Abstract
Background
Knee function deficits may persist after anterior cruciate ligament reconstruction (ACLR). Return to sport (RTS) testing batteries assess recovery after ACLR and can guide RTS progression, but the ideal test components are debatable. The single leg vertical hop for height (SLVH) test using a commercially available jump mat may provide a valuable assessment of knee function.
Hypothesis/Purpose
The purpose of this study was to compare the limb symmetry index (LSI) of SLVH to horizontal hop testing in a cohort of National Collegiate Athletic Association (NCAA) Division 1 collegiate athletes after ACLR. The hypothesis was the SLVH would elicit significantly lower LSI than horizontal hop tests.
Study design
Cross-Sectional Study
Methods
Eighteen National Collegiate Athletic Association (NCAA) Division 1 collegiate athletes (7 males, 11 females) at 7.33 ± 2.05 months after ACLR were included in this retrospective study. LSI was calculated for single hop for distance (SHD), triple hop for distance (THD), cross-over hop for distance (CHD), timed 6-meter hop (T6H), and SLVH. A repeated measures ANOVA was performed to identify differences in LSI for each test. Spearman’s Rho correlation coefficient was calculated to examine the relationship between LSIs for each test.
Results
The LSI for SLVH (84.48% ± 11.41%) was significantly lower than LSI for SHD (95.48 ± 8.02%, p = 0.003), THD (94.40 ± 3.70%, p = 0.002), CHD (95.85 ± 7.00, p = 0.007), and T6H (97.69 ± 6.60%, p = 0.001). The correlation of LSI between SLVH and the horizontal hop tests was weak and non-significant for SHD (rs = 0.166, p = 0.509), CHD (rs = 0.199, p = 0.428), and T6H (rs = 0.211, p = 0.401) and moderate and non-significant for THD (rs = 0.405, p = 0.096).
Conclusions
Individuals after ACLR had lower LSI on the SLVH than on horizontal hop tests and weak to moderate correlations between the tests suggest SLVH detects performance deficits not identified by the horizontal hop tests.
Level of evidence
3
Keywords: hop testing, return to sport, rehabilitation, acl reconstruction, anterior cruciate ligament, movement system
INTRODUCTION
Over 120,000 anterior cruciate ligament (ACL) tears per year occur in the United States.1 In athletes, the majority of these tears are addressed with ACL reconstruction (ACLR) surgery.2 Post-operatively, rehabilitation is crucial to restore function and promote a safe return to activities of daily living and sport. Despite current rehabilitation standards and return to sport criteria, outcomes still may not be optimal. A systematic review of prospective studies that followed patients for at least five years post-surgery reported in the pooled data that 5.8% of ipsilateral ACLR autografts failed and 11.8% of patients had an ACL tear in the contralateral limb.3 Ardern et al. reported pooled return to sport rates of 74% to 87%, however, only 59% to 72% of patients returned to their preinjury sport, and only 46% to 63% returned to competitive sports.4 Level of play is an important variable to consider after ACLR as it may help discern whether athletes are not doing as well as originally thought.5,6
Return to sport (RTS) testing batteries are used by sports medicine and rehabilitation professionals to measure outcomes and provide guidelines for clinical decision making during the RTS progression.7–12 They may be a helpful component of the return to sport process and ultimately improve outcomes by identifying athletes in need of continued rehabilitation. Traditional horizontal hop testing that measures the distance one can hop forward is a commonly used component of these batteries.7,13 These tests include a number of hopping tasks that assess either the distance one can hop in single or multiple unilateral jumps, or the time it takes an individual to hop on the impaired limb a specified distance. However, all of these tasks assess hopping in a primarily forward direction. In contrast, the single leg vertical hop for height (SLVH) test measures the height that one can hop upward and is emerging as a useful assessment of knee function after ACLR.14–17 This is because the SLVH test relies more heavily on the power generated by the quadriceps to create a vertical impulse than the traditional horizontal hop tests.15,18 Achieving ≥ 90% limb symmetry index (LSI), a value comparing the performance on the involved to the uninvolved limb, is often advocated as a marker of successful rehabilitation.10,11,19 A benefit of hop testing is that it is easy to perform in the clinic and has demonstrated appropriate reliability and validity to use after ACLR.20 Other common tests/measures include measurements of strength, power, graft integrity, movement quality, psychological readiness, and patient reported outcomes.5,9,15,21–27 However, controversy exists over the ideal combination of tests to use, if results on these tests are associated with better outcomes, and how these tests assess knee function.23,28–34 This conflicting information poses challenges to sports medicine and rehabilitation professionals when considering how to objectively guide RTS decision making.35
Further exploration of RTS testing options will allow clinicians to better select outcome measures that assess relevant components of knee function.36,37 The SLVH test is easy to administer and may provide helpful information regarding knee function after ACLR.14,15,33 Taylor et al. found greater LSI asymmetries on the SLVH compared to horizontal hop tests and poor correlation between SLVH and the horizontal hop tests, suggesting that SLVH may measure constructs that horizontal tests cannot.16 While promising, that study had wide inclusion criteria that analyzed individuals many years (4.7 ± 2.6) after surgery and used 3D motion capture and force plate assessment, which may not be applicable to traditional rehabilitation settings. Exploration of SLVH performance earlier after ACLR through the lens of clinical practice and may help guide clinical decision making during the later stages of rehabilitation. The purpose of this study was to compare the LSI of SLVH to horizontal hop testing in a cohort of National Collegiate Athletic Association (NCAA) Division 1 collegiate athletes after ACLR. It was hypothesized that the SLVH would elicit significantly lower LSI than the horizontal hopping tests and provide unique information from the horizontal hopping tests to be used in clinical decision making after ACLR.
METHODS
Participants
A retrospective review was conducted to examine a consecutive series of patients between August 2018- November 2020 who met the inclusion criteria of NCAA Division 1 collegiate athletes referred to the University of Maryland Sports Medicine practice to assess their recovery after unilateral ACLR. Patients were excluded from the study for 1) a history of prior ACLR to either knee or 2) any other lower extremity musculoskeletal surgery within the previous two years. To determine sample size, an a priori power analysis was conducted based on the work of Taylor et al.16 A sample size of 14 was required to detect an effect size of 0.8 for the primary outcome measure, limb symmetry index (LSI), with α =0.05 and a power (1- β) = 0.80. The Institutional Review Board at the University of Maryland, Baltimore determined this study to be exempt.
Procedures
The necessary demographic and hop testing data were extracted and de-identified from subjects’ electronic medical records. Demographic data is included in Table 1. Hop testing data collected included limb symmetry indices (LSIs) for a battery of single leg hop tests including: single hop for distance (SHD), triple hop for distance (THD), cross-over hop for distance (CHD), timed 6-meter hop (T6H), and single leg vertical hop for height (SLVH). Data were collected as part of usual clinical practice by physical therapists (authors MZ or RR) who are board-certified in either sports or orthopedic physical therapy and each have over eight years of experience working with patients with ACL injuries.
Table 1. Patient demographics.
| Demographic variable | All (n=18) |
|---|---|
| Male: Number (%) | 7 (39%) |
| Female: Number (%) | 11 (61%) |
| Age, years | 20.39 ± 1.11 |
| Height, meters | 1.75 ± 0.09 |
| Weight, kilograms | 75.61 ± 15.38 |
| Body mass index, kilograms/meters2 | 24.5 ± 0.40 |
| Time since surgery, months | 7.33 ± 2.05 |
Nominal data are displayed as number (%), interval and ratio data are displayed as mean ± standard deviation
Testing procedures were based upon previously published instructions and included a warmup, two practice trials, and two test trials; the two test trials were averaged for the final result for each test which was used for statistical analysis.7,8,14 Horizontal hop tests (SHD, THD, and CHD) were performed over ground and measured with a tape measure. The T6H was performed over ground and measured with a standard timer on a smart phone device. The SLVH was performed on the Just Jump System (JJS, Probotics Inc, Huntsville, AL, USA), which is a commercially available jump mat that calculates jump height from flight time between foot contacts and is valid when compared to three-dimensional camera motion capture.38
For the SHD, the instructions were to hop as far forward as possible and hold the landing on the testing leg for two seconds. For the THD and CHD, participants were instructed to perform three continuous forward hops and hold the final landing on the testing leg for two seconds. For the T6H, the instructions were to hop on the testing leg as fast as possible down a 6-meter course, with the time needed to complete the course recorded for analysis. For the SLVH (Figure 1), the instructions were to perform a countermovement, single leg vertical hop as high as possible and hold the landing on the testing leg for two seconds. The patients were also instructed not to excessively flex their hips while in the air to prevent artificially increasing flight time but were allowed to use their arms. Limb symmetry indices (LSIs) were calculated by dividing the result on the involved limb by the result on the uninvolved limb and multiplying by 100 to produce a percentage. For the T6H, the numerator and denominator were reversed in the calculation, as a lower time indicates better performance. Therefore, for all tests, a value less than 100% indicates a worse performance on the surgical limb compared to the non-surgical.
Figure 1. Single Limb Vertical Hop for height, using the Just Jump System.
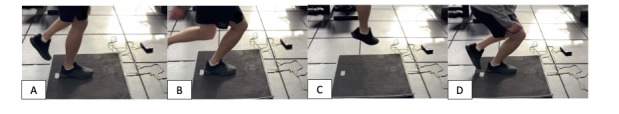
- Starting position, B. End of eccentric phase, C. Flight phase, D. Landing position
Statistical Analysis
Descriptive statistics (means and standard deviations) were calculated for all dependent variables. Shapiro-Wilk test was used to assess the normality of the LSI data for each hop test. Repeated measures ANOVAs (within-subject factor: test) were performed to identify differences in LSI across the tests. Post-hoc analysis was conducted when significant main effects were found to evaluate pairwise comparisons for LSI between specific tests. As the Shapiro-Wilk test determined that the LSI for two of the five tests was not normally distributed, non-parametric Spearman’s Rho correlation coefficient was used to examine the relationship between limb symmetry index for each test. Additionally, this test has been reported to be more robust to outliers than the traditional Pearson correlation coefficient.39 All statistical analyses were performed using SPSS version 27 (IBM Corp.) with p ≤ 0.05 indicating statistically significant differences.
RESULTS
A total of 18 patients (7 males, 11 females) with an average age of 20.39 ± 1.11 years were included (Table 1). Sports played by patients are presented in Table 2. Data was not analyzed by sport, but this information helps characterize the sample. All patients had undergone primary ACLR with bone-patellar tendon-bone autograft and were an average of 7.33 ± 2.05 months since surgery.
Table 2. Sports played by subjects.
| Sport Played | Number (n=18) |
|---|---|
| Men’s Lacrosse | 3 |
| Women’s Lacrosse | 2 |
| Football | 3 |
| Field Hockey | 2 |
| Women’s Soccer | 6 |
| Softball | 2 |
There was a difference in LSI across the hop tests, with a significant main effect of hop test on the LSI (F(4,14)=5.549, p = 0.007) seen across the participants (Figure 2). Post-hoc pairwise comparisons show that the LSI for SLVH (84.48% ± 11.41%) was significantly lower than the LSI calculated for each of the horizontal hop tests: SHD (95.48 ± 8.02%, p = 0.003), THD (94.40 ± 3.70%, p = 0.002), CHD (95.85 ± 7.00, p = 0.007), and T6H (97.69 ± 6.60%, p = 0.001).
Figure 2. LSI results across the five hop tests, presented as %, with <100% indicating that the involved (surgical) limb performed worse than the non-surgical limb.
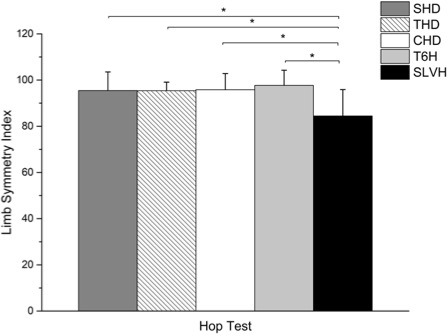
LSI: Limb Symmetry Index, SHD: Single hop for distance, THD: Triple hop for distance, CHD: Crossover hop for distance, T6H: Timed 6-meter hop SLVH: Single leg vertical hop for height.
* = statistically significant difference (p 0.05)
Fourteen patients (77.78%) scored ≥ 90% on all four horizontal hop tests. In contrast, only six patients (33.33%) scored ≥ 90% on the SLVH. Of the fourteen patients who scored ≥ 90% on all four horizontal hop tests, only five patients (35.71%) scored ≥ 90% on the SLVH. None of the five patients who scored ≤ 90% on the horizontal hop tests scored ≥ 90% on the SLVH.
There were no statistically significant correlations observed between the LSI for the SLVH to the other four tests (Figure 3). Overall, there were weak correlations between the limb symmetry indices for the SLVH to the SHD (rs = 0.166, p = 0.509), CHD (rs = 0.199, p = 0.428), and T6H (rs = 0.211, p = 0.401) and a moderate correlation when comparing the SLVH to the THD (rs = 0.405, p = 0.096).
Figure 3. LSI for the SLVH compared to the four horizontal hop test, with SLVH (y-axis) compared to the four horizontal hop tests (A-D, x-axis).
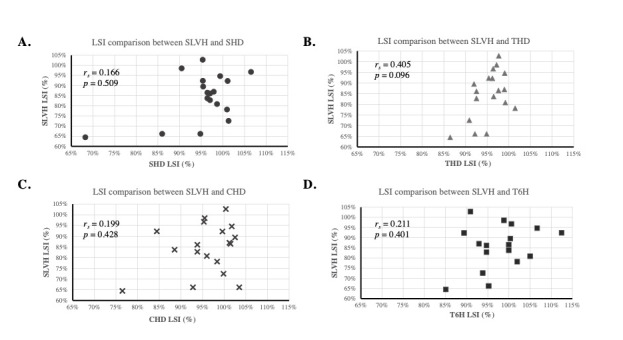
LSI: Limb Symmetry Index, SHD: Single hop for distance, THD: Triple hop for distance, CHD: Crossover hop for distance, T6H: Timed 6-meter hop, SLVH: Single leg vertical hop for height
DISCUSSION
The aim of this study was to compare LSI calculated from the SLVH to four horizontal hop tests after ACLR. The main findings supported the hypothesis that LSI of the SLVH test would be significantly lower than all horizontal hop tests. Additionally, the non-signficiant, weak to moderate correlations may indicate the SLVH and horizontal jump tests assess different performance constructs. It is important to recall the context of these findings as the data in the current study is from patients during middle to later stages of rehabilitation after ACLR, all of whom had the goal of returning to sport.
In this cohort, the asymmetry of LSI on the SLVH was approximately 10% or more than each of the horizontal hop tests. This large asymmetry is relevant to clinicians as the lower LSI on the SLVH compared to the horizontal hop tests may indicate that the SLVH test identifies performance deficits that commonly used horizontal hop tests may not. The results are in agreement with those of Taylor et al. who found that participants after ACLR exhibited significant side-to-side differences during the SLVH with the involved limb hopping to a lower height.16 Biomechanical studies have found that participants after ACLR demonstrate a reduced angular impulse at the knee and greater inter-joint coordination asymmetry on the SLVH test.16,33 King et al. demonstrated similar findings with large effect size differences in internal knee valgus moment and posterior center of mass distance on a single leg drop jump task at nine months post ACLR.40 Performance deficits on the SLVH may correlate to these biomechanical deficits and may be clinically relevant for healthcare providers who use these tests in determining readiness for athletic activities or to guide rehabilitation.
Previous authors have shown that the SLVH is positively correlated with patient-reported IKDC scores, Tegner activity scale, ACL-RSI scale, isokinetic extensor muscle strength, carioca, and shuttle run tests.14,15,17,29 The relationship between SLVH and quadriceps strength may be of particular importance as better quadriceps function after ACLR is associated with improved patient reported outcome measures, gait quality, and return to sport rates, and reduced risk of re-injury.10,15,41–44 These additional measures were not directly measured in this study, however the previously documented findings serve to justify the use of the simple clinical test.
The weak correlations between the SLVH test and the horizontal hop tests indicate that the SLVH test likely provides a different assessment of the functional status of the knee. In this cohort, 77.78% of patients demonstrated LSI ≥ 90% on all horizontal hop tests at 7.33 ± 2.05 months after surgery. The pass rate exceeds the pass rate of 52.5% at 12 months after surgery reported by Logerstedt et al. from the Delaware-Oslo Cohort.45 This suggests the current cohort was made up of high performers, however only 33.33% of patients demonstrated LSI ≥ 90% on the SLVH. This is clinically relevant as the horizontal hop testing data would suggest this group was made up of high performers, while the SLVH detected persistent knee function deficits.
Traditional horizontal hop testing alone after ACLR may not capture bilateral or absolute deficits.36,46 Similarly, normal hopping function is difficult to define as even healthy athletes may not be symmetrical.47 Patterson et al. identified performance deterioration of the uninvolved limb between one and five years after ACLR suggesting inter-limb comparisons may be flawed as the uninvolved limb may not be functioning optimally after surgery due to deconditioning.48 Acknowledging the importance of absolute values, Wellsandt et al. proposed testing the contralateral limb pre-operatively to establish a baseline value before surgery when using LSI as part of RTS decision making.30 It is important to acknowledge the limitations of hop testing.
Even if LSI calculated on horizontal hopping performance is to be used as part of the RTS decision, the strategy by which athletes hop must be considered. In their systematic review with meta-analysis of 624 patients after ACLR, Kotsifaki et al. found that athletes may demonstrate adequate distance on the SHD by adopting hip, knee, and ankle strategies suggesting horizontal hop tests alone may be misleading.34
Recent studies observing the validity of RTS testing and outcomes have shown no significant relationship between passing hop tests and re-injury.19,31,32 Similarly, passing RTS batteries may not guarantee successful return to sport or be associated with optimal knee function.31 However, other authors have suggested that RTS testing is associated with reduced re-injury risk.10–12 Clinical testing for RTS remains controversial however a primary benefit testing is that it provides the ability to longitudinally track progress over time. Clinical tests such as SLVH and horizontal hop testing are cost-effective, simple to perform, and empower both the patient and healthcare team to objectively assess recovery and guide functional progression through the rehabilitation process. Additionally, more comprehensive testing procedures that include outcome measures such as diverse hopping tasks, strength, power, movement quality, and psychological status can provide valuable information and more broadly assess recovery and may add value.26,27,49,50 A holistic approach to RTS testing can help clinicians carefully assess and guide each patient through return to sport rather than be used as a simple pass or fail concept.37,51–53
While the data from this study adds to the discussion regarding hop testing, there are several limitations. This study was a retrospective cohort analysis, which could introduce selection bias. Careful consideration was given to the inclusion and exclusion criterion to minimize this risk. Similarly, in this cohort, only the included hop tests were uniformly performed and reported on. Other assessments of function, strength, power, and patient-reported outcome measures were used, but in an evolving manner that reflects clinical practice and were not identical among subjects or appropriate to report. Relationships between these additional measures and SLVH are purely speculative. All subjects were NCAA Division 1 collegiate athletes, played a variety of sports, and were operated on and provided rehabilitation by providers from a single institution; the results therefore cannot be generalized to all patients. Furthermore, the horizontal hop test pass rates at 7.33 ± 2.05 months after surgery exceeded previously reported pass rate at 12 months and likely do not reflect the performance of all patients after ACLR. Tests with high inter-rater reliability were used to minimize error.20 For example, jump mats are accurate, reliable, and cost efficient when compared to a 3-dimensional motion capture system and is correlated with force plate assessment of jump height.38,54–56 The T6H test, which was timed with a standard timer may result in faster times compared to automatic timers and should be interpreted with caution.57 Additionally, it is important to consider other variables that could affect jump height such as jump type, strategy, and instructions.54,57–60 Therefore, instructions were to perform countermovement, single leg vertical hop as high as possible and hold the landing on the testing leg for two seconds and not excessively flex the hips while in the air to prevent artificially increasing flight time.
Future studies should assess the relationship between SLVH and other assessments and include longer tracking of outcomes related to autograft failures, contralateral ACL tears, and return to performance.
CONCLUSION
The results of this study indicate that SLVH elicits different LSI values after ACLR than horizontal hop tests. In this cohort, the majority of patients who performed well on horizontal hop tests did not perform as well on the SLVH. Clinicians should strive to use the most valid and appropriate tests to assess outcomes after ACLR and should consider using SLVH as horizontal hop testing may not capture all deficits in performance.
Conflicts of Interest
The authors have no financial disclosures to report.
References
- Gornitzky Alex L., Lott Ariana, Yellin Joseph L., Fabricant Peter D., Lawrence J. Todd, Ganley Theodore J. Sport-specific yearly risk and incidence of anterior cruciate ligament tears in high school athletes: A systematic review and meta-analysis. 10. Vol. 44. SAGE Publications; pp. 2716–2723. [DOI] [PubMed] [Google Scholar]
- Herzog Mackenzie M., Marshall Stephen W., Lund Jennifer L., Pate Virginia, Mack Christina D., Spang Jeffrey T. Trends in incidence of ACL reconstruction and concomitant procedures among commercially insured individuals in the United States, 2002-2014. 6. Vol. 10. SAGE Publications; pp. 523–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: A systematic review. Wright Rick W., Magnussen Robert A., Dunn Warren R., Spindler Kurt P. Jun;2011 The Journal of Bone & Joint Surgery. 93(12):1159–1165. doi: 10.2106/jbjs.j.00898. doi: 10.2106/jbjs.j.00898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardern Clare L, Taylor Nicholas F, Feller Julian A, Webster Kate E. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: An updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. 21. Vol. 48. BMJ; pp. 1543–1552. [DOI] [PubMed] [Google Scholar]
- Return to sport after anterior cruciate ligament injury: Panther Symposium ACL injury return to sport consensus group. Meredith Sean J., Rauer Thomas, Chmielewski Terese L., Fink Christian, Diermeier Theresa, Rothrauff Benjamin B., Svantesson Eleonor, Hamrin Senorski Eric, Hewett Timothy E., Sherman Seth L., Lesniak Bryson P., Bizzini Mario, Chen Shiyi, Cohen Moises, Villa Stefano Della, Engebretsen Lars, Feng Hua, Ferretti Mario, Fu Freddie H., Imhoff Andreas B., Kaeding Christopher C., Karlsson Jon, Kuroda Ryosuke, Lynch Andrew D., Menetrey Jacques, Musahl Volker, Navarro Ronald A., Rabuck Stephen J., Siebold Rainer, Snyder-Mackler Lynn, Spalding Tim, van Eck Carola, Vyas Dharmesh, Webster Kate, Wilk Kevin, the Panther Symposium ACL Injury Return to Sport Consensus Group Jun 1;2020 Orthopaedic Journal of Sports Medicine. 8(6):2325967120930829. doi: 10.1177/2325967120930829. doi: 10.1177/2325967120930829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai Courtney C H, Ardern Clare L, Feller Julian A, Webster Kate E. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: A systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. 2. Vol. 52. BMJ; pp. 128–138. [DOI] [PubMed] [Google Scholar]
- Noyes Frank R., Barber Sue D., Mangine Robert E. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. 5. Vol. 19. SAGE Publications; pp. 513–518. [DOI] [PubMed] [Google Scholar]
- Test–retest reliability of knee rating scales and functional hop tests one year following anterior cruciate ligament reconstruction. Hopper Diana M, Goh Suet C, Wentworth Laurel A, Chan Derek Y.K, Chau Jay H.W, Wootton Gregory J, Strauss Geoffrey R, Boyle Jeffrey J.W. Feb;2002 Physical Therapy in Sport. 3(1):10–18. doi: 10.1054/ptsp.2001.0094. doi: 10.1054/ptsp.2001.0094. [DOI] [Google Scholar]
- Single-leg hop test performance and isokinetic knee strength after anterior cruciate ligament reconstruction in athletes. Sueyoshi Ted, Nakahata Akihiro, Emoto Gen, Yuasa Tomoki. Nov;2017 Orthopaedic Journal of Sports Medicine. 5(11):232596711773981. doi: 10.1177/2325967117739811. doi: 10.1177/2325967117739811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grindem Hege, Snyder-Mackler Lynn, Moksnes Håvard, Engebretsen Lars, Risberg May Arna. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: The Delaware-Oslo ACL cohort study. 13. Vol. 50. BMJ; pp. 804–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyritsis Polyvios, Bahr Roald, Landreau Philippe, Miladi Riadh, Witvrouw Erik. Likelihood of ACL graft rupture: Not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. 15. Vol. 50. BMJ; pp. 946–951. [DOI] [PubMed] [Google Scholar]
- Capin Jacob John, Snyder-Mackler Lynn, Risberg May Arna, Grindem Hege. Keep calm and carry on testing: A substantive reanalysis and critique of ‘what is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis’. 23. Vol. 53. BMJ; pp. 1444–1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgi Ciara R, Peters Scott, Ardern Clare L, Magill John R, Gomez Christina D, Sylvain Jonathan, Reiman Michael P. Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review. 18. Vol. 53. BMJ; pp. 1154–1161. [DOI] [PubMed] [Google Scholar]
- Lee Dhong Won, Yang Sang Jin, Cho Seung Ik, Lee Jung Ho, Kim Jin Goo. Single-leg vertical jump test as a functional test after anterior cruciate ligament reconstruction. 6. Vol. 25. Elsevier BV; pp. 1016–1026. [DOI] [PubMed] [Google Scholar]
- Isokinetic extension strength is associated with single-leg vertical jump height. Fischer Felix, Blank Cornelia, Dünnwald Tobias, Gföller Peter, Herbst Elmar, Hoser Christian, Fink Christian. Nov;2017 Orthopaedic Journal of Sports Medicine. 5(11):232596711773676. doi: 10.1177/2325967117736766. doi: 10.1177/2325967117736766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The single-leg vertical hop provides unique asymmetry information in individuals after anterior cruciate ligament reconstruction. Taylor Jeffrey B., Westbrook Audrey E., Head Penny L., Glover Katie M., Paquette Max R., Ford Kevin R. Dec;2020 Clinical Biomechanics. 80:105107. doi: 10.1016/j.clinbiomech.2020.105107. doi: 10.1016/j.clinbiomech.2020.105107. [DOI] [PubMed] [Google Scholar]
- Laudner K., Evans D., Wong R.., et al. 2015Relationship between isokinetic knee strength and jump characteristics following anterior cruciate ligament reconstruction. 10(3):272–280. [PMC free article] [PubMed] [Google Scholar]
- Kotsifaki Argyro, Korakakis Vasileios, Graham-Smith Philip, Sideris Vasileios, Whiteley Rod. Vertical and horizontal hop performance: Contributions of the hip, knee, and ankle. 2. Vol. 13. SAGE Publications; pp. 128–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losciale Justin M., Zdeb Rachael M., Ledbetter Leila, Reiman Michael P., Sell Timothy C. The association between passing return-to-sport criteria and second anterior cruciate ligament injury risk: A systematic review with meta-analysis. 2. Vol. 49. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); pp. 43–54. [DOI] [PubMed] [Google Scholar]
- Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Reid Andrea, Birmingham Trevor B, Stratford Paul W, Alcock Greg K, Giffin J Robert. Mar 1;2007 Phys Ther. 87(3):337–349. doi: 10.2522/ptj.20060143. doi: 10.2522/ptj.20060143. [DOI] [PubMed] [Google Scholar]
- Read Paul J., Michael Auliffe Sean, Wilson Mathew G., Graham-Smith Philip. Lower limb kinetic asymmetries in professional soccer players with and without anterior cruciate ligament reconstruction: Nine months is not enough time to restore “functional” symmetry or return to performance. 6. Vol. 48. SAGE Publications; pp. 1365–1373. [DOI] [PubMed] [Google Scholar]
- Diermeier Theresa Anita, Rothrauff Ben B, Engebretsen Lars, Lynch Andrew, Svantesson Eleonor, Hamrin Senorski Eric Andrew, Meredith Sean J, Rauer Thomas, Ayeni Olufemi R, Paterno Mark, Xerogeanes John W, Fu Freddie H, Karlsson Jon, Musahl Volker. Treatment after ACL injury: Panther Symposium ACL treatment consensus group. 1. Vol. 55. BMJ; pp. 14–22. [DOI] [PubMed] [Google Scholar]
- Should return to sport be delayed until 2 years after anterior cruciate ligament reconstruction? Biological and functional considerations. Nagelli Christopher V., Hewett Timothy E. 2017Sports Medicine. 47(2):221–232. doi: 10.1007/s40279-016-0584-z. doi: 10.1007/s40279-016-0584-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angelozzi Massimo, Madama Marco, Corsica Cristiana, Calvisi Vittorio, Properzi Gianfranco, McCaw Steven T., Cacchio Angelo. Rate of force development as an adjunctive outcome measure for return-to-sport decisions after anterior cruciate ligament reconstruction. 9. Vol. 42. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); pp. 772–780. [DOI] [PubMed] [Google Scholar]
- King Enda, Franklyn-Miller Andrew, Richter Chris, O’Reilly Eamon, Doolan Mark, Moran Kieran, Strike Siobhan, Falvey Éanna. Clinical and biomechanical outcomes of rehabilitation targeting intersegmental control in athletic groin pain: Prospective cohort of 205 patients. 16. Vol. 52. BMJ; pp. 1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Webster Kate E., Feller Julian A., Lambros Christina. Feb;2008 Physical Therapy in Sport. 9(1):9–15. doi: 10.1016/j.ptsp.2007.09.003. doi: 10.1016/j.ptsp.2007.09.003. [DOI] [PubMed] [Google Scholar]
- Contractile rate of force development after ACL reconstruction - a comprehensive review and meta-analysis. Turpeinen Juha Tapio, Freitas Tomás T., Rubio-Arias Jacobo Ángel, Jordan Matthew J., Aagaard Per. Jun 18;2020 Scandinavian Journal of Medicine & Science in Sports. 30(9):1572–1585. doi: 10.1111/sms.13733. doi: 10.1111/sms.13733. [DOI] [PubMed] [Google Scholar]
- Orishimo Karl F., Kremenic Ian J., Mullaney Michael J., McHugh Malachy P., Nicholas Stephen J. Adaptations in single-leg hop biomechanics following anterior cruciate ligament reconstruction. 11. Vol. 18. Springer Science and Business Media LLC; pp. 1587–1593. [DOI] [PubMed] [Google Scholar]
- Nagai Takashi, Schilaty Nathan D., Laskowski Edward R., Hewett Timothy E. Hop tests can result in higher limb symmetry index values than isokinetic strength and leg press tests in patients following ACL reconstruction. 3. Vol. 28. Springer Science and Business Media LLC; pp. 816–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limb symmetry indexes can overestimate knee cunction after anterior cruciate ligament injury. Wellsandt Elizabeth, Failla Mathew J., Snyder-Mackler Lynn. May;2017 Journal of Orthopaedic & Sports Physical Therapy. 47(5):334–338. doi: 10.2519/jospt.2017.7285. doi: 10.2519/jospt.2017.7285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losciale Justin M., Bullock Garrett, Cromwell Christina, Ledbetter Leila, Pietrosimone Laura, Sell Timothy C. Hop testing lacks strong association with key outcome variables after primary anterior cruciate ligament reconstruction: A systematic review. 2. Vol. 48. SAGE Publications; pp. 511–522. [DOI] [PubMed] [Google Scholar]
- Webster Kate E., Hewett Timothy E. What is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A Systematic review and meta-analysis. 6. Vol. 49. Springer Science and Business Media LLC; pp. 917–929. [DOI] [PubMed] [Google Scholar]
- Blache Yoann, Pairot de Fontenay Benoit, Argaud Sebastien, Monteil Karine. Asymmetry of inter-joint coordination during single leg jump after anterior cruciate ligament reconstruction. 02. Vol. 38. Georg Thieme Verlag KG; pp. 159–167. [DOI] [PubMed] [Google Scholar]
- Measuring only hop distance during single leg hop testing is insufficient to detect deficits in knee function after ACL reconstruction: a systematic review and meta-analysis. Kotsifaki Argyro, Korakakis Vasileios, Whiteley Rod, Van Rossom Sam, Jonkers Ilse. 2020British Journal of Sports Medicine. 54(3):139–153. doi: 10.1136/bjsports-2018-099918. doi: 10.1136/bjsports-2018-099918. [DOI] [PubMed] [Google Scholar]
- Dingenen Bart, Gokeler Alli. Optimization of the return-to-sport paradigm after anterior cruciate ligament reconstruction: A critical step back to move forward. 8. Vol. 47. Springer Science and Business Media LLC; pp. 1487–1500. [DOI] [PubMed] [Google Scholar]
- A critical analysis of limb symmetry indices of hop tests in athletes after anterior cruciate ligament reconstruction: A case control study. Gokeler A., Welling W., Benjaminse A., Lemmink K., Seil R., Zaffagnini S. Oct;2017 Orthopaedics & Traumatology: Surgery & Research. 103(6):947–951. doi: 10.1016/j.otsr.2017.02.015. doi: 10.1016/j.otsr.2017.02.015. [DOI] [PubMed] [Google Scholar]
- Gokeler Alli, Welling Wouter, Zaffagnini Stefano, Seil Romain, Padua Darin. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. 1. Vol. 25. Springer Science and Business Media LLC; pp. 192–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Validity of two alternative systems for measuring vertical jump height. Leard John S., Cirillo Melissa A., Katsnelson Eugene, Kimiatek Deena A., Miller Tim W., Trebincevic Kenan, Garbalosa Juan C. 2007The Journal of Strength and Conditioning Research. 21(4):1296–1299. doi: 10.1519/r-21536.1. doi: 10.1519/r-21536.1. [DOI] [PubMed] [Google Scholar]
- Correlation coefficients: Appropriate use and interpretation. Schober Patrick, Boer Christa, Schwarte Lothar A. May;2018 Anesthesia & Analgesia. 126(5):1763–1768. doi: 10.1213/ane.0000000000002864. doi: 10.1213/ane.0000000000002864. [DOI] [PubMed] [Google Scholar]
- King Enda, Richter Chris, Franklyn-Miller Andy, Daniels Katherine, Wadey Ross, Moran Ray, Strike Siobhan. Whole-body biomechanical differences between limbs exist 9 months after ACL reconstruction across jump/landing tasks. 12. Vol. 28. Wiley; pp. 2567–2578. [DOI] [PubMed] [Google Scholar]
- Lepley Lindsey K. Deficits in quadriceps strength and patient-oriented outcomes at return to activity after ACL reconstruction: A review of the current literature. 3. Vol. 7. SAGE Publications; pp. 231–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strength of the quadriceps femoris muscle and functional recovery after reconstruction of the anterior cruciate ligament. A prospective, randomized clinical trial of electrical stimulation. Snyder-Mackler L, Delitto A, Bailey S L, Stralka S W. Aug;1995 The Journal of Bone & Joint Surgery. 77(8):1166–1173. doi: 10.2106/00004623-199508000-00004. doi: 10.2106/00004623-199508000-00004. [DOI] [PubMed] [Google Scholar]
- Zwolski Christin, Schmitt Laura C., Quatman-Yates Catherine, Thomas Staci, Hewett Timothy E., Paterno Mark V. The influence of quadriceps strength asymmetry on patient-reported function at time of return to sport after anterior cruciate ligament reconstruction. 9. Vol. 43. SAGE Publications; pp. 2242–2249. [DOI] [PubMed] [Google Scholar]
- Quadriceps strength influences patient function more than single leg forward hop during late-stage ACL rehabilitation. Chaput Meredith, Palimenio Marcus, Farmer Brooke, Katsavelis Dimitrios, Bagwell Jennifer J., Turman Kimberly A., Wichman Chris, Grindstaff Terry L. Feb 1;2021 Int J Sports Phys Ther. 16(1):145–155. doi: 10.26603/001c.18709. doi: 10.26603/001c.18709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Self-reported knee function can identify athletes who fail return-to-activity criteria up to 1 year after anterior cruciate ligament reconstruction: a delaware-oslo ACL cohort study. Logerstedt David, Di Stasi Stephanie, Grindem Hege, Lynch Andrew, Eitzen Ingrid, Engebretsen Lars, Risberg May Arna, Axe Michael J., Snyder-Mackler Lynn. Dec;2014 Journal of Orthopaedic & Sports Physical Therapy. 44(12):914–923. doi: 10.2519/jospt.2014.4852. doi: 10.2519/jospt.2014.4852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King Enda, Richter Chris, Daniels Katherine A.J., Franklyn-Miller Andy, Falvey Eanna, Myer Gregory D., Jackson Mark, Moran Ray, Strike Siobhan. Can biomechanical testing after anterior cruciate ligament reconstruction identify athletes at risk for subsequent ACL injury to the Contralateral Uninjured Limb? 3. Vol. 49. SAGE Publications; pp. 609–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uninjured youth athlete performance on single-leg hop testing: How many can achieve recommended return-to-sport criterion? Greenberg Elliot M., Dyke Julie, Leung Anne, Karl Michael, Lawrence J. Todd, Ganley Theodore. May 11;2020 Sports Health: A Multidisciplinary Approach. 12(6):552–558. doi: 10.1177/1941738120911662. doi: 10.1177/1941738120911662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limb symmetry index on a functional test battery improves between one and five years after anterior cruciate ligament reconstruction, primarily due to worsening contralateral limb function. Patterson Brooke E., Crossley Kay M., Perraton Luke G., Kumar Avnish S., King Matthew G., Heerey Joshua J., Barton Christian J., Culvenor Adam G. Jul;2020 Physical Therapy in Sport. 44:67–74. doi: 10.1016/j.ptsp.2020.04.031. doi: 10.1016/j.ptsp.2020.04.031. [DOI] [PubMed] [Google Scholar]
- Angelozzi Massimo, Madama Marco, Corsica Cristiana, Calvisi Vittorio, Properzi Gianfranco, McCaw Steven T., Cacchio Angelo. Rate of force development as an adjunctive outcome measure for return-to-sport decisions after anterior cruciate ligament reconstruction. 9. Vol. 42. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); pp. 772–780. [DOI] [PubMed] [Google Scholar]
- Lower limb asymmetry in mechanical muscle function: A comparison between ski racers with and without ACL reconstruction: Bilateral asymmetry in ACL-R ski racers. Jordan M. J., Aagaard P., Herzog W. 2015Scandinavian Journal of Medicine & Science in Sports. 25(3):e301–e309. doi: 10.1111/sms.12314. doi: 10.1111/sms.12314. [DOI] [PubMed] [Google Scholar]
- On-field rehabilitation part 1: 4 pillars of high-1uality on-field rehabilitation are restoring movement quality, physical conditioning, restoring sport-specific skills, and progressively developing chronic training load. Buckthorpe Matthew, Della Villa Francesco, Della Villa Stefano, Roi Giulio Sergio. Aug;2019 Journal of Orthopaedic & Sports Physical Therapy. 49(8):565–569. doi: 10.2519/jospt.2019.8954. doi: 10.2519/jospt.2019.8954. [DOI] [PubMed] [Google Scholar]
- Buckthorpe Matthew, Della Villa Francesco, Della Villa Stefano, Roi Giulio Sergio. On-field rehabilitation part 2: A 5-stage program for the soccer player focused on linear movements, multidirectional movements, soccer-specific skills, soccer-specific movements, and modified practice. 8. Vol. 49. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); pp. 570–575. [DOI] [PubMed] [Google Scholar]
- Dingenen Bart, Gokeler Alli. Optimization of the return-to-sport paradigm after anterior cruciate ligament reconstruction: A critical step back to move forward. 8. Vol. 47. Springer Science and Business Media LLC; pp. 1487–1500. [DOI] [PubMed] [Google Scholar]
- Rogan Slavko, Radlinger Lorenz, Imhasly Caroline, Kneubuehler Andrea, Hilfiker Roger. Validity study of a jump mat compared to the reference standard force plate. 4. Vol. 6. Kowsar Medical Institute; [DOI] [PMC free article] [PubMed] [Google Scholar]
- Accuracy of jump-mat systems for measuring jump height. Pueo Basilio, Lipinska Patrycja, Jiménez-Olmedo José M., Zmijewski Piotr, Hopkins Will G. Aug;2017 Int J Sports Physiol Perform. 12(7):959–963. doi: 10.1123/ijspp.2016-0511. doi: 10.1123/ijspp.2016-0511. [DOI] [PubMed] [Google Scholar]
- Accuracy of a vertical jump contact mat for determining jump height and flight time. Whitmer Tyler D., Fry Andrew C., Forsythe Charles M., Andre Matthew J., Lane Michael T., Hudy Andrea, Honnold Darric E. Apr;2015 J Strength Cond Res. 29(4):877–881. doi: 10.1519/jsc.0000000000000542. doi: 10.1519/jsc.0000000000000542. [DOI] [PubMed] [Google Scholar]
- Tests of vertical jump: Countermovement jump with arm swing and reaction jump with arm swing. Acero Rafael Martín, Sánchez José Andrés, Fernández-del-Olmo Miguel. Dec;2012 Strength Cond J. 34(6):87–93. doi: 10.1519/ssc.0b013e318276c353. doi: 10.1519/ssc.0b013e318276c353. [DOI] [Google Scholar]
- Reach height and jump displacement: Implications for standardization of reach determination. Ferreira Lucas C, Schilling Brian K, Weiss Lawrence W, Fry Andrew C, Chiu Loren Z F. Jun;2010 J Strength Cond Res. 24(6):1596–1601. doi: 10.1519/jsc.0b013e3181d54a25. doi: 10.1519/jsc.0b013e3181d54a25. [DOI] [PubMed] [Google Scholar]
- Usefulness of the jump-and-reach test in assessment of vertical jump performance. Menzel Hans-Joachim, Chagas Mauro H., Szmuchrowski Leszek A., Araujo Silvia R., Campos Carlos E., Giannetti Marcus R. Feb;2010 Perceptual and Motor Skills. 110(1):150–159. doi: 10.2466/pms.110.1.150-158. doi: 10.2466/pms.110.1.150-158. [DOI] [PubMed] [Google Scholar]
- Validation of an electronic jump mat to assess stretch-shortening cycle function. Kenny Ian C., Cairealláin Ainle Ó, Comyns Thomas M. Jun;2012 J Strength Cond Res. 26(6):1601–1608. doi: 10.1519/jsc.0b013e318234ebb8. doi: 10.1519/jsc.0b013e318234ebb8. [DOI] [PubMed] [Google Scholar]


