Abstract
Objective:
To investigate whether there is evidence to support the association between cortical thickness (CtTh) and the primary stability of mini-implants (MI).
Materials and Methods:
A search was performed including articles published until September 2013. The inclusion criteria comprised observational clinical studies conducted in patients who received monocortical MI for orthodontic anchorage and in vivo or ex vivo experimental studies performed to evaluate the primary stability of MI, studies that evaluated the association between CtTh and MI primary stability, CtTh measurement performed numerically, and MI primary stability evaluated by implant stability quotient value, Periotest value , pull-out strength, or insertion torque. Studies conducted exclusively in artificial bone or finite elements were excluded.
Results:
Abstract and title reading identified 15 possible articles to be included. After reading the complete text, three were excluded. One article was found by hand searching and another excluded for an overlapping sample. Finally, 12 articles were selected. A positive correlation was found between primary stability and CtTh when studies that evaluated primary stability through PS were grouped (r = .409) and when studies that evaluated stability in humans were grouped (r = .338).
Conclusions:
There is a positive association between MI primary stability and CtTh of the receptor site. However, there is still a lack of well-designed clinical trials.
Keywords: Mini-implant, Miniscrew, Stability, Cortical thickness
INTRODUCTION
Mini-implants (MI) are anchorage devices that were introduced in orthodontics in the past two decades and whose use quickly spread in clinical practice. The success of MI is related to primary stability, which is defined as the absence of mobility in the bone bed after MI placement1 and depends on the mechanical engagement of an implant with the bone socket.2 Lack of immediate stability can lead to progressive mobility of the device and its subsequent loss.3 If the initial mechanical retention of the MI is not observed, a larger MI should be used or the insertion site should be modified.4 On the other hand, exaggerated tension during insertion may result in heating and damage to the bone tissue,5 including ischemia and necrosis, or even fracture of the MI.6
Primary stability depends on the MI design,6 insertion technique,6 and bone quality and quantity at the receptor site.6–9 The term bone quality has not been clearly defined in the literature. It includes physiological and structural aspects and the degree of bone tissue mineralization. In addition, the role of each of these aspects is not completely understood.10 While some authors assumed that bone quality is equivalent to bone mineral density (BMD),10 others have considered that bone quality refers to cortical thickness (CtTh).
The present systematic review and meta-analysis was focused on the following question: is there scientific evidence to support the influence of CtTh on the primary stability of MI?
MATERIALS AND METHODS
Study Design
This is a systematic review of prognosis that evaluated the association between CtTh (prognostic factor) and MI primary stability (outcome). It is not a systematic review of intervention, as described by the Cochrane Handbook and PRISMA. Therefore, the PRISMA statement was followed as possible.
Study Selection Criteria
The inclusion criteria comprised observational clinical studies conducted in patients who received monocortical MI for orthodontic anchorage and in vivo or ex vivo experimental studies performed in animals to evaluate the primary stability of MI, studies that evaluated the association between CtTh and MI primary stability, the CtTh measurement should have been performed numerically, and MI primary stability should have been evaluated by implant stability quotient (ISQ) value (Ostell, Integration Diagnostics, Gothenburg, Sweden), Periotest value (PTV; Periotest, Medizintechnik Gulden, Modautal, Germany), pull-out strength (PS), or insertion torque (IT) measurement. Studies conducted exclusively in artificial bone or finite elements were excluded.
Search Strategy and Screening of Articles
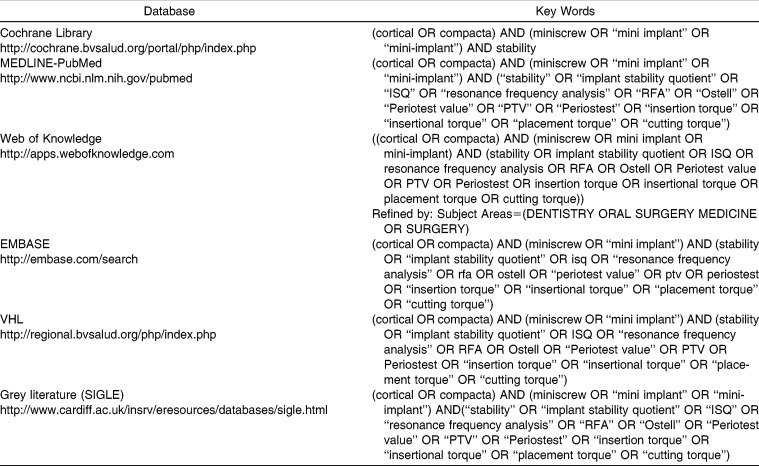
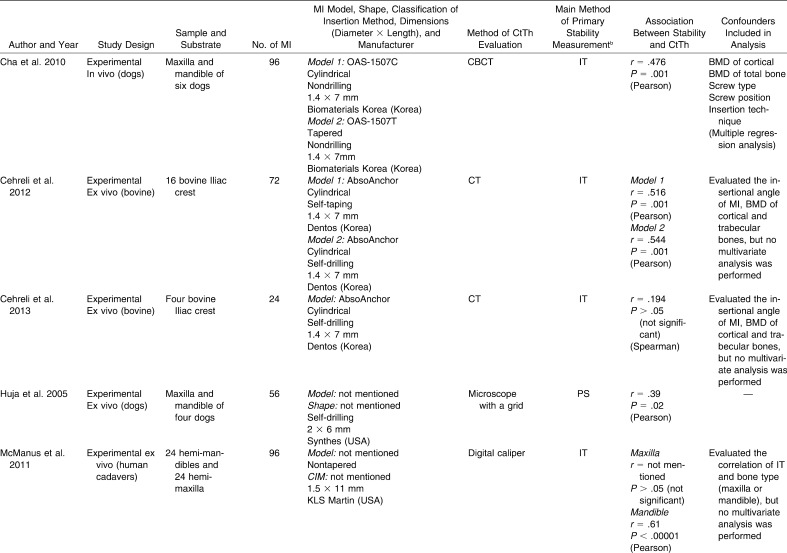
The search process was performed independently by two examiners under the guidance of a librarian. The Cochrane Library, MEDLINE-PubMed, ISI Web of Knowledge, EMBASE, VHL (Virtual Health Library), and gray literature (SIGLE) databases were searched for articles published until September 2013, without language restriction. Appropriate changes in the key words were done to follow the syntax rules of each database (Table 1). The main key words used were “cortical,” “compacta,” “miniscrew,” “mini implant,” “mini-implant,” “stability,” “implant stability quotient,” “ISQ,” “resonance frequency analysis,” “RFA,” “Ostell,” “Periotest value,” “PTV,” “Periostest,” “insertion torque,” “insertional torque,” “placement torque,” and “cutting torque.”
Table 1.
Database and Search Strategy Used
The two examiners evaluated the titles and abstracts of all the studies identified. If the abstract contained insufficient information to allow decision making with regard to inclusion or exclusion, the full article was obtained and reviewed before making a final decision. Articles appearing in more than one database search or containing overlapping samples were considered only once. Any differences between the two readers were solved by consensus. Screening the reference lists of the selected articles complemented the search. The selected articles were then carefully read for quality assessment and control of bias and for data extraction.
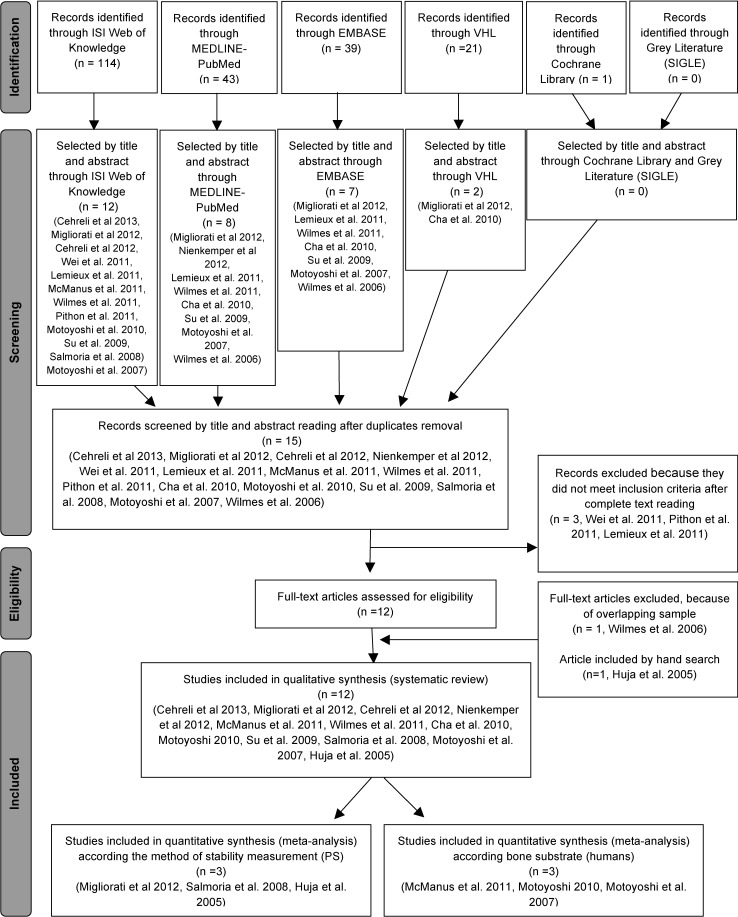
Quality Assessment and Control of Bias
The quality assessment and control of bias were performed using the methodological checklist for prognostic studies developed by the National Institute for Health and Clinical Excellence of the United Kingdom11 (Supplemental Appendix 1).
Data Extraction
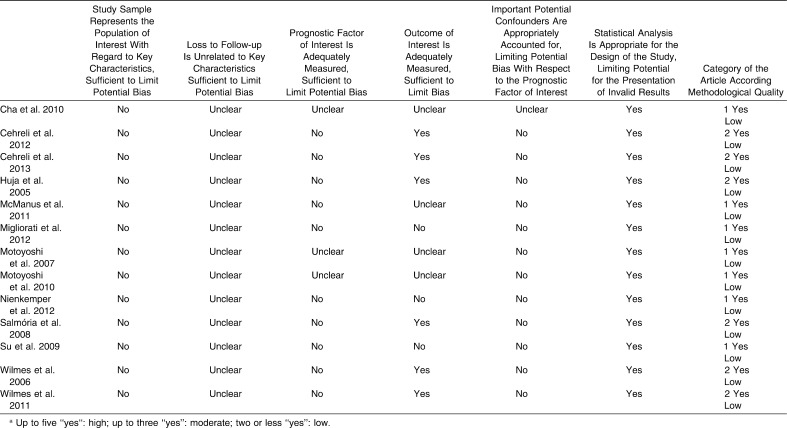
Data on the following issues were extracted from the selected articles and tabulated by the two authors: (1) author and year of publication, (2) study design, (3) sample/bone substrate, (4) number of MI, (5) characterization of MI, (6) method of cortical thickness evaluation, (7) method of primary stability measurement, (8) association between stability and cortical thickness, and (9) confounders included in the analysis. When missing data were identified, the authors were contacted through e-mail.
Meta-analysis
A meta-analysis was performed to combine comparable results. Studies were grouped according to the primary stability measurement method (IT and PS) and bone substrate (humans). The software used in the analyses was the Comprehensive Meta-Analysis (version 2, Biostat, Englewood, Calif).
The individual correlation coefficient from each study was used along with the sample size of screws, discarding the losses. Results were pooled using the random-effects method because the studies compared were not considered to have the same effect size. According to Borenstein et al.,12 when studies are gathered from the published literature, the random-effects model is generally indicated. Heterogeneity was assessed (I2), and the results were expressed in forest plots.
RESULTS
The flow diagram (Figure 1) describes the results of search queries. The search retrieved 114 articles from the ISI Web of Knowledge, 43 from MEDLINE/PubMed, 39 from EMBASE, 21 from VHL, 1 from the Cochrane Library, and none from SIGLE. According to the inclusion and exclusion criteria, a total of 15 articles were selected after title and abstract reading. After full-text reading, four were excluded, three because they did not meet inclusion criteria and one because of an overlapping sample. The two studies conducted by Wilmes et al.6,13 presented some overlapping sample (information confirmed by the author through e-mail contact). During the ranking of these studies (Table 2), it was verified that they had the same score. Therefore, the study that presented more complete data on the results was elected.13 Finally, one study was found by hand search and was included. Thus, 12 studies were included in this systematic review. Data obtained from the articles and e-mail contact are tabulated in Table 3.
Figure 1.
Flow diagram of the literature search.
Table 2.
Articles Ranked According to Quality Assessment and Control of Biasa
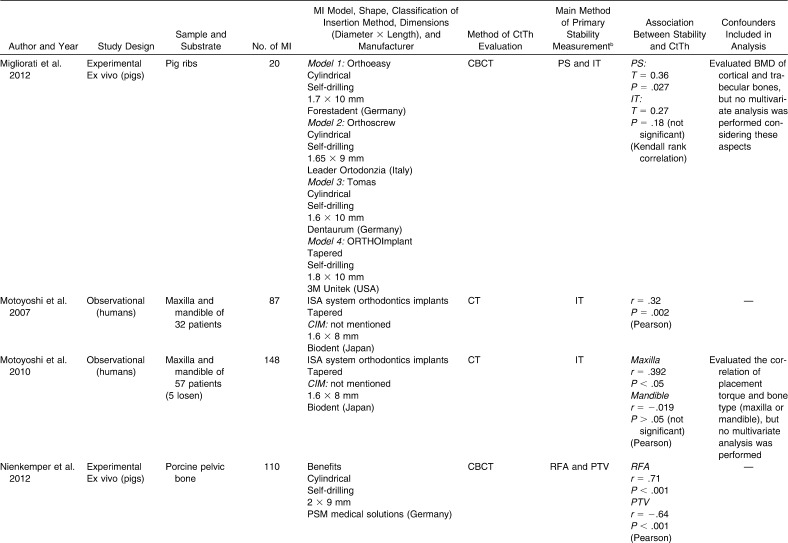
Table 3.
Summarized Data Collected From the Selected Articlesa
Table 3.
Continued
Table 3.
Continued
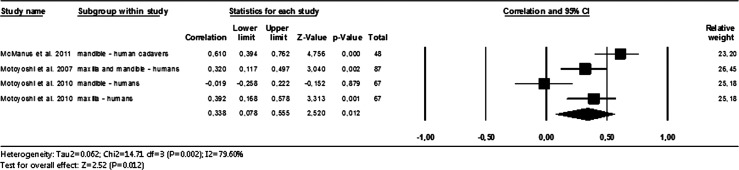
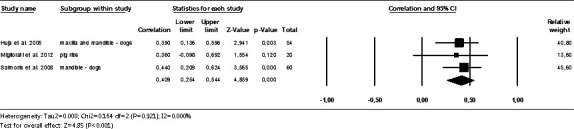
Most of the selected articles presented a positive correlation between primary stability and CtTh.13–15,17–24 The meta-analysis was performed combining comparable results; studies were grouped according to the primary stability measurement method (IT and PS) and bone substrate (humans). The studies that evaluated the primary stability through IT presented high heterogeneity (I2 = 97.23%), and meta-analysis could not be not performed. The studies that used the PS (n = 3) indicated a statistically significant moderate correlation of primary stability and CtTh (r = .409; Figure 2). When evaluating only studies performed in human beings (n = 3), there was also a positive correlation (r = .338; Figure 3). The studies performed in animals were not grouped for meta-analysis because it is difficult to establish whether the bone tissue among the different animals of the selected studies behave in a similar manner.
Figure 2.
Correlation between cortical thickness and primary stability evaluated through pull-out strength.
Figure 3.
Correlation between cortical thickness and primary stability when only studies in human beings were considered.
DISCUSSION
The association between CtTh and MI primary stability in the selected articles was evaluated by correlation tests or linear regression analysis, and most have demonstrated a significant positive association. Correlation coefficients ranged from .32 (moderate correlation)20 to .91 (high correlation).13 When linear regression was performed,13 it was found that 83% of the variation in insertion torque could be explained by CtTh (R2 = .83).
When using PTV to evaluate primary stability,22 the correlation was negative because PTV decreases as stability increases.
Some associations did not present a statistical significance16,18,19,21,23 (Table 3). Methodological differences, such as methods of primary stability and CtTh measurements, MI design and dimensions, and sample size, might be responsible for this difference.
During meta-analysis calculation, the studies that evaluated the primary stability through IT showed a very high heterogeneity (I2 = 97, 23%), invalidating the meta-analysis for this group of studies.
When grouping studies that evaluated primary stability through PS, a moderate positive correlation was found (r = .409; Figure 2). When studies were combined by bone substrate, a weaker positive correlation was found when human beings were evaluated (r = .338; Figure 3). This fact corroborates the assertion that the results of research with animals are applicable to humans, with reservations.26
As cortical thickness is not the only factor related to the primary stability of miniscrews, it is important to include confounders in the analysis. Some authors evaluated the BMD of the bone and found positive correlations between primary stability and the cortical BMD14,15 and bone marrow BMD.19 However, only one of them performed a multivariate analysis.14 The MI design and dimensions are also important parameters for the primary stability of MI.27 All of the selected studies reported the characteristics and dimensions of the MI used, but few of them used more than one type and investigated their influence on the result.13–15 It was verified that the diameter of the MI seemed to have a bigger influence on the primary stability of MI than its length.6,13 This fact reinforces the importance of CtTh in primary stability: as the MI diameter increases, the contact surface between MI and cortical bone also increases. On the other hand, when the length of MI increases, its contact with the trabecular bone increases and the stability is not improved to the same extent.
Even though it was found that CtTh and primary stability are associated, it is important to remember that a very high primary stability is not desirable in clinical practice because of the risk of bone necrosis and subsequent stability loss.6 Motoyoshi et al.25 recommended placement torques between 5 and 10 Ncm. Chaddad et al.28 found higher success rates at torque values greater than 15 Ncm. However, Meursinge Reynders et al.29 performed a systematic review and stated that no evidence indicates that specific maximum insertion torque levels are associated with higher success rates for orthodontic MI mainly because insertional torque measures are not very accurate.30
In this systematic review and meta-analysis, experimental studies were included because there is still a lack of clinical studies with good methodological design evaluating the relationship between CtTh and primary stability of MI. From the selected studies, only two were conducted in living humans, convenience samples were used, and no sample size calculation was made. One study was conducted in human cadavers, without sample size calculation. The other studies were conducted in animals, and only one performed sample size calculation. The authors did not mention calibration, error calculation, or blinding. Therefore, the quality assessment ranked all the articles as “low” considering the quality of evidence and control of bias. A more consistent conclusion could be drawn if only data from clinical studies were used. Although there is great physiological, cellular, and molecular similarity between animal and human models, there are limitations in the use of animals, and extrapolation of results from models to humans should be made with caution.31 Unfortunately, there are few clinical studies in the literature, and it would not be possible to perform a systematic review and meta-analysis if experimental studies were not considered.
Another factor that might have contributed to the low methodological quality was the quality assessment checklist used: the methodological checklist for prognostic studies developed by the National Institute for Health and Clinical Excellence from the United Kingdom. This established checklist focused on clinical studies, while most of the selected studies were experimental. Question 2 of the checklist, for example, which is focused on the loss of sample follow-up, does not accordingly apply to experimental studies. As the clinical studies included in the systematic review did not mention this issue, all of the articles were ranked as “unclear” for this question.
For clinical practice, orthodontists must be aware that very thin cortical bone might generate smaller primary stability of MI. However, other factors such as BMD,14,15,19 MI characteristics, and insertion technique must be considered.6
The evidence to support the relationship between CtTh and MI primary stability is still weak. It is recommended that well-designed clinical trials be conducted to support this question, showing stronger evidence, preferably with the use of multivariate analysis.
CONCLUSION
There is a positive association between MI primary stability and CtTh of the receptor site. However, there is still a lack of well-designed clinical trials.
ACKNOWLEDGMENTS
We are grateful to CAPES (Cordenação de Aperfeiçoamento de Pessoal de Nível Superior) for the PhD scholarship. The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
REFERENCES
- 1.Javed F, Romanos GE. The role of primary stability for successful immediate loading of dental implants: a literature review. J Dent. 2010;38:612–620. doi: 10.1016/j.jdent.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 2.Cehreli MC, Karasoy D, Akca K, Eckert SE. Meta-analysis of methods used to assess implant stability. Int J Oral Maxillofac Implants. 2009;24:1015–1032. [PubMed] [Google Scholar]
- 3.Mischkowski RA, Kneuertz P, Florvaag B, Lazar F, Koebke J, Zoller JE. Biomechanical comparison of four different miniscrew types for skeletal anchorage in the mandibulo-maxillary area. Int J Oral Maxillofac Surg. 2008;37:948–954. doi: 10.1016/j.ijom.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 4.Garfinkle JS, Cunningham LL, Jr, Beeman CS, Kluemper GT, Hicks EP, Kim MO. Evaluation of orthodontic mini-implant anchorage in premolar extraction therapy in adolescents. Am J Orthod Dentofacial Orthop. 2008;133:642–653. doi: 10.1016/j.ajodo.2006.04.053. [DOI] [PubMed] [Google Scholar]
- 5.Park HS, Jeong SH, Kwon OW. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2006;130(1):18–25. doi: 10.1016/j.ajodo.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 6.Wilmes B, Rademacher C, Olthoff G, Drescher D. Parameters affecting primary stability of orthodontic mini-implants. J Orofac Orthop. 2006;67:162–174. doi: 10.1007/s00056-006-0611-z. [DOI] [PubMed] [Google Scholar]
- 7.Cheng SJ, Tseng IY, Lee JJ, Kok SH. A prospective study of the risk factors associated with failure of mini-implants used for orthodontic anchorage. Int J Oral Maxillofac Implants. 2004;19:100–106. [PubMed] [Google Scholar]
- 8.Freudenthaler JW, Haas R, Bantleon HP. Bicortical titanium screws for critical orthodontic anchorage in the mandible: a preliminary report on clinical applications. Clin Oral Implants Res. 2001;12:358–363. doi: 10.1034/j.1600-0501.2001.012004358.x. [DOI] [PubMed] [Google Scholar]
- 9.Trisi P, Rao W, Rebaudi A. A histometric comparison of smooth and rough titanium implants in human low-density jawbone. Int J Oral Maxillofac Implants. 1999;14:689–698. [PubMed] [Google Scholar]
- 10.Bergkvist G, Koh KJ, Sahlholm S, Klintstrom E, Lindh C. Bone density at implant sites and its relationship to assessment of bone quality and treatment outcome. Int J Oral Maxillofac Implants. 2010;25:321–328. [PubMed] [Google Scholar]
- 11.Marquezan M, Osorio A, Sant'Anna E, Souza MM, Maia L. Does bone mineral density influence the primary stability of dental implants? A systematic review. Clin Oral Implants Res. 2012;23:767–774. doi: 10.1111/j.1600-0501.2011.02228.x. [DOI] [PubMed] [Google Scholar]
- 12.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Metaanalysis. London, UK: John Wiley & Sons Ltd; 2009. [Google Scholar]
- 13.Wilmes B, Drescher D. Impact of bone quality, implant type, and implantation site preparation on insertion torques of mini-implants used for orthodontic anchorage. Int J Oral Maxillofac Surg. 2011;40:697–703. doi: 10.1016/j.ijom.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 14.Cha JY, Kil JK, Yoon TM, Hwang CJ. Miniscrew stability evaluated with computerized tomography scanning. Am J Orthod Dentofacial Orthop. 2010;137:73–79. doi: 10.1016/j.ajodo.2008.03.024. [DOI] [PubMed] [Google Scholar]
- 15.Cehreli S, Arman-Ozcirpici A. Primary stability and histomorphometric bone-implant contact of self-drilling and self-tapping orthodontic microimplants. Am J Orthod Dentofacial Orthop. 2012;141:187–195. doi: 10.1016/j.ajodo.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 16.Cehreli S, Yilmaz A, Arman-Ozcirpici A. Cortical bone strains around straight and angulated immediate orthodontic microimplants: a pilot study. Implant Dent. 2013;22(2):133–137. doi: 10.1097/ID.0b013e31827b96c2. [DOI] [PubMed] [Google Scholar]
- 17.Huja SS, Litsky AS, Beck FM, Johnson KA, Larsen PE. Pull-out strength of monocortical screws placed in the maxillae and mandibles of dogs. Am J Orthod Dentofacial Orthop. 2005;127:307–313. doi: 10.1016/j.ajodo.2003.12.023. [DOI] [PubMed] [Google Scholar]
- 18.McManus MM, Qian F, Grosland NM, Marshall SD, Southard TE. Effect of miniscrew placement torque on resistance to miniscrew movement under load. Am J Orthod Dentofacial Orthop. 2011;140:e93–e98. doi: 10.1016/j.ajodo.2011.04.017. [DOI] [PubMed] [Google Scholar]
- 19.Migliorati M, Benedicenti S, Signori A, et al. Miniscrew design and bone characteristics: an experimental study of primary stability. Am J Orthod Dentofacial Orthop. 2012;142:7. doi: 10.1016/j.ajodo.2012.03.029. [DOI] [PubMed] [Google Scholar]
- 20.Motoyoshi M, Yoshida T, Ono A, Shimizu N. Effect of cortical bone thickness and implant placement torque on stability of orthodontic mini-implants. Int J Oral Maxillofac Implants. 2007;22(5):779–784. [PubMed] [Google Scholar]
- 21.Motoyoshi M, Uemura M, Ono A, et al. Factors affecting the long-term stability of orthodontic mini-implants. Am J Orthod Dentofacial Orthop. 2010;137:588.e1–588.e5. doi: 10.1016/j.ajodo.2009.05.019. [DOI] [PubMed] [Google Scholar]
- 22.Nienkemper M, Wilmes B, Panayotidis A, et al. Measurement of mini-implant stability using resonance frequency analysis. Angle Orthod. 2013;83:230–238. doi: 10.2319/043012-354.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salmoria KK, Tanaka OM, Guariza-Filho O, Camargo ES, de Souza LT, Maruo H. Insertional torque and axial pull-out strength of mini-implants in mandibles of dogs. Am J Orthod Dentofacial Orthop. 2008;133:790 e15–e22. doi: 10.1016/j.ajodo.2007.12.020. [DOI] [PubMed] [Google Scholar]
- 24.Su YY, Wilmes B, Honscheid R, Drescher D. Application of a wireless resonance frequency transducer to assess primary stability of orthodontic mini-implants: an in vitro study in pig ilia. Int J Oral Maxillofac Implants. 2009;24:647–654. [PubMed] [Google Scholar]
- 25.Motoyoshi M, Hirabayashi M, Uemura M, Shimizu N. Recommended placement torque when tightening an orthodontic mini-implant. Clin Oral Implants Res. 2006;17:109–114. doi: 10.1111/j.1600-0501.2005.01211.x. [DOI] [PubMed] [Google Scholar]
- 26.Neto J. Ethics in research. In: Estrela C, editor. Scientific Methodology. São Paulo, Brazil: Artes Médicas; 2001. pp. 00–00. [Google Scholar]
- 27.Lim SA, Cha JY, Hwang CJ. Insertion torque of orthodontic miniscrews according to changes in shape, diameter and length. Angle Orthod. 2008;78:234–240. doi: 10.2319/121206-507.1. [DOI] [PubMed] [Google Scholar]
- 28.Chaddad K, Ferreira AF, Geurs N, Reddy MS. Influence of surface characteristics on survival rates of mini-implants. Angle Orthod. 2008;78:107–113. doi: 10.2319/100206-401.1. [DOI] [PubMed] [Google Scholar]
- 29.Meursinge Reynders RA, Ronchi L, Ladu L, van Etten-Jamaludin F, Bipat S. Insertion torque and success of orthodontic mini-implants: a systematic review. Am J Orthod Dentofacial Orthop. 2012;142:596–614.e5. doi: 10.1016/j.ajodo.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 30.Schatzle M, Golland D, Roos M, Stawarczyk B. Accuracy of mechanical torque-limiting gauges for mini-screw placement. Clin Oral Implants Res. 2010;21:781–788. doi: 10.1111/j.1600-0501.2010.01927.x. [DOI] [PubMed] [Google Scholar]
- 31.DaMatta RA. Animal models in biomedical research. Scientia Medica. 2010;20:210–211. [Google Scholar]