Abstract
Introduction:
In the United States, fall-related emergency department (ED) visits among older adults (age 65 and older) have increased over the past decade. Studies document seasonal variation in fall injuries in other countries, while research in the United States is inconclusive. The objectives of this study were to examine seasonal variation in older adult fall-related ED visits and explore if seasonal variation differs by the location of the fall (indoors vs. outdoors), age group, and sex of the faller.
Methods:
Fall-related ED visit data from the National Electronic Injury Surveillance System-All Injury Program were analyzed by season of the ED visit, location of the fall, and demographics for adults aged 65 years and older.
Results:
Total fall-related ED visits were higher during winter compared with other seasons. This seasonal variation was found only for falls occurring outdoors. Among outdoor falls, the variation was found among males and adults aged 65 to 74 years. The percentages of visits for weather-related outdoor falls were also higher among males and the 65–74 year age group.
Conclusions:
In 2015, there was a seasonal variation in fall-related ED visits in the United States. Weather-related slips and trips in winter may partially account for the seasonal variation.
Practical Implications:
These results can inform healthcare providers about the importance of screening all older adults for fall risk and help to identify specific patients at increased risk during winter. They may encourage community-based organizations serving older adults to increase fall prevention messaging during winter.
Keywords: Older adults, Elderly, Falls, Winter, Indoor, Outdoor
1. Introduction
Fall-related emergency department (ED) visits among older adults (65 years and older) in the United States increased from 2.2 million in 2009 to 3.0 million in 2018 (Centers for Disease Control and Prevention [CDC], 2003). Each month an estimated 250,000 older adults were seen in an ED for a fall in 2018 (CDC, 2003). Studies in other countries found that a higher number of fall-related ED visits (Al-Azzani & Mak, 2016; Beynon, Wyke, Jarman, Robinson, Mason, & Murphy, 2011; Jung et al., 2018; Wareham et al., 2003) and fractures (Bulajic-Kopjar, 2000; Grønskag, Forsmo, Romundstad, Langhammer, & Schei, 2010) occur in the winter months when compared with other seasons. Findings on the seasonal variation of falls and related injuries in the United States are inconsistent. One study found that between 1986 and 1990, a higher rate of fall-related fractures was observed during winter compared with other seasons (Bischoff-Ferrari, Orav, Barrett, & Baron, 2007). In another study, there were no noted seasonal differences in the rate of fall-related ED visits during 2001–2002 (Stevens, Thomas, & Sogolow, 2007). While these outcomes differ (i.e., fall-related fracture and fall-related ED visit), there were no consistent findings of seasonal variation in fall-related injuries.
Past studies that examined winter falls focused on those that occurred outdoors due to weather-related factors (e.g., slips or trips on ice, snow, or freezing rain) (Bobb et al., 2017; Dey, Hicks, Benoit, & Tokars, 2010; Gevitz, Madera, Newbern, Lojo, & Johnson, 2017). These studies found that there was a higher risk for fall injuries during (Dey et al., 2010; Gevitz et al., 2017) and immediately after periods of snowfall or freezing rain (Bobb et al., 2017).
Irrespective of season, older adult falls and fall injuries occur more often indoors than outdoors (Boye et al., 2014; Leavy et al., 2013; Moreland, Kakara, Haddad, Shakya, & Bergen, 2020; Schiller, Kramarow, & Dey, 2007). Studies that find seasonal variation in falls or fall injuries often propose that, in addition to outdoor weather-related events, prolonged periods of time spent indoors during winter could be a cause for increased falls (Campbell, Spears, Borrie, & Fitzgerald, 1988; Jacobsen, Sargent, Atkinson, O’Fallon, & Melton, 1995; Leavy et al., 2013; Qian, Chau, Kwan, Lou, & Leung, 2019; Stevens et al., 2007; Wareham et al., 2003). A potential consequence of staying indoors for extended periods of time that could increase fall risk include low physical activity, which leads to diminished muscle strength and bone loss (Jacobsen et al., 1995; Leavy et al., 2013; Mondor, Charland, Verma, & Buckeridge, 2015; Qian et al., 2019; Stevens et al., 2007; Wareham et al., 2003). Other consequences may include seasonal affective disorder, a form of depression due to low light and isolation (Jacobsen et al., 1995; O’Hare, O’Sullivan, Flood, & Kenny, 2016), tripping over objects inside homes and disturbance in circadian rhythms due to low natural light in winter (Johansen, Boulton, & Neuburger, 2016; Vikman, Nordlund, Näslund, & Nyberg, 2011). However, there is limited research examining seasonal variation by location of fall to support this discussion. Understanding seasonal variation by location could help us identify the factors driving seasonal variation, if any.
The objectives of this study were to examine seasonal variation in ED visits among adults age 65 and older and to explore if seasonal variation differs by the location (indoors vs. outdoors) of the fall, and the age and sex of the faller.
2. Methods
Data and narratives from the 2015 National Electronic Injury Surveillance System-All Injury Program (NEISS-AIP) were reviewed to determine the season and location of nonfatal falls that led to an ED visit among adults age 65 and older (NEISS, 2021). The NEISS-AIP is a nationally representative data system operated by the United States Consumer Product Safety Commission. It includes data from a sample of about 66 of 100 NEISS-participating hospitals in U.S. states and territories. NEISS-AIP captures data from a patient’s initial ED visit for an injury. The data are then weighted to represent the U.S. population using the inverse probability of hospital selection in each stratum and adjusted for non-response (Schroeder & Ault, 2001). For each ED visit, the date of treatment, age, sex, primary diagnosis, precipitating cause of injury, intent of injury, and a 2-line free-form narrative describing the circumstance of injury are abstracted from the medical record. Only ED visits made by adults over the age of 65, and whose precipitating cause of injury was an unintentional fall, were included in this analysis making the initial sample size 38,654 ED visits. Date of treatment was used to define the season in which the fall occurred. Seasons were defined as spring (March – May), summer (June – August), autumn (September – November), and winter (December – February).
The narratives were used to create three additional variables: place of residence, fall location, and weather-related fall. This was done by dividing the 38,654 ED records into four groups. One of four researchers then reviewed each group. A codebook was developed (Appendix A) by reading 100 narratives and then updated for every 2,000 narratives read. A second researcher reviewed 10% of all narratives and the four researchers discussed coding discrepancies until they reached a consensus. Previous narratives were recoded based on changes made to the codebook.
Place of residence –
If a narrative indicated that the fall occurred in a residential facility such as a nursing home, assisted living facility, or another type of facility, the person was considered non-community dwelling. If the narrative did not mention these keywords, the person was assumed to be community dwelling. There were nine cases where a fall occurred in a prison. These nine were excluded from the analysis reducing the sample size to 38,645.
Fall location –
The location of the fall was then assessed for older adults who resided in the community (n = 34,336). Location was coded as either indoor (n = 14,131) or outdoor (n = 6,485). Cases where the narratives did not have sufficient information to identify indoor or outdoor location were coded as unknown (n = 13,720) (e.g., falls on stairs without any additional information were difficult to determine if indoor or outdoor). Events classified as unknown were excluded from location-based analyses. Location was not analyzed among non-community dwelling adults given the small number of events that occurred outdoors (n = 51).
Weather-related fall –
Weather was classified for ED visits among community dwelling adults who sustained a fall outdoors. The ED visit for a fall was coded as potentially weather related (n = 1,092) when a term indicative of weather (e.g., rain, snow, ice) was mentioned in the narrative or non-weather related (n = 5,393) in their absence. Additional information on how narratives were coded for place of residence, fall location, and weather are included in the Appendix A.
Percentages and 95% confidence intervals were calculated for season in which the fall-related ED visit occurred, by place of residence, sex, and age group. For community-dwelling older adults, percentages were calculated for fall-related ED visits by location (indoor vs. outdoor), sex, and age group. For weather-related fall injuries, percentages and 95% confidence intervals were calculated for each sub-group of season, sex, and age. Percentages for each sub-group used the number of fall injuries sustained outdoors for that sub-group as the denominator. All analyses were weighted to be representative of the 2015 U.S. population. The conservative method of non-overlapping confidence intervals was used to estimate significant differences between categories. All analyses were performed using Survey Procedures in SAS version 9.4 (SAS Institute, Inc., Cary, NC, USA).
3. Results
The 38,645 narratives represented 3.04 million fall-related ED visits among older adults in 2015. Around 65% of these visits were made by females (data not shown). Fall-related ED visits were more common in winter (26.2%; 95%CI = 25.7, 26.8) than in spring (24.8%, 95%CI = 24.3, 25.4), summer (24.7%, 95%CI = 24.1, 25.2), and autumn (24.3%, 95%CI = 23.7, 24.8) (Table 1). When examined by place of residence, both community and non-community dwelling older adults had more ED visits due to a fall during winter. However, a statistically significant difference was found only among the community dwelling adults. Among community-dwelling males, the percentage of fall-related ED visits was highest in winter (27.3%; 95%CI = 26.3, 28.4) compared with spring (24.8%; 95% CI = 23.9, 25.8), summer (24.3%; 95%CI = 23.3, 25.2), and autumn (23.6%; 95%CI = 22.6, 24.5).
Table 1.
Characteristics of older adults with a fall-related emergency department visit by season and place of residence – National Electronic Injury Surveillance System – All Injury Program, 2015.
| Characteristic | Total | Spring (March-May) |
Summer (June-August) |
Autumn (September-November) |
Winter (December-February) |
||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | 95%CI | % | 95%CI | % | 95%CI | % | 95%CI | |
| Total | 38,645 | 24.8 | (24.3, 25.4) | 24.7 | (24.1, 25.2) | 24.3 | (23.7, 24.8) | 26.2 | (25.7, 26.8) |
| Community Dwelling Older Adults | |||||||||
| Total | 34,336 | 24.8 | (24.3, 25.4) | 24.8 | (24.3, 25.4) | 24.2 | (23.6, 24.7) | 26.2 | (25.6, 26.8) |
| Sex | |||||||||
| Male | 12,083 | 24.8 | (23.9, 25.8) | 24.3 | (23.3, 25.2) | 23.6 | (22.6, 24.5) | 27.3 | (26.3, 28.4) |
| Female | 22,253 | 24.8 | (24.1, 25.6) | 25.0 | (24.3, 25.8) | 24.5 | (23.8, 25.2) | 25.6 | (24.9, 26.4) |
| Age Group | |||||||||
| 65–74 | 12,591 | 25.0 | (24.0, 25.9) | 25.1 | (24.1, 26.1) | 23.4 | (22.5, 24.4) | 26.5 | (25.5, 27.5) |
| 75–84 | 11,716 | 25.6 | (24.6, 26.6) | 24.0 | (23.0, 24.9) | 24.3 | (23.3, 25.3) | 26.2 | (25.1, 27.2) |
| 85+ | 10,029 | 23.8 | (22.8, 24.8) | 25.3 | (24.2, 26.4) | 24.9 | (23.8, 26.0) | 26.0 | (24.9, 27.1) |
| Non-Community Dwelling Older Adults | |||||||||
| Total | 4309 | 24.7 | (23.0, 26.3) | 24.0 | (22.4, 25.7) | 25.1 | (23.4, 26.8) | 26.2 | (24.5, 27.9) |
| Sex | |||||||||
| Male | 1271 | 25.2 | (22.1, 28.3) | 26.9 | (23.7, 30.1) | 20.5 | (17.6, 23.4) | 27.5 | (24.2, 30.7) |
| Female | 3038 | 24.5 | (22.5, 26.4) | 22.9 | (21.0, 24.8) | 26.9 | (24.9, 28.9) | 25.7 | (23.7, 27.7) |
| Age Group | |||||||||
| 65–74 | 530 | 25.6 | (20.7, 30.4) | 20.7 | (16.3, 25.1) | 24.3 | (19.6, 29.0) | 29.5 | (24.2, 34.7) |
| 75–84 | 1184 | 25.9 | (22.7, 29.1) | 24.4 | (21.2, 27.6) | 25.9 | (22.7, 29.2) | 23.8 | (20.5, 27.0) |
| 85+ | 2595 | 24.0 | (21.9, 26.1) | 24.4 | (22.3, 26.5) | 24.9 | (22.8, 27.0) | 26.7 | (24.5, 28.9) |
n - Unweighted sample size.
% - Weighted percent.
95%CI - 95% Confidence interval.
Fall injuries were two times as common indoors (n = 14,131) as outdoors (n = 6,485) (Table 2). However, a higher percent of ED visits occurred due to a fall sustained outdoors during winter (29.8%, 95%CI = 28.4, 31.2) compared with spring (25.8%, 95%CI = 24.5, 27.1), summer (22.2%, 95%CI = 20.9, 23.4), and autumn (22.2%, 95%CI = 20.9, 23.5). Males had a higher percentage of outdoor injuries during winter (31.4%, 95%CI = 29.2, 33.6) compared with spring (26.4%, 95%CI = 24.3, 28.4), summer (20.7%, 95%CI = 18.8, 22.6), and autumn (21.5%, 95%CI = 19.6, 23.4). Older adults in the age group 65 to 74 had more ED visits due to an outdoor fall in winter compared with other seasons (Table 2).
Table 2.
Characteristics of community dwelling older adults who sought emergency department care for a fall by season and indoor/outdoor location – National Electronic Injury Surveillance System – All Injury Program, 2015.
| Characteristic | Total | Spring (March-May) |
Summer (June-August) |
Autumn (September-November) |
Winter (December-February) |
||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | 95%CI | % | 95%CI | % | 95%CI | % | 95%CI | |
| Fall Injury Occurred Indoors | |||||||||
| Total | 14,131 | 24.4 | (23.6, 25.3) | 25.4 | (24.5, 26.3) | 24.6 | (23.7, 25.5) | 25.6 | (24.7, 26.5) |
| Sex | |||||||||
| Male | 4392 | 23.8 | (22.2, 25.4) | 25.5 | (23.8, 27.1) | 24.1 | (22.5, 25.7) | 26.7 | (25.0, 28.3) |
| Female | 9739 | 24.7 | (23.7, 25.8) | 25.3 | (24.2, 26.4) | 24.8 | (23.7, 25.9) | 25.1 | (24.0, 26.2) |
| Age group | |||||||||
| 65–74 | 4334 | 25.0 | (23.4, 26.6) | 25.7 | (24.1, 27.3) | 24.5 | (22.9, 26.2) | 24.8 | (23.1, 26.4) |
| 75–84 | 4880 | 25.3 | (23.8, 26.8) | 24.6 | (23.1, 26.1) | 24.3 | (22.8, 25.8) | 25.8 | (24.2, 27.3) |
| 85+ | 4917 | 23.0 | (21.6, 24.5) | 25.9 | (24.3, 27.4) | 24.9 | (23.3, 26.4) | 26.2 | (24.6, 27.8) |
| Fall Injury Occurred Outdoors | |||||||||
| Total | 6485 | 25.8 | (24.5, 27.1) | 22.2 | (20.9, 23.4) | 22.2 | (20.9, 23.5) | 29.8 | (28.4, 31.2) |
| Sex | |||||||||
| Male | 2794 | 26.4 | (24.3, 28.4) | 20.7 | (18.8, 22.6) | 21.5 | (19.6, 23.4) | 31.4 | (29.2, 33.6) |
| Female | 3691 | 25.4 | (23.6, 27.1) | 23.2 | (21.5, 24.9) | 22.7 | (21.0, 24.4) | 28.7 | (26.9, 30.5) |
| Age group | |||||||||
| 65–74 | 3001 | 26.1 | (24.1, 28.1) | 21.7 | (19.9, 23.6) | 20.8 | (18.9, 22.6) | 31.4 | (29.3, 33.5) |
| 75–84 | 2253 | 26.1 | (23.8, 28.3) | 22.4 | (20.3, 24.6) | 22.5 | (20.3, 24.6) | 29.0 | (26.7, 31.3) |
| 85+ | 1231 | 24.5 | (21.6, 27.5) | 22.7 | (19.8, 25.6) | 25.2 | (22.1, 28.2) | 27.6 | (24.5, 30.7) |
n - Unweighted sample size.
% - Weighted percent.
95%CI - 95% Confidence interval.
Out of the 6,485 fall injuries that occurred outdoors, 1,092 were reported to be weather related. Around 97% of all weather-related injuries were attributed to slips or trips on ice or snow (data not shown). The remainder were due to rain. Fig. 1 shows that, out of all fall injuries sustained outdoors, 34.4% in the winter were weather related compared with 14.5% in spring, 0.9% in summer, and 1.5% in autumn. Out of all fall injuries sustained outdoors by males, a higher percentage (17.2%, 95%CI = 15.5, 18.9) were weather related than that for females (12.7%, 95%CI = 11.4, 13.9). Out of all fall injuries sustained outdoors by 65–74 year olds (18.9%, 95%CI = 17.2, 20.6), a higher percentage were weather related than for those who were 75–84 (11.6%, 95%CI = 10.1, 13.1) and 85 years and above (9.8%, 95%CI = 7.8, 11.7).
Fig. 1.
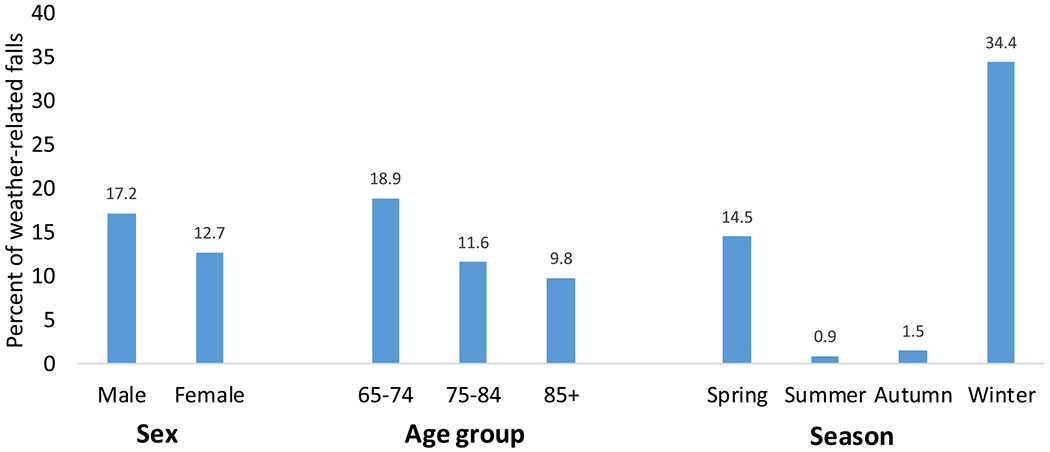
Characteristics of community dwelling older adults who sought emergency department care for weather-related falls - National Electronic Injury Surveillance System – All Injury Program, 2015.
Sample for this figure includes only those older adults who made an ED visit due to a fall sustained outdoors (n = 6,485).
Percent for each sub-group was calculated with the denominator as the number of older adults who made an ED visit due to a fall sustained outdoors in that sub-group. E.g., Out of all the fall injuries sustained by males in the outdoors, 17.2% were weather-related and 82.8% (not shown) were not weather-related.
4. Discussion
In 2015, there was seasonal variation in fall-related ED visits among older Americans, with a higher percentage of visits occurring in winter compared with any other season. By location, this seasonal variation was found only among falls sustained outdoors. That is, the percentage of ED visits due to falls that occurred outdoors was higher in winter than other seasons.
Previously, the two studies that investigated seasonal variation in the United States found conflicting results (Bischoff-Ferrari et al., 2007; Stevens et al., 2007). Bischoff-Ferrari et al. found that between 1986 and 1990, there was a higher incidence of all types of fractures during winter. Stevens et al. studied fall-related ED visits using 2001–2002 NEISS data. Though they found that the rates of fall-related ED visits were higher in winter, no statistical difference was found between the seasons. From 2001 to 2015, the age-adjusted rate of fall-related ED visits in NEISS-AIP increased by 37% (CDC, 2003). This relative increase in the number of fall-related ED visits could have powered the current study sufficiently to identify a statistical difference between the percent of fall-related ED visits in winter and other seasons.
The percentage of ED visits made due to a fall injury that was sustained outdoors, was higher in winter compared with other seasons. This may be due to adverse weather conditions. In the current study, about one-third of outdoor fall-related ED visits in winter were due to slips or trips on ice, in snow, or rain. No seasonal variation in ED visits from indoor falls was observed suggesting that prolonged periods of time spent indoors during winter may not be a contributing factor for seasonal variation. This is in line with a 2013 Swedish study that examined seasonal variation by location of falls. The study found that fractures sustained indoors tended to peak in February but the findings were not statistically significant (Leavy et al., 2013).
Among ED visits made due to an outdoor fall, seasonal variation was found in the 65–74 year age group with the percentage of such ED visits being higher in winter compared with other seasons. The percentage of outdoor falls related to a weather event like a slip or a trip on ice, in snow, or rain was also higher in this age group compared with older age groups. While we could not measure the amount of time an older adult spent indoors or outdoors, it might be that 65–74 year olds are more likely to go outside during adverse weather. The percentage of older adults in the labor force increased drastically in the past few years (Centers for Disease Control and Prevention, 2015). The largest increase occurred in the younger age groups (Kromer & Howard, 2013). Twice as many 65–74 year olds were in the labor force in 2016, compared with those in the 75–84 year age group (Roberts, Ogunwole, Blakeslee, & Rabe, 2018). In addition, this subgroup of older adults tends to be more physically active than adults 75 and older (Keadle, McKinnon, Graubard, & Troiano, 2016). Therefore, they may have more exposure to weather-related risk factors whether it may be getting to and from work, shoveling a driveway, going out to purchase groceries, or other activities.
Similar to the 65–74 year age group, males had a higher percent of ED visits from outdoor falls in winter than in other seasons. Such a difference was not found among females. Additionally, a higher percentage of males sustained a fall-related injury during a weather-related event compared with females. In relation to this finding, studies have found mixed results. Some studies found that older males were more likely to fall and have fractures in winter and on snowy and icy surfaces than older females (Bischoff-Ferrari et al., 2007; Duckham et al., 2013), others found no differences between the sexes (Leavy et al., 2013; Morency, Voyer, Burrows, & Goudreau, 2012), and one found females had a higher percentage of fall-related fractures on ice or snow when compared with males (Al-Azzani & Mak, 2016).
Our study has at least six limitations. First, state or region variables were not available in the NEISS-AIP data so we could not examine seasonal variation by geographical weather patterns. Second, fall location was unknown for over a third (38.5%) of the sample. There was no seasonal variation observed in this subset of ED visits. No seasonal variation was found in any of the three age-groups or among the sexes (Appendix B). Third, only narratives that mentioned a weather-related event in the notes were considered weather related. Therefore, weather-related injuries may have been underestimated. Fourth, these data do not include all falls but only those that warranted ED care. Fifth, the amount of time an older adult spent indoors or outdoors could not be measured. Sixth, this analysis being descriptive in nature, used non-overlapping confidence intervals to describe differences. A formal hypothesis test could have identified additional differences that would have been overlooked by comparing confidence intervals.
5. Conclusion
In 2015, over 3 million older adults went to the ED for a fall injury. This study found that there was seasonal variation with 26.2% of these ED visits occurring in winter. This may be in part due to adverse weather in winter such as ice, snow and rain that could increase fall risk. Interventions to reduce the risk posed by weather such as removing snow, treating sidewalks with salt or sand (Al-Azzani & Mak, 2016; Morency et al., 2012; Stansbury et al., 1995), promoting work closures or delayed openings during bad weather (Gevitz et al., 2017), utilizing weather alerts as a public health tool (Mondor et al., 2015), and encouraging the use of gait stabilizing footwear (McKiernan, 2005) have been proposed by others. Except for the use of gait stabilizing footwear (McKiernan, 2005), these interventions have not been evaluated for fall prevention.
6. Practical Implications
While it is important to consider potential risk factors such as adverse weather, fall risk increases as the number of risk factors increase (Ambrose, Paul, & Hausdorff, 2013). Therefore, it is important to identify all modifiable fall risk factors such as impaired vision, medications that increase fall risk, and gait and balance difficulties. CDC’s STEADI (Stopping Elderly Accidents, Deaths, and Injuries) initiative (www.cdc.gov/steadi) recommends a physician-directed approach to identify older adult patients who may be at increased risk for a fall. Acknowledging the potentially increased risk of an outdoor fall during winter, for some segments of the older adult population, may help providers address and intervene to reduce their patients’ unique fall risk. These results may encourage community-based organizations serving older adults to increase fall prevention messaging during winter.
Acknowledgements
The authors thank Tadesse Haileyesus, MS (Mathematical statistician) with the National Center of Injury Prevention and Control for his guidance with coding and analysis of the National Electronic Injury Surveillance System-All Injury Program data.
Funding source
No outside funding was used to support this work.
Biographies
Ramakrishna S. Kakara MPH, is an ORISE Fellow in the Division of Injury Prevention at CDC’s National Center for Injury Prevention and Control. His research focuses on older adult fall surveillance and prevention.
Briana L. Moreland MPH, is a public health analyst and Synergy America Inc contractor for the Division of Injury Prevention at CDC’s National Center for Injury Prevention and Control. Her research focuses on older adult fall prevention.
Yara K. Haddad PharmD, MPH, is a geriatric pharmacist and epidemiologist at the Centers for Disease Control and Prevention, Division of Injury Prevention. Her areas of concentration are geriatric care, older adult injury prevention, promoting older adult safe mobility and aging without injury, and exploring effects of medications and polypharmacy on older adult safety.
Iju Shakya MPH, is an ORISE Fellow in the Division of Injury Prevention at CDC’s National Center for Injury Prevention and Control. Her research includes older adult fall prevention.
Gwen Bergen PhD, MPH, MS, is a behavioral scientist for the Safety Promotion Team at CDC’s National Center for Injury Prevention and Control. Her research focuses primarily on older adult fall prevention and older adult safe mobility.
Appendix A. Seasonal variation by location of fall narrative codebook
Residential status (3 options)
- Residential facility (non-community), includes:
- nursing home, skilled nursing facility, extended care facility, long term care, assisted living, hospice, rehab, detox, or Alzheimer’s unit, convalescent home, group home, then these are coded as nursing home. If it doesn’t mention this assume it didn’t happen in a nursing home
- Community, includes:
- Doesn’t specifically mention nursing home.
- Adult day care or senior center
- If visiting a family member in a nursing home then community
- Prison, includes:
- Jail, prison or corrections facility
Location (3 options)
- Indoor, includes:
- Rooms in a house or apartment: bedroom, kitchen, living room, bathroom
- Stairs: any mention of stairs or steps where evident they are indoors, otherwise outdoors or unknown. If stairs have carpet then indoors, if stairs have baseboards then indoors.
- Public places: restaurant, store, hotel, jail, church, work, lobby/lounge, stairs in public place, escalator, elevator (had to be apparent that these occurred inside) If “at public place”, for example fell “at restaurant” assume inside.
- Recreation area: bowling alley, gym, sports courts where evident they were inside
- Unspecified: Any mention of cabinets, sink, lamp, AC, heater, cleaning house, Hoyer lift, or fall out of a window assume indoor. Falls to the floor or carpet is indoor, except concrete/cement floor
- Outdoor, includes:
- Yard, porch, garage, balcony, ramp, and stairs if evident they are outside.
- Recreation area: parks, lakes, camping, rivers, outside sports courts, RV/camper, tent, national park, tree stand, beach, and farm.
- Public places: sidewalk, parking lot, curb, outdoor work place, bus, subway, metal grate, stairs outside a public place, street, and driveway.
- Any mention of falls to grass, gravel, rocks, ditch, shed, mud, ice, snow, rain, falling off ladder or a platform that is greater than 7 feet, uneven concrete.
Unknown: Can’t tell if location is inside or outside, or if stairs are inside or outside. When a fall happens on a concrete/cement floor, ground. While coming in or out of a place (and can’t determine whether the fall happened inside or outside), playing pickle ball, at train station/-catching train. When fall is associated with electric cord (unless more context provided), window sills, and ramps in public places.
Weather:
If any mention of ice, snow, rain, hail, heat or any other term related to weather, then mention the term.
Appendix B
Characteristics of community dwelling older adults who sought emergency department care for a fall by season and unknown location – National Electronic Injury Surveillance System – All Injury Program, 2015.
| Characteristics | Total | Spring (March-May) |
Summer (June-August) |
Autumn (September-November) |
Winter (December-February) |
||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | 95%CI | % | 95%CI | % | 95%CI | % | 95%CI | |
| Total | 13,720 | 24.8 | (23.9–25.7) | 25.4 | (24.5–26.4) | 24.7 | (23.8–25.6) | 25.1 | (24.1–26.0) |
| Gender | |||||||||
| Male | 4,897 | 24.9 | (23.3–26.5) | 25.2 | (23.7–26.8) | 24.3 | (22.7–25.8) | 25.6 | (24.0–27.2) |
| Female | 8,823 | 24.7 | (23.6–25.9) | 25.5 | (24.4–26.7) | 24.9 | (23.8–26.1) | 24.8 | (23.7–26.0) |
| Age-group | |||||||||
| 65–74 | 5,256 | 24.3 | (22.8–25.8) | 26.7 | (25.1–28.2) | 24.0 | (22.6–25.5) | 25.0 | (23.5–26.6) |
| 75–84 | 4,583 | 25.6 | (24.0–27.2) | 24.1 | (22.5–25.6) | 25.3 | (23.7–26.9) | 25.1 | (23.5–26.7) |
| 85+ | 3,881 | 24.5 | (22.8–26.2) | 25.4 | (23.7–27.2) | 24.9 | (23.1–26.6) | 25.2 | (23.4–26.9) |
n - Unweighted sample size.
% - Weighted percent.
95%CI - 95% Confidence interval.
Footnotes
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Publisher's Disclaimer: Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- Al-Azzani W, Adam Maliq Mak D, Hodgson P, & Williams R (2016). Epidemic of fractures during a period of snow and ice: Has anything changed 33 years on? BMJ Open, 6(9), e010582. doi: 10.1136/bmjopen-2015-010582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ambrose AF, Paul G, & Hausdorff JM (2013). Risk factors for falls among older adults: A review of the literature. Maturitas, 75(1), 51–61. 10.1016/j.maturitas.2013.02.009. [DOI] [PubMed] [Google Scholar]
- Beynon C, Wyke S, Jarman I, Robinson M, Mason J, Murphy K, & collaborators (2011). The cost of emergency hospital admissions for falls on snow and ice in England during winter 2009/10: A cross sectional analysis. Environmental Health, 10(1), 60. doi : 10.1186/1476-069X-10-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bischoff-Ferrari HA, Orav JE, Barrett JA, & Baron JA (2007). Effect of seasonality and weather on fracture risk in individuals 65 years and older. Osteoporosis International, 18(9), 1225–1233. 10.1007/s00198-007-0364-6. [DOI] [PubMed] [Google Scholar]
- Bobb JF, Ho KK, Yeh RW, Harrington L, Zai A, Liao KP, & Dominici F (2017). Time-course of cause-specific hospital admissions during snowstorms: An analysis of electronic medical records from major hospitals in Boston, Massachusetts. American Journal of Epidemiology, 185(4), 283–294. 10.1093/aje/kww219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boye ND, Mattace-Raso FU, Van der Velde N, Van Lieshout EM, De Vries OJ, Hartholt KA,… Van Beeck EF (2014). Circumstances leading to injurious falls in older men and women in the Netherlands. Injury, 45(8), 1224–1230. 10.1016/j.injury.2014.03.021. [DOI] [PubMed] [Google Scholar]
- Bulajic-Kopjar M (2000). Seasonal variations in incidence of fractures among elderly people. Injury Prevention, 6(1), 16–19. 10.1136/ip.6.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell AJ, Spears G, Borrie M, & Fitzgerald J (1988). Falls, elderly women and the cold. Gerontology, 34(4), 205–208. 10.1159/000212954. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, Data and Statistics - Productive Aging and Work | NIOSH | CDC. [online] (2015) [cited 2021 Jan 21]. Available from https://www.cdc.gov/niosh/topics/productiveaging/dataandstatistics.html.
- Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) [Online]. (2003). National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. Available from: URL: www.cdc.gov/injury/wisqars. [2021 January 22]. [Google Scholar]
- Dey AN, Hicks P, Benoit S, & Tokars JI (2010). Automated monitoring of clusters of falls associated with severe winter weather using the BioSense system. Injury Prevention, 16(6), 403–407. 10.1136/ip.2009.025841. [DOI] [PubMed] [Google Scholar]
- Duckham RL, Procter-Gray E, Hannan MT, Leveille SG, Lipsitz LA, & Li W (2013). Sex differences in circumstances and consequences of outdoor and indoor falls in older adults in the MOBILIZE Boston cohort study. BMC Geriatrics, 13(1), 133. 10.1186/1471-2318-13-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gevitz K, Madera R, Newbern C, Lojo J, & Johnson CC (2017). Risk of fall-related injury due to adverse weather events, Philadelphia, Pennsylvania, 20062011. Public Health Report, 132(1_suppl), 53S–58S. doi: 10.1177/0033354917706968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gronskag AB, Forsmo S, Romundstad P, Langhammer A, & Schei B (2010). Incidence and seasonal variation in hip fracture incidence among elderly women in Norway. The HUNT Study. Bone, 46(5), 1294–1298. 10.1016/j.bone.2009.11.024. [DOI] [PubMed] [Google Scholar]
- Jacobsen SJ, Sargent DJ, Atkinson EJ, O’Fallon WM, & Melton LJ III, (1995). Population-based study of the contribution of weather to hip fracture seasonality. American Journal of Epidemiology, 141(1), 79–83. 10.1093/oxfordjournals.aje.a117348. [DOI] [PubMed] [Google Scholar]
- Johansen A, Boulton C, & Neuburger J (2016). Diurnal and seasonal patterns in presentations with hip fracture-data from the national hip fracture database. Age and Ageing, 45(6), 883–886. 10.1093/ageing/afw133. [DOI] [PubMed] [Google Scholar]
- Jung HY, Kim SH, Lee SC, Kim S, Cho GC, Kim MJ, … Han C (2018). Relating factors to severe injury from outdoor falls in older people. Geriatrics and Gerontology International, 18(1), 80–87. 10.1111/ggi.13144. [DOI] [PubMed] [Google Scholar]
- Keadle SK, McKinnon R, Graubard BI, & Troiano RP (2016). Prevalence and trends in physical activity among older adults in the United States: A comparison across three national surveys. Preventive Medicine, 89, 37–43. 10.1016/j.ypmed.2016.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kromer B, & Howard D (2013). Labor force participation and work status of people 65 years and older. Retrieved from https://www2.census.gov/library/publications/2013/acs/acsbr11-09.pdf.
- Leavy B, Aberg AC, Melhus H, Mallmin H, Michaelsson K, & Byberg L (2013). When and where do hip fractures occur? A population-based study. Osteoporosis International, 24(9), 2387–2396. 10.1007/s00198-013-2333-6. [DOI] [PubMed] [Google Scholar]
- McKiernan FE (2005). A simple gait-stabilizing device reduces outdoor falls and nonserious injurious falls in fall-prone older people during the winter. Journal of the American Geriatrics Society, 53(6), 943–947. 10.1111/j.1532-5415.2005.53302.x. [DOI] [PubMed] [Google Scholar]
- Mondor L, Charland K, Verma A, & Buckeridge DL (2015). Weather warnings predict fall-related injuries among older adults. Age and Ageing, 44(3), 403–408. 10.1093/ageing/afu199. [DOI] [PubMed] [Google Scholar]
- Moreland B, Kakara R, Haddad Y, Shakya I, & Bergen G (2020). A descriptive analysis of location of older adult falls that resulted in emergency department visits in the United States, 2015. American Journal of Lifestyle Medicine. 10.1177/1559827620942187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morency P, Voyer C, Burrows S, & Goudreau S (2012). Outdoor falls in an urban context: Winter weather impacts and geographical variations. Canadian Journal of Public Health/Revue Canadienne de Sante’e Publique, 103(3), 218–222. 10.1007/BF03403816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Electronic Injury Surveillance System (NEISS). (2021) United States Consumer Product Safety Commission Available from: https://www.cpsc.gov/Research-Statistics/NEISS-Injury-Data [2021 January 21].
- O’Hare C, O’Sullivan V, Flood S, & Kenny RA (2016). Seasonal and meteorological associations with depressive symptoms in older adults: A geo-epidemiological study. Journal of Affective Disorders, 191, 172–179. 10.1016/j.jad.2015.11.029. [DOI] [PubMed] [Google Scholar]
- Qian XX, Chau PH, Kwan CW, Lou VW, Leung AYM, & collaborators. (2019). Seasonal pattern of single falls and recurrent falls amongst community-dwelling older adults first applying for long-term care services in Hong Kong. Age and Ageing, 49(1), 125–129. doi: 10.1093/ageing/afz139. [DOI] [PubMed] [Google Scholar]
- Roberts AW, Ogunwole SU, Blakeslee L, & Rabe MA (2018). The population 65 years and older in the United States: 2016. Retrieved from https://www.census.gov/content/dam/Census/library/publications/2018/acs/ACS-38.pdf.
- Schiller JS, Kramarow EA, & Dey AN (2007). Fall injury episodes among noninstitutionalized older adults: United States, 2001–2003. Advance data (392), 1–16. doi: 10.1037/e671852007-001. [DOI] [PubMed] [Google Scholar]
- Schroeder T, & Ault K (2001). The NEISS sample: Design and implementation. Washington, DC: US Consumer Product Safety Commission. [Google Scholar]
- Stansbury L, Swinson A, Schmitt J, Stevens M, Kobayashi K, & Vangellow C (1995). Work-related injuries associated with falls during ice storms-National Institutes of Health, January 1994. MMWR Morbidity Mortality Weekly Report, 44 (49), 920–922. [PubMed] [Google Scholar]
- Stevens JA, Thomas KE, & Sogolow ED (2007). Seasonal patterns of fatal and nonfatal falls among older adults in the U.S. Accidental Analysis and Prevention, 39(6), 1239–1244. 10.1016/j.aap.2007.03.011. [DOI] [PubMed] [Google Scholar]
- Vikman I, Nordlund A, Näslund A, & Nyberg L (2011). Incidence and seasonality of falls amongst old people receiving home help services in a municipality in northern Sweden. International Journal of Circumpolar Health, 70(2), 195–204. 10.3402/ijch.v70i2.17813. [DOI] [PubMed] [Google Scholar]
- Wareham K, Johansen A, Stone MD, Saunders J, Jones S, & Lyons RA (2003). Seasonal variation in the incidence of wrist and forearm fractures, and its consequences. Injury, 34(3), 219–222. 10.1016/s0020-1383(02)00212-7. [DOI] [PubMed] [Google Scholar]


