Summary
Background
Understanding the predictive factors for tobacco use, and initiation among the youth is critical for effective intervention and prevention. We, therefore, aimed to determine the profile, associated factors, the regional disparities in the use of tobacco products among the youth in Ghana.
Method
The study used the 2017 Ghana Global Youth Tobacco Survey (GYTS) to obtain tobacco-related information among the youth in Junior High Schools across the country. The survey used a two-stage cluster randomized sampling technique to obtain nationally representative data. Weighted univariate and multivariate logistic regression analyses were used to assess the association of participant’s characteristics and use of tobacco.
Results
Out of the 6039 targeted respondents, 5,664 (93.8%) participated, 2,707 males, 2,929 females, and 28 of the participants had missing gender data. The use of any tobacco product (cigarette, smokeless tobacco, electronic cigarette, or waterpipe tobacco) was 28.3, 7.0, and 4.8% in the Savanna/northern zone, middle/forest zone, and Coastal zone respectively. From the univariate analysis, age (p = 0.005), pocket money (p < 0.001), and exposure to secondhand smoke (SHS) at home (p < 0.001) were significantly associated with tobacco use. In the multivariate analysis, age (p = 0.002), pocket money (p < 0.001), exposure to SHS at home (p < 0.001), and being taught about the dangers of tobacco use (p = 0.043) were significantly associated with tobacco use.
Conclusion
Multiple factors including age, pocket money, exposure to SHS were identified to be associated with tobacco use among the youth in Ghana. Promoting anti-smoking campaigns in early adolescence, as well as programmes targeting early tobacco use can guard the youth against initiating tobacco use.
Keywords: Adolescence, Predictors, Profile, Second-hand smoke, Tobacco use, Waterpipe tobacco
Background
The tobacco epidemic is a prime public health challenge facing the world and killing over 8 million people every year [1]. Among these deaths, over 7 million are because of direct tobacco use whiles the rest are non-smokers being exposed to SHS. It is also the single most preventable cause of disease and disability globally.
The tobacco menace does not affect only adults, but persons of all ages of life including children and adolescents. Tobacco smoke exposure in the form of SHS exposure among children is also high. Close to half of children regularly breathe air polluted by tobacco smoke in their homes and other public places, resulting in over 65000 deaths each year from illnesses because of SHS [2] and sudden infant death syndrome globally [3]. Also, over 25 million and 13 million boys and girls aged 13-15 years in school are currently using cigarette or smokeless tobacco respectively across the world [4]. Among developed countries, we have observed a significant decrease compared to developing countries where reports show higher prevalence. Despite the drop in cigarette smoking among the youth in developed countries, the overall tobacco use especially among adolescent girls continues to surge globally [4, 5].
In sub-Saharan Africa (SSA), tobacco consumption among the youth varies, ranging from a prevalence of 1.4% in Zimbabwe, 1.5% in Nigeria, to as high as 34.4% in South Africa. This has been attributed to income growth and increasing cigarette affordability, non-adherence to restrictions and bans, as well as the tobacco industry’s aggressive marketing strategies in some countries in SSA [6, 8]. In Ghana, close to 9% (boys = 8.9% ; girls = 8.2%) are currently using some form of tobacco products [7]. The recent shift from conventional cigarettes to the use of other tobacco often promoted by the tobacco industry as a safe alternative to smoking among the youth populations is of particular concern because of the rise in nicotine dependence and tobacco use persistence into adulthood [8]. The decline in the cigarette is due to the sustained and highly effective regulation, public health, and clinical efforts informed by extensive scientific data [9]. Regrettably, the decline in cigarette use among the youth has led to the surge in new, non-cigarette tobacco and nicotine-delivery products, commonly referred to as alternative tobacco products (ATPs). These include Shisha (hookah), cigars, smokeless tobacco, and electronic cigarettes [9]. The use of ATPs among the youth has been attributed to the increased availability; perception of safety; lack of or non-implemented regulations surrounding their use; reduced cost and easy availability and accessibility; attractive smell and taste [9]. ATPs also, affect smoking cessation rates negatively and expands the nicotine market by attracting the youth [10]. For instance, in Ghana, the recent GYTS findings align with this global trend, showing decreasing trends for cigarette smoking, from 3.6% in the year 2000 [11] to 2.8% in 2017, whiles higher rates of other tobacco products such as smokeless tobacco use (3.6%), shisha use (1.5%), and electronic cigarette use (4.9%) [7] have been reported for the first time among the youth. The use of ATPs among the youth and young adults is of concern due to their increased vulnerability to nicotine dependence. Studies on predictors of early tobacco use among Hispanic adolescence include family separation, school failure, and association to deviant peers [12, 13]. A study among Norwegian youth also indicated family control factors and peer pressure [14], as a powerful predictor of smoking initiation and also reported among the youth in the Middle East (Iran) [15], and as well as Whites, Blacks, and Hispanic adolescents in Europe [16].
Studies on predictors of tobacco use among the youth in Africa are lacking. To prevent future growth in tobacco use mainly as a result of the shifting attention of the tobacco industry and the increased vulnerability of the youth population in Africa, there is the need to document the key predictors of tobacco initiation among the youth. The study aims to determine the profile of tobacco use and to assess the factors associated with tobacco use among adolescents in Ghana using data from the 2017 GYTS
Methods
The study used the 2017 Ghana Global Youth Tobacco Survey (GYTS) to obtain tobacco-related information among adolescents in Junior High School across the country. They sampled participants from the three main ecological/epidemiological zones of Ghana, namely the savanna or the northern zone, the middle of the forest zone, and the coastal zone. The savannah/northern zone covers the current five northern regions (Northern, Savannah, North East, Upper East, and Upper West regions). The middle/forest zone comprises the current Ashanti, Bono, Bono East, Ahafo, Eastern, Volta, and Oti regions, and the coastal zone covers the current Greater Accra, Central, Western, and Western North regions. Students from seventy-seven (n = 77) schools across the country were included in the survey. The Ghana GYTS is a standard school-based survey designed to collect information on cigarette and non-cigarette tobacco products and on five determinants of tobacco use – access/availability and price, SHS exposure, cessation, media messages, and tobacco advertising sponsorship and promotion. The survey design and methodology have been described in earlier studies [7, 17]. In brief, the study used a two-stage cluster sampling to obtain representative data of Ghanaian youth in school. In the first stage, we selected schools proportional to their enrollment size, followed by a random selection of classes within these schools in the second stage. Inclusion and exclusion criteria for selection were; all registered schools, both public and private, and grades or classes that represent the student population of boys and girls of 13-15 years of age enrolled in schools. The authors included all schools with an enrolment size of 80 and above in the sample frame unless the schools did not comprise grades/classes that represent students aged 13-15 years. All students in selected classes were eligible to participate in the survey.
Parental consent and assent from students were sought before data collection and participation. Students were also informed that participation was voluntary and therefore they could discontinue when they wished, or decide not to respond to a question that they were not comfortable with.
STUDY MEASURES
This study used four primary outcome measures to assess tobacco use among the youth in Ghana. These were the use of cigarettes, smokeless tobacco, electronic cigarette, and waterpipe tobacco (shisha) (Tab. I). We determined these by the participant’s response to the questions: ‘‘During the past 30 days, on how many days did you smoke cigarettes?’’, During the past 30 days, did you use any form of smoked tobacco products other than cigarettes (e.g., cigars, waterpipes, cigarillos, little cigars, pipes)?’’, “During the past 30 days, on how many days did you smoke waterpipe tobacco (shisha)? ‘‘During the past 30 days, did you use any form of smokeless tobacco products (e.g., chewing tobacco, snuff, dip)?’’, “During the past 30 days, on how many days did you use electronic cigarettes?” In total, on how many days have you used an electronic cigarette or e-cigarette in your entire life?”, We classified those who smoked one or more days during the past 30 days as current cigarette smokers. Among the ever-users of any tobacco products we determined their status by a positive response to any of the following questions: “Have you ever tried or experimented with any form of smokeless tobacco products (such as snuff, “Bonto”, chewing tobacco)?”, ‘‘Have you ever tried or experimented with waterpipe tobacco (shisha) smoking, even one or two puffs?” respectively.
Tab. I.
Description of variables used in the study.
| Variable | Description/definition |
|---|---|
| Age | Participants age at the time of the survey (11-12 years, 13-15 years, and 16-17 years) |
| Grade | The participants’ grade in Junior High School (1st year of Junior High School (JHS1), 2nd year of Junior High School (JHS2), 3rd year of Junior High School (JHS3) |
| Current cigarette smokers | Participants who currently smoke cigarettes 1 or more days in the past 30 days |
| Ever cigarette smokers | Participants who ever smoked cigarettes or who tried or experimented with cigarette smoking, even one or two puffs |
| Current smokeless tobacco users | Participants who currently use smokeless tobacco products in the past 30 days |
| Exposure to secondhand smoke at home | Participants who were exposed to tobacco smoke at home in the past 7 days or who reported that smoking occurred in their presence inside their home on 1 or more days in the past 7 days |
| Taught about the dangers of tobacco use at school | Participants were taught about the dangers of tobacco use in class during the past 12 months |
| Exposure to anti-tobacco messages in the media | Participants who saw or heard any anti-tobacco messages in the media (e.g., television, radio, internet, billboards, posters, newspapers, magazines, or movies) in the past 30 days |
| Current electronic cigarette users | Participants who used electronic cigarettes during the past 30 days |
| Current waterpipe (shisha) users | Participants who used waterpipe (shisha) during the past 30 days |
| Pocket money | The amount of pocket money that participants spend on themselves on the average per week (No pocket money, Less than 2 cedis, 2-5 cedis, 6-10 cedis, 11-20 cedis, 21 cedis, or more) |
We constructed predictors from selected questions that could hypothetically and in theory be associated with tobacco use among adolescents in Ghana, including exposure to SHS inside the home (public place), exposure to smoking or anti-smoking media messages, age, and gender.
Ethical approval for the study was obtained from the Ghana Health Service Ethics Review Committee. Approval was also obtained from the Ministry of Education/Ghana Education Service and the heads of the selected schools. We obtained parental consent and written assent from children after a detailed explanation of the study objectives, procedures, risks, and benefits had been presented to them.
STATISTICAL ANALYSIS
Data were weighted by taking into account the design characteristics of the survey. The following weighting formula was used:
| W = W1 × W2 × f1 × f2 × f3 × f4 |
W1 is the inverse of the probability of selecting the school; W2 is the inverse of the probability of selecting the class within the school; f1 is a school-level nonresponse adjustment factor calculated by school size category (small, medium, large); f2 is a class adjustment factor calculated by school; f3 is a student-level nonresponse adjustment factor calculated by class; f4 is a post-stratification adjustment factor calculated by gender and grade.
The background characteristics of the study participants were presented as unweighted frequencies and weighted percentages. The prevalence of tobacco use was mapped to show regional disparities in the use of cigarettes, smokeless tobacco, electronic cigarette, and waterpipe tobacco (shisha). Tobacco use was also presented by background characteristics of the respondents, stratified by gender. Chi-squared tests were used to assess the association between participant’s characteristics and the use of any tobacco product. The use of any tobacco product implies the use of cigarettes, smokeless tobacco, electronic cigarette, or waterpipe tobacco.
Weighted univariate and multivariate logistic regression analyses were used to obtain estimates of the association between the following – gender, age, grade/form, amount of pocket money, exposure to SHS at home, exposure to antismoking media message, and being taught about the danger of tobacco use during the past 12 months and use of any tobacco product. Given the interest in these selected variables, they were all included in the multivariate analysis irrespective of their statistical significance in the univariate analysis. All test results were considered to be statistically significant at a default alpha of 5%. STATA version 15 (StataCorp, Texas) was used for the statistical analysis.
Results
CHARACTERISTICS OF STUDY RESPONDENTS
Out of the 6,039 targeted respondents, 5,664 (93.8%) participated in the survey 2,707 males, 2,929 females, and 28 with missing gender. As presented in Table II, about 90% (n = 5,116) of the students were within the 13-15 years age group. Regarding pocket money, close to 90% (n = 4,777) of the students reported having money to spend every week. About a quarter of the respondents (23.7%, n = 1,239) reported being exposed to SHS at home. Of all the respondents, 52.5% (n = 2804) said they were taught about the dangers of tobacco use in school. The tobacco products used among the Junior High Students in Ghana included cigarette: 3.0% (boys = 3.2%; girls = 2.7%), smokeless tobacco: 3.6% (boys = 3.2%; girls = 3.9), electronic cigarette: 5.8% (boys = 5.5%, girls 6.1%) and water pipe (Shisha): 1.7% (boys = 0.9%; girls 2.1%) (Tab. II).
Tab. II.
Background and smoking characteristics of study participants-GYTS Ghana, 2017.
| Characteristics | Overall (n = 5,664) | Malesβ (n = 2,707) | Femalesβ (n = 2,929) | |||
|---|---|---|---|---|---|---|
| Unweighted frequency | Weighted percentage | Unweighted frequency | Weighted percentage | Unweighted frequency | Weighted percentage | |
| Age* | ||||||
| 11 to 12 years | 137 | 2.7 | 63 | 2.8 | 70 | 2.6 |
| 13 to 15 years | 5,116 | 90.9 | 2,412 | 89.9 | 2,681 | 91.9 |
| 16 to 17 years | 402 | 6.4 | 228 | 7.3 | 173 | 5.6 |
| Grade# | ||||||
| JHS1 | 2,104 | 37.5 | 1,016 | 37.5 | 1,085 | 37.8 |
| JHS2 | 2873 | 34.1 | 1,351 | 33.9 | 1,508 | 34.3 |
| JHS3 | 662 | 28.4 | 329 | 28.6 | 328 | 27.9 |
| Pocket money $ | ||||||
| No pocket money | 874 | 10.9 | 431 | 10.0 | 436 | 11.8 |
| Less than 2 cedis | 1,206 | 19.2 | 572 | 19.7 | 627 | 18.4 |
| 2-5 cedis | 1,455 | 28.1 | 701 | 29.5 | 746 | 26.6 |
| 6-10 cedis | 826 | 17.0 | 382 | 16.3 | 443 | 18.0 |
| 11-20 cedis | 627 | 13.1 | 292 | 12.8 | 333 | 13.5 |
| 21 cedis or more | 663 | 11.7 | 323 | 11.7 | 337 | 11.7 |
| Exposure to SHS at home ¥ | ||||||
| Yes | 1,239 | 23.7 | 608 | 25.7 | 617 | 21.6 |
| No | 4,410 | 76.3 | 2,092 | 74.3 | 2,304 | 78.4 |
| Exposure to antismoking media message £ | ||||||
| Yes | 2,694 | 48.8 | 1,274 | 47.6 | 1,403 | 49.6 |
| No | 2,825 | 51.2 | 1359 | 52.4 | 1,457 | 50.4 |
| Taught about the danger of tobacco use during the past 12 months € | ||||||
| Yes | 2,804 | 52.5 | 1,336 | 52.7 | 1455 | 52.5 |
| No | 1,743 | 29.8 | 838 | 28.2 | 898 | 31.1 |
| Don’t know | 1,092 | 17.8 | 521 | 19.2 | 565 | 16.4 |
| Region | ||||||
| Savanna/Northern | 1,862 | 17.5 | 899 | 17.6 | 951 | 17.1 |
| Middle/forest | 1,804 | 47.5 | 846 | 48.2 | 952 | 47.2 |
| Coastal | 1,998 | 35.0 | 962 | 34.3 | 1,026 | 35.8 |
| Current cigarette use ® | ||||||
| Yes | 162 | 3.0 | 92 | 3.2 | 66 | 2.7 |
| No | 5,053 | 97.0 | 2383 | 96.8 | 2651 | 97.3 |
| Current use of smokeless tobacco © | ||||||
| Yes | 211 | 3.6 | 104 | 3.2 | 105 | 3.9 |
| No | 5,146 | 96.4 | 2,451 | 96.8 | 2,675 | 96.1 |
| Current use of electronic cigarette™ | ||||||
| Yes | 349 | 5.8 | 148 | 5.5 | 198 | 6.1 |
| No | 5,081 | 94.2 | 2,440 | 94.5 | 2618 | 93.9 |
| Current use of waterpipe @ | ||||||
| Yes | 77 | 1.7 | 31 | 0.9 | 44 | 2.1 |
| No | 5,293 | 98.3 | 2,534 | 99.1 | 2,735 | 97.9 |
* 9 missing value
# 25 missing value
$ 13 missing value
¥ 15 missing value
£ 145 missing value
€ 25 missing value
® 449 missing value
© 307 missing value
™ 234 missing value
@ 294 missing value
β 28 respondents had missing gender.
REGIONAL DISPARITIES IN TOBACCO USE
In Figure 1, a map of Ghana has been used to present the regional disparities in the use of cigarettes, smokeless tobacco, electronic cigarette, and waterpipe tobacco (shisha). Compared to the other regions, tobacco use was higher in the Savanna/northern zone. In particular, the use of any tobacco product (cigarette, smokeless tobacco, electronic cigarette, or waterpipe tobacco) was 28.3, 7.0, and 4.8% in the Savanna/northern zone, middle/forest zone, and Coastal zone respectively.
Fig. 1.
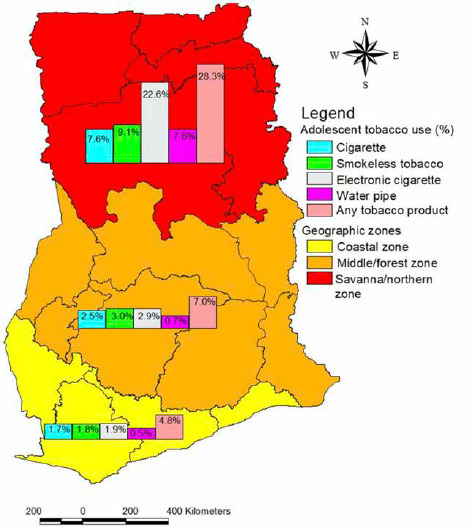
Regional disparities in tobacco use among junior high school students in Ghana.
USE OF TOBACCO BY RESPONDENT’S CHARACTERISTICS
Out of the 5,664 study participants, 99.9% (n = 5,659) responded to the questions on the use of cigarette, smokeless tobacco, electronic cigarette, or waterpipe tobacco. Among these 5,659 respondents, 2,706 were males, 2,926 were females and 27 students had missing gender. The results from the Chi-squared tests are presented in Table III. Overall, 9.9% (7.5-13.1%) of junior high school students in Ghana were using some form of tobacco product (cigarette, smokeless tobacco, electronic cigarette, or waterpipe tobacco). Among all respondents, age (p = 0.001), amount of pocket money (p < 0.001), and exposure to SHS at home (p < 0.001) were significantly associated with tobacco use among Junior High students in Ghana. Gender (p = 0.779), grade (p = 0.050), exposure to antismoking media message (p = 0.111), and taught about the danger of tobacco use during the past 12 months (p = 0.063) were not significantly associated with tobacco use.
Tab. III.
Profile of cigarette, smokeless tobacco, electronic tobacco, and/or waterpipe use.
| Overall (n = 5,659) | Males (n = 2,706) | Females (n = 2,926) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Characteristics | n/N * | % (95% CI)ɠ | P-value§ | n/N | % (95% CI) | P-value§ | n/N | % (95% CI) | P-value§ |
| Overall | 582/ 5,659 | 9.9 (7.5-13.1) | |||||||
| Gender | |||||||||
| Males | 288/ 2,706 | 9.9 (7.6-12.9) | 0.779 | - | - | - | - | - | - |
| Females | 287/ 2,926 | 9.4 (6.2-14.0) | - | - | - | - | |||
| Age | |||||||||
| 11 to 12 years | 32/136 | 28.1 (12.2-52.3) | 0.001 | 17/63 | 25.3 (11.9-45.9) | 0.003 | 15/70 | 32.0 (8.2-71.2) | 0.035 |
| 13 to 15 years | 472/5,112 | 9.0 (6.9-11.7) | 223/2,411 | 8.9 (6.7-11.7) | 242/2,678 | 8.5 (5.8-12.5) | |||
| 16 to 17 years | 77/402 | 15.4 (9.3-24.3) | 47/228 | 16.7 (10.5-25.6) | 30/173 | 13.6 (5.2-31.1) | |||
| Grade | |||||||||
| JHS1 | 263/2,102 | 8.5 (6.2-11.5) | 0.050 | 135/1,016 | 10.0 (7.1-13.9) | 0.790 | 127/1,083 | 6.9 (4.9-9.7) | 0.028 |
| JHS2 | 264/2,872 | 8.1 (6.3-10.3) | 131/1,350 | 9.0 (6.7-12.0) | 132/1,508 | 7.0 (5.2-9.4) | |||
| JHS3 | 47/661 | 14.0 (8.2-22.9) | 20/329 | 10.9 (5.6-20.0) | 25/327 | 15.7 (7.3-30.7) | |||
| Pocket money | |||||||||
| No pocket money | 122/872 | 18.2 (10.7-29.1) | < 0.001 | 58/430 | 13.3 (9.7-18.0) | 0.122 | 62/435 | 22.2 (10.5-40.8) | < 0.001 |
| Less than 2 cedis | 162/1,204 | 15.6 (11.3-21.2) | 74/572 | 13.0 (9.0-18.5) | 86/626 | 16.3 (10.8-23.8) | |||
| 2-5 cedis | 139/1,455 | 8.3 (5.5-12.3) | 75/701 | 10.3 (6.0-17.2) | 63/746 | 6.0 (3.6-9.7) | |||
| 6-10 cedis | 56/825 | 5.4 (3.2-9.2) | 29/382 | 5.8 (2.8-11.9) | 26/442 | 5.0 (2.2-10.7) | |||
| 11-20 cedis | 61/627 | 8.6 (5.5-13.3) | 31/292 | 10.7 (5.3-20.3) | 29/333 | 6.2 (3.9-9.9) | |||
| 21 cedis or more | 37/663 | 4.0 (2.2-7.0) | 19/323 | 4.5 (2.3-8.7) | 18/337 | 3.5 (1.7-6.9) | |||
| Exposure to SHS at home | |||||||||
| Yes | 327/1,236 | 24.8 (17.9-33.2) | < 0.001 | 156/608 | 22.5 (15.9-30.8) | < 0.001 | 166/615 | 27.3 (17.5-39.9) | < 0.001 |
| No | 247/4,408 | 5.1 (4.0-6.6) | 129/2,091 | 5.6 (4.0-7.7) | 116/2,303 | 4.1 (3.0-5.7) | |||
| Exposure to the antismoking media message | |||||||||
| Yes | 299/2,690 | 11.0 (7.9-15.1) | 0.111 | 145/1,273 | 9.8 (7.2-13.1) | 0.781 | 149/1,400 | 11.1 (6.5-18.5) | 0.117 |
| No | 245/2,824 | 8.3 (6.0-11.3) | 120/1,359 | 9.3 (6.6-12.9) | 125/1,457 | 7.2 (4.8-10.5) | |||
| Taught about the danger of tobacco use during the past 12 months | |||||||||
| Yes | 225/2,802 | 7.8 (5.7-10.6) | 0.063 | 127/1,335 | 9.0 (6.3-12.8) | 0.578 | 97/1,454 | 6.4 (4.0-10.3) | 0.021 |
| No | 189/1,742 | 11.5 (7.8-16.6) | 91/838 | 9.9 (6.6-14.6) | 95/897 | 11.5 (6.6-19.3) | |||
| Don’t know | 155/1,091 | 11.8 (8.2-16.8) | 64/521 | 11.9 (7.3-18.9) | 89/564 | 11.4 (7.8-16.5) | |||
* unweighted, N: total number of the respondent; n: number of respondents using some form of tobacco product (cigarette, smokeless tobacco, electronic cigarette, or waterpipe tobacco)
ɠ Weighted
§ p-value based on Chi-squared test.
In males, age (p = 0.003) and exposure to SHS at home (p < 0.001) were significantly associated with tobacco use. Among females, age (p = 0.035), grade (p = 0.028), amount of pocket money (p < 0.001), exposure to SHS at home (p < 0.001), and taught about the dangers of tobacco use during the past 12 months (p = 0.021) were significantly associated with tobacco use.
PREDICTORS OF TOBACCO USE
The results of the univariable and multivariable logistic regression analysis are presented in Table IV. From the univariate analysis, compared to students between 16 to 17 years, tobacco use was significantly lower among the 13 to 15 years group (OR: 0.55, 95% CI: 0.31-0.95, p = 0.005). Tobacco use was also significantly lower among those who receive 2 Ghana cedis (GH¢2) (0.35USD) or more pocket money compared to those who do not usually have pocket money (p < 0.001). Those exposed to SHS at home are also more likely to use tobacco compared to those who are not exposed (OR: 6.08, 95% CI: 4.08-9.05, p < 0.001).
Tab. IV.
Association between respondent’s characteristic and use of any tobacco product.
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| Characteristics | OR | 95% CI | Overall p-value | OR | 95% CI | Overall p-value |
| Gender | ||||||
| Males | 1 | 0.779 | 1 | 0.901 | ||
| Females | 0.94 | 0.62-1.43 | 0.98 | 0.67-1.42 | ||
| Age | ||||||
| 11 to 12 years | 2.15 | 0.76-6.11 | 0.005 | 2.27 | 1.02-5.03 | 0.002 |
| 13 to 15 years | 0.55 | 0.31-0.95 | 0.69 | 0.44-1.10 | ||
| 16 to 17 years | 1 | 1 | ||||
| Grade | ||||||
| JHS1 | 1 | 0.123 | 1 | 0.225 | ||
| JHS2 | 0.95 | 0.63-1.43 | 0.95 | 0.66-1.37 | ||
| JHS3 | 1.75 | 0.96-3.18 | 1.50 | 0.86-2.63 | ||
| Pocket money | ||||||
| No pocket money | 1 | < 0.001 | 1 | < 0.001 | ||
| Less than 2 cedis | 0.83 | 0.47-1.48 | 0.87 | 0.47-1.61 | ||
| 2-5 cedis | 0.41 | 0.20-0.83 | 0.46 | 0.22-0.94 | ||
| 6-10 cedis | 0.26 | 0.12-0.56 | 0.30 | 0.14-0.67 | ||
| 11-20 cedis | 0.43 | 0.20-0.92 | 0.48 | 0.22-1.00 | ||
| 21 cedis or more | 0.19 | 0.08-0.42 | 0.28 | 0.12-0.62 | ||
| Exposure to SHS at home | ||||||
| Yes | 6.08 | 4.08-9.05 | < 0.001 | 5.99 | 4.04-8.89 | < 0.001 |
| No | 1 | 1 | ||||
| Exposure to the antismoking media message | ||||||
| Yes | 1.37 | 0.93-2.03 | 0.112 | 1.17 | 0.85-1.62 | 0.321 |
| No | 1 | 1 | ||||
| Taught about the danger of tobacco use during the past 12 months | ||||||
| Yes | 0.65 | 0.43-1.00 | 0.097 | 0.56 | 0.35-0.88 | 0.043 |
| No | 1 | 1 | ||||
| Don’t Know | 1.04 | 0.64-1.68 | 0.95 | 0.58-1.54 | ||
In the multivariate analysis, age (p = 0.002), amount of pocket money (p < 0.001), exposure to SHS at home (p < 0.001), and being taught about the dangers of tobacco use during the past 12 months (p = 0.043) were significantly associated with tobacco use. The association is such that, tobacco use is significantly higher among those between 11-12 years compared to those between 16-17 years (OR: 2.27, 95% CI: 1.02-5.03), higher among those who receive GH¢ 2(0.35USD) or more pocket money compared to those who do not usually have pocket money, higher among those exposed to SHS at home (OR: 5.99, 95% CI: 4.04-8.89), and lower among those who have been taught about the dangers of tobacco use during the past 12 months (OR: 0.56, 95% CI: 0.35-0.88).
Discussion
This study used data from the Ghana 2017 GYTS to present nationally representative estimates of the profile and predictors, and also to assess regional disparities in tobacco use among junior high school students in Ghana. About 3.0% of Junior High School students smoke cigarettes, close to 6% use electronic cigarettes, close to 2% use water-pipe tobacco (shisha), and close to 4% also, use smokeless tobacco. The current decline in cigarette smoking compared to the previous findings could be described as an improvement in disguise, because other tobacco products’ use has emerged including smokeless tobacco use (3.6%), shisha use (1.5%), and electronic cigarette use (4.9%) [7, 17].
We also found that close to one-third of the participants were exposed to SHS at home, and had a six-fold likelihood of using tobacco compared to those who are not (OR: 6.08, 95% CI: 4.08-9.05, p < 0.001). Studies on adolescent tobacco use in SSA have reported a similar association of higher tobacco use among those exposed to SHS [17-20]. Mamudu et al. [19] in their study among adolescents in West Africa, indicated that exposure to SHS inside the homes ranged from 13.0 to 45.0%. The authors also associated parental or peer smoking behaviors with adolescent tobacco use in those countries, including Ghana [19]. Another study in West Africa (Nigeria) also indicates a similar finding [20]. The World Health Organization on Framework Convention on Tobacco Control (WHO FCTC) has emphasized that 100% smoke-free policies are the only proven way to effectively protect people from the harmful effects of SHS [21]. Other pressing issues cannot override the challenge of SHS exposure because tobacco alone kills more people than coronavirus pandemic (COVID-19) daily. Therefore, public education campaigns could inform parents of the dangers of SHS exposure for their wards and promote smoke-free households. Also, educating the youth about the health implications of SHS could make smoking socially offensive and prevent tobacco initiation and continue to use.
Tobacco use was lower among students who received education about the dangers of tobacco. This is consistent with other studies across SSA [22-24], even though other studies report conflicting findings [20, 25]. Certainly, school-based tobacco educational programmes have produced varying results in previous research with regards to their effectiveness in making a behavioural change among the youth who use tobacco and/or prevent initiation [26, 27]. Our findings together with other existing literature highlight the need for a comprehensive approach to youth tobacco prevention, such as strongly enforced smoke-free school policies, as well as engaging communities to include out-of-school youth in the programmes which may be more effective than only concentrating efforts on the classroom educational methods.
Among the three main ecological/epidemiological zones in Ghana, the Savanna/Northern zone which is most deprived and the poorest had the highest prevalence of tobacco use among the youth compared to the southern zone which has a better economic livelihood. We have reported similar findings in other studies in Ghana [17, 28, 29]. This suggests that the socioeconomic environment where the school is located may influence the smoking behaviours of students through several mechanisms, including exposure to tobacco advertising, availability of tobacco products, and the development of social norms that may facilitate the uptake of tobacco products.
Our study finding also indicates that pocket money was a predictor of tobacco use among the respondents. Respondents who received GH¢ 2(0.35USD) or more as pocket money were less likely to use tobacco compared to those who received no pocket money. This is in contrast to other studies [30, 31] that report a strong association between higher tobacco use among adolescents and increase pocket money. In our setting, the finding of higher tobacco use among those without pocket money compared with those with pocket money can be interpreted in the context of socioeconomic status. This study, however, agrees with other studies from Ghana [17, 28], which showed the northern zone (the most deprived and the poorest) had the highest prevalence of tobacco use among the youth compared to the southern zone which has a better economic livelihood. We recommend targeted policies that will create awareness about the dangers of tobacco use, especially among the youth.
Age was significantly associated with tobacco use; tobacco use was higher among 11-12 years as compared to 16-17 years (OR: 2.27, 95% CI: 1.02-5.03). Our findings agreed with other studies [18, 19, 23]. We consider children to be vulnerable, hence their rights to a smoke-free environment become paramount in the discussions on tobacco control. Therefore, for a successful implementation of tobacco control policies, children must be the prime target, because approximately 90% of adult smokers today started the habit in their teens [32], and also the tobacco industry sees children as a replacement for smokers [33].
Children and adolescents are a vulnerable population, hence need full protection from tobacco use. Countries with WHO FCTC comprehensive smoke-free implementation sets the obvious examples for the rest of the world to mimic.
STRENGTHS AND LIMITATIONS
The main strength of our study is the large sample size and robust sampling methodology which is nationally representative and with high response rates among schools and students. Limitations of our study include the use of self-administered questionnaires by students which may have led to under/over-reporting. However, some studies have reported high reliability of the results on self-administered youth smoking questionnaires [34,35]. Also, the survey was limited to school-going youth and this may not represent all youth in Ghana. We suggest further investigation on electronic cigarette use among the youth.
Conclusions
Multiple predictive factors influence youth smoking initiation and continuous use in Ghana. These findings call for the support and the adoption of multi-level comprehensive tobacco control strategies as proposed by the WHO-FCTC and other tobacco control bodies such as the Center for Disease Control’s Best Practice for Comprehensive Tobacco Control (CDC-Georgia Atlanta). There is the need to have policies and interventions developed to prevent early smoking initiation among the youth especially targeting children with lower socioeconomic status. Also, the younger teenagers may be targeted with special anti-smoking programmes both in and out of school. Finally, culturally accepted refusal skills and sensitization about the dangers of tobacco should be developed by the Ministry of Health/Health Promotion Division targeting particularly the youth in the northern zone, for effective prevention and/or reduction in tobacco uptake.
Figures and tables
Acknowledgements
Funding sources: this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
We are thankful to the Research and Development Division of the Ghana Health Service, Ministry of Health Ghana for allowing us to use the GYTS data. We are also grateful to the School of Public Health, Kwame Nkrumah University of Science and Technology for providing all the technical assistance for this study.
Footnotes
Conflict of interest statement
The authors declare no conflict of interest.
Authors’ contributions
DDL, FBO, and EOD conceived the idea and conceptualized the study. DDL and FBO conducted the data analysis and wrote the first draft. SA, AS, STA contributed significantly to the statistical analyses. KW, LB, SKF, JA, and EOD provided critical contributions to the discussion of the findings of the study. All authors contributed to the study design and review of the manuscript.
References
- [1].WHO. Tobacco - World Health Organization;tobacco fact sheet from WHO providing key facts and information on surveillance, second-hand smoke, quitting picture warnings, ad bans. WHO Newsroom/Factsheet; 2020. www.who.int/news-room/fact-sheets/detail/tobaccoWHO2020 (accessed Aug 30, 2020). [Google Scholar]
- [2].WHO-FCTC-Safeguarding children’s wellbeing through protection from tobacco smoke. WHO framework on Tobacco Control 2020. https://www.who.int/fctc/mediacentre/news/2019/childrens-wellbeing-through-protection-from-tobacco-smoke/en (accessed Nov 29, 2020).
- [3].Office on Smoking and Health (US). The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US) 2006. [PubMed] [Google Scholar]
- [4].Drope J, Schluger N, Cahn Z, Drope J, Hamill S, Islami F, Liber A, Nargis N. The Tobacco Atlas. Atlanta: 2018. Available: https://tobaccoatlas.org/topic/youth (Accessed: 20-Sep-2020). [Google Scholar]
- [5].Jafari A, Rajabi A, Gholian-Aval M, Peyman N, Mahdizadeh M, Tehrani H. National, regional, and global prevalence of cigarette smoking among women/females in the general population: a systematic review and meta-analysis. Environ Health Prev Med 2021;26:5. https://doi.org/10.1186/s12199-020-00924-y 10.1186/s12199-020-00924-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Townsend L, Flisher AJ, Gilreath T, King G. A systematic review of tobacco use among sub-Saharan African youth. J Subst Use 2006;11:245-69. https://doi.org/10.1080/14659890500420004 10.1080/14659890500420004 [DOI] [PubMed] [Google Scholar]
- [7].Ghana-GYTS; Centers for Disease Control and Prevention. Global Youth Tobacco Survey. Accra, Ghana: 2017. Available: https://nccd.cdc.gov/GTSSDataSurveyResources/Ancillary/DataReports.aspx?CAID=1 (accessed: 20-Sep-2020). [Google Scholar]
- [8].Harrell PT, Naqvi SMH, Plunk AD, Ji M, Martins SS. Patterns of youth tobacco and polytobacco usage: the shift to alternative tobacco products. Am J Drug Alcohol Abuse 2017;43:694-702. https://doi.org/10.1080/00952990.2016.1225072 10.1080/00952990.2016.1225072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Lauterstein D, Hoshino R, Gordon T, Watkins BX, Weitzman M, Zelikoff J. The changing face of tobacco use among United States youth. Curr Drug Abuse Rev 2014;7:29-43. https://doi.org/10.2174/1874473707666141015220110 10.2174/1874473707666141015220110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Glantz SA, Bareham DW. E-Cigarettes: use, effects on smoking, risks, and policy implications. Annu Rev Public Health 2018;39:215-35. https://doi.org/10.1146/annurev-publhealth-040617-013757 10.1146/annurev-publhealth-040617-013757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ghana-GYTS. Global Youth Tobacco Survey (GYTS), Ghana Fact Sheet. USA, Georgia Atlanta: 2009. Available: https://www.tobaccofreekids.org/assets/global/pdfs/en/Ghana_GYTS_2009_en.pdf (accessed: 20-Sep-2020). [Google Scholar]
- [12].Lopez B, Wang W, Schwartz SJ, Prado G, Huang S, Hendricks Brown C, Pantin H, Szapocznik J. School, family, and peer factors and their association with substance use in Hispanic adolescents. J Prim Prev 2009;30:622-41. https://doi.org/10.1007/s10935-009-0197-5 10.1007/s10935-009-0197-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Van Ryzin MJ, Fosco GM, Dishion TJ. Family and peer predictors of substance use from early adolescence to early adulthood: an 11-year prospective analysis. Addict Behav 2012;37:1314-24. https://doi.org/10.1016/j.addbeh.2012.06.020 10.1016/j.addbeh.2012.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Tjora T, Hetland J, Aarø LE, Øverland S. Distal and proximal family predictors of adolescents’ smoking initiation and development: a longitudinal latent curve model analysis. BMC Public Health 2011;11:911. https://doi.org/10.1186/1471-2458-11-911 10.1186/1471-2458-11-911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Baheiraei A, Soltani F, Ebadi A, Cheraghi MA, Rahimi Foroushani A. Family and peer risk factors as predictors of lifetime tobacco use among Iranian adolescents: gender similarities and differences. Glob J Health Sci 2014;6:63-75. https://doi.org/10.5539/gjhs.v6n4p63 10.5539/gjhs.v6n4p63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Mahabee-Gittens EM, Xiao Y, Gordon JS, Khoury JC. Continued importance of family factors in youth smoking behavior. Nicotine Tob Res 2012;14:1458-66. https://doi.org/10.1093/ntr/nts078 10.1093/ntr/nts078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Logo DD, Kyei-Faried S, Oppong FB, Ae-Ngibise KA, Ansong J, Amenyaglo S, Ankrah ST, Singh A, Owusu-Dabo E. Waterpipe use among the youth in Ghana: lessons from the Global Youth Tobacco Survey (GYTS) 2017. Tob Induc Dis 2020;18:47. https://doi.org/10.18332/tid/120937 10.18332/tid/120937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Jallow IK, Britton J, Langley T. Prevalence and determinants of tobacco use among young people in The Gambia. BMJ Glob Health 2017;2:e000482. https://doi.org/10.1136/bmjgh-2017-000482 10.1136/bmjgh-2017-000482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Mamudu HM, Veeranki SP, John RM, Kioko DM, Ogwell Ouma AE. Secondhand smoke exposure among nonsmoking adolescents in West Africa. Am J Public Health 2015;105:1823-30. https://doi.org/10.2105/AJPH.2015.302661 10.2105/AJPH.2015.302661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Itanyi IU, Onwasigwe CN, Ossip D, Uzochukwu BSC, McIntosh S, Aguwa EN, Wang S, Onoka CA, Ezeanolue EE. Predictors of current tobacco smoking by adolescents in Nigeria: interaction between school location and socioeconomic status. Tob Induc Dis 2020;18:13. https://doi.org/10.18332/tid/117959 10.18332/tid/117959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].WHO-FCTC. Who framework convention on tobacco control. Geneva, Switzerland: 2005. Available: https://www.who.int/tobacco/framework/WHO_FCTC_english.pdf?ua=1 (accessed: 20-Jun-2020). [Google Scholar]
- [22].Talley B, Masyn K, Chandora R, Vivolo-Kantor A. Multilevel analysis of school anti-smoking education and current cigarette use among South African students. Pan Afr Med J 2017;26:37. https://doi.org/10.11604/pamj.2017.26.37.7880 10.11604/pamj.2017.26.37.7880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Kapito-Tembo A, Muula AS, Rudatsikira E, Siziya S. Smoking among in-school adolescents in Dar Es Salam, Tanzania: results from the Global Youth Tobacco Survey. Tanzan J Health Res 2011;13.196-204. https://doi.org/10.4314/thrb.v13i3.64138 10.4314/thrb.v13i3.64138 [DOI] [Google Scholar]
- [24].Mamudu HM, Veeranki SP, John RM. Tobacco use among school-going adolescents (11-17 years) in Ghana. Nicotine Tob Res 2013;15:1355-64. https://doi.org/10.1093/ntr/nts269 10.1093/ntr/nts269 [DOI] [PubMed] [Google Scholar]
- [25].Siziya S, Rudatsikira E, Muula AS. Antismoking messages and current cigarette smoking status in Somaliland: results from the Global Youth Tobacco Survey 2004. Confl Health 2008;2:6. https://doi.org/10.1186/1752-1505-2-6 10.1186/1752-1505-2-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Thomas RE, McLellan J, Perera R. School-based programmes for preventing smoking. Cochrane Database Syst Rev 2013;2013:CD001293. https://doi.org/10.1002/14651858.CD001293.pub3 10.1002/14651858.CD001293.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Peterson AV, Jr, Kealey KA, Mann SL, Marek PM, Sarason IG. Hutchinson Smoking Prevention Project: long-term randomized trial in school-based tobacco use prevention results on smoking. J Natl Cancer Inst 2000;92:1979-91. https://doi.org/10.1093/jnci/92.24.1979 10.1093/jnci/92.24.1979 [DOI] [PubMed] [Google Scholar]
- [28].Debrah E. Alleviating poverty in Ghana: the case of Livelihood Empowerment against Poverty (LEAP). Afr Today 2013;59:41-67. https://doi.org/10.2979/africatoday.59.4.41 10.2979/africatoday.59.4.41 [DOI] [Google Scholar]
- [29].Ghana. Covid-19 & Tobacco. The Unuversity of Edinburgh, Usher Institute, UK: 2020. https://www.ed.ac.uk/files/atoms/files/covid19_and_tobacco_briefing_-_ghana.pdf (accessed Feb 06, 2021). [Google Scholar]
- [30].Rachiotis G, Barbouni A, Basagiannis A, Katsioulis A, Kostikas K, Mouchtouri V, Merakou K, Kremastinou J, Hadjichristodoulou CS. Prevalence and determinants of current cigarette smoking and secondhand smoking among Greek adolescents: the Global Youth Tobacco Survey (GYTS) 2013 study. BMJ Open 2020;10:e034760. https://doi.org/10.1136/bmjopen-2019-034760 10.1136/bmjopen-2019-034760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Asare S, Stoklosa M, Drope J, Larsen A. Effects of prices on youth cigarette smoking and tobacco use initiation in Ghana and Nigeria. Int J Environ Res Public Health 2019;16:3114. https://doi.org/10.3390/ijerph16173114 10.3390/ijerph16173114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].US Surgeon General; US Department of Health and Human Services. The health consequences of smoking – 50 years of progress: a report of the surgeon general. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center; 2014. [Google Scholar]
- [33].Perry CL. The tobacco industry and underage youth smoking: tobacco industry documents from the Minnesota litigation. Arch Pediatr Adolesc Med 1999;153:935-41. https://doi.org/10.1001/archpedi.153.9.935 10.1001/archpedi.153.9.935 [DOI] [PubMed] [Google Scholar]
- [34].Brener ND, Kann L, McManus T, Kinchen SA, Sundberg EC, Ross JG. Reliability of the 1999 youth risk behavior survey questionnaire. J Adolesc Health 2002;31:336-42. https://doi.org/10.1016/s1054-139x(02)00339-7 10.1016/s1054-139x(02)00339-7 [DOI] [PubMed] [Google Scholar]
- [35].Brener ND, Mcmanus T, Galuska DA, Lowry R, Wechsler H. Reliability and validity of self-reported height and weight among high school students. J Adolesc Health 2003;32:281-7. https://doi.org/10.1016/s1054-139x(02)00708-5 10.1016/s1054-139x(02)00708-5 [DOI] [PubMed] [Google Scholar]


