Abstract
Sporadic spreads of swine-origin influenza H3N2 variant (H3N2v) viruses were reported in humans, resulting in 437 human infections between 2011 and 2021 in the USA. Thus, an effective vaccine is needed to better control a potential pandemic for these antigenically distinct viruses from seasonal influenza. In this study, a candidate vaccine strain with efficient growth capacity in chicken embryos was established through serial blind passaging of A/Indiana/08/2011 (H3N2)v in mice and chicken embryos. Seven amino acid substitutions (M21I in PA; A138T, N165K, and V226A in HA; S312L in NP; T167I in M1; G62A in NS1 proteins) were found in the passaged viruses without a major change in the antigenicity. This mouse- and egg-adapted virus was used as a vaccine and challenge strain in mice to evaluate the efficacy of the H3N2v vaccine in different doses. Antibodies with high neutralizing titers were induced in mice immunized with 100 µg of inactivated whole-virus particles, and those mice were significantly protected from the challenge of homologous strain. The findings indicated that the established strain in the study was useful for vaccine study in mouse models.
Keywords: adaptation, H3N2 variant, influenza, mouse model, vaccine
Humans are periodically infected with influenza viruses that cause seasonal epidemics, making it a public health burden. Influenza viruses are enveloped negative-stranded RNA viruses with segmented genomes and belong to the family Orthomyxoviridae. Influenza A viruses have been classified into different subtypes based on their antigenic characteristics of surface glycoproteins, hemagglutinin (HA) and neuraminidase (NA), in which various subtypes are known (H1–H16 for HA and N1–N9 for NA) [9]. Currently, H1N1 and H3N2 subtype viruses are circulating in the human population [22]. It is well known that all influenza A viruses originate from waterfowl, which are natural reservoirs of influenza A viruses, and transmitted to birds and mammals, including pigs and humans. Genetic analysis illustrated that past pandemic viruses were circulating in the pig population and were transmitted to humans directly or after genetic reassortment [22, 23].
Vaccines are the most effective tool to reduce the impact of influenza virus infection on public health proactively, although antiviral drugs are currently available for treatment use [35]. For public health concerns, the candidate vaccine strains are regularly updated based on the monitoring of human influenza viruses, as well as animal influenza viruses which potentially emerge as pandemic influenza viruses in the future [35]. For developing an effective vaccine against human influenza, the selection of candidate vaccine strains and evaluation of vaccine potency using an appropriate animal model are required until the application to humans [5].
In 2011, swine-origin influenza H3N2 viruses sporadically affected the human population by direct contact with pigs in Indiana, USA, resulting in human infections with non-human H3N2 virus called variant H3N2 (H3N2v) [19, 31]. The documentation reported 437 cases of human infection with H3N2v viruses in 13 states presently, and the largest outbreak with 321 human cases was recorded during 2011–2012 [29, 35]. Even though reports of human infections with these H3N2v viruses decreased recently, there are still public health concerns for H3N2v infection in humans. This is because these viruses are antigenically distinct from the seasonal H3N2 influenza viruses and vaccines currently available vaccines against human seasonal H3N2 viruses are not cross-reactive to H3N2v viruses [13]. A serological surveillance study in Canada demonstrated that a substantial population of adolescents and young adults showed cross-reactivity to H3N2v viruses by seasonal influenza vaccine; however, children and older adults were considered to be widely susceptible to these viruses due to lack of cross-immunity [30]. These facts suggested that an effective vaccination strategy against the H3N2v virus infection, which raises concerns on potential future pandemics, should be established immediately.
Ferrets were susceptible to H3N2v viruses without any adaptations. The viruses replicated well and showed moderate pathogenicity in host animals [8, 31]. Accordingly, the evaluation of certain vaccines against H3N2v viruses was conducted in ferrets as well as their original host species, pigs, resulting in different levels of effectiveness in preventing their infections [8, 20]. Alternatively, these viruses were poorly replicated in mice [31]. No mouse model for H3N2v vaccine evaluation has been developed until presently. Another serious concern for vaccine development for H3N2v viruses is their poor replication potential in chicken embryos [1].
Our study aims to develop a suitable virus strain from an H3N2v virus, A/Indiana/08/2011 (H3N2)v [Ind/08/11], for the evaluation of egg-based vaccine against H3N2v virus infection in mice, by assessing viral growth in mice and chicken embryos, and immunogenicity of H3N2v whole-virus particle (WV) vaccine in mice. The adapted virus after serial passages in mice and chicken eggs did not cause major antigenic changes. The potency test was conducted in mice with homologous strain, mouse- and egg-adapted Ind/08/11 virus, which was used for both vaccine preparation and challenge study in mice. Inactivated H3N2v WV vaccine with 100-µg dose conferred high immunity enough to protect clinically and reduce the viral growth in mouse lungs.
MATERIALS AND METHODS
Viruses and cells
Human influenza virus, Ind/08/11 was kindly provided by Dr. Richard Webby, the St. Jude Children Research Hospital, Memphis, TN, USA. Madin-Darby canine kidney (MDCK) cells were maintained in minimum essential medium (MEM; Nissui Pharmaceutical, Tokyo, Japan), supplemented with 0.3-mg/ml L-glutamine (Nacalai Tesque, Kyoto, Japan), 100 U/ml penicillin G (Meiji Seika Pharma, Tokyo, Japan), 0.1 mg/ml streptomycin (Meiji Seika Pharma), 8 mg/ml gentamicin (Takara Pharmaceutical, Saitama, Japan), and 10% fetal calf serum (FCS; Sigma-Aldrich, St. Louis, MO, USA) to propagate influenza viruses. Virus stocks were propagated in MDCK cells at 35°C under 5% CO2 or in 10-day-old chicken embryos at 35°C, for 48 hr. The infectious fluids were stored at −80°C until use.
Virus titration
Ten-fold serial dilutions of viruses in serum-free MEM were inoculated into MDCK cells. The cells were incubated in serum-free MEM supplemented with 5 µg/ml trypsin acetylated (Sigma-Aldrich) at 35°C under 5% CO2 for 72 hr. The presence of cytopathic effects (CPE) of infected cells was judged, and 50% tissue culture infective dose (TCID50) was calculated by the Reed and Muench method [26]. For viruses exhibiting unclear CPE into MDCK cells, virus titration was performed by immunoperoxidase (IPX) staining assay with slight modification from Kameyama et al. [11] using polyclonal chicken antisera against A/Hong Kong/4801/2014 (H3N2) and anti-chicken IgG horseradish peroxidase-conjugated antibody (Bethyl Laboratory, Montgomery, TX, USA). For the evaluation of the result of the IPX assay, the reactivity of viral antigen was recorded as negative (−) and positive (1+ to 4+), and the virus titers were introduced by calculating TCID50.
Blind passages of Ind/08/11 virus in mice and chicken embryos
Five 8-week-old female BALB/c mice (Japan SLC, Hamamatsu, Japan) were intranasally inoculated with 105.2 TCID50/50 µl of Ind/08/11 at the first passage under intraperitoneal administration of an anesthetic reagent [15]. At 3 days of post-challenge (dpc), mice were euthanized using thiopental sodium (Nipro ES Pharma, Osaka, Japan), and their lungs were collected. Lung homogenates were prepared using a Multi-Beads Shocker (Yasui Kikai, Osaka, Japan) to make 10% (w/v) suspension in a viral transport medium. The pooled homogenates were inoculated into MDCK cells, and the supernatants were further passaged in mice. The virus obtained from blind passages in mice was 10-fold serially diluted and inoculated into the allantoic cavities of two 10-day-old chicken embryos. All the embryos were incubated at 35°C for 48 hr, and allantoic fluids were collected separately. In each dilution, pooled allantoic fluids were directly inoculated into two 10-day-old chicken embryos for the following passage. Virus titers and HA titers were monitored throughout all egg passages. Finally, mouse- and egg-adapted Ind/08/11 (Ind/08/11 ma-P7/e-P3) was obtained through seven times passage in mice and three times passage in chicken embryos.
Characterization of a developed strain
For detailed characterization of Ind/08/11 ma-P7/e-P3, amino acid substitutions in all viral proteins were determined, and growth potentials were assessed in chicken embryos and mice. The amino acid substitutions in the viral proteins of the developed strain was identified by nucleotide sequencing of the genes as previously described [7]. Briefly, the RNA extracted using TRIzol LS Reagent (Life Technologies, Carlsbad, CA, USA) was reverse-transcribed using the Uni12 primer and M-MLV reverse transcriptase (Promega, Madison, WI, USA). The full-length of each of eight viral segments was amplified via polymerase chain reaction using gene-specific primer sets and Ex Taq polymerase (Takara Bio, Kusatsu, Japan). Direct sequencing of the all gene segments was performed using a BigDye Terminator version 3.1 Cycle Sequencing Kit (Life Technologies) and a 3500 Genetic Analyzer (Life Technologies). Amino acid substitutions in the viral proteins between Ind/08/11 and Ind/08/11 ma-P7/e-P3 were analyzed using GENETYX network version 12.0 (Genetyx Co., Tokyo, Japan). The H3-numbering system was referred to determine the amino acid position in the HA [34].
In order to assess growth potentials, Ind/08/11 or Ind/08/11 ma-P7/e-P3 with 102.0 TCID50/0.1 ml was inoculated into 10-day-old chicken embryos and incubated at 35°C. Allantoic fluids were collected at 0, 12, 24, 36, 48, and 72 hr of post-inoculation (hpi) to assess the virus growth expressed by TCID50 in MDCK cells and HA titers.
To assess growth potentials of viruses in mouse lungs, eight 8-week-old female BALB/c mice were intranasally challenged either with 105.2 TCID50/30 µl of Ind/08/11 or 105.0 TCID50/30 µl of Ind/08/11 ma-P7/e-P3 under anesthesia. At 3 dpc, four mice in each group were euthanized, and their lungs were collected for making 10% (w/v) of lung homogenates to investigate virus growth. The body weights of the other mice were monitored daily for weight loss and clinical signs until 14 dpc.
Assessment of antigenicity in the developed strain
For the vaccine preparation, the candidate vaccine strain, Ind/08/11 ma-P7/e-P3, was propagated in 10-day-old chicken embryos. After inactivation of infectious allantoic fluid with 0.1% formalin at 4°C for 7 days, the virus was purified using the methods of ultracentrifugation and sedimentation through a sucrose gradient, as modified from Kida et al. [14]. The total protein concentration was measured using the Pierce™ BCA Proteins Assay Kit (Thermo Fisher Scientific, Waltham, MA, USA).
Five 4-week-old mice were administered with the inactivated vaccine containing 100-µg purified Ind/08/11 ma-P7/e-P3 by subcutaneous injection, and double doses were given a two-week interval. Blood samples were collected from the tail vein of mice after two weeks of the second immunization.
Neutralizing antibody (NT) titers in mouse serum samples were measured using serum neutralization test (SNT). All serum samples were treated by heating at 56°C for 30 min and were mixed with 100 TCID50 of the virus, then incubated at room temperature for 1 hr. This mixture was inoculated onto MDCK cells and incubated at 35°C under 5% CO2 for 1 hr. After washing unbounded viruses by serum-free MEM, the cells were subsequently incubated with serum-free MEM containing 5 µg/ml acetylated trypsin. After incubation for 72 hr, CPE was monitored, and the NT titer of each serum sample was determined as the reciprocals of serum dilution resulting in 50% inhibition of CPE of 100 TCID50 of the virus.
Potency test of H3 vaccine against Ind/08/11 in mice
The potency test of the inactivated vaccine prepared by purified viruses was conducted based on the previous study [6]. Briefly, the inactivated vaccine containing 4-, 20-, and 100-µg purified Ind/08/11 ma-P7/e-P3 was administered subcutaneously twice with a two-week interval into 10 4-week-old female BALB/c mice in each dose group. Phosphate buffered saline (PBS) was administered as containing without purified viruses as a control group. Blood samples were collected from the tail vein after two weeks of each immunization, and NT titer in the serum was measured by the SNT test. After the second blood correction, all the mice were challenged intranasally with 105.0 TCID50/30 µl of Ind/08/11 ma-P7/e-P3 strain under the anesthesia. At 3 dpc, the 5 mice from each group were euthanized to collect their lungs for measuring viral growth. The other 5 mice were monitored daily for their weights and clinical manifestations until 14 dpc.
Statistical analysis
The Student’s t-test was applied to confirm differences in the body weight of mice, virus recovery, and NT titer between the two groups. A P-value less than 0.05 was considered significant.
Ethics statement
All animal experiments were performed in the animal BSL-3 facility at the Faculty of Veterinary Medicine of Hokkaido University and were approved by the Institutional Animal Care and Use Committee of the Faculty of Veterinary Medicine, Hokkaido University (Approval number: 16-0105 and 21-0016). All experiments were conducted per the guidance of this committee. The Faculty of Veterinary Medicine, Hokkaido University, has been accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International (AAALAC International) since 2007. In all mouse experiments, the humane endpoint was determined as 70% of body weight at the challenge.
RESULTS
Establishment of a candidate vaccine strain Ind/08/11 ma-P7/e-P3 and its growth in mice and chicken embryos
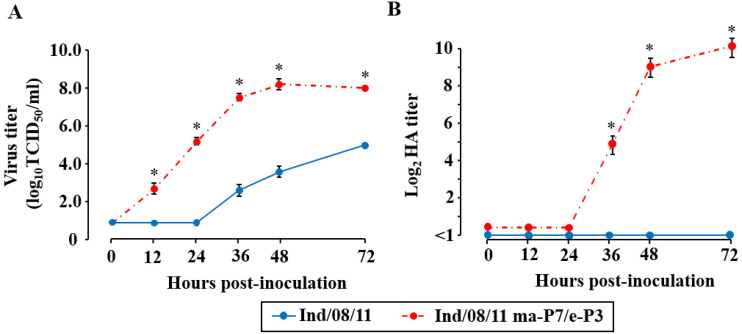
Even though the maximum titer (105.2 TCID50/head) of Ind/08/11 was intranasally inoculated into mice, none of the challenged mice died, and the viruses were only recovered from lungs of 2 out of 5 mice with virus titers less than 104.0 TCID50/g (data not shown). To select the virus that sufficiently replicates in the mouse lung, the virus was passaged seven times in mice. Furthermore, mouse-adapted Ind/08/11 was serially passaged three times in chicken embryos to improve virus replication in eggs. The growth ability of two viruses, Ind/08/11 and Ind/08/11 ma-P7/e-P3, were compared and assessed in chicken embryos. Ten-day-old chicken embryos were inoculated with these viruses with 102.0 TCID50/0.1 ml, and viral growth was monitored at different time points (Fig. 1). The virus titers of the passaged virus reached 108.1 TCID50/ml at 48 hpi, whereas those of the parental virus were at most 104.9 TCID50/ml at 72 hpi. In addition, the virus growth with significant HA titers was observed from 36 hpi in the passaged virus, whereas no detectable HA activity was observed in the parental virus. The results indicated that Ind/08/11 ma-P7/e-P3 showed higher replication capacity in chicken embryos compared with the parental virus.
Fig. 1.
Growth kinetics of Ind/08/11 (H3N2)v viruses in chicken embryos. The viral growth was assessed using three chicken embryos inoculated with viruses of 102.0 50% tissue culture infective dose (TCID50) per 0.1 ml for 72 hpi. The viral growth was quantitatively indicated by TCID50 in Madin–Darby canine kidney (MDCK) cells (A) and by hemagglutination (HA) titer using chicken red blood cells (B) at each time point. The blue line and dash-dotted red line represented Ind/08/11 and Ind/08/11 ma-P7/e-P3, respectively. Asterisk indicated a significant difference between the Ind/08/11 and Ind/08/11 ma-P7/e-P3 groups (P<0.05) at each time point.
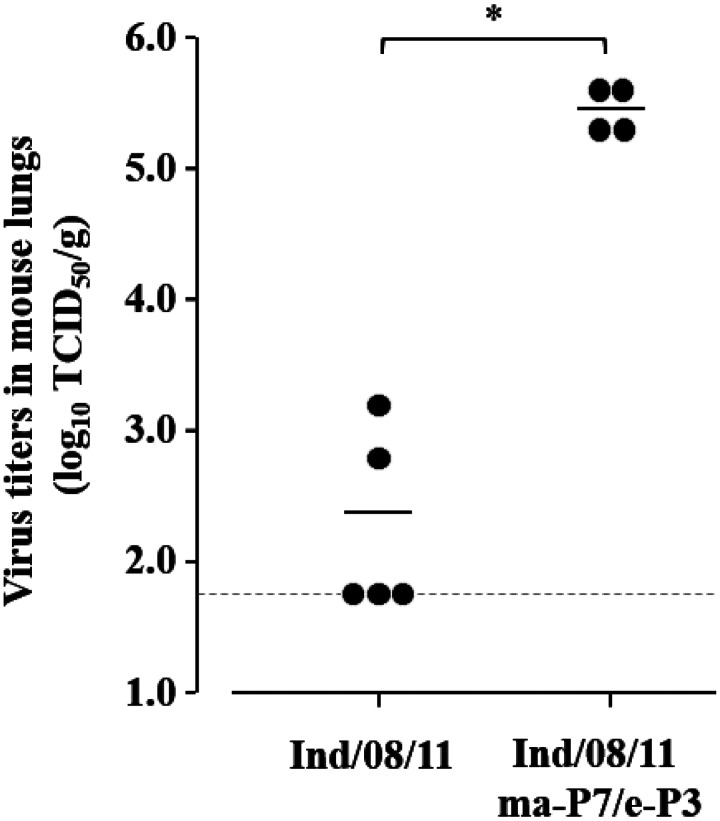
Moreover, mice were challenged with Ind/08/11 or Ind/08/11 ma-P7/e-P3 to compare their replication ability in mice. For the challenge study, 4 mice were inoculated with 105.0 TCID50/head of Ind/08/11 ma-P7/e-P3, and the other 5 mice were inoculated with 105.2 TCID50/head of Ind/08/11 (the maximum dose in the MDCK cell culture). At 3 dpc, viral growth in the lungs of the challenged mice was assessed (Fig. 2). The parental Ind/08/11 virus was recovered from 2 out of the 5 mice, and the virus titers were ranged between 102.7 and 103.3 TCID50/g. On the other hand, Ind/08/11 ma-P7/e-P3 virus was recovered from all 4 mice with significantly higher titers in their lungs as an average titer 105.5 TCID50/g. All the mice survived after the challenge for the 14 days (data not shown). Based on these results, a challenge strain was successfully established for the evaluation of the Ind/08/11 ma-P7/e-P3 vaccine, although it is sublethal in mice.
Fig. 2.
Virus recovery of Ind/08/11 (H3N2)v viruses from mice after serial passages. Lungs of mice inoculated with Ind/08/11 or Ind/08/11 ma-P7/e-P3 were collected at 3 dpc. Virus titers of each mouse lungs were expressed as dots, and the average virus titer in the group are indicated with bars. The dashed line indicates the lower detection limit of virus titration (101.8 50% tissue culture infective dose (TCID50) per gram). Asterisk showed the significant difference (P<0.05) under the hypothesis that the titer below than lower limit is set as 101.8 TCID50/g, which may provide the highest significant titer in the group.
Amino acid substitutions on Ind/08/11 ma-P7/e-P3 and antigenicity analysis
During these blind passages, seven amino acid substitutions were observed in viral proteins, M21I in PA, A138T, N165K, and V226A in HA, S312L in NP, T167I in M1, and G62A in NS1. Of these, two amino acid substitutions, A138T and N165K, were recognized on the head domain of the HA protein, and the other substitution, V226A, was found on the receptor-binding site of the HA protein. Antigenic correlation of Ind/08/11 ma-P7/e-P3 with the parental Ind/08/11 strain was assessed by the SNT test using mouse sera after immunization with Ind/08/11 ma-P7/e-P3 (Table 1). Two to 4-fold differences were observed between titers against the parental and passaged viruses in each serum. This indicated that after serial passages in mice and chicken eggs, the antigenicity of Ind/08/11 ma-P7/e-P3 changed slightly, but not remarkably. Overall, the viruses derived from serial passages in mice and chicken embryos were potentially replicated well in both of them, and this Ind/08/11 ma-P7/e-P3 virus was used as a candidate strain for the vaccine preparation and challenge studies.
Table 1. Neutralizing antibody titers of immunized mice against two virus strains.
| Vaccine strain | Ind/08/11* |
Ind/08/11 ma-P7/e-P3 |
||
|---|---|---|---|---|
| Titers in each mouse | GM | Titers in each mouse | GM | |
| Ind/08/11 ma-P7/e-P3 | 80, 160, 160, 160, 160 | 139 | 160, 320, 320, 640, 640 | 368 |
Ind/08/11, A/Indiana/08/2011 (H3N2)v; Ind/08/11 ma-P7/e-P3, mouse- and egg-adapted A/Indiana/08/2011 (H3N2)v after seven passages in mice and three passages in chicken embryos; GM, geometric mean. *Titration of neutralizing antibody using Ind/08/11 was assessed by IPX staining assay.
Potency of the vaccine against H3N2v virus in mice
The vaccine was prepared from Ind/08/11 ma-P7/e-P3 virus and injected twice into mice in three different doses to conduct the potency test. Table 2 shows NT titers of the serum samples collected from immunized mice against homologous strain. The induction of neutralizing antibodies was observed in a dose-dependent manner. After the second immunization, NT titers induced with 100 µg of the vaccine were ranged between 160 and 640 (geometric mean (GM) titer, 403). Alternatively, in the 20-µg groups, the GM of induced antibody titers was 202. NT titers in serum collected from the 4-µg group ranged from 40 to 80, and GM titer was 66.
Table 2. Neutralizing antibody titers of immunized mice in three different doses against Ind/08/11 ma-P7/e-P3.
| Vaccine dose (µg) | Titers in each mouse | GM |
|---|---|---|
| 4 | 40, 40, 80, 80, 80, 80, 80, 80, 80, 80 | 66 |
| 20 | 80, 160, 160, 160, 160, 320, 320, 320, 320, 320 | 202 |
| 100 | 160, 320, 320, 320, 320, 640, 640, 640, 640, 640 | 403 |
| PBS | <20, <20, <20, <20, <20, <20, <20, <20, <20, <20 | <20 |
Ind/08/11 ma-P7/e-P3, mouse- and egg-adapted A/Indiana/08/2011 (H3N2)v after seven passages in mice and three passages in chicken embryos; GM, geometric mean; PBS, phosphate buffered saline.
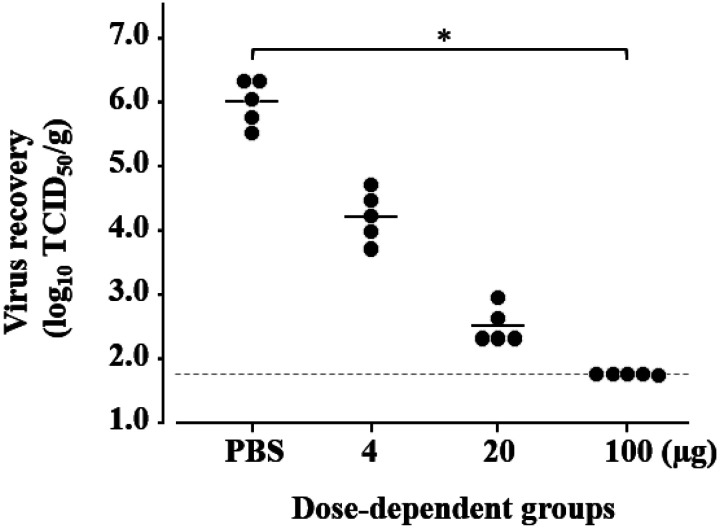
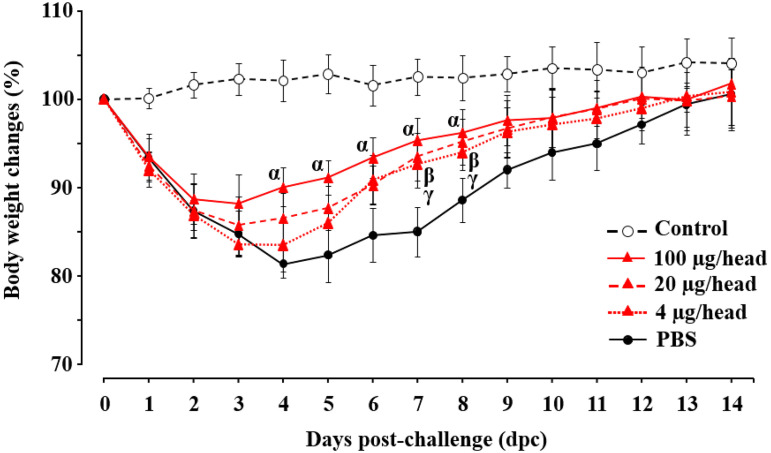
Then, the mice were challenged with 105.0 TCID50/head of homologous strain. Five mice were euthanized at 3 dpc, and their lungs were collected for assessing viral growth in mice (Fig. 3). In the PBS group, the challenge virus was recovered at a relatively high titer (105.5–106.3 TCID50/g) at 3 dpc, whereas no virus was detected in the mice immunized with the highest dose of the vaccine. Additionally, viral growth was apparently suppressed in the mice immunized with 4 or 20 µg of the vaccine. All challenged mice even immunized or non-immunized, showed a significant reduction in body weight compared with the no challenge group (Fig. 4). Among them, the significant differences in body weight were observed between the groups of the 100-µg and PBS from 4 to 8 dpc, and the body weight of the mice in the 100-µg group more quickly recovered than those in other groups. In the 20-µg group, body weights decreased until 3 dpc and slightly recovered; this was significantly different at 7 and 8 dpc compared with that of the PBS group. The same pattern of body weight change was observed in the 4-µg group, although a slightly severe reduction of body weight was observed compared with those of the 20-µg group. Overall, the vaccine prepared from Ind/08/11 ma-P7/e-P3 induced enough immunity in mice with decreasing the impact of disease caused by the homologous challenge strain.
Fig. 3.
Virus recovery from the lungs of immunized mice after the challenge. Five mice in each vaccine-dose group were challenged with 105.0 50% tissue culture infective dose (TCID50) per 30 µl of the homologous strain, Ind/08/11 ma-P7/e-P3, after two times of subcutaneous vaccination with 4, 20, and 100 µg of the vaccine strain, as well as without antigen (Phosphate Buffered Saline (PBS)), respectively. Viruses in the lungs were titrated from the mice in each group at 3 dpc. Virus titers of individual lung samples were expressed as dots, and the geometric mean of virus titers in the group is shown with the bar. The dashed line indicates the lower detection limit of the virus titration (101.8 TCID50/g). Asterisk indicated the significant difference (P<0.05) under the hypothesis that the titer below than lower limit is set as 101.8 TCID50/g, which may provide the highest considerable titer in the group.
Fig. 4.
Body weight changes of immunized mice after virus challenge. Five mice in each vaccine-dose group were challenged with 105.0 50% tissue culture infective dose (TCID50) per 30 µl of the homologous strain, Ind/08/11 ma-P7/e-P3, after two times of subcutaneous vaccination with 4, 20, and 100 µg of the vaccine strain, as well as without antigen (Phosphate Buffered Saline (PBS)), respectively. Body weight of the mice was monitored daily for 14 days after the challenge. An average of the body weight proportion on each post-challenge day to day 0 was indicated with open (no challenge) or closed points with lines (vaccinated in different doses). In the figure, α, β, and γ indicate the significant difference from the PBS group to the 100-, 20-, or 4-µg dose groups (P<0.05), respectively.
DISCUSSION
Vaccination is one of the strongest measures to control transmissible diseases, including influenza. This is by suppressing the impact of disease manifestation by inducing acquired immunity in the host. In previous studies, a failure to confer protective immunity against H3N2v virus on naïve host was confirmed by low cross-reactivity of it to recently available influenza vaccines in humans [10]. It should be essential to establish specific vaccine strains for H3N2v viral infections and their evaluation models. The pathogenicity of H3N2v viruses in different animal models, including mouse, ferret, and pig, had been assessed in previous studies [12, 31]. The H3N2v viruses caused moderate pathogenicity in ferrets with slight body weight loss, whereas they showed low pathogenicity with limited replication in mice. With these findings, there was a concern raised to develop adequate virus strains that can replicate in mice to evaluate vaccine efficacy in vivo settings. Indeed, in the study, parental Ind/08/11 was recovered from only 2 out of 5 mice inoculated (Fig. 2). Alternatively, candidate strains for vaccine production should be antigenically close to circulating viruses and confer protective immunity against them. Generally, influenza vaccines were produced in chicken eggs [3, 6, 33]. However, viruses isolated from humans do not grow efficiently in embryonated chicken eggs, which may a negative impact on vaccine development.
In this study, the H3N2v virus replicated more efficiently in mice than the parental virus after ten passages (Fig. 2). Due to multiple passages in mice and embryonated chicken eggs, amino acid substitutions were confirmed at HA, PA, NP, M1, and NS1 proteins, whereas no mutation was observed in PB2, PB1, and NA. Three amino acid substitutions, A138T, N165K, and V226A, were found in HA proteins. Among them, two amino acid substitutions (A138T and N165K) were in the head domains of the HA protein near antigenic sites A and B [34], and the mutation N165K was previously reported to contribute to viral replication in mouse lung [32]. Interestingly, the mutation N165K was also observed in the independent egg adaptation study of the Ind/08/11 strain conducted by Barman et al. [1]. The other amino acid substitution of V226A was recognized at position 226 which should be a critical determinant for host adaptation [27] and contributed to high affinity to host cells [21]. The single adaptive mutations at the positions 156, 186, and 228 that were found during the previous egg adaptation studies led to antigenic changes [16, 17]. Moreover, the amino acid substitutions were observed in PA (M21I), NP (S312L), M1 (T167I), and NS1 (G62A) proteins, respectively. The mutation M21I in PA was identified in the previous passage study of A/Hong Kong/1/1968 (H3N2) strain in mice [25]. Although a detailed mechanism was not revealed, the site was known to be located in the PA endonuclease domain [25, 28]. Contributions of the other mutations to egg or mice adaptations were not known. The amino acid position 312 of NP protein is located in the body domain [36]. The amino acid position 167 of M1 protein is located in the C-terminal region, which is involved in the M1–RNP interaction [37]. The amino acid position 62 of NS1 protein is located in the N-terminal region, which is involved in the double-strand RNA binding [4]. Overall, these mutations could contribute to the enhanced pathogenicity in mice and virus propagation in eggs, although further studies are needed to elucidate the detailed molecular mechanisms.
Influenza vaccine strains are generally established through egg adaptation [5, 24]. On the other hand, our established strain, Ind/08/11 ma-P7/e-P3, underwent the mice-adaptation process in addition to egg adaptation. Indeed, the passaged virus possessed amino acid mutations that were related to the growth in mice rather than growth in eggs (i.e., N165K in HA and M21I in PA). Although the major antigenic change was not observed between the parental and passaged viruses (Table 1), unnecessary mutation in adaptation process should be avoided to maintain the original character of the virus in vaccine development. In this context, Ind/08/11 ma-P7/e-P3 may not be ideal for actual human-use vaccine strain. However, serial passages in mice could not be avoided to obtain the mice-adapted strain to evaluate the vaccine efficacy in the challenge study using mice. Nevertheless, our Ind/08/11 ma-P7/e-P3 strain conferred protective immunities to mice in the homologous challenge (Table 2 and Fig. 3). This suggests that our established animal model gives a critical reference for further vaccine efficacy tests against H3N2v viruses, including vaccination with a heterologous strain or adjuvant efficacy.
The present study confirmed the high immunogenicity of the WV vaccines using mouse models. Our previous study demonstrated that the WV vaccine had higher immunogenicity than currently available ether-split vaccines [24]. However, current technological advance provides novel platforms for the vaccine, i.e., mRNA, plasmid, viral vector, etc. [18]. Additionally, the use of adjuvant or other immune modulators that stimulate innate immunity is discussed to enhance vaccine efficacy [2]. Mouse models should be initially employed for the evaluation of these platforms in the previous studies. It is therefore important to evaluate each platform by comparing its efficacy with the WV vaccine using mouse models. Our established model significantly contributes to the future preparation of developing an effective vaccine for humans against H3N2v infection, under a concept of better response for a potential pandemic.
CONFLICT OF INTEREST
The authors have nothing to disclose.
Acknowledgments
We greatly thank to Dr. Richard Webby, St. Jude Children Research Hospital, for kindly providing Ind/08/11 virus used in the study. This research work was supported by the World-leading Innovative and Smart Education (WISE) Program (1801) from the Ministry of Education, Culture, Sports, Science, and Technology, Japan. The study was partially provided by the Japan International Cooperation Agency (JICA) within the framework of the Science and Technology Research Partnership for Sustainable Development (SATREPS), grant number JP20jm0110019.
REFERENCES
- 1.Barman S., Franks J., Turner J. C., Yoon S. W., Webster R. G., Webby R. J.2015. Egg-adaptive mutations in H3N2v vaccine virus enhance egg-based production without loss of antigenicity or immunogenicity. Vaccine 33: 3186–3192. doi: 10.1016/j.vaccine.2015.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caldera F., Mercer M., Samson S. I., Pitt J. M., Hayney M. S.2021. Influenza vaccination in immunocompromised populations: Strategies to improve immunogenicity. Vaccine 39 Suppl 1: A15–A23. doi: 10.1016/j.vaccine.2020.11.037 [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention.2020. How influenza (Flu) vaccines are made? https://www.cdc.gov/flu/prevent/how-fluvaccine-made.htm [accessed on June 7, 2021].
- 4.Chien C. Y., Xu Y., Xiao R., Aramini J. M., Sahasrabudhe P. V., Krug R. M., Montelione G. T.2004. Biophysical characterization of the complex between double-stranded RNA and the N-terminal domain of the NS1 protein from influenza A virus: evidence for a novel RNA-binding mode. Biochemistry 43: 1950–1962. doi: 10.1021/bi030176o [DOI] [PubMed] [Google Scholar]
- 5.European Medicines Agency.2017. Guidence on influenza vaccine −Quality module. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-influenza-vaccines-quality-module-revision-1_en.pdf [assessed on Aug 16, 2021].
- 6.Hayashi H., Isoda N., Bazarragchaa E., Nomura N., Matsuno K., Okamatsu M., Kida H., Sakoda Y.2020. Potency of an inactivated influenza vaccine against a challenge with A/Swine/Missouri/A01727926/2015 (H4N6) in mice for pandemic preparedness. Vaccines (Basel) 8: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoffmann E., Stech J., Guan Y., Webster R. G., Perez D. R.2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 146: 2275–2289. doi: 10.1007/s007050170002 [DOI] [PubMed] [Google Scholar]
- 8.Houser K. V., Pearce M. B., Katz J. M., Tumpey T. M.2013. Impact of prior seasonal H3N2 influenza vaccination or infection on protection and transmission of emerging variants of influenza A(H3N2)v virus in ferrets. J. Virol. 87: 13480–13489. doi: 10.1128/JVI.02434-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Howley M., Knipe D.2020. Orthomyxoriruses. pp. 649–673. In: Fields Virology: Emerging Viruses, 7th ed., Wolters Kluwer, Philadelphia. [Google Scholar]
- 10.Johnson C., Hohenboken M., Poling T., Jaehnig P., Kanesa-Thasan N.2015. Safety and immunogenicity of cell culture-derived A/H3N2 variant influenza vaccines: a phase I randomized, observer-blind, dose-ranging study. J. Infect. Dis. 212: 72–80. doi: 10.1093/infdis/jiu826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kameyama K., Sakoda Y., Tamai K., Igarashi H., Tajima M., Mochizuki T., Namba Y., Kida H.2006. Development of an immunochromatographic test kit for rapid detection of bovine viral diarrhea virus antigen. J. Virol. Methods 138: 140–146. doi: 10.1016/j.jviromet.2006.08.005 [DOI] [PubMed] [Google Scholar]
- 12.Kaplan B. S., Kimble J. B., Chang J., Anderson T. K., Gauger P. C., Janas-Martindale A., Killian M. L., Bowman A. S., Vincent A. L.2020. Aerosol transmission from infected swine to ferrets of an H3N2 virus collected from an agricultural fair and associated with human variant infections. J. Virol. 94: 1–15. doi: 10.1128/JVI.01009-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keitel W. A., Jackson L. A., Edupuganti S., Winokur P. L., Mulligan M. J., Thornburg N. J., Patel S. M., Rouphael N. G., Lai L., Bangaru S., McNeal M. M., Bellamy A. R., Hill H. R., VTEU H3N2v Vaccine Study Work Group. 2015. Safety and immunogenicity of a subvirion monovalent unadjuvanted inactivated influenza A(H3N2) variant vaccine in healthy persons ≥18 years old. J. Infect. Dis. 212: 552–561. doi: 10.1093/infdis/jiv056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kida H., Brown L. E., Webster R. G.1982. Biological activity of monoclonal antibodies to operationally defined antigenic regions on the hemagglutinin molecule of A/Seal/Massachusetts/1/80 (H7N7) influenza virus. Virology 122: 38–47. doi: 10.1016/0042-6822(82)90375-0 [DOI] [PubMed] [Google Scholar]
- 15.Kirihara Y., Takechi M., Kurosaki K., Kobayashi Y., Kurosawa T.2013. Anesthetic effects of a mixture of medetomidine, midazolam and butorphanol in two strains of mice. Exp. Anim. 62: 173–180. doi: 10.1538/expanim.62.173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kishida N., Fujisaki S., Yokoyama M., Sato H., Saito R., Ikematsu H., Xu H., Takashita E., Tashiro M., Takao S., Yano T., Suga T., Kawakami C., Yamamoto M., Kajiyama K., Saito H., Shimada S., Watanabe S., Aoki S., Taira K., Kon M., Lin J. H., Odagiri T.2012. Evaluation of influenza virus A/H3N2 and B vaccines on the basis of cross-reactivity of postvaccination human serum antibodies against influenza viruses A/H3N2 and B isolated in MDCK cells and embryonated hen eggs. Clin. Vaccine Immunol. 19: 897–908. doi: 10.1128/CVI.05726-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kodihalli S., Justewicz D. M., Gubareva L. V., Webster R. G.1995. Selection of a single amino acid substitution in the hemagglutinin molecule by chicken eggs can render influenza A virus (H3) candidate vaccine ineffective. J. Virol. 69: 4888–4897. doi: 10.1128/jvi.69.8.4888-4897.1995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kumar A., Meldgaard T. S., Bertholet S.2018. Novel platforms for the development of a universal influenza vaccine. Front. Immunol. 9: 600. doi: 10.3389/fimmu.2018.00600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lindstrom S., Garten R., Balish A., Shu B., Emery S., Berman L., Barnes N., Sleeman K., Gubareva L., Villanueva J., Klimov A.2012. Human infections with novel reassortant influenza A(H3N2)v viruses, United States, 2011. Emerg. Infect. Dis. 18: 834–837. doi: 10.3201/eid1805.111922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Loving C. L., Lager K. M., Vincent A. L., Brockmeier S. L., Gauger P. C., Anderson T. K., Kitikoon P., Perez D. R., Kehrli M. E., Jr. 2013. Efficacy in pigs of inactivated and live attenuated influenza virus vaccines against infection and transmission of an emerging H3N2 similar to the 2011–2012 H3N2v. J. Virol. 87: 9895–9903. doi: 10.1128/JVI.01038-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lu B., Zhou H., Ye D., Kemble G., Jin H.2005. Improvement of influenza A/Fujian/411/02 (H3N2) virus growth in embryonated chicken eggs by balancing the hemagglutinin and neuraminidase activities, using reverse genetics. J. Virol. 79: 6763–6771. doi: 10.1128/JVI.79.11.6763-6771.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mostafa A., Abdelwhab E. M., Mettenleiter T. C., Pleschka S.2018. Zoonotic potential of influenza A viruses: a comprehensive overview. Viruses 10: 1–38. doi: 10.3390/v10090497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nelson M. I., Viboud C., Vincent A. L., Culhane M. R., Detmer S. E., Wentworth D. E., Rambaut A., Suchard M. A., Holmes E. C., Lemey P.2015. Global migration of influenza A viruses in swine. Nat. Commun. 6: 6696. doi: 10.1038/ncomms7696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okamatsu M., Sakoda Y., Hiono T., Yamamoto N., Kida H.2013. Potency of a vaccine prepared from A/swine/Hokkaido/2/1981 (H1N1) against A/Narita/1/2009 (H1N1) pandemic influenza virus strain. Virol. J. 10: 47. doi: 10.1186/1743-422X-10-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ping J., Keleta L., Forbes N. E., Dankar S., Stecho W., Tyler S., Zhou Y., Babiuk L., Weingartl H., Halpin R. A., Boyne A., Bera J., Hostetler J., Fedorova N. B., Proudfoot K., Katzel D. A., Stockwell T. B., Ghedin E., Spiro D. J., Brown E. G.2011. Genomic and protein structural maps of adaptive evolution of human influenza A virus to increased virulence in the mouse. PLoS One 6: e21740. doi: 10.1371/journal.pone.0021740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reed L. J., Muench H.1938. A simple method of estimating fifty per cent endpoints. Am. J. Hyg. 27: 493–497. [Google Scholar]
- 27.Rogers G. N., Daniels R. S., Skehel J. J., Wiley D. C., Wang X. F., Higa H. H., Paulson J. C.1985. Host-mediated selection of influenza virus receptor variants. Sialic acid-alpha 2,6Gal-specific clones of A/duck/Ukraine/1/63 revert to sialic acid-alpha 2,3Gal-specific wild type in ovo. J. Biol. Chem. 260: 7362–7367. doi: 10.1016/S0021-9258(17)39617-5 [DOI] [PubMed] [Google Scholar]
- 28.Sakabe S., Ozawa M., Takano R., Iwastuki-Horimoto K., Kawaoka Y.2011. Mutations in PA, NP, and HA of a pandemic (H1N1) 2009 influenza virus contribute to its adaptation to mice. Virus Res. 158: 124–129. doi: 10.1016/j.virusres.2011.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schicker R. S., Rossow J., Eckel S., Fisher N., Bidol S., Tatham L., Matthews-Greer J., Sohner K.2016. Outbreak of influenza A(H3N2) variant virus infections among persons attending agricultural fairs housing infected swine—Michigan and Ohio, July–August 2016. pp. 1–4. In: Morbidity and Mortality Weekly Report, Centers for Disease Control and Prevention. https://www.cdc.gov/mmwr/volumes/65/wr/mm6542a1.htm [assessed on June 2, 2021]. [DOI] [PubMed]
- 30.Skowronski D. M., Janjua N. Z., De Serres G., Purych D., Gilca V., Scheifele D. W., Dionne M., Sabaiduc S., Gardy J. L., Li G., Bastien N., Petric M., Boivin G., Li Y.2012. Cross-reactive and vaccine-induced antibody to an emerging swine-origin variant of influenza A virus subtype H3N2 (H3N2v). J. Infect. Dis. 206: 1852–1861. doi: 10.1093/infdis/jis500 [DOI] [PubMed] [Google Scholar]
- 31.Sun X., Pulit-Penaloza J. A., Belser J. A., Pappas C., Pearce M. B., Brock N., Zeng H., Creager H. M., Zanders N., Jang Y., Tumpey T. M., Davis C. T., Maines T. R.2018. Pathogenesis and transmission of genetically diverse swine-origin H3N2 variant influenza A viruses from multiple lineages isolated in the United States, 2011–2016. J. Virol. 92: 1–15. doi: 10.1128/JVI.00665-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tate M. D., Job E. R., Brooks A. G., Reading P. C.2011. Glycosylation of the hemagglutinin modulates the sensitivity of H3N2 influenza viruses to innate proteins in airway secretions and virulence in mice. Virology 413: 84–92. doi: 10.1016/j.virol.2011.01.036 [DOI] [PubMed] [Google Scholar]
- 33.Tseng Y. C., Wu C. Y., Liu M. L., Chen T. H., Chiang W. L., Yu Y. H., Jan J. T., Lin K. I., Wong C. H., Ma C.2019. Egg-based influenza split virus vaccine with monoglycosylation induces cross-strain protection against influenza virus infections. Proc. Natl. Acad. Sci. USA 116: 4200–4205. doi: 10.1073/pnas.1819197116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilson A. I., Skehel J. J., Wiley D. C.1981. Structure of the haemagglutinin membrane glycoprotein of influenza virus at 3A resolution. Nature 289: 367–373. doi: 10.1038/289366a0 [DOI] [PubMed] [Google Scholar]
- 35.World Health Organization.2021. Antigenic and genetic characteristics of zoonotic influenza A viruses and development of candidate vaccine viruses for pandemic preparedness. pp. 88–104. In: Weekly Epidemiological Record, 96. https://apps.who.int/iris/handle/10665/340335 [assessed on August 17, 2021].
- 36.Ye Q., Krug R. M., Tao Y. J.2006. The mechanism by which influenza A virus nucleoprotein forms oligomers and binds RNA. Nature 444: 1078–1082. doi: 10.1038/nature05379 [DOI] [PubMed] [Google Scholar]
- 37.Ye Z., Liu T., Offringa D. P., McInnis J., Levandowski R. A.1999. Association of influenza virus matrix protein with ribonucleoproteins. J. Virol. 73: 7467–7473. doi: 10.1128/JVI.73.9.7467-7473.1999 [DOI] [PMC free article] [PubMed] [Google Scholar]