Abstract
Background
Psychosis is associated with many forms of adversity, deprivation and living in urban areas.
Aims
To investigate whether psychosis is part of a syndemic of multiple adversities.
Method
Drawing on UK Biobank (UKBB) data (Project ID: 57601), we sought to understand mechanisms by which childhood, recent/contemporary and place-based adversities might cluster and interact to be implicated in pathways by which psychoses evolve. We investigated the associations between adversities, potential mediating inflammatory markers and ICD-10 diagnoses (F20–F31) of psychotic disorders. We fitted logistic regression models initially including all relevant candidate variables and used backwards deletion to retain theoretically plausible and statistically significant (P < 0.05) associations with psychotic disorders. The candidate variables were entered in a partial least squares structural equation model (PLS-SEM) to test for syndemic interactions between risk factors. We tested whether the findings were sensitive to demographics, gender and ethnicity.
Results
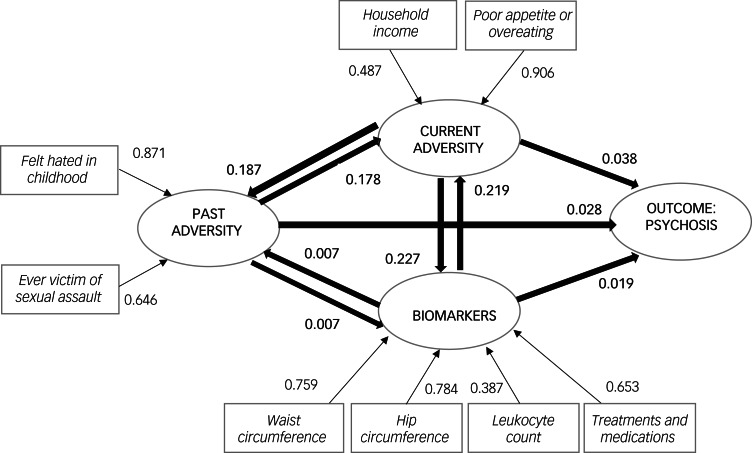
We fitted a PLS-SEM including psychosis as a syndemic outcome, and identified three latent constructs: lifetime adversity, current adversity and biomarkers. Factor loadings were above 0.30, and all structural paths were significant (P < 0.05). There were moderate associations between lifetime adversity and current adversity (standardised coefficient s.c. = 0.178) and between current adversity and biomarkers (s.c. = 0.227). All three latent constructs showed small but significant associations with psychosis (s.c. < 0.04). Lifetime adversity and current adversity were more strongly associated among ethnic minorities (combined) than White British people.
Conclusions
Our findings stress the importance of interactions between childhood and contemporary adversities in preventive and therapeutic interventions for psychotic disorders, especially among ethnic minorities.
Keywords: Psychosis, syndemic, inflammation, adversity, social deprivation
Psychoses
Psychosis is a severe mental illness with a multifactorial aetiology. Psychosis has an incidence of around 1% in the population, and this is higher among Black, Asian and ethnic minorities, and in migrant populations and urban settings.1–3 People from lower socioeconomic and ethnic minority backgrounds typically experience a higher number of negative life events, more ‘generic life stressors’ of modern life (e.g. occupational, financial, relational) and greater psychological distress.4–9 Some evidence8,10–12 suggests that psychological distress stems from comparatively limited access to resources for coping, whether socioeconomic, intrapersonal, interpersonal or more place-based factors (e.g. ethnic density and related support) that might buffer the effects of deprivation.13 Disproportionate exposure to stressors, adversity and trauma may explain the higher incidence of psychosis in ethnic minorities.14,15 Little research investigates mechanisms by which adversity, discrimination and racism, for example, lead to poor health outcomes.16,17
Childhood adversity, such as abuse and parental death, has been consistently shown to double the odds of developing psychosis.18 Adversities can result in over-utilisation and depletion of limited resources (personal, family, and community assets) to tackle chronic stress and in the use of alternative and potentially unhelpful health behaviours (e.g. alcohol, drugs or cigarette smoking); the cumulative effects can trigger dysregulation of biological endocrine and inflammatory responses.5,19 Childhood trauma and adversity can lead to elevated inflammation, which is implicated in the aetiology of mental disorders.20–22 Inflammation is a potential mechanism by which psychoses may emerge.23,24 Thus, adverse childhood experiences may be driving higher risks of pronounced inflammation, related cognitive impacts and greater risks of psychosis and poor outcomes.22,25,26
This biosocial strain, or ‘allostatic load’, leads to weathering, premature ageing and chronic illness.5 A growing body of research suggests that adversity also leads to physical multimorbidity in psychosis.27 Yet, the precise nature and balance of influences from adverse childhood trauma, deprivation, unemployment, poor housing, negative health behaviours (alcohol intake, unhealthy diet) and inflammation remain uncertain. Emerging research on ‘syndemics’ offers a helpful theoretical framework to link these diverse influences, including the role of racism and ethnic discrimination.
Syndemics
The term ‘syndemic’ was introduced by Singer in 199628 to outline synergistically related epidemics that cluster in places and in people, with the interaction of adverse socioenvironmental contexts and risks. The concept of a ‘syndemic’ is different from conceptualisations of comorbidity or multimorbidity, in which diseases coincidentally occur together rather than sharing fundamental causes that reinforce each other. There are similarities with ecosocial and sociodevelopmental models of poor health and psychoses respectively.29–31 The first syndemic described by Singer in 199628,32 showed linkages between substance misuse, violence and AIDS among people living in low-income urban environments. This first confirmed syndemic explained complex causation of multiple diseases through social and structural conditions such as poverty, marginalisation, gender inequality, malnutrition and stigma.29 Since then, the number of proposed syndemics has expanded32 to include mental health outcomes such as depression. For example, studies of Mexican immigrant women in the USA show linkages between violence, immigration, depression, type 2 diabetes and abuse.33 More recently, studies of ethnicity and psychosis propose that ethnic disparities may be better understood and tackled as a syndemic.13
Investigations of syndemics of psychosis are warranted, particularly in light of the recent realisation and intensified UK policy agenda34 of tackling the stark social, health, racial and spatial inequalities in the incidence, care and outcomes, including premature mortality, among people living with psychosis.35,36 We propose that a deeper understanding of the complex social, health, racial and spatial factors that drive health inequalities may be best understood through a ‘syndemic’ lens, followed by commensurate integrated care and policy.
This paper tests the complex interplay of risk factors such as psychosocial adversity (including adverse childhood experiences and discrimination, deprivation and demographics), inflammatory processes and psychoses. We also investigate whether the potential mechanisms in this interplay of influences might be relevant in explaining a higher risk of psychosis in ethnic minorities using a syndemic framework.
Method
The UKBB data-set
We used data from the UK Biobank (UKBB) (Project ID: 57601). This is an ongoing cohort collecting information about a range of background and health-related variables among more than 500 000 participants aged 40–69 years, recruited between 2006 and 2010.37 In accord with UKBB policies, any participants who subsequently withdrew were removed from our analyses.
We derived a dichotomous measure of psychosis meaning at least one ICD-10 diagnosis between F20 and F31; we derived subcategories of psychosis (i.e. non-affective: F20–29; affective: F30–31). These diagnoses were made for the majority on entry or at one of the follow-up interviews in UKBB (see https://biobank.ndph.ox.ac.uk/showcase/label.cgi?id=1712, and their timing). We used the variables from reporting sources consisting of ‘death register only’, ‘death register and other sources’, ‘primary care only’, ‘primary care and other source(s)’, ‘hospital admissions data only’, ‘hospital admissions data and other source(s)’, ‘self-report only’, ‘self-report and other source(s)’, as these options were mutually exclusive for each individual code. We assessed completion rates of relevant independent variables identified from previous syndemic models38,39 and in particular Beckie's heuristic model of allostatic load, health and health disparities.5
Selected variables
Lifetime adversity (individual)
This was assessed using self-report items covering childhood adverse experiences (ACEs), intimate partner violence, sexual violence and war experience. The specific items were:
felt hated by family member as a child
felt loved by family member as a child (reverse coded)
had someone to take them to a doctor when needed as a child (reverse coded)
physically abused as a child
sexually assaulted as a child
ever victim of physically violent crime
ever witnessed sudden violent death
ever victim of sexual assault
ever belittled by partner or ex-partner
ever experienced physical violence by partner or ex-partner
ever experienced sexual interference without consent
ever been exposed to combat or war.
Current adversity (individual/household)
Average total household income before tax (self-reported ordinal variable captured at baseline ranging from ‘less than £18 000’ to ‘greater than £100 000’: we reverse coded this for lower income categories to correspond to higher scores on the scale and therefore deprivation consistent with the direction of other variables)
Member of leisure/social group (also reverse coded and self-reported at baseline)
Age at recruitment (continuous based on date of birth)
Felt very upset when reminded of stressful experience in past month (self-reported ordinal variable in online follow-up).
Current adversity (area-based)
Townsend deprivation index (ordinal variable ranging in UKBB from −6.25826 to 11.0013; higher scores mean more deprivation, relating the participant's postcode at baseline to: the proportion not owning a car, in overcrowded accommodation, not owner–occupier and unemployed).
Risky health behaviours
Alcohol intake frequency (self-reported ordinal at baseline depending on frequency per day/week/month, reverse coded for higher frequency, corresponding to higher scores on scale and deprivation consistent with direction of other variables)
Smoking status (self-reported ordinal at baseline with the categories ‘never’, ‘previous’ or ‘current’)
Physical activity: International Physical Activity Questionnaire activity level (UKBB verified at baseline as ‘high’, ‘moderate’ or ‘low’ level of exercise, we reverse coded this)
Poor appetite or overeating
Trouble falling or staying asleep, or sleeping too much (self-reported measures dichotomised by UKBB in online follow-up)
Lifetime number of sex partners (numeric self-reported at baseline)
We dropped drug misuse as there were too few responses (<10 000) compared with other measures.
Biomarkers
C-reactive protein (CRP) (measured by UKBB in mg/L)
Albumin (g/L); cholesterol (mmol/L)
Creatinine (umol/L); glucose (mmol/L)
Glycated haemoglobin (HbA1c) (mmol/mol)
Insulin-like growth factor 1 (IGF-1) (nmol/L)
Triglycerides (mmol/L); pulse rate (bpm); diastolic and systolic blood pressure (automated readings in mmHg)
White blood cell (leukocyte) count (109 cells/L)
red blood cell (erythrocyte) count (1012 cells/L)
body mass index (BMI) (kg/m2)
waist circumference (cm)
hip circumference (cm)
number of treatments and medications taken (self-reported)
a diagnosis (1) or not (0) of diabetes (insulin dependent), hypertension (primary), and gastro-oesophageal reflux disease
All biomarker variables were clinically verified at baseline. These biomarkers were collected from the entire sample. Additional measures, including imaging and cognitive tests, were not considered in this paper as they were available only for a subsample.
Statistical analyses
One approach to analysis is to include all variables in models irrespective of statistical significance, if plausibly implicated in studies of mechanisms.13 However, this is not the standard approach.40 In this paper we first included conceptually relevant variables implicated in the aetiology of psychosis. We then tested statistical associations with psychosis and used a significance criterion in a backwards stepwise deletion (stepwise command in Stata), entering all the above variables in a full model. We retained variables showing significance (we initially considered P < 0.050), and a more stringent and a more liberal cut-off of P < 0.010 and P < 0.100), respectively. The general approach to variable selection was to assemble as many conceptually and statistically relevant variables as possible, and so we wished to adopt the least stringent P-value while assuring reasonable model fit. After backwards elimination of candidate independent variables at P < 0.050 and P < 0.100, there was support only for variables with significant associations at P < 0.050 with a reported diagnosis of psychosis overall. Rather than select variables using overly restrictive statistical criteria of P < 0.010, we compared the findings with those when using P < 0.050 as the threshold for inclusion.
After non-significant variables were removed, their respective contributions to the regression models were predicted with seemingly unrelated estimation (SUEST),41 a method for testing comparability as unadjusted and adjusted odds ratios (ORs) with 95% confidence intervals (CIs). The SUEST test used in the models is appropriate in this context to estimate whether respective differences by ethnic and gender subgroups are significant. So with the ethnicity between-group comparisons as an example, our final model was first estimated separately on the White British and combined ethnic minority groups respectively, before the SUEST command in Stata was then invoked to enable cross-group comparisons estimating these two samples together and comparing whether any differences between estimates of the respective model variables were significant (through the deployment of a chi-squared test and its associated P-value).42 Several diagnostic tests of model fit were performed. This included the link test for model specification (interpreted as a correctly specified model if the parameter _hat in this test is significant (P < 0.050) while the parameter _hatsq is not significant).43
Then a goodness-of-fit (GOF) test was applied to logistic regression models that included one or more continuous independent variables. Incremental sample size principles were applied to a standardised Hosmer–Lemeshow test44 (with non-significant values set by P ≥ 0.050). This suggested reasonable model fit. Finally, tolerance values (the reciprocal of the variance inflation factor: 1/VIF) greater than 0.200 for included variables indicate no suspected multicollinearity issues.43
The retained variables from the logistic regressions were then featured in a structural equation model (SEM) using constructs (latent variables) that cannot be observed directly, but are each composed/explained by the different independent observable variables added to the model.45 These latent constructs enabled us to outline the various interactions in a syndemics framework (in path diagrams) including adversity, demographics, biomarkers and psychosis. Rather than a standard covariance-based SEM approach (CB-SEM) that would prerequisite the inclusion of continuous variables only, we opted for a bootstrapped partial least squares SEM (PLS-SEM) allowing the inclusion of both the continuous and discrete/categorical observed variables as the most suitable signifiers of our unobservable latent constructs.40,46
To check PLS-SEM quality, we considered factor loadings (>0.30 as minimal acceptance level47) of the observed variables associated with their latent constructs, as well as the significance (P < 0.050) of the standardised beta path coefficients between the overarching latent constructs. Following interpretation for the size of standardised coefficients, we interpreted a coefficient equal to or lower than 0.090 as a small effect, between 0.100 and 0.200 as a moderate effect and above 0.200 as a large effect.43 With the absolute GOF indices measuring the discrepancy between the proposed model and empirical covariance matrices of the data, researchers often concentrate on the relative fit owing to the inherent estimation inaccuracies in PLS-SEM (compared with CB-SEM).48–52 Support from available guidelines enabled a threshold to be set for interpreting relative GOF values equal to or higher than 0.900 as arguing in favour of the model.51,53–56
In addition, we conducted subgroup analyses by: gender (dichotomised by UKBB, with male as the reference) based on National Health Service records and self-report; and ethnicity (ethnic minorities aggregated; then Black, South Asian, White other, Other, and White British.
All analyses were conducted in Stata version 16.1 (Windows) by K.H. and reviewed with K.B.
Secondary analysis of UKBB data is covered by the study's ethical approval from the North West Multi-Centre Research Ethics Committee (ref.: 16/NW/0274; see: https://www.ukbiobank.ac.uk/learn-more-about-uk-biobank/about-us/ethics). All participants consented for data to be used in research and are able to withdraw consent at any point. Where this happened, we removed their data from the analyses and the reported findings.
Results
Altogether, 480 participants were classified as having a psychotic disorder (i.e. at least one diagnosis between F20 and F31) and 133 976 participants were in the comparison group. The link (_hat: P = 0.012; _hatsq: P = 0.215), goodness-of-fit (P = 0.460) and multicollinearity (all 1/VIF values >0.430) tests all indicated promising results.
The final PLS-SEM included the following variables:
felt hated in childhood
ever victim of sexual assault
household income
poor appetite or overeating
waist circumference
hip circumference
leukocyte count
number of treatments and medications taken.
We present the background characteristics of the UKBB participants featuring in the final PLS-SEM analysis (in Tables 1 and 2).
Table 1.
PLS-SEM Sample characteristics by gender
| Total sample (n = 134 456) | Gender | ||
|---|---|---|---|
| Male (n = 60 997) | Female (n = 73 459) | ||
| Age, years: mean (s.d.) | 55.72 (7.74) | 56.45 (7.80) | 55.13 (7.64) |
| Ethnicity n (%) | |||
| White British | 122 135 (90.84) | 55 804 (91.49) | 66 331 (90.30) |
| White other | 8298 (6.17) | 3331 (5.46) | 4967 (6.76) |
| Black groups | 900 (0.67) | 385 (0.63) | 515 (0.70) |
| South Asian | 840 (0.62) | 494 (0.81) | 346 (0.47) |
| Other ethnicity | 1968 (1.46) | 781 (1.28) | 1187 (1.62) |
| Average household income <£18 000, n (%) | 18 287 (13.60) | 6968 (11.42) | 11 319 (15.41) |
| Townsend (area) deprivation index, mean (s.d.)a | −1.69 (2.84) | −1.76 (2.84) | −1.64 (2.84) |
| Any psychosis reported (ICD-10 F20–F31), n (%) | 480 (0.36) | 226 (0.37) | 254 (0.35) |
PLS-SEM, partial least squares structural equation model.
Higher value denotes greater deprivation.
Table 2.
PLS-SEM sample characteristics by ethnicity
| Ethnicity | |||||
|---|---|---|---|---|---|
| White British (n = 122 135) | White other (n = 8298) | Black (n = 900) | South Asian (n = 840) | Other ethnicity (n = 1968) | |
| Age, years: mean (s.d.) | 55.93 (7.69) | 54.46 (7.93) | 50.29 (7.05) | 52.10 (8.14) | 52.10 (7.69) |
| Gender, n (%) | |||||
| Male | 55 804 (45.69) | 3331 (40.14) | 385 (42.78) | 494 (58.81) | 781 (39.68) |
| Female | 66 331 (54.31) | 4967 (59.86) | 515 (57.22) | 346 (41.19) | 1187 (60.32) |
| Average household income less than £18 000, n (%) | 16 615 (13.60) | 1015 (12.23) | 154 (17.11) | 113 (13.45) | 332 (16.87) |
| Townsend (area) deprivation index, mean (s.d.)a | −1.83 (2.75) | −0.61 (3.22) | 1.63 (3.47) | −0.55 (2.98 | −0.02 (3.47) |
| Any psychosis reported (ICD-10 F20–F31), n (%) | 403 (0.33) | 50 (0.60) | 7 (0.78) | 3 (0.36) | 14 (0.71) |
PLS-SEM, partial least squares structural equation model.
Higher value denotes greater deprivation.
Table 3 and Table 4 outline the results of the logistic regression models as unadjusted ORs and adjusted ORs with associated confidence intervals. The tables show that the highest point estimate in the unadjusted analyses is represented by ‘ever victim of sexual assault’, with the odds of psychosis increasing by 99% for each score on the adversity measure (1.99–1.00). In the adjusted analyses, the highest estimate is ‘average total household income before tax’, with a 54% increased odds of reported psychosis for each lower bracket/category on the ordinal scale (1.54–1.00).
Table 3.
Unadjusted logistic regressions with variables individually measured on reported diagnosis of psychosis
| Total sample, OR (95% CI) | Ethnicity, OR (95% CI) | Gender, OR (95% CI) | |||||
|---|---|---|---|---|---|---|---|
| White British | Ethnic minority | P-value of SUEST test | Male | Female | P-value of SUEST test | ||
| Felt hated in childhood | 1.57 (1.47–1.68)* | 1.54 (1.43–1.66)* | 1.60 (1.38–1.85)* | 0.672 | 1.66 (1.49–1.84)* | 1.55 (1.42–1.68)* | 0.300 |
| Ever exposed to combat or war | 1.41 (0.98–2.01) | 1.27 (0.83–1.95) | 1.44 (0.71–2.92) | 0.757 | 1.53 (1.02–2.28)* | 0.96 (0.40–2.29) | 0.333 |
| Ever victim of sexual assault | 1.99 (1.65–2.39)* | 1.98 (1.62–2.43)* | 1.79 (1.12–2.85)* | 0.693 | 2.19 (1.57–3.05)* | 2.04 (1.62–2.56)* | 0.732 |
| Age at recruitment | 0.98 (0.98–0.99)* | 0.98 (0.98–0.99)* | 0.99 (0.98–1.00)* | 0.844 | 0.98 (0.97–0.98)* | 0.98 (0.98–0.99)* | 0.173 |
| Household income | 1.96 (1.88–2.03)* | 1.91 (1.83–1.99)* | 2.13 (1.93–2.35)* | 0.083 | 2.25 (2.13–2.38)* | 1.73 (1.64–1.82)* | <0.001* |
| Poor appetite or overeating | 1.84 (1.70–1.99)* | 1.84 (1.69–2.00)* | 1.77 (1.45–2.16)* | 0.717 | 2.09 (1.86–2.35)* | 1.72 (1.55–1.91)* | 0.014* |
| Waist circumference | 1.02 (1.02–1.03)* | 1.02 (1.02–1.03)* | 1.03 (1.02–1.03)* | 0.084 | 1.02 (1.02–1.03)* | 1.03 (1.03–1.03)* | 0.027* |
| Hip circumference | 1.02 (1.01–1.02)* | 1.01 (1.01–1.02)* | 1.02 (1.02–1.03)* | 0.029* | 1.01 (1.01–1.02)* | 1.02 (1.02–1.02)* | 0.092 |
| Leukocyte count | 1.04 (1.04–1.05)* | 1.04 (1.03–1.05)* | 1.12 (1.08–1.15)* | <0.001* | 1.04 (1.03–1.05)* | 1.05 (1.04–1.07)* | 0.394 |
| Number of treatments and medications | 1.17 (1.16–1.18)* | 1.17 (1.16–1.18)* | 1.16 (1.14–1.18)* | 0.268 | 1.17 (1.16–1.19)* | 1.17 (1.16–1.18)* | 0.583 |
SUEST, seemingly unrelated estimation.
P < 0.050.
Table 4.
Logistic regressions with variables adjusted for other model variables on reported diagnosis of psychosis
| Total sample, OR (95% CI) | Ethnicity, OR (95% CI) | Gender, OR (95% CI) | |||||
|---|---|---|---|---|---|---|---|
| White British | Ethnic minority | P-value of SUEST test | Male | Female | P-value of SUEST test | ||
| Felt hated in childhood | 1.28 (1.18–1.39)* | 1.28 (1.17–1.40)* | 1.20 (1.00–1.45) | 0.570 | 1.27 (1.12–1.44)* | 1.29 (1.16–1.43)* | 0.865 |
| Ever exposed to combat or war | 1.13 (0.76–1.69) | 1.11 (0.70–1.76) | 1.11 (0.48–2.55) | 0.995 | 1.16 (0.73–1.83) | 0.95 (0.39–2.28) | 0.692 |
| Ever victim of sexual assault | 1.34 (1.08–1.67)* | 1.38 (1.09–1.75)* | 1.09 (0.62–1.89) | 0.432 | 1.34 (0.91–1.97) | 1.41 (1.08–1.85)* | 0.822 |
| Age at recruitment | 0.95 (0.94–0.96)* | 0.95 (0.94–0.97)* | 0.95 (0.92–0.98)* | 0.770 | 0.94 (0.93–0.96)* | 0.96 (0.95–0.98)* | 0.101 |
| Household income | 1.54 (1.42–1.68)* | 1.47 (1.34–1.62)* | 1.94 (1.56–2.43)* | 0.035* | 1.77 (1.56–2.01)* | 1.37 (1.22–1.53)* | 0.007* |
| Poor appetite or overeating | 1.34 (1.21–1.48)* | 1.35 (1.21–1.51)* | 1.32 (1.03–1.70)* | 0.859 | 1.40 (1.20–1.64)* | 1.31 (1.14–1.50)* | 0.515 |
| Waist circumference | 1.03 (1.02–1.04)* | 1.02 (1.01–1.03)* | 1.03 (1.00–1.06)* | 0.645 | 1.03 (1.01–1.05)* | 1.02 (1.00–1.03) | 0.352 |
| Hip circumference | 0.97 (0.95–0.98)* | 0.97 (0.95–0.98)* | 0.96 (0.93–1.00)* | 0.842 | 0.96 (0.93–0.99)* | 0.98 (0.96–1.00) | 0.221 |
| Leukocyte count | 1.03 (1.01–1.06)* | 1.03 (1.01–1.06)* | 1.11 (1.01–1.22)* | 0.114 | 1.03 (1.00–1.07) | 1.04 (1.01–1.07)* | 0.689 |
| Number of treatments and medications | 1.13 (1.10–1.16)* | 1.13 (1.10–1.16)* | 1.13 (1.05–1.22)* | 0.990 | 1.12 (1.07–1.17)* | 1.14 (1.10–1.18)* | 0.421 |
SUEST, seemingly unrelated estimation.
P < 0.050.
The retained variables for the logistic regression model were then investigated in the context of a PLS-SEM model. We combined ‘felt hated in childhood’, ‘victim of sexual assault’ and ‘experience of combat or war’ in a latent construct for lifetime adversity. Low household income, unhealthy diet and age contributed to current adversity. Age was included as ageing relates to a greater risk of poor health generally and although not strictly a form of adversity, the risks associated with ageing might best be captured as an immediate risk – reflecting age at the time of the study – rather than lifetime risk. Furthermore, in women, there is a second peak of risk at an older age.57 Waist circumference, hip circumference, high white blood cell count, and number of treatments and medications taken contributed to the latent construct of biomarkers. The initial results showed that the factor loadings for ‘experience of combat or war’ on the latent construct of lifetime adversity (0.235) and for age on current adversity (0.287) were both suboptimal, so were removed from the final PLS-SEM model.
The relative GOF statistic for the final model was high (0.900) and the standardised path coefficients between the latent constructs were all significant (P < 0.050), with a moderate direct effect size from lifetime and current adversity (0.178; the effect size in the reverse direction was 0.187, suggesting possible recall bias). There were large direct effects between current adversity and biomarkers (0.227; with 0.219 in the reverse direction, perhaps an indication of recall bias among those who are unwell). All other effects were small.
The main results are outlined in Table 5 (direct effects for total sample and subgroups) and Table 6 (combination of direct, indirect and total effects for total sample), and in Fig. 1.
Table 5.
Syndemics PLS-SEM with direct effects in total sample and comparison by subgroups (ethnicity and gender)a
| Structural comparison | Total sample, s.c. (P) | Ethnicity | Gender | ||
|---|---|---|---|---|---|
| White British (reference), s.c. | Ethnic minority (combined), s.c. (P compared with White British reference) | Male (reference), s.c. | Female, s.c. (P compared with male reference) | ||
| Past adversity → current adversity | 0.178 (P < 0.001) | 0.175 | 0.203 (P = 0.027) | 0.154 | 0.155 (P = 0.144) |
| Past adversity → biomarkers | 0.007 (P = 0.048) | 0.009 | 0.006 (P = 0.806) | 0.021 | 0.032 (P = 0.128) |
| Past adversity → psychosis | 0.028 (P < 0.001) | 0.026 | 0.028 (P = 0.855) | 0.028 | 0.031 (P = 0.802) |
| Current adversity → past adversity | 0.187 (P < 0.001) | 0.184 | 0.213 (P = 0.026) | 0.161 | 0.167 (P = 0.056) |
| Current adversity → biomarkers | 0.227 (P < 0.001) | 0.226 | 0.230 (P = 0.763) | 0.213 | 0.267 (P < 0.001) |
| Current adversity → psychosis | 0.038 (P < 0.001) | 0.035 | 0.062 (P = 0.115) | 0.052 | 0.031 (P = 0.022) |
| Biomarkers → past adversity | 0.007 (P = 0.048) | 0.009 | 0.006 (P = 0.801) | 0.021 | 0.034 (P = 0.109) |
| Biomarkers → current adversity | 0.219 (P < 0.001) | 0.219 | 0.220 (P = 0.980) | 0.208 | 0.261 (P < 0.001) |
| Biomarkers → psychosis | 0.019 (P = 0.048) | 0.017 | 0.034 (P = 0.180) | 0.014 | 0.016 (P = 0.995) |
PLS-SEM, partial least squares structural equation model; s.c., standardised coefficient; arrows indicate directions of associated tested.
Bold denotes significance at P < 0.050 (in total sample; or compared with White British (ethnicity); or male (gender)).
Table 6.
Syndemics PLS-SEM for total sample showing combination of the direct, indirect and total effects
| Structural comparison | Direct effects, s.c. | Indirect effects, s.c. | Total effects, s.c. |
|---|---|---|---|
| Past adversity → current adversity | 0.178 | 0.016 | 0.194 |
| Past adversity → biomarkers | 0.007 | 0.041 | 0.047 |
| Past adversity → psychosis | 0.028 | 0.009 | 0.037 |
| Current adversity → past adversity | 0.187 | 0.017 | 0.205 |
| Current adversity → biomarkers | 0.227 | 0.020 | 0.247 |
| Current adversity → psychosis | 0.038 | 0.013 | 0.050 |
| Biomarkers → past adversity | 0.007 | 0.042 | 0.048 |
| Biomarkers → current adversity | 0.219 | 0.019 | 0.239 |
| Biomarkers → psychosis | 0.019 | 0.011 | 0.029 |
PLS-SEM, partial least squares structural equation model; s.c., standardised coefficient; arrows indicate directions of associated tested.
Fig. 1.
Proposed syndemics partial least squares structural equation model (PLS-SEM) for psychosis in the UK (showing direct effects).
Latent constructs are shown in circles, observable variables in squares. The standardised coefficients between latent constructs (inner model) are depicted next to thicker arrows (directions of effects might go both ways), whereas factor loadings associated with latent constructs (outer model) are next to thinner arrows.
Only ‘poor appetite or overeating’ would have been dropped from the final PLS-SEM analysis had we used a more stringent cut-off of P < 0.010 instead of P < 0.050, and as a sensitivity check we ran the overall model without this variable to verify that similar results (significant associations) were retained for all other variables.
The subgroup analyses (also displayed in Tables 3–5) reveal some, but relatively few, significant modifications by ethnicity and gender. Perhaps most notable are the significantly greater effects of low household income in adjusted analyses and the paths between lifetime and current adversity for the combined ethnic minority category compared with the White British group.
Discussion
Summary of key findings
We have drawn on the available (and rapidly emerging) literature on syndemics and the cumulative effects of experiencing co-occurring adversities in the context of lifetime adversities (past and potentially ongoing). We examined the complex interplay between a range of potential explanatory variables as social and fundamental causes of psychosis and potentially of inequalities in experience of psychoses.29 There appear to be important links between lifetime adversity and current adversity, perhaps reflecting recall bias but likely also showing that the experience of adversity early in life will lead to later adversity also. Contemporary adversity was associated with raised inflammatory markers, more so than lifetime adversity, again suggesting an interplay between lifetime and present adversity and inflammation. The relationship between lifetime and present adversity was especially marked among ethnic minorities (aggregated group). Thus, findings suggest an overall model of psychosis that needs to consider early-life adversity as a preventive target as well as a therapeutic target for those who develop psychosis. Further work is needed on ethnicity and gender with larger samples. The small associations with psychosis are not surprising given that this is a low-incidence condition; the effects are not insignificant in the context of public health approaches to prevention, which shift the population distributions of risk factors to the left, to reduce the total samples that might develop a condition. In large populations, even small effect sizes may result in significant numbers of people developing psychosis and related disabilities.
A recent study13 found that ethnic inequalities in psychosis were better explained by a syndemic whereby harmful social and health conditions co-occur in geographical/temporal contexts. The study evidenced that the co-existence of crime and violence, mental health problems, substance misuse and risky sexual behaviours explained the risk of psychosis in a specific London borough (Hackney). It also showed that all ethnic groups were vulnerable to this area effect, for example White men in Hackney reporting comparatively more anxiety, depression and adverse health behaviours than White men in the general UK population. The authors argued that ethnic minority and other marginalised groups are more likely to live in lower income households, often concentrated in relatively deprived areas affected by these unfavourable socioeconomic conditions. We explored such findings at a national level through a combined measure representing childhood adversity, low household income, adverse health behaviour in addition to biomarkers as possible intermediate mechanisms associated with psychosis. However, we are limited by relying on national data and that a more extensive investigation and confirmation of the wider range of potential variables interacting with specific location parameters (such as in the Hackney study) was not possible. There was a low number of significant adverse health behaviour variables that our analyses could return. As a consequence, our (national) model had to be simplified and requires replication in specific locations and prospective developments.
Implications for research
We propose that further analyses are necessary using larger data-sets, yet many cohorts do not include ACEs, inflammatory markers and ICD-10 diagnoses, which were a strength of the UKBB data. There are no standard approaches to testing syndemic models. We therefore had to consider alternative approaches and chose the methods that seemed transparent and suitable for large data-sets with many variables that may all be interacting. For example, a seminal paper on syndemics theory32 suggests that many researchers have used a ‘sum score’ to demonstrate the existence of syndemics. This is an approach whereby a syndemic is expressed via a combined variable containing the sum total of all candidate health risks experienced by the study participants. The problem with this approach is that all risks are seen as equal (only one variable exists in the regression model, for example). This both increases the chance of generating a statistically significant finding and masks the individual contributions of each candidate risk variable. Furthermore, these studies tend to focus predominantly on individual risk factors only, while neglecting the potential influence of multiple risk factors (as central to syndemics frameworks). For instance, variables such as level of area deprivation32 (which was also included in the present study) are not always considered, nor are life-course exposures.
The techniques applied in this study were logistic regression and SEM, but there are other statistical techniques previously employed to measure and describe syndemic effects.32 Our study has shown one possible way that synergies between components comprising measures of adversity and relatively high biomarker values may increase a person's risk of transition to a clinical diagnosis of psychosis. However, we realise that other factors not accounted for here might be at play, as for example environmental exposures such as stress have in previous studies been shown to interact with genetic risk.58 Additionally, owing to a lack of more optimal measures in the data-set, there are opportunities for future studies to assess the detrimental effects of experienced racism and discrimination, as well as the suspected role of and the extent to which social support mechanisms – known in some wider literature to exert a potentially preventive effect on adverse health outcomes59 – can help mediate or even significantly dampen syndemic effects.
The emerging research on syndemics suggests the importance of mixed methods to triangulate findings from multiple sources and unearth how large-scale social forces converse in a complex manner to shape the evolution of multiple conditions. Qualitative studies, and anthropological/ethnographic investigations in particular, can complement epidemiological data with richer, deeper and more place-based examinations of potential multiplicative and synergistic interactions, or the ‘microfoundations for macro-level observations’.32
Limitations of this study
The total sample that could be included for our analyses was relatively modest compared with the overall UKBB sample (>500 000). Some questions relating to key variables could not been administered to all participants in the UKBB data-set because of online follow-ups requiring participants’ email addresses. For example, some were important measures in a hypothesised syndemic model (e.g. of traumatic experiences or adverse health behaviours). cross-examination of different variables for our analyses/models reduced numbers further by following conventions of a completer analysis (listwise deletion).60,61
The effects by specific ethnic groups and by gender were not marked, partly owing to limited power. Indeed, UKBB recruits healthy volunteers and shows some under-representation of ethnic minorities. As UKBB is a cross-sectional study, we cannot infer causality. Thus, replication is necessary in early intervention, prospective and ethnically enriched samples. Future studies should also test for place effects, which can be components of a syndemic model, although we did test for area deprivation.
Key variables had to be derived at baseline (between 2006 and 2010) either because they were only available at that time in the data-set, or the numbers that had responded to follow-up questions were markedly lower.
We acknowledge that reported diagnoses of psychosis were relatively low in the overall sample (and even lower by demographic subgroups). We also did not consider the timing of the diagnoses, given the small number of people with specific diagnoses; for example 68% of those receiving a schizophrnia diagnosis did so before enrolment, and 79% by 2010, the rest being diagnosed by 2017.
Furthermore, our markers of inflammation retained in the models might not naturally be expected to be inflammatory biomarkers but indicate a potential inflammatory role. For example, obesity, waist circumference and inflammation are associated in psychoses.62 Adversity variables (e.g. childhood adversity) were based on retrospective reports of past events and in some instances it is possible that there was ongoing adversity.8,13 The findings are best considered hypothesised associations rather than representing causal mechanisms, especially as it is well-known from the literature that mental illnesses are associated with raised inflammatory biomarkers.29
High leukocyte (white blood cell) count is a known marker for severity of inflammation and may signal an underlying problem such as trauma or stress and has also been associated with certain diseases, infections and allergies, with relatively high mortality rates in middle-aged populations.63 However, the fact that this biomarker, along with waist and hip circumference and number of treatments/medications, was significant in our analyses does not tell us why other known biomarkers seemed to have little predictive value. This speaks to a wider issue in the literature, where consensus is yet to be established on which biomarkers are necessary to investigate mechanisms in syndemics and allostatic load models.5 Although needing further work, the relative importance of biomarkers might depend on the specific health outcome under investigation.5
Syndemic theory argues for co-occurring disease entities and interacting risk factors in webs of causation. This is difficult to apply to psychosis for many reasons. Psychoses are diagnosed using symptom patterns and have fuzzy boundaries, and produce categories that are contested, especially across ethnic groups. Thus, a syndemic theory of psychotic disorders needs to accommodate the different diagnostic processes for distinct conditions, for example cancer or infectious disease, which more usually have physiological and anatomical alterations. Psychotic symptoms that do not reach a threshold for a diagnosis are associated with a higher risk of later diagnosis and more severe illness later, and might be part of a syndemic and a component of the mechanism leading to psychotic disorders. Strictly speaking, syndemics reflect co-occurring epidemics. We did not assess these nor separate illnesses. In this study, we have looked primarily at psychosis and inflammatory markers as proxies for comorbidity. Syndemics that have been described usually include behaviours such as violence or drug misuse as well as conditions like HIV. Thus, health behaviours may also be considered, as our study showed that disordered eating patterns were relevant and perhaps a manifestation of distress.
Implications for policy and practice
Public health policies are clearly not meeting the needs of people and stark inequalities persist, perhaps as funding sources are focused on single outcomes and certain diseases receive predominant attention.29 Enhancing the effectiveness of public health and care interventions for syndemic frameworks may tackle systemic drivers and save costs for an already overstretched National Health Service currently fighting a global pandemic. Indeed, COVID-19 may also be a manifestation of similar complex causal pathways. Obviously, practitioners also need assistance in developing, testing and implementing integrated and systemic interventions in partnership with local government and social care agencies.29 The findings suggest that clinical interventions will need to recognise the social and structural drivers of psychosis and that past and ongoing adversity should be a target for both public health prevention efforts and therapies that recognise this complexity. Thus, syndemic policies and practices will need to evolve with the evidence, which will need to be nuanced regarding different types of psychosis, larger samples of ethnic groups, and comorbidities with other psychiatric and medical disorders.
Author contributions
K.B. conceived the idea, which was developed with the research group including R.M., G.M.H. and K.H.. K.H. and K.B. secured UKBB data, and K.H. undertook analysis in discussion with K.B.. All authors reviewed consecutive drafts of the manuscript and contributed intellectually to the theoretical, technical and statistical elements, and K.B. also refined the clinical implications.
Funding
K.H. was supported by the Lankelly Chase grant to K.B. for the Synergi Collaborative Centre. The paper was thus part funded by Lankelly Chase but received no specific additional grant support dedicated to these analyses. UKBB data access was funded by Centre for Psychiatry, Queen Mary, University of London.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1192/bjp.2021.142.
click here to view supplementary material
Data availability
UKBB data are accessible to all researchers by registration and entering into an appropriate institutional agreement with UKBB.
Declaration of interest
K.B. is Editor in Chief of the BJPsych and did not take part in the review or decision-making process of this paper.
References
- 1.Coid JW, Kirkbride JB, Barker D, Cowden F, Stamps R, Yang M, et al. Raised incidence rates of all psychoses among migrant groups: findings from the East London first episode psychosis study. Arch Gen Psychiatry 2008; 65: 1250–8. [DOI] [PubMed] [Google Scholar]
- 2.Del-Ben CM, Shuhama R, Loureiro CM, Ragazzi TCC, Zanatta DP, Tenan SHG, et al. Urbanicity and risk of first-episode psychosis: incidence study in Brazil. Br J Psychiatry 2019; 215: 726–29. [DOI] [PubMed] [Google Scholar]
- 3.Selten JP, van der Ven E, Termorshuizen F. Migration and psychosis: a meta-analysis of incidence studies. Psychol Med 2020; 50: 303–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basu D, Lopez I, Kulkarni A, Sellin JH. Impact of race and ethnicity on inflammatory bowel disease. Am J Gastroenterol 2005; 100: 2254–61. [DOI] [PubMed] [Google Scholar]
- 5.Beckie TM. A systematic review of allostatic load, health, and health disparities. Biol Res Nurs 2012; 14: 311–46. [DOI] [PubMed] [Google Scholar]
- 6.Borrell LN, Crawford ND. Social disparities in periodontitis among US adults: the effect of allostatic load. J Epidemiol Community Health 2011; 65: 144–9. [DOI] [PubMed] [Google Scholar]
- 7.Brody GH, Lei MK, Chae DH, Yu T, Kogan SM, Beach SRH. Perceived discrimination among African American adolescents and allostatic load: a longitudinal analysis with buffering effects. Child Dev 2014; 85: 989–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Myers HF. Ethnicity- and socio-economic status-related stresses in context: an integrative review and conceptual model. J Behav Med 2009; 32: 9–19. [DOI] [PubMed] [Google Scholar]
- 9.Upchurch DM, Stein J, Greendale GA, Chyu L, Tseng CH, Huang MH, et al. A longitudinal investigation of race, socioeconomic status, and psychosocial mediators of allostatic load in midlife women: findings from the study of women's health across the nation. Psychosom Med 2015; 77: 402–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen E, Matthews KA. Cognitive appraisal biases: an approach to understanding the relation between socioeconomic status and cardiovascular reactivity in children. Ann Behav Med 2001; 23: 101–11. [DOI] [PubMed] [Google Scholar]
- 11.Collins JW, Jr., David RJ, Symons R, Handler A, Wall S, Andes S. African-American mothers’ perception of their residential environment, stressful life events, and very low birthweight. Epidemiology 1998; 9: 286–9. [PubMed] [Google Scholar]
- 12.Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: do negative emotions play a role? Psychol Bull 2003; 129: 10–51. [DOI] [PubMed] [Google Scholar]
- 13.Coid J, Gonzalez Rodriguez R, Kallis C, Zhang Y, Bhui K, De Stavola B, et al. Ethnic disparities in psychotic experiences explained by area-level syndemic effects. Br J Psychiatry 2020; 217: 555–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walker EF. Adults with psychosis or psychotic experiences may report adverse life events prior to the onset of symptoms but direction of causality cannot be inferred. Evid Based Ment Health 2013; 16(4): 97. [DOI] [PubMed] [Google Scholar]
- 15.Klippel A, Myin-Germeys I, Chavez-Baldini U, Preacher KJ, Kempton M, Valmaggia L, et al. Modeling the interplay between psychological processes and adverse, stressful contexts and experiences in pathways to psychosis: an experience sampling study. Schizophr Bull 2017; 43: 302–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One 2015; 10(9): e0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Korous KM, Causadias JM, Casper DM. Racial discrimination and cortisol output: a meta-analysis. Soc Sci Med 2017; 193: 90–100. [DOI] [PubMed] [Google Scholar]
- 18.Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, Read J, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull 2012; 38: 661–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sterling P, Eyer J. Allostasis: a new paradigm to explain arousal pathology. InHandbook of Life Stress, Cognition and Health (eds Fisher S, Reason J): 629-49. John Wiley & Sons, 1988. [Google Scholar]
- 20.Baumeister D, Russell A, Pariante CM, Mondelli V. Inflammatory biomarker profiles of mental disorders and their relation to clinical, social and lifestyle factors. Soc Psychiatry Psychiatr Epidemiol 2014; 49: 841–9. [DOI] [PubMed] [Google Scholar]
- 21.Baumeister D, Akhtar R, Ciufolini S, Pariante CM, Mondelli V. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-alpha. Mol Psychiatry 2016; 21: 642–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abdul-Hamid WK, Bhui K. Psychiatry, homeless patients and welfare reforms: historical links and chains. Int J Soc Psychiatry 2014; 60: 71–4. [DOI] [PubMed] [Google Scholar]
- 23.Khandaker GM, Cousins L, Deakin J, Lennox BR, Yolken R, Jones PB. Inflammation and immunity in schizophrenia: implications for pathophysiology and treatment. Lancet Psychiatry 2015; 2: 258–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kohler-Forsberg O, Muller N, Lennox BR. The role of inflammation in the etiology and treatment of schizophrenia. Front Psychiatry 2020; 11: 603296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fraguas D, Diaz-Caneja CM, Rodriguez-Quiroga A, Arango C. Oxidative stress and inflammation in early onset first episode psychosis: a systematic review and meta-analysis. Int J Neuropsychopharmacol 2017; 20: 435–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kogan S, Ospina LH, Mittal VA, Kimhy D. The impact of inflammation on neurocognition and risk for psychosis: a critical review. Eur Arch Psychiatry Clin Neurosci 2020; 270: 793–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rodrigues M, Wiener JC, Stranges S, Ryan BL, Anderson KK. The risk of physical multimorbidity in people with psychotic disorders: a systematic review and meta-analysis. J Psychosom Res 2021; 140: 110315. [DOI] [PubMed] [Google Scholar]
- 28.Singer M. A dose of drugs, a touch of violence, a case of aids: conceptualizing the SAVA syndemic. Free Inq Creat Sociol 1996; 24: 99–110. [Google Scholar]
- 29.Singer M, Bulled N, Ostrach B, Bulled N, Ostrach B, Mendenhall E. Syndemics and the biosocial conception of health. Lancet 2017; 389: 941–50. [DOI] [PubMed] [Google Scholar]
- 30.Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol 2001; 30: 668–77. [DOI] [PubMed] [Google Scholar]
- 31.Morgan C, Charalambides M, Hutchinson G, Murray RM. Migration, ethnicity, and psychosis: toward a sociodevelopmental model. Schizophr Bull 2010; 36: 655–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tsai AC. Syndemics: a theory in search of data or data in search of a theory? Soc Sci Med 2018; 206: 117–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mendenhall E. Syndemic Suffering: Social Distress, Depression, and Diabetes Among Mexican Immigrant Women. Left Coast Press, 2012. [Google Scholar]
- 34.Secretary of State for Health and Social Care, Lord Chancellor, Secretary of State for Justice. Reforming the Mental Health Act (CP 355). TSO (The Stationery Office), 2021. [Google Scholar]
- 35.Halvorsrud K, Nazroo J, Otis M, Hajdukova E Brown, Bhui K. Ethnic inequalities in the incidence of diagnosis of severe mental illness in England: a systematic review and new meta-analyses for non-affective and affective psychoses. Soc Psychiatry Psychiatr Epidemiol 2019; 54: 1311–23. [DOI] [PubMed] [Google Scholar]
- 36.Halvorsrud K, Nazroo J, Otis M, Hajdukova E Brown, Bhui K. Ethnic inequalities and pathways to care in psychosis in England: a systematic review and meta-analysis. BMC Med 2018; 16(1): 223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med 2015; 12(3): e1001779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tsai AC, Burns BF. Syndemics of psychosocial problems and HIV risk: a systematic review of empirical tests of the disease interaction concept. Soc Sci Med 2015; 139: 26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tsai AC, Mendenhall E, Trostle JA, Kawachi I. Co-occurring epidemics, syndemics, and population health. Lancet 2017; 389: 978–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ronaldson A, Freestone MC, Zhang H, Marsh W, Bhui K et al. Using structural equation modelling in routine clinical data: depression, diabetes, and use of accident & emergency. To be published in J Med Int Res. [Preprint] 2020. Available from: 10.2196/22912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mize TD, Doan L, Long JS. A general framework for comparing predictions and marginal effects across models. Sociol Methodol 2019; 49: 152–89. [Google Scholar]
- 42.Weesie J (1999) Seemingly unrelated estimation and cluster-adjusted sandwich estimator. Stata Tech Bull 9: 231–48. [Google Scholar]
- 43.Mehmetoglu M, Jakobsen TG. Applied Statistics Using STATA: A Guide for the Social Sciences. Sage, 2016. [Google Scholar]
- 44.Paul P, Pennell ML, Lemeshow S. Standardizing the power of the Hosmer–Lemeshow goodness of fit test in large data sets. Stat Med 2013; 32: 67–80. [DOI] [PubMed] [Google Scholar]
- 45.Streiner DL. Building a better model: an introduction to structural equation modelling. Can J Psychiatry 2006; 51: 317–24. [DOI] [PubMed] [Google Scholar]
- 46.Venturini S, Mehmetoglu M. plssem: A Stata Package for Structural Equation Modeling with Partial Least Squares. J Stat Soft 2019; 88(8): 1–35. [Google Scholar]
- 47.Hair JF, Black B, Babin B, Anderson RE, Tatham RL. Multivariate Data Analysis (6th edn). Pearson Prentice Hall, 2006. [Google Scholar]
- 48.Ravand H, Baghaei P. Partial least squares structural equation modeling with R. Pract Assess Res Evaluation 2016; 21(11). [Google Scholar]
- 49.Maydeu-Olivares A, Garcia-Forero C. Goodness-of-fit testing. Int Encycloped Educ 2010; 7: 190–96. [Google Scholar]
- 50.Henseler J, Sarstedt M. Goodness-of-fit indices for partial least squares path modeling. Comput Stat 2013; 28: 565–80. [Google Scholar]
- 51.Evermann J, Tate M. Testing Models or Fitting Models? Identifying Model Misspecification in PLS. ICIS Proceedings 2010(21). [Google Scholar]
- 52.Hair JF, Sarstedt M, Ringle CM, Mean JA. An assessment of the use of partial least squares structural equation modeling in marketing research. J Acad Mark Sci 2012; 40: 414–33. [Google Scholar]
- 53.Vinzi VE, Trinchera L, Amato S. PLS path modeling: from foundations to recent developments and open issues for model assessment and improvement. In Handbook of Partial Least Squares (eds Esposito Vinzi V, Chin W, Henseler J, Wang H): 47–82. Springer, 2010. [Google Scholar]
- 54.Chin W. How to write up and report PLS analyses. In Handbook of Partial Least Squares (eds Esposito Vinzi V, Chin W, Henseler J, Wang H): 655–90. Springer, 2010. [Google Scholar]
- 55.Mehmetoglu M. Model-based post hoc segmentation (with REBUS-PLS) for capturing heterogeneous consumer behaviour. J Target Meas Anal Mark 2011; 19: 165–72. [Google Scholar]
- 56.Thun S, Saksvik P, Ose SO, Ose SO, Christensen M. The impact of supervisors’ attitudes on organizational adjustment norms and attendance pressure norms. Scand J Organ Psychol 2013; 5(2): 15–31. [Google Scholar]
- 57.Li R, Ma X, Wang G, Yang J, Wang C. Why sex differences in schizophrenia? J Transl Neurosci 2016; 1: 37–42. [PMC free article] [PubMed] [Google Scholar]
- 58.Linscott RJ, van Os J. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med 2013; 43: 1133–49. [DOI] [PubMed] [Google Scholar]
- 59.Reblin M, Uchino BN. Social and emotional support and its implication for health. Curr Opin Psychiatry 2008; 21: 201–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Niedzwiedz CL, O'Donnell CA, Jani BD, Demou E, Ho FK, Celis-Morales C, et al. Ethnic and socioeconomic differences in SARS-CoV-2 infection: prospective cohort study using UK Biobank. BMC Med 2020; 18(1): 160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sarris J, Thomson R, Hargraves F, Eaton M, de Manincor M, Veronese N, et al. Multiple lifestyle factors and depressed mood: a cross-sectional and longitudinal analysis of the UK Biobank (N=84,860). BMC Med 2020; 18(1): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Keinänen J, Suvisaari J, Reinikainen J, Kieseppä T, Lindgren M, Mäntylä T, et al. Low-grade inflammation in first-episode psychosis is determined by increased waist circumference. Psychiatry Res 2018; 270: 547–53. [DOI] [PubMed] [Google Scholar]
- 63.Dregan A. Arterial stiffness association with chronic inflammatory disorders in the UK Biobank study. Heart 2018; 104: 1257–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1192/bjp.2021.142.
click here to view supplementary material
Data Availability Statement
UKBB data are accessible to all researchers by registration and entering into an appropriate institutional agreement with UKBB.