Abstract
The purpose of this prospective study was to investigate whether sedentary screen time (SST) and physical activity in adolescence were related to sleep duration in adulthood and whether these associations varied by sex. We analyzed data from 9279 adolescents who participated in Waves I and V of the National Longitudinal Study of Adolescent Health (Add Health) in the United States. SST was measured by reported hours spent watching television/videos or playing video/computer games per week. Physical activity was measured with participation in school team club sports and frequency (times/week) of moderate to vigorous physical activity (MVPA). Results from multinomial regression models indicated that adolescents with more SST, particularly 15–21 h (Relative Risk Ratio [RRR] = 1.18, 95% CI: 1.02–1.36) or 22 or more hours (RRR = 1.19, 95% CI: 1.06–1.35) compared to 0–7 h per week SST, had significantly higher relative risk of short sleep (six or fewer hours) in adulthood, after controlling for demographic characteristics, socioeconomic status and health behaviors at Waves I and V, sleep duration at Wave I, and SST and MVPA at Wave V. The association between 22 or more hours per week SST in adolescence and later short sleep varied by sex (RRR = 0.75, 95% CI: 0.58–0.95) and was significantly stronger among males. Measures of physical activity in adolescence did not predict sleep duration. Decreasing adolescents’ SST to prevent suboptimal sleep later in development may be a target for further investigation, particularly for males.
Keywords: Sedentary screen time, Exercise, Sleep duration, Sex differences, Adolescence
1. Introduction
Sleep is essential for physical functioning and well-being. Increasingly, researchers have connected short sleep duration (less than 7 h per 24-h period) to chronic health conditions such as diabetes, obesity, heart disease, and cognitive impairment, and also to longevity (Bruce et al., 2017; Grandner et al., 2016; Kripke et al., 2002; Ruan et al., 2015; St-Onge et al., 2016). Even as the importance of sleep for well-being has become well documented and publicized, self-reports of short sleep duration have increased in recent years among adolescents and adults (Keyes et al., 2015; Sheehan et al., 2019), heightening the importance of understanding the shifting determinants of sleep. Among various factors, studies have stressed active lifestyle and healthy behaviors. For example, cross-sectional and longitudinal cohort studies have consistently linked reported and device-based greater physical activity (Farnsworth et al., 2015; Kim et al., 2016; Kredlow et al., 2015; Xu et al., 2019) and lower sedentary behavior (Buman et al., 2015; Kakinami et al., 2017; Kim et al., 2016; Xu et al., 2019; Yang et al., 2017) with optimal sleep in adolescents and adults. However, research has indicated that sleep is predicted not only by current daily or weekly factors, but also by factors and experiences that occur throughout the life span (Johnson et al., 2004; Sheehan et al., 2020). Here we use a longitudinal nationally representative sample of American adolescents, the National Longitudinal Study of Adolescent Health (hereafter Add Health), to analyze whether sedentary behavior and physical activity in adolescence are associated with sleep duration in adulthood. In doing so, we account for important demographic, socioeconomic, and behavioral health (including sleep in adolescence and sedentary behavior and physical activity in adulthood) characteristics in adolescence and adulthood, and test for sex differences.
Adolescence, which occurs between ages 10 and 19, is a period when gradual, nonlinear, and indelible psychological, social, biological, and neural changes occur as one transitions from childhood to adulthood (Brand and Kirov, 2011; Jaworska and MacQueen, 2015). During adolescence, individuals begin to establish behavioral patterns and personal lifestyle choices, which are likely to become habitual and carry over into adulthood (Kumar et al., 2015; Ortega et al., 2013; Telama, 2009; Telama et al., 2005). Levels of sedentary behavior, for example, tend to be stable or increase from adolescence through adulthood (Hanson et al., 2019; Ortega et al., 2013). Similarly, despite a decreasing trend, physical activity shows low-to-moderate rank-order stability from adolescence to adulthood (Hayes et al., 2019; Telama et al., 2005). Additionally, it is becoming increasingly clear that many chronic diseases and psychiatric illnesses begin to develop in childhood and adolescence, highlighting the importance of understanding how behaviors in these ages can shape health and well-being throughout adulthood (Biddle et al., 2004; Kessler et al., 2005). Regular physical activity and low sedentary time could be such behaviors in adolescence that help limit the development of adverse outcomes such as short sleep later in life (Johnson et al., 2004; Sacker and Cable, 2006). Yet, we were unaware of any previous research that has analyzed how physical activity and sedentary behavior in adolescence are related to sleep in adulthood (for the exception for television viewing see Johnson et al. (2004)), which is surprising given that cross-sectional and short-term longitudinal studies suggest that physical activity and sedentary behavior are related to sleep (Kredlow et al., 2015; Yang et al., 2017). While Johnson et al. (2004) found that watching television three or more hours per day in adolescence was related to increased risk of sleep problems in adulthood, they used only a regional sample and did not account for physical activity. Given that high physical activity and high sedentary behavior can be observed in the same person (e.g., one may exercise vigorously and then be sedentary for the rest of the day) and are differentially associated with sleep (Chen et al., 2018; Kim et al., 2016; Xu et al., 2019), it is important to understand their unique, longitudinal associations with sleep.
Sex differences have been reported in physical activity and sedentary behavior, with males (on average) being more likely to participate in physical activity but also having more hours of sedentary behavior (Chen et al., 2018; Nuutinen et al., 2013; Xu et al., 2019). Importantly, there is some evidence that the associations of physical activity and sedentary behavior with sleep vary by sex, but findings of the patterns are mixed (Lin et al., 2018; McClain et al., 2014; Xu et al., 2019) and thus additional work is warranted. In this study, we analyze if there are associations between sedentary behavior and physical activity in adolescence and self-reported sleep duration in adulthood and test for sex differences.
2. Data and methods
2.1. Data
We analyzed a prospective sample from Add Health (see https://addhealth.cpc.unc.edu for more details). Add Health employed a school-based sampling design to enroll a nationally representative sample of adolescents in grades 7–12 in the United States and then followed them from adolescence through adulthood (Harris, 2013). During 1994 and 1995, over 90,000 students from 145 middle, junior, and high schools completed in-school questionnaires, and 20,745 of them were selected to participate in the Wave I in-home interview. The Wave I in-home sample was followed in 1996 (Wave II, N = 14,738), 2001–2002 (Wave III, N = 15,197), 2008–2009 (Wave IV, N = 15,701), and 2016–2018 (Wave V, N = 12,300). Our sample includes 9279 individuals who provided responses regarding physical activity from the in-school questionnaires and participated in Waves I and V in-home interviews. Add Health was approved by the Institutional Review Board (IRB) at the University of North Carolina at Chapel Hill. The permission to conduct secondary analyses was approved by the IRB at Arizona State University.
2.2. Measures
2.2.1. Sleep duration
Participants reported their sleep duration (in hours) in response to one question in the Wave V in-home interview: “How many hours of sleep do you usually get per day/night?” In accord with sleep duration recommendations by the American Academy of Sleep Medicine (Consensus Conference Panel et al., 2015), we categorized participants as short sleepers (six or fewer hours), optimal sleepers (seven to eight hours), and long sleepers (nine or more hours). Additional specifications in which we coded short, optimal, and long sleep duration of adults as six or fewer hours, seven to nine hours, and ten or more hours, respectively, yielded substantively similar results.
2.2.2. Sedentary behavior
Screen time, one component of sedentary behavior, was assessed in the Wave I in-home interview using three questions: “How many hours a week do you watch television?” “How many hours a week do you watch videos?” and “How many hours a week do you play video or computer games?” Hours given in the three responses were summed to create a measure of non–school related sedentary screen time (SST) per week. The distribution of the sum scores is presented in Supplemental Table 1. Based on the Canadian 24-h movement guidelines, individuals aged 5–17 years should limit recreational screen time to no more than 2 h per day (Tremblay et al., 2016). In addition to the 2-h cut-point, previous studies also stressed the 1-h and 3-h per-day cut-points (Carson et al., 2016). Therefore, we categorized the sum into very low (0–7 h/week), low (8–14 h/week), medium (15–21 h/week), and high (22+ hours/week) SST. Importantly, we also investigated four alternative specifications, with SST being operationalized as a continuous variable (specification A with raw scores of SST and specification B with outliers exceeding 3 SD above the mean being assigned values at 3 SD above the mean), a dichotomous variable of meeting the 2-h per day SST recommendation (0–14 h/week) or not (15+ hours/week) (specification C; Tremblay et al., 2016), and a categorical variable using the 10th and 90th percentiles as cutoffs (specification D). Each specification provided substantively similar results as those provided in the text, please see Supplemental Table 2 for more information.
2.2.3. Physical activity
Adolescents reported their participation in team club sports in school using one question in the in-school questionnaires: “Are you participating/Do you plan to participate in the following clubs, organizations and teams?” Team club sports included cheerleading/dance team, baseball/softball, basketball, field hockey, football, ice hockey, soccer, swimming, tennis, track, volleyball, wrestling, and other sport. Participation in any of these team club sports was coded as 1, and nonparticipation in all of them as 0.
In the Wave I in-home interview, adolescents reported their participation in moderate to vigorous physical activity (MVPA) during the past seven days in response to three questions: “During the past week, how many times did you go roller-blading, roller-skating, skate-boarding, or bicycling?” “During the past week, how many times did you play an active sport, such as baseball, softball, basketball, soccer, swimming, or football?” “During the past week, how many times did you exercise, such as jogging, walking, karate, jumping rope, gymnastics or dancing?” Responses ranged from not at all to five or more times and were scored as 0 times = not at all, 1.5 times = 1 or 2 times, 3.5 times = 3 or 4 times, and 6 times = 5 or more times (Bazaco et al., 2016). Responses to the three questions were summed to create a measure of total times of MVPA each week, classified as no (0 times), some (1–4 times), and high (5 or more times) MVPA per week (Bazaco et al., 2016; Ford et al., 2008).
2.2.4. Covariates
Covariates included demographic variables, socioeconomic status (SES), health behaviors, and sleep duration at Wave I, and SES, health behaviors, MVPA, and SST at Wave V. Demographic characteristics included age at Wave I, biological sex, race/ethnicity, and nationality. Among the Wave I (Mage = 16) covariates, SES included household income, highest education of either of the parents, and neighborhood safety. Health behaviors included smoking in the past 30 days, drinking in the past 12 months, body mass index, self-rated health, and physical limitation. Among the Wave V (Mage = 38) covariates, SES consisted of household income, participants’ education, homeownership, and employment. All measures of health behaviors at Wave I were included at Wave V, with the addition of chronic conditions. MVPA and SST at Wave V were coded consistently with Wave I. Detailed descriptions of measures and/or the exact coding of the categories for each covariate are presented in the supplementary material.
2.3. Data analytic plan
We fit a series of hierarchical multinomial regression models, with optimal sleep duration set as the referent category. Multinomial regression models are an appropriate regression approach for polytomous outcomes (i.e., optimal, short, and long sleep duration; Hoffmann, 2004). The models were calculated in Stata 16.1, and the results are presented in the form of Relative Risk Ratios (hereafter RRR). In Model 1, we included measures of SST and physical activity in adolescence (Wave I). In Model 2, we added demographic characteristics and measures of SES, health behaviors, and sleep duration in adolescence (Wave I). In Model 3, we added measures of SES, health behaviors, MVPA, and SST in adulthood (Wave V). We also investigated whether the associations of physical activity and SST with sleep duration varied significantly by sex, by fitting a model interacting the measures of SST and physical activity with sex. To clarify these interactions we calculated the predicted probability using the margins command which calculated for the predicted probability of short sleep duration by sex and SST level with the covariates held at their mean values (Williams, 2012). Missing data (see Supplemental Table 3 for missing rates of variables) were handled with Stata’s multiple imputation suite using chained equations (Bartlett and Morris, 2015). We generated 40 imputed datasets and parameter estimates across datasets were pooled using Rubin’s rule. Detailed information regarding the imputation process is presented in Supplemental Table 4.
3. Results
Descriptive statistics for the full sample and subsamples of males and females are presented in Table 1. At Wave V (Mage = 38), 54% of the sample reported optimal sleep duration (7–8 h), 42% reported short sleep duration (six or fewer hours), and 4% reported long sleep duration (nine or more hours). At Wave I (Mage = 16), 22% reported very low (0–7 h/week), 24% low (8–14 h/week), 16% medium (15–21 h/week), and 38% high (22+ hours/week) SST. Also, at Wave I, 57% of the sample participated in team club sports, 30% of the sample reported some (1–4 times/week) MVPA, and 65% reported five or more times of MVPA.
Table 1.
Descriptive statistics of sleep duration, sedentary behavior, physical activity, and covariates from the national longitudinal study of adolescent to adult health (add health; N = 9279).
| Variables | Full sample (N = 9279) | Male sample (N = 3989) | Female sample (N = 5290) | |||
|---|---|---|---|---|---|---|
| N | Proportion or M (SE) | N | Proportion or M (SE) | N | Proportion or M (SE) | |
| Sleep duration | ||||||
| W1 sleep duration | 7.75 (0.01) | 7.79 (0.02) | 7.72 (0.02) | |||
| Short (e.g., 0–7 h for adolescents aged 13–18) | 3550 | 0.38 | 1491 | 0.37 | 2059 | 0.39 |
| Optimal (e.g., 8–9 h for adolescents aged 13–18) | 4877 | 0.53 | 2120 | 0.53 | 2756 | 0.52 |
| Long (e.g., 10+ hours for adolescents aged 13–18) | 852 | 0.09 | 378 | 0.09 | 474 | 0.09 |
| W5 sleep duration | 6.73 (0.01) | 6.66 (0.02) | 6.79 (0.02) | |||
| Short (0–6 h) | 3907 | 0.42 | 1772 | 0.44 | 2135 | 0.40 |
| Optimal (7–8 h) | 4991 | 0.54 | 2093 | 0.52 | 2898 | 0.55 |
| Long (9+ hours) | 380 | 0.04 | 123 | 0.03 | 257 | 0.05 |
| Sedentary behavior | ||||||
| W1 sedentary screen time (hours/week) | 22.45 (0.22) | 25.27 (0.36) | 20.32 (0.28) | |||
| 0–7 h/week | 2022 | 0.22 | 650 | 0.16 | 1372 | 0.26 |
| 8–14 h/week | 2200 | 0.24 | 874 | 0.22 | 1326 | 0.25 |
| 15–21 h/week | 1508 | 0.16 | 689 | 0.17 | 819 | 0.15 |
| 22+ hours/week | 3549 | 0.38 | 1776 | 0.45 | 1773 | 0.34 |
| W5 sedentary screen time (hours/week) | 13.02 (0.14) | 14.19 (0.23) | 12.15 (0.17) | |||
| 0–7 h/week | 3899 | 0.42 | 1466 | 0.37 | 2432 | 0.46 |
| 8–14 h/week | 2528 | 0.27 | 1136 | 0.28 | 1392 | 0.26 |
| 15–21 h/week | 1609 | 0.17 | 774 | 0.19 | 834 | 0.16 |
| 22+ hours/week | 1244 | 0.13 | 613 | 0.15 | 631 | 0.12 |
| Physical activity | ||||||
| W1 participation in team Club sports | 5328 | 0.57 | 2480 | 0.62 | 2848 | 0.54 |
| W1 moderate to vigorous physical activity (times/week) | 6.57 (0.04) | 7.59 (0.07) | 5.80 (0.05) | |||
| 0 times | 506 | 0.05 | 158 | 0.04 | 348 | 0.07 |
| 1–4 times | 2773 | 0.30 | 896 | 0.22 | 1877 | 0.35 |
| 5+ times | 6000 | 0.65 | 2935 | 0.74 | 3065 | 0.58 |
| W5 moderate to vigorous physical activity (times/week) | 4.45 (0.05) | 5.19 (0.08) | 3.88 (0.06) | |||
| 0 times | 2227 | 0.24 | 723 | 0.18 | 1505 | 0.28 |
| 1–4 times | 3500 | 0.38 | 1469 | 0.37 | 2030 | 0.38 |
| 5+ times | 3552 | 0.38 | 1797 | 0.45 | 1755 | 0.33 |
| Demographics | ||||||
| W1 age | 16.06 (0.02) | 16.16 (0.03) | 15.99 (0.02) | |||
| Female | 5290 | 0.57 | 0 | 0 | 5290 | 1.00 |
| US citizen | 8690 | 0.94 | 3729 | 0.93 | 4961 | 0.94 |
| Race/ethnicity | ||||||
| Non-Hispanic white | 5125 | 0.55 | 2292 | 0.57 | 2833 | 0.54 |
| Non-Hispanic black | 1807 | 0.19 | 661 | 0.17 | 1146 | 0.22 |
| Hispanic | 1328 | 0.14 | 573 | 0.14 | 755 | 0.14 |
| Non-Hispanic other | 1019 | 0.11 | 463 | 0.12 | 556 | 0.11 |
| W1 socioeconomic status | ||||||
| W1 household income | ||||||
| Less than $39,999 | 4464 | 0.48 | 1823 | 0.46 | 2641 | 0.50 |
| $40,000 to $74,999 | 3470 | 0.37 | 1555 | 0.39 | 1915 | 0.36 |
| $75,000+ | 1344 | 0.14 | 610 | 0.15 | 734 | 0.14 |
| W1 highest education of parents | ||||||
| Below high school | 1002 | 0.11 | 386 | 0.10 | 616 | 0.12 |
| High school graduate to some college | 4688 | 0.51 | 1968 | 0.49 | 2720 | 0.51 |
| College graduate or higher | 3589 | 0.39 | 1635 | 0.41 | 1953 | 0.37 |
| W1 neighborhood safety | 8270 | 0.89 | 3602 | 0.90 | 4668 | 0.88 |
| W5 socioeconomic status | ||||||
| W5 household income | ||||||
| Less than $39,999 | 2306 | 0.25 | 813 | 0.20 | 1493 | 0.28 |
| $40,000 to $74,999 | 2277 | 0.25 | 1009 | 0.25 | 1268 | 0.24 |
| $75,000+ | 4695 | 0.51 | 2167 | 0.54 | 2528 | 0.48 |
| W5 education | ||||||
| Below high school | 307 | 0.03 | 161 | 0.04 | 146 | 0.03 |
| High school graduate to some college | 4959 | 0.53 | 2296 | 0.58 | 2662 | 0.50 |
| College graduate or higher | 4013 | 0.43 | 1532 | 0.38 | 2481 | 0.47 |
| W5 home ownership | 8085 | 0.87 | 3399 | 0.85 | 4686 | 0.89 |
| W5 employment | 7864 | 0.85 | 3564 | 0.89 | 4300 | 0.81 |
| W1 health behaviors | ||||||
| W1 smoke | 2197 | 0.24 | 950 | 0.24 | 1247 | 0.24 |
| W1 alcohol | 2638 | 0.28 | 1203 | 0.30 | 1435 | 0.27 |
| W1 body mass index | ||||||
| Underweight | 272 | 0.03 | 129 | 0.03 | 144 | 0.03 |
| Normal weight/overweight | 8028 | 0.87 | 3366 | 0.84 | 4662 | 0.88 |
| Obese | 978 | 0.11 | 494 | 0.12 | 484 | 0.09 |
| W1 self-rated health | ||||||
| Good, very good, or excellent | 8722 | 0.94 | 3811 | 0.96 | 4911 | 0.93 |
| W1 physical limitation | 246 | 0.03 | 104 | 0.03 | 142 | 0.03 |
| W5 health behaviors | ||||||
| W5 smoke | 2160 | 0.23 | 1055 | 0.26 | 1105 | 0.21 |
| W5 alcohol | 6767 | 0.73 | 3065 | 0.77 | 3703 | 0.70 |
| W5 body mass index | ||||||
| Underweight | 88 | 0.01 | 19 | 0.00 | 69 | 0.01 |
| Normal weight/overweight | 5440 | 0.59 | 2441 | 0.61 | 2999 | 0.57 |
| Obese | 3751 | 0.40 | 1529 | 0.38 | 2222 | 0.42 |
| W5 self-rated health | ||||||
| Good, very good, or excellent | 8071 | 0.87 | 3460 | 0.87 | 4610 | 0.87 |
| W5 chronic conditions | 4878 | 0.53 | 2039 | 0.51 | 2840 | 0.54 |
| W5 physical limitation | 438 | 0.05 | 147 | 0.04 | 290 | 0.05 |
Note. W1 = Wave I (Mage = 16), W5 = Wave V (Mage = 38).
3.1. The associations of SST and physical activity with sleep duration
3.1.1. Short sleep duration
RRRs and their 95% CIs from multinomial regression models predicting sleep duration are presented in Table 2. In Model 1, compared to those who had the least SST, those with medium (RRR = 1.17, 95% CI: 1.02–1.34) or high (RRR = 1.37, 95% CI: 1.22–1.53) SST had significantly higher relative risk of reporting short sleep duration. Participation in team club sports during adolescence was associated with lower risk of short sleep duration (RRR = 0.86, 95% CI: 0.79–0.94) in adulthood. Model 2 included demographic characteristics and covariates at Wave I, and when these controls were included, participation in team club sports was no longer significant. However, even after we adjusted for these characteristics, those with medium (RRR = 1.16, 95% CI: 1.01–1.34) or high (RRR = 1.22, 95% CI: 1.08–1.37) SST had significantly higher relative risk of short sleep duration than those with the lowest SST. The substantive results remained similar when covariates at Wave V were included (Model 3). In sum, those who engaged in medium or high SST in adolescence had significantly higher risk of short sleep in adulthood, more than two decades later—even after we accounted for important covariates, including sleep duration in adolescence and MVPA and SST in adulthood. In sensitivity analyses (see Supplemental Table 2), we compared the fully adjusted models with and without SST at Wave I and found that the Akaike Information Criterion decreased across all specifications of SST when including SST at Wave I, suggesting that adding SST at Wave I improved the model fit (Akaike, 1973). In another sensitivity analyses with complete cases only (N = 6249), we still obtained significant prediction from high SST but not medium SST in all models.
Table 2.
Multinomial logistic regression models predicting short (six or fewer hours per 24-h period) and long sleep duration (nine or more hours per 24-h period) compared to optimal sleep duration (seven to eight hours per 24-h period) (N = 9279).
| Short vs. optimal | Long vs. optimal | |||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
| RRR [95% CI] | RRR [95% CI] | RRR [95% CI] | RRR [95% CI] | RRR [95% CI] | RRR [95% CI] | |
| W1 sedentary screen time (reference: 0–7 h/week) | ||||||
| 8–14 h/week | 1.02 [0.90, 1.16] | 1.01 [0.89, 1.15] | 1.02 [0.90, 1.17] | 1.04 [0.76, 1.41] | 1.06 [0.78, 1.45] | 1.12 [0.81, 1.53] |
| 15–21 h/week | 1.17 [1.02, 1.34] | 1.16 [1.01, 1.34] | 1.18 [1.02, 1.36] | 0.97 [0.68, 1.38] | 1.01 [0.71, 1.43] | 1.05 [0.73, 1.50] |
| 22+ hours/week | 1.37 [1.22, 1.53] | 1.22 [1.08, 1.37] | 1.19 [1.06, 1.35] | 1.18 [0.89, 1.56] | 1.16 [0.87, 1.55] | 1.12 [0.83, 1.50] |
| W1 participation in team Club sports | 0.86 [0.79, 0.94] | 0.92 [0.84, 1.01] | 0.97 [0.89, 1.07] | 0.75 [0.61, 0.93] | 0.82 [0.66, 1.02] | 0.92 [0.73, 1.15] |
| W1 moderate to vigorous physical activity (reference: No times) | ||||||
| 1–4 times/week | 0.95 [0.78, 1.16] | 0.98 [0.80, 1.20] | 0.99 [0.81, 1.22] | 0.91 [0.59, 1.42] | 0.92 [0.59, 1.44] | 0.96 [0.61, 1.50] |
| 5+ times/week | 1.03 [0.85, 1.25] | 1.10 [0.90, 1.34] | 1.12 [0.92, 1.37] | 0.79 [0.51, 1.22] | 0.89 [0.57, 1.38] | 0.92 [0.59, 1.44] |
| W1 age | 1.02 [0.99, 1.05] | 1.02 [1.00, 1.05] | 1.01 [0.95, 1.08] | 1.01 [0.95, 1.09] | ||
| Female | 0.85 [0.78, 0.93] | 0.86 [0.79, 0.95] | 1.45 [1.15, 1.82] | 1.31 [1.03, 1.67] | ||
| US citizen | 1.34 [1.10, 1.63] | 1.23 [1.01, 1.50] | 1.16 [0.70, 1.93] | 1.04 [0.62, 1.74] | ||
| Race/ethnicity (reference: Non-Hispanic white) | ||||||
| Non-Hispanic black | 1.99 [1.77, 2.25] | 1.85 [1.63, 2.09] | 1.22 [0.91, 1.64] | 1.07 [0.79, 1.45] | ||
| Hispanic | 1.29 [1.12, 1.48] | 1.31 [1.14, 1.51] | 0.81 [0.57, 1.16] | 0.87 [0.61, 1.25] | ||
| Non-Hispanic other | 1.66 [1.43, 1.93] | 1.67 [1.43, 1.94] | 0.88 [0.58, 1.33] | 0.88 [0.58, 1.33] | ||
| W1 household income (reference: Less than $39,999) | ||||||
| $40,000 to $74,999 | 0.83 [0.74, 0.93] | 0.90 [0.80, 1.02] | 0.83 [0.64, 1.09] | 0.99 [0.75, 1.30] | ||
| $75,000+ | 0.73 [0.62, 0.87] | 0.84 [0.70, 1.00] | 0.77 [0.52, 1.15] | 0.98 [0.65, 1.49] | ||
| W1 highest education of parents (reference: Below high school) | ||||||
| High school graduate to some college | 1.12 [0.96, 1.31] | 1.16 [0.99, 1.36] | 0.69 [0.49, 0.96] | 0.76 [0.54, 1.08] | ||
| College graduate or higher | 0.95 [0.80, 1.13] | 1.07 [0.89, 1.28] | 0.66 [0.45, 0.97] | 0.81 [0.55, 1.21] | ||
| W1 neighborhood safety | 0.89 [0.78, 1.03] | 0.94 [0.82, 1.09] | 0.86 [0.62, 1.21] | 0.94 [0.67, 1.32] | ||
| W1 smoke | 1.20 [1.07, 1.34] | 1.06 [0.94, 1.20] | 1.26 [0.97, 1.65] | 1.11 [0.84, 1.47] | ||
| W1 alcohol | 0.87 [0.78, 0.97] | 0.89 [0.79, 0.99] | 1.03 [0.79, 1.33] | 1.09 [0.84, 1.42] | ||
| W1 body mass index (reference: Normal weight/overweight) | ||||||
| Underweight | 0.85 [0.65, 1.12] | 0.92 [0.70, 1.21] | 1.95 [1.21, 3.12] | 2.11 [1.29, 3.46] | ||
| Obese | 1.30 [1.13, 1.51] | 1.07 [0.92, 1.25] | 0.96 [0.65, 1.40] | 0.80 [0.54, 1.20] | ||
| W1 self-rated good, very good, or excellent health | 1.03 [0.85, 1.24] | 1.22 [1.01, 1.48] | 0.69 [0.47, 1.02] | 0.87 [0.58, 1.29] | ||
| W1 physical limitation | 1.53 [1.17, 2.00] | 1.38 [1.05, 1.82] | 1.26 [0.68, 2.33] | 1.08 [0.58, 2.01] | ||
| W1 sleep duration (reference: Optimal) | ||||||
| Short | 1.43 [1.31, 1.57] | 1.44 [1.31, 1.59] | 0.82 [0.64, 1.04] | 0.83 [0.65, 1.07] | ||
| Long | 0.84 [0.71, 0.98] | 0.79 [0.67, 0.93] | 1.51 [1.11, 2.05] | 1.36 [0.99, 1.87] | ||
| W5 household income (reference: Less than $39,999) | ||||||
| $40,000 to $74,999 | 0.87 [0.76, 1.00] | 0.78 [0.58, 1.06] | ||||
| $75,000+ | 0.81 [0.71, 0.92] | 0.68 [0.50, 0.92] | ||||
| W5 education (reference: Below high school) | ||||||
| High school graduate to some college | 1.30 [1.01, 1.69] | 0.92 [0.57, 1.49] | ||||
| College graduate or higher | 1.07 [0.82, 1.41] | 0.88 [0.52, 1.51] | ||||
| W5 home ownership | 0.92 [0.80, 1.05] | 0.82 [0.61, 1.10] | ||||
| W5 employment | 1.22 [1.06, 1.40] | 0.44 [0.34, 0.57] | ||||
| W5 smoke | 1.29 [1.15, 1.44] | 1.09 [0.83, 1.42] | ||||
| W5 alcohol | 0.98 [0.88, 1.08] | 0.75 [0.59, 0.94] | ||||
| W5 body mass index (reference: Normal weight/overweight) | ||||||
| Underweight | 0.93 [0.58, 1.51] | 0.73 [0.27, 1.92] | ||||
| Obese | 1.21 [1.09, 1.33] | 1.16 [0.91, 1.48] | ||||
| W5 self-rated good, very good, or excellent health | 0.72 [0.62, 0.83] | 0.78 [0.56, 1.07] | ||||
| W5 chronic conditions | 1.25 [1.14, 1.36] | 1.19 [0.95, 1.49] | ||||
| W5 physical limitation | 1.50 [1.19, 1.89] | 1.00 [0.63, 1.59] | ||||
| W5 sedentary screen time (reference: 0–7 h/week) | ||||||
| 8–14 h/week | 0.94 [0.84, 1.04] | 0.82 [0.61, 1.09] | ||||
| 15–21 h/week | 0.91 [0.80, 1.03] | 1.06 [0.78, 1.45] | ||||
| 22+ hours/week | 1.06 [0.91, 1.22] | 1.31 [0.96, 1.80] | ||||
| W5 moderate to vigorous physical activity (reference: No times) | ||||||
| 1–4 times/week | 0.93 [0.83, 1.04] | 0.84 [0.64, 1.09] | ||||
| 5+ times/week | 0.93 [0.82, 1.05] | 0.78 [0.59, 1.04] | ||||
| Akaike’s information criterion | 15,337.80 | 14,966.06 | 14,696.14 | 15,337.80 | 14,966.06 | 14,696.14 |
Note. Relative Risk Ratios (RRR) and 95% Confidence Intervals (CI) are shown. W1 = Wave I, W5 = Wave V. Bold indicates statistically significant results (p < .05).
3.1.2. Long sleep duration
Participation in team club sports was associated with lower risk of long sleep duration in Model 1 (RRR = 0.75, 95% CI: 0.61–0.93), but this association was no longer significant when demographic characteristics and covariates at Wave I were included in Model 2.
3.2. Sex differences
To examine sex differences, we fit a fully adjusted model (i.e., a model with all the covariates) with interaction terms between the measures of physical activity and SST with sex (see Supplemental Table 5). The results indicated that there was a significant interaction between high SST and sex (RRR = 0.75, 95% CI: 0.58–0.95) on short sleep, as the relationship was significantly stronger for males. We present the predicted probabilities by sex from the interaction model in Fig. 1. Fig. 1 indicates that there is a step-wise association between higher SST and the predicted probability of short sleep for males.
Fig. 1.
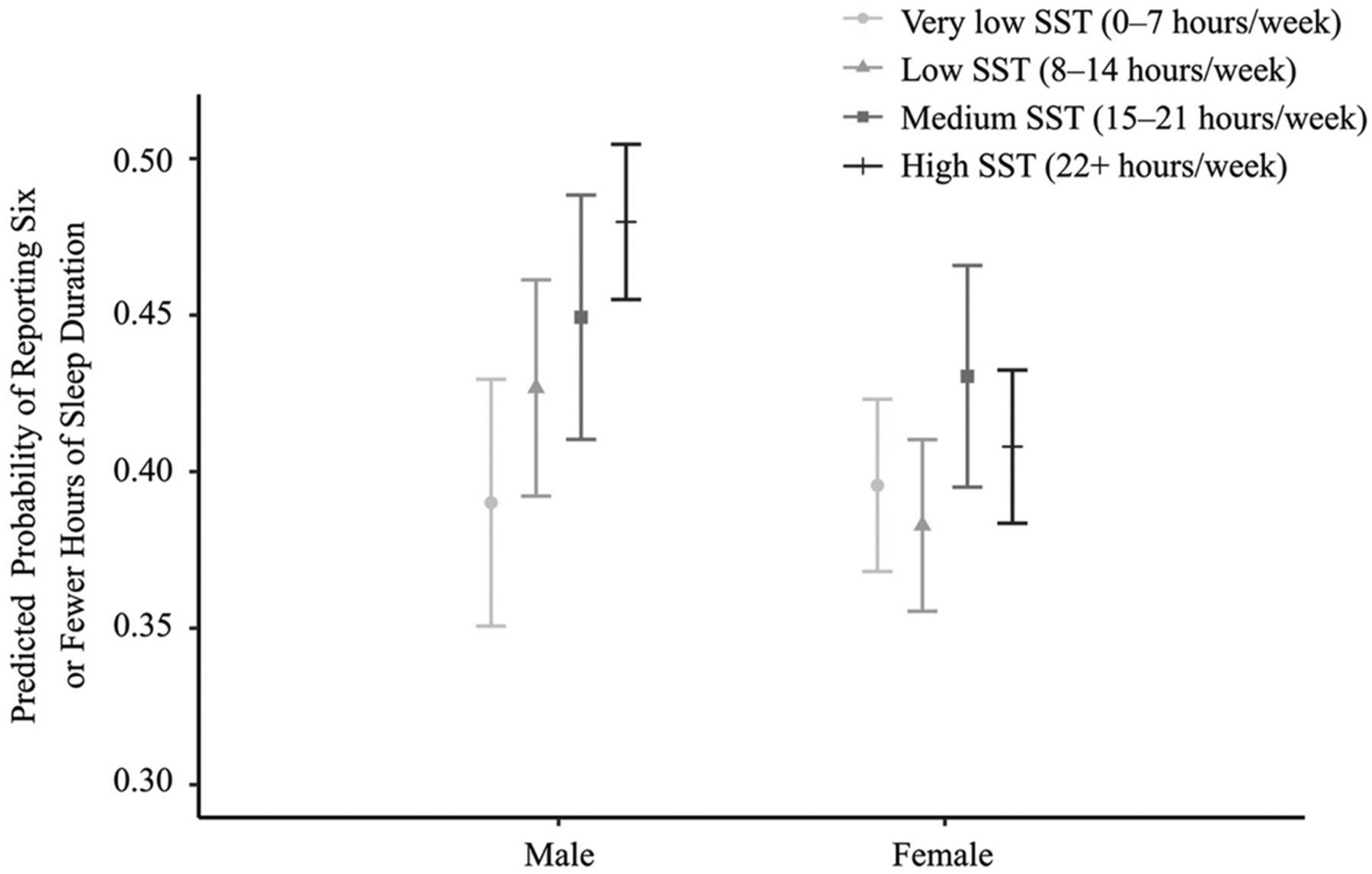
Predicted probability of reporting six or fewer hours of sleep duration (per 24-h period) in male (N = 3989) and female (N = 5290) adults.
Note. SST = sedentary screen time. Error bars represent 95% confidence intervals of estimates.
4. Discussion
Utilizing a 22-year prospective sample, we investigated the unique associations between SST and physical activity during adolescence and sleep duration during adulthood. Our primary findings suggest that more SST in adolescence, especially high (22+ hours/week) SST as compared to very low (0–7 h/week) SST, was associated with higher risk of short sleep duration in adulthood, even after accounting for covariates in adolescence (including sleep duration) and adulthood (including MVPA and SST). These nationally representative results are consistent with studies of regional samples (Johnson et al., 2004; Kakinami et al., 2017; Nuutinen et al., 2013) suggesting the importance of sedentary behavior in determining sleep quality and duration throughout the life course. Our study extended prior research by utilizing a long-term prospective, nationally representative sample, accounting for important covariates, and providing evidence for the “long arm” of sedentary behavior in adolescence for sleep in adulthood.
The long-term association between high SST and elevated risk for short sleep duration was evident. Future studies should further investigate the pathways that might explain the long-term association. For example, it is possible that SST observed in adolescence is likely to carry over and persist into adulthood and is, therefore, prospectively associated with short sleep during adulthood (Falbe et al., 2015; Hanson et al., 2019; Hysing et al., 2015). Indeed, physical activity, sedentary behavior, and sleep time, which are co-dependent within 24-h and weekly time frames (Pedišić, 2014), may be structured in a certain pattern during adolescence and carry over to adulthood (Hanson et al., 2019; Hayes et al., 2019; Ortega et al., 2013; Telama et al., 2005). Additionally, adolescents who have high SST are at increased risk of sleep disorders, which may subsequently be associated with short sleep duration (Grandner and Kripke, 2004; Yang et al., 2017). Likewise, high SST in adolescence may be related to negative physical (e.g., obesity) and psychosocial (e.g., depression, loneliness) outcomes that also likely increase the risk of sleep disorders and short sleep in adulthood (Buman et al., 2011; Tremblay et al., 2010; Vancampfort et al., 2019).
Our results also indicated that the association between SST and sleep duration varied by sex: the association between high SST in adolescence and short sleep in adulthood was significantly stronger among males than females. We were unable to statistically explain why the differences exist, but male and female adolescents may watch different television programs or videos and play different video/computer games. Females are less likely to engage in video games than males, especially competitive and violent video games (Hartmann and Klimmt, 2006). Playing video games, particularly those involving violent elements, may negatively influence sleep (King et al., 2013). It is also plausible that males and females differ in patterns of sedentary behavior. For example, women experience interruptions in sedentary time more often than men do (Bellettiere et al., 2015), and more interruptions in sedentary time are related to more optimal health outcomes (Sardinha et al., 2015). Given that males tend to have longer and more continuous hours of sedentary behavior than females (Bellettiere et al., 2015; Chen et al., 2018; Nuutinen et al., 2013; Xu et al., 2019), males may be at particularly high risk of short sleep duration and these behavior patterns formed in adolescence may carry over into adulthood (Hanson et al., 2019; Ortega et al., 2013).
Physical activity during adolescence, including participation in school team club sports and frequency of MVPA per week, was not related to risk of short or long sleep duration in adulthood in the fully adjusted model. This finding is consistent with one cross-sectional study indicating that when both sedentary behavior and self-reported physical activity were included in models, only sedentary behavior was related to sleep in young adults (Kakinami et al., 2017). These results are not surprising, given that physical activities investigated in this study were likely to occur in the daytime, so that they might have greater influence on sleep quality than on sleep duration (Kredlow et al., 2015). By contrast, sedentary behaviors are not restricted to particular times and are likely to become habitual (Hanson et al., 2019), which could lead to long-term influences on sleep duration.
5. Limitations
This study has some limitations. First, the self-reports of sedentary behavior, physical activity, and sleep duration could suffer from measurement error and social desirability bias. Future studies should use device-based measurements. Of course, given the expensive and often intrusive techniques needed to measure physical activity and sleep, these studies will likely lack the external generalizability that studies using self-reports can provide. Second, sedentary behavior at Wave I was assessed during 1996. Given that the prevalence and conditions in which sedentary behaviors occur have changed in the last two decades, findings of this study are not generalizable but portend poorly for the sleep in adulthood of contemporary cohorts of adolescents who are likely to have increased SST and decreased sleep compared to those analyzed in this study (Matricciani et al., 2012; Yang et al., 2019). Third, Add Health used limited measures of physical activity and sedentary behavior, which did not allow us to test other specifications such as the energy expenditure of MVPA and breaks in SST. Future studies should collect more detailed data on these variables and examine how different specifications are related to sleep. Fourth, given that time of physical activity, sedentary behavior, and sleep may be co-dependent within 24-h or weekly time frames (Pedišić, 2014), future studies should analyze the dynamic balance among these behaviors and how the balance is related to subsequent outcomes. Finally, our missing data were handled with multiple imputation under the assumption of missing at random. It is possible that data were missing not at random, which might lead to biased estimates (Carreras et al., 2021).
6. Conclusion
This study suggests that adolescents, especially adolescent males, who have more SST, particularly high (22+ hours/week) as compared to very low (0–7 h/week) SST, are more likely to get insufficient sleep (six or fewer hours) once they reach adulthood. Given the detrimental effects of insufficient sleep on health and well-being, it is important to investigate whether decreasing adolescents’ SST might promote healthy sleep behaviors and thus greater well-being throughout the life course.
Supplementary Material
Acknowledgments
This work was supported by Global Sport Institute at Arizona State University. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agency. This work uses data from the National Longitudinal Study of Adolescent to Adult Health (Add Health). Add Health is directed by Robert A. Hummer and funded by the National Institute on Aging cooperative agreements U01AG071448 (Hummer) and U01AG071450 (Aiello and Hummer) at the University of North Carolina at Chapel Hill. Waves I–V data are from the Add Health Program Project, grant P01HD31921 (Harris) from Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), with cooperative funding from 23 other federal agencies and foundations. Add Health was designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill.
Footnotes
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ypmed.2021.106812.
References
- Akaike H, 1973. Information theory and an extension of the maximum likelihood principle. In: Petrov BN, Caski F (Eds.), Proceedings of the Second International Symposium on Information Theory. Akademiai Kiado, Budapest, pp. 267–281. [Google Scholar]
- Bartlett JW, Morris TP, 2015. Multiple imputation of covariates by substantive-model compatible fully conditional specification. Stata J. 15, 437–456. [Google Scholar]
- Bazaco MC, Pereira MA, Wisniewski SR, Zgibor JC, Songer TJ, Burke JD, Fabio A, 2016. Is there a relationship between perceived neighborhood contentedness and physical activity in young men and women. J. Urban Health 93, 940–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellettiere J, Carlson JA, Rosenberg D, Singhania A, Natarajan L, Berardi V, LaCroix AZ, Sears DD, Moran K, Crist K, Kerr J, 2015. Gender and age differences in hourly and daily patterns of sedentary time in older adults living in retirement communities. PLoS One 10, e0136161. 10.1371/journal.pone.0136161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biddle SJH, Gorely T, Stensel DJ, 2004. Health-enhancing physical activity and sedentary behaviour in children and adolescents. J. Sports Sci 22, 679–701. 10.1080/02640410410001712412. [DOI] [PubMed] [Google Scholar]
- Brand S, Kirov R, 2011. Sleep and its importance in adolescence and in common adolescent somatic and psychiatric conditions. Int. J. Gen. Med 4, 425. 10.2147/ijgm.s11557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce ES, Lunt L, McDonagh JE, 2017. Sleep in adolescents and young adults. Clin. Med. J. R. Coll. Phys. London 17, 424–4228. 10.7861/clinmedicine.17-5-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buman MP, Hekler EB, Bliwise DL, King AC, 2011. Moderators and mediators of exercise-induced objective sleep improvements in midlife and older adults with sleep complaints. Health Psychol 30, 579–587. 10.1037/a0024293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buman MP, Kline CE, Youngstedt SD, Phillips B, Tulio De Mello M, Hirshkowitz M, 2015. Sitting and television viewing: novel risk factors for sleep disturbance and apnea risk? Results from the 2013 National Sleep Foundation sleep in America poll. Chest 147, 728–734. 10.1378/chest.14-1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carreras G, Miccinesi G, Wilcock A, Preston N, Nieboer D, Deliens L, Groenvold M, Lunder U, van der Heide A, Baccini M, ACTION Consortium, 2021. Missing not at random in end of life care studies: multiple imputation and sensitivity analysis on data from the ACTION study. BMC med. Res. Methodol 21, 1–12. 10.1186/s12874-020-01180-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carson V, Hunter S, Kuzik N, Gray CE, Poitras VJ, Chaput JP, Saunders TJ, Katzmarzyk PT, Okely AD, Connor Gorber S, Kho ME, Sampson M, Lee H, Tremblay MS, 2016. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: An update. Appl. Physiol. Nutr. Metab 41, S240–S265. 10.1139/apnm-2015-0630. [DOI] [PubMed] [Google Scholar]
- Chen ST, Liu Y, Hong JT, Tang Y, Cao ZB, Zhuang J, Zhu Z, Chen PJ, 2018. Co-existence of physical activity and sedentary behavior among children and adolescents in Shanghai, China: do gender and age matter? BMC Public Health 18, 1287. 10.1186/s12889-018-6167-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consensus Conference Panel, Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, Dinges DF, Gangwisch J, Grandner MA, 2015. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of sleep medicine and Sleep Research Society. J. Clin. Sleep Med 11, 591–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falbe J, Davison KK, Franckle RL, Ganter C, Gortmaker SL, Smith L, Land T, Taveras EM, 2015. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics 135, e367–e375. 10.1542/peds.2014-2306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farnsworth JL, Kim Y, Kang M, 2015. Sleep disorders, physical activity, and sedentary behavior among U.S. adults: national health and nutrition examination survey. J. Phys. Act. Health 12, 1567–1575. 10.1123/jpah.2014-0251. [DOI] [PubMed] [Google Scholar]
- Ford CA, Nonnemaker JM, Wirth KE, 2008. The influence of adolescent body mass index, physical activity, and tobacco use on blood pressure and cholesterol in young adulthood. J. Adolesc. Health 43, 576–583. [DOI] [PubMed] [Google Scholar]
- Grandner MA, Kripke DF, 2004. Self-reported sleep complaints with long and short sleep: a nationally representative sample. Psychosom. Med 66, 239–241. 10.1097/01.PSY.0000107881.53228.4D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Seixas A, Shetty S, Shenoy S, 2016. Sleep duration and diabetes risk: population trends and potential mechanisms. Curr. Diab. Rep 16, 106. 10.1007/s11892-016-0805-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson SK, Munthali RJ, Micklesfield LK, Lobelo F, Cunningham SA, Hartman TJ, Norris SA, Stein AD, 2019. Longitudinal patterns of physical activity, sedentary behavior and sleep in urban south African adolescents, birth-to-twenty plus cohort. BMC Pediatr 19, 241. 10.1186/s12887-019-1619-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris KM, 2013. The add health study: design and accomplishments. In: Chapel Hill Carolina Popul. Center, Univ. North Carolina Chapel Hill, pp. 1–22. [Google Scholar]
- Hartmann T, Klimmt C, 2006. Gender and computer games: exploring females’ dislikes. J. Comput. Commun 11, 910–931. [Google Scholar]
- Hayes G, Dowd KP, MacDonncha C, Donnelly AE, 2019. Tracking of physical activity and sedentary behavior from adolescence to young adulthood: a systematic literature review. J. Adolesc. Health 65, 446–454. 10.1016/j.jadohealth.2019.03.013. [DOI] [PubMed] [Google Scholar]
- Hoffmann JP, 2004. Generalized Linear Models: An Applied Approach. Pearson College Division. [Google Scholar]
- Hysing M, Pallesen S, Stormark KM, Jakobsen R, Lundervold AJ, Sivertsen B, 2015. Sleep and use of electronic devices in adolescence: results from a large population-based study. BMJ Open 5, e006748. 10.1136/bmjopen-2014-006748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaworska N, MacQueen G, 2015. Adolescence as a unique developmental period. J. Psychiatry Neurosci 40, 291–293. 10.1503/jpn.150268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, First MB, Brook JS, 2004. Association between television viewing and sleep problems during adolescence and early adulthood. Arch. Pediatr. Adolesc. Med 158, 562–568. 10.1001/archpedi.158.6.562. [DOI] [PubMed] [Google Scholar]
- Kakinami L, O’Loughlin EK, Brunet J, Dugas EN, Constantin E, Sabiston CM, O’Loughlin J, 2017. Associations between physical activity and sedentary behavior with sleep quality and quantity in young adults. Sleep Heal 3, 56–61. 10.1016/j.sleh.2016.11.001. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE, 2005. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatry 62, 593–602. 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Maslowsky J, Hamilton A, Schulenberg J, 2015. The great sleep recession: changes in sleep duration among US adolescents, 1991–2012. Pediatrics 135, 460–468. 10.1542/peds.2014-2707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y, Umeda M, Lochbaum M, Stegemeier S, 2016. Physical activity, screen-based sedentary behavior, and sleep duration in adolescents: youth risk behavior survey, 2011–2013. Prev. Chronic Dis 13, E131. 10.5888/pcd13.160245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King DL, Gradisar M, Drummond A, Lovato N, Wessel J, Micic G, Douglas P, Delfabbro P, 2013. The impact of prolonged violent video-gaming on adolescent sleep: An experimental study. J. Sleep Res 22, 137–143. 10.1111/j.1365-2869.2012.01060.x. [DOI] [PubMed] [Google Scholar]
- Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, Otto MW, 2015. The effects of physical activity on sleep: a meta-analytic review. J. Behav. Med 38, 427–449. 10.1007/s10865-015-9617-6. [DOI] [PubMed] [Google Scholar]
- Kripke DF, Garfinkel L, Wingard DL, 2002. Mortality associated with sleep duration and insomnia. Prim. Care Companion J. Clin. Psychiatry 4, 34. [DOI] [PubMed] [Google Scholar]
- Kumar B, Robinson R, Till S, 2015. Physical activity and health in adolescence. Clin. Med. J. R. Coll. Phys. London 15, 267–272. 10.7861/clinmedicine.15-3-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y, Tremblay MS, Katzmarzyk PT, Fogelholm M, Hu G, Lambert EV, Maher C, Maia J, Olds T, Sarmiento OL, Standage M, Tudor-Locke C, Chaput JP, 2018. Temporal and bi-directional associations between sleep duration and physical activity/sedentary time in children: an international comparison. Prev. Med. (Baltim). 111, 436–441. 10.1016/j.ypmed.2017.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matricciani L, Olds T, Petkov J, 2012. In search of lost sleep: secular trends in the sleep time of school-aged children and adolescents. Sleep Med. Rev 16, 203–211. 10.1016/j.smrv.2011.03.005. [DOI] [PubMed] [Google Scholar]
- McClain JJ, Lewin DS, Laposky AD, Kahle L, Berrigan D, 2014. Associations between physical activity, sedentary time, sleep duration and daytime sleepiness in US adults. Prev. Med. (Baltim). 66, 68–73. 10.1016/j.ypmed.2014.06.003. [DOI] [PubMed] [Google Scholar]
- Nuutinen T, Ray C, Roos E, 2013. Do computer use, TV viewing, and the presence of the media in the bedroom predict school-aged children’s sleep habits in a longitudinal study? BMC Public Health 13, 684. 10.1186/1471-2458-13-684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortega FB, Konstabel K, Pasquali E, Ruiz JR, Hurtig-Wennlöf A, Mäestu J, Löf M, Harro J, Bellocco R, Labayen I, Veidebaum T, Sjöström M, 2013. Objectively measured physical activity and sedentary time during childhood, adolescence and young adulthood: a cohort study. PLoS One 8, e60871. 10.1371/journal.pone.0060871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedišić Ž, 2014. Measurement issues and poor adjustments for physical activity and sleep undermine sedentary behaviour research—the focus should shift to the balance between sleep, sedentary behaviour, standing and activity. Kinesiology 46, 135–146. [Google Scholar]
- Ruan H, Xun P, Cai W, He K, Tang Q, 2015. Habitual sleep duration and risk of childhood obesity: systematic review and dose-response meta-analysis of prospective cohort studies. Sci. Rep 5, 1–14. 10.1038/srep16160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacker A, Cable N, 2006. Do adolescent leisure-time physical activities foster health and well-being in adulthood? Evidence from two British birth cohorts. Eur. J. Pub. Health 16, 331–335. 10.1093/eurpub/cki189. [DOI] [PubMed] [Google Scholar]
- Sardinha LB, Santos DA, Silva AM, Baptista F, Owen N, 2015. Breaking-up sedentary time is associated with physical function in older adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci 70, 119–124. 10.1093/gerona/glu193. [DOI] [PubMed] [Google Scholar]
- Sheehan CM, Frochen SE, Walsemann KM, Ailshire JA, 2019. Are U.S. adults reporting less sleep? findings from sleep duration trends in the National Health Interview Survey, 2004–2017. Sleep 42, zsy221. 10.1093/sleep/zsy221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan CM, Li L, Friedman EM, 2020. Quantity, timing, and type of childhood adversity and sleep quality in adulthood. Sleep Heal 6, 246–252. 10.1016/j.sleh.2020.01.010. [DOI] [PubMed] [Google Scholar]
- St-Onge MP, Grandner MA, Brown D, Conroy MB, Jean-Louis G, Coons M, Bhatt DL, 2016. Sleep duration and quality: impact on lifestyle behaviors and cardiometabolic health: a scientific statement from the American Heart Association. Circulation 134, e367–e386. 10.1161/CIR.0000000000000444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telama R, 2009. Tracking of physical activity from childhood to adulthood: a review. Obes. Facts 2, 187–195. 10.1159/000222244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telama R, Yang X, Viikari J, Välimäki I, Wanne O, Raitakari O, 2005. Physical activity from childhood to adulthood: a 21-year tracking study. Am. J. Prev. Med 28, 267–273. 10.1016/j.amepre.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Tremblay MS, Colley RC, Saunders TJ, Healy GN, Owen N, 2010. Physiological and health implications of a sedentary lifestyle. Appl. Physiol. Nutr. Metab 35, 725–740. [DOI] [PubMed] [Google Scholar]
- Tremblay MS, Carson V, Chaput JP, Connor Gorber S, Dinh T, Duggan M, Faulkner G, Gray CE, Grube R, Janson K, Janssen I, Katzmarzyk PT, Kho ME, Latimer-Cheung AE, LeBlanc C, Okely AD, Olds T, Pate RR, Phillips A, Poitras VJ, Rodenburg S, Sampson M, Saunders TJ, Stone JA, Stratton G, Weiss SK, Zehr L, 2016. Canadian 24-hour movement guidelines for children and youth: An integration of physical activity, sedentary behaviour, and sleep. Appl. Physiol. Nutr. Metab 41, S311–S327. 10.1139/apnm-2016-0151. [DOI] [PubMed] [Google Scholar]
- Vancampfort D, Ashdown-Franks G, Smith L, Firth J, Van Damme T, Christiaansen L, Stubbs B, Koyanagi A, 2019. Leisure-time sedentary behavior and loneliness among 148,045 adolescents aged 12–15 years from 52 low-and middle-income countries. J. Affect. Disord 251, 149–155. [DOI] [PubMed] [Google Scholar]
- Williams R, 2012. Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J 12, 308–331. 10.1177/1536867x1201200209. [DOI] [Google Scholar]
- Xu F, Adams SK, Cohen SA, Earp JE, Greaney ML, 2019. Relationship between physical activity, screen time, and sleep quantity and quality in US adolescents aged 16–19. Int. J. Environ. Res. Public Health 16, 1524. 10.3390/ijerph16091524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L, Cao C, Kantor ED, Nguyen LH, Zheng X, Park Y, Giovannucci EL, Matthews CE, Colditz GA, Cao Y, 2019. Trends in sedentary behavior among the US population, 2001–2016. JAMA - J. Am. Med. Assoc 321, 1587–1597. 10.1001/jama.2019.3636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y, Shin JC, Li D, An R, 2017. Sedentary behavior and sleep problems: a systematic review and meta-analysis. Int. J. Behav. Med 24, 481–492. 10.1007/s12529-016-9609-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


