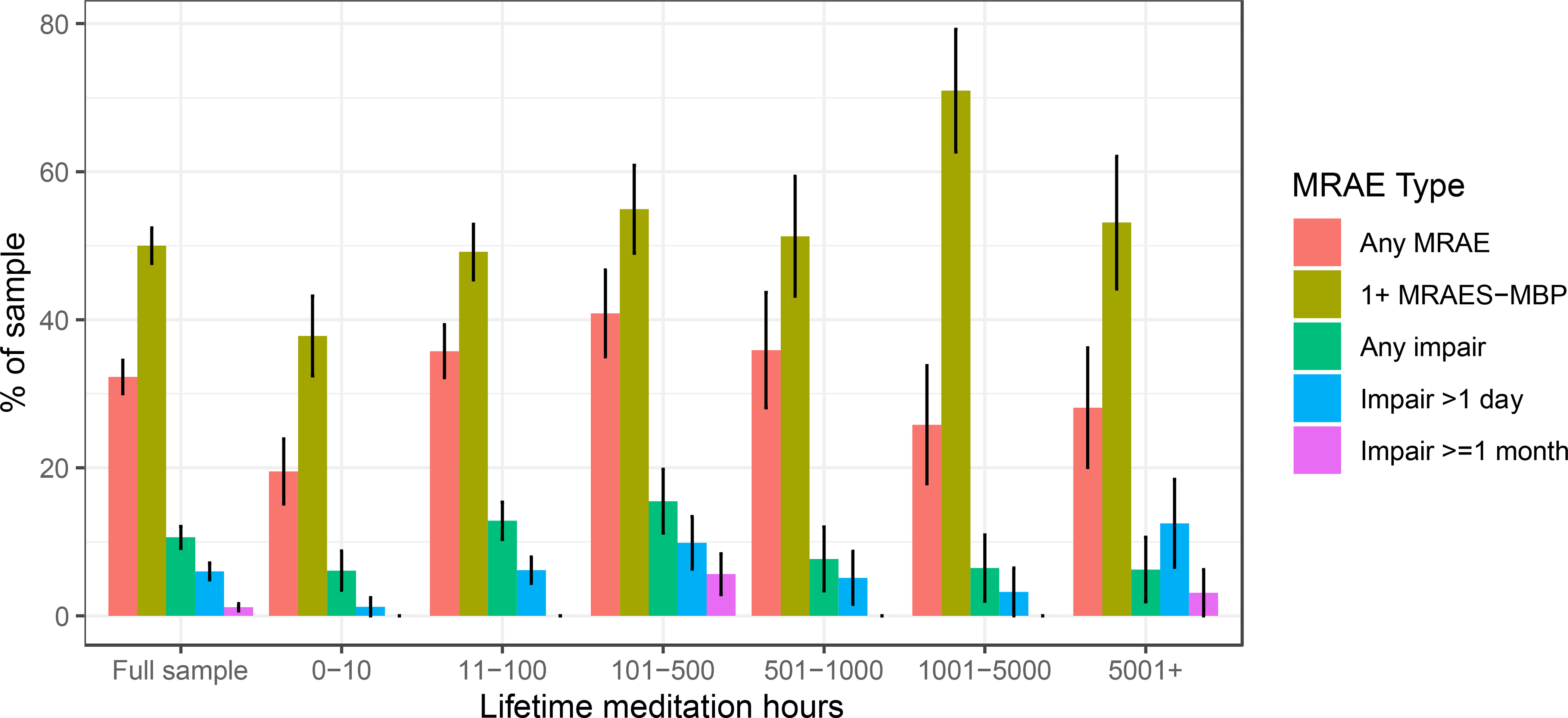
Frequency of meditation-related adverse effects (MRAE) by amount of lifetime meditation practice. MRAE = meditation-related adverse effects; MRAES-MBP = Meditation-Related Adverse Effects Scale – Mindfulness-Based Program (Britton et al., 2018); Impair = impairment. Bars indicate percentage of the sample endorsing any instance of each experience with error bars indicating 95% confidence intervals. See Table 1 and Supplemental Materials Table 6 for these data in tabular format.
Some degree of functional impairment was reported by 10.6% of participants, which was higher than our hypothesized 5% (p < .001). Severity was endorsed as somewhat (7.1%), moderately (2.3%), and severely impairing (0.2%; Supplemental Materials Table 7). Duration of impairment was ≤1 day (7.1%), a few days to 1 week (2.5%), 1 week to 1 month (1.8%), 1 month to 1 year (0.7%), and 1 year or longer (0.5%). When restricted to participants with at least 11–100 hours of practice experience (i.e., similar to what one might have from MBSR or MBCT), 35.2% endorsed the single occurrence item, 52.8% endorsed at least one item on the MRAES-MBP, 11.6% endorsed some degree of functional impairment, and 1.4% endorsed impairment lasting one month or longer. Estimates were also essentially unchanged when excluding 4 participants who were exposed to meditation ≤2 months ago.
Occurrence and duration of specific MRAE assessed via the MRAES-MBP are displayed in Table 2. The most common MRAE were anxiety (27.0%), traumatic re-experiencing (25.8%), and emotional sensitivity (22.8%). As hypothesized, anxiety was more commonly endorsed than most other items (ps < .01), with the exception of traumatic re-experiencing; p = .668) and emotional sensitivity (p = .054). Traumatic re-experiencing was the second most commonly endorsed item and occurred more frequently than all other items (ps < .01) with the exception of anxiety and emotional sensitivity (p = .182).
Results from analyses examining correlates of MRAE are presented in Table 3 and Supplemental Materials Table 8. As hypothesized, participants reporting a greater number of adverse childhood experiences were more likely to report any MRAE (single item occurrence: r = .19, p < .001), a greater number of MRAE (MRAES-MBP total score: r = .19, p < .001), and were more likely to report impairment due to meditation (r = .15, p = .002). Adverse childhood experiences were not associated with a longer duration of impairment (i.e., >1 day; r = .05, p = .323). Significance tests were unchanged when controlling for demographics or applying FDR p-value adjustment.
Table 3.
Correlations between meditation-related adverse effects with demographic, meditation practice, and psychological variables
| Any adverse effect | MRAES-MBP total | Any impairment | Impairment >1 day | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | r | p | p FDR | r | p | p FDR | r | p | p FDR | r | p | p FDR |
| Age | −.12 | .012* | .173 | −.23 | <.001*** | <.001*** | −.11 | .025* | .322 | −.02 | .622 | .999 |
| Male | −.03 | .540 | .999 | .03 | .508 | .999 | −.02 | .746 | .999 | −.07 | .176 | .999 |
| Non-Hispanic White | .02 | .750 | .999 | −.18 | <.001*** | .002** | −.01 | .893 | .999 | −.06 | .194 | .999 |
| Bachelor’s degree | −.07 | .167 | .999 | −.08 | .114 | .999 | −.14 | .004** | .057 | −.05 | .254 | .999 |
| Low income | .10 | .045* | .539 | .07 | .141 | .999 | .18 | <.001*** | .002** | .09 | .050 | .803 |
| Years since first exposure | −.01 | .898 | .999 | −.05 | .313 | .999 | −.01 | .802 | .999 | .04 | .375 | .999 |
| App first exposure | .06 | .184 | .999 | .06 | .251 | .999 | .16 | .001** | .013* | .20 | <.001*** | .001** |
| App ever exposure | .09 | .070 | .715 | .02 | .605 | .999 | .00 | .977 | .999 | .00 | .975 | .999 |
| Any meditation in the past 30 days | .12 | .012* | .173 | .15 | .001** | .020* | .05 | .326 | .999 | .12 | .010* | .183 |
| Lifetime meditation hours continuous | .10 | .041* | .539 | .14 | .004** | .047* | .03 | .479 | .999 | .10 | .038* | .654 |
| Concentration practice | .05 | .267 | .999 | .04 | .462 | .999 | .05 | .345 | .999 | .00 | .967 | .999 |
| Insight practice | .09 | .065 | .715 | .04 | .398 | .999 | .09 | .068 | .678 | −.02 | .744 | .999 |
| Residential retreat | .01 | .896 | .999 | .09 | .062 | .679 | .11 | .019* | .263 | .08 | .079 | .999 |
| PROMIS Depression in the last week | .16 | .001** | .018* | .18 | <.001*** | .004** | .15 | .001** | .022* | .09 | .063 | .952 |
| PROMIS Anxiety in the last week | .15 | .002** | .032* | .14 | .004** | .047* | .10 | .032* | .379 | .08 | .097 | .999 |
| NIH Toolbox Loneliness in the last week | .19 | <.001*** | .001** | .17 | <.001*** | .005** | .10 | .037* | .402 | .06 | .219 | .999 |
| Adverse Childhood Experiences | .19 | <.001*** | .002** | .19 | <.001*** | .001** | .15 | .002** | .031* | .05 | .323 | .999 |
| Socially Desirable Response Set | .03 | .582 | .999 | −.03 | .486 | .999 | .03 | .589 | .999 | −.01 | .893 | .999 |
| Glad to have practiced meditation | −.05 | .283 | .999 | −.02 | .622 | .999 | −.07 | .141 | .999 | .03 | .559 | .999 |
Note: MRAES-MBP = Meditation-Related Adverse Effects Scale – Mindfulness-Based Program; App first exposure = first exposure to meditation through a smartphone app; App ever exposure = ever having been exposed to meditation through a smartphone app; Weekly days of meditation = average days of meditation per week in the past 30 days; Lifetime meditation hours continuous = 0 to 10 (1), 11–100 (2), 101+ (3); PROMIS = Patient-Reported Outcome Measurement Information System; NIH = National Institutes of Health.
In the full sample, 88.7% of participants reported feeling glad to have practiced meditation and 11.3% reported not feeling glad. The proportion feeling glad remained essentially unchanged when restricted to those reporting MRAE on the single item (87.9%) or MRAES-MBP total score ≥1 (88.2%), in all instances representing the majority of the sample (ps < .001). When treated continuously or dichotomously, feeling glad to have practiced meditation was not associated with any of the four MRAE variables (rs = −.07 to .03; ps ≥ .141).
Subsequent analyses examined additional correlates of MRAE. Given the exploratory nature of these analyses, we report unadjusted statistical significance and also note instances in which FDR adjustment or controlling for demographic variables modified statistical significance. First, demographic variables were examined. Higher age was negatively associated with likelihood of MRAE (single item occurrence, MRAES-MBP total; rs = −.12 and −.23, respectively) and with likelihood of impairment (r = −.11), although the latter association did not survive FDR or demographic adjustment. Non-Hispanic White participants reported fewer MRAE (r = −.18), with this result persisting after controlling for other demographic variables (i.e., age, gender, education, income; r = −.13). Having a college education was associated with lower likelihood of impairment (r = −.14), although this association did not survive FDR adjustment.
Next, several meditation-related variables were examined. Initial exposure to meditation through a smartphone app was not associated with greater likelihood of MRAE (single item occurrence, MRAES-MBP total score; rs = .06). However, initial exposure through a smartphone app was associated with greater likelihood of impairment (r = .16) and impairment lasting longer than a day (r = .20), with results unchanged applying FDR adjustment or controlling for demographic variables (including age). Lifetime exposure through a smartphone app was not associated with any of the four MRAE variables. Any meditation practice in the past 30 days was associated with greater likelihood of MRAE (single item occurrence; r = .12), greater number of MRAE (MRAES-MBP total score; r = .15), and greater likelihood of impairment lasting >1 day (r = .12), although the associations with single item occurrence and impairment lasting >1 day did not survive FDR adjustment. Greater lifetime hours of practice was associated with a greater likelihood of MRAE (single item occurrence; r = .10), greater number of MRAE (MRAES-MBP total score; r = .14), and greater likelihood of impairment lasting >1 day (r = .10), although the associations with single item occurrence and impairment lasting >1 day did not survive FDR adjustment. Lifetime concentration and lifetime insight practice were not associated with MRAE. Having attended a meditation retreat was associated with greater likelihood of impairment (r = .11), although this association did not survive FDR adjustment.
Next, we examined associations with depression, anxiety, and loneliness. Higher depression was associated with greater likelihood of MRAE (single item occurrence, MRAES-MBP total score; rs = .16 and .18, respectively) and greater likelihood of impairment (r = .15), although the association with impairment did not survive demographic adjustment. Higher anxiety was associated with greater likelihood of MRAE (single item occurrence, MRAES-MBP total score; rs = .15 and .14, respectively) and greater likelihood of impairment (r = .10), although the associations with likelihood of impairment did not survive demographic or FDR adjustment and the association with MRAES-MBP total score did not survive demographic adjustment. Higher loneliness was associated with greater likelihood of MRAE (single item occurrence, MRAES-MBP total score; rs = .19 and .17, respectively) and greater likelihood of impairment (r = .10), although the latter association did not survive demographic or FDR adjustment. Lastly, none of the four MRAE variables were associated with social desirability.
Discussion
We conducted what we believe to be the first population-based survey study assessing the prevalence of a broad range of adverse effects associated with meditation practice. It is vital to understand risks of meditation practice as it is incorporated into psychological treatments (e.g., National Institute for Health Care Excellence, 2009), prevention programs (van de Weijer-Bergsma et al., 2014), and is increasingly offered in various secular settings (e.g., education, business; Van Dam et al., 2018; Zoogman et al., 2015). Consistent with prior evaluations, our results provide clear evidence that meditation commonly results in adverse effects. Half of participants reported at least one clinically relevant symptom, with anxiety, traumatic re-experiencing, and emotional sensitivity appearing most commonly. MRAE reported ranged in duration. The most common duration for participants’ longest-lasting adverse effect was a few days to a week (30.0%), although the frequency of our a priori definition of “persistent” (i.e., ≥1 month) was higher (10.4%) than our prediction (5%).
Functional impairment was reported by 10.6% of participants, which was higher than our prediction (5%). Impairment varied in severity (7.1% somewhat, 2.3% moderately, 0.2% severely impairing). Impairment that lasted a day or less was reported by 7.1% of participants and impairment lasting longer than a day occurred for 6% of the sample. Impairment lasting 1 month or longer occurred for 1.2% of participants.
Given meditation is associated with adverse effects, one may reasonably ask whether those experiencing negative consequences feel less glad to have practiced meditation (i.e., regret practicing meditation). We did not find evidence this is the case. The proportion of participants endorsing feeling glad to have practiced meditation (88.7%) was essentially unchanged when restricted to those reporting MRAE (87.9% to 88.2%). Feeling glad to have meditated was also not associated with MRAE when treated continuously.
Feeling glad to have practiced meditation despite MRAE supports the possibility that these experiences do not deter continued practice (Anderson et al., 2019; Cebolla et al., 2017). Consistent with this, we found evidence that participants with more meditation practice experience, whether current or previous, were more likely to report MRAE. Several previous studies have also found that meditation-related challenges are more likely with more practice amount or intensity (Britton et al., 2014; Britton et al., 2019; Britton et al., in press; Lindahl et al., 2017; Schlosser et al., 2019). There are several possible explanations for this. One possibility is that meditating more increases the opportunity for MRAE to occur (i.e., a “biological gradient” or dose-response; Hill, 2015). It is also possible that participants are practicing more because of the MRAE. Such a possibility aligns with accounts from long-term meditation practitioners who were instructed to respond to challenging meditation experiences with more meditation (Lindahl et al., 2017; Lindahl & Britton, 2019; Lindahl et al., 2020). Alternatively, it may also be that MRAE are, at least for some, a part of the meditative process. Some level of discomfort may accompany both healing and meditative insights (Lindahl et al., 2017). Importantly, descriptions of the meditative path in early Buddhist accounts (i.e., Pali canon) clearly indicate that practice can be but is not necessarily painful (e.g., Anguttara Nikaya 4.162; Bodhi, 2012). Thus, it is important to avoid both the no pain, no gain fallacy (i.e., “worsening is to be expected and is a positive sign that therapy is working,” Hannan et al., 2005, p. 156) as well as the conclusion that MRAE are necessarily harmful (i.e., pain always means harm). The fact that participants reporting lifetime MRAEs were more likely to report elevated past week depression and anxiety symptoms supports the notion that MRAEs do not lead to decreased symptoms, although we did not assess symptoms prior to the MRAEs (i.e., did not assess change) and, as discussed below, establishing causality in cross-sectional data is generally not possible. Ultimately, instead of attempting to make global appraisals for all meditators, it may be more fruitful to consider multiple contextual and person-centered factors involved in the occurrence and appraisal of MRAEs (Lindahl et al., 2019). Careful future research is required to determine when MRAE are entirely harmful or if there are circumstances or types of MRAE that may ultimately lead to benefit. Longitudinal studies in particular could examine if, when, and for whom MRAEs may be linked with later benefits, deteriorations, or no change in outcome.
Results from correlational analyses provide preliminary indications regarding whom may be at elevated risk for MRAE. As hypothesized, adverse childhood experiences (ACEs) were associated with increased occurrence of MRAE. This may be due to a greater vulnerability to distress associated with childhood adversity (Weems et al., in press). This also highlights the need for increasing trauma-sensitivity within meditation-based interventions (Treleaven, 2018).
In exploratory analyses, symptoms of depression, anxiety, and loneliness in the past week were positively correlated with lifetime occurrence of MRAE. The correlational nature of our data and assessment of current psychiatric symptoms and loneliness makes it impossible to determine the direction of causality. Given the temporal ordering of measurement, it is possible that the causal direction flows from MRAE to increased depression, anxiety, and loneliness. Conversely, if depression, anxiety, and loneliness in the last week can be taken to reflect a more general psychological vulnerability or trait proneness to negative affect (i.e., higher neuroticism), then individuals with these symptoms may find that negatively valenced experiences also arise within the context of meditation. Should this turn out to be the case, it may be prudent to warn individuals experiencing depression, anxiety, and loneliness that meditation may result in MRAE including impairment.
We also found some evidence that younger participants and those from marginalized populations (racial/ethnic minority, without a bachelor’s degree, low income) may be more likely to report MRAE, highlighting the need for increased cultural sensitivity and potential cultural adaptation to increase participant safety (Biggers et al., 2020). Lastly, the only predictor of sustained impairment (>1 day) that survived FDR correction was first exposure through a smartphone app. Due to the exploratory nature of this analysis, the small portion of the sample being initially exposed this way (n = 17), and the recent advent of smartphone apps, this must be interpreted cautiously. However, given the popularity of meditation apps (Wasil et al., 2020), research seeking to more deeply understand potential risks associated with first being exposed in this way is warranted. Available evidence from randomized controlled trials does not indicate that smartphone-based meditation interventions increase risk for harm but may, like in-person meditation training, actually reduce the risk of certain types of harm (e.g., target symptom worsening) relative to a waitlist control (Goldberg et al., 2020). Indeed, the social dimensions of standard in-person, group-based meditation-based interventions, such as the teacher and meditation community, have been found to be associated with the magnitude of benefits and risks (Canby et al., 2021; Lindahl et al., 2017)
Limitations and Future Directions
Although the first population-based survey focused on MRAE, our study has important limitations. Sample demographic characteristics did not perfectly align with current demographics in the US, which raises questions of generalizability. This issue is compounded by the loss of participants during the follow-up survey, especially racial/ethnic minority participants. Relatedly, although crowdsourcing has been shown to have methodological benefits over convenience sampling (e.g., undergraduates; Behrend et al., 2011), our sample was necessarily restricted (e.g., to Internet users) and may differ from the general population in various unmeasured ways. Our sample also reported relatively few hours of meditation practice and limited retreat experience, which makes it difficult to evaluate MRAE occurring in more intensive training. This also makes comparisons with samples including more experienced practitioners (e.g., Schlosser et al., 2019) tenuous. As noted, the correlational nature of our data makes it impossible to infer causality. Also, many of the analyses we conducted were exploratory. While these were intended to be primarily descriptive in nature and applied a p-value correction, it is still likely that some of the observed associations occurred merely by chance alone. Correlations were also modest in magnitude (rs < .30), highlighting that the vast majority of variance in MRAE remains unexplained at least by individual predictors. Lastly, although we attempted a multidimensional assessment of MRAE, different estimates of prevalence rates may have resulted from the use of other measures.
These limitations notwithstanding, there are several implications of this study. Given the rapidly growing popularity of meditation (Clarke et al., 2018), it is important for those offering or promoting meditation practice to be educated and transparent about the possibility of MRAE. Teachers, clinicians, researchers, and product developers involved with meditation must collectively work to avoid a pollyannaish depiction of the practice experience as uniformly pleasant or beneficial. It is also important to acknowledge that harm occurs, and some individuals experience sustained deterioration as a result of meditation. At once, adverse effects and benefits can (and likely do) co-occur. Thus, providers and potential consumers must weigh the risk of MRAE relative to the potential benefit meditation might provide and the opportunity cost associated with not engaging in meditation. As research in this area matures, it will be important to compare prevalence and type of adverse effects occurring in meditation-based interventions to similarly intensive psychological treatments (e.g., psychotherapy) and control conditions, using both randomized and observational designs and with sensitivity to individual differences which may moderate occurrence of MRAE. It will be results from these studies that allow clear estimation of potential costs and benefits of engaging in meditation training (e.g., evaluation of the degree to which meditation practice increases risk for adverse effects beyond what may occur in the absence of practice; Hirshberg et al., 2020). Until such data are available, it is quite difficult (and potentially misleading) to make direct comparisons between risk for adverse effects associated with meditation practice and risks associated with other psychological interventions.
As noted, it is crucial that future studies deepen our understanding of the participant-, provider-, and intervention-level factors that increase risk for MRAE and evaluate methods for reducing this risk. Both qualitative and quantitative designs could be used to further evaluate candidate factors identified in the current study such as a history of childhood adversity, symptoms of depression and anxiety, loneliness, and racial/ethnic minority status. A clearer understanding of precisely how and why MRAE may occur for certain individuals can help guide the development of meditation-based interventions, teacher training, and delivery formats that minimize risk. More consistent measurement and reporting of MRAE is also essential (Baer et al., 2019; Britton et al., in press). This may require validation of instruments specifically designed to assess MRAE, although widespread adoption of other standardized metrics (e.g., clinically significant deterioration) will also be valuable, particularly to allow comparisons with the broader psychotherapy literature. Our results join other recent evaluations (Britton et al., in press) suggesting that items querying specific potential MRAE (e.g., via the MRAES-MBP; Britton et al., 2018) may be more sensitive to detection of a broad range of MRAE than more general items. The accumulation of accurate information regarding the likelihood of various outcomes can allow individuals considering these approaches to decide for themselves whether potential benefits outweigh the associated risk.
Supplementary Material
Clinical or Methodological Significance.
Using a broad definition of adverse effects, this study suggests that many individuals experience adverse effects when practicing meditation, even in relatively modest amounts. Factors that may increase risk include both person-related (childhood adversity) and practice-related variables (amount of meditation). More systematic evaluation of prevalence and predictors of adverse effects associated with meditation training can help providers and consumers accurately evaluate potential costs and benefits.
Acknowledgments
We include data from an online survey study that was preregistered at the Open Science Framework (https://osf.io/sjmpu). Data are available by request. This research was supported by the National Center for Complementary and Integrative Health Grant K23AT010879 (Simon B. Goldberg), the National Institute of Mental Health Grant R01MH43454 (Richard J. Davidson), the Clinical and Translational Science Award program through the NIH National Center for Advancing Translational Sciences Grant UL1TR002373, by the University of Wisconsin - Madison Office of the Vice Chancellor for Research and Graduate Education with funding from the Wisconsin Alumni Research Foundation (Simon B. Goldberg), and with funding from the Wisconsin Center for Education Research (Simon B. Goldberg). Richard J. Davidson is the founder, president, and serves on the board of directors for the nonprofit organization, Healthy Minds Innovations, Inc. We are grateful to Shiri Raphaely for comments on an earlier draft of this manuscript.
Footnotes
Four continuous variables had outliers: years since first exposure (n = 3), ACE score (n = 2), social desirability (n = 8), and feeling glad to have practiced meditation (n = 3). Significance tests of associations with adverse effects were unchanged with these responses removed.
Due to the departure from normality, we also examined results with a dichotomized social desirability variable (i.e., social desirability > 0 = 1). Significance tests of associations with adverse effects were unchanged when social desirability was dichotomized.
References
- Anderson T, Suresh M, & Farb NA (2019). Meditation benefits and drawbacks: empirical codebook and implications for teaching. Journal of Cognitive Enhancement, 3(2), 207–220. [Google Scholar]
- Baer R, Crane C, Miller E, & Kuyken W (2019). Doing no harm in mindfulness-based programs: conceptual issues and empirical findings. Clinical Psychology Review, 71, 101–114. doi: 10.1016/j.cpr.2019.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer R, Crane C, Montero-Marin J, Phillips A, Taylor L, Tickell A, & Kuyken W (2020). Frequency of self-reported unpleasant events and harm in a mindfulness-based program in two general population samples. Mindfulness, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behrend TS, Sharek DJ, Meade AW, & Wiebe EN (2011). The viability of crowdsourcing for survey research. Behavior Research Methods, 43(3), 800–813. [DOI] [PubMed] [Google Scholar]
- Bergin AE (1966). Some implications of psychotherapy research for therapeutic practice. Journal of Abnormal Psychology, 71(4), 235–246. 10.1037/h0023577 [DOI] [PubMed] [Google Scholar]
- Biggers A, Spears CA, Sanders K, Ong J, Sharp LK, & Gerber BS (2020). Promoting Mindfulness in African American Communities. Mindfulness, 11(10), 2274–2282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodhi B (2012). The numerical discourses of the Buddha: A translation of the Anguttara Nikaya. Somerville, MA: Wisdom Publications. [Google Scholar]
- Britton WB (2019). Can mindfulness be too much of a good thing? The value of a middle way. Current Opinion in Psychology, 28, 159–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton WB, Lindahl JR, Cahn BR, Davis JH, & Goldman RE (2014). Awakening is not a metaphor: The effects of Buddhist meditation practices on basic wakefulness. Annals of the New York Academy of Sciences, 1307, 64–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton WB, Lindahl JR, & Cooper DJ (2018). Meditation-Related Adverse Effects Scale, Mindfulness-Based Program version (MRAES-MBP). Brown University. [Google Scholar]
- Britton WB, Lindahl JR, Cooper DJ, Canby NK, & Palitsky R (in press). Defining and measuring meditation-related adverse effects in mindfulness-based programs. Clinical Psychological Science. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canby NK, Eichel K, Lindahl J, Chau S, Cordova J, & Britton W (2020). The Contribution of Common and Specific Therapeutic Factors to Mindfulness-Based Intervention Outcomes. Frontiers in Psychology, 11, 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cebolla A, Demarzo M, Martins P, Soler J, & Garcia-Campayo J (2017). Unwanted effects: Is there a negative side of meditation? A multicentre survey. PLOS ONE, 12(9), e0183137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, ... & Rose M (2007). The Patient-Reported Outcomes Measurement Information System (PROMIS): Progress of an NIH Roadmap cooperative group during its first two years. Medical Care, 45(5 Suppl 1), S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (n. d.). National Health Interview Survey. https://www.cdc.gov/nchs/nhis/index.htm
- Clarke TC, Barnes PM, Black LI, Stussman BJ, & Nahin RL (2018). Use of yoga, meditation, and chiropractors among U.S. adults aged 18 and over. Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, & Aiken LS (2003). Applied multiple regression / correlation analysis for the behavioral sciences (3rd ed.). Mahwah, New Jersey: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Curran PJ, West SG, & Finch JF (1996). The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychological Methods, 1(1), 16–29. [Google Scholar]
- Cyranowski JM, Zill N, Bode R, Butt Z, Kelly MA, Pilkonis PA, ... & Cella D (2013). Assessing social support, companionship, and distress: National Institute of Health (NIH) Toolbox Adult Social Relationship Scales. Health Psychology, 32(3), 293–301. doi: 10.1037/a0028586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimidjian S, & Hollon SD (2010). How would we know if psychotherapy was harmful? American Psychologist, 65, 21–33. [DOI] [PubMed] [Google Scholar]
- Dobkin PL, Irving JA, & Amar S (2012). For whom may participation in a mindfulness-based stress reduction program be contraindicated?. Mindfulness, 3(1), 44–50. [Google Scholar]
- Duggan C, Parry G, McMurran M, Davidson K, & Dennis J (2014). The recording of adverse events from psychological treatments in clinical trials: evidence from a review of NIHR-funded trials. Trials, 15(1), 335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunning DL, Griffiths K, Kuyken W, Crane C, Foulkes L, Parker J, & Dalgleish T (2019). The effects of mindfulness-based interventions on cognition and mental health in children and adolescents–a meta-analysis of randomized controlled trials. Journal of Child Psychology and Psychiatry, 60(3), 244–258. doi: 10.1111/jcpp.12980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farias M, Maraldi E, Wallenkampf KC, & Lucchetti G (2020). Adverse events in meditation practices and meditation-based therapies: a systematic review. Acta Psychiatrica Scandinavica, 142(5), 374–393. [DOI] [PubMed] [Google Scholar]
- Ford DC, Merrick MT, Parks SE, Breiding MJ, Gilbert LK, Edwards VJ, ... & Thompson WW (2014). Examination of the factorial structure of adverse childhood experiences and recommendations for three subscale scores. Psychology of Violence, 4(4), 432–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa TA, Noma H, Caldwell DM, Honyashiki M, Shinohara K, Imai H, ... & Churchill R (2014). Waiting list may be a nocebo condition in psychotherapy trials: A contribution from network meta-analysis. Acta Psychiatrica Scandinavica, 130(3), 181–192. [DOI] [PubMed] [Google Scholar]
- Goldberg SB, Tucker RP, Greene PA, Davidson RJ, Wampold BE, Kearney DJ, & Simpson TL (2018). Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical Psychology Review, 59, 52–60. doi: 10.1016/j.cpr.2017.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Imhoff-Smith T, Bolt DM, Wilson-Mendenhall CD, Dahl CJ, Davidson RJ, & Rosenkranz MA (2020). Testing a multi-component, self-guided, smartphone-based meditation app: three-armed randomized controlled trial. JMIR Mental Health, 7(11), e23825. doi: 10.2196/23825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Riordan K, Sun S, & Davidson RJ (in press). The empirical status of mindfulness-based interventions: A systematic review of 44 meta-analyses of randomized controlled trials. Perspectives on Psychological Science. doi: 10.1177/1745691620968771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddad PM, & Sharma SG (2007). Adverse effects of atypical antipsychotics. CNS Drugs, 21(11), 911–936. [DOI] [PubMed] [Google Scholar]
- Hansen NB, Lambert MJ, & Forman EM (2002). The psychotherapy dose-response effect and its implications for treatment delivery services. Clinical Psychology: Science and Practice, 9, 329–343. [Google Scholar]
- Hays RD, Hayashi T, & Stewart AL (1989). A five-item measure of socially desirable response set. Educational and Psychological Measurement, 49(3), 629–636. [Google Scholar]
- Hill AB (1965). The environment and disease: Association or causation? Proceedings of the Royal Society of Medicine, 58(5), 295–300. [PMC free article] [PubMed] [Google Scholar]
- Hirshberg MJ, Goldberg S, Rosenkranz MA, & Davidson RJ (2020). Prevalence of harm in Mindfulness-Based Stress Reduction. Psychological Medicine. doi: 10.1017/S0033291720002834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonsson U, Alaie I, Parling T, & Arnberg FK (2014). Reporting of harms in randomized controlled trials of psychological interventions for mental and behavioral disorders: A review of current practice. Contemporary Clinical Trials, 38(1), 1–8. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J (2013). Full catastrophe living: How to cope with stress, pain and illness using mindfulness meditation (Revised ed.). London: Piatkus. [Google Scholar]
- Kuyken W, Warren FC, Taylor RS, Whalley B, Crane C, Bondolfi G,...& Dalgeish T (2016). Efficacy of mindfulness-based cognitive therapy in prevention of depressive relapse: An individual patient data meta-analysis from randomized trials. JAMA Psychiatry, 73(6), 565–574. doi: 10.1001/jamapsychiatry.2016.0076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lilienfeld SO (2007). Psychological treatments that cause harm. Perspectives on Psychological Science, 2(1), 53–70. [DOI] [PubMed] [Google Scholar]
- Lindahl JR, & Britton WB (2019). ‘I have this feeling of not really being here’: Buddhist meditation and changes in sense of self. Journal of Consciousness Studies, 26, 157–183. [Google Scholar]
- Lindahl JR, Britton WB, Cooper D, and Kirmayer LJ, (2019). Challenging and Adverse Meditation Experiences: Toward A Person-Centered Approach. In Farias M, Brazier D, and Laljee M, Eds). The Oxford Handbook of Meditation. Oxford University Press. doi: 10.1093/oxfordhb/9780198808640.013.51 [DOI] [Google Scholar]
- Lindahl JR, Cooper DJ, Fisher NE, Kirmayer LJ, and Britton WB (2020). Progress or pathology? Differential diagnosis and intervention criteria for meditation-related challenges: Perspectives from Buddhist meditation teachers and practitioners. Frontiers in Psychology, 11, 1–18. doi: 10.3389/fpsyg.2020.01905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindahl JR, Fisher NE, Cooper DJ, Rosen RK, & Britton WB (2017). The varieties of contemplative experience: A mixed-methods study of meditation-related challenges in Western Buddhists. PLOS ONE, 12(5), e0176239. doi: 10.1371/journal.pone.0176239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden M (2013). How to define, find and classify side effects in psychotherapy: from unwanted events to adverse treatment reactions. Clinical Psychology & Psychotherapy, 20(4), 286–296. [DOI] [PubMed] [Google Scholar]
- Linden M, & Schermuly-Haupt ML (2014). Definition, assessment and rate of psychotherapy side effects. World Psychiatry, 13(3), 306–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munder T, Flückiger C, Leichsenring F, Abbass AA, Hilsenroth MJ, Luyten P, ... & Wampold BE (2019). Is psychotherapy effective? A re-analysis of treatments for depression. Epidemiology and Psychiatric Sciences, 28(3), 268–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (NICE). (2009). Depression in adults: Recognition and management. Retrieved from: https://www.nice.org.uk/guidance/cg90 [PubMed]
- Peer E, Brandimarte L, Samat S, & Acquisti A (2017). Beyond the Turk: Alternative platforms for crowdsourcing behavioral research. Journal of Experimental Social Psychology, 70, 153–163. [Google Scholar]
- Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D, & PROMIS Cooperative Group. (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS): Depression, anxiety, and anger. Assessment, 18(3), 263–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prolific.co (n. d.). Representative samples FAQ. https://researcher-help.prolific.co/hc/en-gb/articles/360019238413-Representative-Samples-FAQ
- Sayadaw M (2016). Manual of insight. Somerville, MA: Wisdom Publications. [Google Scholar]
- Schlosser M, Sparby T, Vörös S, Jones R, & Marchant NL (2019). Unpleasant meditation-related experiences in regular meditators: Prevalence, predictors, and conceptual considerations. PLOS ONE, 14(5), e0216643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, & Teasdale JD (2013). Mindfulness-based cognitive therapy for depression (2nd. ed). New York: Guilford Press. [Google Scholar]
- Treleaven DA (2018). Trauma-sensitive mindfulness: Practices for safe and transformative healing. New York: W.W. Norton & Company. [Google Scholar]
- United States Census Bureau (2019). United States Census Quick Facts, 2018. https://www.census.gov/quickfacts/fact/table/US/PST045219
- Van Dam NT, van Vugt MK, Vago DR, Schmalzl L, Saron CD, Olendzki A, ... & Meyer DE (2018). Mind the hype: A critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspectives on Psychological Science, 13(1), 36–61. doi: 10.1177/1745691617709589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Weijer-Bergsma E, Langenberg G, Brandsma R, Oort FJ, & Bögels SM (2014). The effectiveness of a school-based mindfulness training as a program to prevent stress in elementary school children. Mindfulness, 5(3), 238–248. [Google Scholar]
- Vieten C, Wahbeh H, Cahn BR, MacLean K, Estrada M, Mills P, ... & Delorme A (2018). Future directions in meditation research: Recommendations for expanding the field of contemplative science. PLOS ONE, 13(11), e0205740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasil AR, Gillespie S, Patel R, Petre A, Venturo-Conerly KE, Shingleton RM, ... & DeRubeis RJ (2020). Reassessing evidence-based content in popular smartphone apps for depression and anxiety: Developing and applying user-adjusted analyses. Journal of Consulting and Clinical Psychology, 88(11), 983. [DOI] [PubMed] [Google Scholar]
- Weems CF, Russell DJ, Herringa RJ, & Carrion VG (in press). Translating the neuroscience of adverse childhood experiences to inform policy and foster population level resilience. American Psychologist. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong SY, Chan JY, Zhang D, Lee EK, & Tsoi KK (2018). The safety of mindfulness-based interventions: A systematic review of randomized controlled trials. Mindfulness, 9(5), 1344–1357. [Google Scholar]
- World Health Organization. (2010). Conceptual Framework for the International Classification for Patient Safety. Geneva: World Health Organization. [Google Scholar]
- Zoogman S, Goldberg SB, Hoyt WT, & Miller L (2015). Mindfulness interventions with youth: A meta-analysis. Mindfulness, 6, 290–302. doi: 10.1007/s12671-013-0260-4 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


