Abstract
Background
Tuberculosis (TB) is among the top 10 causes of death worldwide and there are estimated 10.4 million new (incident) patients, of which about one fourth are in India. There has been calls for rigorous investigations and interventions that may address other factors known to have effect on adherence of treatment like Depression but the amount of research into comorbidity is surprisingly low. The aim of the study was to assess magnitude and impact of depression among TB patients and determine the treatment outcomes of TB in District Srinagar.
Methods
In this prospective study the adults with newly diagnosed TB were recruited within one month of initiating treatment and were followed upto the end of treatment. Data collection was done at three time-points: baseline, after 2 months and after 6 months of treatment initiation. The sample size of 200 was calculated using OpenEpi, V3 and identified 202 TB patients were interviewed in their local language and PHQ-9 scale was used to measure Depression.
Results
The prevalence of Depression at baseline was 50.5% with CI (43.7%-57.3%). After two months of treatment the prevalence reduced to 9.4% with CI (5.9%-14.0%) and at the end of treatment to 2.5% with CI (0.91%-5.4%). Association between Depression in TB patients and treatment failure was found to be small to medium as revealed by Cramer’s V test (0.29–0.59). Binary logistic regression estimated that at baseline TB patients with Depression were at 4.46 times at more risk of treatment failure than patients without Depression and those patients who continued Depression even after intensive phase were 34.5 times at higher risk.
Conclusion
Our findings indicate Depression is associated with poor treatment outcome in these patients, despite TB treatment. TB treatment strategies should consider screening and managing the psychologically distressed individuals among TB patients.
Keywords: Depression, Tuberculosis, Prevalence, Incidence, Treatment outcomes
1. Introduction:
TUBERCULOSIS (TB) is among the top 10 causes of death worldwide and the main cause of deaths related to antimicrobial resistance and is the leading killer of people living with HIV (PLHIV) [1]. Globally there has been an estimated 10.4 million new [incident] TB patients, of which 6.2 million were men, 3.2 million women and 1 million children in 2016. About one fourth of the total burden of diseases is in India [2]. Although there has been decline in the incidence of TB since implementation of DOTS but the expectations to bring drastic improvement in treatment completion or cure rates has not been fully achieved and has led to calls for rigorous investigations of extended interventions that may address other factors known to have influence on adherence of treatment like depression. Even though depression has important effect on adherence to treatment for many clinical conditions, the amount of research into comorbidity between TB and mental disorders is surprisingly low [3].
Depression is one of the commonest mental illnesses and a leading cause of disease burden affecting 121 million people through the globe. About 850,000 people lose their lives every year because of suicide due to depression [4]. Depression is fourth most important cause of global disability-adjusted life years as per Global Burden of Disease study [5]. As estimated up to one-third of population with a serious medical condition are prone to symptoms of depression, and the risk increases with severity of illness and the level of disruption of life it causes [6]. In general population, the life time risk of depression is 10% to 25% for women and 5% to 12% for men [6]. Studies have shown that the prevalence of psychiatric disorders especially depression is high among patients with TB [7], [8]. Co morbidity of TB and depression is common and the prevalence of depression with a chronic physical condition range from 25% to 33% [9]. In community-based studies in Tuberculosis patients, the prevalence is about 49% [10] which can increase to 54% in hospitalized Tuberculosis patients [11].
There is no doubt about the fact that people with chronic diseases and comorbid depression are benefited from treatments for depression, including treatment with antidepressants. [12], [13], [14], [15], [16]. As intervention for depression among patients with TB, in the form of pill burden and potential stress is likely to incur additional costs, now we need to know to what extent TB treatment alone is effective against depressive symptoms. This study was conducted with aim to throw some light and provide baseline data about the magnitude of depression among TB patients and determine the course and treatment outcomes in TB patients in District Srinagar of Jammu and Kashmir, India. The primary objective of the study was to assess the impact of Depression on treatment outcomes of Tuberculosis patients in District Srinagar. The secondary objectives were to determine the Prevalence of Depression in Tuberculosis patients at the time of anti-TB treatment initiation, to determine the Incidence of Depression during treatment of Tuberculosis patients at two and six months after starting Anti-TB treatment and to compare the severity of Depression at treatment initiation and two and six months after starting Anti-TB treatment.
2. Methods:
The study was prospective in which adults with newly diagnosed TB were recruited within one month of initiating treatment and were followed up to the end of treatment (6 months after initiation). Data collection was done at three time-points: baseline (within one month of anti-TB treatment), after 2 months (end of intensive phase) and after 6 months (end of continuation phase).
2.1. Inclusion criteria:
-
•
New TB patients (attending the selected health centres who have started their anti-TB treatment within the last 1 month).
-
•
TB patients aged over 18 years.
2.2. Exclusion criteria:
-
•
Patients too ill to be interviewed at baseline as perceived by the interviewer or the patient.
-
•
Patients with Multidrug resistant TB (MDR TB), who constitute a different population because of different treatment (more toxic drugss for a much longer duration).
-
•
Patients on re-treatment, who have experiences of previous failures and usually have MDR-TB.
-
•
TB patients with a plan to be transferred out of the study sites.
-
•
Patients not agreeing to participate in the study, intellectual disability and difficulty of communication due to severe distress.
Srinagar district which also include district Ganderbal (being under administrative control of DTO Srinagar) has four Tubercular Units (TU), two in Srinagar and two in Ganderbal, 15 Designated Microscopy Centres (DMC) and 196 DOT Centres. The study was conducted for a period of one and half years starting from 1st April 2017 to 30th September 2018.
The sample size was calculated using OpenEpi, Version 3 [17] with following parameters: 80% power, 95% confidence (two sided). We estimated that the prevalence of treatment default among patients with TB without depression would be 4%. We used an estimate of four times increase in prevalence of defaulting among comorbid patients (i.e. a prevalence of treatment default of 16% among people with TB and comorbid depression). We estimate that we will find a ratio of 2:1 of non-exposed (not depressed) to exposed (depressed) participants as per prevalence of Depression in Tuberculosis patients in previous studies. With these assumptions, the required sample size calculated was 182. After adding 10% contingency to account for potential loss to follow-up, the total sample size was 200.
The identified 202 TB patients were interviewed in their local (Kashmiri/Urdu) language and examined by using a pre-tested study questionnaire. The questionnaire was divided into two parts. The first part comprised of the socio-demographic characteristics. In second part PHQ-9 scale was used to measure severity of depression in these patients. It is the most widely used and validated for Depression in TBpatients [18], [19], [20]. It has a sensitivity of around 90% and specificity of around 90% as per various validation studies conducted throughout the globe [19], [20], [21], [22], [23], [24], [25] Patients scoring 10 or more were classified as having high depressive symptoms (exposed). Symptoms were categorized using established cut-points 5, 10, 15 and 20 (mild, moderate, moderately severe and severe depression, respectively) [19], [20] to determine the different severities of exposure, and interval level scoring was computed to examine changes in intensity of depression when the comorbid TB is treated. Patients with Depression were clinically examined by Senior Psychiatrist from Psychiatric Hospital Govt. Medical College Srinagar for further management.
Classical TB outcomes as defined by WHO [25], cured, treatment completed, treatment failed, died, lost to follow-up, not evaluated or treatment success were used in analysis. Data on the patient's status on the primary outcome variable was also extracted from the RNTCP TB card.
Ethical consideration: Ethical consideration was obtained for conducting the study from the ethical committee of Government Medical College Srinagar. A written informed consent was obtained from the participating stakeholders at every level.
3. Data analysis
Data was compiled using Microsoft 2016 Excel spreadsheet and analysed by IBM SPSS V.23. Cochran’s Q test was used to test the difference between three matched results of Depression status. Friedman Test was used to assess severity of Depression at Baseline, 2 Months and after 6 months of Anti-TB treatment. Binary Logistic Regression Model was used for negative treatment outcomes, controlling by Depression at Baseline, Type of TB, Age and TB Related Stigma after 2 Months of TB Treatment.
4. Results:
In 202 Tuberculosis (TB) patients recruited, the response rate was 100% and all patients were followed till their treatment outcomes. The sociodemographic characteristics of the study participants is shown in Table 1. Out of 202 patients 116 (57.4%) were having Pulmonary and 86 (42.6%) Extrapulmonary TB. Among Pulmonary patients 101 (87.0%) were Microbiologically positive and 15 (13.0%) were Clinically diagnosed patients of Tuberculosis.
Table 1.
Sociodemographic Characteristics of the Participants.
| Sociodemographic Characteristics | Number (2 0 2) | Percentage (%) |
|---|---|---|
| Place of Residence | ||
| Urban | 116 | 57.4% |
| Rural | 86 | 42.6% |
| Gender | ||
| Males | 94 | 46.5% |
| Females | 108 | 53.5% |
| Age (Years) | ||
| 18–29 | 87 | 43.1% |
| 30–39 | 30 | 14.9% |
| 40–49 | 24 | 11.9% |
| 50–59 | 19 | 9.4% |
| 60 & Above | 42 | 20.7% |
| Marital Status | ||
| Presently Married | 120 | 59.4% |
| Widow/Widower | 2 | 1.0% |
| Never Married | 80 | 39.6% |
| Type of Family | ||
| Nuclear | 90 | 44.6% |
| Non-Nuclear | 112 | 55.4% |
| No. of Family members | ||
| 0–2 | 10 | 4.9% |
| 3–4 | 37 | 18.4% |
| 5–6 | 89 | 44.0% |
| 7 & Above | 66 | 32.7% |
| Educational Qualification | ||
| Illiterate | 86 | 42.5% |
| Primary | 6 | 3.0% |
| Passed Class 8th | 38 | 18.8% |
| Passed Matriculation | 24 | 11.9% |
| Secondary | 29 | 14.4% |
| Graduate/PG | 19 | 9.4% |
| Occupation | ||
| Household/ Unemployed | 91 | 45.0% |
| Student | 32 | 15.8% |
| Shopkeeper | 9 | 4.5% |
| Govt. Employees | 8 | 4.0% |
| Private Sector Employees | 8 | 4.0% |
| Labourer | 7 | 3.5% |
| Pashmina Work | 6 | 3.0% |
| Others | 41 | 20.2% |
| Socioeconomic Status (Kuppuswamy Scale) | ||
| Upper Class | 1 | 0.5% |
| Upper Middle Class | 7 | 3.5% |
| Lower Middle Class | 50 | 24.7% |
| Upper Lower Class | 75 | 37.1% |
| Lower Class | 69 | 34.2% |
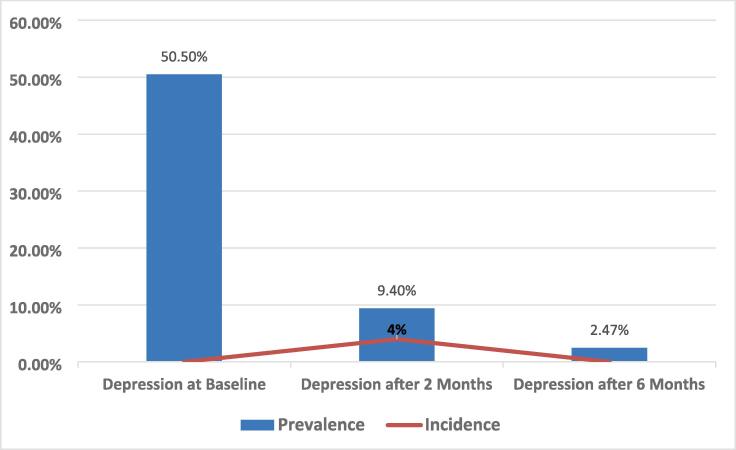
The prevalence of Depression at baseline in this study was 50.5% with CI (43.7%-57.3%) using OpenEpi-Confidence intervals for a proportion by Score (Wilson) method [26]. After two months of anti-TB treatment the prevalence reduced to 9.4% with CI (5.9%-14.0%) and at the end of treatment just 2.5% with CI (0.91%-5.4%) as shown in Fig. 1. The severity of Depression as per PHQ 9 scale, at Baseline, 2 months and after 6 months of anti-TB treatment is shown in Table 2.
Fig. 1.
Bar chart showing the Prevalence and Incidence on secondary axis during the course of Anti-Tb treatment.
Table 2.
Severity of Depression at Baseline, 2 Months and after 6 Months of Anti-TB treatment.
| Severity of Depression | Baseline | After 2 Months | After 6 Months | |||
|---|---|---|---|---|---|---|
| Frequency | Percent | Frequency | Percent | Frequency | Percent | |
| Minimal/No Depression | 49 | 24.3% | 161 | 79.7% | 187 | 92.6% |
| Mild Depression | 51 | 25.2% | 22 | 10.9% | 10 | 5% |
| Moderate Depression | 73 | 36.1% | 17 | 8.4% | 4 | 2% |
| Moderately Severe Depression | 26 | 12.9% | 2 | 1.0% | 1 | 0.5% |
| Severe Depression | 3 | 1.5% | 0 | 0.0% | 0 | 0.0% |
| Total | 202 | 100% | 202 | 100% | 202 | 100% |
| Friedman Test (χ2 = 437.32, df = 4, p-value < 0.0001) | ||||||
The incidence of Depression at 2 months of anti-TB treatment was 4.0% with CI (1.3%-9.3%) %). After 6 months of treatment, it dropped down to zero percent as shown in Fig. 1.
The association between Depression in Tuberculosis patients and treatment outcomes was found to be small to medium as revealed by Cramer’s V test, with statistically significant p-value (<0.001) as shown in Table 3.
Table 3.
Depression at Baseline, after 2 and 6 months and TB Treatment Outcomes (cross tabulation).
| Depression in TB Patients | TB Treatment Outcomes | Total | Statistical Analysis | ||
|---|---|---|---|---|---|
| Cured/Completed | Failure/Default | ||||
| Depression at Baseline | Absent | 98(98.0%) | 2(2.0%) | 100 | χ2 = 9.519df = 1, p-value = 0.003, Cramer’s V = 0.21 |
| Present | 88(88.3%) | 14(13.7%) | 102 | ||
| Total | 186(92.1%) | 16(7.9%) | 202 | ||
| Depression after 2 Months | Absent | 178(97.3%) | 5(2.7%) | 183 | p-value < 0.0001 [By Fisher’s Exact test] Cramer’s V = 0.59 |
| Present | 8(42.1%) | 11(57.9%) | 19 | ||
| Total | 186(92.1%) | 16(7.9%) | 202 | ||
| Depression after 6 Months | Absent | 184(93.4%) | 13(6.6%) | 197 | p-value = 0.004 [By Fisher’s Exact test] Cramer’s V = 0.30 |
| Present | 2(40.0%) | 3(60.0%) | 5 | ||
| Total | 186(92.1%) | 16(7.9%) | 202 | ||
Logistic regression was done after controlling Type of TB, Age, Sex and TB Related Stigma at Baseline, the risk of treatment failure was estimated to be about 59 times (with statistically significant p value) than at Depression at Baseline as shown in Table 4.
Table 4.
Binary Logistic Regression Model of Depression for Negative Treatment outcomes controlling by Depression at Baseline, Type of TB, Age and TB Related Stigma after 2 Months of TB Treatment.
| Predictor Variables | Odds Ratio | (95% CI) | p-value |
|---|---|---|---|
| Depression after 2 Months | 58.91 | 12.56–166.09 | <0.001 |
| Depression at Baseline | 6.70 | 1.01–35.15 | <0.050 |
| Type of TB | 0.11 | 0.02–0.75 | <0.021 |
| Age (years) | 0.99 | 0.95–1.03 | <0.539 |
| TB Related Stigma | 0.47 | 0.79–2.39 | <0.360 |
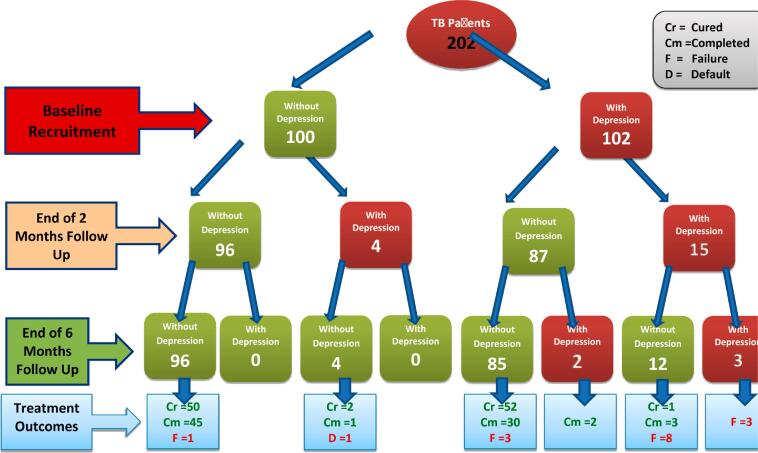
Fig. 2 shows the schematic illustration of TB treatment on Depression on treatment outcomes from baseline to end line of TB treatment.
Fig. 2.
Flow chart analysing the effect of tuberculosis treatment on depression and treatment outcome.
5. Discussion:
In this study the prevalence of Depression in the study participants at baseline was estimated to be more than fifty percent as shown in Fig. 1. The severity of Depression as per PHQ 9 scale, at Baseline, 2 months and after 6 months of anti-TB treatment showed sharp decline through the course of treatment as shown in Table 2. Many cross sectional and longitudinal studies have been conducted throughout world and very high prevalence ranging from 27% to 84% have been documented in these studies [27], [28], [29], [30], [31], [32], [33]. Our results revealed that the prevalence of Depression among Tuberculosis patients was in concordance with the results of the most of the studies conducted in rest of the world. Patients who had symptomatic relief in Tuberculosis started feeling better psychologically which was supported by the decreasing trend in Depressive symptoms as the symptoms got relieved though the course of the treatment from baseline to end line.
Likewise the incidence of Depression during the course of treatment at 2 months of anti-TB treatment in study population was estimated to be 4.0% with CI (1.3%-9.3%), after 6 months of treatment also dropped down to zero percent as shown in Fig. 1. Low incidence during the anti-TB treatment seem to be because of the protective effect of anti TB treatment and feeling of wellbeing by the patients. Although anti-Depressant effect of Anti-TB drugs need to be verified as there seem to be a definite role of Anti-TB drugs on the outcomes of Depression in these patients and many studies hypothesized the role of certain anti-TB drugs in causality of Depression in these patients [34], [35], [36], [37].
Depression in TB patients was found be to associated with negative treatment outcome in the study population and the strength of association between Depression in Tuberculosis patients and treatment outcomes was estimated to be small to medium as revealed by Cramer’s V test (0.21–0.59), with statistically significant p-value (<0.01) as shown in Table 3.
Studies conducted throughout the globe revealed that TB patients which were being diagnosed and treated in time for psychological comorbidities adhere with TB treatment and Depression was associated with worst outcome and increased hazard in these patients [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46]. Treating the psychological aspects of TB may lead to better clinical outcomes. Psychotherapy during TB treatment was found to be leading to higher adherence, treatment, and cure rates in a prospective controlled trial in India [47]. Psychological support as an intervention can improve treatment adherence and completion [48]. Counselling and psycho-education was done in all TB patients irrespective of their Depression status to avoid the intervention bias and only those patients with suicidal ideation were given anti-depressants drugs by the Consultant Psychiatrist.
After two months of anti-TB treatment the strength of association between Depression and worst treatment outcome increased to many folds and those patients who remained depressive for more than two months after the treatment had about 59 times risk of treatment failure than those without Depression as shown in Table 4. Effect of other variables remained almost same compared to baseline figures. It was seen that those patients who responded to counselling, psychoeducation or antidepressants given in few patients (Depression with suicidal ideation) in the intensive phase of anti-TB treatment had good treatment outcome in majority of patients possibly due to better adherence [49], [50].
Binary logistic regression revealed that Depression in Intensive period and its resolution in same period seem to be important so far as good treatment outcome is concerned. As it was noted that those incident patients who developed Depression after two months of intensive period still had good treatment outcome as they responded to Depression quickly and had no Depression after 6 months of anti-TB treatment. Fentie Ambaw et al. in their study in Ethiopia in 2018, found that comorbid depressive symptoms in tuberculosis patients are often associated with poorer outcomes, even with successful treatment so far as duration of treatment is concerned [45].
6. Strengths of the study:
The Validated PHQ 9 questionnaire was used for the study population and the Senior Psychiatrist of the Government Medical College Srinagar confirmed diagnosis of Depression. This study provided the evidence-based impact of comorbid depression on the course and outcome of TB.
The observation of depression in these TB patients from treatment initiation to completion allowed us to investigate whether TB treatment with counselling may be sufficient to reduce depressive symptoms. Although in some cases antidepressants were used because of ethical issues, the intervention did not affect the study design because of the smaller number of cases with suicidal ideation. Moreover, the longitudinal study design allowed us to estimate the incidence of depression among people engaged with TB treatment. In addition, the study enabled us to investigate the impact of depression in determining the course and outcome of TB, independently of other factors such as sociodemographic variables, stigma, perceived social support, medication side effects, and comorbid illnesses.
7. Limitations of the study:
The Sample size in our study was calculated on the assumption of a treatment default rate of 4% in TB cases without depression, which was based on a national report. However, in this study, only 0.5% of patients defaulted. However, it didn’t critically affect our findings and we still obtained estimates even with this sample size. We used an estimate of 2:1 ratio as per our pilot study, although we got a 1:1 ratio (Non exposed to exposed) at the end of the study as shown in the flow chart, the sample of the patients taken was still enough as we didn’t have any non-contingency. If we had taken a 1:1 ratio, the sample size would have been 198. We have already taken 202 patients, so it would not have affected the results of the study. In addition, there were only two follow up of the patients, after two months and 6 months. It was difficult to calculate the exact time taken by anti-TB drugs to affect the Depression symptoms. Intervention in the form of anti-Depressants was used in some cases having suicidal ideation because of the ethical issue, which might have affected the results. Importantly our conclusions cannot be extended to tuberculosis patients who are hospitalized, are being retreated, or have a multidrug-resistant disease, which was excluded from the study because they comprised a different study population. There can be other unknown confounding factors of Depression, which is multifactorial and may have affected the TB treatment outcomes. However, the study population was more or less socio-demographically homogenous and the results were consistent with other studies.
8. Conclusion:
In conclusion, our findings indicate that there is high prevalence of depression in TB patients in Srinagar district of Kashmir valley both in rural and urban population. We found an association between Depression at baseline and negative outcomes (treatment failure and default) to TB treatment with Depression. Depression appears to be a strong risk factor for treatment failure and default in these people with newly diagnosed tuberculosis and is associated with poor treatment outcome despite successful tuberculosis treatment.
Although the overall magnitude of Depression among TB patients on anti-TB treatment was high at baseline, the magnitude was relatively lower at end point in comparison to that at baseline in most of the patients without anti-depressant treatment. Depressive symptoms at Baseline and after 2 months of TB treatment predicted TB treatment outcomes significantly. Thus, Depression and TB seem to be in syndemic relationship and treating TB and Depression jointly may give desired results. Although treatment of TB alone seems to be more important and can take care of both the diseases as revealed by the results of our study.
Our findings indicate that TB treatment strategies should consider screening and managing the psychologically distressed individuals among TB patients. In this regard, health-care workers should be trained in counselling and psycho-education needed to provide depression care and treatment adherence for people with tuberculosis.
It is further recommended that others be encouraged to take up the subject concerned on a large scale and move ahead from where the scholar has concluded.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References:
- 1.World Health Organization. Global Tuberculosis Report 2017.
- 2.Published in the Gazette of India, Part-II, Section-3, Sub-section (ii) Ministry of Environment, Forest and Climate Change Notification New Delhi, the 29. 2016;317(ii):1–15.
- 3.Prince M., Patel V., Saxena S., Maj M., Maselko J., Phillips M.R., et al. No health without mental health. Lancet. 2007;370(9590):859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 4.Rivinder NB; Depression. http://www.webmd.com/depression/default.htm.
- 5.Murray C.JL., Lopez A.D. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997;349(9063):1436–1442. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 6.Cynthia H; Depression caused by chronic illness. http://www.medicinenet.com/script/main/art.asp?ar ticlekey=55170.
- 7.West away MS Wolmarans L; Depression and self-esteem: rapid screening for depression in black, low literacy, hospitalized TB patients. Soc Sci Med. 1992;35:1311–1315. doi: 10.1016/0277-9536(92)90184-r. [DOI] [PubMed] [Google Scholar]
- 8.Aghanwa H.S., Erhabor G.E. Demographic/socioeconomic factors in mental disorders associated with TB in southwest Nigeria. J Psychosom Res. 1998;45:353–360. doi: 10.1016/s0022-3999(98)00006-3. [DOI] [PubMed] [Google Scholar]
- 9.Trenton A.J., Currier G.W. Treatment of co morbid tuberculosis and depression. Primary Care Companion Journal of Clinical Psychiatry. 2001;03(06):236–243. doi: 10.4088/pcc.v03n0610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Natani G.D., Jain N.K., Sharma T.N., Gehlot P.S., Agrawal S.P., Koolwal S., et al. Depression in tuberculosis patients: correlation with duration of disease and response to anti-tuberculous chemotherapy. Ind. J. Tub. 1985;32(4):195–198. [Google Scholar]
- 11.Purohit D.R., Purohit S.D., Dhariwal M.L. Incidence of depression in hospitalized tuberculosis patients in RNT medical college. Udapir. Ind. J. Tub. 1978;25(3):147–151. [Google Scholar]
- 12.Katon W.J. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin Neurosci. 2011;13:7–23. doi: 10.31887/DCNS.2011.13.1/wkaton. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Orhan Aydin I., Uluşahin A. Depression, anxiety comorbidity, and disability in tuberculosis and chronic obstructive pulmonary disease patients:applicability of GHQ-12. Gen Hosp Psychiatry. 2001;23(2):77–83. doi: 10.1016/s0163-8343(01)00116-5. [DOI] [PubMed] [Google Scholar]
- 14.Simon GE, Von Korff M, Lin E. Clinical and functional outcomes of depression treatment in patients with and without chronic medical illness. Psychol Med 2005;35:271–9. [DOI] [PubMed]
- 15.Rodin G., Voshart K. Depression in the medically ill: an overview. Am J Psychiat. 1986;143:696–705. doi: 10.1176/ajp.143.6.696. [DOI] [PubMed] [Google Scholar]
- 16.Doherty A.M., Kelly J., McDonald C., O’Dywer A.M., Keane J., Cooney J. A review of the interplay between tuberculosis and mental health. Gen Hosp Psychiat. 2013;35(4):398–406. doi: 10.1016/j.genhosppsych.2013.03.018. [DOI] [PubMed] [Google Scholar]
- 17.1. Kelsey, J.L; Whittemore, A.S; Evans, A.S; and Thompson W. Documentation for Sample Size for an Unmatched Case-Control Study; Table 12-15; Methods Obs Epidemiol [Internet]. 1996;2–3. Available from: http://www.openepi.com/PDFDocs/SSCCDoc.pdf.
- 18.Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Y.-L., Liang W., Chen Z.-M., Zhang H.-M., Zhang J.-H., Weng X.-Q., et al. Validity and reliability of Patient Health Questionnaire-9 and Patient Health Questionnaire-2 to screen for depression among college students in China. Asia-Pacific. Psychiatry. 2013;5(4):268–275. doi: 10.1111/appy.12103. [DOI] [PubMed] [Google Scholar]
- 20.Arroll B., Goodyear-Smith F., Crengle S., et al. (2010) Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med. 8, 348–353. [DOI] [PMC free article] [PubMed]
- 21.Gelaye B., Williams M.A., Lemma S., Deyessa N., Bahretibeb Y., Shibre T., et al. Validity of the Patient Health Questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. 2013;210(2):653–661. doi: 10.1016/j.psychres.2013.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Monahan P.O., Shacham E., Reece M., Kroenke K., Ong’or W.O., Omollo O., et al. Validity/reliability of PHQ-9 and PHQ-2 depression scales among adults living with HIV/AIDS in western Kenya. J Gen Intern Med. 2009;24(2):189–197. doi: 10.1007/s11606-008-0846-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bhana A., Rathod S.D., Selohilwe O., Kathree T., Petersen I. The validity of the Patient Health Questionnaire for screening depression in chronic care patients in primary health care in South Africa. BMC Psychiatry. 2015;15:118. doi: 10.1186/s12888-015-0503-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.WHO (2014), Global Tuberculosis Report 2014.
- 25.Siedlecki K.L., Salthouse T.A., Oishi S., Jeswani S. The relationship between social support and subjective well-being across age. Soc Indic Res. 2014;117(2):561–576. doi: 10.1007/s11205-013-0361-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Duko B, Gebeyehu A, Ayano G. Prevalence and correlates of depression and anxiety among patients with tuberculosis at WolaitaSodo University Hospital and Sodo Health Center , WolaitaSodo , South Ethiopia , Cross. BMC Psychiatry [Internet]. 2015;1–7. Available from: http://dx.doi.org/10.1186/s12888-015-0598-3. [DOI] [PMC free article] [PubMed]
- 27.Mandaknalli R., Giriraj B. Prevalence of Depression in Tuberculosis Patients in a Tertiary Care Hospital. 2015;3:2445–2448. [Google Scholar]
- 28.Pradesh H., Pradesh H., Pradesh H., Officer M., Pradesh H., Resident S., et al. Assessment of the frequency of Depression and Anxiety among Tuberculosis patients at a Tertiary Care Health Centre. A cross. 2018;5(4):496–499. [Google Scholar]
- 29.Kumar K, Kumar A, Chandra P, Kansal HM. Original Article A study of prevalence of depression and anxiety in patients suffering from tuberculosis. 2016;2016–9. [DOI] [PMC free article] [PubMed]
- 30.Aamir S. Co-Morbid Anxiety and Depression Among Pulmonary Tuberculosis Patients. 2010;20(226):703–704. doi: 10.2010/JCPSP.703704. [DOI] [PubMed] [Google Scholar]
- 31.Dogar A, Sohail H, Mehdi Z, Azam M, Niaz O. Prevalence of Depression Among Tuberculosis Patients. :133–7.
- 32.Peltzer K., Naidoo P., Matseke G., Louw J., Mchunu G., Tutshana B. Prevalence of psychological distress and associated factors in tuberculosis patients in public primary care clinics in South Africa. BMC Psychiatry. 2012;12(1) doi: 10.1186/1471-244X-12-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.WHO. Mental health gap action programme intervention guide for mental, neurological and substance use disorders in non-specialized health settings. 2010. http://whqlibdoc.who.int/publications/2010/ 9789241548069_eng.pdf. [PubMed]
- 34.Yung FY, Study PC Original Research. 2015;11221(April):505–511. [Google Scholar]
- 35.Lee E. Prevalence of Depression among Active TB and Depression Among Active Tb And Tb / HIV Patients In Kisumu. 2015.
- 36.Trenton AJ, Currier GW. Treatment of Comorbid Tuberculosis and Depression. Prim Care Companion J Clin Psychiatry [Internet]. [DOI] [PMC free article] [PubMed]
- 37.Ugarte-gil C, Ruiz P, Zamudio C, Canaza L, Otero L, Kruger H, et al. Association of Major Depressive Episode with Negative Outcomes of Tuberculosis Treatment. 2013;8(7):1–7. [DOI] [PMC free article] [PubMed]
- 38.Tol A, Yekaninejad MS, Ejeta LT. Psychological distress and its effect on tuberculosis treatment outcomes in Ethiopia. 2015;1(November):1–11. [DOI] [PMC free article] [PubMed]
- 39.Rizvi N. Frequency of Depression and Anxiety among Tuberculosis Patients. 2016;183–90.
- 40.Kehbila J, Ekabe CJ, Aminde LN, Noubiap JJN, Fon PN. Prevalence and correlates of depressive symptoms in adult patients with pulmonary tuberculosis in the Southwest Region of Cameroon. Infect Dis Poverty [Internet]. 2016;1–8. Available from: http://dx.doi.org/10.1186/s40249-016-0145-6. [DOI] [PMC free article] [PubMed]
- 41.Koyanagi A, Vancampfort D, Carvalho AF, Devylder JE, Haro JM. Depression comorbid with tuberculosis and its impact on health status: cross-sectional analysis of community-based data from 48 low- and middle-income countries. 2017;1–10. [DOI] [PMC free article] [PubMed]
- 42.Lai S. Increased Risk of Pulmonary Tuberculosis in Patients with Depression: A Cohort Study in Taiwan. 2017;8(November):1–7. [DOI] [PMC free article] [PubMed]
- 43.Ibrahim E, Ibrahim A, Aly M, Messery A. Egyptian Journal of Chest Diseases and Tuberculosis Pattern of prevalence, risk factors and treatment outcomes among Egyptian patients with multidrug resistant tuberculosis. Egypt J Chest Dis Tuberculosis [Internet]. 2017;66(3):405–11. Available from: http://dx.doi.org/10.1016/j.ejcdt.2016.11.002.
- 44.Ambaw F., Mayston R., Hanlon C., Medhin G., Alem A. Untreated depression and tuberculosis treatment outcomes, quality of life and disability, Ethiopia. Bull World Health Organ. 2018;96(4):243–255. doi: 10.2471/BLT.17.192658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pardal PK. tuberculosis – an observational study. 2018;168–71. [DOI] [PMC free article] [PubMed]
- 46.Janmeja A.K., Das S.K., Bhargava R., Chavan B.S. Psychotherapy improves compliance with tuberculosis treatment. Respiration. 2005;72(4):375–380. doi: 10.1159/000086251. [DOI] [PubMed] [Google Scholar]
- 47.Acha J., Sweetland A., Guerra D., Chalco K., Castillo H., Palacios E. Psychosocial support groups for patients with multidrug-resistant tuberculosis: five years of experience. Glob Public Health. 2007;2(4):404–417. doi: 10.1080/17441690701191610. [DOI] [PubMed] [Google Scholar]
- 48.Burman W.J., Cohn D.L., Rietmeijer C.A., Judson F.N., Reves R.R., Sbarbaro J.A. Noncompliance with directly observed therapy for tuberculosis. Epidemiology and effect on the outcome of treatment. Chest. 1997;111(5):1168–1173. doi: 10.1378/chest.111.5.1168. [DOI] [PubMed] [Google Scholar]
- 49.Jaiswal A., Singh V., Ogden J.A., Porter J.D.H., Sharma P.P., Sarin R., et al. Adherence to tuberculosis treatment: lessons from the urban setting of Delhi, India. Trop Med Int Health. 2003;8(7):625–633. doi: 10.1046/j.1365-3156.2003.01061.x. [DOI] [PubMed] [Google Scholar]
- 50.Garner P., Smith H., Munro S., Volmink J. Promoting adherence to tuberculosis treatment. Bull World Health Organ. 2007;85:404–440. doi: 10.2471/06.035568. [DOI] [PMC free article] [PubMed] [Google Scholar]