Abstract
Objective:
To evaluate the effect of different bracket types on the levels of Streptococcus mutans (SM) and Lactobacillus (LB) in saliva, in plaque, and on the periodontal condition.
Materials and Methods:
Forty patients aged 14 to 16 years, who had Angle Class I malocclusion with minimal crowding, were nonsmokers, were without systematic disease, and did not use antibiotics or oral mouth rinses during the 3-month period before the study were randomly selected. The patients were subdivided into two groups with random allocation of bracket type: conventional brackets (CB; Avex Mx, OPAL orth.) with steel wire ligature or self-ligating brackets (SLB; F1000, Leone S.p.A.). Microbial and periodontal records were obtained before bonding (T1) and 1 month after bonding (T2). Microbial samples were collected from the stimulated saliva and the plaque from the labial surfaces of the upper and lower lateral incisors. To estimate the number of colony-forming units of SM and LB, Dentocult SM and LB kits were used. The plaque index (PI), gingival index (GI), and pocket depth (PD) values were recorded to evaluate the periodontal condition. Paired t-test and Mann-Whitney U-test were used to compare the groups statistically.
Results:
No significant differences occurred in SM or LB colonization between the groups. In the SLB group, PI, GI, and PD values increased significantly (P < .05). A greater increase was found in PD value in the SLB group (0.98 mm) compared with the CB group (0.04 mm; P < .05).
Conclusions:
The F1000 SLB do not have an advantage over Avex Mx CB with respect to periodontal status and colonization of SM and LB.
Keywords: Microbial colonization, Periodontal status, Self-ligating brackets, Conventional brackets, Dentocult kits
INTRODUCTION
Fixed orthodontic appliances with the presence of brackets and ligatures create new retention areas for microbial dental plaque that is reported to be the most important etiologic factor in periodontal inflammation and decalcification of enamel.1–4 In conjunction with poor oral hygiene, the number and percentage of oral microorganisms are increasing during fixed orthodontic treatment.5,6 Among other species, Streptococcus mutans (SM) and Lactobacillus (LB) bacteria, which have been identified with high concentration in oral flora and have higher adhesion capacity on brackets, play important roles in the initiation and progression of dental caries.7–9
The effects of bracket materials, designs and different ligations on the levels of cariogenic bacteria and periodontal destruction have been evaluated by several studies.4,10–15 Among bracket ligation types, self-ligating brackets (SLB) were expected to have better values for periodontal status because of the lack of ligature materials and fewer retentive sites.4 On the contrary, others16,17 have mentioned that this theoretical advantage may be eliminated in reality, where SLB consist of opening and closing mechanisms that may provide additional plaque retention sites.
There are few studies in the literature with diverse results comparing SLB with elastomeric ligated conventional brackets (CB).18–23 Some researchers have reported that elastomeric ligated CB cause more plaque accumulation and periodontal inflammation than SLB,6,18,19 whereas others reported no significant difference.20 On the contrary, higher bacterial colonization and poorer periodontal health with SLB was also reported.21
On the other hand, there is no clinical study to our knowledge evaluating the effects of SLB and CB with wire ligation on oral microbiota and periodontal status. Thus, this prospective study was performed to investigate the effect of fixed orthodontic treatment with SLB and CB with steel ligatures on the colonization of SM and LB in saliva, in plaque, and on the status of periodontal health. The null hypothesis assumed that bracket type has no effect on these parameters.
MATERIALS AND METHODS
Forty patients (29 female, 11 male) between the ages of 14 and 16 years were randomly selected from among the patients scheduled for orthodontic treatment in the orthodontic department of the university according to the following inclusion criteria: permanent dentition, Angle Class I malocclusion with minimal crowding, nonsmoker, and without periodontal and systematic disease. Patients who had used antibiotics and oral mouth rinses during the 3-month period before the study were excluded. Patients used standardized fluoridated toothpaste and toothbrush and were asked not to use other oral hygiene supplements during the study. Oral hygiene instructions were given to all patients 1 week before the beginning of treatment.
This study was approved by the Ethics Committee of the University. All patients/parents were informed, and their consent was given prior to entering the study.
It is inferred that a mean colony-forming unit (CFU) difference of approximately one score (standard deviation = approximately 1) will result in a clinically significant increase in SM and LB counts. Although a sample size of 16 patients per group, at α = .05, yields a statistical power very close to .80 for this study, the sample size was increased to 20 patients per group.
Patients were subdivided into two groups with random allocation of bracket type as follows: group 1: conventional (CB; Avex Mx, 0.022-inch, OPAL orth, South Jordan, Utah; n = 20; Figure 1) and group 2: SLB (F1000, 0.022-inch, Leone SpA, Sesto Fiorentino, Firenza, Italy; n = 20; Figure 2). CBs were ligated with 0.010-inch stainless-steel wire.
Figure 1.
Avex Mx conventional brackets.
Figure 2.
F1000 Self-ligating brackets.
Microbial and periodontal records were obtained before upper and lower arch bonding (T1) and 1 month after bonding (T2), which is the time for the appointment to change the first arch wires. All microbial and periodontal records were collected by a single calibrated periodontist; a complete periodontal examination was performed by means of a Williams probe. Periodontal examination included the plaque index (PI), gingival index (GI), and probing pocket depth (PD) measurements at four sites (mesial, midbuccal, distal, and palatinal/lingual) for all teeth.24 PD was recorded as the distance from the gingival margin to the most apical part of the sulcus. Periodontal indices were calculated as a sum of mean scores by each examined tooth divided by the number of evaluated teeth. A mean of all measurements for each patient was considered.
Microbiological analysis was performed by obtaining a sample of stimulated saliva and supragingival dental plaque. The subjects had refrained from eating, drinking, brushing teeth, and chewing gum for at least 2 hours before taking the samples. Sample collection was performed between 8.30 am and 10.30 am. Collection of saliva and supragingival plaque samples was performed before any oral examination or manipulation so as not to disrupt the oral microbiota.
To estimate the number of colony-forming units of SM and LB per milliliter of saliva and supragingival dental plaque, Dentocult SM and LB kits (Orion Diagnostica, Espoo, Finland) were used.
Dentocult SM strip mutans was used to detect SM in stimulated saliva and plaque. Plaque samples were collected from the labial surfaces immediately surrounding the orthodontic brackets of the maxillary and mandibular lateral incisors with a sterilized different dental scaler with the same tip dimensions for each lateral tooth (≠ 8/9 Orban DE hoe scaler, Hu-Friedy, Chicago, Ill). Each sampled site was isolated from saliva contamination with cotton rolls and dried with air, and a four-pass technique was used to move the instrument tip around the circumference of the bracket at the bracket-tooth interface.
For collecting stimulated saliva, patients were instructed to chew a paraffin pellet for 1 to 5 minutes. Saliva produced during the first minute was collected for detection of SM, and then excess saliva was swallowed. The rough surface of the SM strip was pressed against the saliva remaining on the patient's tongue and removed through the gently closed lips. For LB detection, during the following 4 minutes, patients were asked to collect stimulated saliva in the mouth and to expectorate approximately 3 mL of saliva into a chilled empty Petri dish. The collected saliva was poured over both agar surfaces.
SM and LB slides were incubated at room temperature in an upright position for 7 days. The vials were labeled as per their lot numbers.
Interpretation of Results
The presence of SM was confirmed by detection of light-blue to dark-blue raised colonies on the inoculated surface of the strip. However, after incubation of LB, they are visible as white-to-transparent colonies raised on the modified Rogosa agar surface. The density of SM and LB in saliva and plaque was obtained by comparing the colony density on the test strips with the model charts.
The growth densities of SM were categorized as follows: (CFU/mL) 0 = negative or <104 CFU/mL, 1 = <105 CFU/mL, 2 = 105–106 CFU/mL, and 3 = >106 CFU/mL. The growth densities of LB were categorized as follows (CFU/mL): 0 = no count or 103 CFU/mL, 1 = 104 CFU/mL, 2 = 105 CFU/mL, and 3 = 106 CFU/mL.
Statistical Analysis
Bonferroni-corrected Wilcoxon signed-rank tests were used to compare the changes of the periodontal parameters in 1 month within the groups. Mann-Whitney U-test and Student's t-tests were used to compare the results between the groups. P < .05 was considered significant. Related tests were performed by SPSS 15.0 (SPSS Inc, Chicago, Ill). The microbiological measurements were analyzed as a two-way factorial repeated-measures design (with the factors being group and time [1, 2]) using nonparametric methods as defined by Brunner and Langer.25
Demographic characteristics of the sample were investigated with conventional descriptive statistics. Differences of means were determined with the t-test; differences in proportion were studied with the chi-square test.
RESULTS
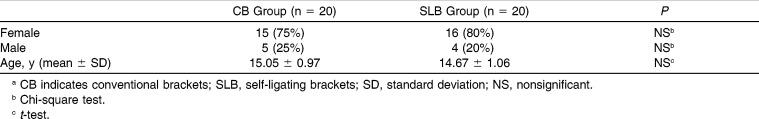
The distribution of gender and age did not differ between the two bracket groups (Table 1). Also, no significant differences were found in pretreatment values of the parameters between the groups (Tables 2 and 3). The results of the statistical analysis of the periodontal indexes scores and microbiological counts of the groups are shown in Tables 2 and 3.
Table 1.
Demographic Characteristics of the Study Cohorts and Comparisons Between Two Groups Based on Chi-Square Test and t-Testa
Table 2.
Periodontal Measurements at the Beginning (T1) and 1 Month After Bonding (T2) and Comparisons of Intra- and Intergroup Differences Based on Nonparametric and Parametric Testsa
Table 3.
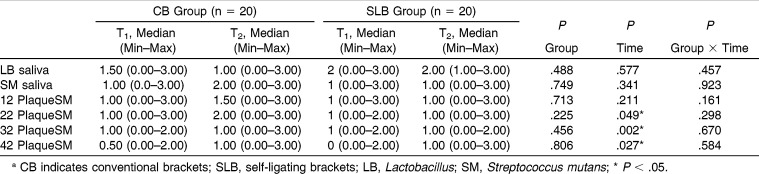
Comparisons of Bacterial Colonizations at the Beginning (T1) and 1 Month After Bonding (T2)a
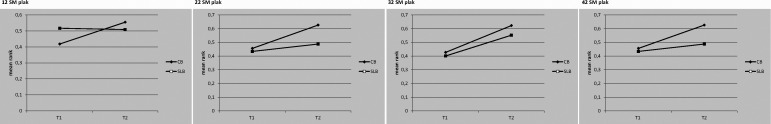
Between the two groups, statistical analysis showed no difference with respect to SM and LB counts (Table 3; Figures 3 and 4).
Figure 3.
Mean ranks of Streptococcus mutans and Lactobacillus counts in saliva samples in the self-ligating bracket and conventional bracket groups at the beginning and 4 weeks after bonding.
Figure 4.
Mean ranks of Streptococcus mutans counts in plaque samples in the self-ligating bracket and conventional bracket groups at the beginning and 4 weeks after bonding.
Although during the 1-month period PI, GI, and PD scores increased in both groups, these increases were found to be significant only in the SLB group (P < .05). A statistically significant difference was found only in PD values between the groups (P < .05; Table 2).
DISCUSSION
To estimate the most hygienic bracket system, SLB and CB with stainless-steel ligature were compared in the present study, as no previous study was found in the literature. Microbial and periodontal records were obtained before upper and lower arch bonding (T1) and 1 month after bonding (T2), which is the time for the appointment to change the first arch wires. The study was terminated on the fourth week as longer periods of observation may affect the results because cooperation, motivation for oral hygiene, and dietary habits can change, as reported by Türkkahraman et al.6
Periodontal Condition
At the beginning of the study, the results showed minimum values that indicated healthy periodontia for all indices. No significant differences were found between the groups at the beginning. This result might be due to the positive effects of oral hygiene instructions given so as to prevent the detrimental effects of orthodontic treatment on periodontal health a weak before placement of the brackets.4,6,26,27 On the other hand, in severe crowding the hygiene supplement may not be enough; in this study, patients with minimal crowding were selected so as to eliminate the effect of crowding.
In the short time period of 1 month, placement of fixed appliances caused increased plaque accumulation, PD, and gingival inflammation in both groups, although these increases were significant only in the SLB group. An increase in PD values was found to be significantly different between the two ligation systems. This might be pseudo PD due to bracket design, size, and the proximity of the gingival margin to the bracket. The SLB used in this study were larger in size than the CB, so both the enamel surface and the distance between the brackets and gingiva were reduced, which may worsen cleanability.
The expectation of better values for periodontal indices in the SLB group was not achieved. Our finding is in accordance with the results of Van Gastel et al.,21 who reported significant alterations in both periodontal and microbiological parameters with the self-ligating speed brackets, and in conflict with the results of Pandis et al.,16 who found no difference in PI, GI, or PD between In-Ovation-R SLB and Microarch CB with elastomeric ligation in which periodontal evaluation was performed after completion of the alignment in the mandibular incisors to eliminate the effect of crowding. Our results may not be considered as comparable with those of Pandis et al.,16 as during the leveling phase, the oral microbiota starts to change, individual reactions begin, and the real effect of the brackets may not be evaluated properly. Our findings are also in conflict with the results of Nalçacı et al.,22 in which the Damon Q SLB group showed better values for the periodontal parameters than the group with Mini-Taurus CB with elastomeric ligation.
Microbiologic Evaluation
The number of colony-forming units of SM and LB per milliliter of saliva and plaque was estimated by Dentocult SM and LB kits as simple and easy chairside methods. The plaque samples were taken from maxillary and mandibular lateral incisors, as they were assumed to have the highest incidence of white spot formation.3,16,19
In both groups, SM colonization was significantly increased in the plaque sample taken from the upper and lower left lateral incisors and lower right lateral incisor (SM 22, 32, 42). It was reported that reduced crown width and small overall teeth sizes contributed to the increase in the plaque accumulation rate on the mandibular anterior teeth.16 All patients were right-handed brushers, and the right sides may not be brushed properly.
LB and SM counts in saliva and plaque were not significantly different between the tested bracket groups. This result is in contrast with results of Pellegrini et al.19 and Mummola et al.,23 who found lower levels of bacteria with the SLB than with elastomeric ligating brackets. In conflict with this, van Gastel et al.21 found higher bacterial colonization with SLB. In accordance with this, Nalçaçı et al.22 and Pandis et al.20 reported no difference in the levels of SM in saliva between elastomeric ligated CB and SLB. The researchers20 claimed that the pretreatment levels of SM are significant predictors of SM levels after placement of brackets. In accordance with this finding, the oral hygiene instructions before the treatment might reduce the levels of SM in this study. In addition, there might be plaque and food impactions in the space under the closing mechanism that could not be brushed by the patient without opening the mechanism. Thus, the expected advantage may not be achieved in reality.16
In the SLB group, as with the findings of Carillo et al.,18 there were no significant differences in SM and LB levels in the 1-month treatment period; however, destruction in periodontal health occurred. Another study demonstrated that 1 week following bonding, the patients with SLB presented higher colonizations of anaerobic and aerobic bacteria and increased gingival hypertrophy relative to CB, but no difference was observed in bleeding on probing between the two groups.21
The differences noted between the results of the present study and the others may relate to differences in sample size, sample teeth, registration times, microbiological methods, variations in the design and sizes of the brackets, methodological differences, types of ligation, bonding procedures,26,27 the level of oral hygiene, and the ages of the subjects.28
In the light of these findings, the expected beneficial effect of the SLB is not confirmed. Even though the SLB eliminate the use of ligatures, they consist of opening and closing mechanisms, which may provide additional plaque retention sites. The results of the present study suggest that bracket type may not have a significant effect on bacterial colonization on orthodontic appliances. This might be due to oral hygiene education given at the early stages of orthodontic treatment. This result agrees with several literature reports emphasizing the main role of the oral hygiene.26,28
CONCLUSIONS
A greater increase was found in PD value in the SLB group. The SLB do not have an advantage over CB with respect to the periodontal status and colonization of SM and LB.
Dentocult tests are simple and easy chairside methods that could be used in the orthodontic profession.
REFERENCES
- 1.Atack NE, Sandy JR, Addy M. Periodontal and microbiological changes associated with the placement of orthodontic appliances: a review. J Periodontol. 1996;57:78–85. doi: 10.1902/jop.1996.67.2.78. [DOI] [PubMed] [Google Scholar]
- 2.Balansefien JW, Madonia JV. Study of dental plaque in orthodontic patients. J Dent Res. 1970;49:320–324. doi: 10.1177/00220345700490022101. [DOI] [PubMed] [Google Scholar]
- 3.Gorelick L, Geiger AM, Gwinnet AJ. Incidence of white spot formation after banding and bonding. Am J Orthod. 1982;81:93–98. doi: 10.1016/0002-9416(82)90032-x. [DOI] [PubMed] [Google Scholar]
- 4.Qgaard B, Rolla G, Arends J. Orthodontic appliances and enamel demineralization. Part 1: lesion development. Am J Orthod. 1998;94:68–73. doi: 10.1016/0889-5406(88)90453-2. [DOI] [PubMed] [Google Scholar]
- 5.Naranjo AA, Trivino ML, Jaramillo A, Betancourth M, Botero JE. Changes in the subgingival microbiota and periodontal parameters before and 3 months after bracket placement. Am J Orthod Dentofacial Orthop. 2006;130:275.e17–22. doi: 10.1016/j.ajodo.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 6.Türkkahraman H, Sayın O, Bozkurt Y, Yetkin Z, Kaya S, Onal S. Archwire ligation techniques, microbial colonization, and periodontal status in orthodontically treated patients. Angle Orthod. 2005;75:231–236. doi: 10.1043/0003-3219(2005)075<0227:ALTMCA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Fournier A, Payant L, Bouclin R. Adherence of Streptococcus mutans to orthodontic brackets. Am J Orthod Dent Orthop. 1998;114:414–417. doi: 10.1016/s0889-5406(98)70186-6. [DOI] [PubMed] [Google Scholar]
- 8.Rosenbloom RG, Tinanoff N. Salivary Streptococcus mutans levels in patients before, during and after treatment. Am J Orthod. 1991;100:35–37. doi: 10.1016/0889-5406(91)70046-Y. [DOI] [PubMed] [Google Scholar]
- 9.Jenatschke F, Elsenberger E, Welte HD, Schlagenhauf U. Influence of repeated chlorhexidine varnish applications on mutans streptococci counts and caries increment in patients treated with fixed orthodontic appliances. J Orofac Orthop. 2001;62:136–145. doi: 10.1007/pl00001917. [DOI] [PubMed] [Google Scholar]
- 10.Jurela A, Repic D, Pejda S, et al. The effect of two different bracket types on the salivary levels of S mutans and S sobrinus in the early phase of orthodontic treatment. Angle Orthod. 2013;83:140–145. doi: 10.2319/030612-187.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Papaioannou W, Gizani S, Nassika M, Kontou E, Nakou M. Adhesion of Streptococcus mutans to different types of brackets. Angle Orthod. 2007;77:1090–1095. doi: 10.2319/091706-375.1. [DOI] [PubMed] [Google Scholar]
- 12.Ahn SJ, Lee SJ, Lim BS, Nahm DS. Quantitative determination of adhesion patterns of cariogenic streptococci to various orthodontic brackets. Am J Orthod Dentofacial Orthop. 2007;132:815–821. doi: 10.1016/j.ajodo.2005.09.034. [DOI] [PubMed] [Google Scholar]
- 13.Forsberg CM, Brattstrom V, Malmberg E, Nord CE. Ligature wires and elastomeric rings: two methods of ligation, and their association with microbial colonization of Streptococcus mutans and lactobacilli. Eur J Orthod. 1991;13:416–420. doi: 10.1093/ejo/13.5.416. [DOI] [PubMed] [Google Scholar]
- 14.Ristic M, Vlahovic Svabic M, Sasic M, Zelic O. Clinical and microbiological effects of fixed orthodontic appliances on periodontal tissues in adolescents. Orthod Craniofacial Res. 2007;10:187–195. doi: 10.1111/j.1601-6343.2007.00396.x. [DOI] [PubMed] [Google Scholar]
- 15.Attin R, Thon C, Schlagenhauf U, et al. Recolonization of mutans streptococci on teeth with orthodontic appliances after antimicrobial therapy. Eur J Orthod. 2005;27:489–493. doi: 10.1093/ejo/cji018. [DOI] [PubMed] [Google Scholar]
- 16.Pandis N, Vlachopoulos K, Polychronopoulou A, Madianos P, Eliades T. Periodontal condition of the mandibular anterior dentition in patients with conventional and self-ligating brackets. Orthod Craniofac Res. 2008;11:211–215. doi: 10.1111/j.1601-6343.2008.00432.x. [DOI] [PubMed] [Google Scholar]
- 17.Garcez AS, Suzuki SS, Riberio MS, et al. Biofilm retention by 3 methods of ligation on orthodontic brackets: a microbiologic and optical coherence tomography analysis. Am J Orthod Dentofacial Orthop. 2011;140:e193–e198. doi: 10.1016/j.ajodo.2011.04.019. [DOI] [PubMed] [Google Scholar]
- 18.Carillo LE, Montiel-Bastida NM, Sanchez-Perez L, Alanis-Tavira J. Effect of orthodontic treatment on saliva, plaque and the levels of Streptococcus mutans and Lactobacillus. Med Oral Patol Oral Cir Bucal. 2010;15:924–929. doi: 10.4317/medoral.15.e924. [DOI] [PubMed] [Google Scholar]
- 19.Pellegrini P, Sauerwein R, Finlayson T, et al. Plaque retention by self-ligating vs elastomeric orthodontic brackets: quantitative comparison of oral bacteria and detection with adenosine triphosphate-driven bioluminescence. Am J Orthod Dentofacial Orthop. 2009;135:426.e1–9. doi: 10.1016/j.ajodo.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 20.Pandis N, Papaioannou W, Kontou E, Nakou M, Makou M, Eliades T. Salivary Streptococcus mutans levels in patients with conventional and self-ligating brackets. Eur J Orthod. 2010;32:94–99. doi: 10.1093/ejo/cjp033. [DOI] [PubMed] [Google Scholar]
- 21.van Gastel J, Quirynen M, Teughels W, Coucke W, Carels C. Influence of bracket design on microbial and periodontal parameters in vivo. J Clin Periodontol. 2007;34:423–431. doi: 10.1111/j.1600-051X.2007.01070.x. [DOI] [PubMed] [Google Scholar]
- 22.Nalçacı R, Özat Y, Çokakoğlu S, Türkkahraman H, Önal S, Kaya S. Effect of bracket type on halitosis, periodontal status and microbial colonization [Epub ahead of print] Angle Orthod. 2013 doi: 10.2319/061913-461.1. dx.doi.org/10.2319/061913-461.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mummola S, Marchetti E, Giuca MR, et al. In-office bacteria test for a microbial monitoring during the conventional and self-ligating orthodontic treatment. Head Face Med. 2013;9:7. doi: 10.1186/1746-160X-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Löe H. The gingival index, plaque index and the retention index system. J Periodontol. 1967;38:610–616. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 25.Brunner E, Langer F. Nonparametric analysis of ordered categorical data in designs with longitudinal observations and small sample sizes. Biometrical Journal. 2000;42:663–675. [Google Scholar]
- 26.Amasyalı M, Enhos S, Uysal T, Saygun I, Kilic A, Bedir O. Effect of a self-etching adhesive containing an antibacterial monomer on clinical periodontal parameters and subgingival microbiologic composition in orthodontic patients. Am J Orthod Dentofacial Orthop. 2011;140:147e–e153. doi: 10.1016/j.ajodo.2011.02.022. [DOI] [PubMed] [Google Scholar]
- 27.Sukontapatipark W, El-Agroudi M, Selliseth NJ, Thunold K, Selvig KA. Bacterial colonization associated with fixed orthodontic appliances: a scanning electron microscopy study. Eur J Orthod. 2001;23:475–484. doi: 10.1093/ejo/23.5.475. [DOI] [PubMed] [Google Scholar]
- 28.Smiech-Slomkowska G, Jablonska-Zrobek J. The effect of oral health education on dental plaque development and the level of caries-related Streptococcus mutans and Lactobacillus spp. Eur J Orthod. 2007;29:157–160. doi: 10.1093/ejo/cjm001. [DOI] [PubMed] [Google Scholar]