Abstract
There is growing evidence that transgender and gender diverse (TGD) persons are impacted by disparities across a variety of cardiovascular (CV) risk factors compared to their cisgender peers. Prior literature has characterized TGD disparities in cardiovascular morbidity and mortality as a result of minority stress and a higher prevalence of health risk behaviors. Mounting research has revealed CV risk factors at the individual level likely do not fully account for increased CV risk in TGD CV health disparities. Excess CV morbidity and mortality is hypothesized to be driven in part by psychosocial stressors across the lifespan, including structural violence (e.g., discrimination, affordable housing, access to health care, violence). This American Heart Association scientific statement reviews the extant literature on the CV health of TGD persons. When applicable, the effects of gender affirming hormone use on individual CV risk factors are also reviewed. Informed by a conceptual model building upon minority stress theory, the statement identifies research gaps and provides suggestions for improving CV research and clinical care for TGD persons, including the role of resilience promoting factors. Advancing the CV health of TGD persons requires a multi-faceted approach to integrate best practices into research, health promotion, and CV care of this understudied population.
Introduction
Transgender and gender diverse (TGD) populations comprise a large and growing population in the United States (US). Though estimates vary, approximately 2% of high school aged youth populations1 and 0.5–0.6% of adult populations2 in the US identify as TGD. As noted in the National Academies of Medicine Report on Sexual and Gender Minority (SGM) health, TGD persons face significant health disparities over the life course compared to their cisgender peers. Despite a heightened focus on the health of TGD populations in recent years, significant research gaps remain. In the fiscal year of 2018 (FY 2018), 19.8% of NIH funded sexual and gender minority (SGM) research projects included transgender populations, while 1.6% included gender diverse individuals (e.g., non-binary, gender non-conforming). The majority of these studies focused on HIV infection, mental health, and substance use; none had a focus on cardiovascular (CV) outcomes.
Yet, a growing body of research demonstrates that TGD populations may be at disproportionate risk for poor CV outcomes and risk factors, in addition to broad-ranging disparities.3 Within the Behavioral Risk Factor Surveillance System (BRFSS) dataset – one of two federal epidemiologic datasets that reports data on adult participants who identify as transgender – TGD individuals had a higher odds of CV events.4,5 The reasons for these disparities are multifaceted. To improve the health of TGD persons, more studies investigating not only CV risk factors but also mechanisms responsible for CV disparities are urgently needed. The objective of this scientific statement is to synthesize the literature describing CV health as well as emerging CV risk factors and outcomes among TGD populations using a theory-informed approach. The statement uses Life’s Simple 7 to describe traditional CV risk factors that shape CV health,16 and explores evidence on emerging CV risk factors thought to impact the CV health of TGD populations. The final section focuses on modifiable factors that can strengthen resilience promoting factors to improve CV health equity for TGD populations.
Moving Beyond Minority Stress Theory: An Expanded Conceptual Model of TGD
Cardiovascular Health
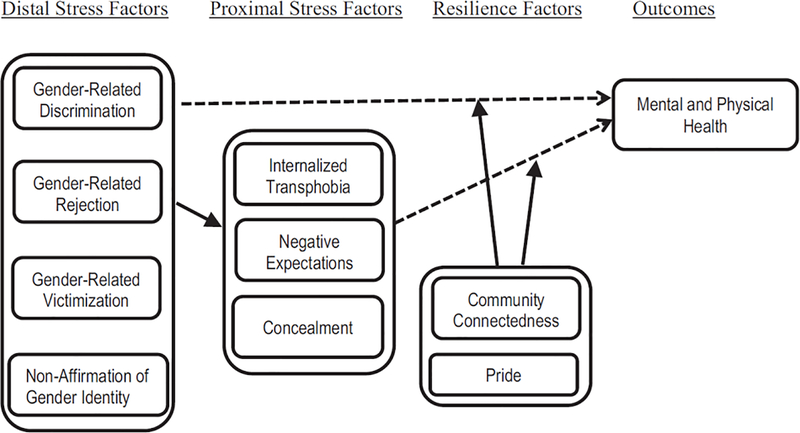
Minority Stress Theory (MST) has historically served as the leading theory to explain broad-ranging TGD health disparities. The Gender Minority Stress and Resilience Model (Figure 1) depicts how distal and proximal minority stressors experienced by TGD people contribute to TGD health disparities.6,7 Distal stressors include gender non-affirmation (e.g., being called by incorrect pronoun or name) and discrimination, rejection, and victimization based on gender identity. Proximal stressor include internalized transphobia, negative expectations, hypervigilance, and concealment of gender identity.1 Taken together, distal and proximal minority stressors are hypothesized to contribute to higher overall stress levels, which in turn reshape CV health behaviors as well as increase the likelihood of broad-ranging poor mental and physical health outcomes, including cardiovascular disease (CVD).
Figure 1.
Gender minority stress and resilience model. Minority stress and resilience factors in people who are transgender and gender diverse. Dashed line indicates inverse relationships. Copyright © 2015 by American Psychological Association. Reproduced with permission from Testa et al.14
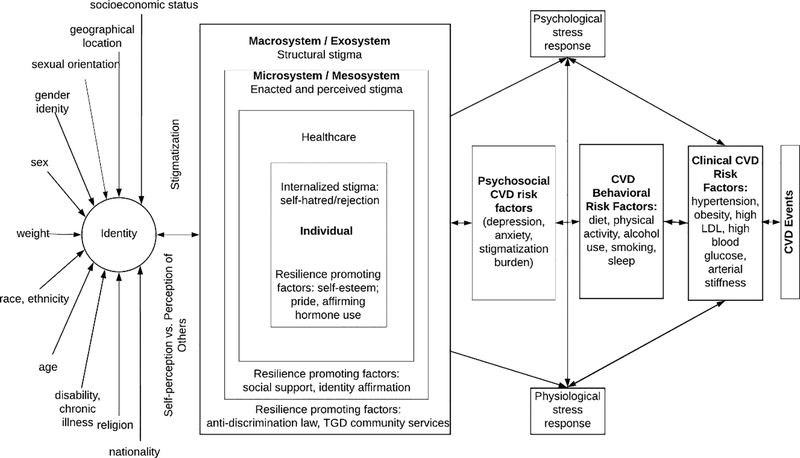
In recent times, MST has been critiqued for not adequately capturing the effects of stigmatization at the intersections of multiple marginalized identities, structural level factors, or resilience promoting factors on the health of TGD populations. Building from MST, Figure 2 therefore presents an expanded conceptual model. The model depicts how stigmatization at the intersections of multiple marginalized identities and multilevel social determinants of health contribute to higher general and minority stressors impacting TGD CV health. Further, the model depicts how resilience promoting factors at the individual, interpersonal, and structural levels can counteract the effects of transphobic violence and stigma to promote TGD health equity.
Figure 2.
The Intersectional Transgender Multilevel Minority Stress model reframes and expands the scope of minority stress theory to include an explicit intersectional lens and to clarify the role of multilevel socioecological factors on the health of TGD populations. In brief, marginalization on the basis of intersecting socialized identities is depicted as leading to a degree of stigmatization in relation to social power systems. Stigma-related stressors are depicted dynamically in relation to resilience promoting factors, which are theorized to combat the harmful effects of stigma and thereby offer potential points for future multilevel health equity promotion interventions. When stigmatization rather than resilience is the dominant effect in the model, the resulting net effect of intersectional stigmatization contributes to poor population health via 1) psychological distress, 2) CVD behavioral risk factors, and 3) physiological response to chronic stress. These pathways independently contribute to clinical CVD risk factors and outcomes. They also add to the higher chronic stress burden associated with the development of clinical CVD risk factors and ultimately CVD and CVD disparities among marginalized populations, including TGD persons.
A growing body of empirical research has demonstrated the harmful impact of minority stress on CVD among several minority groups including racial and ethnic minority adults,8,9 and sexual minority adolescents.10 Research has been limited on the relationships between minority stressors and CVD for TGD populations.11 However, it is reasonable to expect that similar mechanisms linking minority stress and resilience promoting factors to CV health in other populations apply to TGD people.
Cardiovascular Risk Factors for Transgender and Gender Diverse Persons
Tobacco Use
Tobacco use is a known risk factor for CVD. The prevalence of tobacco use among TGD populations has been evaluated in several studies with conflicting results, in part due to different sampling techniques, methods to measure tobacco use, and identification of TGD persons. The U.S. Trans Survey, a non-probability survey conducted with 28,000 TGD persons, found 23.6% of respondents currently smoked cigarettes,12 a rate higher than the US population (17.6%). These results suggest that the increased prevalence of tobacco use in TGD populations is likely related to underlying differences in baseline characteristics. However, analyses of data from the 2014 and 2016 BRFSS as well as the Population Assessment of Tobacco and Health (PATH) study did not demonstrate a higher prevalence of current or former cigarette smoking in transgender persons.13
Utilizing MST, analyses of the U.S. Trans Survey revealed that experiencing discrimination accounted for significantly higher odds of cigarette smoking and dual cigarette use (i.e., using both cigarettes and vaping). Further, participants who believed they were visually gender non-conforming had greater odds of cigarette smoking, vaping, and dual use than those who reported they were visually conforming.12
Physical activity
The measurement of physical activity levels in TGD persons is an understudied area. Survey data suggests that TGD adolescents are less likely to participate in regular physical activity, physical education classes, school athletics or extracurricular activities.14 The lack of participation in physical activity has been attributed to a tendency to feel unsafe or uncomfortable in school environments, especially those segregated by gender.14 Similarly, TGD adults report participating in less physical activity than cisgender adults.4,15 Data from the 2014–2016 BRFSS report that transgender men have a higher odds of reporting no exercise compared with cisgender men and women even after adjusting for socioeconomic factors and state.4 Further, research has found that 23% of TGD older adults reported low physical activity levels.15 Notably, TGD adults taking gender affirming hormone therapy are more likely to be engaged in physical activity than those who are not, and the best predictor of participating in physical activity is high body satisfaction.16
Diet/Nutrition
While caloric intake, nutritional value, and access to adequate nutrition are modifiable factors in CV health, there is limited research on diet quality in TGD persons across the lifespan. Survey data of TGD adolescents found less frequent intake of fruit and milk and more frequent intake of fast food and soft drinks than cisgender peers.14 In addition to inadequate nutrition, TGD adolescents disproportionately self-report unsafe weight management behaviors (i.e., fasting, diet pill use, laxative abuse) compared to cisgender peers.17 While caloric intake, nutritional value, and access to adequate nutrition are modifiable factors in CVH, there is limited research on diet quality in TGD persons across the lifespan. Survey data of TGD adolescents found less frequent intake of fruit and milk and more frequent intake of fast food and soft drinks than cisgender peers.14 In addition to inadequate nutrition, TGD adolescents are more likely to report disordered eating behaviors (i.e., fasting, diet pill use, laxative abuse) and be diagnosed with an eating disorder when compared to cisgender peers.17
Weight Management
BRFSS data reveal a significantly higher prevalence of self-reported Body Mass Index (BMI) greater than 25kg/m2 among TGD persons compared to cisgender adults (72.4% vs 65.5%). Few studies have investigated BMI among TGD populations. A growing number of studies have investigated changes in BMI among TGD populations prescribed gender affirming hormone therapy. A systematic review evaluating the effects of testosterone use on BMI in transgender men revealed significant increases (1.3–11.4%) in BMI.18 However, a U.S. longitudinal study investigating BMI changes over seven years did not demonstrate an increase in BMI among transgender men.19 In adolescents, the use of testosterone shows similarly contradictory results.20–22 Among transgender women taking estrogen, European studies report increases in BMI,22–24 waist circumference, and weight.24 U.S. studies have not demonstrated an increase in BMI.20,21
Lipid Profile
An analysis of 2014–2017 BRFSS found no differences in self-reported hypercholesterolemia between TGD and cisgender adults.5 An observational study of TGD youth assigned male at birth recruited prior to any hormonal intervention found no differences in total or LDL cholesterol compared to an NHANES comparison group but reported lower levels of HDL cholesterol in TGD youth independent of BMI, race, or socioeconomic status. An analysis of 2014–2017 BRFSS found no differences in self-reported hypercholesterolemia between TGD and cisgender adults. An observational study of TGD youth assigned male at birth recruited prior to any hormonal intervention found no differences in total or LDL cholesterol. However, lower levels of HDL cholesterol were detected, independent of BMI, race, or socioeconomic status between TGD youth and an NHANES comparison group.25 Studies conducted among TGD persons taking hormone therapy have revealed that - as seen in cisgender persons - hormone therapy affects the lipid profiles of TGD persons.26 Cross-sectional comparisons of transgender youth receiving hormone therapy compared to cisgender controls showed that adolescent transgender men had lower HDL cholesterol compared to matched adolescent cisgender women, whereas adolescent transgender women had higher HDL cholesterol than adolescent cisgender men;26 no differences in total or LDL cholesterol or triglycerides were noted.27 Cross-sectional comparisons of transgender youth receiving hormone therapy compared to cisgender controls showed that adolescent transgender men had lower HDL cholesterol compared to matched adolescent cisgender women, whereas adolescent transgender women had higher HDL cholesterol than adolescent cisgender men;26 no differences in total or LDL cholesterol or triglycerides were noted.26
Among transgender adult men, testosterone therapy has been consistently associated with decreased HDL cholesterol ranging from 3.4% to 23.4% and increased triglycerides ranging from 17.5% to 44%,28–30 with some studies also noting increases in total and/or LDL cholesterol ranging from 3.6% and 18.7%.30,31 Importantly, the lipid and lipoprotein levels following testosterone therapy were still in the desirable range.
Among transgender women, the effects of estrogen therapy on lipid profiles are discrepant with favorable, unfavorable, and no changes being reported. In sensitivity analyses, larger decreases in lipids were observed in transgender women aged 30–45 years that were receiving transdermal estradiol plus daily cypionate acetate (CPA) compared to their age-matched peers receiving oral estradiol plus CPA.32 In contrast to the reported favorable effects of estrogen therapy on lipids, two separate meta-analysis, showed estrogen therapy was associated with an increase in triglycerides without significant changes in total cholesterol or other lipoprotein fractions.33 It is speculated that the increase in triglycerides was driven by the use of oral estrogens, as sensitivity analyses showed an increase in triglycerides of 28.2 mg/dL (95% CI: 0.5 to 55.9 mg/dL; I2 = 0%) with oral estradiol compared with a decrease of 4.8 mg/dL (95% CI: −21.2 to 11.6 mg/dL; I2 = 0%) with transdermal estradiol.33 The differential effects between oral and transdermal estradiol on triglycerides is a phenomenon that has been previously reported in postmenopausal cisgender women.34 Collectively, there does not appear to be adverse effects of estrogen therapy on blood lipids and lipoproteins in transgender women, with the exception of possible increases in triglycerides and decreases in HDL cholesterol depending on the type of anti-androgen co-administered with estradiol.
In summary, changes across lipid profiles in TGD persons due to gender-affirming hormone therapy are measurably small and of unknown, if any, clinical significance. Future studies should focus on analyzing the effect of hormone therapy among older TGD persons.
Glycemic Status
Few studies have evaluated the prevalence of diabetes in TGD persons. In the 2014 and 2015 BRFSS, no difference in the prevalence of self-reported diabetes between transgender and cisgender adults was detected.35 However, a study from the Netherlands found that transgender men and women had a higher prevalence of diabetes compared to cisgender persons, both before and after using hormone therapy.36 A systemic review assessing the effect of testosterone on insulin resistance found overall no apparent negative effect of testosterone on insulin resistance, with only 2 out of 13 studies showing increased insulin resistance, whereas the majority showed no effects (10 studies), and 1 study showing improvements in insulin sensitivity. For transgender women receiving estrogen, 5 of 8 studies showed increased insulin resistance, whereas 3 found no effect.37 Another study showed that insulin sensitivity and post-OGTT incretin responses decreased with estrogen treatment.38 Overall, research exploring gender affirming hormone therapy effects on the acquisition of diabetes mellitus provides contradictory results and points to the need for more research utilizing longitudinal data.
Blood Pressure
Evidence of elevated blood pressure in TGD populations is limited. Most research on hypertension in TGD adults has focused on the impact of hormone therapy on BP. Multiple systematic reviews indicate findings are inconclusive with studies reporting small but not clinically significant elevations in systolic BP among transgender men.27,39 Similarly, a recent retrospective cohort study that examined electronic health records of transgender men and women (N = 4,402) found no significant associations between hormone use and hypertension among transgender men. Among transgender women, a higher blood concentration of testosterone was associated with higher odds of having hypertension. In addition, investigators found that transgender women who had received a progestin prescription had lower odds of having hypertension.40 To date, there has been limited investigation of potential social determinants of hypertension in this population. This is an important area for future research in TGD persons.
Additional Risk Factors and Considerations
HIV
Rates of CVD are significantly higher for persons living with HIV.41 This elevated CVD risk persists even after achieving sustained viral suppression with effective antiretroviral therapy.41 This risk is particularly relevant for TGD adults who experience a disproportionate burden of HIV. The most recent laboratory-confirmed HIV prevalence estimates indicate that 14% of transgender women and 2% of transgender men are living with HIV, respectively.42 Racial disparities among transgender women are marked, with 44% of Black transgender women and 25% of Latina transgender women living with HIV, respectively.42 Disaggregated data on TGD persons living with HIV are limited. However, existing research suggests that TGD persons living with HIV may be at even higher risk for cardiovascular disease than cisgender people with HIV.43
Vascular health & function
Vascular dysfunction, featuring endothelial dysfunction and large elastic artery stiffening, is a key antecedent in the development of CVD and are independent predictors of CV events.44 Psychological and physiological stress responses are associated with large artery stiffening and endothelial dysfunction, and vascular dysfunction is a central feature of psychosocial and behavioral CVD risk factors, in addition to traditional clinical CVD risk factors (see Figure 2).45 However, to our knowledge there are no data on generalized data with regards to vascular dysfunction in TGD persons independent of studying the effects of sex hormone treatment. While estrogen and testosterone treatment generally are associated with enhanced endothelial function and reduced large elastic artery stiffness (or increased arterial compliance) in cisgender adults,46–48 limited data are available regarding vascular function in TGD adults and none exists in TGD youth.
Cross-sectional comparisons between transgender men receiving testosterone cypionate compared with age-matched cisgender women found reduced endothelial function measured via brachial artery flow-mediated dilation (FMD).49 In a cross-sectional study, arterial stiffness, measured via brachial-ankle pulse wave velocity (baPWV) and carotid augmentation index (AI), showed higher baPWV (i.e., greater stiffening) in transgender men receiving testosterone compared with transgender men not receiving hormone therapy.31 Because there were no differences in carotid AI, a measure of large elastic artery stiffness, the significance of a higher baPWV, a measure of muscular artery stiffness, is unclear.
In contrast to data in transgender men, endothelial function has been reported to be enhanced and arterial stiffness decreased in transgender women receiving hormone therapy.50,51 Brachial artery FMD was higher in transgender women treated with estrogen compared with age-matched cisgender men, but was similar to cisgender women.52 In the only study that we are aware of that examined endothelial function at the microvascular (i.e., resistance vessel) level, transgender women aged 30–60 years receiving estrogen had a greater forearm blood flow response to acetylcholine, an endothelial-dependent vasodilator, than age-matched cisgender men.50
Further, TGD persons who had undergone gender affirming surgery and were receiving hormone therapy had reduced brachial artery FMD compared with transgender women and men who had not undergone surgery but who were taking hormone therapy.53 In secondary analyses, the results remained the same when separating by gender. However, the sample sizes in the surgery group likely lacked the power to detect differences.53
Sleep
Inadequate sleep duration and poor sleep quality have been identified as risk factors for incident hypertension, diabetes, and CVD.45 A recent review of sleep among sexual and gender minority (SGM) populations found that only four studies had been conducted that examined sleep health among TGD adults.54 A qualitative study of 40 TGD adults living in New York City found that more than 35% of participants attributed sleep problems to gender identity concerns.55 Additionally, a study of TGD adults found that internalized transphobia and sexual victimization were positively associated with sleep disturbances, whereas resilience promoting factors (i.e., community connectedness) were negatively associated with sleep disturbances.56 The study of sleep in TGD adults is an emerging area of research that warrants further investigation.
Alcohol
While TGD alcohol use studies are scarce, a 2018 systematic review found methodological weaknesses and limited measurement of alcohol use outcomes.57 Notably, data from the 2017 Youth Risk Behavior Surveillance System show that transgender youth were more likely than cisgender youth to report lifetime alcohol use.1 Additional research reports elevated patterns of alcohol use for TGD vs. cisgender youth,58 as well as a clear association between past-year experiences of bullying and alcohol use for TGD youth.59 Further, research in TGD adults has demonstrated elevated levels of alcohol use compared to the general population, including distinct patterns of use based on gender identity,60 sex assigned at birth,61 and sexual orientation. Elevated rates of drinking in TGD persons has been consistently linked to victimization and minority stress.62,63
Limitations of Existing Research
Lack and Limitation of Existing Data
The current lack of standardized gender identity data across various sources limit our examination of the prevalence, incidence, and disparities in CV health among TGD populations. Existing population-based surveys rely on self-report of CV outcomes, which lack clinical factors relevant to current measures of CV health. Existing longitudinal studies of CV health do not collect gender identity data, thereby invisibilizing TGD individuals and limiting the opportunity to report objective measures of CV health. Analysis of claims-based datasets erases the possibility of examination of CV health across gender identities beyond the binary categories of man/woman and transgender man/woman.64 Electronic health records (EHRs) that appropriately collect gender identity data often lack complete clinical data and do not allow for generalizability of health outcome results beyond the health system examined.65 Additionally, it is important to recognize EHR data exclude transgender persons who are not engaged in healthcare or who feel uncomfortable disclosing their gender identity to clinicians. In addition, many EHR systems lack the ability to capture sociocultural factors relevant to understanding CV health. Overall, however, EHR data represent an advance in the absence of other sources of objective measures of CV health.
Testing of Mechanisms
There is a lack of understanding about mechanisms that link TGD-specific stressors to CV health. Despite increased CVD risk, no evidence-based interventions for CVD risk reduction specific to TGD persons currently exist. Longitudinal research is needed to better characterize pathways from distal and proximal stressors to CV outcomes and to identify psychosocial and behavioral targets for interventions to improve the CV health of TGD persons over the life-course (Figure 2).
Additionally, qualitative research is needed to understand how cultural and neighborhood level contextual factors influence the health of diverse TGD sub-populations. Increasing knowledge about group-specific attitudes and beliefs regarding health behaviors is needed to enhance the acceptability of interventions designed to improve the CV health of transgender persons. These interventions should account for the influence of interpersonal and structural drivers of CV health in TGD persons.
Social and Clinical Determinants of Cardiovascular Health
How social determinants of health and minority stress influence CVD risk factors and outcomes has been well characterized among marginalized racial and ethnic populations.66 However, qualitative and quantitative research studies exploring how these pathways influence CV health among TGD persons are only now being conducted. Empirical studies have found that stigmatization of TGD persons vary by other intersectional stigmatized and marginalized characteristics (e.g., race, class). However, limited research has examined social determinants of CV health among TGD persons.
Additionally, there is evidence that gender-affirming hormones reduce psychosocial and behavioral risk factors in TGD persons. Therefore, the potential CV effects of gender-affirming hormone therapy should be evaluated against the benefits for mental health, health behaviors, and downstream physiological health effects (Figure 2).
Suggestions for Research and Clinical Practice Research
Primary prevention of CVD relies on the accuracy of prediction models and the data utilized to create them. However, current prediction models (e.g., Pooled Cohort Risk Assessment Equation) are limited due to prior research utilizing binary categories of “male” and “female” that exclude transgender persons. While population-based studies have provided a greater understanding of the CV health of TGD persons, the data on relevant social and clinical determinants for TGD persons remain scarce. Only three CV cohorts currently have plans to collect gender identity data. Current and future NIH-funded CV cohort studies should include standardized measures of gender identity and expression that will permit data harmonization to achieve larger samples of understudied groups within TGD populations.65
Several steps should be taken to increase TGD persons’ trust of the research community. The critical mantra in doing any research focused on minoritized and marginalized populations should be “nothing about us without us.” Consequently, research teams conducting TGD research should reflect the diversity that exists within the population. Researchers should also partner with TGD communities during all stages of the scientific process to increase trust in research and ensure research agendas are informed by and aligned with community needs.
Clinical Training and Care
Many institutions acknowledge the paucity of education in TGD health. Yet, efforts to instill these topics into curricula has been subsumed by the larger topic of SGM health inequity.67 While broader SGM content is needed, a curriculum that specifically encompasses the unique issues that affect TGD persons can improve TGD-specific care: gender-affirming hormone therapy and surgical procedures, and anatomy-based preventive health.68 A collaborative effort with organizational-level mandates across governing bodies to improve clinical competencies and didactic education during training across the health professions and specialties would serve to enhance effective clinical practice and compassionate care for TGD persons.
Critical to improving TGD health and access to appropriate health care is creating welcoming and compassionate spaces and clinical care teams. Health care institutions and organizations must commit to this goal and measure their success using national benchmarking tools that evaluate healthcare institutional policies and practices to achieve equity and inclusion.
Since 2018, recording of sexual orientation and gender identity data has been required as one of the EHR meaningful use criteria, but culturally responsive care requires additional steps to ensure appropriate collection and use of such data. In addition to recording affirmed name and pronouns it is critical that clinicians obtain an anatomy inventory when appropriate. Such errors in classifications and assumptions about anatomy based on ones identified gender may lead to poor clinical decision making in diagnosis and treatment of CVD. Therefore, all providers trained in CV health must understand such issues. Additionally, health systems and clinicians must advocate to uphold and create new policies at the local, state, and federal levels that promote access.
Conclusion
TGD persons experience significant stressors that affect CV health across the lifespan. In addition to disparities across traditional risk factors for CVD, TGD persons experience disparities across factors associated with CV health and CVD. Further, the use of gender affirming hormone therapy may be associated with cardiometabolic changes, but the field of CV health research in TGD persons remains limited. To address knowledge gaps in the literature, longitudinal research that examines mechanisms that link social and clinical determinants with CV health in TGD persons is needed across the lifespan. TGD health content must be incorporated in health professions training, accreditation, and licensure requirements. There are opportunities for research, clinical, and public health efforts to better understand and reduce CV health disparities among TGD persons.
Table 1.
Glossary of Terms for Transgender Health
| Cisgender | A term used to describe people whose gender identity is congruent with what is traditionally expected based on their sex assigned at birth. |
| Gender diverse | |
| Gender expression | The ways in which a person communicates femininity, masculinity, androgyny, or other aspects of gender, often through speech, mannerisms, gait, or style of dress. Everyone has ways in which they express their gender. |
| Gender identity | A person’s inner sense of being a girl/woman, a boy/man, a combination of girl/woman and boy/man, something else, or having no gender at all. Everyone has a gender identity. |
| Gender minority | A broad diversity of people who experience an incongruence between their gender identity and what is traditionally expected based on their sex assigned at birth, such as transgender and gender diverse persons. |
| Gender non-binary | A term used by some people who identify as a combination of girl/woman and boy/man, as something else, or as having no gender. Often used interchangeably with “gender non-conforming.” |
| Gender non-conforming | A term used by some people who identify as a combination of girl/woman and boy/man, as something else, or as having no gender. Often used interchangeably with “gender non-binary.” |
| Queer | Historically a derogatory term used against LGBTQ people, it has been embraced and reclaimed by LGBTQ communities. Queer is often used to represent all individuals who identify outside of other categories of sexual and gender identity. Queer may also be used by an individual who feels as though other sexual or gender identity labels do not adequately describe their experience. |
| Sex assigned at birth | Usually based on phenotypic presentation (i.e., genitals) of an infant and categorized as female or male; distinct from gender identity. |
| Sex | Biological sex characteristics (chromosomes, gonads, sex hormones, and/or genitals); male, female, intersex. Synonymous with “sex assigned at birth.” |
| Transgender man | Someone who identifies as male but was assigned female sex at birth. |
| Transgender woman | Someone who identifies as female but was assigned male sex at birth. |
Table 2.
Suggestions for Research and Clinical Practice with Transgender Persons
| Cardiovascular Research | Clinical Practice |
|---|---|
|
| |
| • Develop standardized sexual orientation and gender identity measures and integrate these in current and future NIH-funded cardiovascular prospective cohort studies to allow for data harmonization • Integrate biobehavioral measures into cardiovascular research with transgender populations • Interrogate research methods and choose measures that avoid perpetuating discrimination (e.g., reevaluate the use of BMI as a measure of body composition) • Leverage electronic health record data to increase understanding of transgender cardiovascular health |
• Ensure collection of sexual orientation and gender identity data in electronic health records through providing clinicians with training on transgender health disparities and the proper assessment of sexual orientation and gender identity in healthcare settings • Incorporate transgender content in the curricula of health professions schools and post-graduate training • Require continuing education on transgender health for all practicing clinicians that includes content on cardiovascular health disparities |
| • Partner with transgender communities for measurement development, study design and conduct, and research dissemination to ensure research reflects the needs of transgender persons, especially stigmatized groups | |
| • Develop and test multi-level interventions for cardiovascular risk reduction in transgender adults | |
| • Examine social and clinical determinants of cardiovascular health in transgender adults | |
| • Characterize the role of resilience in buffering the cardiovascular effects of stress in transgender people | |
Footnotes
Statement from Writing Group
The writing group included scholars with extensive experience conducting research regarding health and well-being of gender minority populations with many identifying as LGBTQ themselves.
References
- 1.Johns MM, Lowry R, Andrzejewski J, et al. Transgender Identity and Experiences of Violence Victimization, Substance Use, Suicide Risk, and Sexual Risk Behaviors Among High School Students - 19 States and Large Urban School Districts, 2017. MMWR Morb Mortal Wkly Rep 2019;68(3):67–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baker KE. Findings From the Behavioral Risk Factor Surveillance System on Health-Related Quality of Life Among US Transgender Adults, 2014–2017. JAMA Intern Med. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caceres BA, Streed CG Jr., Corliss HL, et al. Assessing and Addressing Cardiovascular Health in LGBTQ Adults: A Scientific Statement From the American Heart Association. Circulation. 2020:CIR0000000000000914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Downing JM, Przedworski JM. Health of Transgender Adults in the U.S., 2014–2016. Am J Prev Med 2018;55(3):336–344. [DOI] [PubMed] [Google Scholar]
- 5.Alzahrani T, Nguyen T, Ryan A, et al. Cardiovascular Disease Risk Factors and Myocardial Infarction in the Transgender Population. Circ Cardiovasc Qual Outcomes. 2019;12(4):e005597. [DOI] [PubMed] [Google Scholar]
- 6.Delozier AM, Kamody RC, Rodgers S, Chen D. Health Disparities in Transgender and Gender Expansive Adolescents: A Topical Review From a Minority Stress Framework. J Pediatr Psychol. 2020;45(8):842–847. [DOI] [PubMed] [Google Scholar]
- 7.Lefevor GT, Boyd-Rogers CC, Sprague BM, Janis RA. Health disparities between genderqueer, transgender, and cisgender individuals: An extension of minority stress theory. J Couns Psychol. 2019;66(4):385–395. [DOI] [PubMed] [Google Scholar]
- 8.Sims M, Glover LSM, Gebreab SY, Spruill TM. Cumulative psychosocial factors are associated with cardiovascular disease risk factors and management among African Americans in the Jackson Heart Study. BMC Public Health. 2020;20(1):566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cavanagh L, Obasi EM. The Moderating Role of Coping Style on Chronic Stress Exposure and Cardiovascular Reactivity Among African American Emerging Adults. Prev Sci 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hatzenbuehler ML, Slopen N, McLaughlin KA. Stressful life events, sexual orientation, and cardiometabolic risk among young adults in the United States. Health Psychol 2014;33(10):1185–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rich AJ, Williams J, Malik M, et al. Biopsychosocial Mechanisms Linking Gender Minority Stress to HIV Comorbidities Among Black and Latina Transgender Women (LITE Plus): Protocol for a Mixed Methods Longitudinal Study. JMIR Res Protoc 2020;9(4):e17076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kcomt L, Evans-Polce RJ, Veliz PT, Boyd CJ, McCabe SE. Use of Cigarettes and E-Cigarettes/Vaping Among Transgender People: Results From the 2015 U.S. Transgender Survey. Am J Prev Med 2020;59(4):538–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wheldon CW, Wiseman KP. Tobacco Use Among Transgender and Gender Non-conforming Adults in the United States. Tob Use Insights. 2019;12:1179173X19849419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bishop A, Overcash F, McGuire J, Reicks M. Diet and Physical Activity Behaviors Among Adolescent Transgender Students: School Survey Results. J Adolesc Health. 2020;66(4):484–490. [DOI] [PubMed] [Google Scholar]
- 15.Fredriksen-Goldsen KI, Cook-Daniels L, Kim H-J, et al. Physical and mental health of transgender older adults: an at-risk and underserved population. The Gerontologist. 2014;54(3):488–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones BA, Haycraft E, Bouman WP, Arcelus J. The Levels and Predictors of Physical Activity Engagement Within the Treatment-Seeking Transgender Population: A Matched Control Study. J Phys Act Health. 2018;15(2):99–107. [DOI] [PubMed] [Google Scholar]
- 17.Guss CE, Williams DN, Reisner SL, Austin SB, Katz-Wise SL. Disordered Weight Management Behaviors, Nonprescription Steroid Use, and Weight Perception in Transgender Youth. Journal of Adolescent Health. 2017;60(1):17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Velho I, Fighera TM, Ziegelmann PK, Spritzer PM. Effects of testosterone therapy on BMI, blood pressure, and laboratory profile of transgender men: a systematic review. Andrology. 2017;5(5):881–888. [DOI] [PubMed] [Google Scholar]
- 19.Suppakitjanusant P, Ji Y, Stevenson MO, et al. Effects of gender affirming hormone therapy on body mass index in transgender individuals: A longitudinal cohort study. Journal of clinical & translational endocrinology. 2020;21:100230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Olson-Kennedy J, Okonta V, Clark LF, Belzer M. Physiologic Response to Gender-Affirming Hormones Among Transgender Youth. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2018;62(4):397–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jarin J, Pine-Twaddell E, Trotman G, et al. Cross-Sex Hormones and Metabolic Parameters in Adolescents With Gender Dysphoria. Pediatrics. 2017;139(5). [DOI] [PubMed] [Google Scholar]
- 22.Klaver M, de Mutsert R, van der Loos M, et al. Hormonal Treatment and Cardiovascular Risk Profile in Transgender Adolescents. Pediatrics. 2020;145(3). [DOI] [PubMed] [Google Scholar]
- 23.Mueller A, Zollver H, Kronawitter D, et al. Body composition and bone mineral density in male-to-female transsexuals during cross-sex hormone therapy using gonadotrophin-releasing hormone agonist. Experimental and clinical endocrinology & diabetes : official journal, German Society of Endocrinology [and] German Diabetes Association. 2011;119(2):95–100. [DOI] [PubMed] [Google Scholar]
- 24.Fisher AD, Castellini G, Ristori J, et al. Cross-Sex Hormone Treatment and Psychobiological Changes in Transsexual Persons: Two-Year Follow-Up Data. The Journal of clinical endocrinology and metabolism. 2016;101(11):4260–4269. [DOI] [PubMed] [Google Scholar]
- 25.Millington K, Schulmeister C, Finlayson C, et al. Physiological and Metabolic Characteristics of a Cohort of Transgender and Gender-Diverse Youth in the United States. Journal of Adolescent Health. 2020;67(3):376–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nokoff NJ, Scarbro SL, Moreau KL, et al. Body Composition and Markers of Cardiometabolic Health in Transgender Youth Compared With Cisgender Youth. J Clin Endocrinol Metab. 2020;105(3):e704–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Streed CG Jr., Harfouch O, Marvel F, Blumenthal RS, Martin SS, Mukherjee M Cardiovascular Disease Among Transgender Adults Receiving Hormone Therapy: A Narrative Review. Ann Intern Med. 2017;167(4):256–267. [DOI] [PubMed] [Google Scholar]
- 28.Deutsch MB, Bhakri V, Kubicek K. Effects of cross-sex hormone treatment on transgender women and men. Obstetrics and gynecology. 2015;125(3):605–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.SoRelle JA, Jiao R, Gao E, et al. Impact of Hormone Therapy on Laboratory Values in Transgender Patients. Clin Chem. 2019;65(1):170–179. [DOI] [PubMed] [Google Scholar]
- 30.Pelusi C, Costantino A, Martelli V, et al. Effects of three different testosterone formulations in female-to-male transsexual persons. J Sex Med. 2014;11(12):3002–3011. [DOI] [PubMed] [Google Scholar]
- 31.Emi Y, Adachi M, Sasaki A, Nakamura Y, Nakatsuka M. Increased arterial stiffness in female-to-male transsexuals treated with androgen. Journal of Obstetrics and Gynaecology Research. 2008;34(5):890–897. [DOI] [PubMed] [Google Scholar]
- 32.van Velzen DM, Paldino A, Klaver M, et al. Cardiometabolic Effects of Testosterone in Transmen and Estrogen Plus Cyproterone Acetate in Transwomen. J Clin Endocrinol Metab. 2019;104(6):1937–1947. [DOI] [PubMed] [Google Scholar]
- 33.Maraka S, Singh Ospina N, Rodriguez-Gutierrez R, et al. Sex Steroids and Cardiovascular Outcomes in Transgender Individuals: A Systematic Review and Meta-Analysis. J Clin Endocrinol Metab. 2017;102(11):3914–3923. [DOI] [PubMed] [Google Scholar]
- 34.Vehkavaara S, Silveira A, Hakala-Ala-Pietila T, et al. Effects of oral and transdermal estrogen replacement therapy on markers of coagulation, fibrinolysis, inflammation and serum lipids and lipoproteins in postmenopausal women. Thromb Haemost. 2001;85(4):619–625. [PubMed] [Google Scholar]
- 35.Nokoff NJ, Scarbro S, Juarez-Colunga E, Moreau KL, Kempe A. Health and Cardiometabolic Disease in Transgender Adults in the United States: Behavioral Risk Factor Surveillance System 2015. J Endocr Soc 2018;2(4):349–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wierckx K, Elaut E, Declercq E, et al. Prevalence of cardiovascular disease and cancer during cross-sex hormone therapy in a large cohort of trans persons: a case-control study. Eur J Endocrinol. 2013;169(4):471–478. [DOI] [PubMed] [Google Scholar]
- 37.Spanos C, Bretherton I, Zajac JD, Cheung AS. Effects of gender-affirming hormone therapy on insulin resistance and body composition in transgender individuals: A systematic review. World journal of diabetes. 2020;11(3):66–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shadid S, Abosi-Appeadu K, De Maertelaere AS, et al. Effects of Gender-Affirming Hormone Therapy on Insulin Sensitivity and Incretin Responses in Transgender People. Diabetes care. 2020;43(2):411–417. [DOI] [PubMed] [Google Scholar]
- 39.Defreyne J, Van de Bruaene LDL, Rietzschel E, Van Schuylenbergh J, T'Sjoen GGR. Effects of Gender-Affirming Hormones on Lipid, Metabolic, and Cardiac Surrogate Blood Markers in Transgender Persons. Clin Chem. 2019;65(1):119–134. [DOI] [PubMed] [Google Scholar]
- 40.Pyra M, Casimiro I, Rusie L, et al. An Observational Study of Hypertension and Thromboembolism Among Transgender Patients Using Gender-Affirming Hormone Therapy. Transgend Health 2020;5(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Feinstein Matthew J, Hsue Priscilla Y, Benjamin Laura A, et al. Characteristics, Prevention, and Management of Cardiovascular Disease in People Living With HIV: A Scientific Statement From the American Heart Association. Circulation. 2019;140(2):e98–e124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Becasen JS, Denard CL, Mullins MM, Higa DH, Sipe TA. Estimating the Prevalence of HIV and Sexual Behaviors Among the US Transgender Population: A Systematic Review and Meta-Analysis, 2006–2017. Am J Public Health. 2018:e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gosiker BJ, Lesko CR, Rich AJ, et al. Cardiovascular disease risk among transgender women living with HIV in the United States. PLoS One. 2020;15(7):e0236177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xu Y, Arora RC, Hiebert BM, et al. Non-invasive endothelial function testing and the risk of adverse outcomes: a systematic review and meta-analysis. European Heart Journal – Cardiovascular Imaging. 2014. [DOI] [PubMed] [Google Scholar]
- 45.Inoue N Stress and atherosclerotic cardiovascular disease. J Atheroscler Thromb. 2014;21(5):391–401. [DOI] [PubMed] [Google Scholar]
- 46.Moreau KL, Hildreth KL, Klawitter J, Blatchford P, Kohrt WM. Decline in endothelial function across the menopause transition in healthy women is related to decreased estradiol and increased oxidative stress. Geroscience. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moreau KL, Stauffer BL, Kohrt WM, Seals DR. Essential Role of Estrogen for Improvements in Vascular Endothelial Function With Endurance Exercise in Postmenopausal Women. Journal of Clinical Endocrinology & Metabolism. 2013;98(11):4507–4515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sansone A, Rastrelli G, Cignarelli A, et al. Effect of treatment with testosterone on endothelial function in hypogonadal men: a systematic review and meta-analysis. International Journal of Impotence Research. 2019. [DOI] [PubMed] [Google Scholar]
- 49.Gulanski BI, Flannery CA, Peter PR, Leone CA, Stachenfeld NS. Compromised endothelial function in transgender men taking testosterone. Clin Endocrinol (Oxf) 2020;92(2):138–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.New G, Duffy SJ, Harper RW, Meredith IT. Long-term oestrogen therapy is associated with improved endothelium-dependent vasodilation in the forearm resistance circulation of biological males. Clin Exp Pharmacol Physiol. 2000;27(1–2):25–33. [DOI] [PubMed] [Google Scholar]
- 51.Sharula, Chekir C, Emi Y, et al. Altered arterial stiffness in male-to-female transsexuals undergoing hormonal treatment. J Obstet Gynaecol Res. 2012;38(6):932–940. [DOI] [PubMed] [Google Scholar]
- 52.New G, Timmins KL, Duffy SJ, et al. Long-term estrogen therapy improves vascular function in male to female transsexuals. J Am Coll Cardiol. 1997;29(7):1437–1444. [DOI] [PubMed] [Google Scholar]
- 53.Ciccone MM, Loverro G, Scicchitano P, et al. Surgical and pharmacological reassignment: influence on transsexual cardiovascular risk profile. Intern Med J. 2017;47(11):1255–1262. [DOI] [PubMed] [Google Scholar]
- 54.Butler ES, McGlinchey E, Juster RP. Sexual and gender minority sleep: A narrative review and suggestions for future research. J Sleep Res. 2020;29(1):e12928. [DOI] [PubMed] [Google Scholar]
- 55.Harry-Hernandez S, Reisner SL, Schrimshaw EW, et al. Gender Dysphoria, Mental Health, and Poor Sleep Health Among Transgender and Gender Nonbinary Individuals: A Qualitative Study in New York City. Transgend Health 2020;5(1):59–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kolp H, Wilder S, Andersen C, et al. Gender minority stress, sleep disturbance, and sexual victimization in transgender and gender nonconforming adults. J Clin Psychol. 2020;76(4):688–698. [DOI] [PubMed] [Google Scholar]
- 57.Gilbert PA, Pass LE, Keuroghlian AS, Greenfield TK, Reisner SL. Alcohol research with transgender populations: A systematic review and recommendations to strengthen future studies. Drug Alcohol Depend. 2018;186:138–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Day JK, Fish JN, Perez-Brumer A, Hatzenbuehler ML, Russell ST. Transgender Youth Substance Use Disparities: Results From a Population-Based Sample. Journal of Adolescent Health. 2017;61(6):729–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Reisner SL, Greytak EA, Parsons JT, Ybarra ML. Gender Minority Social Stress in Adolescence: Disparities in Adolescent Bullying and Substance Use by Gender Identity. Journal of Sex Research. 2015;52(3):243–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Staples JM, Neilson EC, George WH, Flaherty BP, Davis KC. A descriptive analysis of alcohol behaviors across gender subgroups within a sample of transgender adults. Addict Behav. 2018;76:355–362. [DOI] [PubMed] [Google Scholar]
- 61.Kidd JD, Levin FR, Dolezal C, Hughes TL, Bockting WO. Understanding predictors of improvement in risky drinking in a U.S. multi-site, longitudinal cohort study of transgender individuals: Implications for culturally-tailored prevention and treatment efforts. Addictive Behaviors. 2019;96:68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Coulter RWS, Bersamin M, Russell ST, Mair C. The Effects of Gender- and Sexuality-Based Harassment on Lesbian, Gay, Bisexual, and Transgender Substance Use Disparities. J Adolesc Health. 2018;62(6):688–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rowe C, Santos G-M, McFarland W, Wilson EC. Prevalence and correlates of substance use among trans female youth ages 16–24 years in the San Francisco Bay Area. Drug Alcohol Depend. 2015;147:160–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jasuja GK, de Groot A, Quinn EK, et al. Beyond Gender Identity Disorder Diagnoses Codes: An Examination of Additional Methods to Identify Transgender Individuals in Administrative Databases. Med Care 2020;58(10):903–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Streed CG Jr., Grasso C, Reisner SL, Mayer KH. Sexual Orientation and Gender Identity Data Collection: Clinical and Public Health Importance. American Journal of Public Health. 2020;110(7):991–993. [Google Scholar]
- 66.Mensah GA. Eliminating disparities in cardiovascular health: six strategic imperatives and a framework for action. Circulation. 2005;111(10):1332–1336. [DOI] [PubMed] [Google Scholar]
- 67.Streed CG Jr., Lunn MR, Siegel J, Obedin-Maliver J Meeting the Patient Care, Education, and Research Missions: Academic Medical Centers Must Comprehensively Address Sexual and Gender Minority Health. Acad Med 2020. [DOI] [PubMed] [Google Scholar]
- 68.Dubin SN, Nolan IT, Streed CG, Greene RE, Radix AE, Morrison SD. Transgender health care: improving medical students' and residents' training and awareness. Adv Med Educ Pract. 2018;9:377–391. [DOI] [PMC free article] [PubMed] [Google Scholar]