Abstract
An etiological study of sexually transmitted infections (STIs) was conducted among female sex workers (FSWs) in Dhaka, Bangladesh. Endocervical swab and blood samples from 269 street-based FSWs were examined for Neisseria gonorrhoeae, Chlamydia trachomatis, and Trichomonas vaginalis as well as for antibodies to Treponema pallidum and herpes simplex virus 2 (HSV-2). Sociodemographic data and data regarding behavior were also collected. A total of 226 of the 269 FSWs (84%) were positive for the STI pathogens studied. Among the 269 FSWs, 35.5% were positive for N. gonorrhoeae, 25% were positive for C. trachomatis, 45.5% were positive for T. vaginalis, 32.6% were seropositive for T. pallidum, 62.5% were seropositive for HSV-2, and 51% had infections with two or more pathogens.
Sexually transmitted infections (STIs) represent a major public health problem in developing countries, including Bangladesh. It is estimated that there are 333 million new cases of STIs per annum and that 10 to 15 million people are infected with human immunodeficiency virus worldwide every year. Southeast Asia is an important area for STIs, with an estimated 150 million new cases in 1995 (11). Female sex workers (FSWs) have been considered to be an important reservoir of STIs and a high-risk population for STIs and human immunodeficiency virus (4). In most parts of Asia and Africa, 80 to 90% of the venereal infections, including gonorrhea, originate from FSWs (10). In Bangladesh, there are approximately 100,000 FSWs who are distributed in urban, semiurban, and rural areas. They either are organized in brothels or work as independent sex workers (3). The prevalence of reproductive tract infections (RTIs) and STIs among females in the general population and among FSWs in Bangladesh is not well documented. In a cross-sectional study among slum dwellers in Dhaka city, it was shown that the prevalence of gonorrhea was 1% and that the prevalence of syphilis was 11.5% (K. Sabin, M. Rahman, S. Hawkes, K. Ahsan, L. Begum, S. E. Arifeen, and A. H. Baqui, Programmes Abstr. Sixth Annu. Sci. Conf., abstr. 13, 1997). In a recent brothel-based study, it was found that the prevalence of gonorrhea and/or chlamydia was 28% and 57.1% of FSWs were positive for syphilis though none was HIV positive (7). The prevalence of gonorrhea among street-based FSWs and the antimicrobial susceptibility of the isolates were subsequently studied; 42% of the street-based FSWs were found to be culture positive for gonorrhea (1, 2). However, the prevalence of other STIs among the street-based FSWs has never been studied in Bangladesh.
Between May and December 1998, we conducted a prevalence study of STIs among street-based FSWs attending a rehabilitation center under a government rehabilitation program in Dhaka, Bangladesh. All street-based FSWs attending the rehabilitation center were enrolled in the study irrespective of symptoms. The only exclusion criterion was antibiotic use in the preceding 2 weeks. All eligible women were requested to participate in the study after receiving a brief description of the purpose and procedure of the study. The participants were interviewed by a trained social worker to obtain information about sociodemographic data and sexual and medical histories. A physician interviewed the FSWs for symptoms of STIs (abnormal vaginal discharge, dysuria, and lower abdominal pain) and performed a gynecological examination including speculum examination. A high vaginal swabs, an endocervical swab, and 5 ml of venous blood were collected for diagnosis of STIs. At the study clinic, a wet mount of vaginal fluid was prepared and examined microscopically for the presence of motile Trichomonas vaginalis. A Gram-stained endocervical smear was also made for detection of gram-negative intra- and/or extracellular diplococci and pus cells. Each endocervical swab was inoculated on prewarmed modified Thayer-Martin medium and incubated at 37°C in a candle extinction jar, and identification of Neisseria gonorrhoeae was made as described earlier (2). Chlamydia trachomatis was diagnosed in batches by a PCR assay, as described earlier (8). A duplicate endocervical swab in phosphate-buffered saline (pH 7.2) preserved at −70°C was thawed and centrifuged at 13,000 × g for 15 min. The pellet was dissolved in 50 μl of lysis buffer containing 1 mM EDTA, 1% Triton X-100 (Sigma, St. Louis, Mo.), 50 mM Tris hydrochloride (pH 7.5), and proteinase K (0.4 μg/μl). The sample was incubated at 37°C for 60 min and then heated at 95°C for 10 min. The sample was centrifuged at 13,000 × g for 5 min, and 2 μl of the supernatant was used as the template for PCR assay. The PCR product was electrophoresed on a 2% agarose gel at 120 V for 1 h and stained with ethidium bromide.
All serum samples were screened for antibodies to Treponema pallidum by rapid plasma reagin RFR test (Becton-Dickinson, Cockeysville, Md.) and by T. pallidum hemagglutination (TPHA) test (Fujirrbio, Tokyo, Japan). A patient was considered to have syphilis if both RPR and TPHA test results were found to be positive. Serum antibody to herpes simplex virus 2 (HSV-2) was detected by bioelisa HSV-2 IgG enzyme immunoassay (Biokit, Barcelona, Spain) as instructed by the manufacturer.
A total of 269 FSWs were included in the study. Endocervical swabs for culture of N. gonorrhoeae were collected from all 269 subjects. Endocervical swabs for diagnosis of C. trachomatis were collected from 244 subjects, microscopic examination of a wet-mount preparation of vaginal fluid was done for 237 subjects, and a blood sample for serological diagnosis of T. pallidum and HSV-2 was collected from 203 subjects. However, serological analysis for T. pallidum could not be done on one sample due to loss of the sample after performing serological analysis for HSV-2.
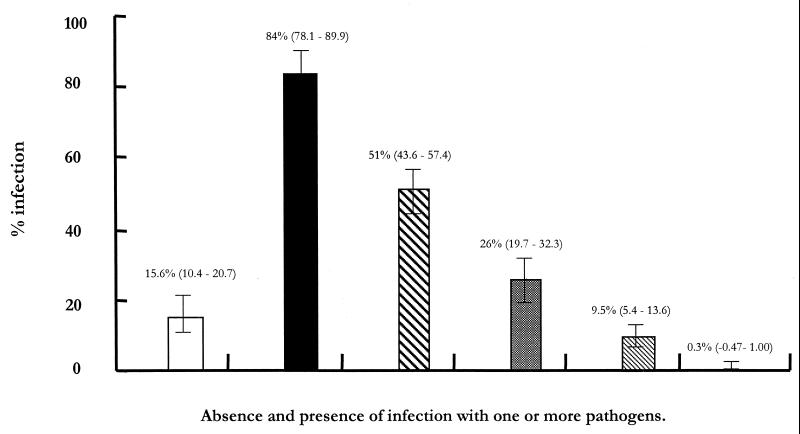
More than half of the FSWs were between 18 and 30 years of age, were married, had 1 to 2 children, did not have any education, and never used a condom. Less than half had been in the trade for less than 6 months and entertained up to 21 clients a week. The data on prevalence of STIs and RTIs among the FSWs are shown in Table 1. A cervical pathogen, N. gonorrhoeae or C. trachomatis, was present in up to 46% of the cases; up to 46% of the cases were positive for the vaginal pathogen T. vaginalis. Some 33% of the FSWs were seropositive for syphilis and 63% were seropositive for HSV-2. The absence or presence of infection with one or more pathogens is summarized in Fig. 1. Approximately half of the infections were mixed infections with two pathogens, and a small proportion demonstrated a mixed infection with all five pathogens.
TABLE 1.
Prevalence of STI pathogens among 269 FSWs in Dhaka, Bangladesh
| Pathogen, disease, or virus | No. of positive samples/no. tested (%) | 95% Confidence interval |
|---|---|---|
| Cervical pathogens | ||
| N. gonorrhoeae | 96/269 (35.6) | 29.8–41.3 |
| C. trachomatis | 61/244 (25.0) | 19.5–30.4 |
| N. gonorrhoeae or C. trachomatis | 123/269 (45.7) | 39.7–51.6 |
| Vaginal pathogen | ||
| T. vaginalis | 108/237 (45.5) | 39.1–51.8 |
| Syphilis (RPR and TPHA positive) | 66/202 (32.6) | 26.1–39.0 |
| HSV-2 | 127/203 (62.5) | 55.8–69.1 |
FIG. 1.
Summary of prevalence (values in parentheses are 95% confidence intervals [also indicated by error bars]) of single and multiple STIs among 269 FSWs surveyed. Bars indicate FSWs with no infection (□), with any one infection (■), with any two infections (▧), with any three infections ( ), with any four infections (▧), and with all five infections (
), with any four infections (▧), and with all five infections ( ).
).
The prevalence of gonorrhea among the FSWs with and without symptoms of STIs or RTIs was analyzed; 69.5% (187 of 269) of the FSWs were symptomatic, and 32.6% (61 of 187) of them had gonorrhea; 30.5% (82 of 269) of the FSWs were asymptomatic, and of them, 42.7% (35 of 82) had gonorrhea. On examination of the symptomatic patients infected with gonococci, 60% (36 of 61) were found to have vaginal discharge, and among the asymptomatic group, 38% (13 of 35) had vaginal discharge. Cervical mucopus was present in 56% (34 of 61) of gonorrhea-positive symptomatic cases and in 26% (9 of 35) of gonorrhea-positive asymptomatic cases (P > 0.05). There was mixed chlamydial infection in 33% (33 of 96) of gonorrhea cases. Analysis of gonorrhea cases in relation to age showed that the oldest subjects (older than 30 years) had the highest prevalence (57.9% [11 of 19]), followed by the 18- to 30-year-old subjects, with 36.3% (62 of 171) prevalence, and those younger than 18 years, with 29.1% (23 of 79) prevalence. A decreasing trend in the prevalence of gonorrhea in relation to duration of involvement in the trade was observed. The highest prevalence of 41% (20 of 49) was seen in those with 6 to 11 months in the trade, followed by 39% (44 of 113) in those with less than 6 months in trade, 32% (22 of 69) in those with 1 to 2 years in the trade, and the lowest prevalence, 26% (10 of 38), in those with more than 2 years in the trade. The sensitivity of a Gram-stained smear of each endocervical swab for diagnosis of gonorrhea was also evaluated. All 18 cases with typical intracellular gram-negative diplococci with pus cells were culture positive for N. gonorrhoeae (sensitivity and specificity, 100%), whereas among the cases with extracellular gram-negative diplococci with or without pus cells, only 41.8% (65 of 156) were positive for gonorrhea. The microscopic findings in the latter category showed no significant association with gonorrhea (χ2 test, P > 0.05). In 13 (13.5%) cases with culture-positive gonorrhea, no gram-negative diplococci or pus cells were found by microscopy.
The prevalence of STIs among the street-based FSWs studied was high, as expected, because among this group no effective intervention strategy has been implemented. About 35% of the FSWs in the present study were culture positive for gonorrhea, which is in agreement with results of a previous study, where 42% of FSWs were positive for gonorrhea (1, 2). Similar high rates of STIs were found in FSWs in African countries, with gonorrhea rates of up to 51% in Rwanda, of 30 to 55% in Kenya, and of up to 31% in Ivory Coast (4, 5). The prevalence of chlamydia and trichomoniasis were 25 and 45%, respectively, with similar prevalence rates reported from Africa (6). The prevalence rate of syphilis in our study was 32.6%, which is lower than the 57% prevalence found in a brothel-based study in Bangladesh (7). As observed elsewhere, about one-third of the women with cervical infection were asymptomatic. The lack of symptoms among women with STIs is a major constraint in using syndromic algorithms for screening for gonococcal and/or chlamydial cervicitis (9). In poor countries, data on STIs and related complications are limited which means that the burden of these diseases is substantially underestimated. STIs are often asymptomatic and are technically difficult and often expensive to diagnose. Gathering information on STIs and sexual practices prevailing among sex workers and adopting protective measures against infections are of paramount importance in developing any intervention program.
Acknowledgments
This research was funded by ICDDR,B: Centre for Health and Population Research, which is supported by countries and agencies that share its concern for the health problems of developing countries. Current donors providing unrestricted support include the aid agencies of the governments of Australia, Bangladesh, Belgium, Canada, Saudi Arabia, Sweden, Switzerland, the United Kingdom, and the United States of America; international organizations include United Nations Children's Fund (UNICEF).
We thank Concern Bangladesh for their cooperation in specimen collection. We thank Aklima Begum and Nargis Akther for their assistance.
REFERENCES
- 1.Bhuiyan B U, Rahman M, Miah R A, Rahman M, Albert M J. High prevalence of ciprofloxacin resistant Neisseria gonorrhoeae among the commercial sex workers in Bangladesh. J Antimicrob Chemother. 1998;48:675–676. doi: 10.1093/jac/42.5.675. [DOI] [PubMed] [Google Scholar]
- 2.Bhuiyan B U, Rahman M, Miah M R A, Nahar S, Islam N, Ahmed M, Rahman K M, Albert M J. Antimicrobial susceptibilities and plasmid contents of Neisseria gonorrhoeae isolates from commercial sex workers in Dhaka, Bangladesh: emergence of high-level resistance to ciprofloxacin. J Clin Microbiol. 1999;37:1130–1136. doi: 10.1128/jcm.37.4.1130-1136.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Choudhury M R, Islam N, Rasul G. Meeting the challenges of HIV/AIDS in Bangladesh. 1997. p. 19. . Bangladesh AIDS Prevention and Control Program, Dhaka, Bangladesh. [Google Scholar]
- 4.D'Costa L J, Plummer F A, Bowmer I, Fransen L, Piot P, Ronald A R, Nsanze H. Prostitutes are a major reservoir of sexually transmitted diseases in Nairobi, Kenya. Sex Transm Dis. 1985;12:64–67. doi: 10.1097/00007435-198504000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Meheus A, De Clercq A, Prat R. Prevalence of gonorrhoea in prostitutes in a Central African town. Br J Vener Dis. 1974;50:50–52. doi: 10.1136/sti.50.1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ndoye I, Mboup S, De Schryver A, Van Dyck E, Moran J, Samb N D, Sakho M L, Thior I, Wade A, Heymann D L, Meheus A. Diagnosis of sexually transmitted infections in female prostitutes in Dakar, Senegal. Sex Transm Dis. 1998;74(Suppl. 1):S112–S117. [PubMed] [Google Scholar]
- 7.Sarker S, Islam N, Durandin F, Siddique N, Panda S, Jana S, Klapper P, Mandal D. Low HIV and high STD among commercial sex workers in a brothel in Bangladesh: scope for prevention of larger epidemic. Int J STD AIDS. 1998;9:45–57. doi: 10.1258/0956462981920856. [DOI] [PubMed] [Google Scholar]
- 8.Vogels W H, van Voorst Vader P C, Schroder F P. Chlamydia trachomatis infection in a high-risk population: comparison of polymerase chain reaction and cell culture for diagnosis and follow-up. J Clin Microbiol. 1993;31:1103–1107. doi: 10.1128/jcm.31.5.1103-1107.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vuylsteke B, Laga M, Alary M, Gerniers M M, Lebughe J P, Nzila N, Behets F, Van Dyck E, Piot P. Clinical algorithms for the screening of women for gonococcal and chlamydial infection: evaluation of pregnant women and prostitutes in Zaire. Clin Infect Dis. 1993;17:82–88. doi: 10.1093/clinids/17.1.82. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. WHO Expert Committee on Gonococcal Infections: first report. Technical report series no. 262. Geneva, Switzerland: World Health Organization; 1963. [PubMed] [Google Scholar]
- 11.World Health Organization. Global programme on AIDS. Management of sexually transmitted diseases. WHO/GPA/TEM/94.1. Geneva, Switzerland: World Health Organization; 1995. [Google Scholar]