Abstract
Background:
Elevated temperature is well-recognized as a health hazard, and may be particularly harmful to pregnant women, including increasing risk of stillbirth. We conducted a study in Northern and Central Florida, an area prone to periodic extreme heat but with significant seasonal variation, focusing on the most socioeconomically vulnerable populations least able to mitigate the impact of heat.
Methods:
We obtained electronic health records data from the OneFlorida Data Trust for the period 2012-2017, with 1,876 stillbirths included in the analysis. We used a case-crossover design to examine the risk of stillbirth associated with acute exposures to elevated heat prior to the outcome, contrasting the case period (the week preceding the stillbirth) with a control period (the week prior to the case period and the week after the stillbirth). Average heat index and maximum warning level during the case and control periods of each woman were assigned by ZIP code. Conditional logistic regression models were used to assess the association between stillbirth and heat exposure, controlling for PM2.5 and O3.
Results:
The adjusted odds ratio showed no overall association with stillbirth except for a weak association for exposure above the 90th percentile which was larger among the most socioeconomically deprived and non-Hispanic Black women. In the hot months, there was a clear association for all indices of heat exposure, but largest again for the most socioeconomically deprived population (aOR = 2.4, 95% CI: 1.2-5.2 in the 4th vs. 1st quartile) and among non-Hispanic Black women (aOR = 1.8, 95% CI: 1.0-3.2 in the 4th vs. 1st quartile).
Conclusions:
Our results provide further evidence that elevated ambient heat is related to stillbirth and encourage a focus on the most susceptible individuals and possible clinical pathways.
Keywords: Stillbirth, Ambient Heat
Introduction
Heat waves and elevated temperature more generally have long been associated with adverse health outcomes, most notably increased mortality among elderly and other vulnerable populations (Kovats and Hajat, 2008). Climate change exacerbates this threat to health, with the environmental and public health consequences calling for remedial action. It is important to determine the most sensitive health consequences of elevated temperature, particularly those that may be suitable for monitoring the impact of rising temperature on vulnerable populations and in order to target mitigation efforts optimally.
As for many environmental insults, pregnancy is a time of particular vulnerability, which may include elevated temperature. Discomfort from heat is a familiar symptom in late pregnancy and there is physiologic evidence that elevated core temperature is detrimental to pregnancy (Ravanelli et al., 2019). While there are not clear biologic pathways directly linking heat to stillbirth, there is indirect support for a possible effect from studies of maternal physiology and heat regulation during exercise (Laburn, 1996; Soultanakis-Aligianni, 2003) and harm to the pregnancy from dehydration which can result from heat stress (Stan et al., 2013). The health of the fetus and newborn is of profound personal and societal importance, and the loss of a fetus at an advanced stage of pregnancy (stillbirth) is among the most devastating experiences a mother and her family can suffer.
There is growing evidence that high temperatures may have an acute adverse impact on risk of stillbirth (Bekkar et al., 2020). Among the pregnancy outcomes that have been examined thus far in relation to temperature, it seems that the magnitude of association of elevated temperature is greatest for stillbirth. A focus on acute effects of heat allows for use of the case-crossover design, a highly effective means of eliminating confounding by individual risk factors such as socioeconomic status and medical conditions. Furthermore, the routine collection of high quality and comprehensive data on stillbirth in the US and many countries offers the possibility of using this endpoint for public health surveillance at a national and local level. To extend our understanding of the relationship between elevated temperature and stillbirth, we have conducted a study in Northern and Central Florida, an area that is prone to periodic extreme heat but with significant seasonal variation, considering multiple candidate indicators of heat and focusing in particular on the most socioeconomically vulnerable populations who may have home environments or occupations that are least able to mitigate the impact of heat.
Methods
Study population
We obtained electronic health records data from the OneFlorida Data Trust for the period 2012-2017. OneFlorida is a statewide clinical data research network in Florida and part of the National Patient Centered Clinical Research Network funded by the Patient-Centered Outcomes Research Institute (Shenkman et al., 2018). Through partnerships with 12 academic institutions and health systems, the OneFlorida Data Trust contains linked, longitudinal patient-level health record data for approximately 15 million Floridians across the state, over 60% of the state’s population. The OneFlorida data is a HIPAA-limited data set (i.e., dates are not shifted; and patients’ geocoded residential histories are available) and follows the National Patient Centered Clinical Research Network Common Data Model (Fleurence et al., 2014).
Women who had experienced stillbirths were identified from the OneFlorida Data Trust based on International Classification of Diseases-9 or 10 codes (ICD-9 code: V27.1, ICD-10 code: Z37.1). To differentiate encounters associated with separate stillbirths, we required ≥ 28 weeks between two separate stillbirths. The 28-week cut-point was selected since stillbirth is defined as fetal death after 20 weeks of pregnancy, with the 8-week interval which is widely used to differentiate separate pregnancy outcomes (Ailes et al., 2016). A total of 2,019 stillbirths among 1,985 women were identified. We excluded 64 stillbirths from 30 women with recurrent stillbirths (Lamont et al., 2015) and 79 stillbirths from women with missing ZIP Code information, leaving a total of 1,876 stillbirths were included in the final analyses. This study was approved by OneFlorida’s institutional review board at the University of Florida (IRB202003173).
Study design
We used a case-crossover design, where each case serves as her own control, to examine the risk of stillbirth associated with acute exposures to elevated heat prior to the outcome. Since the median time for stillborn delivery is around 1 day (Genest et al., 1992), we considered the period starting from one day preceding the delivery (lag day 1) through seven days preceding the delivery (lag day 7) as the window of interest. Similar to previous studies (Ha et al., 2017; Kanner et al., 2020; Rammah et al., 2019), to account for the changes in temperature over time, we used a symmetric bidirectional approach to define two control periods: one control period starting from 13 days after delivery through 7 days after delivery, and the other control period starting from 15 days preceding the delivery through 21 days preceding the delivery. While other time periods could be considered, we determined that correlations for varying intervals are quite high (Supplementary Figure 1) and there is not a clear biological basis for favoring one over another.
Exposure assessment
Daily estimates of average temperature and relative humidity with a 2.5 arc minute (~4km) spatial resolution were obtained from GRIDMET, a well-validated gridded surface meteorological dataset from University of Idaho (Abatzoglou, 2013). Area weighted averages were calculated to estimate daily average temperatures and relative humidity for each 5-digit ZIP Code tabulation area (ZCTA5) in Florida. We then calculated the mean daily heat index (or apparent temperature) for each ZCTA5 using the formula from the National Weather Service (Schmitt, 2004): Heat Index = − 42.379 + (2.04901523 × T) + (10.14333127 × rh) − (0.22475541 × T × rh) − (6.83783 × 10−3 × T2) − (5.481717 × 10−2 × rh2) + (1.22874 × 10−3 × T2 × rh) + (8.5282 × 10−4 × T × rh2) − (1.99 × 10−6 × T2 × rh2), where T is the daily average temperature (°F) and rh is the daily average relative humidity. Combining temperature and relative humidity more accurately reflects the physiological effects of heat than temperature alone. We further categorized the heat index based on different warnings assigned by the National Weather Service (Schmitt, 2004), including no warning (< 80°F / 26.7°C), caution (80°F-90°F / 26.7°C-32.2°C), and extreme caution (≥ 90°F / 32.2°C) to consider the applicability of these warnings to risk during pregnancy. We then spatiotemporally linked the heat index to each woman based on their ZIP Code to generate the average heat index and the maximum warning level during the case and control periods of each woman.
Covariates
Since the case-crossover design controls for all potential individual confounders (e.g., body mass index, tobacco use, socioeconomic status) by design, only time-varying confounders were considered. Since previous studies have linked ambient air pollution to stillbirth (Faiz et al., 2012), we included two criteria air pollutants, fine particulate matter (PM2.5) and ozone (O3), as potential confounders. We obtained data from the US Environmental Protection Agency and Centers for Disease Control and Prevention National Environmental Public Health Tracking Network (US EPA, 2016), which fuses daily PM2.5 and O3 data monitoring data from the National Air Monitoring Stations/State and Local Air Monitoring Stations with 12 km gridded output from the Models-3/Community Multiscale Air Quality model. Daily estimates were obtained at the Census Tract level and area-weighted averages were calculated to estimate daily PM2.5 and O3 levels for each ZCTA5 in Florida. Similar to the heat index, we assigned PM2.5 and O3 to each woman based on her residence, assessing exposure during the case (−1 to −7) days and control (−15 to −21 days and +7 to +13 days) periods.
To assess whether the association between heat and stillbirth varied across groups, we considered race/ethnicity (Non-Hispanic White, Non-Hispanic Black, Hispanics, and others) and neighborhood deprivation index (NDI) as potential effect modifiers. The NDI is derived from 20 US Census items reflecting wealth and income, education, occupation, and housing conditions as a summary measure (Messer et al., 2006). The NDI was linked to each woman using the 2013-2017 American Community Survey (ACS) data at the ZCTA5 level. A higher NDI indicates a greater degree of socioeconomic deprivation, i.e., a more deprived neighborhood. NDI was categorized into quartiles for analysis.
Statistical analysis
The distribution of maternal characteristics was examined. Average temperature and heat index were calculated for each month in Florida, and we then categorized each year into three periods based on the monthly average temperature and heat index: the hot period (heat index > 80°F / 26.7°C, June to September), the warm period (70°F-80°F / 21.1°C-26.7°C, April, May, and October), and the cool period (≤70°F / 26.7°C, November to March). Conditional logistic regression models were used to assess the association between stillbirth and average heat index and maximum warning levels in lag day 1 through lag day 7. Both unadjusted models and adjusted models controlling for PM2.5 and O3 were used, and odds ratios (ORs) and 95% confidence intervals (95% CIs) were reported. To examine whether the associations varied by season, we stratified the results into the three periods defined above. In addition, we also examined potential effect modification by race/ethnicity and NDI as an indicator of socioeconomic status. To consider a potential nonlinear association between stillbirth and average heat index, we used a natural spline to model potentially increased risks at low and high heat indices. All statistical analyses were conducted using R 3.6.1.
Results
The OneFlorida population that experienced stillbirth was of typical reproductive age and highly diverse in ethnicity (with nearly 60% Black or Hispanic) and geographic region (Table 1). The mean temperature by month (Table 2) reflects seasonal patterns, the generally hot summers (mean heat index of 85.1°F / 29.5°C, 88.3°F / 31.3°C, and 89.1°F/31.7°C in June, July, and August), and the rather sizable deviation between air temperature and heat index in the hot period.
Table 1.
Characteristics of women with stillbirths in OneFlorida, 2012-2017 (n=1,876).
| n (%) | |
|---|---|
| Age (years) | |
| <18 | 22 (1.2) |
| 18-24 | 467 (24.9) |
| 25-29 | 472 (25.2) |
| 30-34 | 492 (26.2) |
| 35-39 | 304 (16.2) |
| ≥40 | 119 (6.3) |
| Race/ethnicity | |
| Non-Hispanic White | 614 (32.7) |
| Non-Hispanic Black | 732 (39.0) |
| Hispanics | 368 (19.6) |
| Others | 109 (5.8) |
| Missing | 53 (2.8) |
| Region | |
| Northwest | 17 (0.9) |
| Northcentral | 346 (18.4) |
| Northeast | 336 (17.9) |
| Central | 1,048 (55.9) |
| Westcentral | 19 (1.0) |
| Eastcentral | 95 (5.1) |
| Southwest | 3 (0.2) |
| Southeast | 12 (0.6) |
Table 2.
Average temperature and heat index by month in Florida, 2012-2017.
| Temperature (Mean±SD) |
Heat Index (Mean±SD) |
|||
|---|---|---|---|---|
| °F | °C | °F | °C | |
| January | 60.7±9.4 | 15.9±5.2 | 60.7±9.4 | 15.9±5.2 |
| February | 63.3±8.6 | 17.4±4.8 | 63.3±8.6 | 17.4±4.8 |
| March | 67.3±8.0 | 19.6±4.5 | 67.3±8.0 | 19.6±4.5 |
| April | 73.3±5.2 | 23.0±2.9 | 73.6±5.6 | 23.1±3.1 |
| May | 77.1±4.5 | 25.1±2.5 | 78.2±5.8 | 25.7±3.2 |
| June | 81.0±2.6 | 27.2±1.5 | 85.1±5.6 | 29.5±3.1 |
| July | 82.4±2.3 | 28.0±1.3 | 88.3±5.4 | 31.3±3.0 |
| August | 82.6±2.2 | 28.1±1.2 | 89.1±5.4 | 31.7±3.0 |
| September | 80.5±2.8 | 27.0±1.6 | 84.4±5.9 | 29.1±3.3 |
| October | 75.1±6.2 | 23.9±3.4 | 76.2±7.6 | 24.5±4.2 |
| November | 67.7±8.1 | 19.8±4.5 | 67.8±8.4 | 19.9±4.7 |
| December | 65.9±8.9 | 18.8±4.9 | 65.9±8.9 | 18.8±4.9 |
The air pollution-adjusted odds ratio showed no overall association with stillbirth for the heat index measured continuously or across quartiles, a small association for exposure above the 90th percentile, and no association for the maximum heat risk level assignment (Table 3). While there was little support for effect-modification across quartiles of temperature or risk level assignment, there were clear differences found for exposure above the 90th percentile: In the most socioeconomically deprived group (with NDI in the 4th quartile), the adjusted odds ratio rose to 1.5 (95% CI: 0.9-2.4) and among non-Hispanic Black women it was 1.6 (95% CI: 1.0-2.4) (versus no increase among Hispanics and a lesser increase among non-Hispanic whites).
Table 3.
Associations between ambient heat and stillbirth in OneFlorida, 2012-2017 (n=1,876).
| Adjusteda OR (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Unstratified | Stratified by NDI | Stratified by Race/ethnicity | ||||
| NDI (Quartile 4) | NDI (Quartiles 1-3) | Non-Hispanic White | Non-Hispanic Black | Hispanics | ||
| n | 1,876 | 460 | 1,416 | 614 | 732 | 368 |
| Average Heat Index (Lag 1-7 day) | ||||||
| Continuous | ||||||
| Each 1°F increase | 1.00 (0.99, 1.01) | 1.00 (0.98, 1.03) | 1.00 (0.99, 1.02) | 1.00 (0.98, 1.02) | 1.01 (0.99, 1.02) | 1.01 (0.98, 1.04) |
| Each 1°C increase | 1.00 (0.98, 1.02) | 1.00 (0.97, 1.05) | 1.00 (0.98, 1.03) | 0.99 (0.96, 1.03) | 1.01 (0.98, 1.04) | 1.02 (0.97, 1.07) |
| Quartiles | ||||||
| Quartile 1 (≤66.0°F / 18.9°C) | Reference | Reference | Reference | Reference | Reference | Reference |
| Quartile 2 (66.0-74.3°F / 18.9-23.5°C) | 0.9 (0.7, 1.1) | 0.9 (0.6, 1.3) | 0.9 (0.7, 1.1) | 1.0 (0.7, 1.4) | 0.8 (0.6, 1.1) | 0.9 (0.6, 1.4) |
| Quartile 3 (74.3-83.9°F / 23.5-28.8°C) | 0.9 (0.7, 1.2) | 0.7 (0.4, 1.2) | 1.0 (0.7, 1.4) | 1.1 (0.7, 1.8) | 0.9 (0.6, 1.4) | 0.8 (0.4, 1.6) |
| Quartile 4 (>83.9°F / 28.8°C) | 0.8 (0.6, 1.1) | 0.5 (0.3, 1.0) | 0.9 (0.6, 1.4) | 0.8 (0.4, 1.4) | 0.8 (0.5, 1.5) | 0.8 (0.4, 1.9) |
| 90th Percentile | ||||||
| ≤90th Percentile (≤89.5°F / 31.9°C) | Reference | Reference | Reference | Reference | Reference | Reference |
| >90th Percentile (>89.5°F / 31.9°C) | 1.2 (0.9, 1.5) | 1.5 (0.9, 2.4) | 1.1 (0.8, 1.4) | 1.3 (0.9, 1.9) | 1.6 (1.0, 2.4) | 0.9 (0.6, 1.5) |
| Maximum Heat Index Risk Level (Lag 1-7 day) | ||||||
| No warning | Reference | Reference | Reference | Reference | Reference | Reference |
| Caution | 1.0 (0.8, 1.3) | 0.8 (0.5, 1.3) | 1.1 (0.9, 1.4) | 1.1 (0.7, 1.5) | 1.0 (0.7, 1.4) | 1.1 (0.6, 1.8) |
| ≥Extreme caution | 1.0 (0.8, 1.3) | 0.9 (0.5, 1.6) | 1.1 (0.8, 1.5) | 1.0 (0.6, 1.5) | 1.0 (0.6, 1.6) | 1.0 (0.5, 1.9) |
Adjusted for PM2.5 and O3.
Examining the patterns by season showed considerable differences across the hot, warm, and cool months (Table 4). In the hot months, there was a clear association of varying magnitude for all indices of heat exposure across all subsets of the population, but largest again for the most socioeconomically deprived population and among non-Hispanic Black women, and essentially absent for non-Hispanic white women. Interestingly, the associations were most modest for exposures at or above the 90th percentile and notably high for the uppermost quartile and in relation to the heat index risk level. In the warm months, the only notable association was in the analysis by quartiles with the lowest temperature quartile associated with the lowest risk and the upper three quartiles showing a similar magnitude of elevation. In the cool months, the results were essentially null. The models considering potential nonlinear effects (Figure 1 and Supplementary Figure 2) provided evidence consistent with a potential adverse effect concentrated in the upper end of the distribution.
Table 4.
Associations between ambient heat and stillbirth in different periods in OneFlorida, 2012-2017 (n=1,876).
| Adjusted OR (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Unstratified | Stratified by NDI | Stratified by Race/ethnicity | ||||
| NDI (Quartile 4) | NDI (Quartiles 1-3) | Non-Hispanic White | Non-Hispanic Black | Hispanics | ||
| Stillbirths in June to September | ||||||
| n | 646 | 154 | 492 | 223 | 241 | 125 |
| Average Heat Index (Lag 1-7 day) | ||||||
| Continuous | ||||||
| Each 1°F increase | 1.03 (1.00, 1.06) | 1.09 (1.03, 1.16) | 1.01 (0.98, 1.04) | 1.02 (0.97, 1.07) | 1.04 (1.00, 1.09) | 1.04 (0.97, 1.12) |
| Each 1°C increase | 1.05 (1.00, 1.10) | 1.17 (1.05, 1.31) | 1.02 (0.96, 1.08) | 1.03 (0.95, 1.12) | 1.08 (1.00, 1.17) | 1.08 (0.95, 1.22) |
| Quartiles | ||||||
| Quartile 1 (≤82.7°F / 28.2°C) | Reference | Reference | Reference | Reference | Reference | Reference |
| Quartile 2 (82.7-86.9°F / 28.2-30.5°C) | 1.2 (0.9, 1.6) | 0.8 (0.4, 1.5) | 1.4 (0.9, 1.9) | 1.0 (0.6, 1.6) | 1.4 (0.9, 2.3) | 1.7 (0.9, 3.4) |
| Quartile 3 (86.9-89.8°F / 30.5-32.1°C) | 1.1 (0.8, 1.5) | 1.9 (1.0, 3.9) | 0.9 (0.7, 1.4) | 1.0 (0.6, 1.7) | 1.1 (0.6, 1.8) | 1.3 (0.6, 2.7) |
| Quartile 4 (>89.8°F / 32.1°C) | 1.5 (1.0, 2.1) | 2.4 (1.2, 5.2) | 1.3 (0.8, 1.9) | 1.4 (0.8, 2.6) | 1.8 (1.0, 3.2) | 1.5 (0.7, 3.3) |
| 90th Percentile | ||||||
| ≤90th Percentile (≤91.5°F / 33.1°C) | Reference | Reference | Reference | Reference | Reference | Reference |
| >90th Percentile (>91.5°F / 33.1°C) | 1.2 (0.8, 1.6) | 2.0 (1.0, 3.9) | 1.0 (0.7, 1.4) | 0.9 (0.5, 1.7) | 1.2 (0.8, 2.0) | 1.2 (0.6, 2.4) |
| Maximum Heat Index Risk Level (Lag 1-7 day) | ||||||
| No warning | Reference | Reference | Reference | Reference | Reference | Reference |
| Caution | 1.6 (1.0, 2.7) | 1.2 (0.4, 3.2) | 1.8 (1.0, 3.2) | 1.1 (0.5, 2.2) | 3.6 (1.2, 10.6) | 1.7 (0.3, 8.3) |
| ≥Extreme caution | 1.6 (0.9, 2.7) | 1.6 (0.5, 4.6) | 1.6 (0.9, 2.9) | 1.2 (0.6, 2.6) | 3.4 (1.1, 10.7) | 1.3 (0.2, 7.1) |
| Stillbirths in April, May, and October | ||||||
| n | 473 | 117 | 356 | 162 | 179 | 88 |
| Average Heat Index (Lag 1-7 day) | ||||||
| Continuous | ||||||
| Each 1°F increase | 1.03 (1.00, 1.05) | 1.02 (0.96, 1.08) | 1.03 (1.00, 1.06) | 1.04 (1.00, 1.09) | 1.03 (0.98, 1.07) | 1.00 (0.94, 1.07) |
| Each 1°C increase | 1.05 (1.00, 1.10) | 1.03 (0.94, 1.14) | 1.05 (1.00, 1.11) | 1.08 (1.00, 1.17) | 1.05 (0.97, 1.13) | 1.00 (0.90, 1.12) |
| Quartiles | ||||||
| Quartile 1 (≤71.3°F / 21.8°C) | Reference | Reference | Reference | Reference | Reference | Reference |
| Quartile 2 (71.3-74.8°F / 21.8-23.8°C) | 2.1 (1.5, 2.9) | 2.1 (1.1, 4.2) | 2.0 (1.4, 3.0) | 2.3 (1.3, 4.1) | 1.7 (1.0, 2.8) | 2.1 (0.9, 4.8) |
| Quartile 3 (74.8-78.8°F / 23.8-26.0°C) | 1.8 (1.3, 2.7) | 1.2 (0.6, 2.3) | 2.1 (1.4, 3.2) | 1.9 (1.0, 3.6) | 2.0 (1.1, 3.6) | 1.5 (0.6, 3.8) |
| Quartile 4 (>78.8°F / 26.0°C) | 1.6 (1.1, 2.5) | 1.1 (0.5, 2.8) | 1.8 (1.1, 3.0) | 1.7 (0.8, 3.5) | 1.6 (0.8, 3.2) | 1.5 (0.6, 4.1) |
| 90th Percentile | ||||||
| ≤90th Percentile (≤82.0°F / 27.8°C) | Reference | Reference | Reference | Reference | Reference | Reference |
| >90th Percentile (>82.0°F / 27.8°C) | 0.6 (0.4, 1.0) | 0.7 (0.3, 1.5) | 0.6 (0.4, 1.1) | 0.5 (0.2, 1.2) | 0.8 (0.4, 1.7) | 0.4 (0.2, 1.1) |
| Maximum Heat Index Risk Level (Lag 1-7 day) | ||||||
| No warning | Reference | Reference | Reference | Reference | Reference | Reference |
| Caution | 1.2 (0.9, 1.6) | 0.8 (0.5, 1.5) | 1.4 (1.0, 1.9) | 1.4 (0.9, 2.2) | 1.0 (0.6, 1.6) | 1.3 (0.7, 2.4) |
| ≥Extreme caution | 0.9 (0.5, 1.7) | 0.4 (0.1, 1.8) | 1.2 (0.6, 2.4) | 0.5 (0.1, 1.8) | 0.9 (0.3, 2.4) | 1.5 (0.4, 5.7) |
| Stillbirths in November to March | ||||||
| n | 757 | 185 | 572 | 229 | 312 | 155 |
| Average Heat Index (Lag 1-7 day) | ||||||
| Continuous | ||||||
| Each 1°F increase | 0.99 (0.97, 1.01) | 0.99 (0.96, 1.02) | 0.99 (0.97, 1.01) | 0.98 (0.95, 1.01) | 0.99 (0.97, 1.02) | 1.00 (0.96, 1.04) |
| Each 1°C increase | 0.98 (0.95, 1.01) | 0.98 (0.92, 1.04) | 0.98 (0.94, 1.01) | 0.96 (0.91, 1.02) | 0.99 (0.94, 1.03) | 1.00 (0.93, 1.07) |
| Quartiles | ||||||
| Quartile 1 (≤58.2°F / 14.6°C) | Reference | Reference | Reference | Reference | Reference | Reference |
| Quartile 2 (58.2-63.9°F / 14.6-17.7°C) | 1.0 (0.8, 1.2) | 1.1 (0.6, 1.8) | 0.9 (0.7, 1.3) | 0.8 (0.5, 1.3) | 1.0 (0.7, 1.5) | 1.4 (0.8, 2.6) |
| Quartile 3 (63.9-68.7°F / 17.7-20.5°C) | 0.8 (0.6, 1.1) | 1.1 (0.6, 1.9) | 0.8 (0.6, 1.1) | 0.7 (0.4, 1.3) | 0.8 (0.5, 1.3) | 1.2 (0.6, 2.4) |
| Quartile 4 (>68.7°F / 20.5°C) | 0.7 (0.5, 1.0) | 0.7 (0.4, 1.4) | 0.7 (0.5, 1.1) | 0.6 (0.3, 1.1) | 0.8 (0.5, 1.3) | 1.4 (0.6, 2.9) |
| 90th Percentile | ||||||
| ≤90th Percentile (≤72.1°F / 22.3°C) | Reference | Reference | Reference | Reference | Reference | Reference |
| >90th Percentile (>72.1°F / 22.3°C) | 1.0 (0.7, 1.4) | 0.7 (0.3, 1.5) | 1.1 (0.8, 1.6) | 0.8 (0.4, 1.6) | 1.1 (0.6, 1.8) | 1.0 (0.5, 2.0) |
| Maximum Heat Index Risk Level (Lag 1-7 day) | ||||||
| No warning | Reference | Reference | Reference | Reference | Reference | Reference |
| Caution | 0.5 (0.3, 0.9) | 0.5 (0.1, 2.5) | 0.5 (0.2, 1.0) | 0.3 (0.1, 1.5) | 0.6 (0.2, 1.3) | 0.2 (0.1, 1.4) |
| ≥Extreme caution | - | - | - | - | - | - |
Adjusted for PM2.5 and O3.
Figure 1.
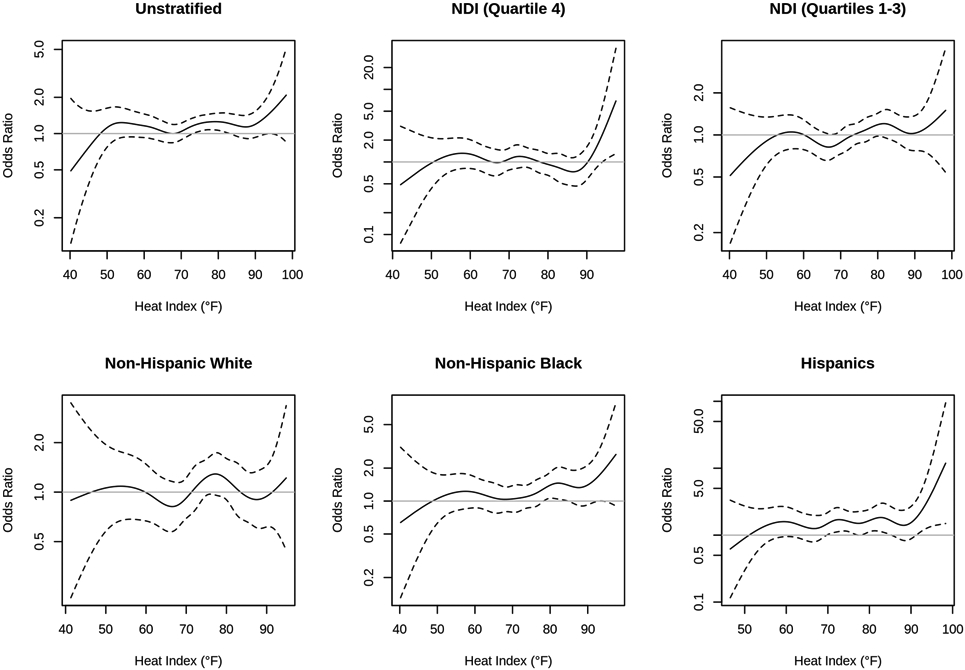
Natural spline models of temperature and stillbirth in relation to socioeconomic deprivation and ethnicity.
Discussion
While there was little support for an association between elevated temperature and stillbirth when aggregated across season and sociodemographic characteristics, there were distinctive indicators of a clear relationship concentrated in the hot season and among those in the most socioeconomically deprived neighborhoods. Both of these indicators of effect modification are consistent with a potential causal effect, given that temperature differences in the cool months are of little consequence relative to contrasts in the hotter periods of the year, and the reduced opportunity to mitigate hot temperatures among those of lower economic means would predict greater vulnerability.
Recent reviews of heat exposure and pregnancy outcome (Bekkar et al., 2020; Chersich et al., 2020) identified a pattern of association with multiple outcomes, including but not limited to stillbirth. An average across studies indicated an adjusted odds ratio of 1.05 (95% CI: 1.01, 1.08) per 1 degree Centigrade rise in temperature which was larger among women of lower socioeconomic status and at the extremes of age (Bekkar et al., 2020). In the short history of publications on this topic, beginning with Strand et al. (2012) only 10 years ago, multiple studies have reported associations between some measures of heat exposure and stillbirth (Auger et al., 2017; Basu et al., 2016; Ha et al., 2017; Kanner et al., 2020; Li et al., 2018; Rammah et al., 2019; Wang et al., 2019; Weng et al., 2018). The geographic locations vary widely including multiple locations in Australia, US, Canada, and Taiwan. It is difficult to compare the magnitudes of association since the exposure metrics themselves are quite variable and the time period of exposure differs across studies.
The replication of this finding has value, but there are diminishing returns from repeated replications of the basic pattern. Attention should turn now towards identifying time periods and population subgroups warranting preventive interventions. Although not universally assessed or found, multiple studies like ours point towards the warmer times of year (Basu et al., 2016; Ha et al., 2017; Rammah et al., 2019) and the most socioeconomically deprived (Basu et al., 2016) as particularly high risk. Risk by ethnicity among the US studies varied, with elevated risk for ethnic minorities in some (Rammah et al., 2019) but for all (Basu et al., 2016) prior studies. Overall, our results clearly indicated a stronger association for non-Hispanic black and Hispanic women. In essence, these subgroup findings point towards the pregnant women for whom intervention should be considered, whether in the form of providing resources to mitigate the effects of heat or behavioral guidance. Given that temperature over short periods is reasonably predictable and women at advanced stages of pregnancy have ongoing contact with health care providers through prenatal care, there is an opportunity to identify the high-risk population and time period if we can develop effective approaches to mitigation.
While our study had the advantages of a large population, an informative geographical setting prone to extreme heat, and a study design that controls for all individual and spatial determinant of risk, there are limitations. We were lacking medical detail to determine, for example, the gestational age at the time of the stillbirth which has been found to modify risk (Auger et al., 2017), or information on the causes of stillbirth which may well have varying susceptibility to adverse effects of heat. Since the mechanism by which heat might affect risk of stillbirth is not well understood, ideally we would focus on subsets of stillbirth that are most plausibly affected by ambient heat.
Conclusions
Our results provide further documentation of the statistical relationship between elevated ambient heat and stillbirth and encourage a closer look at which individuals are at particularly elevated risk and the clinical pathways through which this association may be causal.
Supplementary Material
Acknowledgments:
Research reported in this publication was supported in part by the OneFlorida Clinical Data Network, funded by the Patient-Centered Outcomes Research Institute numbers CDRN-1501-26692 and RI-CRN-2020-005; in part by the OneFlorida Cancer Control Alliance, funded by the Florida Department of Health’s James and Esther King Biomedical Research Program number 4KB16; and in part by the University of Florida Clinical and Translational Science Institute and its Clinical and Translational Science Award (CTSA) hub partner, Florida State University (FSU), which are supported in part by the National Center for Advancing Translational Sciences of the National Institutes of Health grant numbers UL1TR001427, KL2TR001429 and TL1TR001428. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology, the OneFlorida Clinical Research Consortium, the UF-FSU Clinical and Translational Science Institute, the Florida Department of Health, or the National Institutes of Health.
Abbreviations
- ACS
American Community Survey
- CI
Confidence Interval
- ICD-9
International Classification of Diseases-9
- ICD-10
International Classification of Diseases-10
- NDI
Neighborhood Deprivation Index
- O3
Ozone
- OR
Odds Ratio
- PM2.5
Fine Particulate Matter
- ZCTA5
5-digit ZIP Code Tabulation Area
Contributor Information
David A. Savitz, Department of Epidemiology, Brown University School of Public Health, Providence, Rhode Island, USA
Hui Hu, Department of Epidemiology, College of Public Health and Health Professions & College of Medicine, University of Florida, Gainesville, Florida, USA
References
- Abatzoglou JT, 2013. Development of gridded surface meteorological data for ecological applications and modelling. International Journal of Climatology. 33, 121–131. [Google Scholar]
- Ailes EC, et al. , 2016. Using insurance claims data to identify and estimate critical periods in pregnancy: an application to antidepressants. Birth Defects Research Part A: Clinical and Molecular Teratology. 106, 927–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auger N, et al. , 2017. Elevated outdoor temperatures and risk of stillbirth. International journal of epidemiology. 46, 200–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu R, et al. , 2016. Association between high ambient temperature and risk of stillbirth in California. American journal of epidemiology. 183, 894–901. [DOI] [PubMed] [Google Scholar]
- Bekkar B, et al. , 2020. Association of air pollution and heat exposure with preterm birth, low birth weight, and stillbirth in the US: a systematic review. JAMA network open. 3, e208243–e208243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chersich MF, et al. , 2020. Associations between high temperatures in pregnancy and risk of preterm birth, low birth weight, and stillbirths: systematic review and meta-analysis. bmj. 371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faiz AS, et al. , 2012. Ambient air pollution and the risk of stillbirth. American journal of epidemiology. 176, 308–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleurence RL, et al. , 2014. Launching PCORnet, a national patient-centered clinical research network. J Am Med Inform Assoc. 21, 578–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genest DR, et al. , 1992. Estimating the time of death in stillborn fetuses: I. Histologic evaluation of fetal organs; an autopsy study of 150 stillborns. Obstetrics and gynecology. 80, 575–584. [PubMed] [Google Scholar]
- Ha S, et al. , 2017. Ambient temperature and stillbirth: a multi-center retrospective cohort study. Environmental health perspectives. 125, 067011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanner J, et al. , 2020. Ambient temperature and stillbirth: Risks associated with chronic extreme temperature and acute temperature change. Environmental Research. 189, 109958. [DOI] [PubMed] [Google Scholar]
- Kovats RS, Hajat S, 2008. Heat stress and public health: a critical review. Annu. Rev. Public Health 29, 41–55. [DOI] [PubMed] [Google Scholar]
- Laburn HP, 1996. How does the fetus cope with thermal challenges? Physiology. 11, 96–100. [Google Scholar]
- Lamont K, et al. , 2015. Risk of recurrent stillbirth: systematic review and meta-analysis. bmj. 350. [DOI] [PubMed] [Google Scholar]
- Li S, et al. , 2018. Temporal change in the impacts of ambient temperature on preterm birth and stillbirth: Brisbane, 1994–2013. Science of the Total Environment. 634, 579–585. [DOI] [PubMed] [Google Scholar]
- Messer LC, et al. , 2006. The development of a standardized neighborhood deprivation index. Journal of Urban Health. 83, 1041–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rammah A, et al. , 2019. Temperature, placental abruption and stillbirth. Environment international. 131, 105067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravanelli N, et al. , 2019. Heat stress and fetal risk. Environmental limits for exercise and passive heat stress during pregnancy: a systematic review with best evidence synthesis. British journal of sports medicine. 53, 799–805. [DOI] [PubMed] [Google Scholar]
- Schmitt S, 2004. Heat Index Calculator. [Google Scholar]
- Shenkman E, et al. , 2018. OneFlorida Clinical Research Consortium: linking a clinical and translational science institute with a community-based distributive medical education model. Academic Medicine. 93, 451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soultanakis-Aligianni HN, 2003. Thermoregulation during exercise in pregnancy. Clinical obstetrics and gynecology. 46, 442–455. [DOI] [PubMed] [Google Scholar]
- Stan CM, et al. , 2013. Hydration for treatment of preterm labour. Cochrane Database of Systematic Reviews. [DOI] [PubMed] [Google Scholar]
- Strand LB, et al. , 2012. Maternal exposure to ambient temperature and the risks of preterm birth and stillbirth in Brisbane, Australia. American journal of epidemiology. 175, 99–107. [DOI] [PubMed] [Google Scholar]
- US EPA, Fused Air Quality Predictions Using Downscaling. 2016.
- Wang J, et al. , 2019. Exposure to heat wave during pregnancy and adverse birth outcomes: an exploration of susceptible windows. Epidemiology. 30, S115–S121. [DOI] [PubMed] [Google Scholar]
- Weng Y-H, et al. , 2018. Adverse neonatal outcomes in relation to ambient temperatures at birth: a nationwide survey in Taiwan. Archives of environmental & occupational health. 73, 48–55. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


