Abstract
A 39-year-old male was admitted in the emergency room with chest pain. He had been given the second dose of Pfizer–BioNTech COVID-19 vaccine 3 days before. The patient denied taking any other medication beyond the usual. He didn’t feel sick in the previous days/weeks. Laboratory studies revealed elevated serum levels of troponin and C-reactive protein. An autoantibody screen and a serologic panel to detect common viruses were negative. A cardiac MRI showed myocardial edema/inflammation and confirmed the diagnosis of perimyocarditis which was considered to be a consequence of COVID-19 vaccination. Physicians should be aware of the possibility of cardiovascular complications after COVID-19 vaccination.
Keywords: Myocarditis, vaccination, COVID-19, mRNA vaccine
Introduction
Globally, as of 30th July 2021, there have been 196 553 009 confirmed cases of COVID-19, including 4 200 412 deaths. As of 29th July 2021, a total of 3 839 816 037 vaccine doses have been administered. 1 As of 26th July 2021, Vaccine Adverse Event Reporting System (VAERS) has received 1194 reports of myocarditis or pericarditis among people aged 30 and younger who received COVID-19 vaccine. Through follow-up, including medical record reviews, Centers for Disease Control (CDC) 2 and Food and Drug Administration (FDA) have confirmed 699 reports of myocarditis or pericarditis.
Case Report
A 39-year-old male, was admitted to the emergency room (ER) with pleuritic chest pain, which started the night before and progressively worsened. The patient also mentioned fever, headache, and myalgias in the 3 previous days.
Physical examination showed tachycardia (120 bpm) and a pericardial friction on cardiac auscultation.
The patient had a personal medical history of gastritis and depressive syndrome. No relevant family medical history of cardiac disease was reported. The patient was medicated with lansoprazole, escitalopram, sulpiride, and mexazolam. He had been given the second dose of Pfizer-BioNTech COVID-19 COMIRNATY® vaccine 3 days before the onset of chest pain. He didn’t have any symptom after the administration of the first dose of the vaccine.
The patient denied taking any other medication beyond the usual, drug use or drug allergies. He didn’t feel sick in the previous days/weeks neither did his cohabitants.
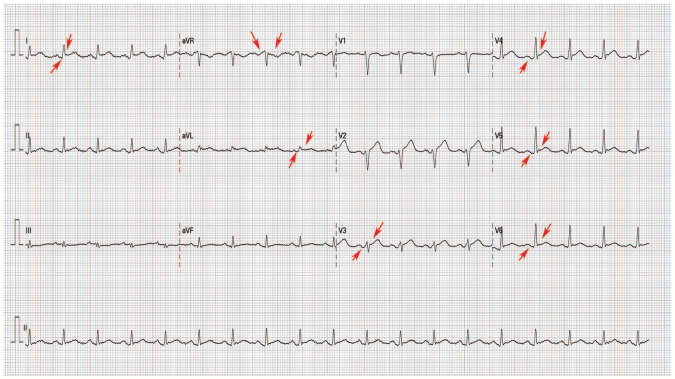
The electrocardiogram revealed sinus tachycardia, concave ST segment elevation with depressed PR segment in leads V3 to V6, DI, DII, aVL, and ST segment depression with PR segment elevation in lead aVR (Figure 1).
Figure 1.
Electrocardiogram on the patient’s presentation to emergency room. Noted sinus tachycardia with, concave ST segment elevation with depressed PR segment in leads V3 to V6, DI, DII, aVL, and ST segment depression with PR segment elevation in lead aVR.
Notable laboratory tests:
| C-reactive protein (CRP) | IL-6 | Erythrocyte sedimentation rate | Ferritin | LDH | Eosinophil count | Troponin I | NT-pro-B type natriuretic peptide |
|---|---|---|---|---|---|---|---|
| 122 mg/L (<3 mg/L) |
5.1 pg/mL (<4.4 pg/mL) | 13 mm (<12 mm) | 280 ng/mL (22-322 ng/mL) | 307 IU/L (120-246) | 0.1 × µL (0-0.49) | 1.27 ng/mL (<0.045 ng/mL) |
3169 pg/mL (<125 pg/mL) |
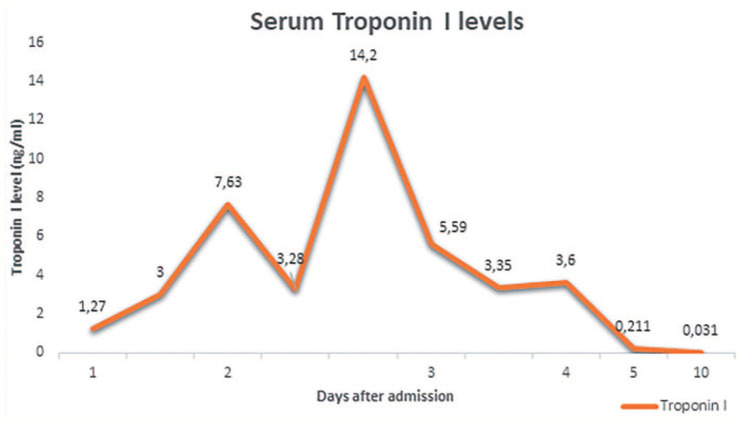
Transthoracic echocardiography showed slightly thickened ventricular walls and a left ventricular ejection fraction (LVEF) of 48% due to global hypokinesia. No pericardial effusion was observed (Figure 2).
Figure 2.
Transthoracic echocardiography (parasternal long-axis view) showed cardiac cavities of normal dimension and slightly thickened ventricular walls (with an 12 mm ventricular septum). No pericardial effusion was observed.
CT pulmonary angiography excluded pulmonary embolism, acute aortic syndrome, and pulmonary disease.
One gram of lysine acetylsalicylate was administered in the ER, which resulted in the resolution of the chest pain.
The patient was admitted in the Intensive Cardiac Care Unit with a presumed diagnosis of perimyocarditis.
Two PCR test for SARS-CoV-2, which were collected 3 days apart, were negative.
An autoantibody screen was negative.
A viral serology for hepatitis, HIV, Epstein-Barr virus, Cytomegalovirus, Parvovirus, Mycoplasma, Influenza A/B, Respiratory Syncytial Virus, Rhinovirus, Enterovirus (Coxsackie A, Coxsackie B), and Adenovirus were negative for acute or active infection.
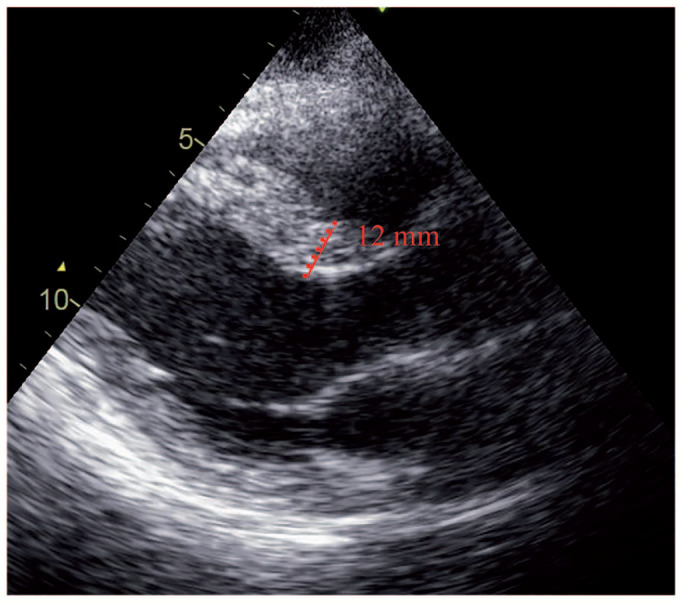
During hospitalization, the patient received anti-inflammatory treatment: 1 g of IV lysine acetylsalicylate every 8 hours and colchicine 0.5 mg every 12 hours. There were no recurrence of chest pain or fever and the CRP level normalized. Serum Troponin I peak level was 14.2 ng/mL (<0.045 ng/mL) with an initial oscillating profile which later decreased (Figure 3).
Figure 3.
Trends in cardiac troponin I levels. The peak level was 14.2 ng/mL. The cut off value was 0.045 ng/mL.
The patient was discharged and instructed to take ibuprofen 600 mg every 8 hours and colchicine 0.5 mg every 12 hours.
A cardiac MRI, that was performed 3 days after discharge, revealed a T2-hyperintensity foci and a late gadolinium enhancement (LGE) with subepicardial involvement of the left ventricle, which demonstrated the presence of myocardial edema/inflammation. The LVEF was normal. A minimum circumferential pericardial effusion was observed. Stress myocardial perfusion study showed no evidence of ischemia. These results and the medical history suggest the diagnosis of perimyocarditis which was considered to be a consequence of COVID-19 vaccination (Figure 4A and B).
Figure 4.
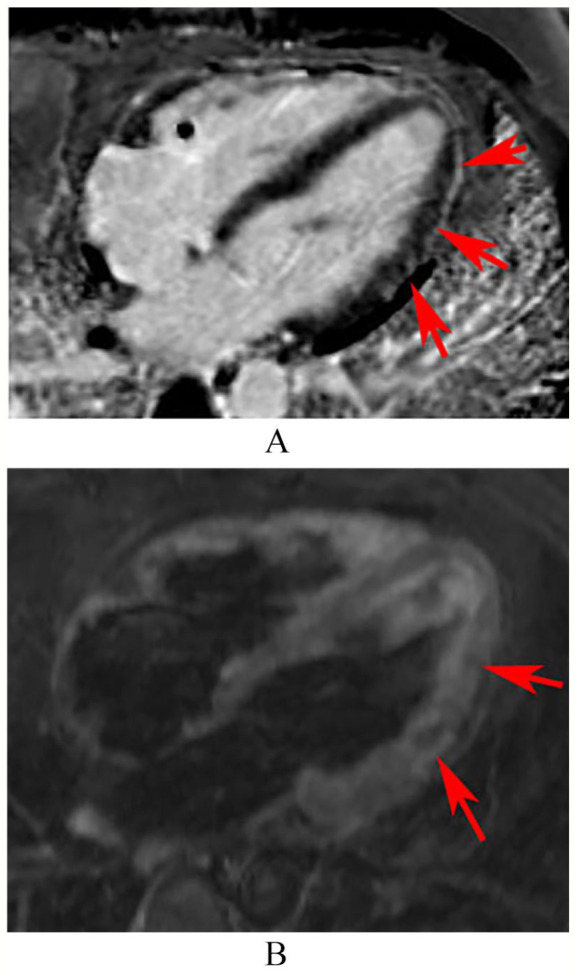
(A) Four-chamber view of late gadolinium enhancement image, (B) Four-chamber view of T2-weighted image. The image obtained after administration of intravenous gadolinium (A) showed multiple nodular foci of late gadolinium enhancement in subepicardial topography in the mid-distal segments of the anterolateral wall. These segments were hyperintense on T2-weighted image (B) which demonstrate the presence of myocardial edema/inflammation.
In a medical consultation performed after 10 days the patient had no symptoms.
Discussion
According to CDC, 3 myocarditis/pericarditis rates are approximately 12.6 cases per million doses of second dose mRNA vaccine (Pfizer-BioNTech or Moderna) among 12 to 39-year-olds.
Myocarditis following vaccination has been reported as a rare adverse event following vaccinations, especially smallpox vaccination, influenza and hepatitis B. 4
Recently, a CDC 3 Advisory Committee on Immunization Practices identified a “likely association” between the 2 COVID-19 mRNA vaccines and cases of myocarditis/pericarditis. Additional analyses of CDC Vaccine Safety Datalink revealed an increased risk of myocarditis/pericarditis events with mRNA COVID-19 vaccines compared with unvaccinated individuals or individuals vaccinated with non-mRNA COVID-19 vaccines on the same calendar days.
Myocarditis is increasingly recognized as a complication of COVID-19 and may result from direct viral injury or from exaggerated host immune response. 5 Mishra et al 6 quantified and reported cardiac findings in imaging of COVID-19 patients, including pericardial effusion, myocarditis, and cardiomegaly, most of them have been consistently reported in patients with significant acute myocardial injury. In a patient with myocarditis, biventricular myocardial interstitial edema, diffuse biventricular hypokinesia, increased ventricular wall thickness, and severe LV dysfunction has been reported. Myocarditis was the most common imaging diagnosis (~40%) on cardiac MRI in patients with COVID-19. 7
A number of myocarditis cases after COVID-19 vaccination have been published in peer reviewed journals. Patients in these reports invariably presented with chest pain, usually 2 to 3 days after a second dose of mRNA vaccination. These were predominantly young males requiring hospitalization and without prior history of COVID-19 or comorbidities. ECG was abnormal with ST segment elevation in most patients. Transthoracic echocardiography was abnormal only in 40%, with only a small percentage having an LVEF <50%. Cardiac MRI was abnormal in all tested patients. CRP levels were elevated in most and decreased along with troponin through hospital stay. Almost all patients had resolution of symptoms and signs and improvement in diagnostic markers and imaging. In Montgomery et al’s case series, 7 in 23 patients continued to have chest discomfort at the time of the report.3,8-11
The case presented here has most of the features found in other cases. Noninvasive techniques were used to rule out other diagnoses and indirectly recognize myocarditis. Given the negative PCR tests for COVID-19, as well as the negative viral serologies, and the temporal association between vaccination and the onset of symptoms, we suggest that this acute myocarditis was an adverse reaction to the Pfizer-BioNTech vaccine. Since our patient remained clinically stable and had a favorable response to therapy, he did not undergo endomyocardial biopsy.
Although the mechanisms for development of myocarditis are not clear, molecular mimicry between the spike protein of SARS-CoV-2 and self-antigens, trigger of pre-existing dysregulated immune pathways in certain individuals, immune response to mRNA and activation of immunological pathways, and dysregulated cytokine expression have been proposed. 11
Reports of death after COVID-19 vaccination are rare (0.0019%). 2 In the European Economic Area, there were 5 deaths due to myocarditis following COVID-19 vaccination. They were either of advanced age or had concomitant diseases. Available data suggest that the course of myocarditis/pericarditis following vaccination is similar to the typical course of these conditions. 12 Up to 7% of COVID-19–related deaths were attributable to myocarditis. 13
CDC 3 continues to recommend COVID-19 vaccination for everyone older than 12 years of age, given the greater risk of COVID-19 illness and related, possibly severe, complications. However, physicians should be aware of the possibility of cardiovascular complications after vaccination and be aimed to actively search for acute myocarditis when chest pain or discomfort is reported. Studies are needed to elucidate the incidence, risk factors, prognosis, potential mechanisms, clinical course, treatment strategies, and long-term impact of myocarditis following COVID-19 vaccination.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration Of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated context has been obtained from the patient in line with COPE guidance.
ORCID iD: Mariana Tinoco  https://orcid.org/0000-0001-8214-7193
https://orcid.org/0000-0001-8214-7193
References
- 1. WHO. Coronavirus (COVID-19) dashboard; 2021. Accessed August 1, 2021. https://covid19.who.int/
- 2. CDC. Selected adverse events reported after COVID-19 vaccination; 2021. Accessed August 1, 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/adverse-events.html
- 3. CDC. COVID-19 vaccine safety updates; 2021. Accessed August 1, 2021. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-06/03-COVID-Shimabukuro-508.pdf
- 4. Su JR, McNeil MM, Welsh KJ, et al. Myopericarditis after vaccination, Vaccine Adverse Event Reporting System (VAERS), 1990-2018. Vaccine. 2021;39:839-845. [DOI] [PubMed] [Google Scholar]
- 5. Agdamag ACC, Edmiston JB, Charpentier V, et al. Update on COVID-19 myocarditis. Medicina. 2020;56:678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mishra AK, Lal A, Sahu KK, Kranis M, Sargent J. Quantifying and reporting cardiac findings in imaging of COVID-19 patients. Monaldi Arch Chest Dis. 2020;90:627-632. [DOI] [PubMed] [Google Scholar]
- 7. Ojha V, Verma M, Pandey NN, et al. Cardiac magnetic resonance imaging in coronavirus disease 2019 (COVID-19): a systematic review of cardiac magnetic resonance imaging findings in 199 patients. J Thorac Imaging. 2021;36:73-83. [DOI] [PubMed] [Google Scholar]
- 8. Shaw KE, Cavalcante JL, Han BK, Gössl M. Possible association between COVID-19 vaccine and myocarditis: clinical and CMR findings. JACC Cardiovasc Imaging. 2021;14:1856-1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shaikh N, Friedlander EJ, Tate PJ, et al. Performance of a rapid SARS-CoV-2 antigen detection assay in symptomatic children. Pediatrics. 2021;148:e2021050832. [DOI] [PubMed] [Google Scholar]
- 10. Montgomery J, Ryan M, Engler R, et al. Myocarditis following immunization with mRNA COVID-19 vaccines in members of the US military. JAMA Cardiol. 2021;6:1202-1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bozkurt B, Kamat I, Hotez PJ. Myocarditis with COVID-19 mRNA vaccines. Circulation. 144:471-484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. EMA. COVID-19 vaccine safety update; 2021. Accessed August 1, 2021. https://www.ema.europa.eu/en/documents/covid-19-vaccine-safety-update/covid-19-vaccine-safety-update-comirnaty-14-july-2021_en.pdf
- 13. Driggin E, Madhavan MV, Bikdeli B, et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2352-2371. [DOI] [PMC free article] [PubMed] [Google Scholar]