Introduction
Foreign body ingestion comprises a true foreign body (ie, non-food) ingestion and food bolus impaction. Foreign body ingestion is not uncommon and accounts for roughly 4% of urgent endoscopies undertaken.1 2 True foreign body ingestion is mostly encountered in paediatric populations with 75% of cases occurring in less than 5-year-old children.1 Coins, buttons, plastic items, batteries and bones are common culprits.3 Food bolus impaction on the other hand is mostly seen in adults, usually accidental (95% of cases). Steakhouse syndrome, animal bones, toothpicks and fish bones are the most frequent.2 True foreign body ingestion (coins and dentures) is rare in adults. Intentional true foreign body ingestion can be seen in patients with psychiatric illness, prisoners (secondary gain) and drug dealers (‘body packing’). Underlying oesophageal conditions including eosinophilic oesophagitis (10% in adults, up to 50% in children), motility disorder, stenosis and diverticula are frequent.2 4 Most ingested foreign bodies will pass spontaneously.5 However, 10%–20% require endoscopic removal, and less than 1% require surgical extraction or treatment of a complication.6 This review focuses on the management of foreign bodies located in the upper gastrointestinal tract, in adults. The quality of evidence of the guidelines is low; however, substantial clinical experience provides strong levels of recommendation.7 8 The management of rectal foreign bodies mostly relies on surgical, transanal extraction and is not detailed herein.
Initial evaluation
Precise history (type of foreign body, time of onset) is essential. Physical examination is also mandatory. Most patients are asymptomatic. Symptoms arise when the foreign body is stuck in the oesophagus or when a complication occurs (obstruction and perforation).9 Emesis, retching, blood-stained saliva, hypersialorrhoea, wheezing and/or respiratory distress in non-communicative patients (children and psychiatric patients) are suggestive of foreign body impaction.7 Oesophageal impaction (food bolus) is often symptomatic: retching, vomiting, foreign body sensation, dysphagia, odynophagia, sore throat and retrosternal pain. Hypersialorrhoea and inability to manage secretions suggest complete oesophageal obstruction, warranting urgent endoscopic retrieval.7 Cervical crepitus, neck swelling or pneumomediastinum are suggestive of oesophageal perforation. Choking, stridor, wheezing or dyspnoea can be seen as a result of aspiration or tracheal compression by the foreign body.
Radiographic evaluation is not always necessary and should not delay urgent treatment. It is not useful in non-complicated non-bony food impaction.7 Plain (or biplane if not contributive) radiographic evaluation of the neck, chest and abdomen is recommended to assess the presence, number, location, size and shape of the radiopaque foreign body. Also, signs of complications can be detected such as aspiration, free mediastinal or peritoneal air and subcutaneous emphysema. Contrast studies can delay treatment, impair visualisation during subsequent endoscopy and worsen complications. A barium swallow is contraindicated when perforation is suspected, and aspiration of hypertonic contrast agents can cause acute pulmonary oedema.2 X-ray contrast study for the evaluation of non-radiopaque objects is not recommended. A CT scan is the preferred method in this setting, although rarely needed.7
Endoscopy: setting and equipment
Informed consent must be obtained before endoscopy, although it may be challenging in psychiatric patients and in prisoners.2 Usually, oesophagogastroduodenoscopy (OGD) is performed under conscious sedation, with patients on left lateral position and slight lowering of the head, so as to reduce the risk of aspiration.2 General anaesthesia with endotracheal intubation is required in difficult cases to ensure airway protection (younger children, poor tolerance, multiple foreign bodies, anticipated difficult extraction and when rigid oesophagoscopy is needed).
A nasogastroscope with an external diameter less than 6 mm and a 2 mm large operating channel should be used in children aged less than 1 year. Only small polypectomy retrieval nets (20 mm width), polypectomy snares and Dormia baskets can pass through the operating channel. Standard flexible gastroscopes with an external diameter of 9.8 mm and a 2.8 mm large operating channel or therapeutic gastroscopes with a>3.2 mm single operating channel are used otherwise. Double-channel endoscopes, allowing the combined use of devices, small-calibre endoscopes, allowing a transnasal approach, and enteroscopes can be used in specific settings.7 Lastly, several studies have suggested that rigid oesopharyngoscopy can be safely used for body extraction.10 11 The choice between rigid and flexible oesophagoscopy mainly depends on the size, shape and location of the ingested foreign body. The availability of the equipment and trained physician also play a role.12 Flexible oesophagoscopy performed by gastroenterologists is easy technically wise and allows a complete evaluation of the oesophagus.13 Rigid oesophagoscopy performed by ENTs can be useful when the foreign body is located at the pharyngoesophageal junction because in such cases, flexible oesophagoscopy is limited by a small working space and poor visual field. Rigid oesophagoscopes on the other hand have a larger working channel thus making it possible to use a large forceps (with a stronger grasp).14 For foreign bodies that have passed the oesophagus, rigid oesophagoscopy should be attempted only when flexible endoscopy has failed as the complication rate is higher (10% vs 5%).15
Numerous retrieval devices are available. The chosen device will depend not only on the size and shape of the foreign body but also on the length and operating channel width of the endoscope and the endoscopist’s preference and habits.16 Foreign body retrieval forceps such as rat-tooth (most common), alligator-tooth or shark-tooth forceps (reusable) are most often used. Retrieval forceps with 2 to 5 prongs can be useful to retrieve soft objects (ie, food bolus impaction), but do not provide a secure enough grip for harder/heavy foreign bodies. Standard biopsy forceps have a small opening width and are therefore preferably used in small and soft foreign bodies. Baskets with three, four or six wires, such as the Dormia basket, can be used for round foreign bodies. Standard polypectomy snares and retrieval nets are also used and widely available. Polypectomy snares are inexpensive and their size ranges from 10 to 30 mm. Retrieval nets on the other hand are expensive but are useful for certain types of foreign bodies (coins, disc batteries or magnets) and for en bloc removal of food boluses. Lastly, balloons can be used for the removal of hollow foreign bodies.16
Special equipment must be used to protect the airways and the oesophageal mucosa in case of sharp or bulky foreign bodies.16 For instance, an overtube can be placed over the endoscope prior to the procedure. A long overtube advanced passed the gastro-oesophageal junction (GEJ), a hood placed upside down at the tip of the endoscope (which unfurls at the GEJ when the endoscope is pulled out), or a transparent distal cap (from elastic band ligation or mucosectomy kits) can be used for the removal of sharp or pointed foreign bodies located distal to the oesophagus.16
Management
Endoscopic extraction of food bolus impaction and foreign body ingestion from the upper digestive tract is successful in 95% of cases.2 17 When endoscopic extraction fails, rigid oesophagoscopy for the upper oesophageal foreign body can be considered. Referral to a tertiary endoscopy centre should be discussed in difficult cases (2% in adult series).2 Surgical management is required in 1% of cases.2
In 30% of cases, no foreign body is identified by OGD.2 Enteroscopy and surgery should be considered for long, sharp/pointed foreign bodies, batteries or magnets that have passed the duodenojejunal angle because of the risk of complication (perforation). In other cases, outpatient management is suggested with daily stool observation and radiographic evaluation every 72 hours to monitor the progress through the gastrointestinal tract.7 Patients should be informed of the clinical signs of perforation prompting rapid consult.
Overall, 80% of foreign bodies pass through the digestive tract.5 In 20% of cases, they remain impacted in the narrower segments of the digestive tract, mainly in the oesophagus (50%–75%).2 Oesophageal impaction carries the highest risk of complication (25% higher than other parts of the digestive tract) that can be life threatening given the proximity to vital organs.18 Urgent endoscopic extraction, irrespective of a full stomach or not, must be performed without delay in the following cases: (1) foreign body in the upper third part of the oesophagus, (2) complete obstruction, (3) sharp foreign bodies or button batteries.7 Any foreign body lodged in the oesophagus should in any case be extracted within 24 hours following ingestion as the risk of complication increases with time. Conversely, blunt and small foreign bodies that have reached the stomach will likely pass the digestive tract spontaneously with a limited risk of perforation. Extraction should be performed in case of failure to pass the pylorus after 3–4 weeks.7 Perforation may occur in narrow parts of the small bowel (duodenum, ileocaecal valve). A blunt foreign body should thus be extracted from the duodenum after 4–8 days.7 A sharp foreign body beyond the duodenum should be surgically extracted if it does not progress after 3 days based on the daily radiographic evaluation. We propose an algorithm of the timing of extraction in figure 1.
Figure 1.
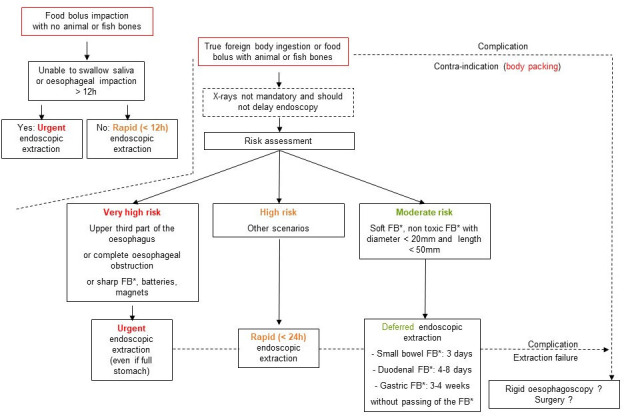
Foreign body (FB*) ingestion management algorithm. Proposal of an algorithm of the timing of endoscopic extraction of upper gastrointestinal foreign bodies, based on current European Society of Gastrointestinal Endoscopy (ESGE) and American Society for Gastrointestinal Endoscopy (ASGE) guidelines7 8 and on our experience (Parisian on-call endoscopy team, APHP, Paris, France). NB: timings are given with hour of ingestion as reference mark.
Food bolus impaction
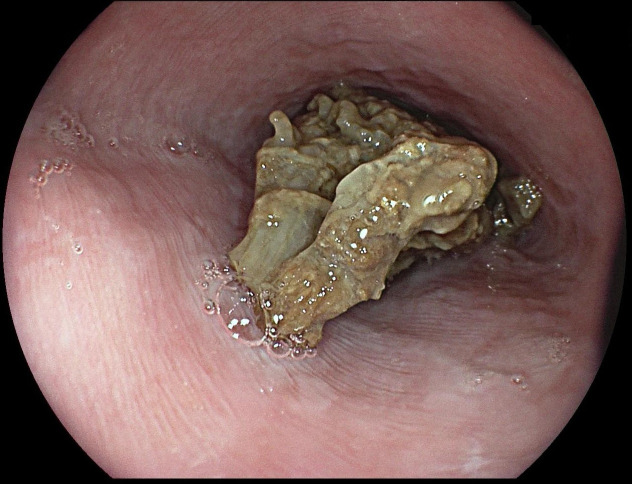
In adults, meat bones (Western world) and fishbones (Asia) are the most frequent cause of food bolus impaction.19 20 The presence of a meat bone or fishbone must be assessed. Most food bolus impactions are oesophageal. Urgent treatment is required if the patient is unable to swallow saliva. Treatment must otherwise be performed within 12–24 hours of impaction.7 Given the risk of perforation and/or fistula, treatment within 6 hours is probably safer.21 In the case of oesophageal soft food impaction, intervention after 12 hours does not yield a higher rate of complications or mortality, which suggests that early intervention might not be needed in such cases.22 Data are conflicting regarding pharmaceutical treatment. Glucagon (1 mg, intravenously) has been shown to be no better than a placebo to achieve disimpaction,23 but studies have also suggested its efficacy in 34.5% of cases.24 In any case, a medication trial should not delay endoscopic extraction. Effervescent agents (so-called fizzy drinks) have long been suggested for food bolus disimpaction. A review published in 2005 suggests, based on six low level of evidence papers, that fizzy drinks seem to be effective.25 However, given the risk of aspiration, we would not recommend this type of treatment in cases of obstructive impaction (unable to swallow saliva), especially in the upper third part of the oesophagus. The suction of saliva in the hypopharynx with the endoscope reduces the risk of aspiration and allows proper visualisation when intubating the oesophagus thus preventing from pushing the food bolus and/or associated denture/toothpick through a diverticulum or against a stricture. When the food bolus is in view (figure 2), extraction is favoured over pushing blindly into the stomach as the distal oesophageal anatomy is often not assessable. However, data suggest that the risk of complication is similar.24 En bloc or piecemeal (after fragmentation) extraction, using the most appropriate device available, is the recommended technique.16 An overtube is helpful when multiples passages are needed, such as cases of gastric bezoar. If the pushing technique is attempted, then progressive pressure on the central part of the bolus is the safer way. Pressure should be interrupted if the progression of the bolus comes to a halt.26 In case of food bolus impaction in a stent, the pushing technique is contraindicated due to the risk of perforation and stent migration.
Figure 2.
Food bolus impaction in the oesophagus. A middle-aged patient was admitted for food bolus impaction. She presented 2 hours after the ingestion and presented with chest pain and hypersialorrhoea, but no crepitus or fever. No biological or imaging workup was performed. The patient was promptly transferred to the endoscopy unit, 3 hours postingestion, for endoscopic extraction. Rapid sequence intubation was performed given the aspiration risk. A meat bolus (without bones) was impacted in the lower third part of the oesophagus. No sign of perforation was noted. On scope advancement, the bolus passed spontaneously into the stomach. Endoscopic extraction was thus not performed. The oesophageal wall appeared normal. Biopsies showed a normal oesophageal mucosa, with no eosinophilic infiltration. The patient was discharged on the same day.
Sharp and pointed objects
Sharp or pointed accessible foreign body must be extracted without delay.7 27 Retrieval forceps, retrieval nets, and/or polypectomy snares are best suited for the task. Using protective devices (cap, latex protector hood or overtube) reduces the risk of perforation and mucosal damage during extraction.5 The sharp tip for the foreign body can be either orientated in the upwards position or trailed distally to the endoscope (figure 3).
Figure 3.
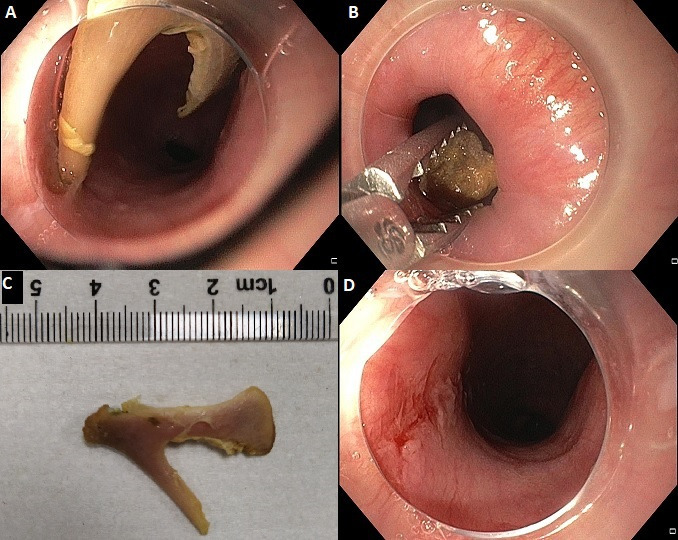
Chicken bone impaction in the oesophagus. A middle-aged patient was admitted after accidental ingestion of a chicken bone during his lunch. The patient had chest pain and hypersialorrhoea, but no crepitus or fever. No biological or imaging workup was performed. The patient was urgently transferred to the endoscopy unit, 2 hours postingestion, for endoscopic extraction. Rapid sequence intubation was performed given the aspiration risk. A transparent cap was placed at the tip of a 9.8 mm diameter gastroscope. The chicken bone was found impacted in the upper third part of the oesophagus. No sign of perforation was noted. Endoscopic extraction was performed with an alligator-tooth forceps. No significant mucosal damage was observed after extraction. The patient was discharged on the same day.
Long or bulky objects
Extraction of blunt foreign bodies longer than 3 cm in children younger than 1 year and longer than 5 cm in children older than 1 year is recommended.5 7 In adults, foreign bodies larger than 2–2.5 cm or longer than 5–6 cm must be extracted before passing the pylorus because of the risk of perforation (15%–35%).28 Retrieval nets, polypectomy snares or Dormia baskets are best suited for this scenario (figure 4). For very long objects (ie, spoons or forks), a double operating channel endoscope allows the use of two snares. Surgery can be considered in this setting as well.
Figure 4.
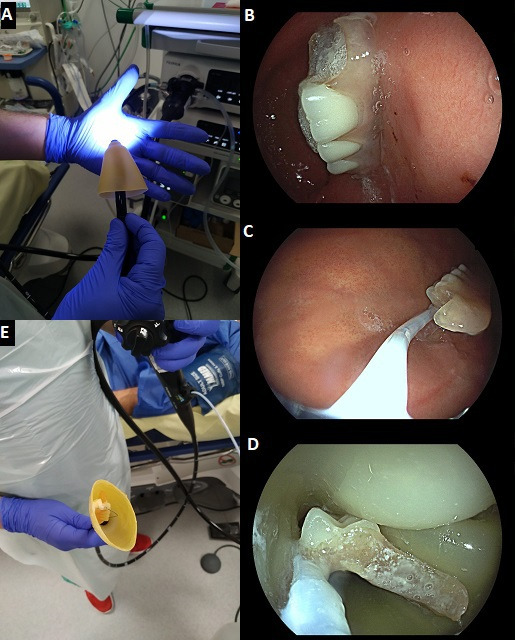
Dental bridge ingestion. An elderly patient was admitted to the endoscopy suite 4 hours after the accidental ingestion of his dental bridge. The patient was asymptomatic. No biological or imaging workup had been performed. A latex hood was placed at the tip of a gastroscope (A). The dental bridge was found in the stomach, with no sign of mucosal damage (B). It was approximately 6 cm long with two sharp edges. Endoscopic extraction was performed with a 10 mm polypectomy snare (C). The latex hood unfolded while passing of the gastro-oesophageal junction, thus protecting the oesophageal wall from the foreign body’s sharp edges (D, E). No significant mucosal damage was observed after extraction. The patient was discharged the next day.
Coins
Coins are the most frequently ingested foreign body in the western paediatric population. Coins are also seen in adults with psychiatric disorders or prisoners. Oesophageal impaction (73% of paediatric cases) requires urgent removal.3 Coins larger than 20 mm or that fail to pass the stomach within 3 days should also be removed. Retrieval forceps allow a quick and easy extraction in most cases.
Magnets
Ingested magnets carry a high risk of wall necrosis (causing fistula and/or perforation), occlusion and volvulus. Biplanar radiography is important to check for any metal foreign body or other magnets. Urgent extraction is then required.5 7
Batteries
Ingestion of cylindrical battery (AA, AAA) is rare (0.6% of ingestions) and usually non-severe. These batteries will often migrate rapidly in the stomach where the risk of electrical burn is low as compared with the oesophagus. However, after over 24 hours in the stomach, batteries should be extracted within the next 24 hours. Retrieval nets are most useful in this indication. In contrast, the widespread use of large (>20 mm) and high-voltage (3 V) button batteries is associated with an increased number of ingestions, which can be life threatening.29 Most of these cases are seen in children under 4 years.29 Button batteries impacted in the oesophagus can cause electrical burns, caustic burns and necrosis and should therefore be extracted urgently (figure 5).
Figure 5.

Button battery impaction in the oesophagus. A young adult patient was admitted after the accidental ingestion of a button battery. The patient had chest pain, but no hypersialorrhoea, crepitus or fever. The patient was immediately transferred to the endoscopy suite at 2 hours postingestion. The battery was extracted from the lower third part oesophagus with a retrieval net. Two large oesophageal ulcerations with a black necrotic base and a blue halo (lithium crystals) were found. The lithium crystals were flushed and aspirated to prevent further caustic injury. A CT scan showed no sign of perforation. A nasogastric tube was placed followed by 4 weeks of enteral nutrition. Endoscopic evaluation at week 4 showed complete mucosal healing and no stenosis. Oral intake was resumed. Follow-up was uneventful.
Drugs
Body packing is the concealment of illicit drugs packed in latex condoms or balloons by insertion into the rectum or swallowing (figure 6). Endoscopic extraction is not recommended because the rupture of the package and subsequent leakage of the contents can lead to fatal overdose.7 Conservative management is recommended: hospitalisation, clinical observation, bowel irrigation and radiographic monitoring. In case of signs of intoxication or obstruction or impaction with failure to pass, surgery is warranted.7
Figure 6.
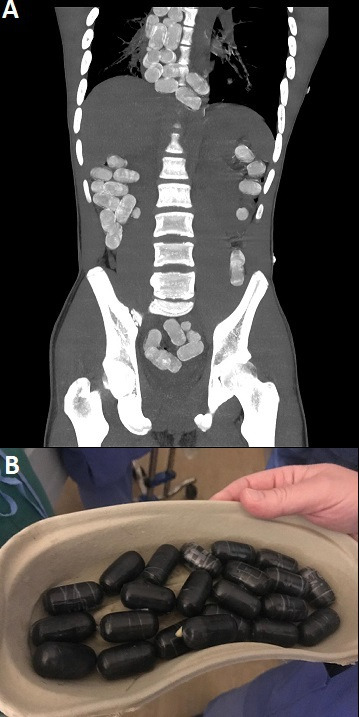
Body packing*. A young adult male patient was admitted at for chest pain and hypersialorrhoea, 24 hours after he had ingested dozens of narcotic packs. He had no sign of shock or perforation. A CT scan showed multiple drug packs along the gastrointestinal tract (A). Numerous packs were impacted in the oesophagus. Despite being contraindicated in theory, due to the risk of rupture, endoscopic extraction was decided as surgical management of this very dilated oesophagus was felt at an even higher risk of fistula. The patient was admitted to the operating room at 26 hours of ingestion. The surgical team was standing by in case of rupture. Rapid sequence intubation was performed given the aspiration risk. All oesophageal packs were extracted with a retrieval net and none showed any sign of rupture (B). The patient was admitted to the intensive care unit for surveillance. He received laxatives to accelerate the passing of the other packs. Follow-up was uneventful. *Courtesy of Dr Heythem Soliman, Parisian On-call Endoscopy Team, Paris, France.
Complications
Complications such as perforation, obstruction, infection, haemorrhage, fistula and foreign body migration through the digestive wall occur in 1%–5% of cases.2 15 30–32 Oesophageal perforation is the most feared and most frequent (2%) complication.18
In a prospective study of 105 patients, the complication rate was 38%. Overall, 9% of patients had a complication that occurred during endoscopic extraction, 1% of which was a perforation.30 The mortality rate was low. A single death case has been reported in a series of 2206 children.33 Five severe outcomes were observed in an adult series of 127 000 foreign body ingestion but no death was reported.1 In retrospective studies from Asia, risk factors for complications were identified including: age over 50 years, impaction over 24 hours, bone-type foreign body, foreign body larger than 30 mm, impaction higher than the mid-oesophagus and positive radiographic findings.20 31 32
All in all, it seems most severe complications (specifically perforations) occur before endoscopic retrieval and are rarely due to the latter. Complications from the extraction that are recognised early have a better outcome. Hospitalisation should thus be considered after a difficult extraction. In the case of perforation, nothing by mouth, parenteral nutrition, broad-spectrum antibiotics and proton pump inhibitors are the cornerstone of management. Endoscopic treatment (metal, fully covered self-expandable metal stent and vacuum therapy), when diagnosed early, should be considered. Finally, surgery is required when endoscopic treatment is impossible or has failed.
Follow-up and recurrence
Underlying conditions such as fragile dentures, psychiatric disorders and gastrointestinal diseases (specifically eosinophilic oesophagitis)34 are not uncommon and should be dealt with so as to avoid recurrence. In the case of food bolus impaction, oesophageal biopsies or dilation can be performed during the endoscopy provided there is no severe mucosal injury, to screen for eosinophilic oesophagitis or treat a stricture. Elective diagnostic and therapeutic procedures should be differed otherwise. Follow-up after an initial episode of food bolus impaction has been shown to significantly decrease the risk of recurrence.35
Dos and don’ts
Dos
Anticipate the need for intubation for airway protection before urgent endoscopic retrieval.
Don’ts
Attempt an endoscopic extraction of drug-containing packets.
Differ endoscopic extraction of food bolus impaction later than 12–24 hours.
Differ endoscopic extraction of a sharp or pointed foreign body.
Attempt endoscopic extraction of a rectal foreign body.
Differ endoscopic extraction because of radiographic evaluation.
Footnotes
Contributors: XD has selected the relevant references for review, the various cases for illustrations, and has written the outline of the article. AB and MC have written the complete version of the article. All authors have revised the final version of the article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: MC is a consultant for Boston Scientific and Cook Medical. XD is cofounder and shareholder of Augmented Endoscopy and has acted as a consultant for Alfasigma, Bouchara Recordati, Boston Scientific, Fujifilm, Medtronic, and Pentax.
Provenance and peer review: Commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
References
- 1. Bronstein AC, Spyker DA, Cantilena LR, et al. 2007 annual report of the American association of poison control centers' national poison data system (NPDS): 25th annual report. Clin Toxicol 2008;46:927–1057. 10.1080/15563650802559632 [DOI] [PubMed] [Google Scholar]
- 2. Mosca S, Manes G, Martino R, et al. Endoscopic management of foreign bodies in the upper gastrointestinal tract: report on a series of 414 adult patients. Endoscopy 2001;33:692–6. 10.1055/s-2001-16212 [DOI] [PubMed] [Google Scholar]
- 3. Little DC, Shah SR, St Peter SD, et al. Esophageal foreign bodies in the pediatric population: our first 500 cases. J Pediatr Surg 2006;41:914–8. 10.1016/j.jpedsurg.2006.01.022 [DOI] [PubMed] [Google Scholar]
- 4. Diniz LO, Towbin AJ. Causes of esophageal food bolus impaction in the pediatric population. Dig Dis Sci 2012;57:690–3. 10.1007/s10620-011-1911-8 [DOI] [PubMed] [Google Scholar]
- 5. Chen MK, Beierle EA. Gastrointestinal foreign bodies. Pediatr Ann 2001;30:736–42. 10.3928/0090-4481-20011201-08 [DOI] [PubMed] [Google Scholar]
- 6. Eisen GM, Baron TH, Dominitz JA, et al. Guideline for the management of ingested foreign bodies. Gastrointest Endosc 2002;55:802–6. 10.1016/S0016-5107(02)70407-0 [DOI] [PubMed] [Google Scholar]
- 7. ASGE Standards of Practice Committee, Ikenberry SO, Jue TL, et al. Management of ingested foreign bodies and food impactions. Gastrointest Endosc 2011;73:1085–91. 10.1016/j.gie.2010.11.010 [DOI] [PubMed] [Google Scholar]
- 8. Birk M, Bauerfeind P, Deprez PH, et al. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of gastrointestinal endoscopy (ESGE) clinical guideline. Endoscopy 2016;48:489–96. 10.1055/s-0042-100456 [DOI] [PubMed] [Google Scholar]
- 9. Arana A, Hauser B, Hachimi-Idrissi S, et al. Management of ingested foreign bodies in childhood and review of the literature. Eur J Pediatr 2001;160:468–72. 10.1007/s004310100788 [DOI] [PubMed] [Google Scholar]
- 10. Kim JK, Kim SS, Kim JI, et al. Management of foreign bodies in the gastrointestinal tract: an analysis of 104 cases in children. Endoscopy 1999;31:302–4. 10.1055/s-1999-13 [DOI] [PubMed] [Google Scholar]
- 11. Wang ZX, Cao XM, Ge XY, et al. [Clinical analysis of 234 esophageal foreign bodies]. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2019;33:148–51. 10.13201/j.issn.1001-1781.2019.02.013 [DOI] [PubMed] [Google Scholar]
- 12. Zhang X, Zhang X, Tu C, et al. Analysis of the management and risk factors for complications of esophageal foreign body impaction of jujube pits in adults. Wideochir Inne Tech Maloinwazyjne 2018;13:250–6. 10.5114/wiitm.2018.73132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhang S, Cui Y, Gong X, et al. Endoscopic management of foreign bodies in the upper gastrointestinal tract in South China: a retrospective study of 561 cases. Dig Dis Sci 2010;55:1305–12. 10.1007/s10620-009-0900-7 [DOI] [PubMed] [Google Scholar]
- 14. Nadir A, Sahin E, Nadir I, et al. Esophageal foreign bodies: 177 cases. Dis Esophagus 2011;24:6–9. 10.1111/j.1442-2050.2010.01085.x [DOI] [PubMed] [Google Scholar]
- 15. Berggreen PJ, Harrison E, Sanowski RA, et al. Techniques and complications of esophageal foreign body extraction in children and adults. Gastrointest Endosc 1993;39:626–30. 10.1016/S0016-5107(93)70212-6 [DOI] [PubMed] [Google Scholar]
- 16. Asge Technology Committee, Diehl DL, Adler DG, et al. Endoscopic retrieval devices. Gastrointest Endosc 2009;69:997–1003. 10.1016/j.gie.2009.01.005 [DOI] [PubMed] [Google Scholar]
- 17. Li Z-S, Sun Z-X, Zou D-W, et al. Endoscopic management of foreign bodies in the upper-GI tract: experience with 1088 cases in China. Gastrointest Endosc 2006;64:485–92. 10.1016/j.gie.2006.01.059 [DOI] [PubMed] [Google Scholar]
- 18. Tokar B, Cevik AA, Ilhan H. Ingested gastrointestinal foreign bodies: predisposing factors for complications in children having surgical or endoscopic removal. Pediatr Surg Int 2007;23:135–9. 10.1007/s00383-006-1819-0 [DOI] [PubMed] [Google Scholar]
- 19. Kirchner GI, Zuber-Jerger I, Endlicher E, et al. Causes of bolus impaction in the esophagus. Surg Endosc 2011;25:3170–4. 10.1007/s00464-011-1681-6 [DOI] [PubMed] [Google Scholar]
- 20. Hung C-W, Hung S-C, Lee CJ, et al. Risk factors for complications after a foreign body is retained in the esophagus. J Emerg Med 2012;43:423–7. 10.1016/j.jemermed.2011.01.030 [DOI] [PubMed] [Google Scholar]
- 21. Mosca S. Management and endoscopic techniques in cases of ingestion of foreign bodies. Endoscopy 2000;32:272–3. [PubMed] [Google Scholar]
- 22. Krill T, Samuel R, Vela A, et al. Outcomes of delayed endoscopic management for esophageal soft food impactions. Gastrointest Endosc 2020;91:806–12. 10.1016/j.gie.2019.12.020 [DOI] [PubMed] [Google Scholar]
- 23. Tibbling L, Bjorkhoel A, Jansson E, et al. Effect of spasmolytic drugs on esophageal foreign bodies. Dysphagia 1995;10:126–7. 10.1007/BF00440084 [DOI] [PubMed] [Google Scholar]
- 24. Schupack DA, Lenz CJ, Geno DM, et al. The evolution of treatment and complications of esophageal food impaction. United European Gastroenterol J 2019;7:548–56. 10.1177/2050640619836052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lee J, Anderson R. Best evidence topic report. effervescent agents for oesophageal food bolus impaction. Emerg Med J 2005;22:123–4. 10.1136/emj.2004.022053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vicari JJ, Johanson JF, Frakes JT. Outcomes of acute esophageal food impaction: success of the push technique. Gastrointest Endosc 2001;53:178–81. 10.1067/mge.2001.111039 [DOI] [PubMed] [Google Scholar]
- 27. Michaud L, Bellaïche M, Olives J-P, et al. [Ingestion of foreign bodies in children. Recommendations of the French-Speaking Group of Pediatric Hepatology, Gastroenterology and Nutrition]. Arch Pediatr 2009;16:54–61. 10.1016/j.arcped.2008.10.018 [DOI] [PubMed] [Google Scholar]
- 28. Palta R, Sahota A, Bemarki A, et al. Foreign-body ingestion: characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. Gastrointest Endosc 2009;69:426–33. 10.1016/j.gie.2008.05.072 [DOI] [PubMed] [Google Scholar]
- 29. Litovitz T, Whitaker N, Clark L, et al. Emerging battery-ingestion hazard: clinical implications. Pediatrics 2010;125:1168–77. 10.1542/peds.2009-3037 [DOI] [PubMed] [Google Scholar]
- 30. Chaves DM, Ishioka S, Félix VN, et al. Removal of a foreign body from the upper gastrointestinal tract with a flexible endoscope: a prospective study. Endoscopy 2004;36:887–92. 10.1055/s-2004-825856 [DOI] [PubMed] [Google Scholar]
- 31. Lai ATY, Chow TL, Lee DTY, ATY L, DTY L, et al. Risk factors predicting the development of complications after foreign body ingestion. Br J Surg 2003;90:1531–5. 10.1002/bjs.4356 [DOI] [PubMed] [Google Scholar]
- 32. Sung SH, Jeon SW, Son HS, et al. Factors predictive of risk for complications in patients with oesophageal foreign bodies. Dig Liver Dis 2011;43:632–5. 10.1016/j.dld.2011.02.018 [DOI] [PubMed] [Google Scholar]
- 33. Cheng W, Tam PK. Foreign-body ingestion in children: experience with 1,265 cases. J Pediatr Surg 1999;34:1472–6. 10.1016/S0022-3468(99)90106-9 [DOI] [PubMed] [Google Scholar]
- 34. Sperry SLW, Crockett SD, Miller CB, et al. Esophageal foreign-body impactions: epidemiology, time trends, and the impact of the increasing prevalence of eosinophilic esophagitis. Gastrointest Endosc 2011;74:985–91. 10.1016/j.gie.2011.06.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Prasad GA, Reddy JG, Boyd-Enders FT, et al. Predictors of recurrent esophageal food impaction: a case-control study. J Clin Gastroenterol 2008;42:771–5. 10.1097/MCG.0b013e31815576d2 [DOI] [PubMed] [Google Scholar]