Summary
Ignác Fülöp Semmelweis (1818-1865) and Florence Nightingale (1820-1910) were two important personalities in the history of medicine and public health. They dealt with the problem of handwashing. Semmelweis is also known as the “father of hand hygiene”; just in 1847 he discovered the etiology and prophylaxis of puerperal sepsis and imposed a new rule mandating handwashing with chlorine for doctors. He also tried to persuade European scientific community of the advantages of handwashing. During the Crimean War, in Scutary (Turkey), Florence Nightingale strengthened handwashing and other hygiene practices in the war hospital where she worked and her handwashing practices reached a reductions in infections. Unfortunately the hygiene practices promoted by Semmelweis and Nightingale were not widely adopted. In general handwashing promotion stood still for over a century. During current pandemic SARS-CoV-2 (COVID-19) one of the most important way to prevent the spread of the virus is still to wash the hands frequently.
Keywords: History of public health, Hand washing, I. Semmelweis, F. Nightingale, Hand hygiene, SARS-CoV-2 (COVID-19)
Historical background
In the middle of the 19th century, two great personalities in the history of medicine, dealt with the problem of hand washing.
Ignác Fülöp Semmelweis (1818-1865) [Wikipedia commons]
On one side, Florence Nightingale (1820-1910), the founder of modern nursing; on the other one, the Hungarian doctor Ignác Fülöp Semmelweis (1818-1865).

Florence Nightingale (1820-1910)2 [Wikipedia commons]
Florence Nightingale, was born in Italy, in Florence in 1820 (Florence Nightingale’s wealthy parents were on a leisurely trip through Europe after their marriage).

[Florence Nightingale, An angel of mercy. Scutari hospital 1855 [Wikipedia commons]
Florence Nightingale revolutionized conditions in hospitals around the world, established nursing as a profession, and helped inspire the foundation of the Red Cross. She was known for her night rounds to aid the wounded, establishing her image as the “Lady with the Lamp”.
As a matter of fact, the original nickname was the ‘Lady with the hammer’, but the journalist of the Times, who described Nightingale’s activity in Scutari, decided that a hammer was not suitable for a young lady and transformed it into a lamp. Florence had received this nickname after having opened a cupboard with a hammer, as a doctor had refused to give her medicines for the wounded [1].
Ignác F. Semmelweis was born on 1 July 1818, in Buda (now Budapest), across the Danube River from Pest, before both cities became one. Educated at the universities of Pest and Vienna, Semmelweis received his doctor’s degree in Vienna in 1844 and was appointed assistant at the obstetric clinic of Vienna; he soon became involved in the problem of puerperal infection.
Germs were yet to be revealed, and in the 1840s it was still supposed that disease was caused and spread by corrupt smells in the air (miasma), originating from rotting corpses, dirt or shrubbery.
There was no theoretical impediment for doctors to perform autopsies in the morgue and then go to the maternity ward to visit a pregnant woman or deliver a baby, without washing their hands.
Semmelweis, who worked as an assistant at the First Obstetric Clinic of the Vienna General Hospital, did not understand why mortality for puerperal fever was higher in the wards frequented by medical students than in those where midwives were trained [2].

Statue of Semmelweis in front of Szent Rókus Hospital, Budapest, Hungary (erected in 1904, work of Alajos Stróbl) [Wikipedia commons]
When, in 1847, Jakob Kolletschka (1803-1847), one of Semmelweis’ colleagues, died after having pricked his finger with the knife that was being used in the autopsy, developing the same symptoms of puerperal fever, Semmelweis noted the similarity between these circumstances.
He postulated that cadaverous particles from the morgue were to blame, and that such particles on the hands of doctors were making their way also into women’s bodies during childbirth [3, 4].
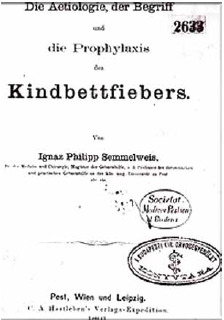
Semmelweis’s main work: Die Ätiologie, der Begriff und die Prophylaxis des Kindbettfiebers, 1861 (front page) [Wikipedia commons]
Therefore, he required students and doctors to wash their hands in a chlorinated lime solution before every patient contact and in particular after leaving the autopsy room. The results were amazing; following implementation of this measure, the mortality rate dramatically declined [5-7].
Despite these results, Semmelweis’ theory was rejected, above all because it undermined the prestige of the medical profession. Sadly this life-saving contribution by Semmelweis went unappreciated and he was forced to step down from his position and returned to Hungary [8].
In the same years, Florence Nightingale, during the Crimean war, pointed out that the unsanitary conditions of the soldiers were a major cause of death: she implemented hand washing and other hygiene practices in British army hospitals and her work led to reduced death rates from 42% to 2%.
Florence Nightingale wrote in her book about nursing: “Every nurse ought to be careful to wash her hands very frequently during the day. If her face, too, so much the better” [9].
Both Ignac Semmelweis and Florence Nightingale seized on statistics as a way of demonstrating the efficacy of different interventions and provided the evidence of their statements, but after almost two centuries, it is still necessary to remind the importance in maintaining a clear environment to best promote the health of patients.
Evolution of hand hygiene and health care: the pivotal role of “handwashing”
In 1847 Semmelweis demonstrated that the mortality rate among mothers delivering at the First Obstetrics Clinic at the General Hospital of Vienna was significantly lower when hospital staff cleaned their hands with an antiseptic agent [10].
Semmelweis is considered not only the father of hand hygiene, but his crucial intervention became also a model of epidemiology driven strategies to prevent infection [10].
Unfortunately, the “hand hygiene practices” promoted by Semmelweis and Nightingale were not commonly adopted. Handwashing promotion stood still for over a century. It was not until the 1980s, when a string of foodborne outbreaks and healthcare-associated infections led to public concern that the United States Centers for the Disease Control and Prevention identified hand hygiene as an important way to prevent the spread of infection.
The 1980s represent a milestone in the historical evolution of concepts of “hand hygiene” in health care, as the first national hand hygiene guidelines were published, followed by many others over the years in different countries [11, 12].
We must also remember that healthcare workers’ hands are the most common vehicle for the transmission of healthcare-associated pathogens from patient to patient and within the healthcare environment.
Contact transmission occurs when contaminated hands touch the mucosa of the mouth, nose, or eyes; a virus can also be transferred from one surface to another by contaminated hands, which facilitates indirect contact transmission.
Hand hygiene is the leading measure for preventing the spread of antimicrobial resistance and reducing healthcare-associated infections (HCAIs), but healthcare worker compliance with optimal practices remains low in most settings [13]
Nowadays, handwashing remains the number one tip during current pandemic for preventing the spread of Coronavirus (COVID-19). To make it work well, however, it must be done properly, with soap and water and chlorine solutions [14].
Droplets that come from coughing and sneezing spread many of the germs that cause respiratory (breathing) diseases, but some people may become infected by touching surfaces or objects that might be contaminated with respiratory droplets, or after touching persons who suffer from respiratory symptoms [15].
Therefore, hand hygiene is really important to prevent the spread of the COVID- 19 virus. It also interrupts transmission of other viruses and bacteria causing common colds, flu and pneumonia, thus reducing the general burden of disease.
Although awareness of the importance of hand hygiene in preventing infection with the COVID-19 virus is high, access to hand hygiene facilities that include alcohol-based hand rubs as well as soap and water is often suboptimal in the community and in health care facility settings, especially in low-and middle-income countries [15].
For this reason, hands must be washed regularly: proper handwashing not only reduces the spread of COVID-19, as it can prevent the spread of other viral illnesses such as cold and flu. Handwashing also reduces the risk of getting other easily spread infections.
During a global pandemic, one of the cheapest, easiest, but most important ways to prevent the spread of a virus is, first of all, to wash the hands frequently with soap and water, as Ignàc Semmelweis and Florence Nightingale demonstrated more than half a century ago, in the mid-nineteenth century [16].
Semmelweis and Nightingale’s teaching is still topical today; but after over more than a century and a half, did we really learn the lesson?
Acknowledgements
Funding sources: this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Conflict of interest statement
The authors declare no conflict of interest.
Authors’ contributions
MM and DL conceived the study, drafted the manuscript, revised the manuscript and performed a search of the literature. Both authors critically revised the manuscript, have read and approved the latest version of the manuscript.
References
- [1].Borghi L, Lippi D. La penna di Florence Nightingale (Firenze 1820 - Londra 1910). Aforismi e riflessioni. Firenze: A. Pontecorboli; ed. 2020. [Google Scholar]
- [2].McIntyre N. Ignác Fülöp Semmelweis (1818-65). J Med Biogr 2009;17:22. https://doi.org/10.1258/jmb.2008.008008 10.1258/jmb.2008.008008 [DOI] [PubMed] [Google Scholar]
- [3].Semmelweis Ignaz. (1861). Etiology, concept and prophylaxis of childbed fever. K. Codell Carter (translator and extensive foreword). University of Wisconsin Press 1983, pp. 87-8. [Google Scholar]
- [4].Lancaster HO. Semmelweis: a rereading of Die aetiologie. Part I: Puerperal sepsis before 1845. Die aetiologieJ Med Biogr 1994;2:12-21. https://doi.org/10.1177/096777209400200104 10.1177/096777209400200104 [DOI] [PubMed] [Google Scholar]
- [5].Raju TN. Ignác Semmelweis and the etiology of fetal and neonatal sepsis. J Perinatol 1999;19:307-10. [DOI] [PubMed] [Google Scholar]
- [6].La Rochelle P, Julien AS. How dramatic were the effects of handwashing on maternal mortality observed by Ignaz Semmelweis? J R Soc Med 2013;106:459-60. https://doi.org/10.1177/0141076813507843 10.1177/0141076813507843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Sonja Schreiner. Ignaz Semmelweis: a victim of harassment? Med Wochenschr 2020;170:293-302. https://doi.org/10.1007/s10354-020-00738-1 10.1007/s10354-020-00738-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Citrome L. Happy birthday Ignác Semmelweiss! Now, let’s all wash our hands! Int J Clin Pract 2018;72:e13256. https://doi.org/10.1111/ijcp.13256 10.1111/ijcp.13256 [DOI] [PubMed] [Google Scholar]
- [9].Nightingale F. Notes on nursing: what it is and what it is not. London: Harrison and Sons; 1860. [Google Scholar]
- [10].WHO Guidelines on Hand Hygiene in Health Care. First global patient safety challenge clean care is safer care. World Health Organization, WHO Library Cataloguing-in-Publication Data, 2009. [PubMed] [Google Scholar]
- [11].Simmons BP. Guidelines for hospital environmental control. Section 1. Antiseptics, handwashing, and handwashing facilities. In: Centers for Disease Control and Prevention (CDC), ed. CDC Hospital infections program (HIP) guidelines for prevention and control of nosocomial infections. Atlanta, GA, Springfield; 1981, pp. 6-10. [Google Scholar]
- [12].Garner JS, Favero MS. CDC guideline for handwashing and hospital environmental control, 1985. Infect Control 1986;7:231-43. https://doi.org/10.1017/s0195941700084022 10.1017/s0195941700084022 [DOI] [PubMed] [Google Scholar]
- [13].Allegranzi B, Pittet B. Role of hand hygiene in healthcare-associated infection prevention. J Hosp Infect 2009;73:305-15. https://doi.org/10.1016/j.jhin.2009.04.019 10.1016/j.jhin.2009.04.019 [DOI] [PubMed] [Google Scholar]
- [14].Abigail M, Shannon H, Tiffany W, Emma B. Hand hygiene: a quality improvement project. Biomed J Sci & Tech Res 2017;1(7). https://doi.org/10.26717/BJSTR.2017.01.000601 10.26717/BJSTR.2017.01.000601 [DOI] [Google Scholar]
- [15].WHO. Interim Recommendation. 1 April 2020. [Google Scholar]
- [16].Hillier MD. Using effective hand hygiene practice to prevent and control infection. Nurs Stand 2020;35:45-50. https://doi.org/10.7748/ns.2020.e11552 10.7748/ns.2020.e11552 [DOI] [PubMed] [Google Scholar]


