Abstract
Objective:
To evaluate treatment and posttreatment dentoskeletal effects induced by the Forsus device (FRD) in growing patients with Class II malocclusion in a retrospective controlled clinical study.
Materials and Methods:
Thirty-six Class II patients (mean [SD] age 12.3 [1.2] years) were treated consecutively with the FRD protocol and compared with a sample of 20 subjects with untreated Class II malocclusion (mean [SD] age 12.2 [0.9] years). Lateral cephalograms were taken at the beginning of treatment, at the end of comprehensive treatment (after 2.3 ± 0.4 years), and at a postretention period (after 2.3 ± 1.1 years from the end of comprehensive treatment). Statistical comparisons were carried out with the unpaired t-test and Benjamini-Hochberg correction (P < .05).
Results:
After comprehensive treatment, the FRD sample showed a significant restriction of the sagittal maxillary growth together with a significant correction in overjet, overbite, and molar relationship. During the overall observation interval, the FRD group exhibited no significant sagittal or vertical skeletal changes, while significant improvements were recorded in overjet (−3.8 mm), overbite (−1.5 mm), and molar relationship (+3.7 mm).
Conclusion:
The FRD protocol was effective in correcting Class II malocclusion mainly at the dentoalveolar level when evaluated 2 years after the end of comprehensive treatment.
Keywords: Class II treatment, Fixed functional appliances
INTRODUCTION
Class II malocclusion is one of the most frequent problems in orthodontics, as it affects one third of patients seeking orthodontic treatment.1 According to McNamara,2 the most common characteristic of Class II malocclusion is mandibular retrusion, rather than maxillary prognathism. Thus, among the various orthodontic appliances introduced to treat Class II malocclusion, functional orthopedic appliances are widely used.3–6 Contrary to removable appliances, fixed devices do not require the patient's collaboration and can be worn in association with multibracket therapy, so that Class II malocclusion can be corrected in a single phase treatment. Fixed functional appliances can be grouped into rigid or flexible devices.7 The most commonly used rigid fixed functional appliances are the Herbst8–11 and MARA.12–14 Most popular flexible devices are the Jasper Jumper,15,16 Eureka Spring,17,18 and the Forsus device (FRD).19–24
The FRD is a three-piece (L pin module) or two-piece (EZ2 module) system, composed of a telescoping spring that attaches at the upper first molar and a push rod linked to the lower archwire, distal to either the canine or first premolar bracket. The FRD spring and rod create an equal and opposite force to the maxillary and the mandibular dentition. The appliance is relatively well accepted by patients who may experience some initial discomfort and functional limitations that generally diminish with time.24 The dental, skeletal, and soft tissue short-term effects of comprehensive fixed appliance treatment combined with the FRD in Class II patients were evaluated previously.19–23 No previous study assessed the posttreatment effects of the FRD.
The aim of this retrospective controlled clinical study was to evaluate the treatment and posttreatment dentoskeletal effects induced by FRD in growing patients with Class II malocclusion.
MATERIALS AND METHODS
Study Design
The treatment sample (FRD group) consisted of 36 subjects (21 male, 15 female), consecutively treated from August 2004 to September 2010 at a single private practice by one of the authors. To be included in the study, patients had to present at the first observation (T1) Class II dentoskeletal relationships with overjet larger than 5 mm, full Class II or Class II tendency molar relationship, and ANB larger than 3°. Patients were included in the study regardless of treatment outcomes in terms of correction of Class II malocclusion. This allowed for a further reduction in potential selection biases in the study.
All treated patients were in permanent dentition at T1, and they underwent a specific nonextraction treatment protocol with .022-inch slot preadjusted fixed appliances in combination with the FRD. The FRD was applied at the end of the aligning and leveling phase of orthodontic treatment, when a 0.019 × 0.025-inch stainless steel archwire was inserted in both arches. The mandibular archwire was consistently cinched distal to the molars. In addition, brackets on the lower incisors had a torque of −6° to limit the buccal inclination of the lower incisors. The rods of the FRD were placed on the mandibular archwire distal to the first premolars. No transpalatal arches were used in any phase of comprehensive treatment. The phase with the FRD was undertaken until Class II occlusion was overcorrected to an edge-to-edge incisor relationship. The mean duration of the FRD active phase was 4.8 ± 2.4 months. Thereafter, fixed appliances were maintained in order to finalize the occlusion. The retention protocol after removal of fixed appliance consisted of a removable Hawley retainer in the upper arch used at nighttime for 2 years and a permanent fixed retention wire bonded from canine to canine in the lower arch.
Lateral cephalograms were taken at the beginning of treatment (T1, mean [SD] age 12.3 [1.2] years), at the end of comprehensive treatment (T2, mean [SD] age 14.6 [1.2] years), and at a postretention period (T3, mean [SD] age 16.9 [1.6] years). The duration of the observation intervals were: T1-T2, 2.3 ± 0.4 years; T2-T3, 2.3 ± 1.1; and T1-T3, 4.6 ± 1.2 years. At T1 patients were in the circumpubertal phase of skeletal development, as assessed with the cervical vertebral maturation method25 (15% prepubertal, 70% pubertal, 15% postpubertal). At T3 all patients were in a postpubertal stage of skeletal development. Informed consent was obtained from the patients' parents who also approved use of their children's records in this study.
A sample of 20 subjects with untreated Class II malocclusion was selected from the files of the University of Michigan Growth Study (11 subjects) and of the Denver Child Growth Study (9 subjects). Control subjects presented with the same dentoskeletal characteristics and skeletal maturational stages at T1 as did the patients of the FRD group. Lateral cephalograms of the controls were taken at T1 (mean [SD] age 12.2 [0.9] years), at T2 (mean [SD] age 14.5 [0.9] years), and at T3 (mean [SD] age 16.9 [1.0] years). The duration of the observation intervals were: T1-T2, 2.3 ± 0.5 years; T2-T3, 2.4 ± 0.5; and T1-T3, 4.7 ± 0.7 years. The mean ages at the three observation periods and the duration of the observation intervals in the control group matched those in the treatment group.
Cephalometric Analysis
A customized digitization regimen and analysis provided by cephalometric software (Viewbox, ver 3.0, dHAL Software, Kifissia, Greece) were utilized for all of the cephalograms that were examined in this study. All of the cephalograms were taken with the same radiographic equipment with a magnification factor of 8%. A customized cephalometric analysis containing measurements from the analyses of Steiner,26 Ricketts,27 and McNamara28 was used and generated 20 variables, 8 angular and 12 linear, for each tracing. Tracing involved anatomic stable structures like the inner contour of the symphysis, the alveolar nerve canal, and the inner contour of the palatal bone. A preliminary tracing was made on T1 cephalograms for each patient, and fiducial points were placed (two in the maxilla and two in the mandible). Fiducial markers were then transferred to the T2 and T3 tracings based on superimposition, via software, over anatomic stable structures29 as described by Stahl et al.30 This superimposition allowed describing the movement of the maxillary dentition relative to the maxilla and of mandibular dentition relative to the mandible.
Error of the Method and Power of the Study
The examiner who analyzed lateral cephalograms of treated patients was blind with regard to the origin of the films and the group to which individual subjects belonged.
All cephalograms were traced and superimposed by the same operator and were checked by a second operator to verify anatomic outlines, landmark placement, and superimposition tracing. Any disagreements were resolved to the satisfaction of both observers who were blinded as to group assignment of examined cephalograms.
Twenty randomly selected cephalograms were redigitized by the same operator, and the variables were recalculated to determine the method error with the intraclass correlation coefficient (ICC). The ICCs ranged from 0.93 to 0.99 for linear measurements and from 0.94 to 0.98 for angular measurements. All recalculated measures were within 1 mm or 1° from the original.
The power of the study for the unpaired t-test was assessed on the basis of the sample size of the FRD and control samples, an alpha level of .05, with a mean difference for the clinically relevant variable (ANB) of −1.7° with a standard deviation of 1.2°.21 The calculated power was 0.99 (SigmaStat version 3.5, Systat Software, Point Richmond, Calif).
Statistical Analysis
The homogeneity between the FRD and control groups as to skeletal maturity at each observation time and as to mean duration of observation intervals allowed for comparisons without annualizing the data. Therefore, changes were compared directly in the two groups by means of Student's t-test for independent samples, as normal distribution (Kolmogorov-Smirnov test) was assessed for all the variables (SPSS version 12.0, SPSS Inc, Chicago, Ill).
Before making the comparisons of the longitudinal changes, significant differences between the craniofacial starting forms at T1 were assessed. To evaluate the differences between the FRD and control groups with regard to T2-T1, T3-T2, and overall T3-T1 changes, independent sample t-tests were used (SPSS version 12.0). However, considering that 60 tests were performed on the T2-T1, T3-T2, and overall T3-T1 changes for the 20 cephalometric variables, a correction for the level of significance was introduced. In particular, we applied a Benjamini-Hochberg correction for multiple tests.31 Other corrections like the Bonferroni or the Holm-Bonferroni corrections are considered too conservative for large families of comparisons. The Benjamini-Hochberg correction is less conservative but more powerful with respect to either the Bonferroni or the Holm-Bonferroni corrections, and it appears to be especially suitable when conducting numerous hypothesis tests as in the present study.32
RESULTS
The statistical comparison on starting forms (Table 1) between the two groups did not reveal any significant differences for any cephalometric variable. Results for statistical comparisons on the T2-T1, T3-T2, and T3-T1 changes for the FRD group vs the Class II untreated controls are shown in Tables 2 through 4. The results are hereafter illustrated as differences between the mean changes in the FRD group and the control sample.
Table 1.
Comparison of Starting Forms (T1)
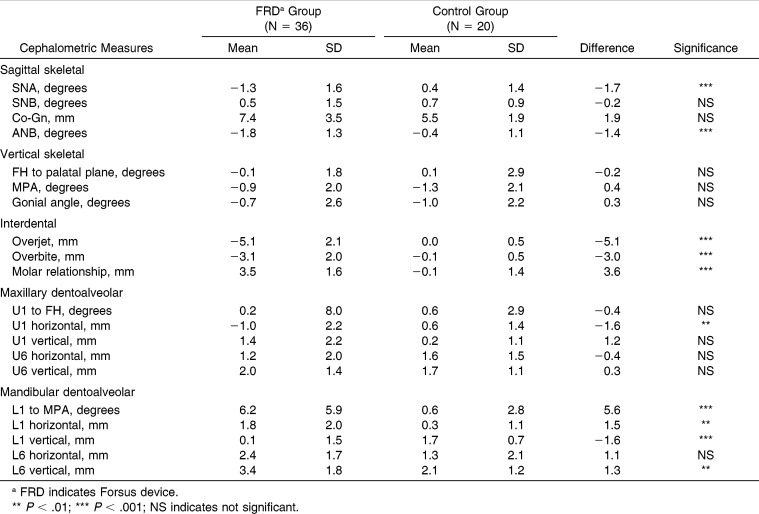
Table 2.
Comparison of Change During Treatment (T1 to T2)
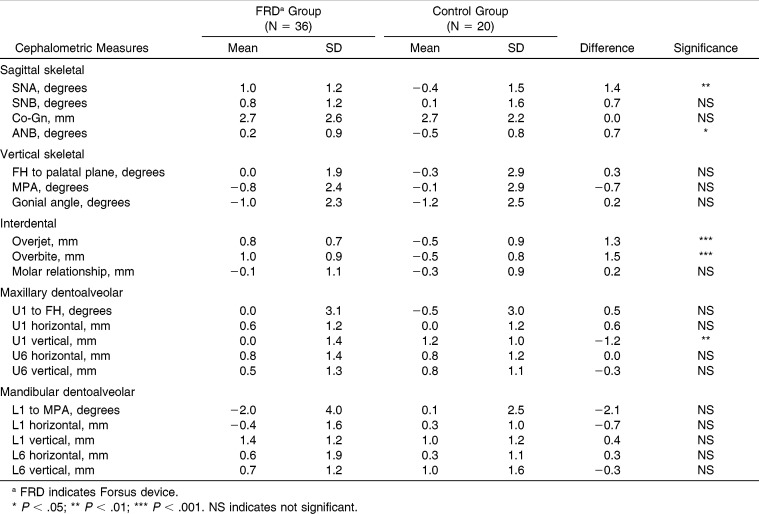
Table 3.
Comparison of Change During Posttreatment (T2 to T3)
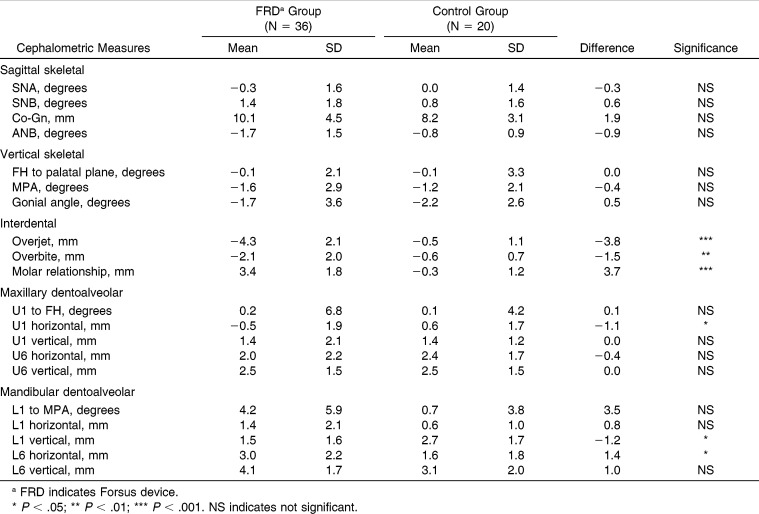
Table 4.
Comparison of Change During Overall Observation Period (T1 to T3)
During the T2-T1 interval, the maxilla exhibited a significantly greater decrease in the sagittal skeletal position (SNA −1.7°) in the FRD group than in the control group. No significant differences were recorded in mandibular sagittal skeletal changes. The FRD group showed significantly greater decreases in the intermaxillary sagittal skeletal relationships (ANB −1.8°). No statistically significant differences between the two groups were found for any of the vertical skeletal cephalometric variables. All interdental measurements showed statistically significant corrections in the FRD group vs the control group (overjet −5.1 mm; overbite −3.1 mm; molar relationship +3.5 mm). Upper incisors exhibited a significant retrusion (U1 horizontal −1.6 mm) in the FRD group vs the control group. On the contrary, the lower incisors showed a significant proclination (L1 to MPA +5.6°) associated with a significant protrusion (L1 horizontal +1.5 mm) and intrusion (L1 vertical −1.6 mm). No significant changes were detected in the horizontal or vertical position of the upper molars in the FRD group vs the control group, while the lower first molars showed a significant extrusion (L6 vertical +1.3 mm).
During the posttreatment period (T2-T3), a significantly greater increase in the sagittal position of the maxilla (SNA +1.4°) occurred in the FRD group. Both overjet and overbite showed significant increases (+1.3 mm and +1.5 mm, respectively) in the FRD group. The upper incisors exhibited a significant intrusion (−1.2 mm) in the FRD group with respect to the control group.
At the end of the comprehensive observation interval (T1-T3), no significant sagittal or vertical skeletal changes were detected. With regard to the interdental changes, the FRD group showed significantly greater decreases in both overjet (−3.8 mm) and overbite (−1.5 mm), as well as a significant improvement in molar relationship (+3.7 mm). The upper incisors exhibited a significantly greater retrusion (U1 horizontal, −1.1 mm) in the FRD group. As a result of therapy, the lower incisors demonstrated a significant intrusion (L1 vertical −1.2 mm). In terms of overall correction of Class II division 1 malocclusion, the success rate was 83.3%, which is very similar to that reported in a previous paper.21
DISCUSSION
Only few studies evaluated treatment and posttreatment effects induced by fixed rigid functional appliances,11,13 while no previous study assessed the posttreatment effects of flexible appliances. In the current study, the treated and control groups were comparable as they did not exhibit any significant differences at T1 in any of the cephalometric variables. A limitation of this study is related to the use of historical controls. The use of historical controls with untreated Class II malocclusions, though not ideal, was due mainly to the ethical issue of leaving subjects with Class II malocclusions without orthodontic treatment during the circum-pubertal stages of development, a biological period which has been demonstrated to be associated with the most favorable treatment effects in Class II patients.10,25
In this section, only those variables that were showing both statistically and clinically significant net differences in the changes between the FRD group and the control group will be discussed. The level of clinical significance was set at 1.5 mm or 1.5°.
In a recent study,24 it was reported that 87.9% of the patients were able to adapt to the FRD. In those patients that do not adapt to this appliance, treatment alternatives like Class II elastics can be taken into account.20 All patients included in this study adapted well to the FRD, and it was not necessary to remove it during active treatment. To prevent initial discomfort, each patient received a care kit (which included an instructional paper on how to reengage springs if necessary and cotton rolls to be placed against the cheeks for any nighttime irritation), wax, and an anesthetic gel (9% benzocaine) in an antiseptic base with instructions for application to any irritated areas.
During the T1-T2 interval, FRD produced dentoskeletal effects that were similar to those described by Franchi et al.21 The most relevant sagittal skeletal changes occurred in the maxillary region, where a significant restraint in the sagittal position of the maxilla was recorded (SNA −1.7°). This “headgear effect” has been described for both fixed rigid functional appliances (Herbst10,33 and MARA11,14) and for flexible devices (Jasper Jumper15,16 and FRD20,21). The FRD protocol did not induce significant mandibular skeletal changes, though the amount of supplementary mandibular growth (Co-Gn +1.9 mm) was similar to that reported by Franchi et al.21 The FRD revealed to be an effective tool in inducing a significant dentoalveolar correction of Class II malocclusions. Significant decreases in both overjet and overbite were recorded (−5.1 mm and −3.0 mm, respectively), as well as a net improvement of the molar relationship (+3.5 mm). The upper incisors exhibited a significant amount of retrusion (−1.6 mm).
However, the most relevant dental changes occurred in the lower arch with the lower incisors demonstrating significant protrusion (+1.5 mm), intrusion (−1.6 mm), and a large amount of proclination (+5.6°). All of these outcomes during the T1-T2 interval were similar to those reported by Baccetti et al.10 for the Herbst appliance, Siara-Olds et al.11 for the MARA, and Franchi et al.21 for the FRD. It should be emphasized that this relevant amount of incisor proclination occurred in spite of the cinching back of the mandibular archwire distal to the molars and despite the torque of −6° embedded in the brackets on the lower incisors. A possible explanation for this lack of control in incisor inclination could be related to the wire-slot interplay (0.022-inch slot with 0.019 × 0.025-inch stainless steel archwire).34 In order to prevent incisor proclination, the use of mandibular rectangular archwires of greater size (0.021 × 0.025-inch) and the addition of a negative torque, also to the archwire in the lower incisor region, can be considered. Recently, the dentoskeletal effects of the FRD with miniscrew anchorage in the lower anterior region have been analyzed with respect to both the conventional FRD and an untreated control sample.35 Proclination of the mandibular incisors was effectively minimized with the usage of miniscrews (L1/MP 3.6° in the FRD and miniscrews group vs 9.3° in the FRD group), though it was recorded during a short interval (6 months).
During the posttreatment period (T2-T3), a statistically, though not clinically, significant relapse of the “headgear effect” was observed (SNA +1.4°).33 With regard to the dentoalveolar measurements, overbite revealed the greatest amount of relapse (+1.5 mm). In previous studies, Siara-Olds et al.11 and Ghislanzoni et al.13 found no statistically significant differences for SNA, overjet, overbite, and the mandibular dentoalveolar measurements during the T2-T3 interval, for the MARA appliance.
During the overall observation interval (T1-T3), no significant sagittal or vertical skeletal changes occurred in the FRD group. In particular, the significant T1-T2 restraint in the sagittal skeletal position of the maxilla was lost due to the relapse that occurred in the T2-T3 interval (SNA T3-T1 net difference, −0.3°). On the other hand, most of the T1-T2 improvements in occlusal relationships were stable. The FRD within a comprehensive orthodontic treatment with preadjusted fixed appliances was effective in correcting overjet (−3.8 mm), overbite (−1.5 mm), and molar relationship (+3.7 mm). As for the T1-T3 dentoalveolar changes, it is interesting to note that the significant T1-T2 proclination of the lower incisors (+5.6°) relapsed during the T2-T3 interval (−2.1°), thus leading to a final nonsignificant net difference of +3.5°. A similar tendency to relapse of the inclination of the lower incisors during the posttreatment period was found for the MARA appliance (−2.2°).13
A general overview of the outcomes of FRD in combination with fixed appliances, when including an average posttreatment period of 2 years, leads to the consideration that the main effects of this treatment protocol are located at the dentoalveolar level, with statistically and clinically significant corrections of overjet, overbite, and molar relationship. These effects appear to be similar to those described for the Class II elastics,36 with the major difference of not having to count on patient's compliance to achieve the desired correction.
CONCLUSIONS
The FRD protocol revealed to be effective in correcting Class II malocclusion mainly at the dentoalveolar level.
At the end of the treatment period, significant improvements in dentoalveolar sagittal intermaxillary relationships were found, together with a slight “headgear effect” on the maxilla.
At the end of the posttreatment period, only the dentoalveolar changes remained stable, while no significant sagittal or vertical skeletal change was present.
REFERENCES
- 1.Proffit WR, Fields HW, Moray LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES-III survey. Int J Adult Orthod Orthognath Surg. 1998;13:97–106. [PubMed] [Google Scholar]
- 2.McNamara JA., Jr Components of Class II malocclusion in children 8–10 years of age. Angle Orthod. 1981;51:177–202. doi: 10.1043/0003-3219(1981)051<0177:COCIMI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Nelson C, Harkness M, Herbison P. Mandibular changes during functional appliance treatment. Am J Orthod Dentofacial Orthop. 1993;104:153–161. doi: 10.1016/S0889-5406(05)81005-4. [DOI] [PubMed] [Google Scholar]
- 4.Patel HP, Moseley HC, Noar JH. Cephalometric determinants of successful functional appliance therapy. Angle Orthod. 2002;72:410–417. doi: 10.1043/0003-3219(2002)072<0410:CDOSFA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Cozza P, Baccetti T, Franchi L, De Toffol L, McNamara JA., Jr Mandibular changes produced by functional appliances in Class II malocclusion: a systematic review. Am J Orthod Dentofacial Orthop. 2006;129:599.e1–12. doi: 10.1016/j.ajodo.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 6.Schaefer AT, McNamara JA, Jr, Franchi L, Baccetti T. A cephalometric comparison of treatment with the twin-block and stainless steel crown Herbst appliance followed by fixed appliance therapy. Am J Orthod Dentofacial Orthop. 2004;126:7–15. doi: 10.1016/j.ajodo.2003.06.017. [DOI] [PubMed] [Google Scholar]
- 7.Ritto AK, Ferreira AP. Fixed functional appliances—a classification. Funct Orthod. 2000;17:2–32. [PubMed] [Google Scholar]
- 8.Pancherz H. The mechanism of Class II correction in Herbst appliance treatment. A cephalometric investigation. Am J Orthod. 1982;82:104–113. doi: 10.1016/0002-9416(82)90489-4. [DOI] [PubMed] [Google Scholar]
- 9.McNamara JA, Jr, Howe RP, Dischinger TG. A comparison of the Herbst appliance. Am J Orthod Dentofacial Orthop. 1990;98:134–144. doi: 10.1016/0889-5406(90)70007-Y. [DOI] [PubMed] [Google Scholar]
- 10.Baccetti T, Franchi L, Stahl F. Comparison of 2 comprehensive Class II treatment protocols including the bonded Herbst and headgear appliances: a double-blind study of consecutively treated patients at puberty. Am J Orthod Dentofacial Orthop. 2009;135:698.e1–e10. doi: 10.1016/j.ajodo.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 11.Siara-Olds NJ, Pangrazio-Kulbersh V, Berger J, Bayirli B. Long-term dentoskeletal changes with the Bionator, Herbst, Twin Block, and MARA functional appliances. Angle Orthod. 2010;80:18–29. doi: 10.2319/020109-11.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gonner U, Ozkan V, Jahn E, Toll DE. Effect of the MARA appliance on the position of the lower anteriors in children, adolescents and adults with Class II malocclusion. J Orofac Orthop. 2007;68:397–412. doi: 10.1007/s00056-007-0656-7. [DOI] [PubMed] [Google Scholar]
- 13.Ghislanzoni LT, Toll DE, Defraia E, Baccetti T, Franchi L. Treatment and posttreatment outcomes induced by the mandibular advancement repositioning appliance; a controlled clinical study. Angle Orthod. 2011;81:684–691. doi: 10.2319/111010-656.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pangrazio-Kulbersh V, Berger JL, Chermak DS, Kaczynski R, Simon ES, Haerian A. Treatment effects of the mandibular anterior repositioning appliance on patients with Class II malocclusion. Am J Orthod Dentofacial Orthop. 2003;123:286–295. doi: 10.1067/mod.2003.8. [DOI] [PubMed] [Google Scholar]
- 15.Jasper JJ, McNamara JA., Jr The correction of interarch malocclusions using a fixed force module. Am J Orthod Dentofacial Orthop. 1995;108:641–650. doi: 10.1016/s0889-5406(95)70010-2. [DOI] [PubMed] [Google Scholar]
- 16.Küçükkeleş N, Ilhan I, Orgun IA. Treatment efficiency in skeletal Class II patients treated with the jasper jumper. Angle Orthod. 2007;77:449–456. doi: 10.2319/0003-3219(2007)077[0449:TEISCI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.DeVincenzo J. The Eureka Spring: a new interarch force delivery system. J Clin Orthod. 1997;31:454–467. [PubMed] [Google Scholar]
- 18.Stromeyer EL, Caruso JM, DeVincenzo JP. A cephalometric study of the Class II correction effects of the Eureka Spring. Angle Orthod. 2002;72:203–210. doi: 10.1043/0003-3219(2002)072<0203:ACSOTC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Vogt W. The Forsus Fatigue Resistant Device. J Clin Orthod. 2006;40:368–377. [PubMed] [Google Scholar]
- 20.Jones G, Buschang PH, Kim KB, Oliver DR. Class II non-extraction patients treated with the Forsus fatigue resistant device versus intermaxillary elastics. Angle Orthod. 2008;78:332–338. doi: 10.2319/030607-115.1. [DOI] [PubMed] [Google Scholar]
- 21.Franchi L, Alvetro L, Giuntini V, Masucci C, Defraia E, Baccetti T. Effectiveness of comprehensive fixed appliance treatment used with the Forsus Fatigue Resistant Device in Class II patients. Angle Orthod. 2011;81:678–683. doi: 10.2319/102710-629.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gunay EA, Arun T, Nalbantgil D. Evaluation of the immediate dentofacial changes in late adolescent patients treated with the Forsus(™) FRD. Eur J Dent. 2011;5:423–432. [PMC free article] [PubMed] [Google Scholar]
- 23.Aras A, Ada E, Saracoğlu H, Gezer NS, Aras I. Comparison of treatments with the Forsus fatigue resistant device in relation to skeletal maturity: a cephalometric and magnetic resonance imaging study. Am J Orthod Dentofacial Orthop. 2011;140:616–625. doi: 10.1016/j.ajodo.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 24.Bowman AC, Saltaji H, Flores-Mir C, Preston B, Tabbaa S. Patient experiences with the Forsus Fatigue Resistant Device. Angle Orthod. 2013;83:437–446. doi: 10.2319/081112-647.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baccetti T, Franchi L, McNamara JA., Jr The cervical vertebral maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod. 2005;11:119–129. [Google Scholar]
- 26.Steiner CC. Cephalometrics for you and me. Am J Orthod. 1953;39:729–755. [Google Scholar]
- 27.Ricketts RM. Perspectives in the clinical application of cephalometrics. The first fifty years. Angle Orthod. 1981;51:115–150. doi: 10.1043/0003-3219(1981)051<0115:PITCAO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.McNamara JA., Jr A method of cephalometric evaluation. Am J Orthod. 1984;86:449–469. doi: 10.1016/s0002-9416(84)90352-x. [DOI] [PubMed] [Google Scholar]
- 29.Bjork A, Skieller V. Facial development and tooth eruption. An implant study at the age of puberty. Am J Orthod. 1972;62:339–383. doi: 10.1016/s0002-9416(72)90277-1. [DOI] [PubMed] [Google Scholar]
- 30.Stahl F, Baccetti T, Franchi L, McNamara JA., Jr Longitudinal growth changes in untreated subjects with Class II Division 1 malocclusion. Am J Orthod Dentofacial Orthop. 2008;134:125–137. doi: 10.1016/j.ajodo.2006.06.028. [DOI] [PubMed] [Google Scholar]
- 31.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B. 1995;57:289–300. [Google Scholar]
- 32.Lesack K, Naugler C. An open-source software program for performing Bonferroni and related corrections for multiple comparisons. J Pathol Inform. 2011;2:52. doi: 10.4103/2153-3539.91130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pancherz H, Anehus-Pancherz M. The headgear effect of the Herbst appliance: a cephalometric long-term study. Am J Orthod Dentofacial Orthop. 1993;103:510–520. doi: 10.1016/0889-5406(93)70090-B. [DOI] [PubMed] [Google Scholar]
- 34.Morina E, Eliades T, Pandis N, Jäger A, Bourauel C. Torque expression of self-ligating brackets compared with conventional metallic, ceramic, and plastic brackets. Eur J Orthod. 2008;30:233–238. doi: 10.1093/ejo/cjn005. [DOI] [PubMed] [Google Scholar]
- 35.Aslan BI, Kucukkaraca E, Turkoz C, Dincer M. Treatment effects of the Forsus Fatigue Resistant Device used with miniscrew anchorage. Angle Orthod. 2014;84:76–87. doi: 10.2319/032613-240.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Janson G, Sathler R, Fernandes TM, Branco NC, Freitas MR. Correction of Class II malocclusion with Class II elastics: a systematic review. Am J Orthod Dentofacial Orthop. 2013;143:383–392. doi: 10.1016/j.ajodo.2012.10.015. [DOI] [PubMed] [Google Scholar]