Abstract
Purpose
The review aims to reach a common consensus regarding the swashbuckler approach for distal femur fractures by a systematic review of the available literature and to evaluate the complications, union, and outcomes.
Methods
Electronic database search engines like Cochrane Library, PubMed, Google Scholar, and Scopus were searched until May 2021. Studies comparing the clinical complications, and functional outcome scores of Swashbuckler approach for distal femur were considered. The quality of the articles were evaluated using Methodological Index for Non-Randomized Studies score.
Results
Eleven studies were included for the final analysis. An anterior midline incision was used in the majority of studies. Superficial infection was the most common complication seen followed by knee stiffness and deep infections. 66.45% of the patients had excellent/good outcomes. 1.08% had a painful implant and 1.89% had deep infection.
Conclusion
Swashbuckler approach offers itself as a viable option in cases of distal femur fractures, especially in AO type C. The quadriceps sparing approach provides excellent/good outcomes in approximately 66.45% of the patients.
Keywords: Swashbuckler, Distal femur fracture, Lateral parapatellar approach, Functional outcomes
1. Introduction
Distal femur fractures account for 7% of emergency trauma cases.1 The varying presentations along with the difficulty in treating the complex distal femur fractures make them tricky for orthopedic surgeons. The fracture follows a bimodal distribution with young patients often affected by high-velocity accidents and elderly to low energy fractures due to osteoporosis.2 The intraarticular fractures especially AO type C3 with multiple fragments are challenging due to their known complications such as malunion, infection, knee stiffness, and secondary osteoarthritis. Various exposures have been devised to effectively treat the intraarticular component and to improve the patients’ outcome both subjectively and objectively.1,3 These approaches include anteromedial/anterolateral parapatellar approaches, Olerud extensile anterior approach, Anterior approach, Tibial tubercle osteotomy, Combined medial and lateral approach, Posterior approach, and Swashbuckler approach.4,5
The most commonly used in clinical practice is the lateral parapatellar or anterolateral approach.6,7 Distal femur fractures especially the AO type C require good intraarticular exposure for anatomic reduction. The usual lateral and medial parapatellar approaches have been often cited for their inability to fully show the intraarticular component. The Olerud approach (extensile anterior approach with tibial tuberosity osteotomy) in a recent systematic review was shown to have good/excellent functional outcomes in 57% of patients.8 Swashbuckler approach was described by Starr et al. as a modified anterior approach to the distal femur, that facilitated complete exposure of distal femur articular surface and provided quicker rehabilitation.9 The anterior skin incision utilized for the approach would not compromise the future skin incisions necessary for total knee replacements.9 Modifications of the incision such as small lateral incision which the authors termed as “Mini Swashbuckler” were also introduced later on a cadaver which theoretically decreases the operative time.10
Each approach has its advantages and disadvantages. The swashbuckler approach introduced in the late 1990s offers itself as an exposure option for surgeons to treat distal femur fractures. The current literature lacks consensus on the use of the above-said approach and the outcomes various studies have reported along with the complications. The purpose of the current study was to systematically review the available literature on the use of the swashbuckler approach in distal femur fractures and to evaluate and analyze the patient outcomes such as quality of studies, approach, operative time, blood loss, length of stay, complications, union, and functional outcomes.
2. Methods
The current review was conducted as per the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) guidelines using a predetermined protocol.11
2.1. Literature search and study selection
The search was conducted by two authors (B.S.R. and A.K.S.G.) in the online databases PubMed, Embase, Cochrane, and Google scholar until 24th April 2021. The articles were searched using the keywords ‘distal femur fracture’, ‘distal femur comminuted fracture’, ‘AO type C3’, ’Hoffa fracture’, ‘distal femur intraarticular fracture’, ‘approach’, ‘swashbuckler approach’, ‘swashbuckler’, ‘modified swashbuckler approach’. The articles were selected based on the inclusion criteria discussed below in two stages. First, the abstracts of the articles identified by the above method were downloaded and screened for studies that deal with distal femur fracture and fixation. Secondly, the full texts of the shortlisted abstracts were downloaded and assessed for eligibility. The reference list of the final selected articles were searched for additional studies. Any disagreements between the authors were resolved with discussion and mutual agreement.
2.2. Eligibility criteria
The studies were included if (1) evaluated outcomes of distal femur fracture, (2) ORIF using swashbuckler approach as the primary surgical intervention, and (3) English language. The exclusion criteria included case reports, case series of fewer than 3 patients, letters to the editor, reviews, cadaveric studies, animal studies, and biomechanical studies.
2.3. Data extraction and analysis
The data extraction was done by two authors (B.K.B and S.C.) using a predetermined form. Data regarding the authors, journal, place/location of surgery, study design, level of evidence, sample size, surgery details, follow-up periods, and functional outcomes were extracted. The extracted data were entered in an MS excel sheet and if data was found to be inadequate, the authors were approached for the same. If data couldn't be retrieved, the article was avoided. Any disagreements were thoroughly discussed and the senior author (P.K.M) made the final decision.
2.4. Quality assessment
The quality assessment of the included articles would be assessed using the MINORs score.12 The score consists of 12 questions with each of the questions having individual scores of scored 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate). The non-comparative studies considered ideal if score 16 and 24 for comparative studies. However, the MINORs score would not be taken as a criterion for exclusion or inclusion in the study.
2.5. Surgical technique
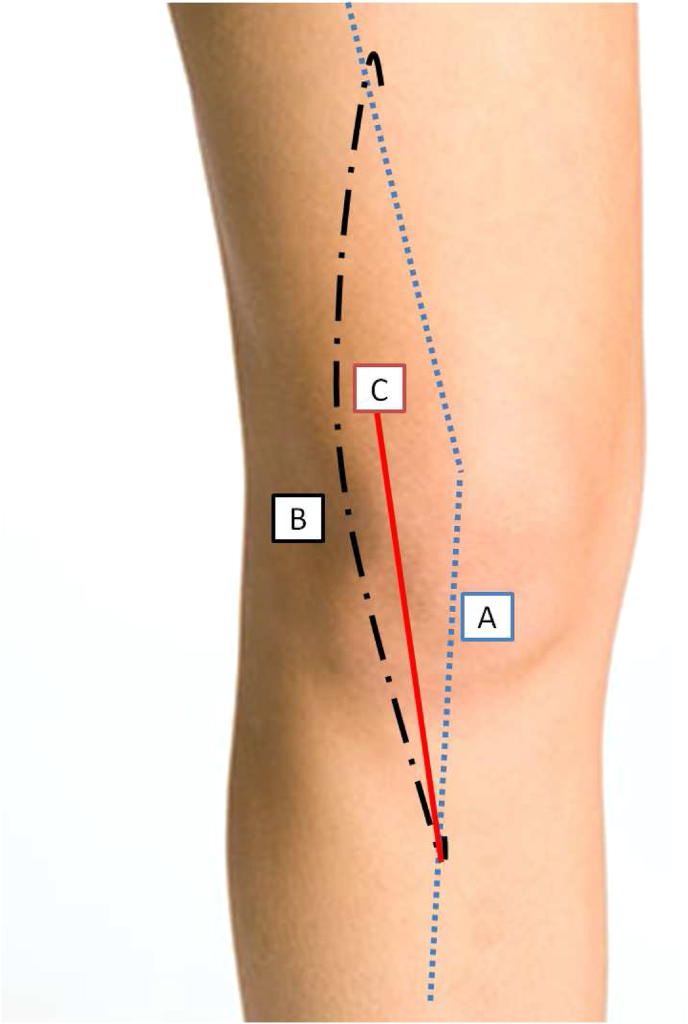
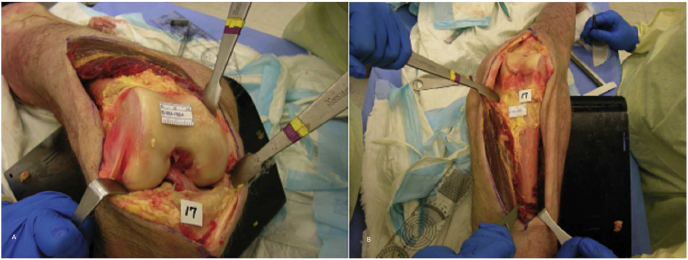
The patient is usually positioned supine with the knee flexed with a roll or triangle. A midline anterior knee incision is made from above the fracture laterally across the patella (Fig. 1). The incision is extended directly down to the fascia of the quadriceps and incised in line with the skin incision. The iliotibial band is bluntly retracted from the vastus lateralis muscle laterally. The vastus lateralis muscle is then detached from lateral intermuscular septum and quadriceps muscle is displaced medially to access distal femur. Further exposure distally includes lateral parapatellar arthrotomy to expose the femoral condyles.13 Perforating vessels may be ligated and vastus lateralis is elevated to completely expose the distal femur9 (Fig. 2).
Fig. 1.
Schematic Representation of the Incisions A: Classical Swashbuckler incision as described by Starr et al.B: Modified Swashbuckler incisioC: Mini Swashbuckler incision as described by Beltran et al.
Fig. 2.
Classical Swashbuckler approach exposure (image curtesy: Beltran MJ et al.: Articular exposure with the swashbuckler versus a "Mini-swashbuckler" approach. Injury. 2013).
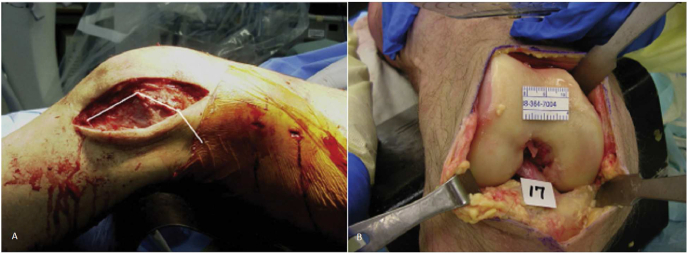
The main drawback of the Swashbuckler approach is the parapatellar arthrotomy which may undermine the lateral supply to the anastomotic patellar ring. Poor vascularization is considered one of the etiological factors for anterior knee pain and patellar stress fractures. The modified Swashbuckler approach is proposed by defining patellar anastomotic ring ‘safety margins’ while performing knee arthrotomy. So, in modified approach, arthrotomy is done with a minimum margin of 2 cm from the lateral border of the patellar tendon and at the base of the patella the incision deviated slightly, aiming for the posterior depression of the vastus lateralis till it reached the anterolateral aspect of the thigh.9,14 In the case of the Mini-swashbuckler approach, we can use a 12 cm incision from the lateral edge of the tibial tubercle upwards to the superolateral margin of patella15(Fig. 3). Full-thickness skin flaps are elevated to identify the underlying lateral patellar retinaculum. To expose the knee joint, a trapezoidal-shaped incision is made in the patellar retinaculum which remains within the lateral retinaculum and does not violate the vastus muscle belly. For extending proximally traditional Swashbuckler approach may be used.9
Fig. 3.
Mini Swashbuckler approach exposure (image curtesy: Beltran MJ et al.: Articular exposure with the swashbuckler versus a "Mini-swashbuckler" approach. Injury. 2013).
3. Results
3.1. Search results
The search yielded a total of 1790 results of which 314 duplicates were removed. Of 1476 screened, 1462 were removed after evaluating the title and abstract. Fourteen articles were downloaded for full-text review of which the final 11 made the list. A total of 11 studies with 369 knees were included in the review using the eligibility criteria.
3.2. Study characteristics
The average age of patients included 39.03 years (range: 30.7–44.9years) and 13.218 months(6–28months) was the average follow-up. 255 were males and 84 were females. A total of 11 studies were from 5 countries. Ten were prospective, one was retrospective studies. Nine studies used AO classification for fracture morphology. Of the included studies two focused on the outcomes of distal femur fractures AO type A,16,17 four on AO type B,14,17, 18, 19 and nine on AO type C.6,14, 15, 16, 17, 18, 19, 20, 21 Singh R et al. study utilized the approach for Hoffa fracture.22 Ahire et al.14 compared the lateral approach with the Swashbuckler approach and Xiang et al.15 compared the swashbuckler approach vs the mini swashbuckler approach. C3 fractures were the indications to operate in 7 studies, C2 in 5 and C1 in 4. Four studies used the approach for type B fractures.14,17, 18, 19 The follow-up period averaged 13.218 months with a range of 6 months–28 months and three studies had a follow-up of less than a year.17, 18, 19 The study characteristics are listed in Table 1 and an overview of clinical and functional outcomes are listed in Table 2.
Table 1.
Study characteristics of different studies included.
| Author | Study design | Journal | Location of study | Sample size | Mean age, M/F | Fracture classification | Follow up (mean) | Quality of studies (MINORS score) |
|---|---|---|---|---|---|---|---|---|
| YS Kumar 202116 | Prospective | IJHCR | India | 50 | 35. 1 ± 8. 3 years, 30/20 | Muller's type A, type B and type C fractures. | 10.6 month | 13 |
| Mustofa 202118 | Prospective | MT | Bangladesh | 30: randomized Group A:15 Group B: 15 |
DCS- 44.9 ± 12.9 year; 9/6 LCP: 42.6 ± 15.7 year; 10/5 |
AO type 33-B and 33-C fractures | 6 months | 18 |
| Obiegbu 202017 | Prospective | NJSS | Nigeria | 6 | 43.2, 1/5 | B2-2, B3-2, C2-1, C3-1 | 6 months | 12 |
| Chandra R 202015 | Prospective | IJOS | India | 30 | 30.7, 25/5 | A2-5, A3-6, C1-4, C2-10, C3-5 | 1 year | 11 |
| Singh DJ 20205 | Prospective | IJOS | India | 20 | 35.15,18/2 | NS (intercondylar and supracondylar fractures) | 1 year | 9 |
| Khan 2020†19 | Prospective | IJRO | India | 72 | 36.17, 59/13, | 42 closed, 30 open. C1-20, C2-50, C3-2 |
16.4 months | 19 |
| Xiang 2019†14 | Retrospective | CJRRS | China | 43. 22-MSA, 21-SA |
MS: 44.5, 15/7. S: 41.6, 13/8 | All closed fractures MS: C1-8, C2-10, C4-4. S: C1-7, C2-11, C3-3 | 7.2 months | 15 |
| Ahire R 2018†13 | Prospective | IJOS | India | 60. SA(Group B)-30 LA(Group A)-30 |
36.01. group A: 26/4, Group B: 29/1 | Group A: B1-1, B2-2, B3-0, C1-1, C2-16, C3-10. Group B: B1-1, C2-9, C3-20 | 1 year | 18 |
| Singh R 201721 | Prospective | MOJ | India | 7 (8 hoffa fragments: 5L/3 M) | 39.8, 5/2 | Hoffa's fracture | 28 ± 3.8 months | 10 |
| Agarwal A 201720 | Prospective | IJO | India | 12 | 44.3, 8/4 | C3 (2-open, 4 -had associated ligament injuries) | 17.6 months | 9 |
| Khalil 20156 | Prospective | COP | Egypt | 9 | 33.4, 7/2 | C3 (closed) | 17.6 months | 10 |
Foot note: NJSS: Nigerian Journal of Surgical Science; IJHCR: International Journal of Health and Clinical Research, MOJ: Malaysian Orthopedic Journal; IJO: Indian Journal of Orthopedics; CJRRS: Chinese Journal of Reparative and Reconstructive Surgery; MT: Medicine Today; IJRO: International Journal of Research in Orthopaedics; COP: Current orthopaedic Practice; IJOS: International Journal of Orthopedics Sciences; NS: Nothing Significant; L:Lateral; M:Medial; MSA: Mini-swashbuckler Approach; SA: Swashbuckler approach; LA: Lateral approach MINORS: Methodological Index for Non-Randomized Studies; DCS: Dynamic condylar screw; LCP: locking compression plate.
MINORS Score: The items are scored 0 (not reported), 1 (reported but inadequate) or 2 (reported and adequate). The global ideal score being 16 for non-comparative studies and 24 for comparative studies†.
Table 2.
Overview of clinical and functional outcomes.
| Author | Operative time (in minutes) | Blood loss (mL) | Length of stay (days) | Union time (in weeks) | Complications | Functional outcomes |
|---|---|---|---|---|---|---|
| YS Kumar 202116 | NS | NS | NS | 18 (10–36 wk) | 4 implant failure; 1 non-union; 1-deep infection; 1 knee pain requiring implant exit |
HSS Outcome: Excellent 28 (56%) Good 8 (16%), Fair 8 (16%), Failure 6 (12%) |
| Mustofa 202118 | DCS 92.3 ± 7.5 m LCP 90.4 ± 6.9 m |
NS | DCS 6.0 ± 0.9 LCP 5.9 ± 0.9 |
DCS 20.6 ± 5.0 LCP 18.7 ± 3.3 |
Superficial wound infection-5 Postoperative stiffness-7 Varus deformity-3 Implant failure-3 |
DCS group: excellent in 13.3%, good in 33.3%, fair in 33.3% poor in 20.0% cases LCP group: excellent in 53.3%, good in 20.0% fair in 6.7% poor in 20.0% of cases |
| Obiegbu 202017 | NS | NS | NS | 3.8 months (3–5 months) (100%) | NIL/NS | NEER's criteria. 4- excellent (67%), 1-good 1 fair (C3 PT) |
| Chandra R 202015 | 70 m (60–90) | NS | NS | 17, 100% | Delayed union-2, Superficial infection-5, |
n = 22 had (0–120) rom (73%). KSS: Excellent-80% (>80), Good-20% (70–79) |
| Singh DJ 20205 | 87.35 m | NS | NS | 17.35 (12–24). in 70% of patients | Superficial infection-1, restriction of motion-1 | KSS: Knee score: 83.70, Function score: 80.25. Excellent - 12, Good-5, Fair-3 |
| Khan 202019 | 90.19 ± 20.05. Open: 98.46 ± 22.47, Closed: 84.28 ± 18.32 | NS | NS | 15.64 ± 2.65. Closed: 14.52 ± 2.21, Open: 17.20 ± 2.44 |
Superficial wound infection and gaping-7, Malunion with varus-2, Limb length discrepancy-2, Knee stiffness-10, Chronic infection with sinus-4, Painful implant-1 (needed removal) |
ROM: 99.03 ± 24.73, Closed: 105.83 ± 19.41, Open: 89.50 ± 28.36. HSS (modified): 80.13 ± 13.38, Closed: 82.67 ± 10.81, Open: 76.67 ± 15.84. Excellent results- 35 patients overall (21 closed and 14 open), Good results-22 patients (15 closed and 7 open), Fair results-10 patients (5 each in closed and open fractures) poor results-5 (1 closed and 4open) |
| Xiang 201914 | MS: 96.23 ± 12.39. S: 78.00 ± 7.60 | MS: 265.18 ± 16.52 mL. S: 369.52 ± 11.33 mL |
MS: 17.73 ± 2.39 S: 17.52 ± 2.42 |
MS: 13.38 ± 1.24. S: 13.73 ± 1.39 |
MS: Varus deformity- underwent osteotomy, 1 implant loosening. S: Superficial infection-1, DVT-1. Flexion deficit-2, |
HSS score: MS: 89.28 ± 3.63. S: 81.48 ± 4.55. Difference statistically significant |
| Ahire R 201813 | Group A: 99.6, Group B: 85 | NS | NS | Group A: <3months-9, 3-6 months-21. Group B: <3 months-13, 3–6 months -17 |
Group A: Restriction of movement −4, Terminal extension lag-2, Superficial infection-2, Chronic swelling of limb-1. Group B: Restriction of movement-2, Terminal extension lag −2 |
Neer's Score: Group A; 76.96 ± 8.54, Excellent-13, Good-13, Fair-4. Group B: 81.83 ± 11.16, Excellent-19, Good-6, Fair-5. |
| Agrawal A 201720 | NS | NS | NS | 14.3 (6–26), 100% | Secondary bone grafting at 3 months-1. Radiological arthritis-3 (of which 1 symptomatic) |
ROM: 120° ± 14.8°. KSS score: Excellent-7, Good-3. Fair-2. |
| Singh R 201721 | NS | NS | NS | 16 union in all | NIL | ROM: 110 (90–120). KSS SCORE: 86(65–95) |
| Khalil 20156 | NS | NS | NS | 19.2 (13–27) (100%) | 2 stiff knee of which one needed quadricepsplasty. Delayed union-2. Iliac crest Pain-2, Prolonged rehabilitation-2 (had severe metaphyseal comminution), Exuberant callus-2, Superficial wound infection-1, Delayed wound healing-1 |
Sanders et al. method: excellent-3, Good-4, Fair-1, Poor-1. ROM 85-130 |
Foot note: NS: nothing significant; MS: Mini-Swashbuckler; S: Swashbuckler; ROM: Range of motion; HSS: Hospital for special surgery score; KSS: Knee society score; DCS: Dynamic condylar screw; LCP: locking compression plate; DVT; Deep Vein Thrombosis; m-minutes; wk-weeks.
3.3. Approach
In the study, all 11 authors used the Swashbuckler approach, and one study used the mini swashbuckler approach.15 We didn't find any study which commented upon the length of the incision. The majority of the authors used a length of incision determining the extension of fracture line or metaphyseal comminution.3,5,6,13,15,18,22 Most of the authors preferred a midline anterior incision.3,5,6,14,16,20,23 Agrawal et al. and Obiegbu et al. used a laterally based midline incision.18,21 Singh et al. and Obiegbu et al. used the modified swashbuckler approach where the vastus lateralis was separated.18,22 Quadriceps integrity was preserved in all cases of study by Khalil et al.6
3.4. Operative time
The operative time was recorded by 6 studies. One study14 compared the operative time between the lateral approach and swashbuckler approach and one study15 compared the swashbuckler approach and mini swashbuckler approach. Ahire et al. noted a longer duration of surgery for the lateral exposure group in comparison to the latter.14 Khan et al. noted that open fractures undergoing surgery with swashbuckler approach recorded more operative time than the closed fractures.20
3.5. Blood loss
Blood loss was assessed by Xiang et al. alone. He noted a larger volume of blood loss in the traditional swashbuckler group in comparison to the mini swashbuckler group.15
3.6. Length of stay
Length of stay was assessed by Xiang et al. The author noted a mean duration of 17 days in both the mini swashbuckler and the swashbuckler groups.15
3.7. Union
The radiological union rates were recorded by all 11 studies.5,6,14, 15, 16, 17, 18, 19, 20, 21, 22 The mean average of 16.2weeks with a range of 9weeks–27weeks was required for the union. Two studies commented on delayed union.6,16 No non-unions were recorded. Two cases of malunion were seen in the review.20 Ahire et al. noted that the union rates of distal femurs operated by lateral or swashbuckler approach were similar. The time for the union was less than 3 months for 13 and 3–6 months for 17 patients.14 Khan et al. noted that the open fractures required more meantime for union in comparison to closed fractures (17.20 vs 14.52 weeks).20 Xiang et al. noted similar union rates and time for the union for distal femur fractures operated using mini swashbuckler or swashbuckler approach.13
4. Complications
Overall, 89 complications were seen in the review. Two studies noted no complications.18,22 Superficial infection was the most commonly seen complication. Restriction of knee motion postoperatively was seen in five studies,5,6,14,19,20 out of which one required quadriceps-plasty.6 Superficial infection was seen in 7 studies and subsided with antibiotics.5,6,14, 15, 16,19,20 Five cases of deep infection with the sinus were seen.17,20 Post-operative radiological arthritis was seen in 3 out of which 1 was symptomatic.21
4.1. Functional outcomes
The scores seen used for functional outcomes in the review were heterogeneous. Range of motion, Hospital for special surgery (HSS) score Knee society score (KSS), Neer's, and other functional scores were used. In the review, 149 patients out of 339 postoperatively had excellent/good scores. Xiang et al. noted improved modified HSS scores for patients operated with mini swashbuckler in comparison with swashbuckler approach.15 Khan et al. noted more patients with closed fractures having excellent scores in comparison to patients with open fractures postoperatively.20 Ahire et al. noted that patients with the swashbuckler approach had a significantly higher Neer's score in comparison to patients who underwent open reduction internal fixation with lateral approach.14 The range of motion was assessed by five studies.6,16,20, 21, 22 The mean ROM postoperatively was ranging from 0∗ to 114.8∗. Overall, most studies noted a regain in the range of motion postoperatively. The restriction of movement was seen in five studies.5,6,14,19,20 Khan et al. noted a decreased ROM in the open fracture group in comparison to the closed fracture group.20
4.2. Quality of studies
The average minor score of the included studies was 12.18. The score consists of 12 questions with each of the questions having individual scores of scored 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate). The non-comparative studies considered ideal if score 16 and 24 for comparative studies.12 We had 7 non-comparative and 4 comparative studies. The score was not considered as an exclusion criterion.
5. Discussion
In this current review, we analyzed studies from the literature dealing with the swashbuckler approach for distal femur fractures. The swashbuckler or modified anterior approach was seen to provide excellent functional outcomes in 66.45%. We could find only one study which compared the swashbuckler approach with the traditional lateral approach for distal femur fractures.14
Distal femur fractures especially the AO type C with intraarticular involvement are often associated with difficulty in treating and obtaining an adequate reduction.6,15,24 The need for anatomical reduction of the intraarticular fragments is of paramount importance as untreated cases land up in post-traumatic arthritis.21 The lateral/lateral parapatellar approach in the distal femur often needs extensive tissue dissection and at times the intraarticular reductions are not proper. Various approaches have been introduced over the years to meet the need for adequate exposure in such cases. Starr et al. introduced the swashbuckler approach as an alternative for the lateral approach to decrease the amount of soft tissue injury and to limit the injury to the quadriceps belly.9 The use of this approach is often limited to C3 or comminuted intraarticular fractures.17,22 To the best of our knowledge, there is no systematic review that analyses the Swashbuckler approach, its indications, complications, and outcomes. The current systematic review is the first one to analyze the same.
The review revealed a dearth of literature on the Swashbuckler approach. Only 1 study was seen to compare the swashbuckler to the lateral approach.14 However, in this review, many outcomes measure of the surgery was evaluated as possible. The swashbuckler approach was seen to be predominantly used for the C2/C3 type of fractures.6,14, 15, 16,18,20,21 The need for more visualization of the fracture fragments intraarticularly is well satisfied with the exposure. Moreover, the current exposure was also seen to be used for Hoffa's fracture and particularly of the lateral femoral condyle.22 There are case reports of Hoffa's fracture being treated with a swashbuckler approach.4 The study revealed that using the Swashbuckler approach doesn't increase the chance of nonunion. The rates of complications were also similar.4,22
Ahire et al. compared the current approach with the lateral approach in the treatment of the distal femur fractures with 30 patients in each group. The patients were followed up for 1 year wherein the author noticed union in all cases but the lateral approach group was seen to have more major complications and significantly lesser functional outcomes.14 Khan et al. had the maximum number of knees operated with swashbuckler approach (n = 72), with 42 closed and 30 open fractures. The open group was associated with less postoperative function scores and more complications.20 Singh R et al. revealed the extended indication of using the swashbuckler approach in dealing with lateral Hoffa's fracture.22 Khalil et al. utilized the approach for 9C3 fracture patients and noted that postoperatively 2 had restriction of motion of which one required quadricepsplasty.6 Agarwal et al. used the approach to treat 12C3 fractures and had a follow-up of 17.6 months. Three cases of radiological arthritis were seen in the cohort of which one patient was symptomatic.21 Chandra et al. noted more than 80% of 30 patients operated for distal femur fractures had a KSS score excellent. However, 2 cases had a delayed union.16 Singh DJ et al. prospectively assessed 20 patients with intercondylar and supracondylar fractures over 1 year and noticed that 1 patient had restriction of movement postoperatively and in 70% of the patients the union was achieved in 17.35 weeks.5 Xiang et compared the mini swashbuckler approach with the swashbuckler approach in 43 patients. The author noted that compared with the Swashbuckler approach, the mini-Swashbuckler approach has limited visual field exposure leading to prolonged operation time and increased fluoroscopy times. However, the risks of complications do not increase as the mini approach is associated with less soft tissue injury, less blood loss and is conducive to the recovery of knee joint function after operation.15 Obiegbu et al. in their prospective study of 6 distal femur fractures noted no complications associated with the swashbuckler approach in the postoperative period.18
The current review sheds light on the available literature on the Swashbuckler approach for distal femur fractures. The exposure offers good visualization of the intraarticular fragments and can be extended proximally to include the metaphyseal fragments. The belly of the quadriceps is spared leaving the entire quadriceps mechanism intact which helps in the postoperative rehabilitation. The blood loss can be controlled if needed with a tourniquet if it doesn't alter the quadriceps action or come in the way of exposure. The swashbuckler approach offers more visualization of the medial condyle and trochlea in comparison to the lateral approach. Using the former approach often helps in limiting the use of medial parapatellar arthrotomy needed along with the lateral approach in cases of medial communication.9,24
The review has limitations. The main limitation was that there were very few studies in the literature that evaluated the use of the swashbuckler approach. More studies are required to adequately obtain the outcomes. Second, there was heterogeneity in the studies for evaluating the outcomes. Third, the protocol for this review was not preregistered or published elsewhere. Fourth, only one study was seen to compare the swashbuckler approach to the lateral approach.23 More randomized controlled trials comparing the various approaches to distal femur fractures will provide an answer to which is the best approach for distal femur fractures.
6. Conclusion
Swashbuckler approach offers itself as a viable option in cases of distal femur fractures, especially in AO type C. The quadriceps sparing approach provides excellent/good outcomes in approximately 66.45% of the patients and has a trivial complication rate. However, literature is lacking to show the superiority of the approach with the existing counterparts. To answer the question on which approach gives the best possible outcome in distal femur fractures more comprehensive comparative studies are needed.
References
- 1.Machhi D.R., Namsha D.B., Dindod D.V. Outcome of intra articular distal femur fracture treated with locking compression plate. Int J Orthop Sci. 2017;3(3):503–507. doi: 10.22271/ortho.2017.v3.i3h.81. [DOI] [Google Scholar]
- 2.Singer B.R., McLauchlan G.J., Robinson C.M., Christie J. Epidemiology of fractures in 15,000 adults: the influence of age and gender. J Bone Joint Surg Br. 1998;80(2):243–248. doi: 10.1302/0301-620x.80b2.7762. [DOI] [PubMed] [Google Scholar]
- 3.Daroch M.S., Vashisht D., Sreen S. Management of intra-articular fracture of distal femur with LCP and Lag screws in adults. International Journal of Research in Medical Sciences. 2017;5(4):1434–1438. doi: 10.18203/2320-6012.ijrms20171241. [DOI] [Google Scholar]
- 4.Solanki D.R., Tolani D.A., Asati D.S., Kansara D.H., Pathria D.V. AO type C distal femur fracture: results of operative management in 52 patients. Int J Orthop Sci. 2018;4(4):73–77. doi: 10.22271/ortho.2018.v4.i4b.16. [DOI] [Google Scholar]
- 5.Singh D.J., Singh D.P., Jain D.S., Singh D.G.P. Operative treatment of inter-condylar and supra-condylar fracture of femur by swashbuckler approach. Int J Orthop Sci. 2020;6(2):677–680. doi: 10.22271/ortho.2020.v6.i2k.2118. [DOI] [Google Scholar]
- 6.Khalil M.A., Farid W., Gad S. Swashbuckler approach and surgical technique in severely comminuted fractures of the distal femur. Current Orthopaedic Practice. 2015;26(3):269–276. doi: 10.1097/BCO.0000000000000226. [DOI] [Google Scholar]
- 7.Collinge C.A., Gardner M.J., Crist B.D. Pitfalls in the application of distal femur plates for fractures. J Orthop Trauma. 2011;25(11):695–706. doi: 10.1097/BOT.0b013e31821d7a56. [DOI] [PubMed] [Google Scholar]
- 8.Khlopas A., Samuel L.T., Sultan A.A., Yao B., Billow D.G., Kamath A.F. The Olerud extensile anterior approach for complex distal femoral fractures: a systematic review. J Knee Surg. Published online November. 2019;27 doi: 10.1055/s-0039-3400954. [DOI] [PubMed] [Google Scholar]
- 9.Starr A.J., Jones A.L., Reinert C.M. The “swashbuckler”: a modified anterior approach for fractures of the distal femur. J Orthop Trauma. 1999;13(2):138–140. doi: 10.1097/00005131-199902000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Beltran M.J., Blair J.A., Huh J., Kirby J.M., Hsu J.R. Skeletal trauma Research consortium(STReC). Articular exposure with the swashbuckler versus a “mini-swashbuckler” approach. Injury. 2013;44(2):189–193. doi: 10.1016/j.injury.2012.10.021. [DOI] [PubMed] [Google Scholar]
- 11.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Slim K., Nini E., Forestier D., Kwiatkowski F., Panis Y., Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 13.Harahap R. Surgical incision technique approach on distal femur fracture a literature review. Al-Iqra Medical Journal : Jurnal Berkala Ilmiah Kedokteran. 2021;4(1):31–39. doi: 10.26618/aimj.v4i1.4903. [DOI] [Google Scholar]
- 14.Ahire D.R., Jindal D.S., Phuljhele D.S., Sahu D.N.D., Kashyap D.G. A comparative study between swashbuckler approach (Modified Anterior Approach) and lateral approach for the distal femur fractures. Int J Orthop Sci. 2018;4(3):184–188. doi: 10.22271/ortho.2018.v4.i3d.34. [DOI] [Google Scholar]
- 15.Xiang C., Jiang K., Chen Q., Li Y., Bai H., Chen L. [Early effectiveness of mini-Swashbuckler approach for distal femoral type C fractures] Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2019;33(9):1127–1132. doi: 10.7507/1002-1892.201902073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chandra R., Chhabra A., Arora N.C., Taxak N. Clinical results after open reduction and internal fixation in distal femoral fractures with distal femoral locking compression plate (DF-LCP) using swashbuckler approach. Int J Orthop Sci. 2020;6(3):19–22. doi: 10.22271/ortho.2020.v6.i3a.2170. [DOI] [Google Scholar]
- 17.Kumar Y.S. A prospective study of surgical outcome of distal femoral fractures treated with locking compression plate. Int J Heal Clin Res. 2021;4(4):116–120. [Google Scholar]
- 18.Obiegbu Locking compression plate in distal intra-articular femoral fractures: the swashbuckler's approach. year=2018. https://www.njssjournal.org/article.asp?issn=1116-5898 volume=28;issue=2;spage=23;epage=25;aulast=Obiegbu.
- 19.Mustofa M.G., Rob C.F., Alam M.K., et al. Outcome of dynamic condylar screw with plate versus distal femoral lock compression plate fixation in fracture of distal femur. Med Today. 2021;33(1):45–49. doi: 10.3329/medtoday.v33i01.52159. [DOI] [Google Scholar]
- 20.Khan N.A., Atif A.M., Chatterjee A. Management of intercondylar femur fracture with distal femur locking compression plate: outcome analysis of 72 cases. International Journal of Research in Orthopaedics. 2020;6(5):1022–1026. doi: 10.18203/issn.2455-4510.IntJResOrthop20203725. [DOI] [Google Scholar]
- 21.Agrawal A., Kiyawat V. Complex AO type C3 distal femur fractures: results after fixation with a lateral locked plate using modified swashbuckler approach. Indian J Orthop. 2017;51(1):18–27. doi: 10.4103/0019-5413.197516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singh R., Singh R.B., Mahendra M. Functional outcome of isolated Hoffa fractures treated with cannulated cancellous screw. Malays Orthop J. 2017;11(2):20–24. doi: 10.5704/MOJ.1707.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agrawal D.S., Kanodia D.N., Patel D.P., Singhal D.D.K., Choudhary D.A., Singh D.M.P. Outcome following swashbuckler modified anterior approach versus lateral approach for management of complex distal femur fractures: a prospective comparative study. Nat J Clin Orthop. 2019;3(4):88–93. doi: 10.33545/orthor.2019.v3.i4b.183. [DOI] [Google Scholar]
- 24.Ghirardelli S., Touloupakis G., Theodorakis E., Antonini G., Violante B., Pier I. ”; 2021. A Modified Anterolateral Swashbuckler Approach for Distal Femoral Fractures: Description and Outcomes. [DOI] [PMC free article] [PubMed] [Google Scholar]