Abstract
The novel and unprecedented Coronavirus disease (COVID-19) pandemic has negatively impacted most nations of the world within a short period. While its disproportionate social and spatial variability has been established, the reality in Nigeria is yet to be studied. In this paper, advanced spatial statistical techniques were engaged to study the burden of COVID-19 and its risk factors within the first quarter (March–May) of its incidence in Nigeria. The spatial autocorrelation (Moran's I) test reveals a significant but marginal cluster of COVID-19 occurrence in Nigeria (I = 0.11, p < 0.05). A model comparison between ordinary least square (OLS) and spatial error model (SER) was explored having checked for multicollinearity in the dataset. The OLS model explained about 64% (adjusted R2 = 0.64) of variation in COVID-19 cases, however with significantly clustered residuals. The SER model performed better with randomly distributed residuals. The significant predictors were population density, international airport, and literacy ratio. Furthermore, this study addressed the spatial planning implications of the ongoing disease outbreak while it advocates transdisciplinary approach to urban planning practices in Nigeria.
Keywords: COVID-19, Crude rate, Nigeria, Spatial dependence, Spatial planning, Spatial statistics
1. Introduction
The novel and unprecedented Coronavirus disease (COVID-19) pandemic has negatively impacted nations of the world. Within a short period of the disease outbreak from Wuhan, China in December 2019; the COVID-19 pandemic has become a global threat to the livelihood, survival, and sustainability of humans. With nearly ten million confirmed cases and almost half million deaths across the globe, the disease remains a shock to the global health system. Consequently, this positions COVID-19 and wider issues to scholarly attention and debate. For example, robust biological diagnosis and explanation to the evolution of the disease has been established (Bai et al., 2020; Fauci, Lane, & Redfield, 2020). Beyond the sphere of the biological scientists, the spatial variability of COVID-19 is gradually gaining momentum (Miller, Bhattacharyya, & Miller, 2020; Mollalo, Vahedi, & Rivera, 2020). However, being a newly emerged disease, more and robust research needs to be conducted to gain deeper understanding on the disease.
The critical assertions of the scarcity of information about COVID-19, along with the lack of complete knowledge of the biological, sociological, and fiscal genesis or impact of the disease calls for a multi-disciplinary examination of people and place susceptibility to the disease pandemic (Fauci et al., 2020). This study therefore stems from the evidence of importation of COVID-19 to Africa (Gilbert et al., 2020) and the global recent call for novel submissions on the ongoing global pandemic, towards a good chance to observe the spatial profile of the disease in Nigeria. The documented relevance of geography to disease such as COVID-19 (Desjardins, Hohl, & Delmelle, 2020), social and spatial heterogeneity (Mollalo et al., 2020) has been established. The space-time surveillance and monitoring of the coronavirus pandemic is important to the effective management of disease response, intervention, and resource allocation to places of utmost need. This is peculiarly far more important in Sub-Saharan Africa (SSA) and Nigeria as a nation where the disease exposure is high. In SSA, there has been reported challenge of dealing with the disease burden and health status of African by the global health community (Habte, Dussault, & Dovolo, 2004). The burden, according to the author was because of ill functioning health system that is devoid of modern health technologies, limited financially capability and poor health procedure and capacity implementation.
Describing Africa's exposure to disease pandemics and incidences, Gilbert et al. (2020) study presented few Africa countries (Ethiopia, Algeria, Egypt, South Africa, and Nigeria) to be of high vulnerability to imported COVID-19. It was envisaged that the capacity of many Africa countries including the study area remains minimal, as human resources and testing capacity can be said to be unavailable or generally below par. This health delivery system condition promptly increases the vulnerability of countries and states from medium to high risk. The poor state of the African healthcare delivery system is further compounded by the excess pressure of limited available health infrastructure and personnel. Mainly traced to high population concentration in urban space (Ersoy, 2017), which is evident in the low health workers patient ratio (Habte et al., 2004; Omuta et al., 2014). This health service delivery condition has been reported to be as a result of the unplanned urbanisation and population explosion of the continent (Adewoyin, Chukwu, & Sanni, 2018; Aliyu & Amadu, 2017; Elsey et al., 2019; Farrell, 2018). Buttressing this, McLafferty (2010) has expressed the opinion of the relationship between poor infrastructure availability and accessibility, disease pandemic incidence and spread of urban slums in Africa. This is because there exists a disparity between urban health service and population growth and concentration (Matthews et al., 2010) - thereby resulting to a disadvantaged and vulnerable urban setting.
We argue that the dearth of robust and openly available data makes it difficult to track and document the epidemiological trends and outcomes of COVID-19. Thus, through the meta-syncing of scarce data with GIS and the identified possible risk factors of poverty, access to improved water source, availability of airport, income, gross domestic product (GDP), literacy, population density, unemployment rate (Chung, 2015; Curtis, Sparrow, Ghebreyesus, & Netea, 2020; Diwakar, 2020; Lawyer, 2015; Madhav et al., 2017; World Health Organization and the United Nations Children’s Fund(UNICEF), 2020) were tested to establish the risk factors and variation of the COVID-19 pandemic in Nigeria.
Most cities in Nigeria (such as Kano, Kaduna, Katsina, Ibadan, Lagos, and Dutse) as administrative or commercial headquarters of States (Kano, Kaduna, Katsina, Oyo, Lagos, and Jigawa) are characterized by increased mobility due to the presence of airport and high spatial connectivity (Otuoze, Hunt, & Jefferson, 2021; Taiwo & Olumoyegun, 2020). Therefore, the authors argue that spatial connectivity which is defined by people interaction within a density space and various land-uses can be hypothesised to be a risk factor to the disease spread. This aligns with the assertions of Guo (2007), that population density and space connectivity increase the spread and transportation of disease from one place to another. In the same instance, Centres for Disease Control and Prevention (2020) has attributed poverty, overcrowding (as embedded in population density) and certain occupation to be a risk factor to covid-19 pandemic. In the same instance, the role of income as a determinant of health-related inequality (Nwosu & Oyenubi, 2021) remains a somewhat covariate factor that needs to be investigated in face of COVID-19 pandemic Nigeria. We alluded to the nation income-wealth within the ideology of gross domestic product to be able to predict infection spread and as Mugunga et al. (2021) buttressed that testing and detection may be impacted due to national income wealth and resource of a country. The worse off effect from limited GDP and national resource is expected in low- and middle-income countries (Bong et al., 2020).
The authors owing to scarce open data on the job description and income of covid-19 patients argue that job unemployment and income can be a predictor to COVID-19 variations. Studies (Ndaw, 2020; Popoola, 2020) have reported that with 63% of urban dwellers in Sub-Saharan Africa lacking access to water, the regular washing of hands a preventive measure to the spread of Covid-19 remains difficult. This according to Da Silva, Silva, Alexandre, and Morgado (2020) and Lopes and McKay (2020) will be further impacted by misinformation and low level of literacy. The view was that literacy will serve as a support mechanism to manage COVID-19 conception and promote informed response and management. Owing to this, we hypothesis that State literacy can be a risk factor in covid-19 prevalence in Nigeria.
In fact, Anim and Ofori-Asenso (2020) alluded that with water scarcity, struggle and queues social distancing might be impossible in Africa and Nigeria. This resource struggle and stress and exposure to COVID-19 is further compounded by high population density in urban Nigeria (Popoola, Olatunde, et al., 2020,b) and Africa (Ilesanmi, Oderinde, & Afolabi, 2020; Osayomi et al., 2020). It was further argued by Alkire, Dirksen, Nogales, and Oldiges (2020) and Sunkari, Korboe, Abu, and Kizildeniz (2020), that the high-risk factors of nutrition, water, sanitation, hygiene, air pollution which necessarily defines poverty characterises about 216 million people in Sub-Sahara Africa. In Nigeria, the writer reported that Nigeria States: Lagos and Abuja will be more hit by covid-19 owing to the poverty and its related indicators exposures in such area. In Lawal and Nwegbu (2020) and Osayomi et al. (2020), it was reported that population size and air traffic had significant impact on both COVID-19 prevalence, morbidity and mortality in Nigeria and West Africa. The value addition in this study was now to investigate if availability of airport in any state in Nigeria can be a risk factor to COVID-19.
However, no matter how the risk factors can be easily hypothesised, explaining the variation in COVID-19 crude rate in Nigeria remains imperative to disease putative causal factors and outcomes. Despite its spontaneity and global acceptance of the pandemic capacity to be a leading cause of death, disrupt livelihood, and shape of space and places, its precise burden is not clear in Low-and Middle-Income Countries (LMIC) particularly in Nigeria. The approach of the study is the geospatial analysis of COVID-19 (based on open data from Nigeria Centre for Disease Control — https://ncdc.gov.ng/) and risk factors in Nigeria with robust spatial statistical techniques and packages in R version 3.6.2 (Open source software). Through this, we were able to model COVID-19 variation from place to place, towards the formulation of place-based interventions and resources optimization. This paper addressed the following set of objectives: what is the spatial pattern of COVID-19 in Nigeria? what are the possible variables driving this process? and what is the spatial planning and policy implications of COVID-19 in Nigeria?
2. Materials and methods
2.1. Data collection and preparation
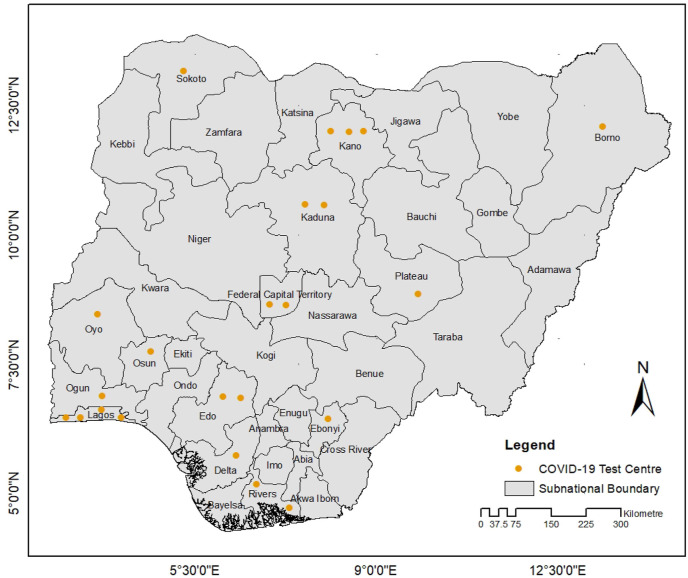
Subnational COVID-19 data and covariates for each of the 36 states including the FCT were sourced from the public domain. For this study, the outcome variable is the COVID-19 crude rate. This was determined by dividing the total number of COVID-19 cases in each state sourced from NCDC with the estimated population for the year 2020. The population of each state was estimated with the growth rate (2.6%) of Nigeria (World Bank, 2018). The covariates sourced from the National Demographic and Health Survey (NDHS, 2018-https://dhsprogram.com/pubs/pdf/FR359/FR359.pdf) and other secondary sources as described in section (2.2) are broadly categorized into two, which are socio-economic characteristics (population, gross domestic product, literacy rate, percentage of people living below one dollar ($), percentage of people with limited access to food, improved water source) and mobility characteristics (availability of local and international airport). The gross domestic product for each states were gotten from National Bureau of Statistics. The COVID-19 data is publicly available on the NCDC website. However, the granularity of this data is not robust enough. Some variables such as subnational age characteristics and sex of the subjects are not made available (www.ncdc.gov.ng). This impedes our ability to calculate age-adjusted rate of COVID-19 in Nigeria. However, according to the report sourced from NCDC, the most affected age group is between 31 and 40 years of age. This group account for about 24% of COVID-19 infection rate in Nigeria (Hassan et al., 2020; Amzat et al., 2020; NCDC, 2020- https://ncdc.gov.ng/diseases/sitreps). Additionally, we had limited access to mobility related data because of its paucity, nature, and administrative constraints. The reported cases of COVID-19 in Nigeria are very low which is because of low national testing capacities and sparse testing facilities as depicted in Figure (1) . As at the month of May 2020, Nigeria has a total of 23 testing centres in 15 states.
Fig. 1.
Subnational boundaries with COVID-19 test centres in Nigeria.
2.2. Definition of covariate and data sources
Gross Domestic Product (GDP): GDP refers to the final products at market prices produced by all resident units in a country (or a region) during a certain period of time. GDP is the core indicator of the national accounts, and also an important indicator to measure the economic conditions and the level of development of a country or region.
Population: This is defined based on the total number of persons in the state. The number is based on the last population census in the country.
Literacy rate: The National Literacy Survey (NLS), was carried out by the National Bureau of Statistics (NBS). The main purpose of the survey was to determine the magnitude, levels and distribution of adult literacy and obtain comprehensive data and information with a view of identifying issues of concern, which needs to be addressed in the promotion of adult literacy at grass root level in Nigeria. Literacy rate is measured by the percentage of persons above fifteen years of age who is able to read and write.
Percentage of people living below one dollar ($): The Nigerian National Bureau of Statistics (NBS) released the 2018/19 Nigerian Living Standards Survey (NLSS) providing the first official estimates of poverty and welfare in Nigeria in almost a decade. In Nigeria, the poverty line is set at 1 U.S. dollar per day (about 334 U.S. dollars) per year (Nigeria Socio-Economic Indicators, November 2012 - https://nigeria.opendataforafrica.org/NSEI2012Nov). The dollar per day refers to the World Bank's Purchasing Power Parity (PPP) index, which defines poverty as the proportion of those living on less than US$1 per day poverty line.
Percentage of people with limited access to food: The food poor or access approach is one of the absolute poverty measurement approach. The food poverty also known as the Food Energy Intake measure of poverty according to the NBS is achieved by obtaining the food basket of the poorest 40 percent of the population. Then compute the food expenditure that can give 3000 calorie per day based on the national food basket for the poorest 40 percent National bureau of Statistics, 2012). Varrella (September 22, 2021) reported that in Nigeria, a person having under 87.8 thousand Naira (about 213 U.S. dollars) in a year available for food was living below the poverty line according to Nigerian national standards.
Improved water source: The data on the improved water source was gotten from NBS website. The data was collected and lastly modified in 2013. Improved water source assessment according to the National Bureau of Statistics are technologies that include household connections, public standpipes, borehole, protected dug well, protected spring, and rainwater harvesting (National Bureau of Statistics, 2013).
Local airport: Data on the location of local airport was gotten from Federal Airports Authority of Nigeria (FAAN) (https://www.faan.gov.ng/). States with local airport were coded 1, while state without local airports were coded 0.
International airport: Data on the location of local airport was gotten from FAAN. States with local airport were coded 1, while state without local airports were coded 0.
2.3. Spatial autocorrelation modelling
Spatial data observes the assumption of dependence (autocorrelation). Spatial autocorrelation simply refers to the relationship between the value of variable (y) in location i with itself in another neighbouring location j within same geographical space. The spatial autocorrelation test can be examined at two levels, which are global (global spatial autocorrelation) and local (local spatial autocorrelation). Broadly, the measure of spatial autocorrelation can be actualized through Geary's C and Moran's I statistics including their corresponding randomization tests (permutation inference). In this study, Moran's I statistics was utilised. The global Moran's I (Moran, 1950) measures spatial autocorrelation in a dataset. Its value ranges from −1 to 1. Negative value of 1 means dispersion (clustering of dissimilar values), positive value of 1 depicts clustering (clustering of similar values) while 0 or values very close to 0 implies complete spatial randomness (CSR), that is no autocorrelation (Tu & Xia, 2008). However, this statistic lacks the capability to determine structural instability in the dataset. The further decomposition of global to local spatial statistical model was put forward by Anselin (1995), which led to development of local indicators of spatial association (LISA) as tool capable of detecting locations of spatial non-stationarity or outliers. Simultaneously, this can be used to describe significant correlation at specific location as local spatial clusters or correlation between observations and neighbouring observation (hot spots). Equation (1) describes the component of Moran's I statistics. Similarities between locations (i,j) is calculated as the product of the difference between Xi and Xj with the overall mean. ω implies the spatial weight between observation i and j, which is not discussed into details. Equation (2) describes LISA statistics.
| (1) |
| (2) |
2.4. Spatial regression modelling
The standard linear regression like Ordinary Least Squares (OLS) models relationship between response variable (y) and set of explanatory variables (x). Linear regression like in classical statistics assume that samples are independently distributed, thus, ignores the assumption of dependency in spatial data. Nevertheless, the OLS functions as global models in spatial data science with advantage of its diagnostic features to test for clustering among model standard errors. Hence, the need for sophisticated spatial (global) models such as the spatial autoregressive model (SAR), spatial error model (SEM) and spatial durbin model (SDM) which accounts for spatial dependency in the data set. The spatial models are extension of the OLS. SLM is simply addition of a spatially lagged variable (Y) to the OLS regression model (see equation (3)) which implies that the dependent variable in location i will affect adjacent observation in location j. The SEM (Equation (4)) introduces spatial effects into the error terms (Osayomi, 2019), while the SDM (Equation (5)) introduces lagged dependent (γ) and covariates (X) i.e an extension of SAR model (Atikah, Rahardjo, & Lestari, 2020).
| (3) |
| (4) |
| (5) |
where are defined by the scalar spatial autocorrelation parameter ρ. γand X remains the vector of observation on the dependent and explanatory variable, W is the neighbourhood matrix while ε is the disturbance (error term); the additional term is a 12 × 1 vector of regression coefficients for the lagged independent measures (Tabb, McClure, Quick, Purtle, & Diez Roux, 2018).
2.5. Analysis
The analytical approach to this study are in three folds. First, spatial autocorrelation among the observation (COVID-19 crude rate) was determined using the Global and Local Moran's I statistical tool. Second, the covariates (independent variables) were included and modelled using the OLS after checking for multicollinearity with the correlation matrix, and spatial dependence in the residuals was tested which informs the need for spatial modelling. Third, spatial dependence and sensitivity analysis was conducted with the lagrange multiplier test to determine the choice of spatial regression technique (Anselin, 2010)..
3. Results
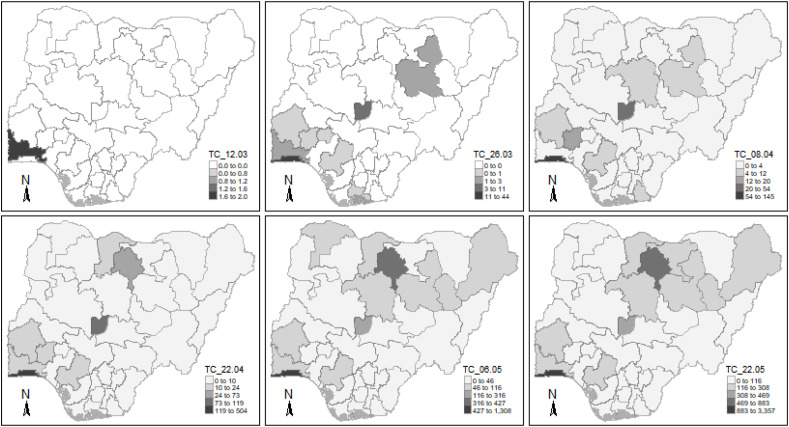
Nigeria recorded index case on the February 27, 2020 in Ogun State. Ever since, the reported cases or total cases (TC) of COVID-19 have been disproportionately increasing across the country as shown in Fig. 2 .
Fig. 2.
Biweekly temporal trend of COVID-19 cases in Nigeria.
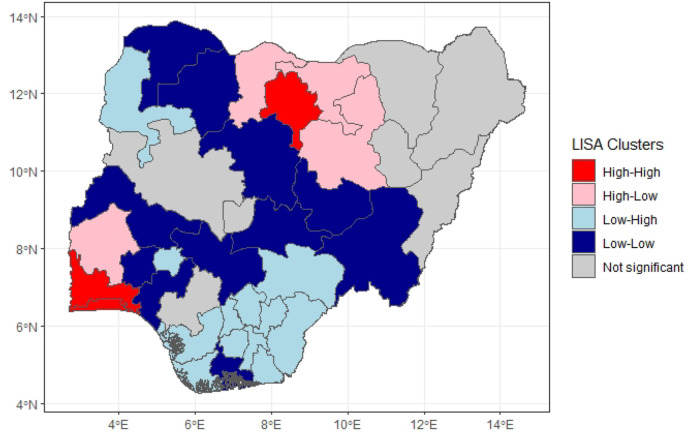
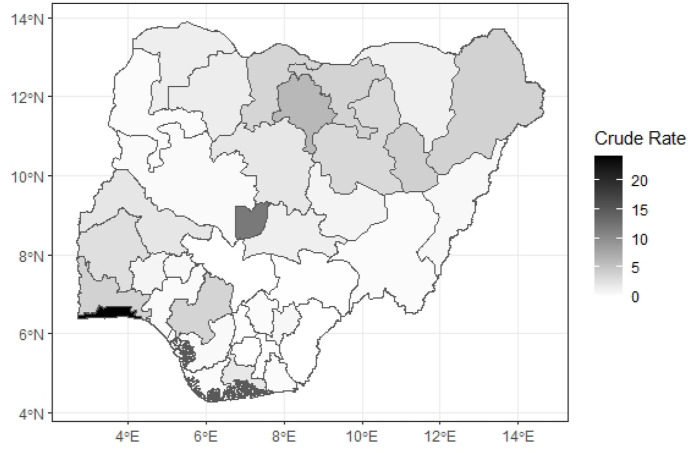
Apparently, Nigeria is experiencing low cases of Covid-19 which is likely due to low testing and reporting rate. Nevertheless, about four weeks into the virus outbreak, a diagonal direction from the South (Lagos) to Central (Abuja) and North (Kano) was observed, and therefore becoming the hot spots of the virus with cases over 500 cases each. This posits the risk variability of COVID-19 in Nigeria. Global Moran's I was utilised to ascertain and gain insight on the potential of spatial dependency in the dataset. The result shows significant but marginal cluster of 0.1 (P = 0.03) of COVID-19 crude rate in Nigeria. A further decomposition of Global Moran's I with the LISA statistics captured the locations with significant high values (p < 0.5) above the national average (Fig. 4). Lagos, Ogun and Kano states were found to be hot spots of the disease burden in Nigeria. For example, in Lagos state, more than 20 out of every 100,000 persons are reported to have contacted the disease compared to places like Cross Rivers which is 0 (Fig. 3 ). Before the development of the OLS model, multicollinearity was accounted for with the aid of the correlation matrix (correlogram). Three variables were found to be highly correlated (gross domestic products, percentage of people with limited access to food and literacy ratio). Intuitively, literacy ratio was retained while the other two were expunged from the dataset. The result of the OLS is reported in Table 1 . The significant variables (p < 0.05) are population density (0.007) and literacy ratio (−0.11). The OLS explains approximately 64% (R2 = 0.643) of the variation in COVID-19 crude rate in Nigeria. Based on the regression coefficients, the COVID-19 crude rate is positively related with population density, and inversely related with literacy ratio. This implies that places with high population density had high rate of COVID-19 cases, while areas with low education had high rate of COVID-19.
Fig. 4.
Crude rate spatial association of COVID-19 in Nigeria.
Fig. 3.
Subnational crude rate of Covid-19 in Nigeria per 100,000 persons.
Table 1.
OLS and SEM models summary with covariates of COVID-19 crude rate in Nigeria.
| Variable | Coefficient (95% CI) |
P-value |
||
|---|---|---|---|---|
| OLS | SEM | OLS | SEM | |
| Intercept | 10.643 (1.63–19.66) | 2.47 (−5.62–10.55) | 0.0222* | 0.54969 |
| Population density | 0.007 (0.005–0.009) | 0.006 (0.004–0.007) | 3.17e-07*** | 2.973e-13*** |
| Literacy ratio | −0.11 (-0.19–0.03) | −0.05 (−0.13–0.03) | 0.0114* | 0.22798 |
| Local airport | 1.875 (-0.17 – 3.92)) | 0.91 (−0.52–2.34) | 0.0709 | 0.21370 |
| % Below 1$ | −0.07 (−0.16–0.02) | −0.014 (−0.08–0.05) | 0.1143 | 0.66619 |
| Improved water source | −0.009 (−0.06–0.04) | 0.02 (−0.02–0.06) | 0.7255 | 0.38331 |
| International airport | 1.543 (−1.47–4.56) | 2.25 (0.18–4.32) | 0.3044 | 0.03302* |
| Adj. R2 | 0.643 | – | 9.014e-07 | – |
| AIC | 183.3 | 178.84 | ||
| Lambda (λ) | – | 0.53 (0.38–0.92) | – | 0.010892 |
0.05, *p < 0.05; **p < 0.01; ***p < 0.001.
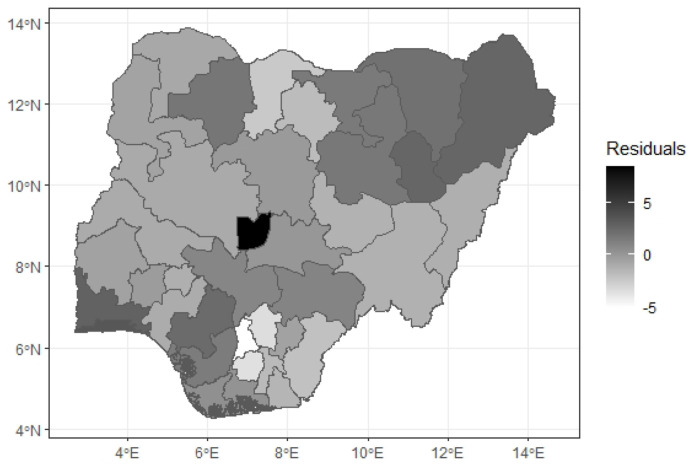
The OLS model does not account for spatial dependency, thus makes it inconsistence in its spatial predictions. This was ascertained by testing for clusters in the OLS error term. The OLS model residuals are spatially clustered (0.17) and significant (p = 0.009). The residuals of the OLS model is depicted by Fig. 5 . Further, the lagrange multiplier test conducted reveals spatial dependence in the error term meaning the residuals are not normally distributed (spatially dependent) and SEM as most appropriate model for this study (LMerr = 4.4301, p = 0.035). The other spatial models (SAR, SDM) were not significant.
Fig. 5.
OLS model residual map.
The clustering of residuals in the OLS model makes it less applicable model. Therefore, the spatial error model which accounts for spatial dependence through the introduction of spatially unstructured (random error) and spatially structured (correlated error) residuals was engaged (Tabb et al., 2018). The SEM model performed slightly better than the OLS model as the AIC reduced from 181.4 to 178. Additionally, the residuals of the SEM model is not significantly clustered (P = 0.33). Population density (0.006), remains significant while other covariates are not as shown in Table 1. The SEM model is a better model in the explanation of the geographic distribution and associated factors in Nigeria.
4. Discussion
The generated results demonstrate the risk variability of COVID-19 from place to place in Nigeria. Hence, it is useful for formulation of place-based policies. Crude rate of COVID-19 affects people disproportionately in Nigeria while the hotspots are in the most urbanized places of Nigeria like Lagos, Ogun, Abuja and Kano states. According to our study, there is strong relationship between crude rate of COVID-19 and population density. A 1% increase in population density is associated with about 0.006% increase in incidence rate of COVID-19. This justifies the result of Tarwater and Martin (2001) which opined the effect of various population density in the spread of disease incidences. According to Feigin, Garg, and Christie (2020), the ease with which virus spreads through a population is not determined solely by population density. Health crisis develop mostly when the population get too dense, resulting from overpopulation (Manisalidis, Stavropoulou, Stavropoulos, & Bezirtzoglou, 2020; Neiderud, 2015; Nkosi, Haman, Naicker, & Mathee, 2019; Popoola et al., 2015). Overpopulation, however, is frequently coupled with deterioration in the quality of living conditions and hygiene, but as a result, the prevalence of agent transmission is generally quite high in these kinds of environments. Iterating the effect of high population concentration in disease spread, in Kano State, Northern Nigeria, Ngwa et al. (2021) reported that ‘over’ population was a driver of cholera disease hotspot. It was further emphasised that in Lagos state, unplanned urbanisation, population influx and limited access to social amenities are major factor in the spread of disease (Aliyu & Amadu, 2017). Put into context, Amoo et al. (2020) argued that population density is a factor in disease management and physician-patient contacts. Therefore, congested neighbourhoods or highly inhabited urban areas may serve as breeding grounds for infectious agents, facilitating their evolution, especially in the case of viruses and bacteria. The rapid cycling of bacteria or viruses between humans and other hosts, such as rats or mice, can result in the creation of novel strains.
Likewise, the country experience in this uncharted COVID-19 period shows the need for pragmatic measures to curb the propagation of COVID-19 in Lagos State being the urban-hub of Nigeria. In the last three decades, global south has experienced significant increase in population. While this is true, the future significant population growth will be experienced in Africa. Nigeria is one of the countries with fastest growing population in Africa with estimated population of about 200 million people with average population growth rate of 2.6% (World Bank, 2018). More population increasing vulnerability to infectious disease especially when the urbanization level is high.
The study evidence shows that the presence of international airport has high impact on incidence of COVID-19 in Nigeria. According to our findings, a total increase COVID-19 rate by 2.25% is observed with 1% increase in the availability of an international airport According to earlier studies, connectivity is a major contributor to spread of Covid-19 since its outbreak in Wuhan, China — irrespective of the scale of travel (International/local flight). Hence, we observed an early spike in High income countries compared to low- and middle-income countries because of low travel. The relevance of airport to city (state) configuration remains relevant to the economic vitality of such state. However, urbanized places with airport such as Lagos, Nigeria have been discovered to be major recipient of the foreign detected diseases.
For example, since the detection of first Ebola case (Otu et al., 2018) and coronavirus disease (Adepoju, 2020a, Adepoju, 2020b) on the July 23, 2014 and February 27, 2020 respectively in Lagos Nigeria, the potency of the airport has a magnet for the mobility and transportation of disease has been commonly recognised. Identified was that the index case of both disease incidence were foreign nationals from Liberia and Italy respectively who traveled into the country via airplanes. Popoola (2020a) iterates that the uncoordinated accelerating urbanisation of Nigerian states with largest cities poses great threat than advantage to her health experience. The argument was that fluidity and rapid migratory characteristics from concentration of automobiles and airport as hypothesised in this study as Lagos can be a risk factor to the recorded incidence of the COVID-19 pandemic. The variable preposition of this study was further nailed by Grais, Ellis, and Glass (2003) when the spread of influenza between northern and southern region of Hong Kong was attributed to airport transport. Nigeria went on lockdown on March 29, 2020. A brave measure taken by the country despite its weak economy. We assume this as further reduced the impact of local travel on the spread of the virus.
It important to note that this study aligns with the widely established impact of the health outcome factors outside the health sector — collectively referred to as the social determinants of health (SDoH). SDoH are structural and systematic; as such affects people and places differently. In this study and according to the OLS model, we observed the negative and significant relationship between Covid-19 crude rate and literacy ratio. Education is an important predictor of health and indicator of economic prosperity. The literacy ratio in Nigeria is low in Northern states such as Kano, Jigawa. These states are associated with high birth rate. According to our study, the crude rate of COVID-19 is higher in these states when compared to other states in the country. This finding aligns with Habib, Dayyab, Iliyasu, and Habib (2021) who established that there exists a low general knowledge on control mechanism on COVID-19 in Kano State. It was reported that social (education status, literacy and awareness) and religious (Muslim belief system) are two factor that account for these findings. Iterating the literacy factor, Okpi (25 June 2019) posed that nearly 50 per cent of Northern young women have access to formal education. This is embedded in the regional (North-South) educational disparity in the country. In reference to the National Bureau of Statistics data, Amzat (2017) and Kazeem (2017) reported that despite educational funding support across Nigeria, Southern States are better off than the North when literacy level is measured. With exception to Taraba State in Northern Nigeria, it was reported that the Northeast, Northwest, and North-central region of Nigeria are characterised by States (Yobe, Zamfara, Katsina, Sokoto, Bauchi, Kebbi, and Niger) where the literacy level is as low as between 7 and 23 per cent. While literacy rate in between 90 and 96 per cent in Southern States (Imo, Lagos, Ekiti, Rivers, Abia, Anambra, Osun, Edo, Enugu, and Cross River).
4.1. Spatial planning in the face of COVID-19
In Nigeria, all existing COVID-19 cases as at the day of writing this report were recorded in urban places across the country; thus, creating shock to the teeming urban population, and has led to the central and state government coming up with a reactionary response in the absence of a planned response to the COVID-19 emergency. Thus, exposing the country's weak or lack of planning and effective urban governance in higher order states such as Lagos, Abuja, Kano and Port Harcourt. Planning is vital in lessening the immediate and potentially calamitous effect of an infectious disease pandemic on society (Shearer, Moss, McVernon, Ross, & McCaw, 2020). Thus, in each state, having a preparedness plan that outlines actions to be taken during national emergencies have the additional challenge of steering a host of disruptive determining factors that requires innovative solutions, given the behaviour of diseases and their human hosts. Thereby, making sure that cities are prepared and equipped for emerging infectious diseases is momentously significant (Lee, Ho, et al., 2020).
Urban centres share standard features, a lot of which are disruptive elements that requires addressing for cities to be appropriately prepared (Lee, Aguilera, Heyman et al., 2020). For instance, population, housing, public transport, and work environment densities which are usually high in cities or states with major cities resulting to regional imbalances and inequalities in Nigeria. Raheem, Oyeleye, Adeniji, and Aladekoyi (2014) illustrated the distributional problems of such inequalities. Our study analysis found population density as a significant predictor of COVID-19 spread in Nigeria (p < 0.001). Lee, Ho, et al. (2020) are of the opinion that inequalities, aggravated by rapid rural-urban migration, often results in inadequate housing, scarce supply of freshwater, inadequate sanitation services, and ineffective ventilation systems, all of which increase outbreak risks. Thus, there is an urgent need to slow down and reverse the rural-urban migration trend that has increased population densities of cities.
In Nigeria, Lagos, Abuja and Kano are the main capital cities. They are important hubs of administration, travel, and trade i.e., they are important trip origin and destinations, and serve as the major entry points into the country; therefore, an uncontrolled outbreak as we have it has resulted in brutal economic costs beyond lives lost. More importantly, capital cities of these states served as transmission pipes to other states in the country. This is why the presence of an international airport is a significant predictor of COVID-19 spread in Nigeria (p < 0.05). The Lagos airport accounted for 73% of international travellers to and from Nigeria, over 38% of total domestic travellers, while the Abuja airport accounted for 32.99% of domestic passengers and 32.99% of international passengers in Q4 2017 (National Bureau of Statistics, 2018). Together the two airports accounted for about 71% of domestic flights in Nigeria. Consequently, improving health and installing biosecurity scanners at local airports are essential activities that should feature at all airports around the country to aid the country start rebooting in preparation for life post-COVID-19.
Making sure that the Nigerian cities are well prepared will require a renewed emphasis on improving capacities to deal with epidemics and other health emergencies. A number of these efforts are relevant in both the urban and rural areas, for example, grasping the local socio-economic and cultural background of city residents and active involvement of communities and local leaders in both planning and implementation. However, the ability to implements these efforts and communicate directives hinges on the ability of the people to read and write with understanding. A literate society is easily governed during emergencies; our model showed that the literacy rate in Nigeria states is significant to the spread of COVID-19 in Nigeria (p < 0.05). For example, Kano state with literacy ratio of 37.4% is one of the most affected states in Nigeria. The situation in Kano state seems dire when the Almanjiris are factored in the present COVID-19 reality. The Almanjiris are young children from poor homes sent to Islamic boarding schools but are found wandering the streets begging from door to door in the pursuit for survival and are deprived of formal education. Consequently, during this lockdown, these children are subjected to continuous hunger, thus, increasing their risk of exposure to COVID-19. The Advocates for Dan Almajiri (2020) states that numerous Almanjiri children are already exposed to poor health conditions, thus, the probability of being infected with the COVID-19 virus and spreading the virus is significantly high.
5. Conclusions
The roles of state, literacy (education and behaviour that comes with learning education and awareness), and the presence of international airport in the spread of the disease has been identified. The study has shown that higher order states (centre of commerce and government) are the most vulnerable location and places to the incidence of diseases. The risk exposure of these states is defined by population density, the presence of international airports and literacy ratio. After this foregone, the study reality of the failed health system and poor disaster preparedness in the planning of our cities and the arrangement of spaces was shown in this pandemic era in Nigeria. In this study, we argue that controlled mobility is key to monitoring and managing the pandemic spread in Nigeria. This we argue as higher order states remains flash point for the spread of the disease. Thus, the relevance of a coordinated airport surveillance and port health planning along city airport station was highlighted in this study.
The ongoing COVID-19 pandemic is a potent aide memoire that urbanisation has altered the city way of life, and thus, there is an urgent need to strengthen systems and local capacities to inhibit the spread of the COVID-19 virus. In addition, there might be necessary to redesign our cities to moving forward to adapt to the dawn of a new reality which is living with the COVID-19 virus.
The authors summarised that away from the poor management mechanism, the study is a pointer to the need for effective and more precautionary process to futuristic planning for disease pandemic in Nigeria. The finding of this study suggests that if other variables such as car mobility and transportation disaggregated local government area and neighbourhood COVID-19, death figure and response data at a sub-national level were thrown into the model, the result might present a different spatial and temporal evidence of the risk factor to COVID-19. Thus, we see this study as a start-point and not the end to explaining COVID-19. That is, it is a step toward the unravelling of the evidence that can explain the potential spread and place vulnerability of the virus in Nigeria. The study raises the need for improved education and literacy in the Northern States. The COVID-19 evidence suggests and emphasise the need for literacy policies to be prioritised.
References
- Adepoju P. Nigeria responds to COVID-19; first case detected in sub-Saharan Africa. Nature Medicine. 2020;26(4):444. doi: 10.1038/d41591-020-00004-2. [DOI] [PubMed] [Google Scholar]
- Adepoju P. Nigeria's widening tuberculosis gap. The Lancet Infectious Diseases. 2020;20 doi: 10.1016/S1473-3099(19)30712-1. [DOI] [PubMed] [Google Scholar]
- Adewoyin Y., Chukwu N., Sanni L. Urbanization, spatial distribution of healthcare facilities and inverse care in Ibadan, Nigeria. Ghana Journal of Geography. 2018;10(2):96–111. [Google Scholar]
- Advocates for Dan Almajiri . Federal Ministry of Education; 2020. COVID-19: Predicting the rights to life of the Almanjiris amidst the pandemic. A position paper. [Google Scholar]
- Aliyu A.A., Amadu L. Urbanization, cities, and health: The challenges to Nigeria–a review. Annals of African Medicine. 2017;16(4):149. doi: 10.4103/aam.aam_1_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkire S., Dirksen J., Nogales R., Oldiges C. Department of International Development (ODID), University of Oxford; United Kingdom: 2020. Multidimensional poverty and COVID-19 risk factors: A rapid overview of interlinked deprivations across 5.8 billion people. OPHI BRIEFING 53. Oxford poverty and human development initiative (OPHI) [Google Scholar]
- Amoo E., Adekeye O., Olawole-Isaac A., Fasina F., Adekola P., Samuel G., et al. Nigeria and Italy divergences in coronavirus experience: Impact of population density. Science World Journal. 2020 doi: 10.1155/2020/8923036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amzat A. Espite decades of funding, literacy level in the northern states remains low. July 24 2017. https://guardian.ng/news/despite-decades-of-funding-literacy-level-in-the-northern-states-remains-low/ Available at:
- Amzat J., et al. Coronavirus outbreak in Nigeria: Burden and socio-medical response during the first 100 days. International Journal of Infectious Diseases. 2020;98:218–224. doi: 10.1016/j.ijid.2020.06.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anim D.O., Ofori-Asenso R. Water scarcity and COVID-19 in sub-Saharan Africa. Journal of Infection. 2020;81(2):e108–e109. doi: 10.1016/j.jinf.2020.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anselin L. Local indicators of spatial association – LISA. Geographical Analysis. 1995;27:93–115. doi: 10.1111/j.1538-4632.1995.tb00338.x. [DOI] [Google Scholar]
- Anselin L. Thirty years of spatial econometrics. Papers in Regional Science. 2010;89(1):3–25. doi: 10.1111/j.1435-5957.2010.00279.x. [DOI] [Google Scholar]
- Atikah N., Rahardjo S., Lestari T.E. 2020. Parameter estimation of spatial durbin model (SDM) using method of moment. 070002. [DOI] [Google Scholar]
- Bai Y., Yao L., Wei T., Tian F., Jin D., Chen L., et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323(14):1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bong C.L., Brasher C., Chikumba E., McDougall R., Mellin-Olsen J., Enright A. The COVID-19 pandemic: Effects on low-and middle-income countries. Anesthesia & Analgesia. 2020;131(1):86–92. doi: 10.1213/ANE.0000000000004846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention Assessing risk factors for severe COVID-19 illness. 30 November, 2020. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/assessing-risk-factors.html Available at:
- Chung L.H. Impact of pandemic control over airport economics: Reconciling public health with airport business through a streamlined approach in pandemic control. Journal of Air Transport Management. 2015;44:42–53. doi: 10.1016/j.jairtraman.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis N., Sparrow A., Ghebreyesus T.A., Netea M.G. Considering BCG vaccination to reduce the impact of COVID-19. The Lancet. 2020;395(10236):1545–1546. doi: 10.1016/S0140-6736(20)31025-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da Silva J.G., Silva C.S., Alexandre B., Morgado P. Health literacy of the Inland population in mitigation phase 3.2 of the COVID-19 pandemic in Portugal: A descriptive cross-sectional study. Portuguese Journal of Public Health. 2020:1–11. [Google Scholar]
- Desjardins M.R., Hohl A., Delmelle E.M. Applied Geography; 2020. Rapid surveillance of COVID-19) in the United States using a prospective space-time scan statistic: Detecting and evaluating emerging clusters. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diwakar V. Overseas Development Institute; London: 2020. From pandemics to poverty Hotspots of vulnerability in times of crisis. [Google Scholar]
- Elsey H., Agyepong I., Huque R., Quayyem Z., Baral S., Ebenso B., et al. Rethinking health systems in the context of urbanisation: Challenges from four rapidly urbanising low-income and middle-income countries. BMJ global health. 2019;4(3) doi: 10.1136/bmjgh-2019-001501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ersoy A. Smart cities as a mechanism towards a broader understanding of infrastructure interdependencies. Regional Studies, Regional Science. 2017;4(1):26–31. doi: 10.1080/21681376.2017.1281154. [DOI] [Google Scholar]
- Farrell K. An inquiry into the nature and causes of Nigeria's rapid urban transition. Urban Forum. 2018;29:277–298. doi: 10.1007/s12132-018-9335-6. [DOI] [Google Scholar]
- Fauci A., Lane H., Redfield R. Covid-19—navigating the uncharted. New England Journal of Medicine. 2020;382:1268–1269. doi: 10.1056/NEJMe2002387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feigin R.D., Garg R., Christie A.B. Infectious disease. Encyclopedia Britannica. 2020. https://www.britannica.com/science/infectious-disease
- Gilbert M., Pullano G., Pinotti F., Valdano E., Poletto C., Boëlle P., et al. Preparedness and vulnerability of African countries against importations of COVID-19: A modelling study. The Lancet. 2020;395(10227):871–877. doi: 10.1016/S0140-6736(20)30411-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grais R., Ellis J., Glass G. Assessing the impact of airline travel on the geographic spread of pandemic influenza. European Journal of Epidemiology. 2003;18(11):1065–1072. doi: 10.1023/a:1026140019146. [DOI] [PubMed] [Google Scholar]
- Guo D. Visual analytics of spatial interaction patterns for pandemic decision support. International Journal of Geographical Information Science. 2007;21(8):859–877. doi: 10.1080/13658810701349037. [DOI] [Google Scholar]
- Habib M., Dayyab F., Iliyasu G., Habib A. Knowledge, attitude and practice survey of COVID-19 pandemic in Northern Nigeria. PLoS One. 2021;16(1) doi: 10.1371/journal.pone.0245176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habte D., Dussault G., Dovolo D. Challenges confronting the health workforce in sub-Saharan Africa. World Hospitals and Health Services. 2004;40(2):23–26. [PubMed] [Google Scholar]
- Hassan Z., et al. Population risk factors for COVID-19 deaths in Nigeria at sub-national level. The Pan African Medical Journal. 2020;35(2):131. doi: 10.11604/pamj.supp.2020.35.131.25258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilesanmi O.S., Oderinde T.M., Afolabi A.A. The urban slums: Potential source of COVID-19 spikes in Africa. Public Health in Practice. 2020;1:100052. doi: 10.1016/j.puhip.2020.100052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazeem Y. Literacy rates in Nigeria's north are lower than in the south. 2017. https://theatlas.com/charts/Byl1cY_Ox Available at:
- Lawal O., Nwegbu C. GeoJournal; 2020. Movement and risk perception: Evidence from spatial analysis of mobile phone-based mobility during the COVID-19 lockdown, Nigeria. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawyer G. Measuring the potential of individual airports for pandemic spread over the world airline network. BMC Infectious Diseases. 2015;16(1):70. doi: 10.1186/s12879-016-1350-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee V., Aguilera X., Heymann D., et al. Preparedness for emerging epidemicthreats: A lancet infectious diseases commission. The Lancet Infectious Diseases. 2020;20:17–19. doi: 10.1016/S1473-3099(19)30674-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee V., Ho M., Kai C., Aguilera X., Heymann D., Wilder-Smith A. Epidemic preparedness in urban settings: New challenges and opportunities. The Lancet Infectious Diseases. 2020;20:527–528. doi: 10.1016/S1473-3099(20)30249-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopes H., McKay V. Adult learning and education as a tool to contain pandemics: The COVID-19 experience. International Review of Education. 2020;66(4):575–602. doi: 10.1007/s11159-020-09843-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madhav N., Oppenheim B., Gallivan M., Mulembakani P., Rubin E., Wolfe N. Disease control priorities: Improving health and reducing poverty. 3rd ed. The International Bank for Reconstruction and Development/The World Bank; 2017. Pandemics: Risks, impacts, and mitigation. [PubMed] [Google Scholar]
- Manisalidis I., Stavropoulou E., Stavropoulos A., Bezirtzoglou E. Environmental and health impacts of air pollution: A review. Frontiers in Public Health. 2020;8:14. doi: 10.3389/fpubh.2020.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews Z., Channon A., Neal S., Osrin D., Madise N., Stones W. Examining the “urban advantage” in maternal health care in developing countries. PLoS Medicine. 2010;7(9) doi: 10.1371/journal.pmed.1000327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLafferty S. Placing pandemics: Geographical dimensions of vulnerability and spread. Eurasian Geography and Economics. 2010;51(2):143–161. doi: 10.2747/1539-7216.51.2.143. [DOI] [Google Scholar]
- Miller L., Bhattacharyya R., Miller A. Spatial analysis of global variability in covid-19 burden. Risk Management and Healthcare Policy. 2020;13:519–522. doi: 10.2147/RMHP.S255793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollalo A., Vahedi B., Rivera K.M. GIS-based spatial modeling of COVID-19 incidence rate in the continental United States. The Science of the Total Environment. 2020;728(1–8) doi: 10.1016/j.scitotenv.2020.138884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran P.A. Notes on continuous stochastic phenomena. Biometrika. 1950;37(1/2):17–23. doi: 10.2307/2332142. [DOI] [PubMed] [Google Scholar]
- Mugunga J.C., Tyagi K., Bernal-Serrano D., Correa N., Iberico M., Kateera F., et al. SARS-CoV-2 serosurveys in low-income and middle-income countries. The Lancet. 2021;397(10272):353–355. doi: 10.1016/S0140-6736(21)00188-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Bureau of Statistics Nigeria - national water supply and sanitation baseline survey-2006, first round. Federal Ministry of water resources (FMWR) - federal government of Nigeria (FGN) 2013. https://www.nigerianstat.gov.ng/nada/index.php/catalog/29 Available at:
- National Bureau of Statistics 2018. https://www.nigerianstat.gov.ng/ Available at:
- National bureau of Statistics The Nigeria poverty profile 2010 report. Press briefing by the statistician-general of the federation/chief executive officer, National Bureau of Statistics, Dr. Yemi Kale held at the conference room, 5th floor, NBS headquarters, central business district, Abuja on Monday, 13th February, 2012. 2012. https://reliefweb.int/sites/reliefweb.int/files/resources/b410c26c2921c18a6839baebc9b1428fa98fa36a.pdf Available at:
- Ndaw F. COVID-19: Solving Africa's water crisis is more urgent than ever. 2020. https://blogs.worldbank.org/nasikiliza/covid-19-solving-africas-water-crisis-more-urgent-ever Available at:
- 2018. https://dhsprogram.com/pubs/pdf/FR359/FR359.pdf
- Neiderud C. How urbanization affects the epidemiology of emerging infectious diseases. Infection Ecology & Epidemiology. 2015;5(1):27060. doi: 10.3402/iee.v5.27060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngwa M., Ihekweazu C., Okwor T., Yennan S., Williams N., Elimian K., et al. The cholera risk assessment in Kano state, Nigeria: A historical review, mapping of hotspots and evaluation of contextual factors. PLoS Neglected Tropical Diseases. 2021;15(1) doi: 10.1371/journal.pntd.0009046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nkosi V., Haman T., Naicker N., Mathee A. Overcrowding and health in two impoverished suburbs of Johannesburg, South Africa. BMC Public Health. 2019;19(1):1–8. doi: 10.1186/s12889-019-7665-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nwosu C.O., Oyenubi A. Income-related health inequalities associated with the coronavirus pandemic in South Africa: A decomposition analysis. International Journal for Equity in Health. 2021;20(1):1–12. doi: 10.1186/s12939-020-01361-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okpi A. Coca-cola is right: 50% of young women in northern Nigeria have no formal education. 25 June 2019. https://africacheck.org/fact-checks/reports/coca-cola-right-50-young-women-northern-nigeria-have-no-formal-education Available at:
- Omuta G., Onokerhoraye A., Okonofua F., Obanovwe G., Isah E., Chiwuzie J., et al. Perspectives on primary health care in Nigeria: Past, present and future. CPED Monograph Series No. 10. Centre for Population and Environmental Development (CPED): Nigeria. 2014 [Google Scholar]
- Osayomi T. The emergence of a diabetes pocket in Nigeria: The result of a spatial analysis. GeoJournal. 2019;84(5):1149–1164. doi: 10.1007/s10708-018-9911-2. https://link.springer.com/article/10.1007/s10708-018-9911-2#citeas [DOI] [Google Scholar]
- Osayomi T., Adeleke R., Taiwo O.J., Gbadegesin A.S., Fatayo O.C., Akpoterai L.E., et al. Cross-national variations in COVID-19 outbreak in West Africa: Where does Nigeria stand in the pandemic? Spatial Information Research. 2020:1–9. [Google Scholar]
- Otu A., Ameh S., Osifo-Dawodu E., Alade E., Ekuri S., Idris J. An account of the Ebola virus disease outbreak in Nigeria: Implications and lessons learnt. BMC Public Health. 2018;18(1):3. doi: 10.1186/s12889-017-4535-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otuoze S., Hunt D., Jefferson I. Neural network approach to modelling transport system resilience for major cities: Case studies of Lagos and Kano (Nigeria) Sustainability. 2021;13(3):1371. [Google Scholar]
- Popoola A. Fighting disease pandemic with planning: Exploring African COVID-19 experiences. 2020. http://www.chsunilag.com/blog/fighting-disease-pandemic-with-planning-exploring-african-covid-19-experiences Available at:
- Popoola A., Magidimisha-Chipingu H., Chipungu L., Adeleye B., Akogun O., Medayese S. Vol. 654. IOP Publishing; 2020. Household water stress, adaptation and resilience in some selected peri-urban and rural communities of Oyo state, Nigeria. (The association of schools of construction of southern Africa (ASOCSA) 14th built environment conference IOP conference. Series: Earth and environmental science). 2021. [DOI] [Google Scholar]
- Popoola A.A., Olatunde M.O., Magidimisha H.H., Abiodun A., Adeleye B.M., Chipungu L. Urban forced evictions: Experiences in the Metropolitan city of Lagos, Nigeria. The Indonesian Journal of Geography. 2020;52(1):112–127. [Google Scholar]
- Popoola A., Tawose O., Abatan S., Adeleye B., Jiyah F., Majolagbe N. Housing conditions and health of residents in Ibadan north local government area, Ibadan, Oyo state, Nigeria. Journal of Environmental Sciences and Resource Management. 2015;7(2):59–80. [Google Scholar]
- Raheem W.M., Oyeleye O., Adeniji M.A., Aladekoyi O. Regional imbalances and inequalities in Nigeria: Causes, consequences and remedies. Research on Humanities and Social Sciences. 2014;4(18) [Google Scholar]
- Shearer F., Moss R., McVernon J., Ross J., McCaw J. Infectious disease pandemic planning and response: Incorporating decision analysis. PLoS Medicine. 2020;17(1) doi: 10.1371/journal.pmed.1003018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sunkari E.D., Korboe H.M., Abu M., Kizildeniz T. Science of the Total Environment; 2020. Sources and routes of SARS-CoV-2 transmission in water systems in Africa: Are there any sustainable remedies? [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabb L.P., McClure L.A., Quick H., Purtle J., Diez Roux A.V. Assessing the spatial heterogeneity in overall health across the United States using spatial regression methods: The contribution of health factors and county-level demographics. Health & Place. 2018;51:68–77. doi: 10.1016/j.healthplace.2018.02.012. [DOI] [PubMed] [Google Scholar]
- Taiwo O.J., Olumoyegun J.M. In: Proceedings of a special virtual conference on COVID-19 of the association of Nigerian geographers (Southwest Zone), held via Zoom. Gbadegesin A., Oyesiku O., Onafeso O., editors. 2020. Distant decay analysis of airports and the number of confirmed COVID-19 in Nigeria.https://ssrn.com/abstract=3683511 June 29-30, 2020. [Google Scholar]
- Tarwater P., Martin C. Effects of population density on the spread of disease. Complexity. 2001;6(6):29–36. [Google Scholar]
- Tu J., Xia Z.G. Examining spatially varying relationships between land use and water quality using geographically weighted regression I: Model design and evaluation. The Science of the Total Environment. 2008;407:358–378. doi: 10.1016/j.scitotenv.2008.09.031. [DOI] [PubMed] [Google Scholar]
- Varrella S. Poverty headcount rate in Nigeria 2019, by state. September 22, 2021. https://www.statista.com/statistics/1121438/poverty-headcount-rate-in-nigeria-by-state/ Available at:
- World Bank Population growth (annual%)- Nigeria. 2018. https://data.worldbank.org/indicator/SP.POP.GROW?locations=NG&most_recent_year_desc=true
- World Health Organization and the United Nations Children’s Fund (UNICEF) WHO Headquarters; Geneva: 2020. Water, sanitation, hygiene, and waste management for the COVID-19 virus Interim guidance. WHO/2019-nCoV/IPC_WASH/2020.3. [Google Scholar]