Abstract
Objective:
Brief computer-delivered interventions (CDIs) reduce college student drinking and related problems but can be less efficacious and enduring than in-person interventions. The current study examined: (a) the utility of emailed personalized boosters after an evidence-based online CDI for alcohol (i.e., e-CHECKUP TO GO), and (b) the added value of including protective behavioral strategies (PBS) in boosters containing personalized normative feedback (PNF) versus PNF alone.
Method:
528 young adult (ages 18–24) college drinkers (71.6% female; 52.5% Black, 40.3% White) with a mean age of 19.9 years (SD = 1.65) were randomized to receive: CDI-only; CDI plus a PNF-only booster; or CDI plus a booster containing both PNF and PBS feedback. Booster emails were sent 2 weeks post-intervention. Online surveys completed pre-intervention and at 1 and 3 months assessed alcohol consumption, problems, descriptive normative perceptions, and PBS use.
Results:
The CDI led to significant reductions in alcohol consumption across all conditions, with no effect of boosters on drinking. Controlling for quantity, no reductions in problems were observed. Descriptive norms reduced significantly, with no condition differences. Only PBS use showed condition effects, such that the CDI-only and PNF-only booster groups reported reduced PBS use at 1 month, but the norms-plus-PBS booster group did not.
Conclusions:
The CDI was sufficient to change alcohol consumption and perceived norms without boosters, although the inclusion of boosters with PBS feedback may mitigate against PBS use reductions. Longer follow-ups may detect delayed booster benefits, or a larger dose through repeated exposure over time may be needed.
Keywords: brief intervention, boosters, protective behavioral strategies, college students, alcohol
College student heavy episodic drinking is pervasive and problematic (Hingson et al., 2017; SAMHSA, 2020). College students who engage in heavy episodic drinking increase their risk for experiencing negative consequences (Conway & DiPlacido, 2015; Patrick et al., 2020). Brief online alcohol interventions, commonly called computer-delivered interventions (CDIs) can be far-reaching and have demonstrated efficacy for reducing college drinking and related problems, but they can be less efficacious and enduring than their in-person counterparts (Carey et al., 2009, 2012). Boosters have shown promise as a way to strengthen and extend the effects of brief interventions (Braitman & Henson, 2016; Braitman & Lau-Barraco, 2018; Tahaney & Palfai, 2017), but further examination is needed as to what content is most effective. Norms have a robust association of change with brief interventions and boosters, but the findings from studies that have included protective behavioral strategies (PBS) are mixed (Braitman & Lau-Barraco, 2020; Reid & Carey, 2015). The current study aimed to: (1) evaluate whether emailed boosters were effective after an efficacious evidence-based online alcohol intervention, given that prior research has only validated them after an online intervention with less empirical support (Braitman & Henson, 2016; Braitman & Lau-Barraco, 2018), (2) examine the added benefit of including PBS in a booster incorporating personalized normative feedback (PNF) versus a PNF booster alone, and (3) evaluate the impact of the boosters on the proximal outcomes of descriptive norms and PBS use.
Brief Alcohol Interventions
A myriad of brief alcohol interventions have been used across campuses nationwide showing promising effects in regards to reducing problematic drinking and related problems (for systematic reviews and meta-analyses, see Carey et al., 2009, 2012; Hennessy et al., 2019; Moreira et al., 2009; Samson & Tanner-Smith, 2015). In general, prior meta-analytic studies that compared brief alcohol interventions delivered in-person versus remotely or online have found that in the short-term (i.e., 6/13 weeks or less) both types of intervention modalities yielded small effect sizes on alcohol consumption and related problems. These effects were maintained longer term only for the in-person interventions (27+ weeks; Carey et al., 2012; Cole et al., 2018), which typically consisted of brief motivational interventions (BMIs; single-session, feedback interventions conducted in motivational interviewing style). Given that effects of brief online interventions are not as strong or long-lasting as in-person interventions, it is important to explore how to increase their effectiveness.
One well-supported and widely used brief online intervention is eCHECKUP TO GO (San Diego State University Research Foundation, 2018). This evidence-based intervention can be customized with institution-specific information (e.g., adding campus-specific social norms data and resources) and the feedback is personalized for each participant (e.g., personalized BAC chart, reported health and personal consequences, health and wellness goals, family risk factors). eCHECKUP TO GO has been effective at reducing alcohol-related outcomes, as demonstrated repeatedly in college samples, with significant reductions in alcohol outcomes compared to assessment-only controls 1 month later (Hustad et al., 2010), 8 weeks later (Walters et al., 2007), and 3 months later (Doumas et al., 2011; Doumas & Anderson, 2009). A recent network meta-analysis found eCHECKUP TO GO to be the most efficacious completely computerized brief alcohol intervention for short-term reductions in frequency of heavy drinking (i.e., could be delivered online or via CD-ROM, but no required in-person component, including Alcohol 101/101 Plus, AlcoholEdu, Check Your Drinking, College Drinker’s Check-up, and Tertiary Health Research Intervention via Email [THRIVE]; Hennessy et al., 2019). However, longer-term (3–6 months) alcohol consumption was not significantly reduced, making this intervention an ideal target for boosters to strengthen and extend intervention effects.
Boosters after Brief Alcohol Interventions
Boosters have emerged as a promising method to increase intervention efficacy or prolong the duration of intervention effects (e.g., Braitman & Henson, 2016; Meshesha et al., 2020; Tahaney & Paulfai, 2017). Boosters are brief, delayed follow-up sessions designed to target the same behavior. The content can be novel, or reminders of information provided in the original intervention. The modality may be similar or different to the original intervention (e.g., intensive in-person sessions versus text or email). Boosters have the potential to reinforce key program components when their effects are starting to decay. Boosters have been successfully implemented to enhance alcohol outcomes, yielding long-term effects in treatment-seeking (e.g., Mendoza et al., 2012; Meshesha et al., 2020; Walitzer & Connors, 2007) and community-based non-treatment-seeking (Field et al., 2014; Longabaugh et al., 2001; Mello et al., 2005; Monti et al., 2007; Wurdak et al., 2016) samples. Although boosters appear to show promise with these samples, their application to enhance the impact of brief alcohol interventions with college students has been limited.
To date, few studies have assessed the unique impact of adding boosters to a brief intervention targeting college drinking. Many of these studies have focused on reducing problematic college drinking among specific populations such as alcohol-mandated students (Barnett et al., 2007; Carey et al., 2018; Linowski et al., 2016; Suffoletto et al., 2016), or fraternity members (Caudill et al., 2007). However, a limited number of studies have examined boosters in general college drinking samples (Braitman & Henson, 2016; Braitman & Lau-Barraco, 2018; Neighbors et al., 2010; Tahaney & Palfai, 2017; Wood et al., 2010). These will be summarized next.
Boosters among High-Risk College Drinkers
Three studies have focused on the effects of boosters among mandated students, with boosters consisting of electronically-delivered PNF three months later (Linowski et al., 2016), 12 emails delivering PNF across 6 weeks (starting one month post-intervention; Carey et al., 2018), or more time with the intervention one month later (25 additional minutes of in-person motivational interviewing or 25 additional minutes with the Alcohol 101 program; Barnett et al., 2007). These studies found no changes in overall consumption (Barnett et al., 2007; Carey et al., 2018; Linowski et al., 2016), with one study even finding a small but significant increase in alcohol-related problems for those in the booster condition (Carey et al., 2018). Thus, the evidence indicates that mandated students do not demonstrate further reductions in alcohol consumption after receiving a delayed booster, regardless of whether the original intervention was an in-person motivational intervention (Barnett et al., 2007; Carey et al., 2018; Linowski et al., 2016) or computer-delivered alcohol education (Alcohol 101 delivered via CD-ROM; Barnett et al., 2007). These findings suggest that interventions delivered to mandated students are effective, and no additional benefit is derived from adding booster sessions.
In another study of high-risk drinkers, fraternity members were block randomized into three conditions: assessment-only control, intervention only (a three-hour in-person skills-based training), or intervention plus booster sessions (Caudill et al., 2007). The booster sessions consisted of two 90-minute in-person sessions 5 and 11 months later that repeated the intervention content. Both active conditions reported reduced consumption at the 6-month follow-up, but these reductions were not maintained over time. Those in the booster condition showed stronger reductions, but only if they were frequent heavy drinkers at baseline. These mixed findings suggest that boosters may hold promise to curb problematic drinking among high-risk groups (such as frequent heavy drinkers), but further refinement of booster content may be necessary to increase efficacy among other drinkers.
Boosters among General College Drinkers
Five studies have examined boosters in general college drinker samples (Braitman & Henson, 2016; Braitman & Lau-Barraco, 2018; Neighbors et al., 2010; Tahaney & Palfai, 2017; Wood et al., 2010). Wood et al. (2010) randomized incoming students to receive an in-person brief motivational intervention (BMI) or not, and to receive a parent-based intervention or not. Both interventions incorporated booster sessions that consisted of content similar to the initial intervention. Students who received a BMI were less likely to initiate heavy episodic drinking or alcohol-related problems at follow-up. However, because there was no intervention-only group that received the original intervention but no booster, it was not possible to make conclusions about the effectiveness of the booster sessions specifically.
In a study examining text message boosters after the online program eCHECKUP TO GO (Tahaney & Palfai, 2017), college students were randomized to one of three conditions: assessment-only control, intervention only, or intervention plus daily text message boosters for one month (re-iterating the content from eCHECKUP TO GO), starting immediately after completing the intervention. Those who received the text message boosters reported less weekend drinking at the 1-month follow-up than the other groups. They also reported fewer heavy drinking episodes than the assessment-only control, whereas the intervention only condition did not, suggesting the value of intensive boosters. However, the conditions did not differ on alcohol-related problems.
The remaining three studies with general college drinkers provided support for including information on descriptive norms as a central part of the booster content (Braitman & Henson, 2016; Braitman & Lau-Barraco, 2018; Neighbors et al., 2010). Descriptive norms (i.e., an individual’s perceptions of how much other referent groups perform a behavior) are a strong predictor of alcohol use (Borsari & Carey, 2003), and successful interventions often include personalized normative feedback (PNF; Cole et al., 2018). PNF involves providing students with feedback about how their drinking compares with a referent group (e.g., typical student at their school). PNF has been efficacious when delivered both in-person or online (Moreira et al., 2009), and is a robust mechanism of post-intervention change when the PNF provides specific referents rather than generic (Reid & Carey, 2015).
Not surprisingly, findings from studies that provided PNF as part of their boosters have been promising. Neighbors et al. (2010) conducted a study with a 2 (PNF type: gender-specific versus not) x 2 (number of administrations: once versus four times over two years) + 1 (attention control condition) design. The PNF provided included information regarding participant own drinking behavior, participant perceptions of other students’ drinking behavior on the same campus, and other students’ self-reported drinking behavior in text and bar graph formats. The condition that received gender-specific PNF four times over two years (at baseline, plus 6, 12, and 18 months later) observed significant reductions in drinking compared to the control group. These reductions were not significantly different from those in the control group for those who had only received the gender-specific PNF only once, or for those whose PNF was not gender-specific. The repeated administrations of PNF could be conceived of as a multi-session intervention (PNF sent four times), but given the amount of time that passed between the administrations of the PNF (6 months), it is more likely the later PNF administrations served as boosters. These findings suggest receiving delayed reminders of relevant information (i.e., boosters) may help college drinkers maintain drinking reductions, particularly when the information is tailored to salient referent groups.
The two remaining studies with non-mandated college drinkers both incorporated gender-specific PNF and protective behavioral strategies (PBS; strategies individuals use to moderate their drinking; Martens et al., 2004; Sugarman & Carey, 2007). Braitman and Henson (2016) randomized college drinkers to receive an online intervention (i.e., Alcohol 101 Plus) only or the same intervention plus an emailed feedback booster two weeks later. Alcohol 101 Plus has mixed empirical support; as reviewed in Braitman and Henson (2016), only four out of seven studies examining Alcohol 101 found it yielded reductions in alcohol use and/or problems. Tailored booster content consisted of both PNF (percentage of male/female students [gender-matched] at that same institution that drink less than the participant) and reminders of PBS (reported as previously used versus not). For those who had received the booster, reductions in several risky consumption variables were observed at Week 4 when compared to the intervention-only control condition. Baseline levels of PBS moderated the booster effect such that alcohol consumption reductions post-booster were greater for students who had been practicing fewer PBS prior to the study start, suggesting PBS feedback may play an important role in the utility of the booster for those not already engaged in regular use of PBS.
In a subsequent study, Braitman and Lau-Barraco (2018) utilized the same intervention and similar personalized boosters (including PNF [average weekly consumption of male and female students at that same institution] and reminders of PBS reported as previously used versus not), adding an assessment-only control and following participants for up to 9 months post-intervention. The booster email was sent two weeks post- intervention. In the full sample, the intervention plus personalized booster condition did not reduce consumption more than control. However, moderation analyses revealed that the booster was effective in reducing both alcohol consumption and problems for students who were of legal drinking age (ages 21–24), compared to intervention-only and assessment-only controls. A follow-up examination revealed that descriptive norms mediated these post-booster reductions in drinking, but PBS did not (Braitman & Lau-Barraco, 2020), suggesting the PNF may have been more effective than the PBS feedback. Research support for PBS as a post-intervention mechanism of change is mixed. Reid and Carey (2015) found in their review of mechanisms of change for college drinking interventions that half of studies that examined PBS supported it as a mediator of intervention efficacy. Researchers have noted lingering measurement issues regarding PBS (see Prince et al., 2013), and studies have demonstrated that changing response options for these measures can dramatically change associations with alcohol consumption (Braitman et al., 2015; Kite et al., 2013). A comparison of receiving PBS feedback as part of the booster versus not would provide a more direct examination of the utility of PBS feedback.
In summary, the evidence most supportive of booster efficacy comes from general student population samples. However, content of both the primary brief intervention (eCHECKUP TO GO and Alcohol 101 Plus) and the boosters has varied. Notably, a promising booster (PNF plus PBS feedback) has only been tested after Alcohol 101 Plus, an intervention that allows participants to navigate freely through the content and does not necessarily provide tailored feedback. Furthermore, a recent network meta-analysis found non-significant effect sizes for Alcohol 101 Plus compared to controls across all indicators of alcohol consumption examined (Hennessy et al., 2019). In contrast, eCHECKUP TO GO is considered to be the most efficacious computer-delivered brief alcohol intervention (i.e., could be delivered online or via CD-ROM, but no in-person component; Carey et al., 2016; Hennessy et al., 2019). A stringent test of the value of boosters would involve an efficacious preliminary intervention (eCHECKUP TO GO), and a systematic evaluation of booster content.
The Current Study
The current study sought to examine: 1) the utility of emailed personalized boosters after receiving an evidence-based online intervention for alcohol, commonly referred to as a computer-delivered intervention (CDI; i.e., eCHECKUP TO GO), 2) the added value of harm reduction strategies (i.e., PBS) to norms-focused boosters (i.e., PNF) versus PNF alone, and 3) if the boosters impacted the intended proximal outcomes of descriptive norms and PBS use. Participants were assigned to receive: CDI-only; CDI plus a booster containing PNF alone; or CDI plus a booster containing both PNF and PBS feedback. Given the booster has yielded significantly greater alcohol reductions in prior studies (up to 1 month, Braitman & Henson, 2016; up to 9 months for legal age drinkers, Braitman & Lau-Barraco, 2018), we hypothesized that participants who received either booster would have greater reductions in drinking and related problems than those who receive only the CDI. Considering the mixed findings that a booster containing PBS feedback was effective at reducing drinking only for those low in PBS use at baseline (Braitman & Henson, 2018) suggesting the utility of PBS feedback, but that PBS did not serve as a mediator of booster efficacy and was not impacted by the booster (Braitman & Lau-Barraco, 2020), a comparison of the conditions receiving PNF alone versus PNF and PBS feedback in the emailed boosters will serve as a more direct examination of the utility of PBS feedback in boosters. Finally, due to prior findings that emailed booster feedback containing norms and PBS was significantly more effective for legal age college drinkers (ages 21–24) than underage college drinkers (ages 18–20; Braitman & Lau-Barraco, 2018), and was more effective for those lower in PBS use at baseline (Braitman & Henson, 2016), legal drinking status by age and PBS use at baseline were explored as a potential moderators of booster efficacy as an exploratory aim of the study.
Method
Participants
Participants were students enrolled at a large, southeastern public university. To be eligible, participants must have been between the ages of 18–24, and consumed at least one alcoholic beverage in the previous 2 weeks. Potential participants were recruited through both an undergraduate psychology research pool (75.9%) and student announcement emails sent to the general study body (24.1%). Of the 545 students that completed the baseline questionnaire, 13 were excluded due to ineligibility (i.e., alcohol consumption and age) and 4 were excluded for not following the protocol. The final sample included 528 participants (71.6% female) with a mean age of 19.9 years (SD = 1.65). Participants could endorse more than one race; 52.5% identified as Black, 40.3% as White, 9.7% as Asian or Pacific Islander, 3.6% as Native American, and 11.9% reported more than one race.. For compensation, participants in the research pool had their choice of either research credits or a $20 gift card. Participants from the general student body were compensated with the gift card. All participants received a $10 gift card for each follow-up survey they completed, and a $10 bonus gift card if they completed both follow-up surveys, for a maximum of $50 (if monetary compensation was chosen for the baseline protocol, and both follow-up surveys were completed).
Procedure
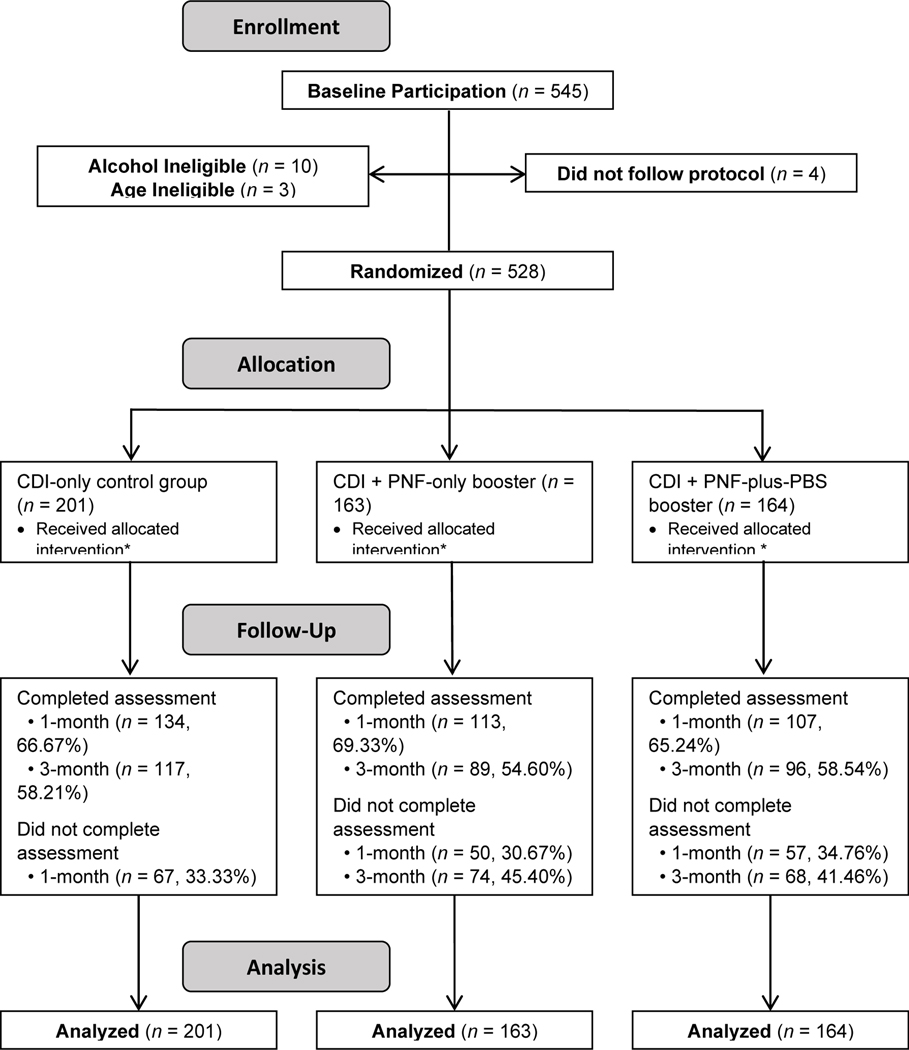
Participants came to the research lab for the baseline session. After consenting to participate, they completed an online survey where they were randomly assigned to study condition. Next, they completed the alcohol-focused online prevention and intervention program, eCHECKUP TO GO (San Diego Research Foundation, 2018). Participants were randomized into one of three intervention groups, stratified by gender: 1) no booster received (CDI-only control), 2) norms-only booster, or 3) norms-plus-PBS booster. The content of both the intervention and booster emails are described in more detail below. Boosters were sent via email two weeks after baseline participation. Emails were signed from a gender-matched research staff member. In the baseline survey, participants were asked to select their gender from three options: male, female, and other. As anticipated, not many participants selected other (n = 1), so rather than creating a separate stratification for this group, they were included with the female stratification and gender-matching emails. Thus, the groups represented male versus not male. Participants then received links to the follow-up surveys 1 and 3 months after baseline. Attrition rates were similar for all groups (see Figure 1), with retention ranging from 65%−69% across condition at the 1-month assessment, and from 55%−59% at the 3-month assessment. Study enrollment began in April 2017 and ended in December 2017, with the final follow-up assessment completed in April 2018. The trial was approved by the university’s Institutional Review Board and registered on the clinicaltrials.gov website (The trial was approved by the university’s Institutional Review Board and registered on the clinicaltrials.gov website.).
Figure 1. CONSORT Participant Flow Diagram.
Note. CDI = computer-delivered intervention, PNF = personalized normative feedback, PBS = protective behavioral strategies. *We can confirm the participants completed the online CDI and their booster email did not bounce back, but we do not know if they read the email.
Materials
Intervention
The eCHECKUP TO GO program is an online CDI in which participants first answer questions about their drinking behaviors (including how much they typically spend, what they like about alcohol, perceptions of peer use), as well as how they like to spend their time and goals they have. The program then provides participants with personalized feedback regarding their alcohol consumption, including information such as a tolerance level, a profile of how their alcohol use compares to others (PNF), personal risk factors and costs, and how alcohol use hinders their goals. Participants are provided a tolerance level that is estimated using the participant’s peak monthly BAC with feedback about whether this reflects low, medium, or high risk for alcohol dependence. In addition, participants select goals related to their health and fitness, relationships, career and life goals, and self-esteem as well as what they could do meet their goals. Then, participants selected things they could decrease or take out of their life completely, such as feeling bad about themselves due to drinking or being hung over. As part of this feedback review, after being reminded of some of their goals and aspirations, participants select PBS they may engage to change their alcohol consumption.
Booster
The norms-only booster included feedback and corrections on descriptive normative perceptions reported in the initial survey (i.e., PNF). The norms-plus-PBS booster included this same PNF, plus reminders of harm reduction strategies (PBS; e.g., “Choose to avoid situations where heavy drinking is likely”) presented separately for those they reported and those they might consider starting to use. The PNF used institution-specific data from the CORE Institute’s Alcohol and Drug Survey, separated by gender. The feedback provided participants with a colorful bar graph and accompanying text that compared: a) their reported typical weekly consumption, b) their normative perceptions (i.e., what they think their close friends and other typical students at their university consume), c) the average consumption of actual male and female students at their university, and d) the percentage of gender-matched students at their university who drink less than them. These norms provided in the booster email are more specific to the participant than what was provided in the intervention (reminder of their own reported consumption, and percentage of men/women in the U.S. who drink less than them). To standardize contact across conditions, the intervention-only control group received an email with no alcohol-focused content, thanking them for their participation so far and reminding them of the upcoming follow-up survey. Due to a coding error, we could not determine if/which emails were read.
Survey
Alcohol Consumption.
A modified version of the Daily Drinking Questionnaire (DDQ; Collins et al., 1985) was used to assess typical alcohol consumption for the past 30 days. Using a grid, with columns corresponding to each day of the week, participants reported the number of standard drinks they typically consumed each day of a typical week, as well as the number of hours they were drinking. Quantity reflects the sum of drinks and frequency reflects the total number of drinking days in a typical week. Peak drinks reflect the highest number of drinks reported for a single day within a typical week.
Alcohol Consequences.
The Young Adult Alcohol Consequences Questionnaire (YAACQ; Read et al., 2006) is a 48-item questionnaire that assesses consequences related to alcohol use for the prior 30 days. Number of consequences reported by a participant are summed for a total score. The scale had good internal consistency at all three assessments (α = .90 – .92).
Norms.
Descriptive normative perceptions were assessed by asking participants how many drinks they believe are consumed each day of a typical week by a typical male student and typical female student at the same institution, as well as close friends. For the current study, total drinks across the week were summed to reflect perceived quantity for each referent. A single norms score was created by summing typical male and typical female student reports. Although separate items were used to assess norms for typical male and typical female students to match the feedback delivered as part of the booster, a single variable was created to represent typical student norms because our hypotheses were not gender specific. We chose to use this approach for reasons of parsimony, as well as to keep the number of analyses (and likelihood of a Type I error) low.
Protective Behavioral Strategies.
The Strategies Questionnaire (Sugarman & Carey, 2007) is a 21-item scale assessing behaviors employed to reduce or control drinking and related harms. There are three subscales: selective avoidance, strategies while drinking, and alternatives to drinking. The first two subscales are contingent on drinking, whereas alternatives to drinking reflects engaging in behaviors instead of consuming alcohol. Consistent with recommendations (Braitman et al., 2015), the response scale was modified to reflect exact frequency. Sums for the selective avoidance and strategies while drinking subscales were divided by number of drinking days to reflect drinking-contingent frequency, whereas the sum for alternatives to drinking was not. A total score was calculated by summing each of the adjusted subscale scores (Braitman et al., 2015). This scale had excellent internal consistency at all assessments (α = .93 – .97).
Demographics.
Participants were asked to self-report demographic information such as their age, gender, race/ethnicity, and class standing.
Analysis Approach
The data were analyzed using latent growth modeling within a structural equation modeling framework. Separate models were conducted for each alcohol outcome: quantity, frequency, peak drinks, and alcohol-related problems. Piecewise slopes were used to capture initial reductions to month 1 (i.e., does the booster strengthen intervention effects; slope 1) and maintenance to month 3 (i.e., does the booster extend the effects of the intervention; slope 2). Piecewise growth can isolate and examine an important segment of time and summarize important aspects of change (Duncan, Duncan, & Strycker, 2006), such as in our examination separating immediate change after the booster (slope 1) from longer-term maintenance (slope 2). Condition served as a predictor of each latent variable (latent intercept, slope 1, and slope 2), and was dummy coded across two variables to directly address the aims of the project. To examine the utility of the emailed boosters after completing the evidence-based online CDI (Aim 1), groups were coded as either receiving a booster (1) or not (0). Thus, the booster variable served to compare the two booster conditions to the intervention-only condition. To examine the added value of harm reduction strategies as compared to norms-only emailed boosters (Aim 2), condition was also dummy coded to reflect receiving feedback about PBS (1) or not (0), directly testing Aim 2. Thus, with regard to the factors booster and PBS feedback, the intervention-only control condition was coded as (0, 0), the norms-only booster condition was coded as (1, 0), and the norms-plus-PBS booster condition was coded as (1, 1). Given that descriptive drinking norms were targeted in both booster conditions, and PBS use was targeted in the norms-plus-PBS feedback booster condition, the proximal outcomes of descriptive norms and PBS use were explored for differences in growth trajectories across conditions. Models identical to the main study outcomes were conducted for these proximal outcomes (e.g., piecewise latent growth models, with condition as a predictor dummy coded across two variables). All models were conducted in Mplus (version 8.3; Muthén & Muthén, 1998–2019) using maximum likelihood estimation, and controlling for gender. The model for alcohol-related problems controlled for alcohol quantity as a time-varying covariate (e.g., problems at month 1 controlled for alcohol quantity at month 1). These analyses assume normally distributed outcomes; thus for any outcomes that demonstrated non-normality, competing approaches to model this were all explored (e.g., variable transformation versus specifying a different distribution), with the best-fitting model for the data chosen.
Given prior findings that emailed booster feedback containing PNF and PBS was significantly more effective for select groups (i.e., those lower in PBS use [Braitman & Henson, 2016], legal age drinkers [Braitman & Lau-Barraco, 2018]), we explored potential moderators of booster efficacy. Legal drinking status by age (coded as 1 = age 21–24 [legal], 0 = age 18–20 [underage]) and baseline PBS use (in its original continuous metric) were explored as potential moderators. For each outcome, two additional models were conducted (one for each moderator). The moderator was added as a predictor of each latent factor (latent intercept, slope 1, and slope 2). Two interactions terms were created to capture the interaction with condition, dummy coded across two variables: the interaction between the moderator and booster, and the interaction between moderator and PBS feedback. These interaction terms were also included as predictors of each latent factor. Thus, the outcome at baseline and change over time were predicted by condition, the moderator, and the interaction between the two, controlling for relevant covariates.
Results
At baseline, 13.8% of the sample (n = 73) reported drinking one day in the past 30 days, whereas 70.6% of the sample (n = 373) reported engaging in heavy episodic drinking in the past 30 days (49.6% [n = 262] reported doing this more than once). On average, participants reported consuming 7.7 drinks in a typical week with a peak of 3.8 drinks in one day at baseline, but reduced to 4.9 drinks in a typical week with a peak of 2.6 drinks in one day one month later. See Table 1 for descriptive information for alcohol use and problems for each timepoint by condition, including effect size estimates for within-person change from baseline to the 3-month follow-up by condition.
Table 1.
Descriptive Statistics for Study Variables over Time by Condition
| Baseline | Month 1 | Month 3 | Cohen’s d Base vs. 3 m | ||||
|---|---|---|---|---|---|---|---|
| M | (SD) | M | (SD) | M | (SD) | ||
| Drinks per Typical Week (Quantity) | |||||||
| CDI-only Control | 8.18 | 8.41 | 5.13 | 5.95 | 4.08 | 5.81 | 0.450 |
| Norms-only Booster | 6.72 | 7.14 | 4.65 | 5.81 | 4.15 | 5.71 | 0.325 |
| Norms + PBS Booster | 8.05 | 10.32 | 5.01 | 6.25 | 4.89 | 7.68 | 0.516 |
| Total | 7.69 | 8.71 | 4.94 | 5.98 | 4.36 | 6.43 | |
| Drinking Days per Typical Week (Frequency) | |||||||
| CDI-only Control | 2.24 | 1.25 | 1.58 | 1.40 | 1.39 | 1.61 | 0.444 |
| Norms-only Booster | 1.96 | 1.13 | 1.59 | 1.62 | 1.36 | 1.47 | 0.352 |
| Norms + PBS Booster | 2.23 | 1.32 | 1.59 | 1.37 | 1.44 | 1.39 | 0.543 |
| Total | 2.15 | 1.24 | 1.59 | 1.46 | 1.40 | 1.50 | |
| Highest Drinking Occasion in a typical week (Peak) | |||||||
| CDI-only Control | 4.01 | 2.98 | 2.76 | 2.76 | 1.93 | 2.33 | 0.651 |
| Norms-only Booster | 3.48 | 2.55 | 2.36 | 2.58 | 2.07 | 2.47 | 0.518 |
| Norms + PBS Booster | 3.71 | 3.20 | 2.48 | 2.72 | 2.28 | 2.76 | 0.554 |
| Total | 3.76 | 2.93 | 2.55 | 2.69 | 2.08 | 2.51 | |
| Alcohol-Related Consequences (Problems) | |||||||
| CDI-only Control | 6.21 | 6.59 | 3.42 | 4.99 | 3.27 | 5.68 | 0.430 |
| Norms-only Booster | 6.07 | 7.05 | 3.04 | 4.63 | 2.37 | 3.73 | 0.478 |
| Norms + PBS Booster | 6.28 | 7.17 | 3.58 | 5.35 | 2.67 | 4.11 | 0.576 |
| Total | 6.19 | 6.91 | 3.35 | 4.98 | 2.81 | 4.70 | |
Note. SD = standard deviation, CDI = computer-delivered intervention, Norms = descriptive normative information, PBS = protective behavioral strategies, Base = baseline, 3m = Month 3. Outcomes include total drinks per typical week (quantity), number of drinking days per typical week (frequency), highest number of drinks for a single day in a typical week (peak drinks), and alcohol-related problems. Descriptive information is based on the raw metric, but all analyses (including Cohen’s d) includes a natural log transformation for quantity and problems.
Normality was confirmed for all outcomes except drinking quantity and alcohol-related problems. To address this, the models for quantity and problems were analyzed three ways: with natural log transformations of the outcomes to reduce positive skew, specifying a Poisson distribution, and specifying a negative binomial distribution. Model fit was substantially better (i.e., lower AIC and BIC values) for the log transformed outcomes, so these were chosen as the final models for these outcomes. Boxplots confirmed no extreme values for frequency, quantity (transformed), or alcohol-related problems (transformed). Extreme values were winsorized for peak drinks, PBS, and descriptive norms. A series of chi-square analyses and t-tests revealed that attrition for the follow-up surveys was significantly associated with select baseline characteristics. Those who did not complete the follow-up surveys reported significantly greater weekly quantity at baseline by 1.30 drinks, t(520) = 3.35, p = .001, drinking more frequently by 0.24 days per week, t(520) = 3.35, p = .001, and higher quantities consumed on their peak drinking occasions by 0.87 drinks, t(520) = 3.35, p = .001. In addition, attrition was higher for male participants (44.3%) versus female participants (28.3%), χ2(1) = 12.39, p < .001. Attrition was unrelated to alcohol-related problems, descriptive norms, PBS use, and age. These associations suggest the data are Missing At Random, and controlling for gender combined with the use of full information maximum likelihood estimation should yield unbiased results (Hallgren & Witkiewitz, 2013; Witkiewitz et al., 2014).
Alcohol Consumption
The results of all latent growth models are presented in Table 2. The columns represent each part of the latent growth model (baseline levels of the outcome, slope 1 [growth to month 1], and slope 2 [growth to month 3]). The rows represent the intercept of that latent variable, and then how it was impacted by condition (defined across two variables as booster receipt, and the additional PBS feedback). As seen in Table 2, surprisingly, conditions differed at baseline. For all three consumption outcomes, the booster variable reflects that the intervention-only control condition began the study with significantly higher quantity, frequency, and peak drinks. For both frequency and peak drinks, the norms-plus-PBS feedback booster condition started significantly higher than the norms-only booster condition.
Table 2.
Impact of Condition on Growth Over Time via Piecewise Latent Growth Models
| Baseline | Slope 1 | Slope 2 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| Outcome | B | SE | β | p | B | SE | β | p | B | SE | β | p |
| Drinks per Typical Week (Quantity) | ||||||||||||
| Intercept | 1.77* | 0.06 | 2.096 | <.001 | −0.42* | 0.07 | −0.507 | <.001 | −0.25* | 0.09 | −0.261 | .005 |
| Booster | −0.18* | 0.09 | −0.103 | .038 | −0.04 | 0.11 | −0.023 | .711 | 0.15 | 0.13 | 0.079 | .246 |
| PBS Feedback | 0.09 | 0.09 | 0.048 | .332 | 0.01 | 0.11 | 0.007 | .906 | −0.06 | 0.14 | −0.030 | .655 |
| Drinking Days per Typical Week (Frequency) | ||||||||||||
| Intercept | 2.15* | 0.09 | 1.728 | <.001 | −0.57* | 0.12 | −0.399 | <.001 | −0.17 | 0.13 | −0.122 | .193 |
| Booster | −0.29* | 0.13 | −0.115 | .023 | 0.20 | 0.18 | 0.070 | .248 | −0.03 | 0.20 | −0.012 | .864 |
| PBS Feedback | 0.27* | 0.14 | 0.100 | .048 | −0.26 | 0.19 | −0.086 | .162 | 0.07 | 0.21 | 0.024 | .729 |
| Highest Drinking Occasion in a Typical Week (Peak) | ||||||||||||
| Intercept | 3.63* | 0.21 | 1.257 | <.001 | −0.94* | 0.20 | −0.391 | <.001 | −0.76* | 0.24 | −0.294 | .001 |
| Booster | −0.59* | 0.30 | −0.098 | .048 | −0.19 | 0.30 | −0.038 | .522 | 0.65 | 0.35 | 0.122 | .064 |
| PBS Feedback | 0.20 | 0.31 | 0.032 | .525 | 0.11 | 0.31 | 0.021 | .722 | −0.20 | 0.37 | −0.036 | .581 |
| Alcohol-Related Consequences (Problems) | ||||||||||||
| Intercept | 0.55* | 0.13 | 0.656 | <.001 | −0.02 | 0.13 | −0.018 | .904 | −0.10 | 0.11 | −0.113 | .375 |
| Booster | −0.12 | 0.12 | −0.070 | .330 | −0.03 | 0.13 | −0.014 | .843 | −0.002 | 0.13 | −0.001 | .990 |
| PBS Feedback | 0.11 | 0.13 | 0.062 | .385 | 0.02 | 0.14 | 0.009 | .898 | −0.09 | 0.14 | −0.046 | .527 |
| Descriptive Normative Perceptions (Typical Student) | ||||||||||||
| Intercept | 19.08* | 0.75 | 1.867 | <.001 | −5.34* | 0.78 | −0.581 | <.001 | 1.68* | 0.69 | 0.255 | .015 |
| Booster | −2.03 | 1.08 | −0.096 | .060 | 0.18 | 1.16 | 0.009 | .878 | −1.32 | 1.07 | −0.097 | .220 |
| PBS Feedback | −0.29 | 1.13 | −0.013 | .799 | −0.67 | 1.22 | −0.034 | .582 | 0.28 | 1.15 | 0.020 | .808 |
| Protective Behavioral Strategies Use | ||||||||||||
| Intercept | 58.34* | 3.03 | 1.403 | <.001 | −8.78* | 4.20 | −0.172 | .037 | −10.42* | 4.16 | −0.229 | .021 |
| Booster | 4.31 | 4.35 | 0.050 | .322 | −12.32* | 6.21 | −0.117 | .047 | 5.27 | 6.21 | 0.056 | .396 |
| PBS Feedback | −6.84 | 4.56 | −0.076 | .134 | 19.37* | 6.55 | 0.175 | .003 | −6.76 | 6.54 | −0.069 | .301 |
Note. SE = Standard error, PBS = Protective Behavioral Strategies. Slope 1 represents growth from baseline to 1 month; Slope 2 represents growth from 1 month to 3 months. Quantity represents the natural log transformation of standard drinks reported. Alcohol-related problems was also natural log transformed, and its model controls for quantity. All models controlled for sex. Booster was coded to reflect receipt of the emailed booster feedback (1) or not (0). PBS feedback was coded to reflect receiving feedback about PBS (1) or not (0). Thus, the intervention-only control condition was coded as (0, 0) for booster and PBS feedback, the norms-only feedback condition was coded as (1, 0) for booster and PBS feedback, and the norms-plus-PBS feedback condition was coded as (1, 1) for booster and PBS feedback.
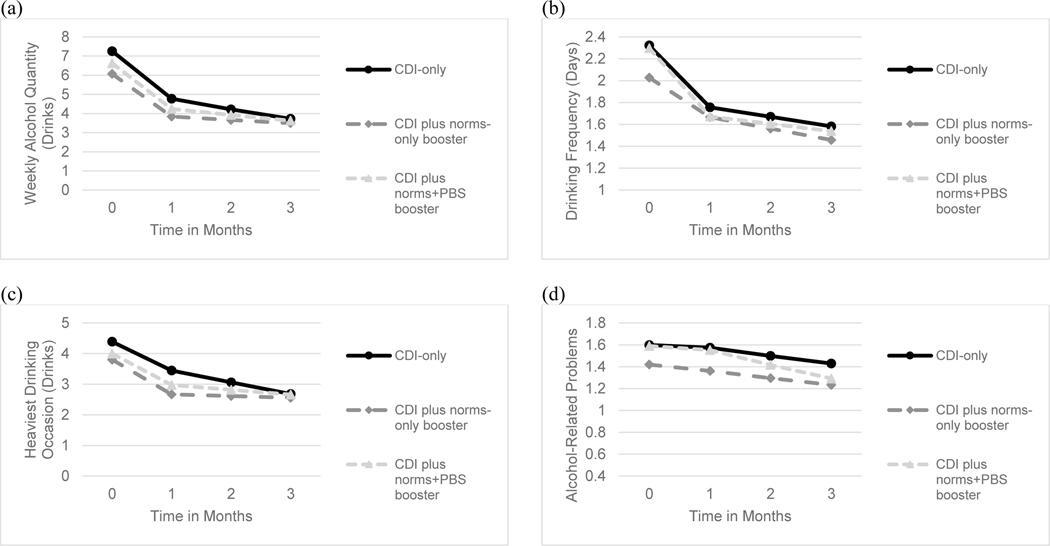
Regarding changes over time, there were significant reductions in consumption (quantity, frequency, peak drinks), with the intercepts for slope 1 being negative and significant for each outcome. Quantity was reduced by 0.42 (or 1.52 standard drinks in the original metric), frequency was reduced by 0.57 days, and peak drinks were reduced by 0.94 standard drinks. In addition, frequency of alcohol use remained relatively low (growth to month 3 being represented with negligible value for slope 2); quantity and peak drinks both reflect continued reductions through month 3 (i.e., significant negative slope 2 intercepts). Quantity was further reduced by 0.25 (or 1.28 additional standard drinks in the original metric, for a total reduction of 2.8 drinks), and peak drinks were reduced by an additional 0.76 standard drinks, for a total reduction of 1.72 drinks. Condition had no significant impact on slopes 1 or 2 in any of the models, indicating no booster effects. These significant reductions over time and the differences at baseline can be seen in Figure 2, panels a-c.
Figure 2. Changes in Alcohol Outcomes over Time by Condition.
Note. CDI = computer-delivered intervention, PBS = protective behavioral strategies. Panel (a) represents quantity (or weekly total drinks), panel (b) represents frequency (or number of drinking days per typical week), panel (c) represents peak drinks (or highest number of drinks on a single day per typical week), and panel (d) represents alcohol-related problems (controlling for quantity).
Alcohol-Related Problems
As seen in Table 2, there were no significant changes in alcohol-related problems over time, after controlling for drinking quantity. Moreover, condition did not significantly impact slopes 1 or 2.
Moderation
Legal drinking status by age and baseline PBS use were both explored as potential moderators of booster efficacy, in separate models for each of the 4 outcomes. In each case, the interaction between condition and the moderator was not a significant predictor of growth over time, meaning the findings were not moderated by legal drinking age or baseline PBS use. Results available upon request.
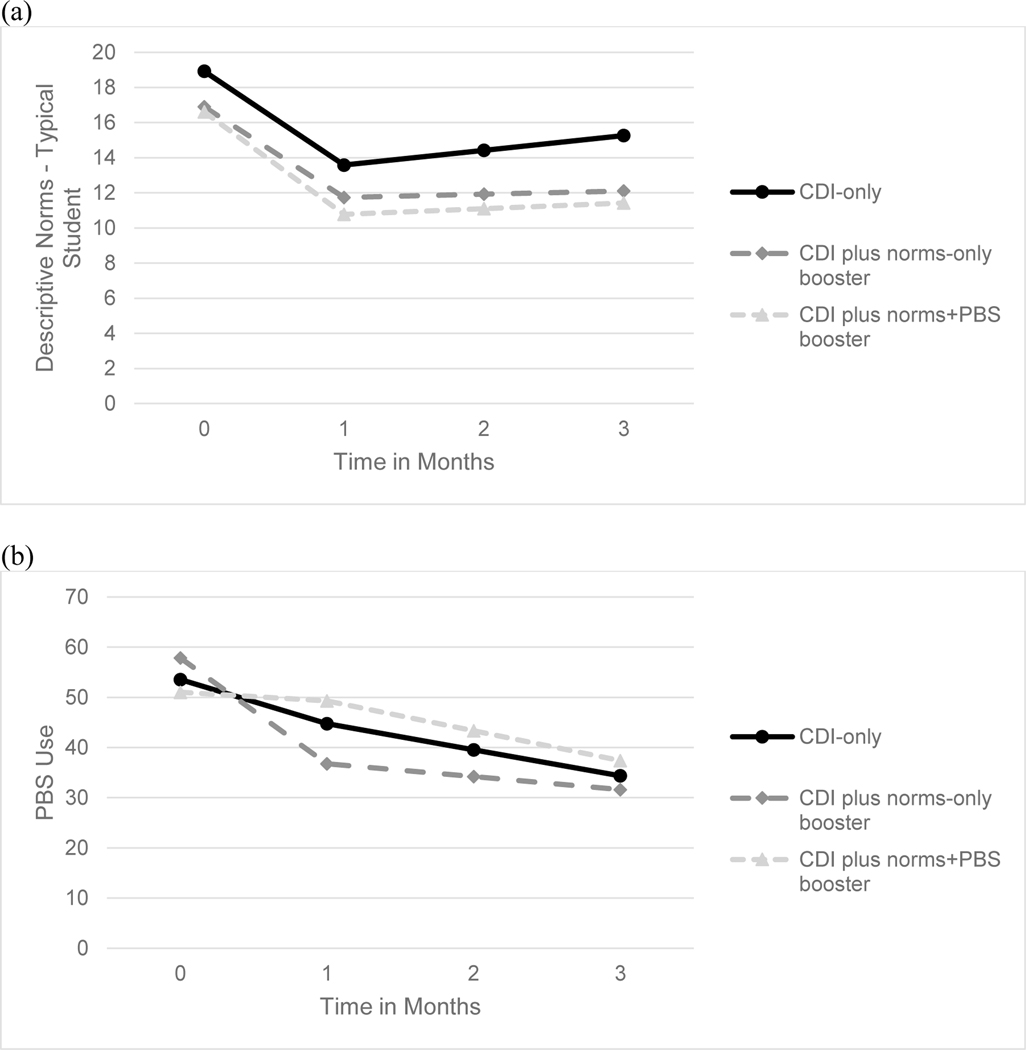
Booster Feedback Content
Descriptive drinking norms were targeted in both booster conditions, and PBS use was targeted in the norms-plus-PBS feedback booster condition. Therefore, the proximal outcomes of descriptive norms and PBS use were explored for differences in growth trajectories across conditions. Models were conducted identical to the main study outcomes (e.g., piecewise latent growth models, with condition as a predictor dummy coded across two variables, controlling for gender). As seen in Table 2, there were significant reductions in perceptions of descriptive norms for the alcohol use of a typical student at the same institution. The intercept for slope 1 was negative and significant, indicating norms were reduced by 5.34 weekly drinks by month 1. However, the intercept for slope 2 was significant and positive, indicating a slight increase (of 1.68 drinks) by month 3. As seen in panel (a) of Figure 3, there was a slight rebound, but not to original pre-intervention levels. These reductions did not differ across condition (i.e., no booster effects). Although the booster explicitly challenged descriptive normative perceptions, the intervention did so as well.
Figure 3. Changes in Descriptive Normative Perceptions and Use of PBS over Time by Condition.
Note. CDI = computer-delivered intervention, PBS = protective behavioral strategies. Panel (a) represents descriptive normative perceptions for a typical student at the same institution (weekly drinking quantity), and panel (b) represents PBS use. Descriptive normative perceptions were targeted in both booster conditions, whereas PBS feedback was contained only in the norms-plus-PBS feedback booster condition.
Significant reductions in PBS use were observed in the control group, as evidenced by a slope 1 being negative and significant in Table 2. Similarly, the significant negative coefficient for booster indicates the norms-only booster group had even stronger reductions in PBS use. However, the group that received the booster with norms-plus-PBS feedback did not initially reduce their PBS use, as evidenced by a significant positive coefficient for PBS feedback. The significant, negative intercept for slope 2 indicated PBS use continued to reduce through month 3. There were no slope 2 differences across condition, so the differences at month 1 across conditions were maintained, as seen in panel (b) of Figure 3.
Discussion
The overall goal of the present study was to test the unique impact of boosters in extending the effects of an empirically-supported online CDI in a sample of college drinkers. Our findings showed that the eCHECKUP TO GO program led to significant reductions in alcohol consumption (i.e., alcohol quantity, frequency, and peak drinks) across all three conditions (i.e., CDI-only, CDI plus a norms-only booster, CDI plus a norms-plus-PBS booster). However, all three conditions produced equivalent drinking reductions at 1- and 3-months after the intervention, suggesting a lack of booster effects on drinking outcomes beyond the impact of the base intervention. Further, there were no changes in alcohol-related problems over time, after controlling for drinking quantity. To inform whether the intervention and follow-up boosters were impactful for particular drinkers, moderator variables were examined. There were no moderation effects for age (under 21 years vs. 21–24 years) or baseline PBS use.
In addition to examining intervention and booster impact on drinking outcomes, we also tested their impact on proximal outcomes specifically targeted in the booster conditions. Feedback on descriptive norms was part of both booster conditions, whereas PBS content was included only in the norms-plus-PBS condition. Our findings showed a significant reduction in participant perceptions of how much their peers drink following the base intervention. This effect, however, was not magnified in the booster conditions, suggesting that the base intervention was successful in reducing perceived norms of peer drinking, leaving less room for change after the norms boosters. It is worth noting that boosters containing normative information appeared to be more impactful after an intervention that did not focus on normative comparisons (i.e., Alcohol 101 Plus; Braitman & Henson, 2016; Braitman & Lau-Barraco, 2018). Taken together, the pattern of findings strongly suggests that PNF, regardless of when it is delivered, is an active ingredient of change. It also may be possible that a greater dose of the booster through repeated exposure over time (e.g., Neighbors et al., 2010) is needed to observe incremental benefit.
The inclusion of PBS feedback in the booster resulted in significant changes in PBS use. Both the CDI-only and CDI plus norms-only booster groups showed erosion of PBS use by 1-month post-intervention and use of PBS continued to decline at the 3-month assessment. This finding may have been a result of reduced consumption and reduced perceived need for PBS. Many strategies are only relevant in heavy use situations (e.g., avoiding risky drinking practices such as drinking games and taking shots). On the other hand, participants receiving the norms-plus-PBS booster continued to implement PBS at 1-month. Although all groups decreased PBS use slightly by 3-months post-intervention, rank was maintained; PBS use by the norms-plus-PBS booster group was still greater than CDI-only and norms-only booster groups. Thus, even with fewer opportunities, the booster group receiving harm reduction feedback continued to use PBS. Greater PBS use has been shown to correspond with less harmful drinking behaviors cross-sectionally and prospectively (Braitman et al., 2015; Martens et al., 2011); however, support for PBS as an underlying mechanism in brief drinking interventions with college drinkers has been mixed (for a review, see Reid & Carey, 2015). Our finding that a norms-plus-PBS booster uniquely impacted use of PBS is encouraging and further investigation into the longer-term implications of regular PBS use may be warranted.
Several potential explanations can be offered for the overall null finding for booster impact on drinking outcomes observed in the present study. It is possible that the base intervention using eCHECKUP TO GO produced an impact on outcomes that is potent enough that it overshadowed any benefits of the boosters. The present study was the first to pair this combination of boosters with eCHECKUP TO GO. In previous studies examining this style of booster (emailed tailored feedback addressing norms and PBS), the base intervention consisted of Alcohol 101 Plus, which has demonstrated lower efficacy than eCHECKUP TO GO (Carey et al., 2016; Hennessy et al., 2019). It may be that the booster was most impactful after a less efficacious intervention (smaller effect size), or that the booster was actually serving as the intervention itself rather than a booster in the previous examinations. A second possible reason for null findings may be related to booster receipt. Given that we could not reliably detect if the feedback emails were read (discussed in more detail below), it is possible students assigned to the booster groups were not actually receiving or viewing their feedback. Another potential explanation of the null booster finding may be related to the timing of the booster. It is possible that the administration of the booster at 2-weeks post-intervention was premature after the relatively efficacious online CDI. Allowing the opportunity for the online CDI to show greater decay before administering the booster could have been critical and should be explored in future research.
A final reason for a lack of booster effects may be due to the timing of the assessments at follow-up. Our findings showed that most alcohol indices show continued reductions (significant, negative intercept) or reduction maintenance (non-significant intercept) at 1- and 3-month post-intervention for all groups, indicating that the intervention is still effective over time. These sustained reductions might indicate that the booster effect is hidden within this time window, and that as the reductions eventually start to wear off, the booster effect could be observed at a later time (perhaps at 6 or 9 months post-intervention). Moreover, more frequent assessment windows (i.e., assessment at weeks 1, 2, 3, 4, or ecological momentary assessments) could have provided greater sensitivity to detecting differences in the rate of change. It is possible the booster group had an accelerated reduction that could not be captured by 1 month. Thus, future work may need to consider more frequent assessment time points proximal to the booster, and assessments at later times post-intervention. These changes in assessment would help to capture any potential differences that may emerge at shorter intervals and to examine potential variability in rates of change between booster conditions.
The present study utilized email as the platform for booster delivery for several reasons related to the nature of the booster content. The email format allowed for large figures that emphasized targeted information (e.g., highlighting normative misperceptions). It also allowed a substantial amount of content to be delivered instantly. One possibility is that boosters sent via email were not viewed by students, or this is not their preferred way to receive information. As such, we explored if student participants were regularly checking their institutional email, and receptive to content delivered via email. Almost all (98.1%) participants reported checking their institutional email at least daily. Moreover, when asked if they would prefer a one-time message with feedback from the study (containing both text and graphics) to be sent via email or text message, participants overwhelmingly endorsed email (88.1%) over text message (11.9%). However, one limitation of email delivery is difficulty in confirming email receipt due to various technical challenges (read receipts can be turned off, tracking images can cause emails to direct to spam/junk, and so forth). Other technology platforms could be used to deliver boosters such as text messaging. While text messaging may restrict the type and amount of content that could be shared, this method may be more flexible and easily accessible. College students send and receive text messages more often than they check their email (Heron, Romano, & Braitman, 2019). Further, rather than providing one large dose of booster at a single point in time, it may be that repeated, timely messaging is more effective. Brief alcohol interventions targeting college drinking delivered via text messaging have shown promise (Bock et al., 2016; Edwards et al., 2020; Mason et al., 2014) and studies have begun to use text message as a booster method for prolonging brief intervention effects (Chavez & Palfai, 2020; Suffoletto et al., 2016; Tahaney & Palfai, 2017). Thus, future work determining optimal booster content should consider text messaging and other potential modes of delivery.
The current findings should be considered in light of several study limitations. First, despite random assignment to study conditions, baseline differences between groups on key drinking variables were observed, with the booster groups reporting significantly lower alcohol use quantity, frequency, and peak drinks to begin with. Between the booster groups, the norms-only booster group reported lower frequency and peak drinks at baseline. Although these differences at baseline were accounted for in the latent growth modeling analyses, the systematic differences between conditions may have led to restriction of range that limited ability to detect significant change. Because of the risk of randomization failure, future research should consider other randomization schemes that impose balance restrictions to help ensure baseline homogeneity across study conditions, including the use of permuted block and covariate adaptive randomization methods (Hedden et al., 2006).
A second limitation is that our study sample, while having strong representation of Black college students (52.5%), lacks representation from other racial and ethnic minority groups, and is predominantly female (71.6%). Future research should replicate our findings with more diverse samples that go beyond a predominately White and Black student sample and include more male participants. Moreover, the stratification approach for randomization and the gender-matched email senders were both biased toward binary gender identities. Although participants could select a third option for this gender identity, they were still stratified as female and received an email from a female sender.
A third limitation was that our study examined typical drinking via the DDQ in which participants estimate their daily drinking behavior in a typical week over the past month. Such an aggregate approach limits fine-grained examinations of drinking behavior change at the daily level. The use of ecological momentary methods should be considered in future research as this approach would be sensitive to assessing how intervention and booster effects develop over time and when effects level off (Voogt et al., 2014). An additional limitation is the relatively high rate of attrition, which may be linked to switching compensation type. The majority of the sample (75.9%) was recruited via the psychology participation pool, receiving course credit as compensation for baseline. They may not have been as motivated by the payments used for the follow-up surveys, contributing to our high attrition rate. Data collection also occurred over the course of a year, which means follow-up survey invitations may have been issued between semesters when students were not keeping up with email, and that seasonal cycles of drinking could have impacted our results. Finally, our follow-up window was restricted to 3 months post-intervention. An extended follow-up interval may reveal when intervention effects disappear and potentially could reveal if and when the booster effect emerges.
The present study examined the unique impact of boosters in improving and extending the impact of a well-supported online intervention, eCHECKUP TO GO, in a sample of college drinkers, finding that the online CDI led to significant reductions in alcohol consumption as well as descriptive normative perceptions across all three study conditions. No differences in growth trajectories were observed across conditions, suggesting a lack of booster effects on drinking outcomes beyond the impact of the base intervention within the 3-month timeframe. Specifically, a booster that delivered PNF within 2 weeks of intervention did not improve upon the impact of the online CDI, which had already successfully reduced normative drinking perceptions. Another study aim was to compare two types of emailed boosters: one focused on providing normative feedback only while the other focused on norms-plus-PBS feedback. Again, there were no differences in growth trajectories of alcohol outcomes. However, individuals receiving the norms-plus-PBS booster implemented greater PBS use at 1-month than the CDI-only and norms-only booster groups. Future research with longer-term follow-ups are needed to determine the significance of maintaining higher levels of PBS even when consumption has been reduced.
Public Health Significance Statement:
This study indicates that an evidence-based online intervention for college drinking may be sufficient to produce substantial reductions in drinking and perceptions of peer drinking up to 3 months later. Emailed feedback after a brief delay (i.e., boosters) had no added benefit for alcohol consumption reductions within this timeframe. However, booster feedback regarding harm reduction strategies may prevent reduction of the use of these strategies.
Author Note
The project described was supported by the National Institute on Alcohol Abuse and Alcoholism award K01 AA023849 (PI: Braitman). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism. All authors declare that they have no conflict of interests. Preliminary findings from the current examination were reported at an invited talk at the Center for Alcohol and Addiction Studies at Brown University.
References
- Barnett NP, Murphy JG, Colby SM, & Monti PM (2007). Efficacy of counselor vs. computer-delivered intervention with mandated college students. Addictive Behaviors, 32(11), 2529–2548. 10.1016/j.addbeh.2007.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bock BC, Barnett NP, Thind H, Rosen R, Walaska K, Traficante R, Foster R, Deutsch C, Fava JL & Scott-Sheldon LA (2016). A text message intervention for alcohol risk reduction among community college students: TMAP. Addictive Behaviors, 63, 107–113. 10.1016/j.addbeh.2016.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, & Carey KB (2003). Descriptive and injunctive norms in college drinking: A meta-analytic integration. Journal of Studies on Alcohol, 64(3), 331–341. 10.15288/jsa.2003.64.331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braitman AL, & Henson JM (2016). Personalized boosters for a computerized intervention targeting college drinking: The influence of protective behavioral strategies. Journal of American College Health, 64(7), 509–519. 10.1080/07448481.2016.1185725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braitman AL, Henson JM, & Carey KB (2015). Clarifying observed relationships between protective behavioral strategies and alcohol outcomes: The importance of response options. Psychology of Addictive Behaviors, 29(2), 455–466. 10.1037/adb0000024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braitman AL, & Lau-Barraco C. (2018). Personalized boosters after a computerized intervention targeting college drinking: A randomized controlled trial. Alcoholism: Clinical and Experimental Research, 42(9), 1735–1747. 10.1111/acer.13815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braitman AL, & Lau-Barraco C. (2020). Descriptive norms but not harm reduction strategies as a mediator of personalized boosters after a computerized college drinking intervention. Alcoholism: Clinical and Experimental Research, 44(1), 284–296. 10.1111/acer.14248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Elliott JC, Bolles JR, & Carey MP (2009). Computer-delivered interventions to reduce college student drinking: A meta-analysis. Addiction, 104(11), 1807–1819. 10.1111/j.1360-0443.2009.02691.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Elliott JC, Garey L, & Carey MP (2012). Face-to-face versus computer-delivered alcohol interventions for college drinkers: A meta-analytic review, 1998 to 2010. Clinical Psychology Review, 32(8), 690–703. 10.1016/j.cpr.2012.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Garey L, Elliott JC, & Carey MP (2016). Alcohol interventions for mandated college students: A meta-analysis review. Journal of Counseling and Clinical Psychology, 84(7), 619–632. 10.1037/a0040275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Walsh JL, Merrill JE, Lust SA, Reid AE, Scott-Sheldon LA, ... & Carey MP (2018). Using e-mail boosters to maintain change after brief alcohol interventions for mandated college students: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 86(9), 787–798. 10.1037/ccp0000339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caudill BD, Luckey B, Crosse SB, Blane HT, Ginexi EM, & Campbell B. (2007). Alcohol risk-reduction skills training in a national fraternity: A randomized intervention trial with longitudinal intent-to-treat analysis. Journal of Studies on Alcohol and Drugs, 68(3), 399–409. 10.15288/jsad.2007.68.399 [DOI] [PubMed] [Google Scholar]
- Chavez K, & Palfai TP (2020). Reducing heavy episodic drinking among college students using a combined web and interactive text messaging intervention. Alcoholism Treatment Quarterly, Advanced online publication. 10.1080/07347324.2020.1784067 [DOI] [Google Scholar]
- Cole HA, Prassel HB, & Carlson CR (2018). A meta-analysis of Computer-Delivered drinking interventions for college students: A comprehensive review of studies from 2010 to 2016. Journal of Studies on Alcohol and Drugs, 79(5), 686–696. 10.15288/jsad.2018.79.686 [DOI] [PubMed] [Google Scholar]
- Collins RL, Parks GA, & Marlatt GA (1985). Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology, 53(2), 189–200. 10.1037/0022-006X.53.2.189 [DOI] [PubMed] [Google Scholar]
- Conway JM, & DiPlacido J. (2015). The indirect effect of alcohol use on GPA in first-semester college students: The mediating role of academic effort. Journal of College Student Retention: Research, Theory & Practice, 17(3), 303–318. 10.1177/1521025115575705 [DOI] [Google Scholar]
- Doumas DM, & Andersen LL (2009). Reducing alcohol use in first-year university students: Evaluation of a web-based personalized feedback program. Journal of College Counseling, 12(1), 18–32. 10.1002/j.2161-1882.2009.tb00037.x [DOI] [Google Scholar]
- Doumas DM, Kane CM, Navarro TB, & Roman J. (2011). Decreasing heavy drinking in first-year students: Evaluation of a web-based personalized feedback program administered during orientation. Journal of College Counseling, 14(1), 5–20. 10.1002/j.2161-1882.2011.tb00060.x [DOI] [Google Scholar]
- Duncan TE, Duncan SC, & Strycker LA (2006). An Introduction to Latent Variable Growth Curve Modeling: Concepts, Issues, and Applications (2nd ed.). Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Edwards SM, Tuliao AP, Kennedy JL, & McChargue DE (2020). Weekend text messages increase protective behavioral strategies and reduce harm among college drinkers. Journal of Technology in Behavioral Science, 5, 395–401. 10.1007/s41347-020-00149-4 [DOI] [Google Scholar]
- Field C, Walters S, Marti CN, Jun J, Foreman M, & Brown C. (2014). A multisite randomized controlled trial of brief intervention to reduce drinking in the trauma care setting: How brief is brief? Annals of Surgery, 259(5), 873–880. 10.1097/SLA.0000000000000339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallgren KA, & Witkiewitz K. (2013). Missing data in alcohol clinical trials: a comparison of methods. Alcoholism: Clinical and Experimental Research, 37(12), 2152–2160. 10.1111/acer.12205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedden SL, Woolson RF, & Malcolm RJ (2006). Randomization in substance abuse clinical trials. Substance Abuse Treatment, Prevention, and Policy, 1(1), 1–17. 10.1186/1747-597X-1-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hennessy EA, Tanner-Smith EE, Mavridis D, & Grant SP (2019). Comparative effectiveness of brief alcohol interventions for college students: Results from a network meta-analysis. Prevention Science, 20(5), 715–740. 10.1007/s11121-018-0960-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heron KE, Romano KA, & Braitman AL (2019). Mobile technology use and mHealth text message preferences: an examination of gender, racial, and ethnic differences among emerging adult college students. mHealth, 5, 2–2. 10.21037/mhealth.2019.01.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson R, Zha W, & Smyth D. (2017). Magnitude and trends in heavy episodic drinking, alcohol-impaired driving, and alcohol-related mortality and overdose hospitalizations among emerging adults of college ages 18–24 in the United States, 1998–2014. Journal of Studies on Alcohol and Drugs, 78(4), 540–548. 10.15288/jsad.2017.78.540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hustad JT, Barnett NP, Borsari B, & Jackson KM (2010). Web-based alcohol prevention for incoming college students: A randomized controlled trial. Addictive Behaviors, 35(3), 183–189. 10.1016/j.addbeh.2009.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kite BA, Pearson MR, & Henson JM (2013). The assessment of protective behavioral strategies: Comparing the absolute frequency and contingent frequency response scales. Psychology of Addictive Behaviors, 27(4), 1010–1018. 10.1037/a0031366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linowski SA, DiFulvio GT, Fedorchak D, & Puleo E. (2016). Effectiveness of an electronic booster session delivered to mandated students. International Quarterly of Community Health Education, 36(2), 123–129. 10.1177/0272684X16628726 [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Woolard RE, Nirenberg TD, Minugh AP, Becker B, Clifford PR, ... & Gogineni A. (2001). Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. Journal of Studies on Alcohol, 62(6), 806–816. 10.15288/jsa.2001.62.806 [DOI] [PubMed] [Google Scholar]
- Martens MP, Martin JL, Littlefield AK, Murphy JG, & Cimini MD (2011). Changes in protective behavioral strategies and alcohol use among college students. Drug and Alcohol Dependence, 118(2–3), 504–507. 10.1016/j.drugalcdep.2011.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Taylor KK, Damann KM, Page JC, Mowry ES, & Cimini MD (2004). Protective behavioral strategies when drinking alcohol and their relationship to negative alcohol-related consequences in college students. Psychology of Addictive Behaviors, 18(4), 390–393. 10.1037/0893-164X.18.4.390 [DOI] [PubMed] [Google Scholar]
- Mason M, Benotsch EG, Way T, Kim H, & Snipes D. (2014). Text messaging to increase readiness to change alcohol use in college student. Journal of Primary Prevention, 35(1), 47–52. 10.1007/s10935-013-0329-9 [DOI] [PubMed] [Google Scholar]
- Matthews DB, & Miller WR (1979). Estimating blood alcohol concentration: Two computer programs and their applications in therapy and research. Addictive Behaviors, 4(1), 55–60. 10.1016/0306-4603(79)90021-2 [DOI] [PubMed] [Google Scholar]
- Mello MJ, Nirenberg TD, Longabaugh R, Woolard R, Minugh A, Becker B, ... & Stein L. (2005). Emergency department brief motivational interventions for alcohol with motor vehicle crash patients. Annals of Emergency Medicine, 45(6), 620–625. 10.1016/j.annemergmed.2005.01.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendoza NS, Walitzer KS, & Connors GJ (2012). Use of treatment strategies in a moderated drinking program for women. Addictive Behaviors, 37(9), 1054–1057. 10.1016/j.addbeh.2012.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meshesha LZ, Soltis KE, Wise EA, Rohsenow DJ, Witkiewitz K, & Murphy JG (2020). Pilot trial investigating a brief behavioral economic intervention as an adjunctive treatment for alcohol use disorder. Journal of Substance Abuse Treatment, 113, 108002. 10.1016/j.jsat.2020.108002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monti PM, Barnett NP, Colby SM, Gwaltney CJ, Spirito A, Rohsenow DJ, & Woolard R. (2007). Motivational interviewing versus feedback only in emergency care for young adult problem drinking. Addiction, 102(8), 1234–1243. 10.1111/j.1360-0443.2007.01878.x [DOI] [PubMed] [Google Scholar]
- Moreira MT, Smith LA, & Foxcroft D. (2009). Social norms interventions to reduce alcohol misuse in university or college students. Cochrane Database of Systematic Reviews, 2009(3), CD006748. 10.1002/14651858.CD006748.pub2 [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998-2019). Mplus User’s Guide. Eighth Edition. Muthén & Muthén [Google Scholar]
- Neighbors C, Lewis MA, Atkins DC, Jensen MM, Walter T, Fossos N, Lee CM, & Larimer ME (2010). Efficacy of web-based personalized normative feedback: A two-year randomized controlled trial. Journal of Consulting and Clinical Psychology, 78(6), 898–911. 10.1037/a0020766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Terry-McElrath YM, Evans-Polce RJ, & Schulenberg JE (2020). Negative alcohol-related consequences experienced by young adults in the past 12 months: Differences by college attendance, living situation, binge drinking, and sex. Addictive Behaviors, 105, 106320. 10.1016/j.addbeh.2020.106320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince MA, Carey KB, & Maisto SA (2013). Protective behavioral strategies for reducing alcohol involvement: A review of the methodological issues. Addictive Behaviors, 38(7), 2343–2351. 10.1016/j.addbeh.2013.03.010 [DOI] [PubMed] [Google Scholar]
- Read JP, Kahler CW, Strong DR, & Colder CR (2006). Development and preliminary validation of the young adult alcohol consequences questionnaire. Journal of Studies on Alcohol, 67(1), 169–177. 10.15288/jsa.2006.67.169 [DOI] [PubMed] [Google Scholar]
- Reid AE, & Carey KB (2015). Interventions to reduce college student drinking: State of the evidence for mechanisms of behavior change. Clinical Psychology Review, 40, 213–224. 10.1016/j.cpr.2015.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA (2020). 2019 National Survey on Drug Use and Health (NSDUH). In Table 6.21B Types of Illicit Drug, Tobacco Product, and Alcohol Use in Past Month among Persons Aged 18 to 22, by College Enrollment Status and Gender: Percentages, 2018 and 2019. Available at: https://www.samhsa.gov/data/report/2019-nsduh-detailed-tables. [Google Scholar]
- Samson JE, & Tanner-Smith EE (2015). Single-session alcohol interventions for heavy drinking college students: A systematic review and meta-analysis. Journal of Studies on Alcohol and Drugs, 76(4), 530–543. 10.15288/jsad.2015.76.530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- San Diego State University Research Foundation. (2018). eCHECKUP TO GO [Online program]. San Diego State University Research Foundation. http://www.echeckuptogo.com/programs/alcohol [Google Scholar]
- Steiner J, Woodall WG, & Yeagley JA (2005). The e-CHUG: A randomized, controlled study of a web-based binge drinking intervention with college freshman. Paper presented at the Society for Prevention Research, Washington, DC. [Google Scholar]
- Suffoletto B, Merrill JE, Chung T, Kristan J, Vanek M, & Clark DB (2016). A text message program as a booster to in-person brief interventions for mandated college students to prevent weekend binge drinking. Journal of American College Health, 64(6), 481–489. 10.1080/07448481.2016.1185107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugarman DE, & Carey KB (2007). The relationship between drinking control strategies and college student alcohol use. Psychology of Addictive Behaviors, 21(3), 338. 10.1037/0893-164X.21.3.338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tahaney KD, & Palfai TP (2017). Text messaging as an adjunct to a web-based intervention for college student alcohol use: A preliminary study. Addictive Behaviors, 73, 63–66. 10.1016/j.addbeh.2017.04.018 [DOI] [PubMed] [Google Scholar]
- Voogt C, Kuntsche E, Kleinjan M, Poelen E, & Engels R. (2014). Using ecological momentary assessment to test the effectiveness of a web-based brief alcohol intervention over time among heavy-drinking students: Randomized controlled trial. Journal of Medical Internet Research, 16, e5. 10.2196/jmir.2817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters ST, Vader AM, & Harris TR (2007). A controlled trial of web-based feedback for heavy drinking college students. Prevention Science, 8(1), 83–88. 10.1007/s11121-006-0059-9 [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Falk DE, Kranzler HR, Litten RZ, Hallgren KA, O’Malley SS, & Anton RF (2014). Methods to analyze treatment effects in the presence of missing data for a continuous heavy drinking outcome measure when participants drop out from treatment in alcohol clinical trials. Alcoholism: Clinical and Experimental Research, 38(11), 2826–2834. 10.1111/acer.12543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood MD, Fairlie AM, Fernandez AC, Borsari B, Capone C, Laforge R, & Carmona-Barros R. (2010). Brief motivational and parent interventions for college students: A randomized factorial study. Journal of Consulting and Clinical Psychology, 78(3), 349. 10.1037/a0019166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurdak M, Kuntsche E, Kraus L, & Wolstein J. (2016). Effectiveness of a brief intervention with and without booster session for adolescents hospitalized due to alcohol intoxication. Journal of Substance Use, 21(1), 72–77. 10.3109/14659891.2014.951415 [DOI] [Google Scholar]