Abstract
AIM
To investigate and compare the quality of life, satisfaction, contrast sensitivity, glare, depth perception, and intraocular lens (IOL) rotation in patients who underwent trifocal toric and bifocal toric IOLs.
METHODS
A total of 80 eyes of 40 patients were included in this prospective study. Twenty patients in each group were implanted with trifocal toric and bifocal toric IOL, respectively. Preoperative and postoperative 6-month measurements were recorded for both patient groups. Comprehensive anterior and posterior segment examinations, distance-intermediate-near visual acuity values and the visual function scale questionnaire results were evaluated at these examinations. Patient satisfaction, contrast sensitivity, glare, intermediate-near and distance stereopsis and IOL rotation were also evaluated.
RESULTS
No significant difference was found between the groups in terms of distance and near visual acuities (P=0.269, P=0.451). Intermediate visual acuity was significantly increased in the trifocal toric group (P<0.001). The visual function scale results were increased after surgery in both groups (P=0.001 and P<0.001), with no difference determined between them (P=0.158 and P=0.691). The number of patients wearing glasses was low in both groups and there was no significant difference between the groups (P>0.05). The overall satisfaction in the trifocal toric group was significantly higher than in the bifocal toric group (P=0.03). The highest sensitivity was observed at 6 cpd spatial frequency in all patients under photopic conditions (1.80±0.24 logU, 1.74±0.20 logU). Distance-intermediate-near binocular depth perception results in both groups were higher in the trifocal toric group (P=0.02, 0.048, 0.003, respectively). Although there was no significant difference for 3 meters stereopsis, the trifocal toric group had higher depth perception (P=0.577). Mean rotation was 5.76°±3.93° in the trifocal toric group and 12°±7.1° in the bifocal toric group.
CONCLUSION
Better results in the middle distance are obtained in the trifocal toric group and less IOL rotation due to digital system-coordinated surgery. Moreover, the overall satisfaction in the trifocal toric group is significantly higher than in the bifocal toric group.
Keywords: cataract, trifocal toric intraocular lens, bifocal toric intraocular lens, stereopsis, satisfaction
INTRODUCTION
Cataract surgery improves vision and refractive defects can also be corrected during surgery. Modern phacoemulsification surgery and recently developed intraocular lenses (IOLs) have increased the visual expectations of patients[1]. Conventional spherical monofocal and bifocal lenses provide a significant increase in visual acuity, visual satisfaction and a reduction in eyeglasses dependence, but not in patients with high corneal astigmatism[2]. Nearly 22% of patients with cataract have ≥1.50 D corneal astigmatism[3]. Although some methods such as corneal incision to the vertical axis and limbal relaxation incisions have been used for the correction of astigmatism during cataract surgery, limited and unpredictable improvements are obtained with these methods due to individual differences in the incision site healing process and surgeon factor[4]–[5]. Toric IOLs are predictable convenient options for the correction of astigmatic refractive defects in patients who don't prefer to wear glasses after cataract surgery[6]–[7].
Trifocal toric lenses have a semi-apodization mechanism (regulates optical crusher for distance-intermediate-near) and enhanced focus of depth (EDOF). These lenses also correct ≥1.00 D corneal astigmatism by toric attachment on their optics. Thus, these lenses aim to obtain best and smooth visual acuity without glasses at distance (6 m and far), intermediate (80 cm) and near (40 cm). Bifocal toric lenses are also preferable options due to satisfactory results at distance-intermediate-near[8], the surgical procedure is safer and successful vision is obtained[9]. Trifocal toric IOL is an alternative option in appropriate patients due to a low residual astigmatism value after cataract surgery and satisfactory functional results in distance-intermediate-near, thereby improving quality of life[10]–[11]. In addition, functional success has been found to be higher in surgeries where rotation of the implanted toric IOL is ≤5° [12]. Glasses dependence after cataract surgery has become almost eliminated with the introduction of trifocal toric lenses[13]–[14]. These lenses can provide high-performance vision at both near and mid distance without affecting distance vision[15]. Significant improvement in quality of daily life are achieved with this gain in intermediate vision[16].
The aim of this study was to investigate and compare quality of life, satisfaction, contrast sensitivity, glare, depth perception, and IOL rotation levels of patients implanted with Acriva Trifocal toric IOL and Acriva bifocal toric IOL.
SUBJECTS AND METHODS
Ethical Approval
The study was conducted according to the principles of the Declaration of Helsinki and approval was obtained from the Ethics Committee of Eskisehir Osmangazi University (No.80558721/122). The Universal Trial Number (UTN): U1111-1264-1020. The informed consent was obtained from the subjects.
The study included 40 patients who were admitted to Eskisehir Osmangazi University Faculty of Medicine Ophthalmology Department between September 2016 and May 2017 with low vision in both eyes and best corrected distance visual acuity (CDVA) of ≤0.5 according to Snellen chart examination. Patients were excluded from the study if they had diabetes mellitus, hypertension, optic neuritis, glaucoma, diabetic retinopathy, age-related macular degeneration, pseudoexfoliation, pterygium, strabismus, corneal nephelion, or a history of ophthalmic surgery. Patients were randomly divided into two groups. A total of 20 eyes of patients with corneal astigmatism of ≥1.00 underwent cataract surgery and the VERION digital microscope-mounted marking system was applied to both eyes with Acriva Reviol tri-ED trifocal toric IOL (Amsterdam, the Netherlands). The other 20 patients underwent cataract surgery and Acriva Reviol bifocal toric IOL (Amsterdam, the Netherlands) was implanted with the conventional corneal marking method. These trifocal toric and bifocal toric IOLs hydrophobic, acrylic and contains 25% water. These IOLs have same optic and haptic diameter, 6 and 11 mm respectively. Both IOLs designs are plate haptic. All ophthalmological examinations of the patients were performed preoperatively and postoperatively by the same examiner. The measurements of IOL rotation and others were performed at operative time and postoperative 1st day, 1st week, 1st-3rd-6th months. Refraction and intraocular pressure (IOP; NIDEK Tonoref II device, 2015, Maehama, Hiroishi, Gamagori, Aichi, Japan) were measured. In both groups, the best uncorrected and corrected distance visual acuities (UDVA and CDVA) were measured at a distance of 6 m with logMAR visual chart. The best uncorrected and corrected intermediate visual acuities (UIVA and CIVA) were determined at a distance of 80 cm with the logMAR near vision chart, and the best uncorrected and corrected near visual acuities (UNVA and CNVA) were measured at a distance of 40 cm. Anterior and posterior segment examinations (tropicamide drops 1%) were performed in all patients. Anterior segment photographs (Topconsl-D7, SN: 1613331, Japan) and macular optical coherence tomography (Zeiss Cirrus HD) images were taken and fundus photographs were recorded with Optos 200Tx. Corneal astigmatism and Kappa angle (Haag-Streit LensstarLS900) were measured and patients with corneal astigmatism of ≥1.00 D and Kappa angle of ≤0.40 were included in the study. Astigmatic axes not evaluated. In both groups, Haag-Streit T-Cone was added to the Lensstar LS 900 for the IOL spherical and cylindrical powers of the patients. To determine the spherical power of IOL, emmetropia was aimed for using SRK-T and Barret formulas. Cylindrical power was calculated using the online module at http://easytoriccalculator.com/acriva.php?lang=en. The NEI-VFQ-25 Visual Function Questionnaire, comprising 25 questions[17], was applied to patients to measure quality of life preoperatively and postoperatively.
In addition to preoperative measurements of the trifocal toric patient group, the Alcon VERION Digital Microscope Mounted Marking System was used to digitally mark the location of corneal incisions during surgery, the size of the capsulorhexis to be opened in the lens capsule and the position of the cylindrical IOL within the eye (within the lens capsule), and a 5.5 mm capsule opening was preferred in this study. The axis was determined according to the keratometric measurements obtained when the cylindrical IOL was placed in the capsule and stabilization was achieved by inserting the IOL into this axis. In the bifocal toric group patients, reference points and IOL position were marked on the astigmatic quadrant of the biomicroscope with a marker pen before surgery. At the 6-month examination, biomicroscopic examination, refraction, IOP, distance-intermediate-near uncorrected and corrected visual acuity were evaluated. Postoperative keratometry was determined after detailed anterior-posterior segment examinations and rotation of the IOL was examined by dilating the pupilla (tropicamide 1%). For the objective measurement of IOL rotation, the method proposed by Wolffshon and Buckhurst[18] in their 2010 study was used. Postoperative photographs were taken using Topcon digital slit lamp (Topconsl-D7, SN: 1613331, Japan) of the lens in situ. All images were photographed at a magnification of ×10 using retro illumination and analyzed. Rotation was determined for each postoperative visit. At the same time, patient satisfaction, the need for glasses and glare symptoms were evaluated by direct questioning of the patients. The Vector Vision CSV-1000E Contrast Sensitivity Test was used for contrast sensitivity and glare measurement. The measurements were performed under normal room illumination conditions after correcting for CDVA. Glare was measured using 2 halogen lamps attached to the CSV-1000E. Glare was tested by switching on the halogen lamps under photopic conditions in the same manner as in the contrast sensitivity test. Near stereopsis (40 and 80 cm) was measured with “TitmusStereotest” and distance stereopsis (2 and 3 m) with the “Distance Randot Stereotest”. The tests were performed using binocular and polarizing glasses and the final arc/s value that the patients could see was recorded.
Statistical Analysis
Data obtained in the study were analyzed statistically using IBM SPSS for Windows version 21.0 software. Using descriptive statistical analysis, numerical variables were summarized as mean±standard deviation (SD) values. The normal distribution of numerical data was evaluated with the Shapiro Wilk test. The paired sample t-test was used to compare the pre- and postoperative values within groups whereas independent samples t-test was used for between groups comparisons. Statistical significance was assumed at P<0.05.
RESULTS
In this study, the trifocal toric group included 40 eyes of 20 patients, comprising 7 males and 13 females with a mean age of 63.7±11.11y (range 47-81y). The bifocal toric group included 40 eyes of 20 patients, comprising 10 males and 10 females with a mean age of 54.66±11.98y (range 36-74y). No statistically significant difference was observed between the patient groups in terms of age and gender (P=0.077, P=4.422, respectively). The surgeries were performed by the same surgical team with the phacoemulsification technique and no complications occurred. No changes were found between postoperative measurements over the time. Therefore, it was defined 6th month. Preoperative and postoperative 6th month best uncorrected and corrected distance-intermediate-near visual acuity results are shown in Table 1.
Table 1. Preoperative and postoperative visual acuity results.
| Time | Trifocal toric | Bifocal toric | ||
| Preop. (logMAR) | UDVA: 0.86±0.19 | CDVA: 0.67±0.22 | UDVA: 0.81±0.22 | CDVA: 0.59±0.11 |
| UIVA: 0.81±0.10 | CIVA: 0.71±0.15 | UIVA: 0.80±0.12 | CIVA: 0.70±0.13 | |
| UNVA: 0.81±0.13 | CNVA: 0.64±0.16 | UNVA: 0.78±0.12 | CNVA: 0.67±0.10 | |
| Postop. (logMAR) | UDVA: 0.07±0.05 | CDVA: 0.05±0.06 | UDVA: 0.19±0.14 | CDVA: 0.11±0.13 |
| UIVA: 0.15±0.06 | CIVA: 0.14±0.06 | UIVA: 0.59±0.15 | CIVA: 0.49±0.10 | |
| UNVA: 0.15±0.06 | CNVA: 0.12±0.04 | UNVA: 0.14±0.60 | CNVA: 0.10±0.04 | |
UDVA: Uncorrected distance visual acuity; CDVA: Corrected distance visual acuity; UIVA: Uncorrected intermediate visual acuity; CIVA: Corrected intermediate visual acuity; UNVA: Uncorrected near visual acuity; CNVA: Corrected near visual acuity.
mean±SD
There was no significant difference between preoperative distance-intermediate-near visual acuities in both groups (P=0.102, 0.647, 0.280, respectively). In the postoperative follow-up, mean distance-intermediate-near visual acuity increased significantly compared to the preoperative values (all P<0.001). There was no significant difference between the groups in terms of postoperative distance and near visual acuities (P=0.269, P=0.451, respectively). The postoperative UIVA and CIVA levels were found to be significantly higher in the trifocal toric group compared to the bifocal toric group (P<0.001).
The preoperative and postoperative 6th month spherical mean values, cylindrical mean values, and spherical equivalent measurements of the patients are shown in Table 2.
Table 2. Preoperative and postoperative refraction measurements.
| Parameters | Trifocal toric |
Bifocal toric |
||
| Preop. | Postop. | Preop. | Postop. | |
| Spherical values | -1.39±3.53 | -0.13±0.40 | -2.90±3.60 | -0.31±1.98 |
| Cylindrical values | 1.91±2.16 | 0.48±0.33 | 2.70 ±3.50 | 1.18±1.53 |
| Spherical equivalent | -2.36±4.39 | -0.41±0.49 | -3.95±4.81 | -0.88±1.48 |
mean±SD, D
There was no statistically significant difference in postoperative spherical, cylindrical and spherical equivalent measurements (P=0.885, 0.676, 1.000, respectively). In both groups, spherical, cylindrical and spherical equivalent measurements were statistically significantly lower postoperative values compared to preoperative values (P<0.005).
The mean spherical and toric powers of the implanted IOL's were found be similar. Spherical and toric powers in the trifocal toric group were +21.00 D and +2.50 D respectively. In the bifocal toric group were +21.50 D and +3.00 D respectively.
The mean scores of the visual function scale (NEI-VFQ-25) questionnaire completed by patients preoperatively and at postoperatively 6th month are shown in Table 3.
Table 3. Mean visual function scale questionnaire (NEI-VFQ-25) scores.
| NEI-VFQ-25 | Trifocal toric | Bifocal toric | P |
| Preop. | 62.41±15.56 | 69.68±9.09 | 0.158 |
| Postop. | 88.18±3.97 | 86.77±6.11 | 0.691 |
| P | <0.001 | <0.001 |
The preoperative and postoperative NEI-VFQ25 questionnaire results of the trifocal toric and bifocal toric groups were found to be statistically similar and there was no significant difference between them (P=0.158, 0.691, respectively). In both groups, the quality of life questionnaire scores were determined to have statistically significantly increased in the postoperative period compared to the preoperative values (P=0.001 and P<0.001).
In the trifocal toric group, 2 (10%) patients were prescribed near glasses and 2 (10%) patients were prescribed distance glasses. Near or distance glasses were not needed by 16 (80%) patients. In the bifocal toric group, 2 patients required near glasses (10%) and 2 patients required distance glasses (10%). There was no significant difference between the two groups in terms of wearing glasses (P>0.05) with a low number of patients wearing glasses in both groups.
In respect of general patient satisfaction, 17 patients (85%) were very satisfied with the surgery and postoperative visual performance in the trifocal toric group and the other 3 patients (15%) were satisfied. In the bifocal toric group, 10 patients (50%) were very satisfied with their visual performance and surgical condition, and 10 patients (50%) were satisfied with their visual performance. The overall satisfaction rate in the trifocal toric group was significantly higher than the bifocal toric group (P=0.03).
In the trifocal toric group, 16 patients (80%) had no glare complaints, 3 patients (15%) had mild complaints and 1 patient (5%) had moderate glare complaints. In the bifocal toric group, 10 patients had mild glare (50%), and the remaining 10 patients had no complaints (50%). Glare complaints were significantly lower in the trifocal toric group compared to the bifocal toric group (P=0.03).
Contrast sensitivity and glare were evaluated at 6th month. The contrast sensitivity and glare results of the patients are shown in Figures 1 and 2.
Figure 1. Contrast sensitivity at postoperative 6th month.
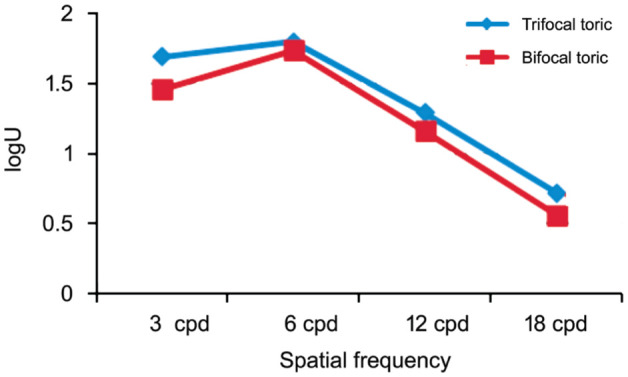
Figure 2. Glare at postoperative 6th month.
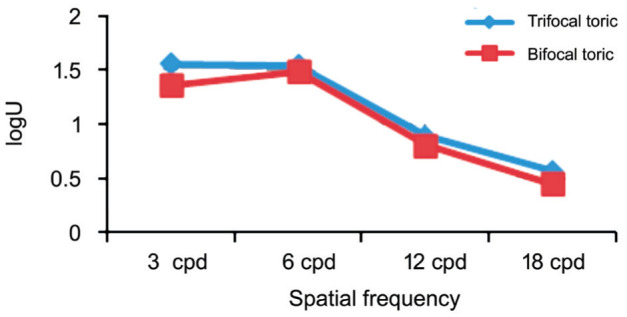
The best contrast sensitivity and glare results were obtained at 6 cpd spatial frequency. Although the contrast sensitivity function was not statistically significant (P>0.05) in the trifocal toric group, it was found to be slightly better than in the bifocal toric group.
In both groups, the patients underwent binocular “Titmus Stereotest” at near and medium distance and “Distance Randot Stereotest” at long distance. The stereopsis results of the patients are shown in Table 4.
Table 4. Postoperative 6th month stereopsis values.
| Stereopsis | Trifocal toric (arc/s) | Bifocal toric (arc/s) | P |
| 40 cm | 57.5±24.25 | 73.63±20.62 | 0.02 |
| 80 cm | 79±28.45 | 92.72±13.48 | 0.048 |
| 2 m | 153±77.94 | 181.81±116.77 | 0.003 |
| 3 m | 270±112.85 | 290.90±104.44 | 0.577 |
In both groups, binocular depth perception at 40 and 80 cm, and 2 m distances were found to be statistically significantly higher in the trifocal toric group than in the bifocal toric group (P=0.02, 0.048, 0.003). Although there was no statistically significant difference in stereopsis, the trifocal toric group had higher depth perception (P=0.577) at a distance of 3 m.
The IOL rotation was evaluated with pupil dilation at postoperative 6th month. The mean rotation was 5.76°±3.93° (min: 0° max: 15°) in the trifocal toric group and 12°±7.1° (min: 2° max: 28°) in bifocal toric group. The amount of rotation was observed to be statistically significantly lower in the trifocal toric group (P=0.004).
DISCUSSION
The result of this study showed a statistically significant increase in visual quality of life in both groups (P<0.001), according to the results of the visual function scale (NEI-VFQ-25). To et al[19] reported that NEI-VFQ-25 significantly improved after cataract surgery (P < 0.001) particularly after bilateral eye surgeries. It can be said that the removal of cataracts and IOL implantation generally improve the quality of life of patients. The general satisfaction of the patients was higher in the trifocal toric group than in the bifocal toric group, which may have been due to better intermediate distance visual acuity. It should be acknowledged that both IOLs have different reading additions, and thus the choice of near/intermediate testing distance has been designed to suit the trifocal and as a consequence could disadvantage the bifocal.
Petzold et al[20] reported that after bilateral implantation of bifocal IOLs, 95.9% of patients started that they could accomplish all common tasks without any significant problems. In another study, Rementería-Capelo et al[21] reported that the questionnaire showed high patient satisfaction for those who had undergone trifocal toric IOL implantation.
In the current study, glasses independence was 80% in both groups. Torun Acar et al[22] reported that >90% of patients had no visual impairment in their daily activities. In a study by Voskresenskaya et al[16], 95% of patients did not need near glasses. Kretz et al[9] documented that only 10.5% of patients required postoperative correction for near or intermediate distance. According to these results, it can be said that the need for distance and near glasses in the current study patients decreased significantly at a similar rate to findings in literature.
In the trifocal toric group of the current study, there were no glare complaints in 80% and mild glare was determined in 15% of the patients. In the bifocal toric group, 50% of patients had no complaints and 50% had mild glare. In the study by Voskresenskaya et al[16], 16.7% of patients had glare complaints while Kretz et al[9] reported 45.7% halo and 30.4% glare in their patients. The Acriva Reviol Tri-ED trifocal toric IOL semi-apodization technology can significantly reduce the loss of light in the eye, which can cause a significant reduction in glare complaints.
In the current study, the highest contrast sensitivity value was observed at 6 cpd spatial frequency (1.80±0.24 logU and 1.74±0.20, respectively) in trifocal toric and bifocal toric IOL under photopic conditions, and contrast sensitivity values decreased at increasing spatial frequencies. The highest contrast sensitivity levels were also at 6 cpd spatial frequency in studies by Kretz et al[23] and Mojzis et al[11]. In contrast to the current study, Voskresenskaya et al[16] reported the highest sensitivity at 3 cpd spatial frequency. The contrast sensitivity curve of the current study patients was found to be highest at 6 cpd spatial frequency, similar to the findings of other studies.
In the current study, the results of the Titmus test, which measures near stereopsis were reported as 57.5±24.25 and 72.63±20.62 arc/s. The distance stereopsis values were found to be 270±112.85 and 290.90±104.44. In a study by Ferrer-Blasco et al[24], 30 patients underwent bilateral bifocal IOL implantation and the near stereopsis Titmus test results were 44.55±1.08 arc/s. Titiyal et al[25] reported that perfect near stereopsis of 20 arc/s was present in 80% of cases, and 82% had good distance stereopsis of 100 arc/s or better. The near and distance stereopsis results in the current study were similar to results in literature.
In the current study, the mean IOL rotation was 5.76°±3.93° (min: 0° max:15°) in the trifocal toric group and 12°±7.1° (min: 2° max: 28°) in the bifocal toric group. In a study by Mojzis et al[11], 40% of patients had 0° rotation, 53% had 1°-3° rotation and 7% had 4°-5° rotational deviation. Lubiński et al[26] performed toric IOL implantation in 26 eyes of 18 patients and reported the mean rotational deviation in the postoperative 6th month to be 1.1°±2.4°. In a study of Dubinsky-Pertzov et al[27], 56 eyes of 56 patients were implanted with monofocal toric IOL and in the postoperative 1st month IOL rotational deviation was reported 3.18°±3.3° and IOL rotation significantly increased between day 1 to day 7 postoperatively. It is known that, after toric IOL implantation, 15° rotation causes loss of half of the desired effect and 30° rotation loses all the desired effect. Rotation of 90° causes the existing astigmatic problem to double. Stabilization of the toric IOL inside the eye postoperatively is closely related to its haptic structure. Bifocal toric IOL was implanted with the conventional corneal marking method and the bifocal IOL group had higher rotation. Although two kind of lenses have same material and designs. Therefore, the Acriva Toric IOL was considered to be very successful due to the plate haptic structure and because the Alcon VERION imaging system used in this study is superior to the classical corneal marking method in IOL placement and axis determination.
In conclusion, trifocal toric or bifocal toric IOL implantation in appropriate patients yields satisfactory and predictable results. Trifocal toric and bifocal toric implantation is considered a satisfactory surgical procedure with the elimination of spectacle dependence, low astigmatism levels and high patient satisfaction. The application of IOL implantation with digital systems rather than manual marking during surgery can be considered to provide more accurate results for IOL stabilization. The main limitation of this study might be the relatively low number of patients. With the evaluation of the 6-month results of trifocal toric and bifocal toric IOL implantation in this study, it was concluded that satisfactory results were obtained especially in intermediate and distance stereopsis, which had a positive effect on the quality of life of the patients.
Acknowledgments
Conflicts of Interest: Bozkurt Gencer M, None; Basmak H, None; Yasar E, None; Onal O, None.
REFERENCES
- 1.Olson RJ. Cataract surgery from 1918 to the present and future-just imagine! Am J Ophthalmol. 2018;185:10–13. doi: 10.1016/j.ajo.2017.08.020. [DOI] [PubMed] [Google Scholar]
- 2.Xu J, Zheng TY, Lu Y. Comparative analysis of visual performance and astigmatism tolerance with monofocal, bifocal, and extended depth-of-focus intraocular lenses targeting slight myopia. J Ophthalmol. 2020;2020:9283021. doi: 10.1155/2020/9283021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Curragh DS, Hassett P. Prevalence of corneal astigmatism in an NHS cataract surgery practice in northern Ireland. Ulster Med J. 2017;86(1):25–27. [PMC free article] [PubMed] [Google Scholar]
- 4.Tsinopoulos IT, Tsaousis KT, Tsakpinis D, Ziakas NG, Dimitrakos SA. Acrylic toric intraocular lens implantation: a single center experience concerning clinical outcomes and postoperative rotation. Clin Ophthalmol. 2010;4:137–142. doi: 10.2147/opth.s9608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kiliç I, Akova YA, Akman A, Eğrilmez S. The results of phacoemulsification and toric intraocular lens implantation in patients with high astigmatism and cataract. Turk Oftalmoloji Gazetesi. 2012;42(2):116–119. [Google Scholar]
- 6.Sandoval HP, Lane S, Slade SG, Donnenfeld ED, Potvin R, Solomon KD. Defocus curve and patient satisfaction with a new extended depth of focus toric intraocular lens targeted for binocular emmetropia or slight myopia in the non-dominant eye. Clin Ophthalmol. 2020;14:1791–1798. doi: 10.2147/OPTH.S247333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zvorničanin J, Zvorničanin E. Premium intraocular lenses: the past, present and future. J Curr Ophthalmol. 2018;30(4):287–296. doi: 10.1016/j.joco.2018.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feng K, Guo HK, Zhang YL, Wu Z. Visual quality comparison after multifocal toric intraocular lens or monofocaltoric intraocular lens implantation. Zhonghua Yan Ke Za Zhi. 2017;53(4):274–280. doi: 10.3760/cma.j.issn.0412-4081.2017.04.009. [DOI] [PubMed] [Google Scholar]
- 9.Kretz FT, Bastelica A, Carreras H, Ferreira T, Müller M, Gerl M, Gerl R, Saeed M, Schmickler S, Auffarth GU. Clinical outcomes and surgeon assessment after implantation of a new diffractive multifocal toric intraocular lens. Br J Ophthalmol. 2015;99(3):405–411. doi: 10.1136/bjophthalmol-2014-305570. [DOI] [PubMed] [Google Scholar]
- 10.Brožková M, Filipec M, Filipová L, Holubová A, Hlinomazová Z. Outcomes of trifocal toric lens implantation in cataract patients. Cesk Slov Oftalmol. 2016;72(3):58–64. [PubMed] [Google Scholar]
- 11.Mojzis P, Majerova K, Plaza-Puche AB, Hrckova L, Alio JL. Visual outcomes of a new toric trifocal diffractive intraocular lens. J Cataract Refract Surg. 2015;41(12):2695–2706. doi: 10.1016/j.jcrs.2015.07.033. [DOI] [PubMed] [Google Scholar]
- 12.Höhn F, Tandogan T, Breyer DR, Kaymak H, Hagen P, Klabe K, Koss MJ, Gerl M, Auffarth GU, Kretz FT. Functional results one year after implantation of a bitoric, trifocal intraocular lens. Klin Monbl Augenheilkd. 2015;232(8):957–961. doi: 10.1055/s-0041-103335. [DOI] [PubMed] [Google Scholar]
- 13.Piovella M, Colonval S, Kapp A, Reiter J, Van Cauwenberge F, Alfonso J. Patient outcomes following implantation with a trifocal toric IOL: twelve-month prospective multicentre study. Eye (Lond) 2019;33(1):144–153. doi: 10.1038/s41433-018-0076-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang JS, Zhao JY, Sun Q, Ma LW. Distance vision after bilateral implantation of AcrySoftoric intraocular lenses: a randomized, controlled, prospective trial. Int J Ophthalmol. 2011;4(2):175–178. doi: 10.3980/j.issn.2222-3959.2011.02.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mojzis P, Peña-García P, Liehneova I, Ziak P, Alió JL. Outcomes of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2014;40(1):60–69. doi: 10.1016/j.jcrs.2013.06.025. [DOI] [PubMed] [Google Scholar]
- 16.Voskresenskaya A, Pozdeyeva N, Pashtaev N, Batkov Y, Treushnicov V, Cherednik V. Initial results of trifocal diffractive IOL implantation. Graefes Arch Clin Exp Ophthalmol. 2010;248(9):1299–1306. doi: 10.1007/s00417-010-1424-8. [DOI] [PubMed] [Google Scholar]
- 17.Toprak AB, Eser E, Guler C, Baser FE, Mayali H. Cross-validation of the Turkish version of the 25-item national eye institute visual functioning questionnaire (NEI-VFQ 25) Ophthalmic Epidemiol. 2005;12(4):259–269. doi: 10.1080/09286580590967763. [DOI] [PubMed] [Google Scholar]
- 18.Wolffsohn JS, Buckhurst PJ. Objective analysis of toric intraocular lens rotation and centration. J Cataract Refract Surg. 2010;36(5):778–782. doi: 10.1016/j.jcrs.2009.12.027. [DOI] [PubMed] [Google Scholar]
- 19.To KG, Meuleners LB, Fraser ML, Do DV, Duong DV, Huynh VA, To QG, Phi TD, Tran HH, Nguyen ND. The impact of cataract surgery on vision-related quality of life for bilateral cataract patients in Ho Chi Minh City, Vietnam: a prospective study. Health Qual Life Outcomes. 2014;12:16. doi: 10.1186/1477-7525-12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Petzold A, Wilke C, Renner K, Kunert K. Retrospective study of long-term patient satisfaction after bilateral implantation of multifocal intraocular lenses of different generations-a 10 year follow-up. Klin Monbl Augenheilkd. 2019;236(8):969–975. doi: 10.1055/a-0842-6735. [DOI] [PubMed] [Google Scholar]
- 21.Rementería-Capelo LA, Contreras I, García-Pérez JL, Blázquez V, Ruiz-Alcocer J. Visual quality and patient satisfaction with a trifocal intraocular lens and its new toric version. J Cataract Refract Surg. 2019;45(11):1584–1590. doi: 10.1016/j.jcrs.2019.06.014. [DOI] [PubMed] [Google Scholar]
- 22.Torun Acar B, Duman E, Simsek S. Clinical outcomes of a new diffractive trifocal intraocular lens with Enhanced Depth of Focus (EDOF) BMC Ophthalmol. 2016;16(1):208. doi: 10.1186/s12886-016-0389-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kretz FT, Breyer D, Klabe K, Hagen P, Kaymak H, Koss MJ, Gerl M, Mueller M, Gerl RH, Auffarth GU. Clinical outcomes after implantation of a trifocal toric intraocular lens. J Refract Surg. 2015;31(8):504–510. doi: 10.3928/1081597X-20150622-01. [DOI] [PubMed] [Google Scholar]
- 24.Ferrer-Blasco T, Madrid-Costa D, García-Lázaro S, Cerviño A, Montés-Micó R. Stereopsis in bilaterally multifocal pseudophakic patients. Graefes Arch Clin Exp Ophthalmol. 2011;249(2):245–251. doi: 10.1007/s00417-010-1558-8. [DOI] [PubMed] [Google Scholar]
- 25.Titiyal JS, Kaur M, Bharti N, Singhal D, Saxena R, Sharma N. Optimal near and distance stereoacuity after binocular implantation of extended range of vision intraocular lenses. J Cataract Refract Surg. 2019;45(6):798–802. doi: 10.1016/j.jcrs.2018.12.024. [DOI] [PubMed] [Google Scholar]
- 26.Lubiński W, Kaźmierczak B, Gronkowska-Serafin J, Podborączyńska-Jodko K. Clinical outcomes after uncomplicated cataract surgery with implantation of the tecnis toric intraocular lens. J Ophthalmol. 2016;2016:3257217. doi: 10.1155/2016/3257217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dubinsky-Pertzov B, Hecht I, Gazit I, Or L, Mahler O, Rotman S, Pras E, Einan-Lifshitz A. Clinical outcomes of Ankoris toric intraocular lens implantation using a computer-assisted marker system. Int Ophthalmol. 2020;40(12):3259–3267. doi: 10.1007/s10792-020-01511-4. [DOI] [PubMed] [Google Scholar]


