Abstract
This study demonstrates the challenges of establishing social determinants of health (SDH) screening at well child visits (WCVs) during the COVID-19 pandemic. We conducted a 6-month pre-intervention retrospective chart review (2/2020-8/2020) and 6-month post-intervention prospective chart review (8/2020-2/2021) of an SDH screening and referral protocol at a single suburban academic pediatric clinic. WCVs were screened for food, financial, and transportation needs. With the new protocol, 46% of eligible WCVs (n = 1253/2729) had documented screening results. Self-report of screened visits found 34.6% with financial strain, 32% with worry about food insecurity, 25.1% with food insecurity, 5.3% with medical transportation difficulties, and 6% with daily living transportation difficulties. There was an increase in resources offered during the post-intervention period (OR = 11.5 [7.1-18.6], P < .001). There was also an increase in resident physician self-reported knowledge in providing referrals (P = .04).
Keywords: general pediatrics, medical education
Background
The World Health Organization defines social determinants of health (SDH) as the “conditions in which people are born, grow, work, live, and age, and the wide set of forces and systems shaping the conditions of daily life.”1,2 Unmet social needs are associated with increased frequency of hospitalization, slower recovery time, and a higher infant mortality rate.3,4 Previous studies have shown that systematic screening and referral for unmet social needs during well child visits (WCVs) are feasible, acceptable to families, and can lead to uptake of more community resources by families.5–8 Barriers to screening during primary care visits include overburdened staff to screen and document, lack of standardized screening procedures, lack of standardized screening tools, difficulty identifying diagnostic codes, inadequate SDH training, lack of familiarity with community resources, and low physician efficacy in addressing patients’ social needs.2,3,6,8-11
A survey by the American Pediatric Association’s Continuity Research Network, which represents 53% of pediatric residency programs, found that 97% of respondents (of a 41% response rate) reported screening for at least 1 SDH. 11 However, published studies focusing on pediatric SDH screening have been small randomized control trials or observational studies limited to 6 months or less.12-14 We present a 12-month single-center study reviewing the pediatric experience with screening and referring families for unmet social needs in the areas of financial resource strain, food insecurity, and transportation needs, unintentionally coinciding with the COVID-19 pandemic. The timing is particularly relevant during the pandemic, which has exposed already-existing inequities in the health system. Greater health and financial burdens are placed on minority and lower socioeconomic status groups.15-17 Public health measures implemented to control the spread of SARS-CoV-2 have inadvertently exacerbated unmet social needs. For example, school closures have unintentionally increased food insecurity for low-income children in school lunch programs. 16 In addition to the immediate negative health effects for vulnerable populations, the pandemic is expected to have long-term socioeconomic impacts on infected families and their communities. 18 Although the location’s SDH pilot study was not originally planned to coincide with the COVID-19 pandemic, the timing provides opportunities to explore the urgent need and feasibility of implementing SDH screening and referral during a period of extreme socioeconomic distress.
Methods
Selection and Sample
Families of children 0 to 17 years of age who presented for in-person WCVs to pediatric residents and attending physicians (n = 51) at a single general pediatric clinic were eligible. The academic clinic is in the Midwest. It serves an ethnically diverse patient population with a large portion of families on public assistance. The patient population is approximately 30% Caucasian, 30% Hispanic, 30% Black, and 10% other. The population’s insurance status is approximately 60% Medicaid, 35% private insurance, and 5% self-pay/uninsured. The clinic is predominantly a resident continuity clinic with some attending-physician-only visits. During the year reviewed, 14.9% of the total visits were completed solely by attending physicians.
Ethical Approval and Informed Consent
The study (#213880) was approved by the Institutional Review Board (IRB). Because our pilot project used methods that were considered standard of care, the IRB waived the formal and separate written informed consent requirement. The completion of the screening tool itself constituted participants’ informed consent.
Intervention Design
A pilot program for screening and referring families for unmet social needs in the areas of financial resource strain, food insecurity, and transportation needs was instituted at the pediatric clinic in August 2020. These SDH domains were preselected by the hospital system as a pilot quality improvement (QI) project. The screening tool utilized screening questions recently implemented in the electronic medical record (EMR) system and used with the adult patient population at our institution. The timeline for implementation was planned prior to the COVID-19 pandemic. Unintentionally, almost the entire project coincided with the pandemic.
All clinic staff and physicians were trained on the protocol for universal screening of SDH at WCVs. Families received a written SDH screen (Supplemental Appendices A and B) in English or Spanish at visit check-in, to be completed in the waiting room. The patient care technician (PCT), medical assistant (MA) or nurse reviewed the SDH screen while the families waited in the examination room for the physician. The PCT, MA, or nurse documented the screens directly into the EMR in the socioeconomic section of the social history. The physician then reviewed the results, discussed any positive screens with the family, and provided written referrals. Standardized resource lists approved by the institution were available. However, physicians also had the opportunity to make community referrals outside of the list.
An outpatient social worker was available if additional assistance was needed at the time of the visit. The decision to include social work was based on clinical judgment and not standardized. However, social work was almost always involved for families with a history of no-show visits, transportation difficulties, and positive SDH screens.
Due to concern regarding lower-than-expected screening rates, multiple additional interventions were completed during the 6-month post-intervention period. These interventions included a resident survey, resident education session, clinical staff meeting, modification of the screening form, and creation of SDH resources in Spanish.
Measures
Chart review of SDH documentation for all scheduled well child visits (age 0-17) by pediatric residents and attending physicians (n = 51) at the clinic over 2 time periods (pre-intervention and post-intervention) was completed. Both time periods overlapped with the COVID-19 pandemic. The pre-intervention period (2/2/2020-8/2/2020, n = 1762) served as a baseline for rates of SDH-specific resources and referrals provided at well child visits during the 6 months prior to the implementation of the SDH screening intervention. The pre-intervention chart reviews were completed retrospectively. A prospective chart review was completed for the post-intervention period (8/3/2020-2/2/2021, n = 2726). See Table 1 for a description of patient and physician provider characteristics by time.
Table 1.
Patient and Physician Characteristics.
| Overall (n = 4488) | Pre-intervention a (n = 1762 [%]) | Post-intervention b (n = 2726 [%]) | P-value | |
|---|---|---|---|---|
| Age, mean (SD) c | 4.28 | 3.72 | 4.69 | <.001 |
| Age range c | ||||
| Infant (<1) | 720 (40.8) | 1023 (37.5) | <.001 | |
| Toddler (≥1-<3) | 406 (23.1) | 474 (17.4) | ||
| Preschool (≥3-<5) | 183 (10.4) | 222 (8.1) | ||
| School age (≥5-<12) | 278 (15.8) | 646 (23.7) | ||
| Adolescent (≥12) | 174 (9.9) | 363 (13.2) | ||
| Physician year of training | ||||
| PGY-1 | 292 (16.6) | 499 (18.3) | <.01 | |
| PGY-2 | 556 (31.6) | 931 (34.1) | ||
| PGY-3 | 555 (31.5) | 734 (26.9) | ||
| PGY-4 | 87 (4.9) | 167 (6.1) | ||
| Attending | 274 (15.4) | 395 (14.5) | ||
Pre-intervention (2/3/2020-7/31/2020).
Post-intervention (8/3/2020-2/2/2021).
Presented to clinic for WCVs.
Online anonymous surveys for all pediatric residents (n = 31) and medicine-pediatric residents (n = 15) were completed at 2 time points to assess SDH screening and referral practices, confidence addressing SDH, and confidence regarding SDH referrals, with an educational session presented in between. The pre-educational session survey was completed in November 2020, which was 3 months after initiation of universal SDH screening. For the pre-educational survey, 31 of out 46 (67.4%) residents completed the survey. The post-educational survey was completed in February 2021, which was 6 months after initiation of universal SDH screening. For the post-educational survey, 21 out of 46 (45.7%) residents completed the survey (see Table 2).
Table 2.
Pediatric Residents’ Survey Results.
| Pre-survey, n (%) | Post-survey, n (%) | |
|---|---|---|
| Level of training | ||
| PGY-1 | 9 (29.0) | 4 (20.0) |
| PGY-2 | 10 (32.3) | 11 (52.4) |
| PGY-3 | 9 (29.0) | 4 (19.0) |
| PGY-4 | 3 (9.7) | 2 (9.5) |
| Screen for SDH | ||
| No | 3 (9.7) | 2 (6.5) |
| Yes | 28 (90.3) | 19 (90.5) |
| SDH areas screened | ||
| Food | 30 (96.8) | 16 (76.2) |
| Housing | 20 (64.5) | 12 (57.1) |
| Transportation | 23 (74.1) | 15 (71.4) |
| Finances | 6 (19.4) | 5 (23.8) |
| Education access | 2 (6.5) | 0 (0.0) |
| Domestic violence | 5 (16.1) | 7 (33.3) |
| Employment | 0 (0.0) | 0 (0.0) |
| Other | 2 (6.5) | 3 (14.2) |
| Interventions for positive SDH | ||
| No intervention | 1 (3.2) | 0 (0.0) |
| Standardized resource list | 23 (74.2) | 14 (66.7) |
| Social work | 19 (61.3) | 14 (66.7) |
| Other | 4 (12.9) | 6 (28.6) |
| Feel comfortable discussing SDH (Fisher’s exact test = 0.40) | ||
| Strongly agree | 4 (12.9) | 5 (23.8) |
| Agree | 13 (41.9) | 10 (47.6) |
| Neutral | 9 (29.0) | 6 (28.6) |
| Disagree | 4 (12.9) | 0 (0.0) |
| Strongly disagree | 1 (3.2) | 0 (0.0) |
| Know where to refer patients for resources (Fisher’s exact test = 0.04) | ||
| Yes | 6 (19.4) | 8 (38.1) |
| Sometimes | 16 (51.6) | 12 (57.1) |
| No | 9 (29.0) | 1 (4.8) |
Analysis
For the pre- and post-intervention periods, t-test and χ2 tests were utilized to determine differences among patient ages and physician clinical training levels during the pre-intervention and post-intervention periods. For the resident survey data, Fisher’s exact test was utilized. Odds ratio was used to compare SDH resources and referrals provided during the 6-month period prior to the intervention with those provided during the first 6 months of the intervention. Intervention effectiveness was evaluated by measuring the monthly compliance of screening documented in the EMR, rates of positive screens, and rates of referrals for positive screens.
Results
Patient and Provider Characteristics
Pre- and post-intervention patient and physician characteristics were analyzed. There were 1761 visits during the pre-intervention period and 2728 visits during the post-intervention period. The patient mean age and age range were statistically different between the 2 time periods, with an older post-intervention population. The mean pre-intervention age was 3.72 and post-intervention age was 4.68 (P < .001) (see Table 1).
There were 51 different physicians who completed the visits. The majority were resident physicians in Post-graduate Year (PGY) 1 to 4. The level of training was statistically different with a higher proportion of PGY-1s, PGY-2s, and PGY-4s participating in the post-intervention period (see Table 1).
Resident Survey Results
There was a significant decrease in response rates for the resident surveys, with 31/46 (67.4%) and 21/46 (45.7%) completing the pre- and post-educational surveys respectively. There was no statistically significant difference between pre- and post-educational surveys for resident self-report of comfort with SDH discussions (P = .40). However, residents were more likely to self-report knowing where to refer patients for resources at least sometimes on the post-educational survey (P = .04) (see Table 2).
Screening Results
Overall, only 46% of eligible visits were screened (n = 1253) during the post-intervention period. Of the screened visits, 34.6% (n = 418) reported financial strain, 32% (n = 384) reported worry about food insecurity, 25.1% (n = 299) reported food insecurity, 5.3% (n = 64) reported medical transportation difficulties, and 6% (n = 73) reported daily living transportation difficulties (see Table 3).
Table 3.
Levels of Unmet Social Needs Among Those Screened Positive Post-Intervention.
| Social determinant | Post-intervention levels of unmet social need | Total (% of those screened) |
|---|---|---|
| Financial strain | Financial strain | 418 (34.6) |
| No financial strain | 789 (65.4) | |
| Not screened | 1519 | |
| Worry about food insecurity | Worry about food insecurity | 384 (32.0) |
| No worry about food insecurity | 815 (68.0) | |
| Not screened | 1527 | |
| Food insecurity | Food insecurity | 299 (25.1) |
| No food insecurity | 892 (74.9) | |
| Not screened | 1535 | |
| Medical transportation | Needs transportation | 64 (5.3) |
| Has transportation | 1156 (94.7) | |
| Not screened | 1506 | |
| Daily living transportation | Needs transportation | 73 (6.0) |
| Has transportation | 1148 (94.0) | |
| Not screened | 1505 |
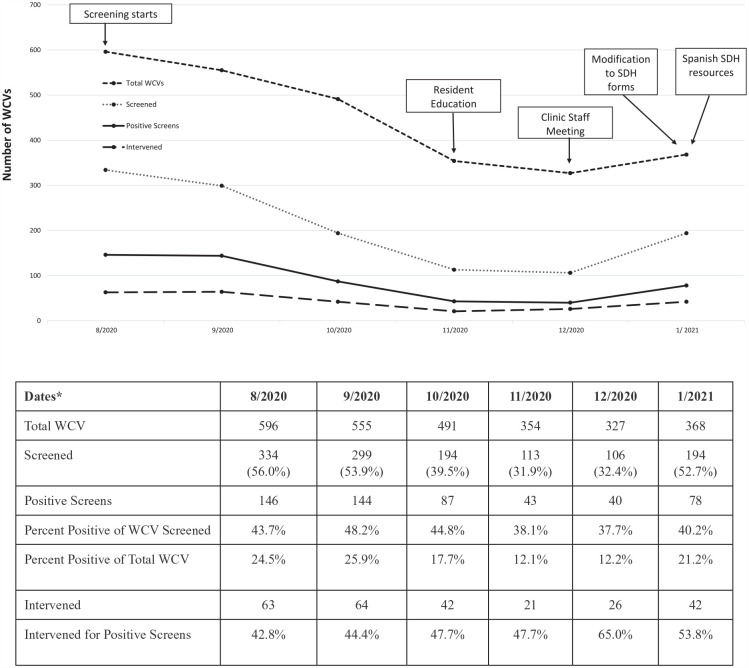
Monthly compliance rates of screening, percentage of positive screens, and interventions provided were determined for the post-intervention period (see Figure 1).
Figure 1.
Post-intervention monthly positive screens, WCVs, and interventions.
*Subjects from 2/2021 were eliminated to compare all full months.
Resources and Referrals
There was a statistically significant increase in resources offered or provided in the post-intervention period compared to the pre-intervention period (OR = 11.5 [7.1-18.6], P < .001). In total, 18 (0.57%) visits received any resource or referral for unmet social needs in the pre-intervention period compared to 289 (10.60%) post-intervention (see Table 4).
Table 4.
Resources Offered and Provided Per WCV.
| Resource | Pre-intervention (% of WCVs) | Post-intervention (% of WCVs)* |
|---|---|---|
| Written resource given | ||
| Any written resource | 8 (0.5) | 205 (7.5) |
| Standard resource list only | 6 (0.3) | 170 (6.2) |
| Written resource excluding the standard resource list | 2 (0.1) | 26 (1.0) |
| Standard resource list plus additional written resource | 0 (0.0) | 9 (0.3) |
| Social work offered | 10 (0.6) | 83 (3.0) |
| Follow-up appointments recommended | 0 (0.0) | 1 (0.0) |
| Any resource/help | 18 (1.0) | 289 (10.6) |
Statistically significant change in resources offered or provided between pre and post, OR = 11.5 (7.1-18.6), P < .001.
In the pre-intervention period, 8 (0.4%) visits received any written referral resource list. Of those, 6 (0.3%) received the standardized SDH referral resource list and 2 (0.11%) received another written resource. During the post-intervention period, 205 (7.6%) received any written referral resources. Of those, 170 (6.2%) received the standardized referral resource list alone, 26 (1.0%) received written resources excluding the standard list, and 9 (0.3%) received the standardized resource list plus other written resource(s) (see Table 4).
For social work referrals, 10 (0.6%) families were given referrals pre-intervention and 83 (3.0%) were given referrals post-intervention. Zero follow-up appointments specifically for SDH were recommended during the pre-intervention period and 1 was recommended post-intervention (see Table 4).
Discussion
Impacts of the Pandemic
The COVID-19 pandemic and its impacts affected the clinic’s patient population prioritized for care during the period of social distancing and limiting exposure from in-person visits. The clinic in the study followed the ambulatory care guidelines released in April 2020 by the American Academy of Pediatrics (AAP) and supported by the Centers for Disease Control (CDC) for pediatric care during the pandemic. In-person newborn care, newborn well visits, and immunizations of infants and young children through 24 months of age were prioritized, and telehealth services were utilized for older children. 19 The clinic followed AAP guidelines and did not prioritize in-person WCVs for older children until May 2020. Since SDH screening was only completed for in-person WCVs, the pre-intervention phase had a much higher proportion of younger children compared to the post-intervention phase. In both the pre-intervention and post-intervention periods, few follow-up visits were recommended for unmet social needs to accommodate the challenges of in-person visits during the pandemic. In the future, an area of improvement could be to encourage follow-up visits to provide additional support for unmet social needs.
Another consequence of limiting in-person visits was the decrease in clinic staff that began during the pre-intervention period. With limited in-person WCVs and the shift to telehealth, staff furloughs and layoffs occurred. Shortage in staff occurred due to a combination of complications related to the furloughs and layoffs of staff. For example, there was a lag between an increase in WCVs and when administration allowed staff to return from furlough. The administration wanted to be assured of the consistency of increased visit numbers. For new staff, the hiring and training process was also time intensive. As a result, there were fewer trained clinic staff available to assist with the SDH screening process. Since SDH screening is initiated by the front desk staff and entered into the EMR by the PCTs, MAs, or nurses, this likely contributed to the lower-than-expected screening rates and interventions for positive screens in the post-intervention period.
The differences in the pre-intervention and post-intervention distribution of resident clinical level of training can be attributed to 2 main causes. The first is that there is a delay before PGY-1s start their continuity clinic. They receive orientation and time to transition to their first rotation in June-July of each academic year. The second is that resident staffing changes were made due to the pandemic. To limit exposure, individual pediatric residents were limited to either inpatient- or outpatient-only services for the first several months of the pandemic.
Impacts of Quality Improvement Initiatives
Universal SDH screening for in-person WCVs was implemented on 8/3/2020. The percentage of WCVs screened was the highest in the first month of implementation at 56% of eligible visits. The first month compliance rate was comparable to the literature for short-term SDH screening rates, ranging from 56% to 70%. However, the compliance rate continued to decrease and reached its nadir for the studied intervention period during 12/2020. Since monthly compliance was tracked, the decreasing rates resulted in several interventions to increase compliance. On 11/30/20, an SDH-focused resident educational session occurred during the morning report conference. On 12/17/20, representatives of the SDH research group met with the clinic medical director, clinical coordinator, and the LUMC quality improvement (QI) team to discuss additional interventions. Outcomes of this meeting included reminders to clinic front desk staff, PCTs, MAs, and nurses about SDH screening. In addition, concerns were raised that SDH questionnaire refusals were not being entered into the EMR. A modification to the SDH screening form was officially implemented on 1/13/21. The italicized message about changes during the pandemic and the fact that we care about our patients’ families, as well as the first pre-screening question clarifying whether families were not interested in completing the screening or had already completed it at a recent visit were added. Since our clinic also serves a significant proportion of Spanish-speaking families, a Spanish SDH resource list was added on 1/25/21.
Most of the QI interventions occurred toward the end of the time reviewed. Therefore, analysis of the longer-term impacts is limited. However, some preliminary short-term impacts are evident. The first 4 months of the post-intervention review period show a marked decline in SDH screening. The latter 2 months show a plateau and then an increase in January. We attribute this increase to the clinic staff meeting and SDH form modifications to capture refusals since the initiation of SDH screening is front-desk-staff driven.
The rate of intervention for positive screens increased overall during the post-intervention period. Since this is mostly resident driven for the majority of WCVs, we attribute this to the cumulative effects of the resident education provided in November, and subsequent availability of a Spanish SDH resource list.
During the first 6 months of the SDH screening and referral pilot program, the monthly rates of documented screening ranged from 31.9% to 56.0%. Previous literature of SDH screening at urban primary care centers have yielded screening rates ranging from 56% to 70%.12-14 These screening rates are higher than the ones observed in our study. However, ours is the only study to coincide with the unique challenges of the worldwide COVID-19 pandemic.
Despite the low compliance rates, the percentage of self-reported unmet SDH needs ranged from 37.7% to 48.2% of those screened. Of those that screened positive, monthly rates of documented interventions ranged from 42.8% to 65.0%. Compared to the 6 months immediately preceding the implementation of the intervention, there was a significant increase in the volume of resources provided by the physicians. Although the resident survey did not find an increase in self-reported comfort level with SDH discussions, residents were more confident in referring patients for resources post-intervention.
Strengths and Limitations
The results highlight both the strengths and limitations of this pilot intervention. The strengths include the introduction of SDH screening and referrals during a period of socioeconomic stress due to the COVID-19 pandemic, when referrals for unmet social needs were very timely. Another strength was that this pilot intervention and study was completed without any outside funding or additional personnel. The new protocol was integrated into the existing infrastructure of the clinic. Finally, this study provided both education and experiential training for resident physicians.
Although the pilot intervention was cost-effective, its use of existing resources likely contributed to lower-than-expected compliance rates. The new protocol required additional training and time investment from heavily burdened clinic staff and physicians. The reliance on multiple layers of clinic staff to provide the screening questionnaire, document the responses, discuss results, and provide resources proved challenging to coordinate. Staff may easily forget to complete one or more of the steps, causing screens to be incomplete. This likely contributed to the number of positive screens lacking any documented referrals since the physicians relied on clinic staff to communicate positive screens to them.
Additionally, there was little flexibility in adapting the SDH screen since the pilot project was part of a larger institutional initiative which was standardized across the hospital system. The standardization resulted in crucial SDH areas of need being excluded, such as housing, mental health, disabilities, substance use, and interpersonal violence.
For the resident survey, there was a substantial decrease in response rates from the pre- to the post-educational resident surveys. We suspect that the decrease in response rates was at least partially related to survey fatigue. The surveys were also completely anonymous and unmatched. Therefore, there was no way to track whether individual residents reported any change in answers from the pre- to the post-educational surveys.
Conclusions
The compliance rates of documented SDH screenings and resource referrals for positive screens remained suboptimal during the first 6 months of the pilot intervention. This reflects the challenges found in previous studies regarding SDH screening and referral. Unlike previous studies, this pilot reviewed a longer period of SDH screening implementation. Additionally, this pilot study is complicated by the fact that its implementation coincided with the beginning of the COVID-19 pandemic. Also, unlike some prior SDH studies, this pilot was completed without any additional funding or personnel and was integrated into the existing workflow of a mostly resident-staffed primary care clinic setting. Despite these challenges, this pilot did show the feasibility of introducing SDH screening and increasing resource referrals during a period of socioeconomic difficulties for families impacted by the COVID-19 pandemic.
Supplemental Material
Supplemental material, sj-doc-1-gph-10.1177_2333794X211060971 for Social Determinants of Health Screening at Well Child Visits: A Pilot Program Implemented During the COVID-19 Pandemic by Pyone David, Nadia K. Qureshi, Lina Ha, Vera Goldberg, Erin McCune, Jennifer Wojtowicz, Katlyn Sullivan, Garry Sigman and Julie C. O’Keefe in Global Pediatric Health
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Pyone David  https://orcid.org/0000-0003-3214-1628
https://orcid.org/0000-0003-3214-1628
Erin McCune  https://orcid.org/0000-0001-5154-2043
https://orcid.org/0000-0001-5154-2043
Julie C. O’Keefe  https://orcid.org/0000-0003-3863-1257
https://orcid.org/0000-0003-3863-1257
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Greater New York Hospital Association. Training primary care residents on social determinants of health. Accessed March 11, 2021. https://www.gnyha.org/tool/training-primary-care-residents-on-the-social-determinants-of-health
- 2. Narayan A, Raphael J, Rattler T, Bocchini C. (eds.). Social determinants of health. Accessed March 11, 2021. https://www.texaschildrens.org/sites/default/files/uploads/documents/83176%20BRIEF%20Social%20Determinants%20of%20Health%20Policy%20Digital.pdf
- 3. Chung EK, Siegel BS, Garg A, et al. Screening for social determinants of health among children and families living in poverty: a guide for clinicians. Curr Probl Pediatr Adolesc Health Care. 2016;46(5):135-153. doi: 10.1016/j.cppeds.2016.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Narayan A, Raphael J, Rattler T, Bocchini C. Social determinants of health. Accessed January 23, 2021. https://www.texaschildrens.org/sites/default/files/uploads/documents/83176%20BRIEF%20Social%20Determinants%20of%20Health%20Policy%20Digital.pdf
- 5. Bittner JC, Thomas N, Correa ET, Hatoun J, Donahue S, Vernacchio L. A broad-based approach to social needs screening in a pediatric primary care network. Acad Pediatr. 2021;21:694-701. [DOI] [PubMed] [Google Scholar]
- 6. Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics. 2015;135(2):e296-e304. doi: 10.1542/peds.2014-2888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Selvaraj K, Ruiz MJ, Aschkenasy J, et al. Screening for toxic stress risk factors at well-child visits: the addressing social key questions for health study [published correction appears in J Pediatr. 2020 Jan;216:255-256]. J Pediatr. 2019;205:244-249.e4. doi: 10.1016/j.jpeds.2018.09.004 [DOI] [PubMed] [Google Scholar]
- 8. Morone J. An integrative review of social determinants of health assessment and screening tools used in pediatrics. J Pediatr Nurs. 2017;37:22-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Andermann A. Screening for social determinants of health in clinical care: moving from the margins to the mainstream. Public Health Rev. 2018;39:19. doi: 10.1186/s40985-018-0094-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Olson DP, Oldfield BJ, Navarro SM. Screening for social determinants of health among children and families living in poverty: a guide for clinicians. Health Aff. Published online March 18, 2019. doi: 10.1377/hblog20190311.823116 [DOI] [Google Scholar]
- 11. Morgenlander MA, Tyrrell H, Garfunkel LC, Serwint JR, Steiner MJ, Schilling S. Screening for social determinants of health in pediatric resident continuity clinic. Acad Pediatr. 2019;19(8):868-874. doi: 10.1016/j.acap.2019.02.008 [DOI] [PubMed] [Google Scholar]
- 12. Garg A, Butz AM, Dworkin PH, Lewis RA, Thompson RE, Serwint JR. Improving the management of family psychosocial problems at low-income children’s well-child care visits: the WE CARE project. Pediatrics. 2007;120(3):547-558. doi: 10.1542/peds.2007-0398 [DOI] [PubMed] [Google Scholar]
- 13. Sokol R, Austin A, Chandler C, et al. Screening children for social determinants of health: a systematic review. Pediatrics. 2019;144(4):e20191622. doi: 10.1542/peds.2019-1622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Buitron de la Vega P, Losi S, Sprague Martinez L, et al. Implementing an EHR-based screening and referral system to address social determinants of health in primary care. Med Care. 2019;57(6 Suppl 2):S133-S139. doi: 10.1097/MLR.0000000000001029 [DOI] [PubMed] [Google Scholar]
- 15. Dorn AV, Cooney RE, Sabin ML. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395(10232):1243-1244. doi: 10.1016/S0140-6736(20)30893-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Abrams EM, Szefler SJ. COVID-19 and the impact of social determinants of health. Lancet Respir Med. 2020;8(7):659-661. doi: 10.1016/S2213-2600(20)30234-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Burström B, Tao W. Social determinants of health and inequalities in COVID-19. Eur J Public Health. 2020;30(4):617-618. doi: 10.1093/eurpub/ckaa095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wang Z, Tang K. Combating COVID-19: health equity matters. Nat Med. 2020;26(4):458. doi: 10.1038/s41591-020-0823-6 [DOI] [PubMed] [Google Scholar]
- 19. Korioth T. AAP issues guidance to ensure continued care for children during pandemic. Am Acad Pediatr. 2020. Accessed November 17, 2021. https://publications.aap.org/aapnews/news/6715 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-doc-1-gph-10.1177_2333794X211060971 for Social Determinants of Health Screening at Well Child Visits: A Pilot Program Implemented During the COVID-19 Pandemic by Pyone David, Nadia K. Qureshi, Lina Ha, Vera Goldberg, Erin McCune, Jennifer Wojtowicz, Katlyn Sullivan, Garry Sigman and Julie C. O’Keefe in Global Pediatric Health