Abstract
Objective
To evaluate the reliability and validity of a standardized ultrasound examination protocol for measuring vastus lateralis muscle size.
Design
Prospective cohort study.
Subjects
Sixteen staff members of the university hospital of Heidelberg.
Methods
Muscle thickness, cross-sectional area and subcutaneous adipose tissue thickness were measurxsed at 3 standardized sites on the right and left vastus lateralis muscle. Ultrasound measurements were collected by 2 independent investigators on 2 different days and compared with magnetic resonance imaging measurements.
Results
Intraclass correlation coefficients (ICC) for intra- and inter-rater reliability showed very good closeness of agreement for all parameters (ICC = 0.929–0.994, p < 0.001). Muscle thickness and subcutaneous adipose tissue thickness ultrasound and magnetic resonance imaging measurements revealed good to very good closeness of agreement (ICC = 0.835–0.969, p < 0.001), whereas cross-sectional area showed only average closeness of agreement (ICC = 0.727, p < 0.001). A strong predictive positive correlation for ultrasound and magnetic resonance imaging-based measurements of cross-sectional area was found (R² = 0.793, p < 0.001).
Conclusion
By standardization of an examination protocol, quantitative vastus lateralis muscle ultrasound proved to be a reliable method for assessing vastus lateralis muscle size. Furthermore, this protocol is valid for measuring muscle thickness and subcutaneous adipose tissue thickness, although there seems to be a systematic underestimation of cross-sectional area depending on subcutaneous adipose tissue thickness.
LAY ABSTRACT
The quantification of muscle mass is crucial for diagnosis and monitoring of muscle atrophy caused by inactivity or in the context of diseases, and could also be used for monitoring the development of muscle hypertrophy during resistance training. Application of a standardized examination protocol for quantitative vastus lateralis muscle ultrasound proved to be a reliable method for assessing vastus lateralis muscle size in people with varying body weight and body composition, respectively. In this regard, it could be considered an alternative examination tool to time- and cost-consuming gold-standard magnetic resonance imaging (MRI), which is seldom readily available in clinical practice. However, compared with MRI measurements, muscle cross-sectional area measured using ultrasound seems to be systematically underestimated, depending on subcutaneous adipose tissue thickness.
Key words: diagnostic imaging, ultrasound, magnetic resonance imaging, skeletal muscle, quadriceps muscle, subcutaneous fat, sarcopaenia, hypertrophy
The quantification of muscle mass is crucial for the diagnosis and monitoring of muscle atrophy caused by inactivity or in the context of diseases, and could also be used for monitoring the development of muscle hypertrophy during resistance training. Magnetic resonance imaging (MRI) and computer tomography (CT) are currently considered the “gold-standard” techniques for assessment of muscle size (1, 2). However, due to radiation exposure (CT), long examination times (MRI), high cost and limited availability, both methods are inappropriate for frequent and routine use in clinical practice. Dual energy X-ray absorptiometry (DEXA) and bioelectrical impedance analysis represent further examination methods. However, several external factors, such as hydration status, obesity, or recent physical activity, can affect the results (3). Therefore, muscle ultrasound is considered an available, safe, cost-efficient and quick alternative to assess skeletal muscle size (4, 5). To date, in both elderly people and younger populations, few studies have shown good reliability and validity of muscle ultrasound compared with MRI, CT or DEXA (6, 7). However, the method of quantitative muscle ultrasound has not been established to date, mostly because of the lack of a standardized examination protocol (6). Apart from the non-specified scanning procedure in most of these studies, there were differences in the specific skeletal muscle being investigated (e.g. rectus femoris, vastus lateralis (VL), gastrocnemius, anterior thigh, biceps brachii), the transducer type (linear or curved) and the parameter used for muscle quantification (e.g. thickness, volume, cross-sectional area).
Consequently, routine or systematic use of quantitative muscle ultrasound is rare. In addition to monitoring of strength training in clinical studies or in competitive sports, muscle ultrasound may also be used as a rapid measuring tool for muscle size in clinical practice. In particular, the screening and assessment of sarcopaenia, which is characterized by loss of skeletal muscle mass and muscle function (8), is an interesting operational area for quantitative muscle ultrasound. Sarcopaenia is associated with limited mobility, reduced quality of life and increased mortality (8), but is often unrecognized. Not only with ageing, but also in patients with chronic diseases, such as heart failure or chronic obstructive pulmonary disease (COPD), the incidence of sarcopaenia is significantly increased (9–11). Due to its functional significance in daily life, and consequently being affected by physical activity or inactivity (12), the VL could serve as the ideal index muscle for diagnosis and monitoring of skeletal muscle atrophy or hypertrophy.
In this study, it was hypothesized that the ultrasonographic measurements of muscle thickness (MT) and cross-sectional area (CSA) of the VL following a standardized examination protocol are reproducible, investigator-independent and comparable to the results of MRI measurements.
METHODS
Subjects
Sixteen subjects (7 males, mean age 33.4 years (standard deviation (SD) 10.7), height 182.3 cm (SD 7.0), weight 80.4 kg (SD 12.5) ; body mass index (BMI) 24.1 kg/m2 (SD 2.4), range 22.2–29.2 kg/m2; 9 females, mean age 46.8 years (SD 11.5), height 164.7 cm (SD 4.0), weight 66.3 kg (SD 12.9); BMI 24.3 kg/m2 (SD 3.8), range 19.5–32.2 kg/m2) volunteered to participate in the study. The subjects were allowed to be physically active, but none of them participated in competitive sports. Each participant received a detailed explanation of the study and provided written conform consent before participation. The study was approved by the local ethics committee and conducted in accordance with the Declaration of Helsinki.
Experimental design
Each participant reported to the ultrasound laboratory twice a week. On these occasions, right and left VL was quantified each by 2 independent investigators. On either the first or second visit, MRI measurements of both VL were performed.
Ultrasonography
Two different investigators scanned both the right and left VL of each subject twice on 2 different days within 1 week. Subjects were asked not to perform intensive physical exercise the day before or on the day of measurement. A Vivid E9 ultrasound scanner (GE Healthcare GmbH, Solingen, Germany), fitted with a 5-cm linear transducer (GE 9L 2.5–9.5 MHz), was used for measurements. Subjects were placed in the supine position with a soft roll below the hollow of their knees and were instructed to relax their leg muscles during the entire examination.
Examination procedure
With some alterations the procedure was based on the publication of Ticinesi et al., who proposed an operative protocol to assess sarcopaenia with VL ultrasound (13). From the middle of the upper patella pole, distances of 10, 15 and 20 cm towards the anterior superior iliac spine were marked on the skin using a flexible tape-measure. On each measurement site, the medial and lateral edges of the VL belly were identified by ultrasound. Then, again, a flexible tape-measure was used to connect the medial and lateral edge of VL by drawing a line and marking the mid-point of this distance. This point was defined as the reference point for each measurement site (10, 15 and 20 cm proximal to the upper patella pole).
At each reference point, 3 fixed images of the VL were taken. Therefore, the probe was oriented longitudinally (in line with the thigh bone), with the reference point matching the mid-point of the active part of the linear probe. Slight tilting movements were used to obtain a clear definition of the rim of the thigh bone in order to ensure that standardized perpendicular images were obtained (Fig. 1). Great care was taken to use sufficient contact gel and to be consistent in applying minimal pressure during scanning. After taking each image, the probe was repositioned. The images obtained with this procedure were used to measure MT and subcutaneous adipose tissue thickness (SAT).
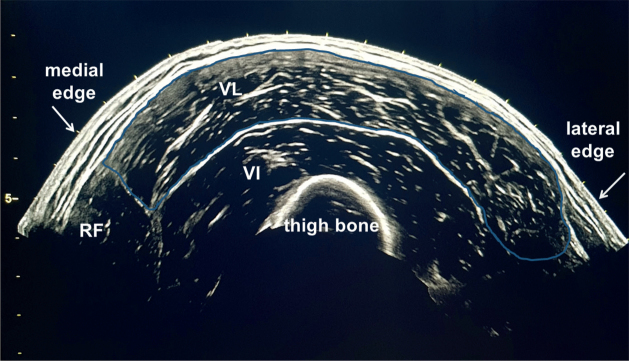
Fig. 1.
Representative fixed ultrasound image measuring muscle thickness (MT) vertically between the superficial aponeurosis (SA) and deep aponeurosis (DA). Subcutaneous adipose tissue thickness (SAT) was measured vertically between cutis and SA. VI: vastus intermedius muscle.
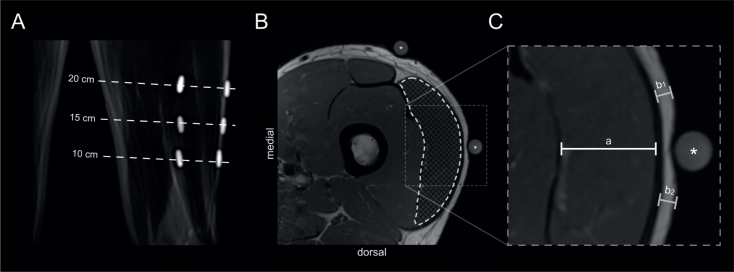
For measuring muscle CSA, the extended field of view (EFOV) software (LOGIQview, GE Healthcare GmbH) was used, reconstructing panoramic images of the VL belly. For this purpose, the probe was set perpendicular to the thigh bone and along the earlier marked connecting line visualizing the medial edge of the VL as a starting position. Then, the EFOV software was activated and the probe was moved along the line to the lateral edge of VL at a constant velocity and with minimal pressure. At each measurement site, at least 3 images were obtained and selected, sorting out unsuccessful or unclear images.
The procedure was similarly performed for the right and left VL.
Analysis of images
Images were pseudonymized, saved separately for date of examination, investigator and side of leg, and analysed by the 2 investigators in a blinded way, using the clinical Picture Archiving and Communication System (PACS, Centricity Cardiology CA 1000 2.0, GE Medical Systems Information Technologies, GE Healthcare GmbH).
The vertical distance in the middle of the acquired fixed images between the superficial and the deep aponeurosis of the VL was measured to assess MT. In the same way the distance between the cutis and the superficial aponeurosis of the VL was measured to assess SAT (Fig. 1). CSA was assessed in the panoramic images by freehand planimetry of the VL belly within the aponeurosis (Fig. 2). Then, the mean value of the 3 measurements of each parameter was calculated for every measurement site.
Fig. 2.
Representative panoramic ultrasound image measuring cross-sectional area (CSA) of the vastus lateralis muscle (VL) with freehand planimetry inside the aponeurosis (blue-rimmed). RF: rectus femoris muscle; VI: vastus intermedius muscle.
MRI imaging and post-processing
Participants were examined feet first and in a supine position on a 3.0 Tesla magnetic resonance system (Magnetom Prisma-FIT, Siemens Healthcare, Erlangen, Germany) using a 18-channel body coil (Body 18, Siemens Healthcare).
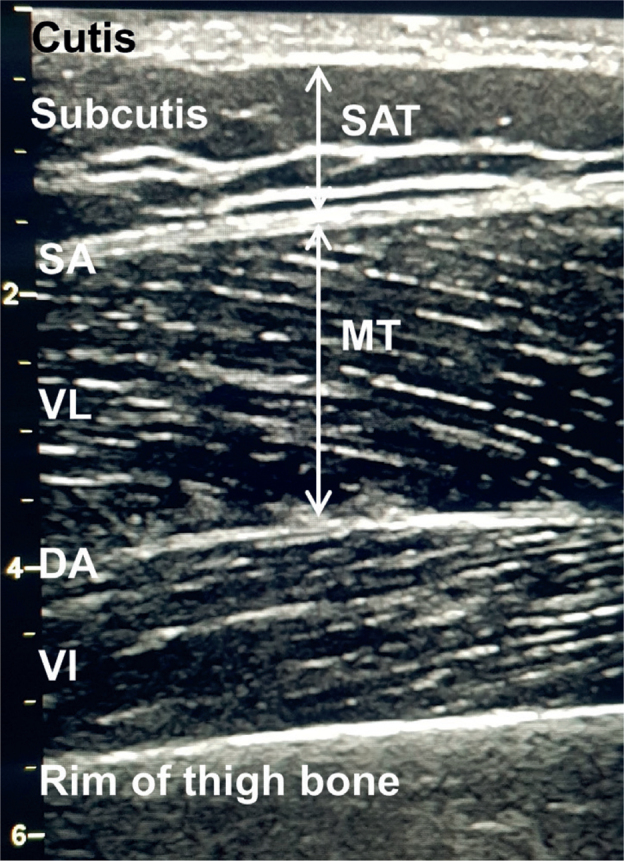
Every measurement site (10, 15 and 20 cm proximal to the upper patellar pole) was marked with 2 fish-oil capsules (Zodin Omega 100 mg, Trommsdorff, Alsdorf, Germany), 1 on the reference point and 1 on the medial edge of VL, to ensure that the measurement site as well as the axial orientation corresponded between MRI and sonography (Fig. 3).
Fig. 3.
Representative images of magnetic resonance imaging (MRI) measurements. (A) A coronal survey scan shows the left leg as an example. Two fish-oil capsules per height were taped onto each thigh to allow for a more precise planning of axial T1-weighted imaging. (B) Measurement of the vastus lateralis muscle cross-sectional area (white dashed line) was performed on an axial slice of interest, in which both fish-oil capsules (asterisk) could be depicted. (C) Inset showing how muscle thickness (MT) (a) and subcutaneous adipose tissue thickness (SAT) are measured. Since the capsule itself led to a slight indentation in the subcutaneous adipose tissue, the thickness of the unaffected neighbouring regions (b1+b2) were measured instead and then averaged to avoid measurement error.
First, coronal and sagittal survey scans were performed to allow for a more precise planning of anatomical T1-weighted sequences (repetition time 8,000 ms, echo time 1,000 ms, field of view 400 × 400 mm2, slice thickness 130 mm, number of slices 1, distance factor 50%, number of averages 2, acquisition time 0 min 18 s). Then, 1 slab of an axial T1-weighted imaging sequence (repetition time 700 ms, echo time 12 ms, field of view 220 × 220 mm2, slice thickness 3.5 mm, number of slices 45, distance factor 10%, number of averages 3, acquisition time 7 min 50 s per slab) was acquired per leg, each covering all 3 measurement sites.
Subsequent image analysis was performed by 1 reader with more than 5 years of experience in neuromuscular imaging using the DICOM-viewer OsiriX MD (Version 11, Pixmeo Sarl, Bernex, Switzerland). For each participant, 6 slices were analysed and, on each, the CSA of VL was calculated by free-hand planimetry. In addition, MT as well as SAT were measured at the equivalent reference point determined in the ultrasound procedure, which was marked with a lateral fish-oil capsule. The reader was blinded to all sonographic measurements.
Statistical analyses
The right and left VL were considered separately, so that the number of cases depending on the particular question constituted at least 32.
Intra-rater and inter-rater reliability of the muscle ultrasound measurements were tested with an intraclass correlation coefficient (ICC) based on a 2-way random effect model, interpreted as described by Koo & Li (14). The validity of the ultrasound measurements compared with MRI were also tested with an ICC, based on a 2-way random effect model, using the mean values of all 4 ultrasound examinations. In a second step, a linear regression model was used to evaluate the correlation between ultrasound-measured CSA and MRI-measured CSA. Furthermore, Spearman’s correlation coefficient r was calculated for ultrasound measured SAT and the particular percentage difference between absolute values of MT and CSA measured by the 2 investigators, at the 2 different days, as well as for the comparison of ultrasound with MRI. Statistical significance was set at p < 0.05. Analyses were performed with the statistical software SPSS (IBM SPSS Statistics 25, SPSS Inc., Chicago, IL, USA). Values are presented as means±standard deviations (SD).
RESULTS
Data regarding intra-rater and inter-rater reliability of ultrasound measurements of MT, SAT and CSA, separated for each measurement site, are shown in Table I and Table II. Intra-rater reliability of the described protocol, with the lowest ICC being 0.928 (MT at measurement site 10 cm, p < 0.001), showed excellent results for all parameters and measurement sites, with the highest closeness of agreement for SAT and measurement site 20 cm. ICC for inter-rater reliability, independent of the observed parameter and at all measurement sites, ranged from 0.929 to 0.983 (p < 0.001), also indicating a very strong closeness of agreement.
Table I.
Intra-rater reliability of ultrasound measurements
| MS | Day I Mean (SD) | Day II Mean (SD) | ICC | 95% CI | p-value | |
|---|---|---|---|---|---|---|
| MT, cm | 10 | 2.10 (0.37) | 2.08 (0.41) | 0.928 | 0.875–0.959 | < 0.001 |
| 15 | 2.33 (0.49) | 2.32 (0.53) | 0.946 | 0.906–0.969 | ||
| 20 | 2.18 (0.48) | 2.18 (0.46) | 0.961 | 0.933–0.978 | ||
| all | 2.20 (0.46) | 2.19 (0.48) | 0.949 | 0.930–0.963 | ||
| SAT, cm | 10 | 0.50 (0.36) | 0.50 (0.35) | 0.993 | 0.988–0.996 | < 0.001 |
| 15 | 0.65 (0.47) | 0.64 (0.46) | 0.992 | 0.985–0.995 | ||
| 20 | 0.98 (0.75) | 0.98 (0.73) | 0.993 | 0.988–0.996 | ||
| all | 0.71 (0.58) | 0.71 (0.57) | 0.994 | 0.991–0.995 | ||
| CSA, cm² | 10 | 11.01 (3.35) | 11.06 (3.56) | 0.969 | 0.943–0.983 | < 0.001 |
| 15 | 15.44 (5.15) | 15.21 (5.23) | 0.98 | 0.964–0.989 | ||
| 20 | 16.25 (6.07) | 16.26 (6.48) | 0.988 | 0.978–0.994 | ||
| all | 14.16 (5.37) | 14.18 (5.66) | 0.973 | 0.961–0.981 |
MT: muscle thickness; SAT: subcutaneous adipose tissue thickness; CSA: crosssectional area; MS: measurement site; ICC: intraclass correlation coefficient; 95% CI: confidence interval; SD: standard deviation.
Table II.
Inter-rater reliability of ultrasound measurements
| MS | Day I Mean (SD) | Day II Mean (SD) | ICC | 95% CI | p-value | |
|---|---|---|---|---|---|---|
| MT, cm | 10 | 2.10 (0.39) | 2.04 (0.37) | 0.936 | 0.885–0.964 | < 0.001 |
| 15 | 2.40 (0.51) | 2.27 (0.47) | 0.96 | 0.819–0.984 | ||
| 20 | 2.23 (0.46) | 2.13 (0.45) | 0.965 | 0.889–0.985 | ||
| all | 2.24 (0.47) | 2.15 (0.44) | 0.958 | 0.900–0.978 | ||
| SAT, cm | 10 | 0.52 (0.37) | 0.44 (0.31) | 0.971 | 0.859–0.989 | < 0.001 |
| 15 | 0.66 (0.49) | 0.57 (0.41) | 0.978 | 0.887–0.992 | ||
| 20 | 1.00 (0.77) | 0.88 (0.67) | 0.984 | 0.928–0.994 | ||
| all | 0.72 (0.60) | 0.63 (0.52) | 0.983 | 0.926–0.993 | ||
| CSA, cm² | 10 | 11.94 (3.34) | 10.18 (2.84) | 0.864 | 0.154–0.956 | < 0.001 |
| 15 | 16.68 (5.18) | 14.58 (4.44) | 0.901 | 0.484–0.965 | ||
| 20 | 17.70 (6.47) | 15.61 (5.65) | 0.931 | 0.671–0.974 | ||
| all | 15.44 (5.71) | 13.46 (5.02) | 0.929 | 0.608–0.973 |
MT: muscle thickness; SAT: subcutaneous adipose tissue thickness; CSA: crosssectional area; MS: measurement site; ICC: intraclass correlation coefficient; 95% CI: 95% confidence interval; SD: standard deviation.
The validity of ultrasound measurements compared with MRI differed depending on the evaluated parameter and the measurement site. ICC for MT, independent of measurement site, showed good to very good closeness of agreement (ICC = 0.835, p < 0.001), with the best result at measurement site 20 cm (ICC = 0.895, p < 0.001). Also, ICC for SAT, independent of measurement site, showed very good closeness of agreement (ICC = 0.969, p < 0.001), with the best result at measurement site 20 cm (ICC = 0.98, p < 0.001). ICC for CSA, independent of measurement site, showed just average to good closeness of agreement (ICC = 0.727, p < 0.001). Calculating the coefficient of determination R² with a linear regression model for ultrasound measured CSA and MRI-based CSA, a significant strong positive correlation was observed (Fig. 4). Again, the best correlation was observed at measurement site 20 cm (R² = 0.807, p < 0.001).
Fig. 4.
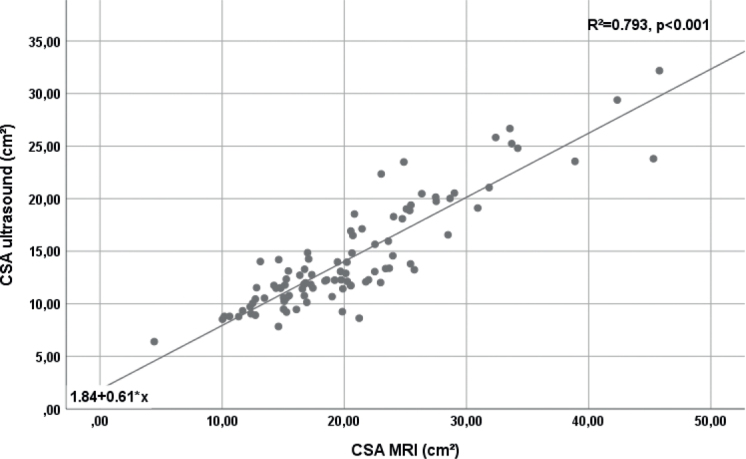
Simple linear regression model of ultrasound- and magnetic resonance imaging (MRI)-measured cross-sectional area (CSA) independent of measurement site. Coefficient of determination (R²).
To test for the accuracy of the ultrasound measurements of MT and CSA in dependence on the thickness of subcutaneous adipose tissue of the thigh, the correlation between the percentage differences in the absolute values measured by the 2 investigators and in the values obtained on 2 different days with SAT was determined using Spearman’s correlation coefficient. No statistically significant correlations between SAT and the percentage differences in the measurements were observed (inter-rater MT: r = 0.142, p = 0.062, inter-rater CSA: r=–0.05; p = 0.544; intra-rater MT: r = –0.049, p = 0.543, intra-rater CSA: r = –0.013; p = 0.935). Likewise, no correlation was found between SAT and the percentage differences between MT measured by ultrasound and MRI (r = –0.15, p = 0.144). However, a statistically significant average to good positive correlation was found for the percentage differences in CSA measurements obtained with ultrasound and with MRI and SAT (Fig. 5).
Fig. 5.
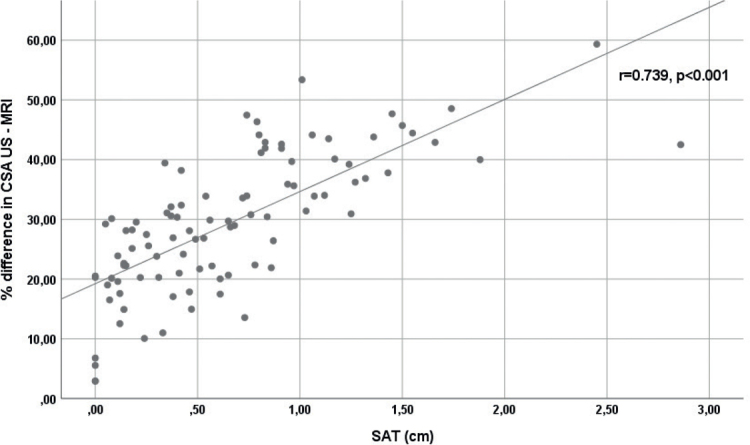
Spearman’s correlation coefficient (r) for ultrasound (US)-measured subcutaneous adipose tissue thickness (SAT) and the percentage differences between absolute values of cross-sectional area measurements obtained with muscle ultrasound and with MRI (% difference in cross-sectional area (CSA) US-MRI).
DISCUSSION
This is the first study to show that, applying a standardized examination protocol, ultrasound measures of VL size are reliable in people with varying body weight and body composition, respectively. While reproducible and investigator-independent muscle ultrasound measurements have been reported in previous studies with slim and trained subjects (15–19), our measurements revealed highly reproducible and investigator-independent values for VL MT and CSA, which also were independent of SAT. Furthermore, high validity was observed for the VL MT and SAT measurements. MT values were also independent of SAT. However, the validity of VL CSA measurements decreased significantly with increasing SAT.
This study focused on a simply and rapidly feasible standardized ultrasound examination protocol for measuring VL size. Due to its size and location, and as part of the quadriceps muscle, the most meaningful proximal lower limb muscle (12), VL should be considered an ideal index muscle to assess the increase or decrease in muscle size through physical training, particularly strength training, or inactivity, and, especially, to detect sarcopaenia-correlated low muscle size (20). VL is easily accessible and muscle biopsies are usually also obtained from this muscle. It is well known that the lower limb is more affected by sarcopaenia than the upper limb (21, 22) and the age-related loss of muscle mass is greater in the proximal than in the distal muscles of the lower limb (20).
As already mentioned, the reliability of MT and CSA measurements has been investigated in previous studies. CSA measurements of VL, performed by Reeves et al. (15) and Ahtiainen et al. (16), only showed either inter-rater reliability (ICC = 0.997–0.999, n = 6; 15) or intra-rater reliability (ICC = 0.997, n = 27; 16). The reliability of MT measurements has been investigated in several studies (17–19). While Staehli et al. (intra-rater ICC = 0.888, n = 30; 17), Raj et al. (interrater ICC = 0.96, n = 21; 18) and Strasser et al. (intra-rater ICC = 0.852, n = 26; 19) only measured at 1 measurement site of VL, we observed, that the accurateness of both intra-rater and inter-rater reliability depends on the selected measurement site of VL. For MT and CSA, the best closeness of agreement was reached at measurement site 20 cm, representing approximately the middle of the VL belly and therefore being homogenous and resistant against small alterations in the scanning position. In the current cohort, the mid distance of the anterior superior iliac spine and the upper patella pole ranged from 19 to 24 cm. The mid distance is most likely the representative measurement site to obtain reliable and comparable measurements. Moreover, at approximately 50% of the femur length, the anatomical CSA of the human quadriceps is described to be at a maximum (23).
The current study also confirmed that the proposed examination protocol results in valid measurements of MT of VL in comparison with the “gold-standard” MRI. There have been a few studies investigating the validity of MT ultrasound measurements of different parts of the quadriceps muscle. Mechelli et al. (rectus femoris + vastus intermedius muscle compared with MRI, ICC = 0.99, n = 20; 24), Thomaes et al. (rectus femoris muscle compared with CT, ICC = 0.92, n = 20; 25), and Worsley et al. (vastus medialis muscle compared with MRI, ICC = 0.84–0.9, n = 12; 26) showed the validity of MT ultrasound measurements, comparable to the current results. However, to the best of our knowledge, none of them explicitly investigated the validity of MT of the VL compared with MRI or CT.
In 2004, Reeves et al. showed the validity of CSA measurements of the VL in comparison with MRI, not by using the EFOV technique, but by fitting single scans of VL using contour matching (ICC 0.998, n = 6; 15). In 2010, Ahtiainen et al. were the first to examine the validity of measuring CSA of VL using the EFOV technique. In accordance with the results of the current study, they reported a systematic underestimation of VL CSA compared with MRI, but to a smaller extent (mean 10%, ICC = 0.905, n = 27, US scanner GE; 16) than in the current study (mean 29%). Ahtiainen et al. attributed the difference between ultrasound and MRI methods in absolute CSA measurements to the algorithms processing panoramic CSA with the EFOV technique. This assumption could be supported by our finding of the percentage difference between ultrasound and MRI-based CSA measurements being significantly correlated with SAT. An explanation might be that, with increasing SAT, the VL belly lies deeper in the processed panoramic image, probably enlarging a systematic bias of the EFOV technique in measuring angle-dependent areas. This could be, at least, part of the reason for a greater difference in absolute CSA measurements in the current study compared with the findings of Ahtiainen et al., who only measured male subjects with low SAT. The current study also examined female subjects with higher mean SAT values of 0.99 cm compared with males (mean SAT 0.23 cm). Furthermore, MT measurements without the EFOV technique were valid compared with MRI and did not show any dependency on SAT. In another study, a very good accordance of ultrasound-measured CSA of the whole quadriceps muscle by using the EFOV technique compared with CT-based measurements was reported, but within a very small number of only male subjects (ICC 0.951–0.998, n = 6; 27). In addition, Noorkooiv et al. used a different ultrasound scanner (Hitachi Aloka), which might, against the background of different algorithms processing panoramic CSA, also have an influence. Nevertheless, by using the applied protocol in the current study, measuring VL CSA by ultrasound with the EFOV technique showed a strong positive predictive correlation with MRI measurements. Therefore, muscle ultrasound can provide useful information about muscle size, especially when assessing the development of VL size through physical activity or inactivity, but also for the comparison of different individuals.
In addition to MT and CSA of VL, we also evaluated SAT measurements. In accordance with Mechelli et al., who already showed the validity of ultrasound measurements of SAT of the anterior thigh compared with MRI (ICC 0.99, n = 20; 24), we could further prove the excellent inter- and intra-rater reliability of ultrasound measurements of SAT. Here, SAT measurements showed almost no dependence on measurement site, probably due to equable distribution all over the thigh.
As mentioned above, measurements of VL size using our protocol were reliable in people with varying body weight and body composition. This finding was surprising, because greater difficulties in recording clear images, especially with the EFOV technique, were reported with increasing SAT. However, our results suggest that the method is applicable not only for slim and trained people with low SAT, but also for people with a higher percentage of subcutaneous adipose tissue.
This study has some limitations. The sample size is rather small, but greater than in previous studies. Furthermore, the study did not include patients with known sarcopaenia or morbid obesity, nor elite strength-trained or endurance-trained athletes. Although in the present investigation, the variation in body composition, reflected by BMI between 19.5 and 32.2 kg/m2 and SAT measurements ranging from 0.01 to 3.13 cm, was larger than in previous studies, the reliability and validity of muscle ultrasound measurements in people with an extreme body composition remain unknown. In addition, it should be considered that, in contrast to MRI measurements, ultrasound measurements were performed with a soft roll positioned below the hollow of the subject knees, which might have an influence on relaxation of the muscle and therefore on the actual values of MT and CSA.
In summary, muscle ultrasound, when applying a standardized examination protocol, is a rapidly feasible, reliable and, with regard to MT and SAT, also valid, method for measuring VL size in subjects with varying body composition. Therefore, it might be used for monitoring the effects of strength training in clinical studies or in elite sports, and for the screening of sarcopaenia in clinical practice. Further studies are needed to investigate the validity of measuring areas with the EFOV technique and to evaluate the reliability and validity of muscle ultrasound in individuals with extreme body composition, e.g. morbid obesity or cachexia.
Footnotes
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Mitsiopoulos N, Baumgartner RN, Heymsfield SB, Lyons W, Gallagher D, Ross R. Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. J Appl Physiol (1985) 1998; 85: 115–122. [DOI] [PubMed] [Google Scholar]
- 2.Sanada K, Kearns CF, Midorikawa T, Abe T. Prediction and validation of total and regional skeletal muscle mass by ultrasound in Japanese adults. Eur J Appl Physiol 2006; 96: 24–31. [DOI] [PubMed] [Google Scholar]
- 3.Tosato M, Marzetti E, Cesari M, Savera G, Miller RR, Bernabei R, et al. Measurement of muscle mass in sarcopenia: from imaging to biochemical markers. Aging Clin Exp Res 2017; 29: 19–27. [DOI] [PubMed] [Google Scholar]
- 4.Ticinesi A, Meschi T, Narici MV, Lauretani F, Maggio M. Muscle ultrasound and sarcopenia in older individuals: a clinical perspective. J Am Med Dir Assoc 2017; 18: 290–300. [DOI] [PubMed] [Google Scholar]
- 5.Leone AF, Schumacher SM, Krotish DE, Eleazer GP. Geriatricians’ interest to learn bedside portable ultrasound (GEBUS) for application in the clinical practice and education. J Am Med Dir Assoc 2012; 13: 308.e7–308.e10. [DOI] [PubMed] [Google Scholar]
- 6.Nijholt W, Scafoglieri A, Jager-Wittenaar H, Hobbelen JSM, van der Schans CP. The reliability and validity of ultrasound to quantify muscles in older adults: a systematic review. J Cachexia Sarcopenia Muscle 2017; 8: 702–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.English C, Fisher L, Thoirs K. Reliability of real-time ultrasound for measuring skeletal muscle size in human limbs in vivo: a systematic review. Clin Rehabil 2012; 26: 934–944. [DOI] [PubMed] [Google Scholar]
- 8.Cruz-Jentoft AJ, Baeyens AP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working group on sarcopenia in older people. Age Aging 2010; 39: 412–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Uchmanowicz I, Loboz-Rudnicka M, Szelag P, Jankowska-Polanska B, Loboz-Grudzien K. Frailty in heart failure. Curr Heart Fail Rep 2014; 11: 266–273. [DOI] [PubMed] [Google Scholar]
- 10.Kato A. Muscle wasting is associated with reduced exercise capacity and advanced disease in patients with chronic heart failure. Future Cardiol 2013; 9: 767–770. [DOI] [PubMed] [Google Scholar]
- 11.Benz E, Trajanoska K, Lahousse L, Schoufour JD, Terzikhan N, De Roos E, et al. Sarcopenia in COPD: a systematic review and meta-analysis. Eur Respir Rev 2019; 28: 190049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wurzinger LJ. Hüfte, Oberschenkel und Knie [Hip, thigh and knee.]. In: Aumüller G, Aust G, Doll A, editors. Anatomie [Anatomy], Duale Reihe 2nd edn. Stuttgart: Georg Thieme Verlag KG; 2010, p.331 (in German). [Google Scholar]
- 13.Ticinesi A, Narici M, Lauretani F, Nouvenne A, Colizzi E, Mantovani M, et al. Assessing sarcopenia with vastus lateralis muscle ultrasound: an operative protocol. Aging Clin Exp Res 2018; 30: 1437–1443. [DOI] [PubMed] [Google Scholar]
- 14.Koo T, Li M. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 2016; 15: 155–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reeves ND, Maganaris CN, Narici MV. Ultrasonographic assessment of human skeletal muscle size. Eur J Appl Physiol 2004; 91: 116–118. [DOI] [PubMed] [Google Scholar]
- 16.Ahtiainen J, Hoffren N, Hulmi J, Pietikäinen M, Mero AA, Avela J, et al. Panoramic ultrasonography is a valid method to measure changes in skeletal muscle cross-sectional area. Eur J Appl Physiol 2010; 108: 273–279. [DOI] [PubMed] [Google Scholar]
- 17.Staehli S, Glatthorn JF, Casartelli N, Maffiuletti NA. Test– retest reliability of quadriceps muscle function outcomes inpatients with knee osteoarthritis. J Electromyogr Kinesiol 2010; 20: 1058–1065. [DOI] [PubMed] [Google Scholar]
- 18.Raj I, Bird S, Shield A. Reliability of ultrasonographic measurement of the architecture of the vastus lateralis and gastrocnemius medialis muscles in older adults. Clin Physiol Funct Imaging 2012; 32: 65–70. [DOI] [PubMed] [Google Scholar]
- 19.Strasser E, Draskovits T, Praschak M, Quittan M, Graf A. Association between ultrasound measurements of muscle thickness, pennation angle, echogenicity and skeletal muscle strength in the elderly. Age 2013; 35: 2377–2388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Minetto MA, Caresio C, Menapace T, Hajdarevic A, Marchini A, Molinari F, et al. Ultrasound based detection of low muscle mass for diagnosis of sarcopenia in older adults. PM R 2016; 8: 453–462. [DOI] [PubMed] [Google Scholar]
- 21.Janssen I, Heymsfield S, Wang Z, Ross R. Skeletal muscle mass and distribution in 468 men and women aged 18–88 yr. J Appl Physiol 2000; 89: 81–88. [DOI] [PubMed] [Google Scholar]
- 22.Gallagher D, Visser M, De Meersman R, Sepulveda D, Baumgartner RN, Piersner RN, et al. Appendicular skeletal muscle mass: effects of age, gender and ethnicity. J Appl Physiol (1985) 1997; 83: 229–239. [DOI] [PubMed] [Google Scholar]
- 23.Narici MV, Roi GS, Landoni L, Minetti AE, Cerretelli P. Changes in force, cross-sectional area and neural activation during strength training and detraining of the human quadriceps. Eur J Appl Physiol Occup Physiol 1989; 59: 310–319. [DOI] [PubMed] [Google Scholar]
- 24.Mechelli F, Arendt-Nielsen L, Stokes M. Validity of ultrasound imaging versus magnetic resonance imaging for measuring anterior thigh muscle, subcutaneous fat, and fascia thickness. Methods Protoc 2019; 2:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thomaes T, Thomis M, Onkelinx S, Coudyzer W, Cornelissen V, Vanhees L. Reliability and validity of the ultrasound technique to measure the rectus femoris muscle diameter in older CAD-patients. BMC Med Imaging 2012; 12: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Worsley P, Kitsell F, Samuel D, Stokes M. Validity of measuring distal vastus medialis muscle using rehabilitative ultrasound imaging versus magnetic resonance imaging. Man Ther 2014; 19: 259–263. [DOI] [PubMed] [Google Scholar]
- 27.Noorkoiv M, Nosaka K, Blazevich A. Assessment of quadriceps muscle cross-sectional area by ultrasound extended-field-of-view imaging. Eur J Appl Physiol 2010; 109: 631–639. [DOI] [PubMed] [Google Scholar]