Abstract
Cancer incidence is rising in low- and especially middle-income countries (MICs), driven primarily by four high-burden cancers (breast, cervix, lung, colorectal). By 2030, more than two-thirds of all cancer deaths will occur in MICs. Prevention and early detection are required alongside efforts to improve access to cancer treatment. Successful strategies for decreasing cancer mortality in high-income countries (HICs) are not always effective, feasible or affordable in other countries. In this review we evaluate strategies for prevention and early detection of breast, cervix, lung and colorectal cancers, focusing on modifiable risk factors and high-risk subpopulations. Tobacco taxation, HPV vaccination, cervical cancer screen-and-treat strategies, and efforts to reduce patient and health-system related delays in the early detection of breast and colorectal cancer represent the highest yield strategies for advancing cancer control in many MICs. An initial focus on high-risk populations is appropriate, with increasing population coverage as resources allow. These strategies can deliver significant cancer mortality gains, and serve as a foundation from which countries can develop comprehensive cancer control programs. Investment in national cancer surveillance infrastructure is needed; the absence of national cancer data to identify at-risk groups remains a barrier to the development of context-specific cancer control strategies.
Keywords: cancer, prevention, detection, screening, low- and middle-income countries (LMICs), middle-income countries (MICs)
Introduction
Cancer incidence and mortality are rapidly increasing in low- and especially middle-income countries (MICs), where 75% of global cancer deaths are projected to occur by 2030.1,2 Middle income economies are defined by the World Bank as those in which the gross national income per capita is between $1,036-12,535 per year.3 They are further subdivided into lower-middle income (GNI $1,036-4045) and upper-middle income (GNI $4046-12,535) groupings. While countries classified as middle-income economies are highly diverse, they face some common challenges in cancer control. Economic evaluation suggests most MICs have the financial resources to deliver a basic set of cancer services tailored to domestic health budgets and cancer burden.4
Rising cancer incidence in MICs has been attributed to population growth, increases in life expectancy and social and economic transitions which are changing the prevalence of major known risk factors for cancer.5 Two defining features of cancer in MICs are the advanced stage of presentation and the high stage-adjusted mortality rate relative to incidence (i.e. case fatality rate).1,6,7 Globally, survival after a cancer diagnosis is highest among women living in the world’s wealthiest countries, with an overall incidence to mortality ratio of 0.31, and lowest among males in the poorest regions, with an incidence to mortality ratio of 0.77. 1 Even for cancers associated with the most favourable outcomes, wide discrepancies in survival between countries remain. In the United States (US), 5-year unadjusted overall survival for breast cancer is 90.2%, compared to only 66% in India and less than 44% in Nigeria.8
The implementation of population-based cancer prevention, screening and early detection (PSED) strategies in high-income countries (HICs) over the past 30 years has led to decreases in cancer mortality rates for common cancers including breast,9 cervical,10 prostate, 11colorectal, 12 and liver cancer.13 Between 1975-2000 earlier detection of breast cancer accounted for almost half of the reduction in breast cancer mortality in the United States (US), with the remainder due to advances in treatment.9 Similarly, greater than 50% of the decrease in colorectal mortality over the same period in the US is attributed to greater acceptance and uptake of colorectal cancer screening.12 Many preventative and early detection strategies have not yet been evaluated in MICs.4,14 Population-based screening strategies that have been credited with reducing cancer incidence and mortality in HICs may not yet be effective, feasible or affordable in many MICs.15 Finally, the ability of screening and early detection policy to improve cancer-specific outcomes is contingent on access to effective treatment. Without addressing inequities in access to multimodal cancer care the potential gains of early detection are significantly curtailed .14,16 Focusing prevention and early detection efforts initially on high-risk individuals and groups, may allow for targeted risk reduction and stage shifting,17–19 as well as provide an entry point from which countries can develop more comprehensive cancer control programs.
This review explores the opportunities and challenges in the prevention and early detection of breast, cervical, lung and colorectal cancer, which represent the highest burden cancers (Table 1) in MIC2. Identifying evidence-based, cost-effective strategies that can be tailored to local resources and system constraints will be critical for reducing the wide gap in cancer outcomes that currently exists between the most developed countries and the rest of the world.
Table 1:
The four highest burden cancers in middle income countries, 2020
| Total new cases | Total deaths | |
|---|---|---|
| Breast | 433 060 | 202 463 |
| Cervical | 236 828 | 189 230 |
| Lung | 210 541 | 146 198 |
| Colorectal | 194 954 | 112 556 |
| All cancers | 3 099 791 | 1 982 660 |
Source: GLOBOCAN 2020, International Agency for Research in Cancer.107
Notes: Estimates of absolute cancer burden in 2020 across 36 cancer sites in 185 countries or territories is built up in GLOBOCAN using the best available sources of cancer incidence and mortality data within a given country; therefore, validity of the national estimates depends on the degree of representativeness and the quality of source information.
Middle income countries (MICs), as defined by the World Bank Income Group Classification 2020, are: Angola, Algeria, Bangladesh, Benin, Bhutan, Bolivia, Cabo Verde, Cambodia, Cameroon, Comoros, Congo, Rep., Cote d;Ivoire, Djibouti, Egypt, El Salvador, Eswatini, Ghana, Honduras, India, Kenya, Kiribati, Kyrgyz Republic, Lao PDR, Lesotho, Mauritania, Federated States of Micronesia, Moldova, Morocco, Myanmar, Nepal, Nicaragua, Nigeria, Pakistan, Papua New Guinea, Philippines, Sao Tome and Principe, Senegal, Solomon Islands, Sri Lanka, Tanzania, Timor-Leste, Tunisia, Ukraine, Uzbekistan, Vanuatu, Vietnam, West Bank and Gaza, Zambia, Zimbabwe, Albania, American Samoa, Argentina, Armenia, Azerbaijan, Belarus, Bosnia and Herzegovina, Botswana, Brazil, Bulgaria, China, Colombia, Costa Rica, Cuba, Dominica, Dominican Republic, Equatorial Guinea, Ecuador, Fiji, Gabon, Georgia, Grenada, Guatemala, Guyana, Indonesia, Islamic Republic of Iran, Iraq, Jamaica, Kazakhstan, Kosovo, Lebanon, Libya, Malaysia, Maldives, Marshall Islands, Mexico, Montenegro, Namibia, North Macedonia, Paraguay, Peru, Russian Federation, Samoa, Serbia, South Africa, St. Lucia, St Vincent and the Grenadines, Suriname, Thailand, Tonga, Turkey, Turkmenistan, Tuvalu, Venezuela.
Improved cancer surveillance
Cancer surveillance is the foundation upon which cancer control efforts, including prevention and early detection strategies, are developed. Cancer risk factors, incidence, mortality, stage of presentation and outcomes following treatment are poorly characterized or absent in most MICs.20,21 Population coverage with cancer registries is low in South America (19% of total population covered by a registry), Asia (15%) and Africa (13%), and sampling is predominantly subnational, urban-biased and of variable quality.1,22 Only one out of five countries globally report cancer data of sufficient quality to determine incidence estimates.1,21 In a recent systematic review on the stage of diagnosis of breast cancer in sub-Saharan Africa (SSA), only one country (i.e. South Africa) had national data on the stage of presentation.23
The World Health Organization (WHO) lists cancer monitoring through the use of population-based cancer registries as part of its Essential Cancer Package.24 To support LMICs develop and improve their cancer surveillance capacity the International Association for Research on Cancer (IARC) leads the Global Initiative for Cancer Registry Development (GICR).25 The GICR provides technical training and support for new population-based cancer registries (PBCRs) and has developed open source software (CanReg5) in seven languages to support cancer registry data entry, maintenance and analysis.26 The GICR regional hub for SSA is administered by the African Cancer Registry Network, which includes 30 members across 19 countries.27 The annual costs of maintaining a registry are estimated at $USD0.01-USD0.22 per person in the population covered by the registry,25,28 with incidence data becoming available within two years of a registry’s establishment,26 making PBCRs a low cost, high value cancer control investment. Despite this, registry development remains underutilised as a cancer control strategy in many countries.25
Modifiable risk factors as targets for prevention strategies
Countries with limited or modest per-capita health spending often allocate most of their cancer resources to therapeutic care, despite the cost-effectiveness of prevention and early detection.29 Major long term gains in cancer control for MICs can be achieved at relatively low cost by strengthening prevention strategies for modifiable cancer risk factors,4 which cause half of all cancers worldwide.22 The relative importance of a particular risk factor varies with geography, demography and development status.5 The Global Burden of Disease consortium identified six broad drivers of cancer incidence in MICs: population growth, population age structures, exposure to environmental risks (e.g. air quality, UV radiation, aflatoxins), shifting behavioural risks (e.g. tobacco, alcohol, sexually transmitted infection, fertility patterns, exercise), new metabolic risks (diet, obesity), and changes due to all other factors.30
Tobacco use remains the leading preventable cause of cancer worldwide. Smoking prevalence is declining globally, but at a slower rate in both LICs and MICs 5,22. Strategies aimed at tobacco cessation and prevention of initiation can have sizeable health and cancer impacts, and achieve relatively quick health gains. Around 90% of the cancer-related risks of smoking can be averted if people quit before the age of 40 years, but unlike in HICs most adults in MICs will only quit after developing cancer and not while healthy.4 The most effective tobacco control strategy for countries at all stages of development is taxation, specifically high excise taxes on tobacco products which promote adult cessation and reduce youth initiation rates. This is especially effective among lower-income and younger populations who are more price-sensitive. The Philippines substantially increased excise taxes on tobacco in 2012. Smoking prevalence subsequently fell sharply, with an estimated 3 million fewer smokers 3 years after the law took effect. The greatest declines were seen among the poorest households.31 Furthermore, 80% of the tax revenue generated from this legislation was channelled back into the health budget, allowing the government to increase health insurance coverage to 25 million poor and elderly households.32 Although 168 countries encompassing 90% of the world’s population are signatories to the WHO Framework Convention on Tobacco Control,33 which includes price and tax measures to reduce demand for tobacco, excise tobacco taxes are still underutilised in many countries as a primary prevention tool for cancer (and many other non-communicable diseases).4
Infection-related cancers, including human papilloma virus (HPV)-related cancers, hepatitis B virus (HBV) and hepatitis C virus (HCV) associated liver cancer, H. pylori-associated gastric cancer and HIV-associated Kaposi sarcoma, comprise a significant proportion of the total cancer burden in many LMICs.22,34 In SSA, infection-related cancers accounted for ~28% of all new cancers in 2018, and as many as 50% of new cancers in East African countries.34–36 Vaccination against HBV infection represents one of the major cancer success stories of the past 30 years. Primary prevention of chronic HBV infection through vaccination is now delivered in 183 countries as part of routine childhood vaccination, with 81% global coverage. In lower-income countries HBV vaccination programs are supported by the Global Alliance for Vaccines Initiatives (GAVI).37 The success of this program has set the stage for vaccination research and development for other infection-related cancers, most notably HPV-related cervical cancer.
The development of a vaccine against high-risk HPV genotypes offers a highly effective primary prevention strategy for cervical cancer, one of the leading causes of cancer-mortality among women in LMICs, as well as for HPV-related oral, throat, penile and anal cancers. HPV infection is common among young, sexually active individuals and usually clears without treatment. However persistent HPV infection with the high-risk oncogenic subtypes 16 and 18 accounts for 70% of all cervical cancer cases. Population-level coverage ≥ 70% of girls ages 9-12 years is considered the most cost effective strategy for cervical cancer prevention at all development levels,38,39 and is included in the WHO and Disease Control Priorities Essential Cancer Packages.4,24 Current commercially available HPV vaccinations require 2-3 doses over 6-12 months and a temperature-controlled supply chain. This poses a challenge in many LMICs where platforms for reaching and following up adolescents are not well developed and the infrastructure needed to ensure a cold chain is often absent. Moreover, the cultural acceptance of vaccination against sexually-transmitted infection for adolescent girls can be variable, with vaccine acceptability (among parents for their daughters) in SSA countries ranging from 59-100% in systematic reviews.40
Delivery of the HPV vaccine to girls in both LICs and MICs with high coverage rates is possible.41 HPV vaccination program coverage in 2019 was ≥ 90% for two doses in Turkmenistan, Mexico and Rwanda, and a further 10 MICs have achieved ≥ 90% coverage for the first dose.41 Cost remains a major barrier to adoption of the HPV vaccine in MICs, particularly those that do not qualify as GAVI eligible (most MICs).38,39 Further efforts to improve uptake and coverage in both LICs and MICs must focus on price reduction and programmatic infrastructure, which may be best achieved by embedding HPV vaccination within a platform of adolescent health interventions. Most of the mortality gains from both HPV vaccination will not be realised until the second half of the century,4 given the lag time between vaccination, infection and development or prevention of related cancers. Screening and early detection strategies among individuals at high risk for HPV-related cancer need to be developed alongside vaccination programs to meet country-level and global targets for cervical cancer reductions.42
As countries transition from a disease burden primarily composed of communicable to non-communicable diseases, infection-related cancers typically fall, and cancers associated with tobacco, alcohol, diet and a lack of exercise begin to dominate.35 The relative contribution of these risk factors to the development of breast and colorectal cancer in particular is poorly understood in MICs.5 For example, delayed childbearing and use of hormone replacement therapy are associated with breast cancer risk in HICs.43,44 These risk factors have a synergistic effect with elevated BMI, inadequate exercise and excessive alcohol consumption, but a smaller effect on overall risk compared to genetic and familial risks.44 The effect and relative contribution of these risk factors to breast cancer in LICs and MICs is poorly established.35 Some hormonal risk factors for breast cancer, such as delayed child-bearing and age at menarche, are associated with positive development outcomes including access to education for women, and improved nutrition status, and reversing these changes is not desirable. Breast cancer prevention should therefore focus on identifying modifiable risk factors relevant to the local and regional context.45
In colorectal cancer, well-established dietary risk factors, such as high intake of red and processed meat and low intake of fiber, account for an estimated 5% of cancer deaths worldwide.36,46 The strength of the association between diet and colorectal cancer varies by study type, sex, and the timing of dietary exposure across the lifecourse.36 The contribution of these dietary changes to the rising rate of colorectal cancer in middle-income countries is unclear. Large case-control studies are lacking and there is a paucity of data in emerging economies that clearly link diet to cancer risk. Moreover, changing dietary patterns are often accompanied by other major lifestyle changes. The interaction of diet with the colonic microbiome is an area of active research. Following diet exchange, CRC associated microbiome changes have been documented in rural SSA.47 However, this has not yet translated into clinically relevant targets (e.g. identification of a higher risk groups for screening).
Detecting pre-cancerous lesions and asymptomatic cancers via screening
Detection of asymptomatic cancer or precancerous lesions through screening allows for the detection of disease at an earlier stage, when curative treatment is more likely.15,48 Given the excess burden of advanced-stage disease, many MICs are considering the role of screening within national cancer control plans.48 Screening also features prominently in the 2017 WHO Resolution on Cancer Prevention and Control, which called upon all member states to develop, implement and monitor programmes for screening, where feasible and cost-effective.49 Organized screening, which defines a targeted population for screening and systematically invites all eligible members of the population to participate, has led to proven mortality reductions for cervical cancer (using cytology-based screening), breast cancer (mammography) and colorectal cancer (stool-based screening and/or colonoscopy) in HICs. Opportunistic screening, or case finding, is provider or patient-driven and occurs on an as-needed basis and typically within the context of national screening guidelines.15
Population-based screening requires high levels of coverage to be effective, is expensive and can rapidly deplete cancer-focused resources in countries with limited per-capita health spending.4 Delivery of screening programs requires a complete diagnostic and treatment referral pathway to be in place and accessible by those being screened, in order to realise the potential benefits of early detection. This represents a major barrier to implementing organized screening in many MICs, where health system infrastructure and supporting processes are still developing.15 A country’s health system must first be able to to manage symptomatic cancers. The processes of designing and implementing a national screening programme in MICs is beyond the scope of this review but is well described elsewhere.48
One approach for MICs that are committed to building cancer screening programs, is to start by targeting high-risk individuals.15,48 However, defining and capturing high-risk individuals for targeted cancer screening in MICs can be challenging. Traditional models have often relied on the identification of at-risk populations based on a single demographic, environmental or genetic risk factor (e.g. HPV infection and cervical cancer). A greater understanding of country-specific cancer risk factors and risk factor interactions is needed to allow for the creation of predictive models.50 The use of existing healthcare platforms or programs, for example those focused on child and maternal health or infectious diseases, to deliver opportunistic cancer screening (e.g. cervical cancer screening) to at risk populations has been successful in Zambia, Tanzania and Botswana.51 However, these programs often do not reach all eligible individuals and may exacerbate existing inequities in access to care.48
Cervical cancer screening is the most established form of cancer screening in LMICs and is well supported by population-based studies and randomized controlled trials. In both LICs and MICs screening using cytology, as is done in HICs, is being displaced by HPV testing as a primary screening technology.38 HPV testing represents a more feasible, cost-effective approach, with better sensitivity than cytology and fewer rounds of screening required to achieve comparable mortality reductions.52 A large randomized trial in rural India53 demonstrated that a single round of HPV screening in women aged 30-59 years reduces advanced cervical cancer incidence and mortality. Another randomized trial in Tamil Nadu, India documented a 35% reduction in cervical cancer mortality after screening with visual inspection with acetic acid.54
The WHO cervical cancer elimination strategy calls for cervical screening at 35 and 45 years of age for 70% of the eligible population in LMICs by 2030. It is estimated that this will reduce mortality by 34% (23-38%).55 Currently, cervical cancer screening in MICs falls well short of this target. In a study of 55 LMICs (of which 53 were MICs), the median lifetime prevalence of self-reported cervical cancer screening (i.e. cytology or HPV-based) was 43% (range 0.3%-97%).56 Attempts to increase opportunistic screening (e.g. during antenatal care) and targeted screening of those at highest risk for HPV-related cancer are strategies that can increase coverage in the absence of an organized screening program. The use of mobile Health (mHealth) technology including text message reminders and social media campaigns targeted to higher-risk women have also been employed in some countries,57 with small studies suggesting improvement in uptake and follow-up.58
Women with HIV, especially those with low CD4 counts, are at the highest risk for persistent HPV infection and progression to cervical cancer59 and are one well-defined high-risk population that benefit from short-interval targeted screening in all countries.29 HPV testing or VIA can be delivered by leveraging existing HIV infrastructure and programs, something Zambia has been doing since 2006 via its Cervical Cancer Prevention Program (Table 2).60 Smoking tobacco is another major risk factor for the development of cervical cancer and should be included in risk prediction models. A recent meta-model using data from China identified 17 risk factors for cervical cancer for inclusion in a clinical predictive model to guide screening for individual patients that may be more generalizable to other MIC settings than predictive models from HICs.50
Table 2:
Prevention and early detection of high burden cancers in MICs: examples of feasible, cost-effective, interventions, target population, health system delivery level and country case examples.
| Target population | Delivery level | Country Examples | |
|---|---|---|---|
| Improved cancer surveillance in MICs | |||
| Population based cancer registries | All cancer cases in a defined population catchment area | National and subnational level, with central coordination | Zimbabwe National Cancer Registry, Kampala Cancer Registry (subnational)34 |
| Participation in epidemiological & clinical studies of cancer risk factors | General population in LMICs | Community based research | H3 Africa consortium on molecular epidemiology and risk factors for NCDs108 |
| Prevention of modifiable risk factors | |||
| Tobacco taxation | General population, current and potential future tobacco users | National, through legislation increasing excise taxes on tobacco | Philippines – introduction of high excise tobacco taxes in 2012 led to an estimated 3 million fewer smokers within 3 years31 |
| HPV vaccination | Girls aged 9-12 years | Primary care/community based School based for those enrolled |
A number of MICs including Zambia & Ethiopia have introduced community and school-based HPV vaccination program over the past 10 years, achieving >90% coverage 109 |
| Targeted & opportunistic cancer screening | |||
| Point of care diagnostics: HPV testing | Sexually-active women, with focus on high risk subpopulations: HIV(+), sex-workers, tobacco users | Primary care or community based | Argentina – used an existing network of trained CHWs to implement self-collection HPV tests among high-risk groups to increase coverage 4 fold110 |
| Screen & treat: VIA + HPV testing | As above | Primary care or community based | Zambia: since 2006 Zambia has used its HIV program infrastructure to introduce the Cervical Cancer Prevention Program, a nurse driven screen and treat program which initially focused on women with HIV and later expanded coverage to oter women, reaching 58,000 women within it’s first 5 years60 |
| Clinical breast examination (conditional recommendation) | Women aged 30 years+ | Primary care or community based | Malawi – delivery of CBE through trained lay women, implemented in primary care health clinics among women presenting for reasons other than a breast concern70 |
| Familial/hereditary risk stratification | First-degree relatives of patients with breast, colorectal cancers | Primary care (family history screening tools), secondary/tertiary care (familial cancer registries, kindred studies) | Nigeria – first-degree relative (FDR) registry maintained within African Research Group for Oncology’s multi-site hospital-based colorectal cancer registry. FDRs in registry invited to participate in high risk screening studies111 |
| Earlier detection of symptomatic cancers | |||
| Risk stratification tools | Symptomatic patients on first contact with health provider | Primary care | Nigeria – development of a cardinal symptoms tool for colorectal cancer, to prompt referral for further investigation of symptoms92 |
| Public awareness campaigns | General population | Community based | Rwanda (a LIC) introduced a public awareness campaign for women’s cancers in 2020 as part of it’s National Cancer Control Plan112 |
| Provider education | Community health workers, primary care | Community health and primary care facilities | Peru: Community-based Program for Breast Health, a collaboration between PATH, the Peruvian Ministry of Health, the National Cancer Institute (Lima), and the Regional Cancer Institute (Trujillo). Phased implementation of public and primary care provider education on breast cancer diagnosis improved capacity for early diagnosis among first-level health workers113 |
| Point of care diagnostics | Symptomatic patients presenting to primary care or a first level hospital | All levels of the health system but targeted at primary care, first level hospitals without advanced imaging and pathology capacity | Nigeria – prospective evaluation of urine-based POC testing for colorectal cancer using metabolomics114 |
The rising incidence of breast cancer in MICs has focused attention on the role of early detection and screening in nascent cancer care systems. Clinicians, policy-makers and patients are increasingly aware of the excess mortality associated with advanced stage of presentation and the relative success of mammography-based screening in reducing mortality in HICs.61 Earlier detection, timely referral and treatment of symptomatic breast cancer should be considered a pre-requisite to screening in all countries and should be prioritized over efforts to introduce screening programs.62 Even in the presence of robust cancer diagnostic and treatment services, the overall incidence of breast cancer is still lower in MICs than in HICs, which can significantly modify the cost-benefit and benefit-to-harm ratio for screening.15
Existing data from MICs do not support a role for breast cancer screening in reducing cancer-specific survival or overall mortality with either CBE or mammography.15 The impact of organized or opportunistic breast cancer screening on clinical stage-shifting (which may represent an earlier surrogate for survival in the presence of appropriate treatment), in LMICs is mixed. A recent national population-based analysis from Brazil did not show a measurable impact on the incidence of late-stage breast cancer ten years after the introduction of a policy recommending mammographic screening for women aged 50-69 years, which may be explained by low coverage rates, inequitable access and low follow up after a concerning screening finding.63 These experiences are explored in Figure 1.
Figure 1:
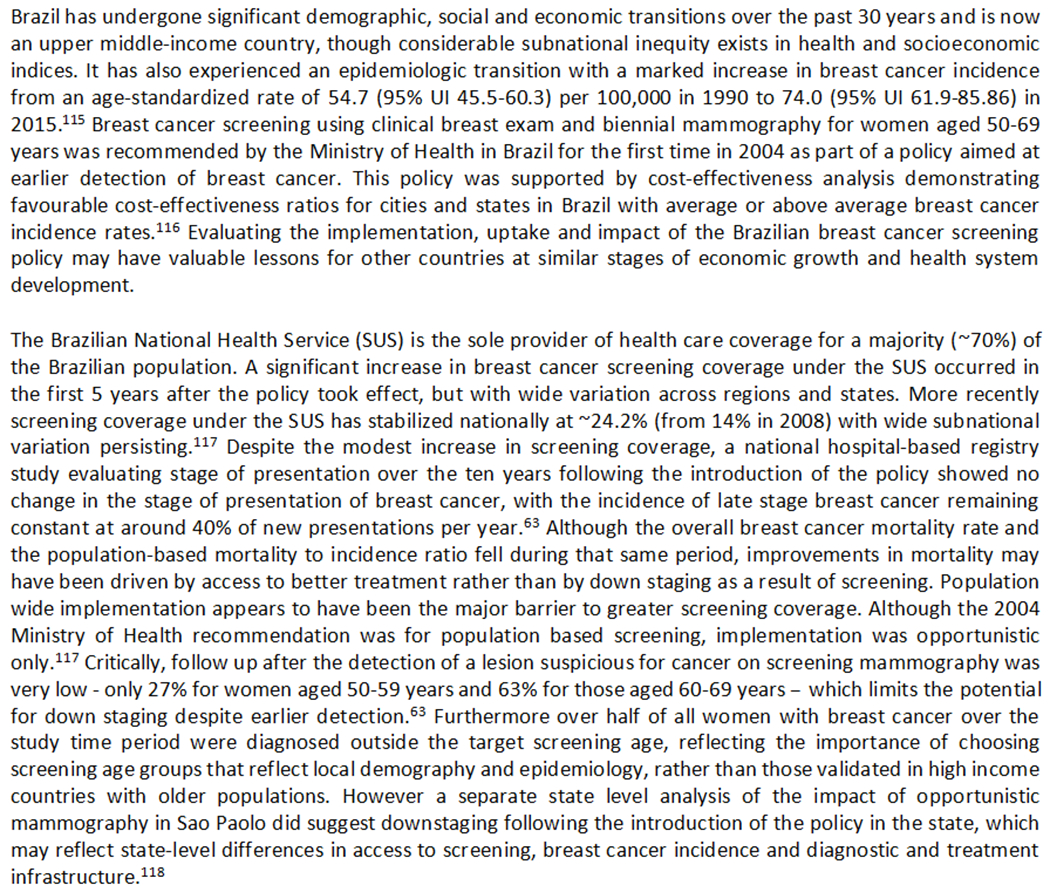
Mammographic screening for breast cancer in middle-income countries: lessons learned from Brazil
Measurable success in stage-shifting has been reported with opportunistic mammography-based screening in post-menopausal women in Malaysia, an upper-MIC, although this program has yet to demonstrate a positive impact on overall mortality.64 Mammography also requires specialized imaging infrastructure and its utility as a screening modality is dependent on image-quality and interpretation.4 Thus, mammographic screening has not been shown to be cost-effective in lower-middle income countries or low-income countries, and is supported by only weak economic data in select upper middle-income countries.65,66
CBE is a universal tool in breast cancer detection and surveillance. In most HICs it is no longer recommended as a screening modality but used as an adjunct in diagnosis and surveillance. However, in countries where mammography-based screening is not available, CBE continues to be investigated as a primary screening modality.15,67 Two large cluster randomized trials in India68 are currently evaluating CBE performed by trained primary health workers compared to breast cancer awareness education alone. .15 Recent results from the Mumbai trial demonstrated that CBE conducted every 2 years detected cancer at an earlier stage and led to a non-significant 15% reduction in breast cancer mortality overall, but a significant reduction in women aged >50.69 Estimates of CBE specificity in a screening setting are also needed, as smaller observational studies suggest highly variable performance, which may place an unmanageable burden on diagnostic facilities.70 A recent economic analysis of screening modalities for breast cancer outside of HICs concluded that both the evidence base for recommending mammography or CBE, and defining at-risk populations for targeted screening is limited and of low-quality.66 In the absence of high-quality experimental evidence, opportunistic screening with CBE by trained primary or community health workers has been conditionally recommended by the Breast Health Global Initiative where mammography is not feasible.62 The WHO has advocated for a focus on earlier detection of symptomatic cancers rather than the introduction of resource-intensive screening in the absence of a strong health system.16,67
The Disease Control Priorities (DCP) Network, which synthesizes evidence on the cost-effectiveness and feasibility of interventions for high burden cancers in LMICs have made several recommendations on screening. Only opportunistic and targeted high-risk cervical cancer screening is considered to meet the criteria for inclusion in the DCP ‘best buy’ interventions for essential cancer care.4 CBE by trained health workers may be a viable option in MICs but a lack of high quality longer-term evidence of its impact prevented its inclusion within the essential package. Interestingly, even where targeted screening of at-risk groups has been offered in MICs uptake is often low, and patient follow up after a suspicious screening finding variable.67 A systematic review suggested that a lack of knowledge about cancer and an understanding of the role of screening in early detection and cure were the key barriers to participation.71 This reinforces the need for education and public awareness as a core tenant of cancer control efforts and should be viewed as a prerequisite for the adoption of screening policy or programs.
Genetic risk factors and targeted screening/early detection
Identification of individuals and families at high risk for cancer based on familial and hereditary risk factors offers the opportunity for targeted screening and early detection. Very little is known about the proportion of common cancers with a hereditary basis in MICs and across geographic regions owing to a lack of cancer registry data, challenges with obtaining family histories and cause of death. For patients who present with clinical risk factors for a heritable syndrome, there is a dearth of affordable genetic testing, counselling and follow up.72 Although hereditary causes are likely to constitute only a small proportion of total cancer cases in MICs, genetic mutations associated with cancer syndromes (e.g. BRCA1/2) confer some of the highest lifetime risks for the development of cancer. Identification of patients and first-degree relatives at risk through clinical criteria, or where feasible genetic testing, would facilitate opportunities for targeted screening and early detection. With decreasing costs, multigene panel testing (e.g. for BRCA1/2, CHEK2, ATM, PALB2) is a cost-effective strategy in high-income countries compared to genetic testing for BRCA1/BRCA2 alone,73 but the cost and availability of next-generation sequencing and gene panel testing remains prohibitively expensive in many LMICs.72,74,75 Development of locally validated risk assessment tools for identifying patients who should undergo further genetic testing is needed alongside increased access to genetic services. This will require strengthening public and private capacity for genetic and molecular analyses. Building that capacity in parallel with cancer registries may be an actionable starting point. In Malaysia, offering BRCA mutation testing to early-stage breast cancer patients with risk factors on a locally validated risk assessment tool has been shown to be cost-effective compared to routine clinical screening.76 However, without a substantial price adjustment, BRCA testing is out of reach for most patients in lower-middle and low-income countries. For this reason, the Breast Health Global Initiative, which provides resource-stratified guidelines for breast cancer, recommends BRCA testing only in maximally resourced settings.77
Hereditary and familial risk factors are more common in colorectal cancer than in breast and cervical cancer. The prevalence and penetrance of hereditary colorectal cancer syndromes (e.g. Lynch Syndrome) are again poorly characterized in most MICs. A multicenter study from Nigeria demonstrated a higher proportion of microsatellite instability (i.e. 28%) and a lower rate of APC mutation in microsatellite stable disease compared to contemporary series from high-income countries. Unique germline risk loci have also recently been identified for CRC patients in East Asia compared to European CRC patients, suggesting hereditary and familial risks may vary across racial, ethnic and geographic regions.78 Translating these findings into clinical risk stratification tools will require a greater emphasis on cancer registry development and case-control studies that incorporate family history, molecular epidemiology, and evaluation of targeted screening strategies that include first degree relatives in MICs.79
Earlier diagnosis of symptomatic cancers
Delays in receiving cancer care have been described at three points: delays in seeking care, delays in reaching care and delays in receiving appropriate diagnosis and treatment. Many factors contribute to delays in seeking care (the time from recognising a symptom to seeking health care for it) - including health literacy, fear, stigma, financial and geographic barriers.80–83 These are well covered in other reviews.84 Delays in diagnosis following initial symptomatic presentation to a health provider can also significantly impact cancer outcomes.
Diagnostic delays (i.e. from first consultation with a health provider to diagnosis) have consistently been reported as the greatest contributor to overall delays for breast cancer in MICs.85–88 In studies from Brazil and Mexico, the average delay between symptomatic presentation to a doctor, and a diagnosis of breast cancer was 6-7 months.86,87 Delays in histological diagnosis after biopsy explained up to 3-4 months of this delay. Referral delays were longer in patients presenting with earlier stages of disease. In India, a mean delay of 2 months was seen after first presentation with symptomatic locally advanced breast cancer, with greater delays reported by patients from rural areas, lower education level, and those who had consulted an unregistered traditional medicine provider first.86 Several opportunities exist for reducing diagnostic delays in symptomatic individuals in MICs, and are summarised in Table 2.
Clinical stage-shifting through the earlier diagnosis of symptomatic cancers in MICs has received far less attention than asymptomatic screening in the literature and policy discourse. However, delays in diagnosis following presentation to a health care provider with cancer specific symptoms represents a considerable opportunity for improvement within existing systems of care. Strategies to improve early detection for cervical, breast and colorectal cancer have been shown to be cost-effective in upper- and lower-MICs, comparable to other commonly funded public health interventions,4 and associated with sizeable mortality reduction.17,42,89 For example, it is estimated that approximately 1/3 of all breast cancer deaths in SSA in the next decade could be prevented through earlier detection and improved access to treatment.89 In MICs, the estimated marginal costs of a package of interventions aimed at earlier detection and treatment of breast cancer ranges from $USD0.43-$1.29 per capita, and $USD0.29-0.87 per capita for cervical cancer.4
Not all patients that present with symptoms of cancer will have advanced disease. Symptomatic presentations with a palpable mass in breast cancer or rectal bleeding in colorectal cancer are common in earlier stage disease. Promoting awareness and recognition of cancer presentations at the time of first contact with a health provider - usually at a community or primary care level – and then ensuring appropriate and timely referral represents a tangible means for reducing supply side delays. This requires provider education of ‘red flag’ symptoms for common, high burden cancers. National and subnational data on demographic, familial and environmental risk factors that increase the pre-test probability of a cancer diagnosis are needed in many MICs to better inform provider education efforts. For example, CRC presents at a younger age than in HICs, increasing the probability that rectal bleeding in a younger patient is not from benign causes. The development of referral guidelines can support appropriate and timely investigation and referral of symptomatic patients, while minimizing unnecessary resource utilization. Patient navigation services are still rare in MICs, and almost exclusively based in tertiary referral centers where they have been used to facilitate linkages with follow-up services, provide counselling, coordinate appointments and maintain communication with patients and families.90,91 Expansion of these concepts into community and first referral sites may mitigate early delays and loss to follow up prior to a definitive diagnosis and serve to support patients through their cancer diagnosis and treatment journey.
The development of simple risk stratification models based on patients’ clinical symptoms may assist in earlier detection of colorectal cancer at the primary care level in MICs. The combination of self-reported rectal bleeding with change in bowel habit and/or weight loss predicted the likelihood of colorectal cancer in a Nigerian cohort of patients whose presenting complaint was rectal bleeding.92 In countries with scarce endoscopy capacity and high rates of non-colorectal cancer associated rectal bleeding (e.g. haemorrhoids, parasitic disease), both under-referral and over-referral can have significant negative impacts on waiting times and patient outcomes. Validated cancer-specific family history tools that are self-administered are in use in a number of HICs in both primary care and specialist settings.93 The role for locally developed family history tools in contexts where large immediate and extended families are common but the cause of death are often unknown or not disclosed to other family members requires further investigation. As efforts to deliver non-communicable disease management through primary care platforms increase in MICs, there is clearly opportunity to include education on common cancer-specific symptoms as part of provider training and public health campaigns.
Point of care (POC) testing can provide rapid results at the time of clinical encounter to inform clinical decision-making, diagnosis and early referrals. In MICs it can overcome some of the diagnostic limitations of a weak health system94 and allow for testing in the absence of traditional laboratories. POC testing has been successfully delivered at scale in both LICs and MICs for infectious diseases such as HIV, malaria and tuberculosis,95 but remains an underdeveloped area globally for cancer. This is in part because of the heavy reliance on advanced imaging techniques and histopathology for cancer diagnosis which are widely available and accessible in HICs, and a paucity of peripheral cancer biomarkers that can be used for screening and diagnostic purposes. The development of POC HPV testing, which can detect high grade pre-cancerous cervical lesions with higher sensitivity and comparable specificity to conventional cytology, represents the most promising POC test for cancer screening of asymptomatic women in MICs. While POC HPV tests have not been fully validated in the clinical setting, promising initial field results are emerging. In addition, POC HPV testing has been developed for self-collected vaginal specimens, which would greatly decrease the resource burden associated with clinician-screening.96 A meta-analysis suggests that while clinician-collected samples are still the gold standard, acceptable sensitivity and specificity can be reliably achieved with self-collection.97 A major benefit of POC HPV testing is that it can be combined with same-day treatment of pre-cancerous lesions (e.g. with cryotherapy) as part of single visit ‘screen and treat’ strategies, improving uptake of treatment and reducing the follow-up burden on both patients and providers.98
The use of visual inspection with acetic acid (VIA) as a POC test for diagnosing cervical cancer and high-grade pre-cancer changes has fallen out of favour as a leading strategy for cervical cancer screening in LICs and MICs with the emergence of HPV testing. In a landmark Indian randomised trial HPV testing was superior to no screening, cytology-based, and VIA screening in reducing advanced presentation and mortality from cervical cancer. 53 However, VIA may still represent a cost-effective strategy where HPV testing is unaffordable and cytopathology infrastructure is not available. Although operator dependent, VIA can be performed by primary care staff, is inexpensive, can be combined in a single visit with cryotherapy treatmen. In the presence of good training and sustained quality assurance, is an effective method to prevent cervical cancer.99,54
Finally, the role of digitisation of pathology and imaging, which allows reading and interpretation of biopsies and images remotely in the absence of local capacity, and the use of artificial intelligence (AI) to detect pre-cancerous and cancerous lesions, hold promise for overcoming major human resource limitations in MICs.18,100 The use of an AI-based program in conjunction with handheld ultrasound for triage of breast masses by minimally-trained health workers in Mexico is one example under evaluation. 101 However the clinical application of AI in cancer diagnostics remains in its infancy, and the utility, cost-effectiveness and feasibility for cancer detection have not yet been proven.102
Screening, Early Detection and Access to Healthcare Resources
Screening and early detection are only effective if treatment is available once latent disease is identified. Effective treatment is contingent on services being both physically accessible and affordable.103 In many MICs, effective health insurance coverage for cancer care is lacking. In Nigeria, only 5% of the population is covered by some form of prepaid health insurance 103 and cancer is often covered later within universal health coverage expansion pathways.104 There is emerging evidence to suggest that screening behaviour and cancer management are dictated by income.105 In the absence of a comprehensive health insurance system (i.e. public, private, or mixed), the efficacy of opportunistic and organized screening is lost to inequitable access to treatment services. Inadequate health services infrastructure, including systems to ensure timely definitive diagnosis, follow-up and treatment after a screen-detected finding, have been described as major barriers to successful implementation in several middle-income countries attempting to introduce mammographic screening. Indeed, women lost to follow up after a screen-detected cancer finding, and prior to either definitive diagnosis or treatment, has been reported in studies investigating the role of screening in LMICs. 63,106 In a study evaluating the effectiveness of screening mammography in Jakarta, of the 1100 women screened, 14 cancers were detected, but only 6 women returned for treatment.106 This may reflect structural, sociocultural, personal and financial barriers to accessing care62 that need to be addressed prior to, or at least alongside, the introduction of screening programs. For the benefits of screening to be realized, patients must undergo further investigation and treatment.
Conclusion
Population coverage with proven, cost-effective prevention and early detection strategies for high burden cancers is a cornerstone of effective cancer control. Direct national and subnational estimates of cancer incidence, prevalence and mortality are a critical first step in cancer control efforts. Without robust local data it is challenging to identify context-specific cancer risk factors and at-risk sub-populations for targeted interventions. In lower MICs and many upper MICs, the major modifiable risk factors for cancer continue to be infection (especially HPV) and tobacco. Large gains in infection- and tobacco-related cancer incidence and mortality can be made in a relatively short time, using proven, affordable, prevention strategies including HPV vaccination of at-risk groups, and tobacco taxation. These remain underutilised levers for cancer control in many MICs and should be considered priorities moving forward.
Presentation with advanced stage cancers, where the opportunity for curative care is greatly diminished, is far more common in LICs and MICs. Efforts to improve earlier detection and treatment of symptomatic cancers can provide marked mortality reductions in settings where advanced presentation is common, and are affordable and cost-effective in upper and lower-MICs where breast cancer incidence is highest. Early detection strategies include increasing public and provider awareness of cancer symptoms and curability and increasing access to providers trained in CBE for breast concerns. Coupled with efforts to strengthen the diagnostic and referral pathways at the health systems level, these should be considered core components of cancer stage-shifting and cancer control in MICs. This should be appropriately supported by national cancer policy, as well as financial and technical resources. Innovations in POC diagnostic tools, particularly those that reduce delays between first presentation, definitive diagnosis and treatment may provide answers to some existing challenges, in much the way HPV testing and ‘screen and treat’ approaches have changed the landscape for cervical cancer (Table 2).
Although the role of screening programs has received much attention in global cancer dialogue it is not the only, nor the most important, mechanism for earlier cancer detection. Screening of at risk-groups in MICs is well supported by high-quality evidence for cervical cancer, but has not been shown to be clinically or cost-effective at reducing cancer-specific survival or overall mortality in MICs for other common cancers. Additional trial results coupled with economic analysis are needed before drawing firm conclusions on the role of CBE in breast cancer screening.
Cancer prevention and early detection strategies cannot occur in isolation. Dedicated resources for the expansion of diagnostic and treatment services are also required, as not all cancers can be prevented, and without this the benefits of earlier diagnosis will be lost. Investment in cancer surveillance mechanisms will be critical for understanding national and subnational needs, and for monitoring the effectiveness of cancer control investments. By considering the continuum of cancer care required, and viewing cancer surveillance, prevention, screening and early detection as processes rather than discrete events, countries will be better placed to balance investments and efforts to scale-up across the cancer system.
FUNDING STATEMENT:
Thompson Family Foundation
Footnotes
CONFLICT OF INTEREST: None declared
References
- 1.Ferlay J, Colombet M, Soerjomataram I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 2019; 144(8): 1941–53. [DOI] [PubMed] [Google Scholar]
- 2.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018; 68(6): 394–424. [DOI] [PubMed] [Google Scholar]
- 3.Data: World Bank Country and Lending Groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups Accessed 03-31-21.
- 4.Gelband H, Sankaranarayanan R, Gauvreau CL, et al. Costs, affordability, and feasibility of an essential package of cancer control interventions in low-income and middle-income countries: key messages from Disease Control Priorities, 3rd edition. Lancet 2016; 387(10033): 2133–44. [DOI] [PubMed] [Google Scholar]
- 5.Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392(10159): 1923–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allemani C, Matsuda T, Di Carlo V, et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 2018; 391(10125): 1023–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crawford SC, Davis JA, Siddiqui NA, et al. The waiting time paradox: population based retrospective study of treatment delay and survival of women with endometrial cancer in Scotland. Bmj 2002; 325(7357): 196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olasehinde O, Alatise O, Omisore A, et al. Contemporary management of breast cancer in Nigeria: Insights from an institutional database. Int J Cancer 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berry DA, Cronin KA, Plevritis SK, et al. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med 2005; 353(17): 1784–92. [DOI] [PubMed] [Google Scholar]
- 10.Landy R, Pesola F, Castañón A, Sasieni P. Impact of cervical screening on cervical cancer mortality: estimation using stage-specific results from a nested case-control study. Br J Cancer 2016; 115(9): 1140–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Getaneh AM, Heijnsdijk EAM, Roobol MJ, de Koning HJ. Assessment of harms, benefits, and cost-effectiveness of prostate cancer screening: A micro-simulation study of 230 scenarios. Cancer Med 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zauber AG. The impact of screening on colorectal cancer mortality and incidence: has it really made a difference? Dig Dis Sci 2015; 60(3): 681–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology 2018; 68(2): 723–50. [DOI] [PubMed] [Google Scholar]
- 14.Ward ZJ, Scott AM, Hricak H, et al. Estimating the impact of treatment and imaging modalities on 5-year net survival of 11 cancers in 200 countries: a simulation-based analysis. Lancet Oncol 2020; 21(8): 1077–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sullivan T, Sullivan R, Ginsburg OM. Screening for Cancer: Considerations for Low- and Middle-Income Countries. In: Gelband H, Jha P, Sankaranarayanan R, Horton S, eds. Cancer: Disease Control Priorities, Third Edition (Volume 3). Washington (DC): The International Bank for Reconstruction and Development / The World Bank © 2015 International Bank for Reconstruction and Development / The World Bank.; 2015. [Google Scholar]
- 16.Yip CH. Downstaging is more important than screening for asymptomatic breast cancer. Lancet Glob Health 2019; 7(6): e690–e1. [DOI] [PubMed] [Google Scholar]
- 17.Birnbaum JK, Duggan C, Anderson BO, Etzioni R. Early detection and treatment strategies for breast cancer in low-income and upper middle-income countries: a modelling study. Lancet Glob Health 2018; 6(8): e885–e93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hosny A, Aerts H. Socially responsible technologies promise to help address health care inequalities. Science 2019; 22 November: 955–6. [Google Scholar]
- 19.Brierley J, O’Sullivan B, Asamura H, et al. Global Consultation on Cancer Staging: promoting consistent understanding and use. Nat Rev Clin Oncol 2019; 16(12): 763–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parkin DM. The evolution of the population-based cancer registry. Nat Rev Cancer 2006; 6(8): 603–12. [DOI] [PubMed] [Google Scholar]
- 21.Bray F, Ferlay J, Laversanne M, et al. Cancer Incidence in Five Continents: Inclusion criteria, highlights from Volume X and the global status of cancer registration. Int J Cancer 2015; 137(9): 2060–71. [DOI] [PubMed] [Google Scholar]
- 22.Jemal A, Torre L, Soerjomataram I, Bray F. The Cancer Atlas. Atlanta, GA: American Cancer Society; 2019. [Google Scholar]
- 23.Jedy-Agba E, McCormack V, Adebamowo C, Dos-Santos-Silva I. Stage at diagnosis of breast cancer in sub-Saharan Africa: a systematic review and meta-analysis. Lancet Glob Health 2016; 4(12): e923–e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gatti A, Haruyama R, Elit L, et al. How to reduce the impact of cervical cancer worldwide: Gaps and priority areas identified through the essential cancer and primary care packages: An analysis of effective interventions. Cancer 2020. [DOI] [PubMed] [Google Scholar]
- 25.Piñeros M, Znaor A, Mery L, Bray F. A Global Cancer Surveillance Framework Within Noncommunicable Disease Surveillance: Making the Case for Population-Based Cancer Registries. Epidemiol Rev 2017; 39(1): 161–9. [DOI] [PubMed] [Google Scholar]
- 26.Global Initiative for Cancer Registry Development. https://gicr.iarc.fr/ (accessed September 20th 2020).
- 27.Global Initiative for Cancer Registry Development: Sub Saharan Africa Hub. https://gicr.iarc.fr/hub/sub-saharan-africa/. Accessed 03-31-21.
- 28.de Vries E, Pardo C, Arias N, et al. Estimating the cost of operating cancer registries: Experience in Colombia. Cancer Epidemiol 2016; 45 Suppl 1(Suppl 1): S13–s9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goss PE, Lee BL, Badovinac-Crnjevic T, et al. Planning cancer control in Latin America and the Caribbean. Lancet Oncol 2013; 14(5): 391–436. [DOI] [PubMed] [Google Scholar]
- 30.Fitzmaurice C, Allen C, Barber RM, et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol 2017; 3(4): 524–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Diosana JL. Raising Tobacco Taxes: The Philippine Experience. Asian Pac J Cancer Prev 2020; 21(S1): 27–31. [DOI] [PubMed] [Google Scholar]
- 32.Kaiser K, Bredenkamp C, Iglesias R. Sin tax reform in the Philippines : transforming public finance, health, and governance for more inclusive development (English). Washington, D.C.: World Bank Group; 2016. [Google Scholar]
- 33.WHO Framework Convention on Tobacco Control. Geneva, Switzerland: World Health Organization, 2005. [Google Scholar]
- 34.Parkin D, Jemal A, Bray F, et al. Cancer in Sub-Saharan Africa. Geneva, Switzerland: Union for International Cancer Control, 2019. [Google Scholar]
- 35.Bray F, Soerjomataram I. The Changing Global Burden of Cancer: Transitions in Human Development and Implications for Cancer Prevention and Control. In: Gelband H, Jha P, Sankaranarayanan R, Horton S, eds. Cancer: Disease Control Priorities, Third Edition (Volume 3). Washington (DC): The International Bank for Reconstruction and Development / The World Bank © 2015 International Bank for Reconstruction and Development / The World Bank.; 2015. [PubMed] [Google Scholar]
- 36.Tabung FK, Brown LS, Fung TT. Dietary Patterns and Colorectal Cancer Risk: A Review of 17 Years of Evidence (2000-2016). Curr Colorectal Cancer Rep 2017; 13(6): 440–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cooke GS, Andrieux-Meyer I, Applegate TL, et al. Accelerating the elimination of viral hepatitis: a Lancet Gastroenterology & Hepatology Commission. Lancet Gastroenterol Hepatol 2019; 4(2): 135–84. [DOI] [PubMed] [Google Scholar]
- 38.Denny L, Herrero R, Levin C, Kim JJ. Cervical Cancer. In: Gelband H, Jha P, Sankaranarayanan R, Horton S, eds. Cancer: Disease Control Priorities, Third Edition (Volume 3). Washington (DC): The International Bank for Reconstruction and Development / The World Bank © 2015 International Bank for Reconstruction and Development / The World Bank.; 2015. [Google Scholar]
- 39.Goldie SJ, O’Shea M, Campos NG, Diaz M, Sweet S, Kim SY. Health and economic outcomes of HPV 16,18 vaccination in 72 GAVI-eligible countries. Vaccine 2008; 26(32): 4080–93. [DOI] [PubMed] [Google Scholar]
- 40.Cunningham MS, Davison C, Aronson KJ. HPV vaccine acceptability in Africa: a systematic review. Prev Med 2014; 69: 274–9. [DOI] [PubMed] [Google Scholar]
- 41.Bruni L, Saura-Lázaro A, Montoliu A, et al. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010-2019. Prev Med 2021; 144: 106399. [DOI] [PubMed] [Google Scholar]
- 42.Canfell K, Kim JJ, Brisson M, et al. Mortality impact of achieving WHO cervical cancer elimination targets: a comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet 2020; 395(10224): 591–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Madigan MP, Ziegler RG, Benichou J, Byrne C, Hoover RN. Proportion of breast cancer cases in the United States explained by well-established risk factors. J Natl Cancer Inst 1995; 87(22): 1681–5. [DOI] [PubMed] [Google Scholar]
- 44.Tamimi RM, Spiegelman D, Smith-Warner SA, et al. Population Attributable Risk of Modifiable and Nonmodifiable Breast Cancer Risk Factors in Postmenopausal Breast Cancer. Am J Epidemiol 2016; 184(12): 884–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McCormack VA, Boffetta P. Today’s lifestyles, tomorrow’s cancers: trends in lifestyle risk factors for cancer in low- and middle-income countries. Ann Oncol 2011; 22(11): 2349–57. [DOI] [PubMed] [Google Scholar]
- 46.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380(9859): 2224–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.O’Keefe SJ, Li JV, Lahti L, et al. Fat, fibre and cancer risk in African Americans and rural Africans. Nat Commun 2015; 6: 6342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sivaram S, Majumdar G, Perin D, et al. Population-based cancer screening programmes in low-income and middle-income countries: regional consultation of the International Cancer Screening Network in India. Lancet Oncol 2018; 19(2): e113–e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.World Health Assembly, 70. (2017). Cancer prevention and control in the context of an integrated approach. World Health Organization. https://apps.who.int/iris/handle/10665/275676. [Google Scholar]
- 50.Aballéa S, Beck E, Cheng X, et al. Risk factors for cervical cancer in women in China: A meta-model. Womens Health (Lond) 2020; 16: 1745506520940875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Parham GP, Mwanahamuntu MH, Kapambwe S, et al. Population-level scale-up of cervical cancer prevention services in a low-resource setting: development, implementation, and evaluation of the cervical cancer prevention program in Zambia. PLoS One 2015; 10(4): e0122169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cuzick J, Arbyn M, Sankaranarayanan R, et al. Overview of human papillomavirus-based and other novel options for cervical cancer screening in developed and developing countries. Vaccine 2008; 26 Suppl 10: K29–41. [DOI] [PubMed] [Google Scholar]
- 53.Sankaranarayanan R, Nene BM, Shastri SS, et al. HPV screening for cervical cancer in rural India. N Engl J Med 2009; 360(14): 1385–94. [DOI] [PubMed] [Google Scholar]
- 54.Sankaranarayanan R, Esmy PO, Rajkumar R, et al. Effect of visual screening on cervical cancer incidence and mortality in Tamil Nadu, India: a cluster-randomised trial. Lancet 2007; 370(9585): 398–406. [DOI] [PubMed] [Google Scholar]
- 55.Hull R, Mbele M, Makhafola T, et al. Cervical cancer in low and middle-income countries. Oncol Lett 2020; 20(3): 2058–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lemp JM, De Neve JW, Bussmann H, et al. Lifetime Prevalence of Cervical Cancer Screening in 55 Low- and Middle-Income Countries. Jama 2020; 324(15): 1532–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ginsburg OM, Chowdhury M, Wu W, et al. An mHealth model to increase clinic attendance for breast symptoms in rural Bangladesh: can bridging the digital divide help close the cancer divide? Oncologist 2014; 19(2): 177–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhang D, Advani S, Waller J, et al. Mobile Technologies and Cervical Cancer Screening in Low- and Middle-Income Countries: A Systematic Review. JCO Glob Oncol 2020; 6: 617–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Clifford GM, Tully S, Franceschi S. Carcinogenicity of Human Papillomavirus (HPV) Types in HIV-Positive Women: A Meta-Analysis From HPV Infection to Cervical Cancer. Clin Infect Dis 2017; 64(9): 1228–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mwanahamuntu MH, Sahasrabuddhe VV, Kapambwe S, et al. Advancing cervical cancer prevention initiatives in resource-constrained settings: insights from the Cervical Cancer Prevention Program in Zambia. PLoS Med 2011; 8(5): e1001032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nyström L, Rutqvist LE, Wall S, et al. Breast cancer screening with mammography: overview of Swedish randomised trials. Lancet 1993; 341(8851): 973–8. [DOI] [PubMed] [Google Scholar]
- 62.Ginsburg O, Yip CH, Brooks A, et al. Breast cancer early detection: A phased approach to implementation. Cancer 2020; 126 Suppl 10(Suppl 10): 2379–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dos-Santos-Silva I, De Stavola BL, Renna NLJ, et al. Ethnoracial and social trends in breast cancer staging at diagnosis in Brazil, 2001-14: a case only analysis. Lancet Glob Health 2019; 7(6): e784–e97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Teh YC, Tan GH, Taib NA, et al. Opportunistic mammography screening provides effective detection rates in a limited resource healthcare system. BMC Cancer 2015; 15: 405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.WHO Position Paper on Mammography Screening. Geneva, Switzerland: World Health Organization, 2014. [PubMed] [Google Scholar]
- 66.Zelle SG, Baltussen RM. Economic analyses of breast cancer control in low- and middle-income countries: a systematic review. Syst Rev 2013; 2: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.O’Donovan J, Newcomb A, MacRae MC, Vieira D, Onyilofor C, Ginsburg O. Community health workers and early detection of breast cancer in low-income and middle-income countries: a systematic scoping review of the literature. BMJ Glob Health 2020; 5(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mittra I, Mishra GA, Singh S, et al. A cluster randomized, controlled trial of breast and cervix cancer screening in Mumbai, India: methodology and interim results after three rounds of screening. Int J Cancer 2010; 126(4): 976–84. [DOI] [PubMed] [Google Scholar]
- 69.Mittra I, Mishra GA, Dikshit RP, et al. Effect of screening by clinical breast examination on breast cancer incidence and mortality after 20 years: prospective, cluster randomised controlled trial in Mumbai. Bmj 2021; 372: n256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gutnik L, Lee C, Msosa V, et al. Clinical breast examination screening by trained laywomen in Malawi integrated with other health services. J Surg Res 2016; 204(1): 61–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Islam RM, Billah B, Hossain MN, Oldroyd J. Barriers to Cervical Cancer and Breast Cancer Screening Uptake in Low-Income and Middle-Income Countries: A Systematic Review. Asian Pac J Cancer Prev 2017; 18(7): 1751–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yip CH, Evans DG, Agarwal G, et al. Global Disparities in Breast Cancer Genetics Testing, Counselling and Management. World J Surg 2019; 43(5): 1264–70. [DOI] [PubMed] [Google Scholar]
- 73.Manchanda R, Patel S, Gordeev VS, et al. Cost-effectiveness of Population-Based BRCA1, BRCA2, RAD51C, RAD51D, BRIP1, PALB2 Mutation Testing in Unselected General Population Women. J Natl Cancer Inst 2018; 110(7): 714–25. [DOI] [PubMed] [Google Scholar]
- 74.Nippert I “CAPABILITY” and “Genetic testing in emerging economies” (GenTEE). J Community Genet 2013; 4(3): 293–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hussain S Molecular-based screening and therapeutics of breast and ovarian cancer in low- and middle-income countries. Cancer Res Stat Tret 2020; 31: 81–4. [Google Scholar]
- 76.Lim KK, Yoon SY, Mohd Taib NA, et al. Is BRCA Mutation Testing Cost Effective for Early Stage Breast Cancer Patients Compared to Routine Clinical Surveillance? The Case of an Upper Middle-Income Country in Asia. Appl Health Econ Health Policy 2018; 16(3): 395–406. [DOI] [PubMed] [Google Scholar]
- 77.Anderson BO, Lipscomb J, Murillo RH, Thomas DB. Breast Cancer. In: Gelband H, Jha P, Sankaranarayanan R, Horton S, eds. Cancer: Disease Control Priorities, Third Edition (Volume 3). Washington (DC): The International Bank for Reconstruction and Development / The World Bank © 2015 International Bank for Reconstruction and Development / The World Bank.; 2015. [PubMed] [Google Scholar]
- 78.Lu Y, Kweon SS, Tanikawa C, et al. Large-Scale Genome-Wide Association Study of East Asians Identifies Loci Associated With Risk for Colorectal Cancer. Gastroenterology 2019; 156(5): 1455–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Knapp GC, Alatise OI, Olasehinde OO, et al. Is Colorectal Cancer Screening Appropriate in Nigeria? J Glob Oncol 2019; 5: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bhatia RK, Rayne S, Rate W, et al. Patient Factors Associated With Delays in Obtaining Cancer Care in Botswana. J Glob Oncol 2018; 4: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Brown CA, Suneja G, Tapela N, et al. Predictors of Timely Access of Oncology Services and Advanced-Stage Cancer in an HIV-Endemic Setting. Oncologist 2016; 21(6): 731–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mapanga W, Norris SA, Chen WC, et al. Consensus study on the health system and patient-related barriers for lung cancer management in South Africa. PLoS One 2021; 16(2): e0246716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pace LE, Mpunga T, Hategekimana V, et al. Delays in Breast Cancer Presentation and Diagnosis at Two Rural Cancer Referral Centers in Rwanda. Oncologist 2015; 20(7): 780–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Brand NR, Qu LG, Chao A, Ilbawi AM. Delays and Barriers to Cancer Care in Low- and Middle-Income Countries: A Systematic Review. Oncologist 2019; 24(12): e1371–e80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Unger-Saldaña K, Guadiamos MC, Vega AMB, Anderson BO, Romanoff A. Delays to diagnosis and barriers to care for breast cancer in Mexico and Peru: a cross sectional study. Lancet Glob Health 2020; 8. [Google Scholar]
- 86.Chintamani Tuteja A, Khandelwal R, et al. Patient and provider delays in breast cancer patients attending a tertiary care centre: a prospective study. JRSM Short Rep 2011; 2(10): 76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Rezende MC, Koch HA, Figueiredo Jde A, Thuler LC. [Factors leading to delay in obtaining definitive diagnosis of suspicious lesions for breast cancer in a dedicated health unit in Rio de Janeiro]. Rev Bras Ginecol Obstet 2009; 31(2): 75–81. [DOI] [PubMed] [Google Scholar]
- 88.Agodirin O, Olatoke S, Rahman G, et al. Impact of Primary Care Delay on Progression of Breast Cancer in a Black African Population: A Multicentered Survey. J Cancer Epidemiol 2019; 2019: 2407138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.McCormack V, McKenzie F, Foerster M, et al. Breast cancer survival and survival gap apportionment in sub-Saharan Africa (ABC-DO): a prospective cohort study. Lancet Glob Health 2020; 8(9): e1203–e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Freeman HP, Rodriguez RL. History and principles of patient navigation. Cancer 2011; 117(15 Suppl): 3539–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dalton M, Holzman E, Erwin E, et al. Patient navigation services for cancer care in low-and middle-income countries: A scoping review. PLoS One 2019; 14(10): e0223537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Alatise OI, Ayandipo OO, Adeyeye A, et al. A symptom-based model to predict colorectal cancer in low-resource countries: Results from a prospective study of patients at high risk for colorectal cancer. Cancer 2018; 124(13): 2766–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cleophat JE, Nabi H, Pelletier S, Bouchard K, Dorval M. What characterizes cancer family history collection tools? A critical literature review. Curr Oncol 2018; 25(4): e335–e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wilson ML, Fleming KA, Kuti MA, Looi LM, Lago N, Ru K. Access to pathology and laboratory medicine services: a crucial gap. Lancet 2018; 391(10133): 1927–38. [DOI] [PubMed] [Google Scholar]
- 95.Xiong Y, Luo Y, Li H, Wu W, Ruan X, Mu X. Rapid visual detection of dengue virus by combining reverse transcription recombinase-aided amplification with lateral-flow dipstick assay. Int J Infect Dis 2020; 95: 406–12. [DOI] [PubMed] [Google Scholar]
- 96.Toliman P, Badman SG, Gabuzzi J, et al. Field Evaluation of Xpert HPV Point-of-Care Test for Detection of Human Papillomavirus Infection by Use of Self-Collected Vaginal and Clinician-Collected Cervical Specimens. J Clin Microbiol 2016; 54(7): 1734–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Arbyn M, Verdoodt F, Snijders PJ, et al. Accuracy of human papillomavirus testing on self-collected versus clinician-collected samples: a meta-analysis. Lancet Oncol 2014; 15(2): 172–83. [DOI] [PubMed] [Google Scholar]
- 98.Lott BE, Trejo MJ, Baum C, et al. Interventions to increase uptake of cervical screening in sub-Saharan Africa: a scoping review using the integrated behavioral model. BMC Public Health 2020; 20(1): 654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sauvaget C, Fayette JM, Muwonge R, Wesley R, Sankaranarayanan R. Accuracy of visual inspection with acetic acid for cervical cancer screening. Int J Gynaecol Obstet 2011; 113(1): 14–24. [DOI] [PubMed] [Google Scholar]
- 100.Xue P, Ng MTA, Qiao Y. The challenges of colposcopy for cervical cancer screening in LMICs and solutions by artificial intelligence. BMC Med 2020; 18(1): 169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Love SM, Berg WA, Podilchuk C, et al. Palpable Breast Lump Triage by Minimally Trained Operators in Mexico Using Computer-Assisted Diagnosis and Low-Cost Ultrasound. J Glob Oncol 2018; 4: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wilson ML, Sayed S, Horton S, Fleming KA. Artificial intelligence can augment global pathology initiatives - Authors’ reply. Lancet 2018; 392(10162): 2352. [DOI] [PubMed] [Google Scholar]
- 103.Gulliford M, Figueroa-Munoz J, Morgan M, et al. What does ‘access to health care’ mean? J Health Serv Res Policy 2002; 7(3): 186–8. [DOI] [PubMed] [Google Scholar]
- 104.Jamison DT, Summers LH, Alleyne G, et al. Global health 2035: a world converging within a generation. Lancet 2013; 382(9908): 1898–955. [DOI] [PubMed] [Google Scholar]
- 105.Okoronkwo IL, Ejike-Okoye P, Chinweuba AU, Nwaneri AC. Financial barriers to utilization of screening and treatment services for breast cancer: an equity analysis in Nigeria. Niger J Clin Pract 2015; 18(2): 287–91. [DOI] [PubMed] [Google Scholar]
- 106.Kardinah D, Anderson BO, Duggan C, Ali IA, Thomas DB. Short report: Limited effectiveness of screening mammography in addition to clinical breast examination by trained nurse midwives in rural Jakarta, Indonesia. Int J Cancer 2014; 134(5): 1250–5. [DOI] [PubMed] [Google Scholar]
- 107.Cancer Today. International Agency for Research on Cancer Global Cancer Observatory. www.gco.iarc/fr. Accessed 04-06-2021.
- 108.H3 Africa: Human Hereditary and Health in Africa. https://h3africa.org/. Accessed 01-12-2021.
- 109.Sayinzoga F, Umulisa MC, Sibomana H, Tenet V, Baussano I, Clifford GM. Human papillomavirus vaccine coverage in Rwanda: A population-level analysis by birth cohort. Vaccine 2020; 38(24): 4001–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Arrossi S, Paolino M, Thouyaret L, Laudi R, Campanera A. Evaluation of scaling-up of HPV self-collection offered by community health workers at home visits to increase screening among socially vulnerable under-screened women in Jujuy Province, Argentina. Implement Sci 2017; 12(1): 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.African Research Group for Oncology (ARGO) Colorectal Cancer Research. https://argo-research.org/colorectal-cancer/. Accessed 01122021.
- 112.Rubagumya F, Costas-Chavarri A, Manirakiza A, et al. State of Cancer Control in Rwanda: Past, Present, and Future Opportunities. JCO Glob Oncol 2020; 6: 1171–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Duggan C, Dvaladze AL, Tsu V, et al. Resource-stratified implementation of a community-based breast cancer management programme in Peru. Lancet Oncol 2017; 18(10): e607–e17. [DOI] [PubMed] [Google Scholar]
- 114.NIH Division of Cancer Prevention, Funding & Grants: Point of care, real-time urine metabolomics test to diagnose colorectal cancers and polyps in low- and middle-income countries. RFA-CA-15-024. https://prevention.cancer.gov/funding-and-grants/funded-grants/UH3CA257869. Accessed 01122021.
- 115.Guerra MR, Nogueira MC, Malta DC, et al. Inequalities in the burden of female breast cancer in Brazil, 1990-2017. Popul Health Metr 2020; 18(Suppl 1): 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ribeiro RA, Caleffi M, Polanczyk CA. [Cost-effectiveness of an organized breast cancer screening program in Southern Brazil]. Cad Saude Publica 2013; 29 Suppl 1: S131–45. [DOI] [PubMed] [Google Scholar]
- 117.Rodrigues DCN, Freitas-Junior R, Rahal RMS, et al. Temporal changes in breast cancer screening coverage provided under the Brazilian National Health Service between 2008 and 2017. BMC Public Health 2019; 19(1): 959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Vale DB, Filho CC, Shinzato JY, Spreafico FS, Basu P, Zeferino LC. Downstaging in opportunistic breast cancer screening in Brazil: a temporal trend analysis. BMC Cancer 2019; 19(1): 432. [DOI] [PMC free article] [PubMed] [Google Scholar]


