Summary
Background
Cirrhosis is known to have a high prevalence and mortality worldwide. However, in Europe, the epidemiology of cirrhosis is possibly undergoing demographic changes, and etiologies may have changed due to improvements in standard of care. The aim of this population-based study was to analyze the trends and the course of liver cirrhosis and its complications in recent years in Germany.
Methods
We analyzed the data of all hospital admissions in Germany within diagnosis-related groups from 2005 to 2018. The diagnostic records of cirrhosis and other categories of diseases were based on ICD-10-GM codes. The primary outcome measurement was in-hospital mortality. Trends were analyzed through Poisson regression of annual number of admissions. The impact of cirrhosis on overall in-hospital mortality were assessed through the multivariate multilevel logistic regression model adjusted for age, sex, and comorbidities.
Findings
Of the 248,085,936 admissions recorded between 2005 and 2018, a total of 2,302,171(0•94%) were admitted with the diagnosis of cirrhosis, mainly as a comorbidity. Compared with other chronic diseases, patients admitted with cirrhosis were younger, mainly male and had the highest in-hospital mortality rate. Diagnosis of cirrhosis was an independent risk factor of in-hospital mortality with the highest odds ratio (OR:6•2[95%CI:6.1-6•3]) among all diagnoses. The prevalence of non-alcoholic fatty liver disease has increased four times from 2005 to 2018, while alcoholic cirrhosis is 20 times than other etiologies. Bleeding was found to be decreasing over time, but ascites remained the most common complication and was increasing.
Interpretation
This nationwide study demonstrates that cirrhosis represents a considerable healthcare burden, as shown by the increasing in-hospital mortality, also in combination with other chronic diseases. Alcohol-related cirrhosis and complications are on the rise. More resources and better management strategies are warranted.
Funding
The funders had no influence on this study.
Keywords: cirrhosis, hospital admission, male, mortality
Abbreviations: ALD, alcoholic liver diseases; DAA, direct-acting antiviral; DALYs, disability-adjusted life years; HBV, hepatitis B virus; HCV, hepatitis C virus; ICD, International Classification of Diseases; NAFLD, non-alcoholic fatty liver disease; NASH, non-alcoholic steatohepatitis; OPS, operation and procedure key system; YLDs, years lived with disability; YLLs, years of life lost
Research in context.
Evidence before this study
We searched Pubmed for key publications describing population-based observational studies of cirrhosis. The search terms ‘liver’, ‘cirrhosis’, ‘admission’ and ‘mortality rate’ were used. However, to the best of our knowledge, limited evidence is available on the profile of cirrhosis in central Europe and worldwide.
Added value of this study
The number of hospital admissions with cirrhosis has increased in recent years. Compared to other chronic diseases, patients admitted with cirrhosis are younger, mainly male and have the highest in-hospital mortality rate. Interestingly, the etiology of cirrhosis has been changing over time, with alcohol being by far the main etiology, 20 times than the other etiologies. The diagnosis of non-alcoholic fatty liver disease has increased four-fold during the observational period of 14 years. In parallel, decompensation episodes, mainly due to ascites, have increased in these years. The present study may represent the basis for development of strategies to improve care in cirrhosis.
Implications of all available evidence
Our study clearly demonstrates the considerable medical burden of cirrhosis, especially due to alcoholic etiology and as concomitant disease. Moreover, non-bleeding complications are increasing and need to be addressed properly.
Alt-text: Unlabelled box
Background
Cirrhosis is the common end stage of most chronic liver diseases. Depending on the grade of decompensation, the one-year mortality rate varies between 1% and 57% over the course of disease.1, 2, 3 The complications of cirrhosis are responsible for 1·3 million deaths worldwide every year and rank as the 14th most common cause of death globally, and the fourth in Central Europe.4, 5, 6, 7
Pivotal changes in the management of chronic liver disease have occurred in Western countries. In particular, the availability of direct-acting antivirals (DAA) to treat chronic hepatitis C virus (HCV) infection has significantly decreased the prevalence rate of cirrhosis due to HCV and therapy has changed the distribution of cirrhosis etiologies. By contrast, alcohol-related liver diseases (ALD) have remained as the major etiology of liver diseases in Northern European countries, such as the UK, for the past three decades.8 Moreover, non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH) have shown increased frequency in the etiologies of cirrhosis.3,9, 10, 11 Importantly, patients with NAFLD induced cirrhosis may be associated with hospital admissions due to other chronic diseases.10 Therefore, cirrhosis due to metabolic changes may not be the primary diagnosis when patients are admitted. To the best of our knowledge, trend changes within the etiology of liver cirrhosis have not been systematically addressed or investigated to date. These data emphasize the necessity of more widespread information on the burden of disease, especially during the last decade with significant changes in the standard of care and consideration of cirrhosis as a major comorbidity.
This population-wide study aimed at investigating the role of diagnosis of cirrhosis on outcome and disease burden in patients admitted to hospital for any reason in Germany from 2005 to 2018.
Methods
Study design and data source
This population-based, observational study evaluates all hospital admissions in Germany between 2005 and 2018. All data from the Federal Statistical Office of Germany are coded at each hospital according to the International Classification of Diseases, tenth edition, Clinical Modification (ICD-10-CM) codes. Diagnosis-related groups (DRG) and German operation and procedure key system codes (OPS) were used. For each observation in the data set, such as demographic data, clinical information, including main diagnosis and secondary diagnosis as well as procedures and reason for hospital discharge, are recorded during each hospitalization episode until patients are discharged or die. Information on disease outside the period of hospitalization could not be followed either before or after hospital admission and individual patient data were not available due to the data-protection law.
Demographic data from the European multicenter CANONIC study and the PREDICT study of decompensated cirrhosis were used and comparisons are listed in Supplementary Methods.12, 13, 14
Study population
We included hospital admissions of patients for any reason in Germany. The unit of analysis is one hospital admission episode (one DRG case). For each admission, ICD-10 codes for one primary diagnosis and up to 99 secondary diagnoses could be assigned. The information regarding specific conditions or outcomes observed in too few patients for each subgroup is censored by the Federal Statistical Office of the federal states to prevent potential access to individual patient data and is therefore censored in our analysis. Detailed descriptions on the dataset and methods of “controlled remote data processing using SAS scripts” have been published elsewhere.15
The patient admissions were further stratified as to whether or not they were diagnosed as liver cirrhosis. Liver cirrhosis was defined by ICD Code K74 or K70·3, either as main diagnosis or as comorbidity at the time of admission. Admissions of cirrhosis patients with complications as main diagnosis were also accounted as admissions mainly for cirrhosis. The coded etiologies of cirrhosis for analysis and definition of compensated or decompensated cirrhosis are listed in Supplementary Methods. The categories of other diseases were defined according to a study by the UK committee (Suppl. Table 1).8
Statistical analysis
We report number and proportions of admissions with different diagnoses, age, male proportion, and number of in-hospital deaths of patients admitted to hospital. We further report the mortality rate and age-standardized mortality rates within the disease categories. Additionally, age and sex-adjusted prevalence and mortality rate in each year were estimated using Poisson regression (Supplementary Methods).
Disability-adjusted life years (DALYs) were also calculated by sex, age and compensated or decompensated cirrhosis (Supplementary Methods). The primary outcome was all-cause in-hospital mortality. Transfer of patients admitted for malignant diseases to a hospice, was also considered as a primary outcome.
To assess the impact of liver cirrhosis and other chronic diseases on mortality, a multilevel logistic regression model was used to identify independent risk factors of in-hospital mortality. For details for the covariates selected into the model and methodology see Supplementary Methods.
Role of the funding source
The funders had no influence on study design, data collection and analysis, interpretation of data, on the writing of the report and decision to publish or preparation of the manuscript.
Results
Number of admissions with cirrhosis or its complications as main diagnosis or comorbidity and with other categories of chronic diseases
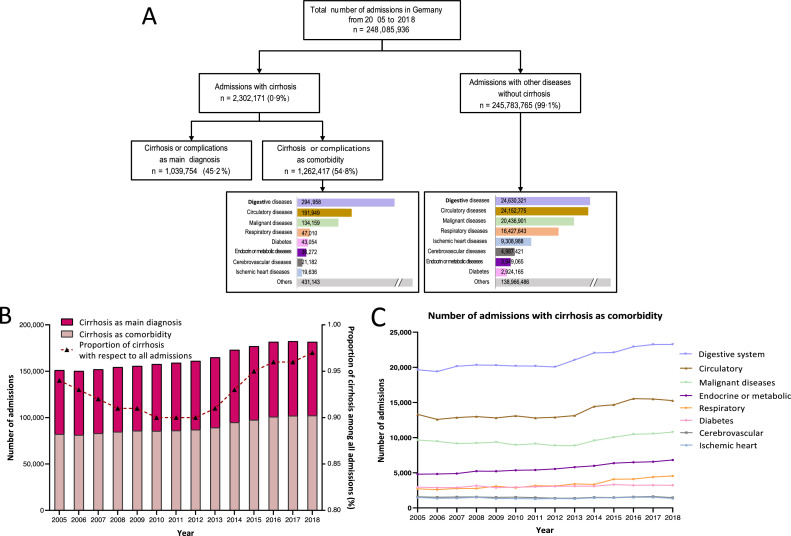
As shown in Fig. 1A and Table 1, 248,085,936 hospital admissions were reported in Germany from 2005 to 2018. Of these admissions during these 14 years, 2,302,171 (0·94%) hospitalized patients were diagnosed with cirrhosis. Interestingly, 54·8% (1,262,417) of these patients were diagnosed with cirrhosis or cirrhosis related complications as a comorbidity, while the primary diagnoses for admission were other categories of disease. Moreover, the number of admissions with cirrhosis increased significantly between 2005 and 2018, namely from 151,108 (0·94%) to 181,688 (0·97%). In addition, cirrhosis coded as a comorbidity has experienced a 24·5% increase (Fig. 1B). In particular, the number of admissions of cirrhosis as a comorbidity most frequently increased in patients admitted mainly for digestive diseases (25,640 to 30,014) and malignant diseases (15,554 to 19,281) (Fig. 1C and Suppl.Table 2).
Fig. 1.
Panel A. Flowchart of diagnosis-related groups database of German hospital admissions between 2005 and 2018. Panel B. Number of admissions with cirrhosis or its complications as main diagnosis or comorbidity for each year from 2005 to 2018. Proportion of cirrhosis admissions with regard to all admissions for each year from 2005 to 2018 was shown by dotted line. Panel C. Number of admissions of different chronic diseases as main diagnosis with cirrhosis as comorbidity for each year from 2005 to 2018.
Table 1.
Demographic data and number of interventions of patients admitted for cirrhosis, number of admissions of patients with different chronic diseases as main diagnosis without additional diagnosis of cirrhosis, and of patients with other diagnosis without cirrhosis.
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cirrhosis | 151108 | 150227 | 151988 | 154441 | 155693 | 157700 | 159098 | 161163 | 164986 | 173048 | 176991 | 181650 | 182390 | 181688 |
| Median age, year | 63 | 63 | 63 | 63 | 63 | 63 | 63 | 63 | 64 | 64 | 64 | 64 | 65 | 65 |
| Male percentage, % | 64·8 | 64·6 | 64·7 | 65 | 65 | 65 | 64·9 | 64·7 | 64·7 | 64·8 | 64·9 | 65·1 | 64·9 | 64·7 |
| Mean days of hospitalization, day | 12·5 | 12·4 | 12·1 | 11·8 | 11·6 | 11·5 | 11·2 | 11·1 | 10·9 | 10·7 | 10·6 | 10·5 | 10·4 | 10·3 |
| Admission of emergency, n | 58960 | 60364 | 62635 | 65978 | 68147 | 70820 | 72665 | 75007 | 79805 | 85942 | 90474 | 94321 | 96731 | 97616 |
| Intervention or examination, n | ||||||||||||||
| Liver transplantation | 619 | 676 | 820 | 774 | 780 | 884 | 840 | 751 | 679 | 665 | 658 | 639 | 560 | 593 |
| Endoscopic banding ligation | 8866 | 9461 | 9924 | 10271 | 10433 | 10921 | 10942 | 11281 | 11365 | 11985 | 12072 | 12452 | 12216 | 12477 |
| Endoscopic injection | 1280 | 1309 | 1188 | 1240 | 1190 | 1135 | 1047 | 972 | 1050 | 1120 | 1080 | 1056 | 1005 | 923 |
| CT scan | 18539 | 19644 | 20728 | 21962 | 23377 | 24366 | 25390 | 26316 | 27249 | 29441 | 30670 | 32771 | 33659 | 34848 |
| MRI/MRCP | 3201 | 3464 | 3619 | 3581 | 4411 | 4512 | 4820 | 5338 | 5772 | 6222 | 6753 | 7069 | 7580 | 7554 |
| Ultrasound | - | - | - | - | - | 1657 | 2342 | 3129 | 3441 | 3965 | 4445 | 4674 | 4763 | 4648 |
| Cirrhosis as comorbidity, n | 82167 | 81247 | 83129 | 84668 | 85860 | 85535 | 86075 | 86979 | 89290 | 94771 | 97582 | 100863 | 101958 | 102293 |
| Main diagnosis, n | ||||||||||||||
| Digestive system | 19667 | 19394 | 20159 | 20331 | 20298 | 20192 | 20186 | 20057 | 21060 | 22053 | 22118 | 22940 | 23245 | 23258 |
| Circulatory | 13318 | 12591 | 12865 | 12994 | 12804 | 13094 | 12803 | 12893 | 13132 | 14444 | 14683 | 15549 | 15502 | 15277 |
| Malignant diseases | 9661 | 9476 | 9163 | 9222 | 9358 | 8958 | 9135 | 8875 | 8857 | 9582 | 10056 | 10468 | 10561 | 10787 |
| Endocrine or metabolic | 4804 | 4831 | 4889 | 5232 | 5223 | 5354 | 5401 | 5543 | 5802 | 5990 | 6375 | 6490 | 6566 | 6826 |
| Diabetes | 2964 | 2887 | 2896 | 3160 | 2888 | 2954 | 3013 | 3071 | 3104 | 3092 | 3322 | 3227 | 3244 | 3232 |
| Respiratory | 2717 | 2610 | 2777 | 2769 | 3081 | 2878 | 3160 | 3126 | 3410 | 3341 | 4088 | 4112 | 4394 | 4547 |
| Cerebrovascular | 1587 | 1523 | 1559 | 1565 | 1504 | 1540 | 1474 | 1385 | 1383 | 1509 | 1483 | 1570 | 1626 | 1474 |
| Ischemic heart | 1491 | 1371 | 1393 | 1510 | 1347 | 1335 | 1288 | 1327 | 1302 | 1451 | 1446 | 1505 | 1516 | 1354 |
| Others | 25958 | 26564 | 27428 | 27885 | 29357 | 29230 | 29615 | 30702 | 31240 | 33309 | 34011 | 35002 | 35304 | 35538 |
| Without cirrhosis, n | ||||||||||||||
| Circulatory | 2516267 | 2534558 | 2597013 | 2643286 | 2672094 | 2726019 | 2767373 | 2832900 | 2788630 | 2866830 | 2872679 | 2910736 | 2892912 | 2827887 |
| Digestive system | 1621834 | 1639516 | 1652877 | 1696852 | 1710885 | 1698107 | 1735044 | 1765672 | 1813867 | 1863939 | 1840426 | 1875522 | 1859518 | 1856262 |
| Malignant diseases | 1456085 | 1454534 | 1471504 | 1479023 | 1449122 | 1448965 | 1460712 | 1450733 | 1431676 | 1454879 | 1449111 | 1465873 | 1476801 | 1487883 |
| Respiratory | 1075358 | 1029648 | 1080397 | 1079970 | 1157563 | 1118214 | 1149096 | 1162191 | 1256621 | 1179368 | 1284314 | 1260095 | 1294206 | 1300602 |
| Ischemic heart | 721586 | 707026 | 697398 | 676767 | 654916 | 659298 | 653779 | 659870 | 646783 | 657877 | 652933 | 654840 | 644003 | 621912 |
| Endocrine or metabolic | 454583 | 464474 | 464949 | 472854 | 487862 | 490677 | 484461 | 488333 | 495766 | 501726 | 511430 | 513693 | 515080 | 527342 |
| Cerebrovascular | 339307 | 343615 | 349763 | 352845 | 351783 | 354722 | 355838 | 358168 | 358186 | 360618 | 363828 | 369055 | 367629 | 362064 |
| Diabetes | 211188 | 211909 | 212312 | 213582 | 211275 | 210976 | 210942 | 210476 | 210503 | 209675 | 206870 | 203814 | 201128 | 199515 |
| Others | 7883762 | 8060607 | 8275002 | 8470151 | 8618416 | 8849692 | 8976822 | 9124505 | 9180006 | 9461449 | 9503525 | 9714640 | 9656799 | 9580932 |
Demographic data of patients admitted with cirrhosis and other categories of diseases
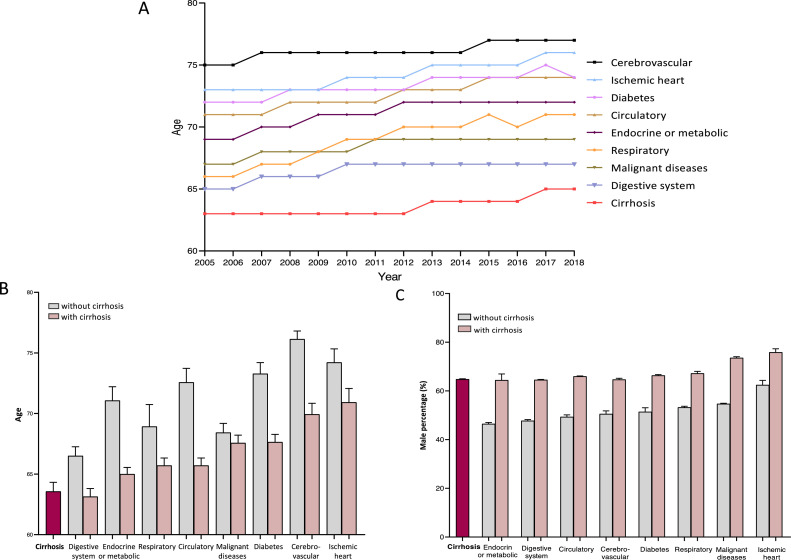
Despite a slight increase in the median age from 2005 (63 years) to 2018 (65 years), patients with cirrhosis had the lowest median age among all categories of chronic diseases (Fig. 2A). Similarly, the age of patients admitted for other categories of chronic diseases significantly decreased if they had concomitant liver cirrhosis (Fig. 2B). Moreover, the majority of patients admitted with cirrhosis was male (64.8%), regardless of comorbidity, and diagnosis of cirrhosis had a higher percentage of male patients (64·8%) among other chronic diseases (Fig 2C, Suppl. Fig. 1A). When comparing patients admitted with other categories of different chronic diseases without cirrhosis, the patients with an additional diagnosis of cirrhosis were significantly more often male (Fig. 2C).
Fig. 2.
Panel A. Median age of patients admitted with liver cirrhosis or admitted with another chronic disease without cirrhosis from 2005 to 2018. Panel B. Median age of patients admitted with chronic diseases with and without additional diagnosis of cirrhosis from 2005 to 2018. Panel C. Percentage of male patients admitted with different chronic diseases with and without additional diagnosis of cirrhosis from 2005 to 2018.
Compared with the demographic data from the European CANONIC (2010-2011) study and the PREDICT (2017-2018) study, we observed a similar trend of a slight increase in male percentage as well as median age from 2010 to 2018, confirming our results (Suppl. Fig. 2 and Suppl. Table 3).
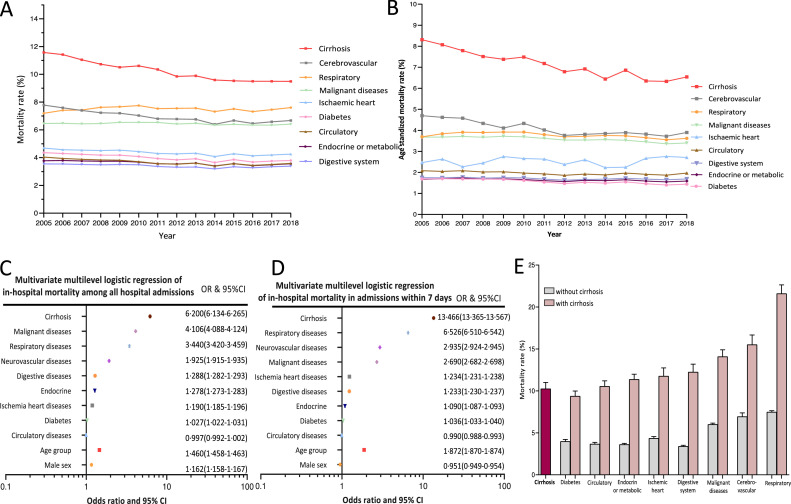
In-hospital mortality of patients admitted with cirrhosis compared to other categories of diseases
Of all patients admitted with liver cirrhosis between 2005 and 2018, regardless of whether cirrhosis or its complications was the main diagnosis [106,094 (9·06%)] or a comorbidity [128,943 (11·40%)], 235,037 (10·21%) died during the respective hospital stay. As shown in Fig. 3A, even though the in-hospital mortality rate of patients admitted with liver cirrhosis decreased from 11·57% in 2005 to 9·49% in 2018, cirrhosis still has by far the highest mortality rate among all categories of chronic diseases (Fig. 3A). Also, the age-standardized mortality rate of cirrhosis is significantly higher than that of other diseases without cirrhosis (Fig. 3B). The mortality rate of other categories of chronic diseases increased at least 2- to 3-fold if cirrhosis was present (Fig. 3E). Among all admissions of patients with cirrhosis, diagnosis of respiratory diseases with infection had the highest mortality rate of 21·61% (without infection: 14.3%), followed by cerebrovascular disease with a rate of 15·53% (Fig. 3E, Table 2 and Suppl. Table 4).
Fig. 3.
Panel A. In-hospital mortality rate of patients admitted with cirrhosis and diagnosis of different chronic diseases without cirrhosis for each year from 2005 to 2018. Panel B. Age-standardized in-hospital mortality rate of patients admitted with cirrhosis and diagnosis of different chronic diseases without cirrhosis for each year from 2005 to 2018. Panel C. Forest plot of odds ratios of cirrhosis as main or secondary diagnosis, and different diagnoses of chronic diseases of in-hospital mortality in all admissions from 2005 to 2018 using multivariate multilevel logistic regression. Panel D. Forest plot of odds ratios of cirrhosis as main or secondary diagnosis, and different diagnoses of chronic diseases of in-hospital mortality in all admissions from 2005 to 2018 using multivariate multilevel logistic regression. Panel E. Mortality rate of patients admitted with different diseases, with and without additional diagnosis of cirrhosis.
Table 2.
Number of hospital deaths due to cirrhosis for each year from 2005 to 2018.
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Digestive system | 12133 | 11968 | 11491 | 11732 | 11787 | 12213 | 11931 | 11775 | 12108 | 12683 | 12925 | 13273 | 13411 | 13248 |
| Circulatory | 11587 | 11382 | 11321 | 11704 | 11831 | 12143 | 12113 | 11919 | 12357 | 12736 | 13215 | 13729 | 13808 | 13897 |
| Endocrine or metabolic | 10414 | 10745 | 11033 | 11244 | 11549 | 12125 | 12313 | 12150 | 12757 | 13321 | 13817 | 14383 | 14453 | 14606 |
| Respiratory | 7044 | 7162 | 7266 | 7674 | 8219 | 8662 | 8839 | 8763 | 9443 | 9851 | 10317 | 10816 | 11152 | 11240 |
| Diabetes | 4073 | 4332 | 4484 | 4490 | 4607 | 4786 | 4887 | 4752 | 4805 | 5037 | 5108 | 5439 | 5378 | 5274 |
| Malignant diseases | 3795 | 3730 | 3652 | 3598 | 3667 | 3737 | 3663 | 3563 | 3496 | 3823 | 3770 | 3899 | 3896 | 3786 |
| Ischemic heart | 2015 | 1865 | 1926 | 1895 | 1981 | 1991 | 2031 | 2037 | 2169 | 2204 | 2383 | 2593 | 2608 | 2581 |
| Cerebrovascular | 1138 | 1071 | 1069 | 1084 | 1006 | 1069 | 1100 | 1016 | 1033 | 1140 | 1149 | 1217 | 1282 | 1265 |
Results of the multivariate multilevel logistic regression of in-hospital mortality between 2005 and 2018 of all admissions in Germany are depicted in Fig. 3C and Suppl. Table 5. Cirrhosis (OR:6·20,95%CI:6·13-6·27]) was found to be a significant independent risk factor of in-hospital mortality among all chronic diseases, followed by malignant diseases (OR:4·11, 95%CI:4·09-4·12) and respiratory diseases (OR: 3·44, 95%CI: 3·42-3·46).
In-hospital mortality of patients admitted with cirrhosis compared to other end-stage diseases and stratified into different length of hospital stay
To compare cirrhosis with other specific end-stage diseases, we have chosen heart failure, renal failure, and chronic obstructive pulmonary disease (COPD). Mortality rate of cirrhosis was also higher than heart failure (8·4%), renal failure (6·4%) and COPD (5·2%), which is consistent with the trends we observed in overall chronic diseases categories (Suppl. Fig. 3). Heart failure, renal failure and COPD were further selected into the multivariate regression model, of which cirrhosis showed the highest OR (8·5) after adjustment for age and gender (Suppl. Table 6).
Notably, more than 70% of admissions of patients had the hospital stay no longer than seven days (Suppl. Fig. 4). A further multilevel logistic regression among admissions within 7 days was performed. Similar results could be observed, whereby cirrhosis still had the highest odds ratio (13·5) (Fig. 3D and Suppl. Table 7).
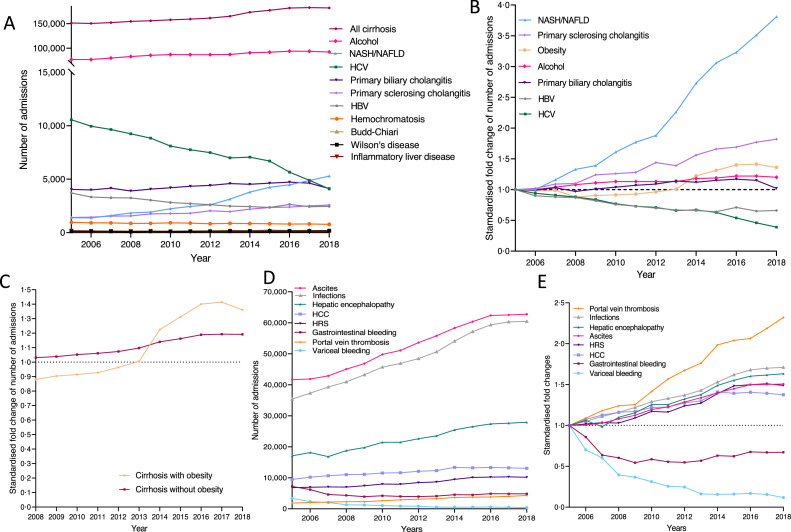
Etiology of liver cirrhosis
As expected, the number of admissions with alcohol-related cirrhosis constitutes the vast majority of etiologies of cirrhosis among all hospital admissions, and it has significantly increased over the years (Fig. 4A and Suppl. Table 8). Table 3 depicts the percentages of hospital admissions with cirrhosis stratified by etiologies. Alcoholic liver cirrhosis accounts for 52% of admissions with cirrhosis. Most frequent non-alcoholic etiologies were chronic HCV infection (4·98%) and primary biliary cirrhosis (2·85%). During the observation time of 14 years, there was a notable decrease in HCV- and hepatitis B virus (HBV) infections as etiologies of cirrhosis (Fig. 4A). Fig. 4B shows the normalized fold change of these etiologies compared to the data of 2005. Among these, NAFLD/NASH increased four-fold in 2018. The number of patients diagnosed with two or more etiologies of cirrhosis account for 2·2%, with a decrease from 3,582 to 3,055. The highest number of admissions was for alcoholic cirrhosis with chronic viral hepatitis (Suppl. Table 9).
Fig. 4.
Panel A. Number of patients admitted with different etiologies of cirrhosis as main diagnosis or comorbidity for each year from 2005 to 2018. Panel B. Fold changes of standardized prevalence of different etiologies of cirrhosis from 2005 to 2018, with year 2005 as reference. Panel C. Fold changes of standardized prevalence of admissions of cirrhosis in patients with and without obesity from 2008 to 2018, with year 2005 as reference. Panel D. Number of different complications in admissions with cirrhosis as main diagnosis or comorbidity for each year from 2005 to 2018. Panel E. Fold changes of standardized prevalence of different complications of cirrhosis from 2005 to 2018, with year 2005 as reference. Abbreviations: HBV, hepatitis B virus; HCC, hepatocellular carcinoma; HCV, hepatitis C virus; HRS, hepatorenal syndrome; NAFLD, non-alcoholic fatty liver disease; NASH, non-alcoholic steatohepatitis.
Table 3.
Percentage of etiologies of admissions with cirrhosis for each year from 2005 to 2018.
| 2005 n=151108 |
2006 n=150227 |
2007 n=151988 |
2008 n=154441 |
2009 n=155693 |
2010 n=157700 |
2011 n=159098 |
2012 n=161163 |
2013 n=164986 |
2014 n=173048 |
2015 n=176991 |
2016 n=181650 |
2017 n=182390 |
2018 n=181688 |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Etiology, % | ||||||||||||||
| Alcohol | 51·03 | 51·38 | 52·68 | 53·9 | 55·1 | 55·3 | 54·7 | 53·9 | 52·9 | 52·6 | 52·0 | 51·8 | 51·5 | 52·3 |
| Chronic HCV | 6·99 | 6·59 | 6·38 | 6·12 | 5·85 | 5·36 | 5·13 | 4·95 | 4·63 | 4·67 | 4·43 | 3·75 | 3·24 | 2·74 |
| Primary biliary cholangitis | 2·67 | 2·64 | 2·75 | 2·58 | 2·69 | 2·78 | 2·87 | 2·93 | 3·04 | 2·99 | 3·06 | 3·13 | 3·06 | 2·73 |
| Chronic HBV | 2·46 | 2·20 | 2·16 | 2·15 | 2·01 | 1·87 | 1·80 | 1·73 | 1·64 | 1·61 | 1·56 | 1·75 | 1·61 | 1·62 |
| Primary sclerosing Cholangitis | 0·94 | 0·96 | 1·02 | 1·03 | 1·16 | 1·18 | 1·20 | 1·35 | 1·30 | 1·46 | 1·56 | 1·58 | 1·66 | 1·71 |
| NAFLD | 0·80 | 0·83 | 0·97 | 1·11 | 1·16 | 1·26 | 1·37 | 1·40 | 1·72 | 2·04 | 2·24 | 2·34 | 2·55 | 2·78 |
| Hemochromatosis | 0·64 | 0·61 | 0·60 | 0·58 | 0·57 | 0·61 | 0·59 | 0·55 | 0·57 | 0·57 | 0·55 | 0·53 | 0·54 | 0·51 |
| NASH | 0·13 | 0·09 | 0·10 | 0·12 | 0·13 | 0·23 | 0·28 | 0·35 | 0·37 | 0·50 | 0·61 | 0·65 | 0·72 | 0·76 |
| Inflammatory liver disease | 0·13 | 0·10 | 0·10 | 0·10 | 0·10 | 0·07 | 0·07 | 0·08 | 0·07 | 0·07 | 0·06 | 0·07 | 0·06 | 0·06 |
| Budd-Chiari syndrome | 0·09 | 0·08 | 0·11 | 0·10 | 0·10 | 0·10 | 0·10 | 0·12 | 0·14 | 0·12 | 0·16 | 0·13 | 0·14 | 0·13 |
| Wilson's disease | 0·08 | 0·08 | 0·08 | 0·06 | 0·08 | 0·07 | 0·08 | 0·09 | 0·10 | 0·10 | 0·10 | 0·11 | 0·11 | 0·12 |
Abbreviations: HBV, hepatitis B virus; HCV, hepatitis C virus; NAFLD, non-alcoholic fatty liver disease; NASH, non-alcoholic steatohepatitis·
Alcoholic cirrhosis and HBV-related cirrhosis patients constituted the highest percentage of male patients among all etiologies of cirrhosis (Suppl. Fig. 1B). Similarly, although the mean age showed a significant increase, patients with alcohol use disorder were still markedly younger than patients with other etiologies of cirrhosis (Suppl. Fig. 1C and D).
Interestingly, the number of admissions with obesity increased substantially from 2008 to 2017, from 0·88- to 1·41-fold compared to 2005 (Fig. 4C). In 2008, 5,866 admissions of patients with liver cirrhosis and obesity were reported, while the number of admissions with liver cirrhosis and obesity had more than doubled by 2018 (12,108) (Fig. 4B and Fig. 4C). Suppl. Fig. 5A shows the BMI distribution in each category of hospital admission with liver cirrhosis and obesity. The proportion of BMI>40 had increased to 27% in 2018. In addition, patients recruited in Germany in the CANONIC and PREDICT studies had a similar etiology distribution to Northern or Central Europe, while slight differences were noticed compared to Southern and Eastern Europe, as highlighted in Suppl. Table 3.
Suppl. Fig. 5B shows the mean hospitalization days of admissions of patients with alcoholic and non-alcoholic cirrhosis. Despite a significant decrease from 2005 to 2018, the mean hospital stay of patients admitted with alcoholic cirrhosis (12·8 days in 2005 to 9·8 days in 2018) was significantly longer than that of patients diagnosed with cirrhosis with other etiologies (12·6 days in 2005 to 8·5 days in 2018). Similarly, patients with alcohol use disorder (11·5% in 2005 to 10·1% in 2018) patients were associated with a significantly higher in-hospital mortality rate than other etiologies (11·3% in 2005 to 8·8% in 2018) (Suppl. Fig. 5C).
Complications of liver cirrhosis
The most common complication of liver cirrhosis leading to hospitalization was ascites (34·75%) (Table 4) and the number of admissions with ascites significantly increased from 41,627 to 62,794 during the observed years (Fig. 4D and Suppl. Table 10). Hepatic encephalopathy and infection were the second and third most common complications of liver cirrhosis. Additionally, infections were found to be independent risk factor of in-hospital mortality (OR: 4·746) (Suppl. Table 5).
Table 4.
Percentage of complications of admissions with liver cirrhosis for each year from 2005 to 2018.
| Complications, % | 2005 n=151108 |
2006 n=150227 |
2007 n=151988 |
2008 n=154441 |
2009 n=155693 |
2010 n=157700 |
2011 n=159098 |
2012 n=161163 |
2013 n=164986 |
2014 n=173048 |
2015 n=176991 |
2016 n=181650 |
2017 n=182390 |
2018 n=181688 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anemia | 28·90 | 29·21 | 29·39 | 30·50 | 30·94 | 31·14 | 31·22 | 30·98 | 31·50 | 32·55 | 32·96 | 33·75 | 34·07 | 34·20 |
| Ascites | 27·58 | 27·72 | 28·37 | 29·81 | 31·00 | 32·95 | 33·80 | 35·48 | 36·93 | 38·59 | 39·96 | 41·29 | 41·40 | 41·56 |
| Hepatic encephalopathy | 11·31 | 12·00 | 11·14 | 12·43 | 13·07 | 14·19 | 14·20 | 14·97 | 15·57 | 16·85 | 17·55 | 18·13 | 18·29 | 18·46 |
| Infections | 9·77 | 9·90 | 10·12 | 10·29 | 11·19 | 11·68 | 11·89 | 12·20 | 13·07 | 13·63 | 14·61 | 15·40 | 15·69 | 15·61 |
| Portal hypertension | 7·51 | 7·32 | 7·19 | 8·16 | 8·29 | 8·44 | 9·25 | 9·83 | 10·16 | 11·43 | 11·98 | 12·60 | 12·55 | 12·69 |
| Hepatocellular carcinoma | 6·28 | 6·75 | 7·07 | 7·29 | 7·35 | 7·65 | 7·69 | 8·02 | 8·16 | 8·84 | 8·75 | 8·82 | 8·74 | 8·63 |
| Gastrointestinal bleeding | 4·77 | 4·09 | 3·04 | 2·88 | 2·59 | 2·79 | 2·65 | 2·61 | 2·71 | 3·01 | 2·97 | 3·23 | 3·20 | 3·20 |
| Hepatorenal syndrome | 4·52 | 4·60 | 4·67 | 4·65 | 4·93 | 5·29 | 5·25 | 5·59 | 5·75 | 6·27 | 6·70 | 6·77 | 6·82 | 6·73 |
| Jaundice | 2·22 | 1·98 | 1·52 | 1·40 | 1·41 | 1·46 | 1·39 | 1·39 | 1·57 | 1·59 | 1·53 | 1·66 | 1·65 | 1·67 |
| Esophageal variceal bleeding | 2·21 | 1·55 | 1·33 | 0·87 | 0·81 | 0·69 | 0·56 | 0·54 | 0·36 | 0·35 | 0·35 | 0·37 | 0·34 | 0·26 |
| Portal-vein thrombosis | 1·22 | 1·33 | 1·44 | 1·51 | 1·53 | 1·73 | 1·92 | 2·04 | 2·15 | 2·43 | 2·49 | 2·52 | 2·67 | 2·84 |
Fig. 4E shows the fold changes of standard prevalence of different complications of liver cirrhosis, with the year 2005 as reference. Gastrointestinal bleeding in general (0·7) and variceal bleeding in particular (0·1) decreased markedly to only one-tenth from 2005 to 2018. However, diagnosis of portal vein thrombosis (2·3) doubled during the observation period of 14 years. Notably, the number of imaging examinations increased in parallel with the increased diagnosis rate of portal vein thrombosis. In particular, the number of CT scans has increased from 18,539 to 34,848 (Table 1 and Suppl. Fig. 6). All other complications experienced substantial changes, including hepatic encephalopathy, infections, ascites, hepatorenal syndrome and hepatocellular carcinoma.
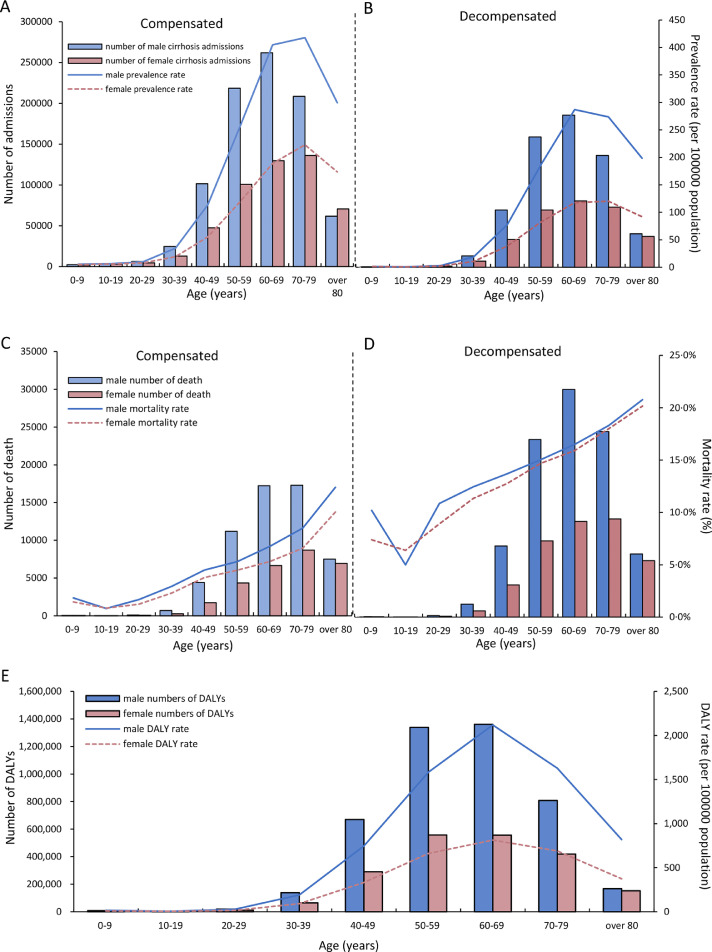
Prevalence, mortality and DALYs of compensated and decompensated cirrhosis admissions in age and sex groups
Interestingly, male patients with liver cirrhosis had not only a higher number of admissions during the observation period of 14 years, but also a higher prevalence rate of 158 per 100,000 population in compensated as well as a higher prevalence rate of 108 per 100,000 population in decompensated cirrhosis (Fig. 5A and Fig. 5B). The highest number of cirrhosis admissions was observed in male patients aged 60-69 (261,799 with compensated and 184,399 with decompensated cirrhosis), followed by patients aged 50-59 years (218,519 with compensated and 157,914 with decompensated cirrhosis). Importantly, male patients in the age group 50-69 years accounted for 34·4% and 54·2% of all admissions with compensated and decompensated cirrhosis, respectively. Although male patients had a slightly higher mortality rate than female patients (67% of deaths were in male patients), which, as expected, increased with age, they had more than twice the number of deaths compared to female patients, both with compensated as well as decompensated liver cirrhosis (Fig. 5C and D).
Fig. 5.
Panel A. Number of admissions and prevalence rate per 100,000 population of compensated cirrhosis in male and female patients in different age groups. Panel B. Number of admissions and prevalence rate per 100,000 population of male and female decompensated cirrhosis patients in different age groups. Panel C. Number of deaths and in-hospital mortality rate of compensated cirrhosis in male and female patients in different age groups. Panel D. Number of deaths and in-hospital mortality rate of decompensated cirrhosis in male and female patients in different age groups. Panel E. Number of DALYs and DALY rate per 100,000 population of cirrhosis in male and female patients in different age groups. Abbreviations: DALYs, disability-adjusted life years.
The total number of DALYs in admissions of male and female patients with cirrhosis in all age groups over the observed period of 14 years was approx. 6·8 million. The highest number of DALYs was observed in admissions of male patients aged 50-59 (1·34 million) and 60-69 (1·36 million) years (Fig. 5E). Thus, male patients aged 50-69 years accounted for almost half of the number of DALYs of liver cirrhosis. Admissions of male cirrhosis patients aged 60-69 years had the highest DALY rate of 2117·75 per 100,000 population.
Discussion
The present study demonstrates that despite considerable efforts, cirrhosis represents a heavy disease burden with a strong impact on the health care system. In-hospital mortality was far higher in patients admitted with liver cirrhosis compared to other chronic diseases. Thereby, it is not relevant whether cirrhosis is the primary diagnosis or just a comorbidity at admission. The study also indicates that great progress has been made in terms of treatment of viral liver diseases and gastrointestinal bleeding leading to a changed landscape of liver disease etiology and its complications. On the other hand, alcoholic liver cirrhosis remains by far the most common etiology of cirrhosis, mostly with complications such as ascites, infections, and organ dysfunctions (hepatic encephalopathy and hepatorenal syndrome), one explanation why decompensation in end-stage liver disease and acute-on-chronic liver failure are on the rise.
Compared to other chronic diseases in Germany, patients admitted to hospital with liver cirrhosis were younger, with a median age of 63 years. Results from the United States shows that while prevalence of liver cirrhosis increases with age, it did so with a bimodal age distribution in the forties and at age 75.16 Our study demonstrates that the European demography of cirrhosis patients is considerably different compared to the United States, although sex distribution was similar, with male patients predominating in both regions.16 In our study, we also compared the demographic data to the CANONIC (2010-2011) and the PREDICT study (2017-2018), which consist of almost 3,000 patients from different centers across Europe.12, 13, 14 Particularly, the demographic (age and sex) and etiologies trends in Germany from 2010 to 2018 was similar to the trend of other European countries described in these studies, which supports the findings of our study and suggests that to some extent, these findings represent the European population beyond Germany.
Interestingly, despite the demographic differences observed between Europe and the United States,3 the number of deaths is higher in patients in their fifties, which is responsible for the increase of DALYs, especially in young male patients, as observed in our study. Therefore, our study highlights the fact that cirrhosis is associated with higher mortality in younger males, especially when combined with extrahepatic diseases. In addition, the socio-economic burden of cirrhosis is significant, since young males still dominate the labor force in Europe.17 Our study advocates for more focused efforts on cirrhosis and raises a clear alarm signal for the health care system. Therefore, prevention and treatment of complications in cirrhosis are anticipated to prevent morbidity and mortality, with a strong impact on society and economy.
Another surprising finding was that in the majority (>50%) of hospital admissions with cirrhosis or its complications, liver cirrhosis was not the primary diagnosis for the hospital admissions of patients, but only a comorbidity. This underlines the fact that liver cirrhosis plays an important role as a comorbidity. Patients with chronic liver disease and especially cirrhosis are excluded from many studies and new drug trials.18 The reasons are diverse, but one is that medication in these patients could be associated with adverse outcome. Although overall mortality of liver cirrhosis has slightly decreased the last decade, cirrhosis still constitutes a major risk factor for mortality. We found that concomitant liver cirrhosis has a huge impact on mortality of other chronic diseases independent of other risk factors, such as age, sex, or other comorbidities. Cirrhosis was found to be an independent risk factor for hospital death for patients. This has not been described previously, since studies have only demonstrated that liver cirrhosis, as a comorbidity of other chronic diseases, only leads to higher readmission rates.19 Our data demonstrate that cirrhosis increases mortality especially in the chronic diseases of younger patients.
This study demonstrates a clear etiologic change in cirrhosis over recent years, at least in Germany. The prevalence of HBV and HCV has dropped due to vaccination and direct-acting antivirals.20,21 The decrease in HCV is especially remarkable and key achievements in this field were awarded with the 2020 Nobel prize for medicine.22 Alcohol, the most prevalent known etiology of cirrhosis in Europe,3 remains the big challenge in liver disease with a notable increase from 2005 to 2018 in Germany, used as an example for Central Europe. The increasing number of patients admitted with NAFLD and NASH and cirrhosis is evident in Germany and it goes in parallel with demographic changes in other parts of the world. These etiological changes were observed and confirmed when comparing findings with those from the CANONIC and PREDICT studies.12, 13, 14 In the past 20 years, NASH and NAFLD have attracted significant attention from the pharmaceutical industry. Our data show that, at least in Germany, admissions from 2005 to 2018 with NASH or NAFLD experienced the highest fold change of more than four times among all etiologies of cirrhosis. Our study emphasizes the importance of metabolic diseases on admission with cirrhosis. This factor is underlined by the increasing obesity in patients with liver cirrhosis as shown in our study. Clearly, obesity increases the risk of other comorbidities, such as diabetes and cardiovascular diseases, and, therefore, may be one reason for the increasing number of admissions with cirrhosis as a comorbidity. Insufficient preventive measures and lack of convincing treatment may also explain the rapid increase of cirrhosis associated with NAFLD/NASH.
Our study demonstrates another remarkable and positive development, namely that admissions for gastrointestinal bleeding have considerably decreased over time. In addition to HCV treatment, this is the second major achievement in the standard of care, probably due to the continuous implementation of the Baveno criteria in the German national guidelines and daily practice.23,24
Surprisingly, the diagnosis of portal vein thrombosis of the liver in cirrhosis increased over the observed period, possibly due to increased awareness for this diagnosis and improvements in quality and ability of imaging. However, the diagnosis of HCC also increased, which is probably due to the implementation of surveillance strategies in daily practice and national guidelines.25,26 Similarly, the steep increase in diagnosis of sarcopenia is probably due to the increased awareness of its important role on survival of cirrhotic patients.27 Both findings are important and demonstrate improvements in standard of care, since early detection of thrombosis as well as HCC have a significant impact on disease outcome, especially when effective treatments of these two complications are implemented at an early stage.
The decrease observed in HCV-related cirrhosis and variceal bleeding, as well as early diagnosis of HCC (and possible also portal vein thrombosis) may be reasons as to why mortality has slightly decreased over the observed time period of 14 years. However, the number of hospital admissions with ascites shows a significantly increasing trend, accounting for the majority of reported complications of cirrhosis.28 Similar to ascites, as a definitive sign of decompensation, other surrogates of organ dysfunction, such as hepatic encephalopathy or hepatorenal syndrome, have also been increasing over time. These data suggest that acute decompensation and its maximal form, acute-on-chronic liver failure, are possible reasons for the increased number of admissions and the still very high mortality rate in patients admitted with cirrhosis during the study period. This hypothesis is clearly supported by the increasing rate of admissions for alcoholic cirrhosis and of patients admitted with infections, since severe alcoholic hepatitis and proven bacterial infection accounted for 96% of the precipitating events that could be determined in acute decompensations and acute-on-chronic liver failure in the recently published PREDICT study.12 Thus, metabolic cirrhosis, especially due to alcohol use disorder, infections, complications of liver cirrhosis, especially ascites, and acute-on-chronic liver failure constitute the most prominent current challenges for cirrhosis in Germany, and probably also worldwide.
There were obvious regional differences in the development and mortality rate of liver cirrhosis across the different federal states of Germany. The hospitalization rate and the in-hospital mortality rate of liver cirrhosis were both generally higher in East German federal states than in West German federal states. These differences may be due to social and economic reasons.29,30 The described lower medical resource distribution and lower number of physicians in East German federal states could be contributing factors for this regional distribution.31
Although our research has revealed extensive and valuable information on hospitalized patients with liver cirrhosis in Germany and thus may provide a reference for an improved allocation of medical resources in Europe, several limitations need to be considered. Given that our analyses were all based on the ICD-10 codes completed by the responsible physician in the individual hospitals, this may have inherent limitations due to inaccuracy, as well as reporting bias due change of diagnostic means and awareness for certain features of liver cirrhosis, especially in the first period described in this study. However, it has been previously shown that ICD-10 codes for cirrhosis and its complications are reliable and accurate.32,33 Furthermore, documentation of every accurate coding and financial auditing process are required for reimbursement.15 Another limitation is that our study could not capture the course of a single patient either before or after hospital admission. Finally, other potentially relevant clinical features without a specific ICD-10 code are only indirectly reflected in our analysis.
To conclude, this nationwide population-based study shows the significant disease burden of liver cirrhosis including high prevalence rate, DALYs, in-hospital mortality rate, especially in younger male admissions, and co-existing chronic diseases. Our study reveals beneficial trends and evolutions in the natural course of liver cirrhosis, especially due to decreased HCV infections, decreased rate of gastrointestinal bleeding, and slightly lower in-hospital mortality rate. It also identifies the emerging fields where health policy and service provider need to invest, namely metabolic cirrhosis, especially of alcoholic etiology, acute decompensation, and acute-on-chronic liver failure. More importantly, we clearly demonstrate the neglected role of liver cirrhosis concomitant to other chronic diseases. This should be taken into account in drug trials performed for other chronic diseases.
Financial support
Jonel Trebicka is supported by grants from the Deutsche Forschungsgemeinschaft (SFB TRR57 to P18, CRC 1382AO9), European Union's Horizon 2020 Research and Innovation Programme (Galaxy, No. 668031, MICROB-PREDICT, No. 825694 and DECISION, No.847949), and Societal Challenges - Health, Demographic Change and Wellbeing (No. 731875), and Cellex Foundation (PREDICT). Wenyi Gu is supported by the China Scholarships Council (CSC: #201906230332). The funders had no influence on study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Author contributions
JT: study concept and design, acquisition of data, analysis, and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, statistical analysis, obtained funding, technical or material support, and study supervision.
WG, HH and HPE: acquisition of data, analysis, and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content, statistical analysis, obtained funding, and technical as well as material support.
LS, YZ, FEU, PF, MS, KHP, AQ, TS, MJB, GR, CS, RM, VA, SZ and CW acquisition of data, interpretation of data and critical revision of the manuscript for important intellectual content.
Declaration of interests
Jonel Trebicka has received speaking and/or consulting fees from Gore, Bayer, Alexion, MSD, Gilead, Intercept, Norgine, Grifols, Versantis, and Martin Pharmaceutical. Philip Ferstl received consultancy for SNIPR Biome. S. Zeuzem received consulting and/or lecture fees from Bayer Health Care and consultancies for AbbVie, BMS, Gilead, Janssen, Merck.
Acknowledgement
The authors would like to thank Sabine Dentler for her critical revision of the manuscript.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanepe.2021.100240.
Contributor Information
Wenyi Gu, Email: wenyi.gu@kgu.de.
Hannah Hortlik, Email: h.hortlik@gmx.de.
Hans-Peter Erasmus, Email: hans-peter.erasmus@kgu.de.
Louisa Schaaf, Email: louisaschaaf@web.de.
Yasmin Zeleke, Email: zeleke.yasmin@gmail.com.
Frank E. Uschner, Email: frank.uschner@kgu.de.
Philip Ferstl, Email: philip.ferstl@kgu.de.
Martin Schulz, Email: martin.schulz2@kgu.de.
Kai-Henrik Peiffer, Email: kai-henrik.peiffer@kgu.de.
Alexander Queck, Email: alexander.queck@kgu.de.
Tilman Sauerbruch, Email: tilman.sauerbruch@ukbonn.de.
Maximilian Joseph Brol, Email: maximilian.brol@kgu.de.
Gernot Rohde, Email: gernot.rohde@kgu.de.
Cristina Sanchez, Email: cristina.sanchez@efclif.com.
Richard Moreau, Email: richard.moreau@inserm.fr.
Vicente Arroyo, Email: vicente.arroyo@efclif.com.
Stefan Zeuzem, Email: stefan.zeuzem@kgu.de.
Christoph Welsch, Email: christoph.welsch@kgu.de.
Jonel Trebicka, Email: jonel.trebicka@kgu.de.
Appendix. Supplementary materials
References
- 1.D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44(1):217–231. doi: 10.1016/j.jhep.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 2.Mokdad AA, Lopez AD, Shahraz S, et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med. 2014;12:145. doi: 10.1186/s12916-014-0145-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5(3):245–266. doi: 10.1016/S2468-1253(19)30349-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blachier M, Leleu H, Peck-Radosavljevic M, Valla DC, Roudot-Thoraval F. The burden of liver disease in Europe: a review of available epidemiological data. J Hepatol. 2013;58(3):593–608. doi: 10.1016/j.jhep.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 6.Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70(1):151–171. doi: 10.1016/j.jhep.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 7.Tsochatzis EA, Bosch J, Burroughs AK. Liver cirrhosis. Lancet. 2014;383(9930):1749–1761. doi: 10.1016/S0140-6736(14)60121-5. [DOI] [PubMed] [Google Scholar]
- 8.Williams R, Aspinall R, Bellis M, et al. Addressing liver disease in the UK: a blueprint for attaining excellence in health care and reducing premature mortality from lifestyle issues of excess consumption of alcohol, obesity, and viral hepatitis. Lancet. 2014;384(9958):1953–1997. doi: 10.1016/S0140-6736(14)61838-9. [DOI] [PubMed] [Google Scholar]
- 9.Sheka AC, Adeyi O, Thompson J, Hameed B, Crawford PA, Ikramuddin S. Nonalcoholic steatohepatitis: a review. Jama. 2020;323(12):1175–1183. doi: 10.1001/jama.2020.2298. [DOI] [PubMed] [Google Scholar]
- 10.Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73(1):202–209. doi: 10.1016/j.jhep.2020.03.039. [DOI] [PubMed] [Google Scholar]
- 11.Kabbany MN, Conjeevaram Selvakumar PK, Watt K, et al. Prevalence of nonalcoholic steatohepatitis-associated cirrhosis in the United States: an analysis of national health and nutrition examination survey data. Am J Gastroenterol. 2017;112(4):581–587. doi: 10.1038/ajg.2017.5. [DOI] [PubMed] [Google Scholar]
- 12.Trebicka J, Fernandez J, Papp M, et al. PREDICT identifies precipitating events associated with the clinical course of acutely decompensated cirrhosis. J Hepatol. 2020 doi: 10.1016/j.jhep.2020.11.019. [DOI] [PubMed] [Google Scholar]
- 13.Moreau R, Jalan R, Gines P, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology. 2013;144(7):1426–1437. doi: 10.1053/j.gastro.2013.02.042. 37.e1-9. [DOI] [PubMed] [Google Scholar]
- 14.Trebicka J, Fernandez J, Papp M, et al. The PREDICT study uncovers three clinical courses of acutely decompensated cirrhosis that have distinct pathophysiology. J Hepatol. 2020;73(4):842–854. doi: 10.1016/j.jhep.2020.06.013. [DOI] [PubMed] [Google Scholar]
- 15.Reutersberg B, Salvermoser M, Trenner M, et al. Hospital incidence and In-hospital mortality of surgically and interventionally treated aortic dissections: secondary data analysis of the Nationwide German Diagnosis-Related Group Statistics From 2006 to 2014. J Am Heart Assoc. 2019;8(8) doi: 10.1161/JAHA.118.011402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scaglione S, Kliethermes S, Cao G, et al. The epidemiology of cirrhosis in the United States: a population-based study. J Clin Gastroenterol. 2015;49(8):690–696. doi: 10.1097/MCG.0000000000000208. [DOI] [PubMed] [Google Scholar]
- 17.World bank. Germany Labor Force Employment | Moody's Analytics. 2020. https://data.worldbank.org/indicator/SP.POP.DPND.OL?locations=DE.
- 18.Loomba R, Wong R, Fraysse J, et al. Nonalcoholic fatty liver disease progression rates to cirrhosis and progression of cirrhosis to decompensation and mortality: a real world analysis of Medicare data. Aliment Pharmacol Ther. 2020;51(11):1149–1159. doi: 10.1111/apt.15679. [DOI] [PubMed] [Google Scholar]
- 19.Rosenblatt R, Cohen-Mekelburg S, Shen N, et al. Cirrhosis as a comorbidity in conditions subject to the hospital readmissions reduction program. Am J Gastroenterol. 2019;114(9):1488–1495. doi: 10.14309/ajg.0000000000000257. [DOI] [PubMed] [Google Scholar]
- 20.Spearman CW, Dusheiko GM, Hellard M, Sonderup M. Hepatitis C. Lancet. 2019;394(10207):1451–1466. doi: 10.1016/S0140-6736(19)32320-7. [DOI] [PubMed] [Google Scholar]
- 21.Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ. Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013. Lancet. 2015;386(10003):1546–1555. doi: 10.1016/S0140-6736(15)61412-X. [DOI] [PubMed] [Google Scholar]
- 22.NobelPrize.org; 2020. The Nobel Prize in Physiology or Medicine 2020. For the discovery of Hepatitis C virus. [Google Scholar]
- 23.de Franchis R. Expanding consensus in portal hypertension: report of the Baveno VI consensus workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63(3):743–752. doi: 10.1016/j.jhep.2015.05.022. [DOI] [PubMed] [Google Scholar]
- 24.Götz M, Anders M, Biecker E, et al. [S2k Guideline gastrointestinal bleeding - guideline of the German Society of Gastroenterology DGVS] Z Gastroenterol. 2017;55(9):883–936. doi: 10.1055/s-0043-116856. [DOI] [PubMed] [Google Scholar]
- 25.Francoz C, Valla D, Durand F. Portal vein thrombosis, cirrhosis, and liver transplantation. J Hepatol. 2012;57(1):203–212. doi: 10.1016/j.jhep.2011.12.034. [DOI] [PubMed] [Google Scholar]
- 26.Qi X, Han G, Fan D. Management of portal vein thrombosis in liver cirrhosis. Nat Rev Gastroenterol Hepatol. 2014;11(7):435–446. doi: 10.1038/nrgastro.2014.36. [DOI] [PubMed] [Google Scholar]
- 27.EASL clinical practice guidelines on nutrition in chronic liver disease. J Hepatol. 2019;70(1):172–193. doi: 10.1016/j.jhep.2018.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53(3):397–417. doi: 10.1016/j.jhep.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 29.Weiss J. [Medical health care in Germany - large regional differences] Dtsch Med Wochenschr. 2011;136(6):4. doi: 10.1055/s-0031-1271822. [DOI] [PubMed] [Google Scholar]
- 30.Göpffarth D, Kopetsch T, Schmitz H. Determinants of regional variation in health expenditures in Germany. Health Econ. 2016;25(7):801–815. doi: 10.1002/hec.3183. [DOI] [PubMed] [Google Scholar]
- 31.Augurzky B, Kopetsch T, Schmitz H. What accounts for the regional differences in the utilisation of hospitals in Germany? Eur J Health Econ. 2013;14(4):615–627. doi: 10.1007/s10198-012-0407-6. [DOI] [PubMed] [Google Scholar]
- 32.Lapointe-Shaw L, Georgie F, Carlone D, et al. Identifying cirrhosis, decompensated cirrhosis and hepatocellular carcinoma in health administrative data: a validation study. PLoS One. 2018;13(8) doi: 10.1371/journal.pone.0201120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mapakshi S, Kramer JR, Richardson P, El-Serag HB, Kanwal F. Positive predictive value of international classification of diseases, 10th revision, codes for cirrhosis and its related complications. Clin Gastroenterol Hepatol. 2018;16(10):1677–1678. doi: 10.1016/j.cgh.2018.01.042. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.