Highlights
-
•
A total of 88 patients experienced light flashes among 416 who received photon radiotherapy and 205 who received proton beam therapy in our prospective study.
-
•
The frequency of light flashes during radiotherapy was associated with the retina dose and younger age, and were commonly blue or white light for brain or head and neck irradiation.
-
•
Light flashes were seen by only 35/524 patients (6.7%) without retinal irradiation, but by 13/33 (39.4%) and 41/64 (64.1%) with retinal maximum isodose lines of 10–50% and 60–100%, respectively.
-
•
Totals of 52, 15, 15, 9, 16 and 8 patients sensed light of blue, purple, yellow, red, white and other colors, respectively.
Keywords: Radiotherapy, Light flash, Cherenkov, Observation study, Prospective
Abstract
Background
Patients who receive radiation therapy sometimes complain of a light flash during irradiation. The details of the characteristics of this light have not been described.
Purpose
To evaluate light flashes during photon and proton radiotherapy.
Methods and Materials
A prospective observational study was performed in all adult patients (≥20 years old) who received photon and proton therapy at two centers between January 2019 and August 2020, except for patients who could not communicate and those with visual abnormality. Evaluations were obtained for the presence or absence of light flashes, light darkness (7 levels), light intensity (5 levels), frequency, light movement, light flashing, and time seeing the light, using a weekly checklist.
Results
A total of 650 courses were examined for 621 patients, of whom 416 received photon radiotherapy and 205 received proton beam therapy. The checklist indicated that 88 patients (16.1%) sensed light during photon or proton radiotherapy. In multivariate logistic regression analysis, the factors that were significantly associated with a light flash were a higher retina dose and younger age (p < 0.001). Light flashes were seen by only 35/524 patients (6.7%) for whom the retina was not irradiated, but by 13/33 (39.4%) and 41/64 (64.1%) with maximum isodose lines for the retina of 10–50% and 60–100%, respectively. The numbers of patients who sensed blue, purple, yellow, red, white and other colors were 52, 15, 15, 9, 16 and 8, respectively (multiple selections possible). Light movement was observed by 52 patients (59%). The location of the light was defined as near, far, and middle by 70, 13, and 5 patients, respectively. The median time the light was seen was 10 s.
Conclusions
Many patients sense light flashes during radiotherapy. The retina dose and a younger age were significantly associated with the frequency of light flashes.
Introduction
Some patients who receive radiation therapy complain that a light appears, even when they close their eyes. This phenomenon is referred to as phosphene or more recently as Cherenkov light [1], [2], [3], which is due to visible photons produced when a charged particle travels through a transparent medium at a speed greater than the speed of light in that medium [4], [5]. Cherenkov light was first observed by Marie Curie in 1910 as a pale blue light from concentrated radium in a dark room [6], [7]. Subsequently, Pavel Alekseyevich Cherenkov, a Russian scientist, first described blue light emission in 1934. In MV radiation therapy, Cherenkov light is produced throughout irradiated tissue, with intensity proportional to the local absorbed dose. Several recent clinical reports indicate that patients rarely see dazzling light during radiotherapy, but light that is sensed is considered to be Cherenkov light. Tender et al. detected Cherenkov light through a patient eye during stereotactic radiotherapy [2]. However, the details of the characteristics of the light that patients see have not been described. Here, we report a multicenter prospective observational study of the perception of light flashes during photon radiotherapy and proton beam therapy.
Patients and methods
The study was performed in two centers from January 2019 to August 2020, and was approved by both institutional review boards (R01-160, Tsukuba Clinical Research & Development Organization; 2019–038, Tsukuba Medical Center Hospital). Photon radiotherapy was performed at both centers and proton beam therapy was performed at one. All adult patients (≥20 years old) who received photon and proton therapy in the study period were included, except for patients who could not communicate and those with visual abnormality. Visual abnormality was defined as the inability to distinguish colors on a chart with or without glasses.
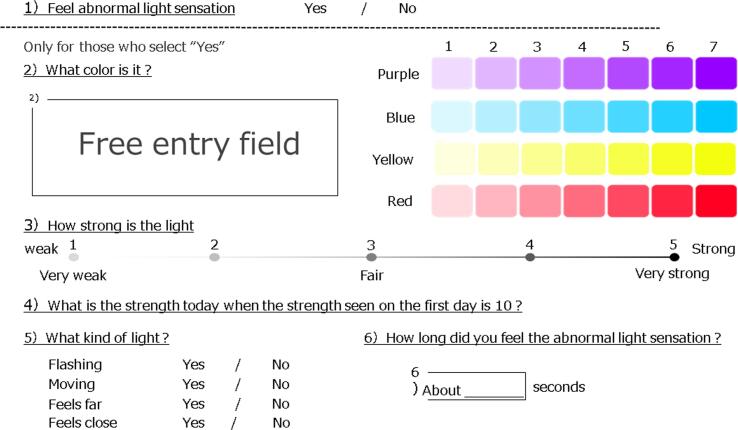
Light flashes observed when the eyes were closed during irradiation were evaluated. Evaluations were made for the presence or absence of light, light darkness (7 levels), light intensity (5 levels), frequency, light movement, light flashing, and time to see the light, using a survey checklist that was completed each week. An English translation of the checklist (originally written in Japanese) is shown in Fig. 1. The light flashes were categorized as: 1 Sense of light flashes (Yes/No); 2 What color? (Purple/Blue/Yellow/Red, 1–7 darkness); 3 How strong? (1–5, 1 very weak, 3 fair, 5 very strong); 4 What kind of light (flashing, moving, feels far, feels close), 5 How long did you sense light flashes during irradiation? This checklist was generated by a team of radiation oncologists.
Fig. 1.
An English translation of the checklist (originally written in Japanese).
The dose-rate of photon therapy was 400–600 MU/min and that of proton therapy was 1300 MU/min. Proton beam irradiation was performed discontinuously. The median total dose of photon radiotherapy was 50 (8–78) Gy in 25 (1–48) fractions, and that of proton beam therapy was 63 (30–78.4) GyE in 22 (10–56) fractions.
Statistical analysis
Multivariate logistic regression, odds ratio, and linear regression models were used for binary (presence or absence of light), ordinal scale (light darkness, light intensity, frequency, light movement, and light flashing), and continuous (natural logarithm of time seeing the light) outcomes, respectively. Each model included gender, age, irradiated site (brain or head and neck, other), retina dose (maximum irradiation dose for either eye), and radiotherapy method (proton, other) as explanatory variables. Statistical significance was defined as p < 0.05.
Results
Some patients received multiple courses of radiation therapy during the study period, and thus, a total of 650 courses for 621 patients were examined. If patients received radiation therapy to multiple sites on the same day, this was counted as one course. The patient characteristics are shown in Table 1. A total of 416 patients received photon radiotherapy (3D-CRT for 297, IMRT for 119) and 205 received scattering proton beam therapy. The patients who received photon radiotherapy had a median age of 69 (28–93) years, and included 241 males and 175 females. The irradiation sites for photon radiotherapy were the brain, head and neck, chest, abdomen, pelvis and limbs in 93, 27, 147, 18, 125 and 6 cases, respectively. The patients who received proton beam therapy had a median age of 69 years (range: 20–92), and included 165 males and 40 females. The irradiation sites for proton beam therapy were the brain, head and neck, chest, abdomen, pelvis and limbs in 12, 29, 28, 41, 94, and 1 cases, respectively.
Table 1.
Patient characteristics.
| Characteristics | Photon (N = 416) | Proton (N = 205) |
|---|---|---|
| Age (years) | 28–93 (range) 69 (median) |
20–92 69 |
| Gender | ||
| Male | 241 | 165 |
| Female | 175 | 40 |
| Irradiated Site | ||
| Brain | 93 | 12 |
| Head and Neck | 27 | 29 |
| Chest | 147 | 28 |
| Abdomen | 18 | 41 |
| Pelvis | 125 | 94 |
| Limbs | 6 | 1 |
| Radiotherapy Technique | ||
| 3D-CRT | 297 | 0 |
| IMRT | 119 | 0 |
| Proton | 0 | 205 |
| Total dose and fractions | ||
| Photon | 50 (8–78) Gy in 25 (1–48) fractions | |
| Proton | 63 (30–78.4) GyE in 22 (10–56) fractions | |
The survey checklist showed that 88 patients (16.1%) sensed light during photon therapy or proton beam therapy. The details of these 88 patients are shown in Table 2. Light flashes during radiotherapy were sensed by 54/97 (62%) and 34/524 (6%) of patients in whom the retina was and was not irradiated, respectively. Of the 88 patients, 73 (83%) received photon radiotherapy. The median age was 64 years, and light flashes occurred in 15/60 (25%) and 73/561 (13%) of patients aged < 50 and ≥50 years, respectively. Light flashes were sensed by 44/105 patients (42%) with a brain tumor, 17/56 (30%) with a head and neck tumor, 18/174 (10%) with a chest tumor, and <5% with other tumors. All 27 patients who sensed a light flash during irradiation of the body trunk received photon radiotherapy.
Table 2.
Rate of light flashes.
| Characteristics | Light Flashes | No Light Flashes | Rate of Light Flashes (%) |
|---|---|---|---|
| Retina | |||
| Irradiated | 54 | 43 | 62% |
| Not irradiated | 34 | 490 | 6% |
| Age (years) | |||
| <50 | 15 | 45 | 25% |
| >50 | 73 | 488 | 13% |
| Gender | |||
| Male | 50 | 356 | 12% |
| Female | 38 | 177 | 18% |
| Irradiated Site | |||
| Brain | 44 | 61 | 42% |
| Head and Neck | 17 | 39 | 30% |
| Chest | 18 | 156 | 10% |
| Abdomen | 1 | 58 | 2% |
| Pelvis | 8 | 211 | 4% |
| Limbs | 0 | 7 | 0% |
| Radiotherapy Technique | |||
| 3D-CRT | 61 | 236 | 21% |
| IMRT | 12 | 107 | 10% |
| Proton | 15 | 190 | 7% |
Most of the patients observed light of a white or blue color. Red and yellow light was seen by 6 and 2 patients, respectively, and all these patients received photon radiotherapy. Of the 88 patients, 53 sensed light in every treatment, and all patients who sensed light with proton therapy had this experience during every treatment.
Factors associated with a sense of light flashes were analyzed by multivariate logistic regression analysis, and retina dose (OR = 1.031, p < 0.001) and age (OR = 0.968, p = 0.003) were identified as significant factors (Table 3). Light flashes occurred in only 35/524 patients (6.7%) in whom the retina was not irradiated, but in 13/33 (39.4%) and 41/64 (64.1%) with maximum isodose lines for the retina of 10–50% and 60–100%, respectively. For patients without retina irradiation, light flashes occurred in 4/53 (7.5%) and 30/471 (6.5%) of age ≤ 50 and >50 years, respectively; whereas in patients with retina irradiation, 11/17 (64.7%) and 43/80 (53.8%) of age ≤ 50 and >50 years, respectively, sensed light flashes.
Table 3.
Multivariate logistic regression analyses for a sense of light, light darkness, light intensity, and light flashing.
| Effect | Variable | Odds ratio | 95% CI | p value |
|---|---|---|---|---|
| Sense of light | Gender (female/male) | 1.150 | 0.648–2.043 | 0.633 |
| Age | 0.968 | 0.947–0.989 | 0.003 | |
| Irradiated site (brain, H&N/other) | 1.359 | 0.643–2.875 | 0.422 | |
| Retina dose | 1.031 | 1.022–1.040 | <0.001 | |
| Radiotherapy method (proton/other) | 0.451 | 0.222–0.916 | 0.028 | |
| Light darkness | Gender (female/male) | 0.117 | 0.065–0.481 | <0.001 |
| Age | 1.024 | 0.986–1.064 | 0.218 | |
| Irradiated site (brain, H&N/other) | 2.809 | 0.879–8.975 | 0.081 | |
| Retina dose | 1.002 | 0.990–1.015 | 0.726 | |
| Radiotherapy method (proton/other) | 0.570 | 0.138–2.363 | 0.439 | |
| Light intensity | Gender (female/male) | 1.358 | 0.597–3.088 | 0.465 |
| Age | 1.026 | 0.992–1.061 | 0.130 | |
| Irradiated site (brain, H&N/other) | 0.820 | 0.308–2.185 | 0.691 | |
| Retina dose | 1.006 | 0.994–1.017 | 0.318 | |
| Radiotherapy method (proton/other) | 0.855 | 0.257–2.846 | 0.798 | |
| Light flashes | Gender (female/male) | 1.683 | 0.469–6.043 | 0.425 |
| Age | 0.979 | 0.933–1.027 | 0.380 | |
| Irradiated site (brain, H&N/other) | 2.370 | 0.529–10.622 | 0.260 | |
| Retina dose | 0.996 | 0.980–1.013 | 0.680 | |
| Radiotherapy method (proton/other) | 19.453 | 3.223–117.423 | 0.001 |
The color and darkness of the light varied, but most was a blue shade color. The numbers of patients who observed blue, purple, yellow, red, white and other colors were 52, 15, 15, 9, 16, and 8, respectively, with multiple selections possible. The median darkness was 4 and females were significantly more likely to sense darker light (OR = 0.177, p < 0.001, Table 3). The median intensity was 3.0 for all patients and there was no significant factor associated with light intensity (Table 3). The irradiation method was significantly associated with a light flash (OR = 19.453, p < 0.001, Table 3). Patients who received proton therapy saw a light flash (10/16; 62.5%) more frequently than those treated with photon radiotherapy (11/72; 15.3%). Light movement was observed by 52 patients (59%). The location of the light was near, far, and middle in 70, 13, and 5 patients, respectively, and the median time the light was seen was 10 s (range: 1–180 s). No significant factor was associated with movement, location, or time.
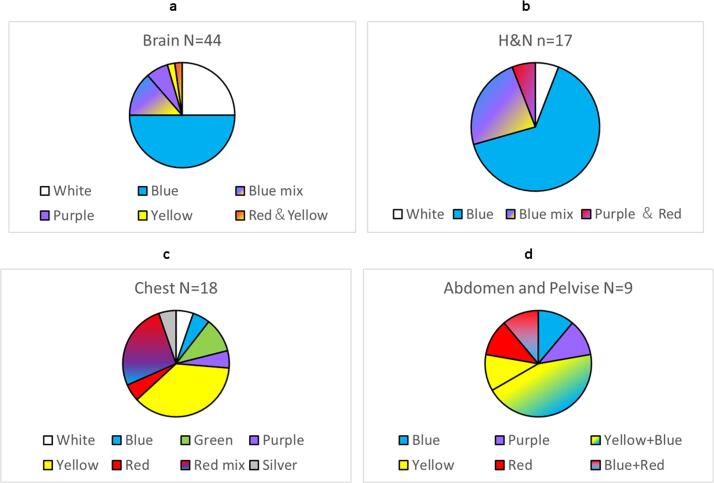
Regarding the relationship between color and the irradiation site, patients who received radiation therapy to the brain and head and neck tended to observe blue or white light, whereas red or yellow light tended to be seen during radiotherapy to other sites. The percentages of colors for each irradiation site are shown in Fig. 2a–2d. Of the 44 patients with brain irradiation, 22 and 11 sensed blue and white light, 6 observed blue mixed color light (blue and yellow, blue and purple, etc.), and 3 saw purple light. Only one patient sensed red-yellow light. Of patients with head and neck irradiation, 11 and 1 sensed blue and white light, 4 saw blue mixed light, and one saw purple and red mixed light. In contrast, among 18 patients with chest irradiation, only 2 each saw blue and white light, and of the 9 patients with abdomen and pelvis irradiation, only one observed blue light and none saw white light.
Fig. 2.
a) The percentages of colors received irradiation for brain. b) The percentages of colors received irradiation for head and neck (H&N). c) The percentages of colors received irradiation for chest. d) The percentages of colors received irradiation for abdomen and pelvis.
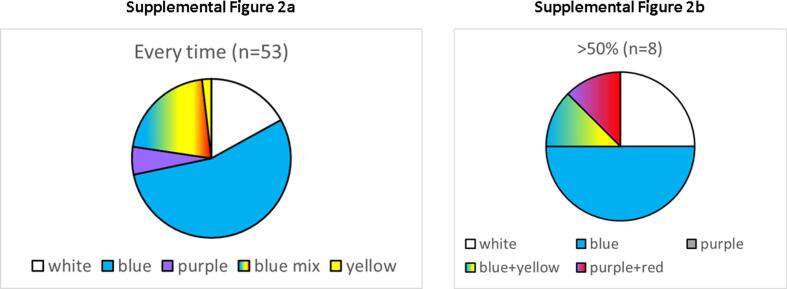
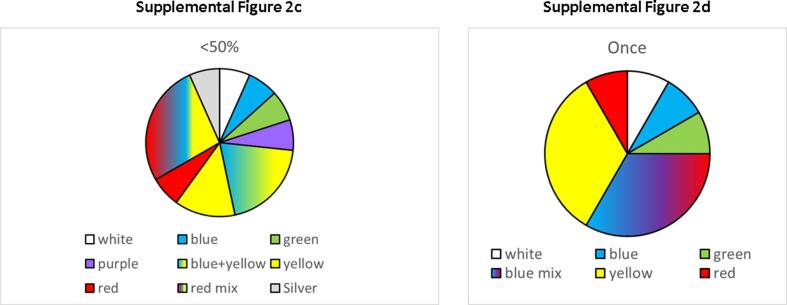
Light was observed at a high frequency in radiotherapy to the brain or head and neck, but at a lower frequency (<50%) in radiotherapy to the body trunk (Supplemental Fig. 1). Blue or white light was observed at a high rate (>50%) during radiotherapy, whereas colors such as yellow and red were observed less frequently (Supplemental Fig. 2a-d). The RGB codes used in the checksheet are shown in Supplemental Fig. 3.
Discussion
Patients may sense light flashes during radiotherapy and this light has been suggested to be Cherenkov light. Tendler et al. visualized Cherenkov light in the eye during SRT [2]. It is generally considered that light flashes are phenomena that occur in radiotherapy to the brain or head and neck area [8], [9], [10], and in the current study, the dose to the retina was the significant factor associated with a light flash. For example, in a chordoma case treated with proton therapy at our center, the retina is covered with a full dose in the initial plan, and then the treatment field is shrunk and the retina dose is reduced to doses of 50% and 0%. Thus, we experience patients who sense a light flash with the initial plan, but the light intensity is reduced with shrinkage. This suggests that the retina and eye dose can affect light flashes.
The proton beam energy is below the Cherenkov light energy, and thus, light flashes may not be caused by Cherenkov light in proton therapy. Schardt et al. reported light flashes in cancer patients treated with heavy ions [11], with patients reporting mostly white light flashes, with 10% yellow. The ion beam energy is also below that of Cherenkov light, indicating that this light flash is also not caused by Cherenkov light. Instead, the main mechanism may be production of energy deposition by charged particles in the retina [11]. Therefore, there may be a similar mechanism of light flashes in proton therapy and ion beam therapy, but most of the color was blue to purple in proton therapy, with 19% (3/16) white. Local energy transfer differs between heavy ions and proton beams, but it is unclear if this difference gives a signal to the optic nerve.
The color of Cherenkov light is blue to purple, and in this study, blue and purple were dominant in radiotherapy to the brain or head and neck. In contrast, red and yellow light was dominant for patients with radiotherapy for the body trunk. However, the red and yellow light was observed incidentally, and no patients who received proton therapy to the trunk sensed a light flash. This may be because light sensing during radiotherapy for the trunk is due to floating secondary electrons produced in the gantry nozzle, which may directly, but incidentally, hit the retina. The energy of secondary electrons in a proton beam is lower than that in a photon beam, and therefore, no patients sensed light during proton therapy for the trunk. The difference in color may be due to the energy of the charged particle, but this is unclear.
The study found that about 50% of patients whose retina was irradiated felt light flashes during radiotherapy. This number was much higher than expected. There were no symptomatic adverse events caused by light flashes during the survey period, but some patients indicated that they felt anxious because they misunderstood the light flashes as a side effect of radiotherapy. Therefore, the results of this study are useful as a basis for an explanation to patients that seeing light flashes during radiotherapy is a common phenomenon when the retina is irradiated. This explanation is likely to reduce patient anxiety. However, the validity of the test method was not established because the checksheet was prepared only by radiation oncologists, and visual performance of the subjects was not evaluated by an ophthalmologist before the study.
In conclusion, light flashes were observed at a high rate by patients who received proton beam therapy or photon radiotherapy, and the dose to the retina was a significant factor. These flashes were also sometimes observed during radiation therapy for the body trunk.
Funding
This work was supported by the University of Tsukuba, Japan.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.tipsro.2021.11.003.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
Supplementary Fig. 1.
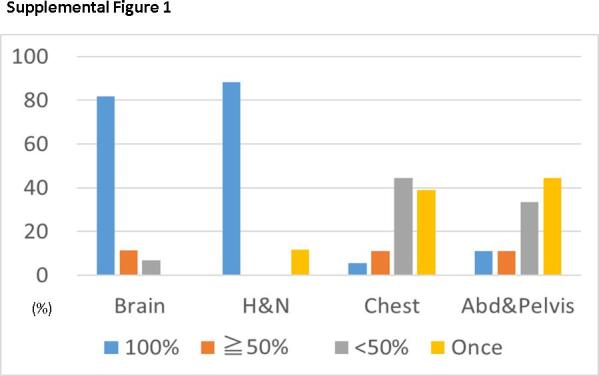
Frequency of light during irradiation to each site.
Supplemental Fig. 2a and 2b.
a). The percentages of colors who felt light every time. b) The percentages of colors who felt light more than 50%.
Supplemental Fig. 2c and 2d.
c) The percentages of colors who felt light less than 50%. d) The percentages of colors who felt light at once.
Supplementary Fig. 4.
References
- 1.Soter J.A., LaRochelle E.P.M., Byrd B.K., et al. Tracking tumor radiotherapy response in vivo with Cherenkov-excited luminescence ink imaging. Phys Med Biol. 2020;65 doi: 10.1088/1361-6560/ab7d16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tendler I.I., Hartford A., Jermyn M., et al. Experimentally observed cherenkov light generation in the eye during radiation therapy. Int J Radiat Oncol Biol Phys. 2020;106:422–429. doi: 10.1016/j.ijrobp.2019.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yoon S.W., Tsvankin V., Shrock Z., et al. Enhancing radiation therapy through cherenkov light-activated phototherapy. Int J Radiat Oncol Biol Phys. 2018;100:794–801. doi: 10.1016/j.ijrobp.2017.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Newman F., Asadi-Zeydabadi M., Durairaj V.D., Ding M., Stuhr K., Kavanagh B. Visual sensations during megavoltage radiotherapy to the orbit attributable to Cherenkov radiation. Med Phys. 2008;35:77–80. doi: 10.1118/1.2815358. [DOI] [PubMed] [Google Scholar]
- 5.Steidley K.D., Eastman R.M., Stabile R.J. Observations of visual sensations produced by Cerenkov radiation from high-energy electrons. Int J Radiat Oncol Biol Phys. 1989;17:685–690. doi: 10.1016/0360-3016(89)90125-9. [DOI] [PubMed] [Google Scholar]
- 6.Fazio G.G., Jelley J.V., Charman W.N. Generation of Cherenkov light flashes by cosmic radiation within the eyes of the Apollo astronauts. Nature. 1970;228:260–264. doi: 10.1038/228260a0. [DOI] [PubMed] [Google Scholar]
- 7.Stevens T.E., Wahlstrand J.K., Kuhl J., Merlin R. Cherenkov radiation at speeds below the light threshold: phonon-assisted phase matching. Science. 2001;291:627–630. doi: 10.1126/science.291.5504.627. [DOI] [PubMed] [Google Scholar]
- 8.Blumenthal D.T., Corn B.W., Shtraus N. Flashes of light-radiation therapy to the brain. Radiother Oncol. 2015;116:331–333. doi: 10.1016/j.radonc.2015.07.034. [DOI] [PubMed] [Google Scholar]
- 9.Thariat J., Leal C., d'Ascoli A., et al. Phosphenes in patients receiving radiotherapy. Lancet Oncol. 2016;17:869–871. doi: 10.1016/S1470-2045(16)30034-1. [DOI] [PubMed] [Google Scholar]
- 10.Mathis T., Vignot S., Leal C., et al. Mechanisms of phosphenes in irradiated patients. Oncotarget. 2017;8:64579–64590. doi: 10.18632/oncotarget.18719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schardt D., Kavatsyuk O., Kramer M., Durante M. Light flashes in cancer patients treated with heavy ions. Brain Stimul. 2013;6:416–417. doi: 10.1016/j.brs.2012.08.003. [DOI] [PubMed] [Google Scholar]