Abstract
Background
This is an update of the section on complications that are associated with coughing in the 2006 CHEST cough guidelines that addresses two aims: (1) to systematically identify and thematically categorize the diverse complications of cough by providing a guide for future studies and (2) to identify gaps in the literature for future research.
Research Question
What are the potential complications that are associated with the act of coughing that have been reported in infants, children, adolescents, and adults?
Study Design and Methods
A scoping review was performed with the use of PubMed and SCOPUS databases that were searched from their beginning until September 6, 2019.
Results
Two hundred forty-seven publications met our inclusion criteria. To these, we added 38 articles from the 2006 complications paper that were not identified in the literature search plus the paper itself for a final total of 286 publications that formed the basis of this review. Since 2006, three new categories of complications have been reported: ear, nose and throat; disease transmission; and laboratory testing. Multiple additional complications that fall outside of these three categories have also been identified and included in the following categories: cardiovascular, constitutional symptoms, dermatologic, GI, genitourinary, musculoskeletal, neurologic, ophthalmologic, psychosocial/quality of life, and respiratory. Not previously highlighted is that some of the complications led to serious morbidity that included death, especially in patients with comorbid conditions, and potentially resulted in harm to others when cough resulted in a motor vehicle accident.
Interpretation
Our work identified a large number of cough complications that we thematically categorized primarily by organ system so that future studies of each system or each complication can be conducted. The gap in the literature that future studies should address is to identify the frequency of the complications and the strength of their association with cough. Only then will one be able to describe the findings in a manner that allows specific recommendations for avoiding these complications. In the meantime, patients with cough should be evaluated and treated according to evidence-based guidelines to mitigate or prevent the myriad of potential complications that are associated with coughing.
Key Words: complication, cough, organ system
Abbreviations: CQLQ, cough quality of life questionnaire
FOR EDITORIAL COMMENT, SEE PAGE 1818
This review provides an update to our article on the topic of complications associated with coughing in the 2006 American College of Chest Physicians Clinical Practice Guidelines on the Diagnosis and Management of Cough.1,2
As previously stated in 2006,1 complications that are associated with coughing stem from physiologic events that teleologically seem to be designed to allow cough to carry out its two main protective functions: to prevent foreign material from entering the lower respiratory tract and to clear foreign material and excessive secretions from the lower respiratory tract. During the physiologic phases of coughing (ie, inspiratory, compressive, and expiratory), sufficiently high expiratory velocities are generated to carry out the aforementioned functions. The potentially injurious nature of these physical forces is recognized; for example, during vigorous coughing, intrathoracic pressures can reach 300 mm Hg3 that help to generate expiratory velocities up to 500 miles per hour4 (ie, 85% of the speed of sound).
From a cardiovascular standpoint, the physiologic effects of coughing can be a two-edged sword. Because intrathoracic pressures generated during coughing may hemodynamically compare favorably with chest compressions, cough CPR can be successfully used in a controlled environment.5 Because vigorous coughing can also generate intrathoracic energies up to 25 J,6 cardiologists, in a monitored in-hospital cardiac catheterization laboratory, often instruct patients, before the procedure begins, to vigorously cough when instructed to do so, if and when awake patients experience ventricular tachycardia and asystole during cardiac catheterization procedures. Because coughing can also be associated with a reflex increase in vagal tone, coughing can interrupt aberrant conduction of atrioventricular junctional tachycardia.7 On the other hand, coughing can also lead to atrioventricular block8 and other arrhythmias (Table 1).
Table 1.
Cough-Associated Complications
| System Category | Complication |
|---|---|
| Cardiovascular | Aortic dissection14 |
| Arterial hypotension3,15, 16, 17, 18, 19 | |
| Arrhythmia | |
| • Bradyarrhythmias with or without heartblock with and without dizziness and syncope8,20, 21, 22, 23, 24, 25, 26, 27 | |
| • Tachyarrhythmias, atrial, or ventricular28, 29, 30 | |
| Coronary artery dissection31,32 | |
| Cardiac luxation after pneumonectomy33 | |
| Stress cardiomyopathy34 | |
| Dislodgement/malfunctioning of intravascular cathetersor other intravascular devices35, 36, 37, 38, 39, 40 | |
| Loss of consciousness3,15 | |
| Pneumopericardium during coronary angiography41 | |
| Constitutional symptoms | Excessive sweating, anorexia, exhaustion, temperature elevation (various combinations), vomiting42 |
| Dermatologic | Petechiae and purpura43 |
| Disruption of surgical wounds (sternal and abdominal)44, 45, 46 | |
| Subcutaneous hematoma not anticoagulated47, 48, 49, 50 | |
| Subcutaneous hematoma receiving anticoagulation therapy51,52 | |
| Ear, nose, and throat | Arytenoid subluxation with or without obliteration of cricoarytenoid space53,54 |
| Hemotympanum55 | |
| Thyroid cartilage fracture with phlegmon56 | |
| GI | Esophageal rupture57 |
| Gastroduodenal artery pseudoaneurysm rupture58 | |
| Gastroesophageal reflux events59 | |
| Gastric hemorrhage after percutaneous endoscopic gastrostomy60 | |
| Gastric perforation after upper endoscopy61 | |
| Hepatic cyst rupture62 | |
| Laceration of stomach and spleen63 | |
| Malfunction of gastrostomy button64 | |
| Mallory-Weiss tear65,66 | |
| Rectal prolapse with rupture of distal colon and evisceration of small intestine through anus and death in an infant67 | |
| Small bowel herniation through laparoscopic trocar site68 | |
| Splenic rupture69, 70, 71, 72, 73 | |
| Spontaneous retroperitoneal bleed with hematoma74 | |
| Inguinal or femoral or umbilical or lumbar or abdominal wall hernia75, 76, 77, 78, 79, 80, 81 | |
| Genitourinary | Inversion of bladder through urethra82 |
| Urinary incontinence77,83, 84, 85, 86, 87 | |
| Vaginal cuff dehiscence with evisceration of ileal loops88 | |
| Musculoskeletal | Avulsion of lesser trochanter of femur89 |
| From asymptomatic elevations of serum creatinine phosphokinase to rupture of rectus abdominus muscles with and without hematoma51,90, 91, 92, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103 | |
| Diaphragmatic rupture with abdominal content herniation (small bowel and omentum)104, 105, 106 | |
| False-positive PET scan uptake in muscle related to cough107 | |
| Intercostal muscle rupture with lung herniation108, 109, 110 | |
| Lung herniation through rib separations49,111 | |
| Lung herniation through previous incision112 | |
| Liver, colon, small bowel, omentum, and lung herniation through transdiaphragmatic intercostal separation113 | |
| Intercostal artery rupture and hematoma with or without hemothorax with or without rib fracture47,114, 115, 116 | |
| Internal oblique muscle tear with hematoma117,118 | |
| Osteophytes of the ribs119 | |
| Rib fractures47,78,120, 121, 122, 123, 124, 125, 126, 127, 128, 129, 130, 131, 132, 133, 134, 135, 136, 137, 138, 139, 140 | |
| • Costal margin separation with or without rib fracture and diaphragmatic rupture with abdominal visceral herniation into thoracic cavity or abdomen and/or subcutaneously141, 142, 143, 144, 145, 146, 147, 148 | |
| • Rib fracture with pseudohernia of abdominal contents149 | |
| • Rib fracture with lung herniation with or without pleural effusion150, 151, 152, 153, 154 | |
| Scapula fracture155 | |
| Neurologic | Acute cervical radiculopathy and disc herniation156 |
| Carotid artery dissection and pseudoaneurysm157 | |
| Carotid artery dissection with stroke158 | |
| Cerebral air embolism causing stroke with and without death159, 160, 161, 162 | |
| Cerebral spinal fluid rhinorrhea163,164 | |
| Cervicobrachial pain165 | |
| Cervical epidural hematoma associated with oral anticoagulation166 | |
| Cough syncope17,167, 168, 169, 170, 171, 172, 173, 174, 175, 176, 177, 178, 179, 180, 181, 182, 183, 184, 185, 186, 187, 188, 189, 190, 191, 192, 193, 194, 195, 196, 197, 198, 199, 200, 201, 202, 203, 204, 205, 206 | |
| Cough syncope causing car crash with injuries187 | |
| Cough syncope causing traffic accident191 | |
| Cough syncope causing traffic accident with death of pedestrians190 | |
| Cough-induced anoxic cerebral injury in child207 | |
| Cough-induced cluster headache208 | |
| Cough-induced transient ischemic attack209 | |
| Cough-induced nystagmus210 | |
| Cough-induced recurrence of spinal anesthesia211 | |
| Cough-induced vertigo192 | |
| Cough headache77,212, 213, 214, 215, 216, 217, 218, 219, 220, 221, 222, 223, 224, 225 | |
| Cough headache presenting as toothache226 | |
| Cough-induced hemiparesis227 | |
| Cough-induced hemiplegic migraine228 | |
| Cough-induced myxoma embolism causing paraplegia229 | |
| Dizziness230 | |
| Cough-induced seizures172,176,185,201,231 | |
| Malfunctioning ventriculoartrial shunts232 | |
| Pneumocephalus233 | |
| Pneumorrhachis233, 234, 235, 236 | |
| Spontaneous dissection of cerebral arteries237 | |
| Stroke due to vertebral artery dissection238, 239, 240 | |
| Stroke due to bilateral carotid artery thrombus formation241 | |
| Ophthalmologic | Extrusion of ocular contents during surgery242 |
| Spontaneous compressive orbital emphysema of rhinogenic origin243 | |
| Orbital emphysema compressing the eyeball and the optic nerve243 | |
| Periorbital ecchymosis (Panda sign)244,245 | |
| Subconjunctival hemorrhages77,180,245,246 | |
| Retinal detachment247 | |
| Subhyaloid hemorrhage248 | |
| Suprachoroidal hemorrhage249,250 | |
| Transient blindness251 | |
| Postoperative Trabeculectomy bleb leak252 | |
| Psychosocial/quality of life | Fear of serious disease230,253,254 |
| Lifestyle changes230,254,255 | |
| Self-consciousness230,254,255 | |
| Adverse effects on quality of life87,254, 255, 256, 257, 258, 259, 260, 261, 262, 263, 264 | |
| Respiratory | Apical lung herniation with tracheal displacement265 |
| Chylothorax266 | |
| Diaphragmatic rupture with herniation of small intestine or stomach into chest63,267 | |
| Exacerbation of asthma268 | |
| Hemothorax116,144 | |
| Herniations of the lung (eg, intercostal and supraclavicular) with and without incarceration269, 270, 271, 272, 273 | |
| Hydrothorax in peritoneal dialysis274 | |
| Hydropneumothorax and tension pneumothorax57 | |
| Laryngeal trauma (eg, laryngeal edema and hoarseness)230,254,255,275,276 | |
| Pulmonary interstitial emphysema, with one or more of pneumatosis intestinalis, pneumomediastinum, pneumoperitoneum, pneumopericardium, pneumoretroperitoneum, pneumorrhacis, pneumothorax, subcutaneous emphysema, retropharyngeal, paraesophageal air49,111,161,233, 234, 235,271,277, 278, 279, 280, 281, 282, 283, 284, 285, 286, 287, 288, 289, 290, 291, 292, 293 | |
| Rupture of bronchus during bronchoscopy with or without pneumothorax294,295 | |
| Rupture of trachea287,296 | |
| Tracheobronchial trauma (eg, bronchitis and bronchial rupture)233,297 | |
| Transmission of infectious disease298,299 | |
| Disease transmission | Transmission of infectious disease298,299 |
| Laboratory testing | False-positive PET scan uptake in muscle related to cough107 |
Modified from Table 1 in Irwin RS. Complications of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl1):54S-58S.1 Complications that are new since 2006 are given in bold italic type.
As noted in 2006,1 although the pressures, velocities, and energy described earlier, particularly those that relate to the effects on the cardiovascular system, allow coughing to be an effective way of protecting the lungs from near aspiration and aspiration and of providing CPR and arrhythmia control, they can also cause a variety of complications that can be categorized as cardiovascular, constitutional, dermatologic, GI, genitourinary, health-related quality of life, musculoskeletal, neurologic, ophthalmologic, psychosocial, and respiratory.
In planning this update, we followed current CHEST guideline methods9 that emphasizes that guidelines should be based on high-quality systematic reviews to address clearly formulated key clinical questions. Because our question was broad and the literature had not been reviewed comprehensively, we chose to conduct a scoping review. A scoping review is based on similar established methods to a systematic review with the intent to clarify working definitions, to identify key concepts, and to establish conceptual boundaries by examining the extent and nature of the evidence.10,11 Our specific aims were to (1) systematically identify and thematically categorize the diverse complications of cough providing a guide for future studies and (2) identify gaps in the literature for future research.
Methods
To begin our literature search, we asked the following key clinical question: What are the potential complications associated with the act of coughing that have been reported in infants, children, adolescents and adults? A complication was defined as “a morbid process or event that occurs during the course of a disease that is not an essential part of that disease, although it may result from it or from independent causes.”12 We considered death to be associated with a complication when the authors of the case report or case series described the death as following the complication of cough and it did not appear to be due to another event. To guide the search of our scoping review, we sought the following elements: population (infants, children, adolescents, and adults), concept (does the study report on the complications as defined earlier secondary to the act of coughing), and context (cough of any duration in patients who are either ambulatory or in the hospital). Inclusion criteria were limited to the English language, cough of any duration, and any study design such as systematic reviews with or without a metaanalysis, diagnostic cohort, case-control study, cross-sectional study, letter to the editor, case reports/series, other reports. Exclusion criterion was a report of an adverse event rather than a complication, unless cough initiated the event. An adverse event was defined as “an incident in which harm resulted to a person receiving health care.”13
Search Strategy
A systematic review of the literature was performed. Studies published in PubMed and SCOPUS databases were identified from the beginning of the database to September 6, 2019. Because cough and complication retrieved 13,750 citations in PubMed alone, the search was limited to subject heading. The search strings can be found in e-Appendix 1.
Data Screening and Extraction
Two authors (C. L. F. and R. S. I.) independently analyzed the titles and content of the abstracts to assess inclusion criteria. From the selected titles and abstracts, full reports about potentially relevant studies were obtained, and two authors (C. L. F., N. D., or R. S. I.) independently assessed the eligibility of the studies and completed data extraction. Disagreements were discussed and resolved by consensus. A third author was available to help resolve disagreements if necessary. Even though the screening focused on publications not published in the 2006 guideline, all the articles cited in the 2006 review were reanalyzed. During this re-review of the articles published in the 2006 review, we came across 38 articles that did not appear in the current search.
Results
Literature Study Selection
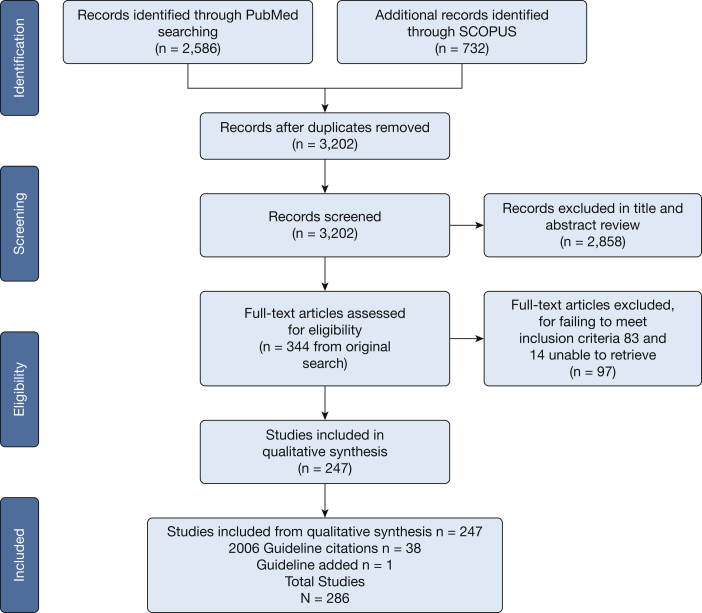
The process of study selection is outlined in Figure 1, which shows that there were an initial 3,202 unique articles identified by our search string. After being screened, 2,858 abstracts and titles were excluded based on the inclusion and exclusion criteria, which left 344 that underwent full text review. Full text review resulted in the inclusion of 247 articles plus 38 additional citations from the 2006 guideline that were not identified by our search string. The 2006 guideline was also included, which resulted in 286 articles.
Figure 1.
Flow diagram of preferred reporting items for study selection. From Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(7):e1000097. For more information, visitwww.consort-statement.org.
Complications
The complications associated with cough, as identified by the scoping review, are summarized in Tables 1 and 2. The spectra of complications that are associated with coughing are listed in Table 1 in categories that are primarily organ system based and have been modified only minimally from that previously reported in 2006. The new complications, which were identified by the review, that have been added to the original table are included. Since 2006, three new categories of complications have been identified: ear, nose and throat; disease transmission; and laboratory testing. Those complications that were reported as leading to death are listed in Table 2. A data table (e-Table 1) shows more detail about the complications in the articles from the new search that are categorized and summarized in Tables 1 and 2.
Table 2.
Cough-Associated Complications That Lead to Death
| Cough-Associated Complication | Age/Sex | Comorbid Illness | Comment |
|---|---|---|---|
| Death to self and others | |||
| Cough syncope in heavy goods-vehicle drivers causing serious traffic accidents resulting in death of two drivers and two pedestrians190 | UA, UA | UA | Cough syncope can lead to death for the drivers and others. |
| Death to self | |||
| Cough associated with spontaneous arterial gas embolism in patient with chronic necrotizing pneumonia, bullae, and brain infarct with death from complications160 | 78 y, M | COPD, smoker, chronic Enterobacter cloacae pneumonia, hypertension, atrial fibrillation, type 2 diabetes mellitus, hypothyroidism, dyslipidemia | Spontaneous arterial gas embolism resulted in brain infarcts and air in the cavernous sinuses, which led to death precipitated by coughing in a patient with preexisting chronic necrotizing pneumonia, blebs, and bullae. Proposed mechanism is likely weakened parenchyma that led to bleb rupture with entrainment of air into the pulmonary veins and left heart. |
| Paroxysms of cough followed by fainting in patients with asthma (four deaths in the series)173 | UA, M (n = 281); F (n = 9) (N = 290) |
Case series included patients with emphysema, bronchitis, TB, asthma, laryngitis, bronchiectasis, pneumoconiosis, sarcoidosis | Death reported as unequivocal cause after post-tussive syncope in four cases, which accounted for 1% mortality rate in the collective series included two in the literature and two personal cases |
| Fatal rectus sheath hematoma102 | 82 y, F | Polymyositis and related collagen disorders, well controlled with long-term corticosteroids (prednisone 5 mg daily), occult coronary artery disease | Rectus sheath hematoma in one of three patients reported may have been attributed to coughing associated with pneumonia. She was also on thromboprophylaxis with heparin and prednisone for polymyositis. Her course was complicated by a large hematoma, hypotension, and ultimately death. |
| Cough-induced lung intercostal (8th space) hernia with large abdominal hematoma in patient with COPD exacerbation and death49 | 73 y, M | COPD, total laryngectomy for laryngeal cancer with tracheostomy | Cough-induced intercostal muscle rupture with lung hernia associated with hematoma of the left chest and abdomen, massive subcutaneous emphysema of the left chest and lumbar region in a patient presenting with an exacerbation of COPD that was improving before the coughing insult, which ultimately resulted in death. |
| Fatal gas cerebral embolism after heavy coughing while using noninvasive ventilation (bilevel positive airway pressure) for fibrotic lung disease162 | 78 y, M | Severe restrictive lung disease due to fibrotic remodeling due to TB, MALT lymphoma | Cerebral air embolism precipitated by episodes of severe coughing that led to catastrophic stroke in a patient presenting with hemoptysis treated with left bronchial artery embolization, on noninvasive positive pressure ventilation and ultimately death due to intractable treatment of resistant cough. |
| Pneumomediastinum in children with cough with a death286 | 4 y, M | Measles and pneumonia | In a case series of five patients with severe cough, one patient had refractory cough due to measles, bronchopneumonia that resulted in extensive subcutaneous emphysema, pneumomediastinum that ultimately led to progressive decline and death. |
| Pneumomediastinum secondary to coughing in an elderly patient with emphysema with death due to complications288 | 96 y, M | Under custodial care in the geriatrics division | In this case series of three patients, the current patient experienced extensive subcutaneous emphysema and pneumomediastinum after an episode of coughing that resulted in progressive decline and death. |
| Prolapse of the rectum with spontaneous rupture of the distal colon and evisceration of the small intestine through the anus in an infant after a bout of coughing and death due to complications67 | 4 Mo, F | Low birthweight | Severe bout of coughing putatively resulted in increased abdominal pressure that caused rectal prolapse, spontaneous rupture of visceral colon, and evisceration of the small bowel. |
| Cough-induced syncope that resulted in death in the setting of cor pulmonale and obstructive lung disease198 | 61 y, M | Anthracosilicosis, COPD, cor pulmonale, right ventricle myocardial infarction | Cough exacerbated the existing pulmonary hypertension and cor pulmonale as measured by right heart catheterization which led to hypotension, syncope, and ultimately death due to cardiac arrest. |
F = female; M = male; MALT = mucosal associated lymphoid tissue; UA = unavailable.
Discussion
Reviews of complications of cough have appeared periodically in the medical literature for many years. Prior to and even after 1991, these publications primarily focused on complications of a physical nature.42,300, 301, 302 In 1991, we published a prospective study that involved 108 consecutive and unselected patients who were referred to our Cough Clinic with chronic cough that included the results of qualitative interviews that identified reasons for which these patients sought medical attention.230 The reasons all related to cough-associated complications; some were physical, and others were of a psychosocial nature such as fearing that something is wrong, exhaustion, life style change, self-consciousness, and/or fearing cancer, AIDS, or TB (Table 3).230 These results broadened our understanding of the reasons that patients with chronic cough were seeking care and led to the development of our Adverse Cough Outcome Survey254 that eventually led to our development of the first cough quality of life questionnaire, the CQLQ.255 The importance of the development of validated and reliable cough quality of life patient reported outcome questionnaires in the new millennium has now allowed us to assess not only for and quantify the common physical but also for psychosocial complications as summarized in this review.255,264,303,304
Table 3.
Reasons That Patients With Chronic Cough Seek Medical Attention
| Reason | Frequency, % | Most Troublesome, % |
|---|---|---|
| Something’s wrong | 98 | 12 |
| Exhaustion | 57 | 17 |
| Self-conscious | 55 | 10 |
| Insomnia | 45 | 4 |
| Lifestyle change | 45 | 12 |
| Musculoskeletal paina | 44 | 3 |
| Hoarseness | 43 | 2 |
| Excessive perspiration | 42 | 1 |
| Urinary incontinenceb | 39 | 9 |
| Dizziness | 38 | 0 |
| Fear of cancer | 33 | 11 |
| Headache | 32 | 3 |
| Fear of AIDS or TB | 28 | 11 |
| Retching | 21 | 4 |
| Vomiting | 18 | 1 |
| Nausea | 16 | 0 |
| Anorexia | 15 | 0 |
| Syncope or near syncope | 5 | 0 |
Musculoskeletal pain was documented by chest radiography to be due to rib fracture in only one patient.
Urinary incontinence complicated by cough only in women and two men who had undergone prior transurethral prostatectomy.
Reprinted from Irwin RS, Curley FJ. The treatment of cough: a comprehensive review. Chest. 1991;99(6):1477-1484.230 With permission from Elsevier.
This scoping review has confirmed the psychosocial complications mentioned earlier as well as more broadly identifying physical complications compared with our 2006 report. The physical complications that have been identified, while primarily drawn from case reports and small case series, suggest that coughing can lead to a variety of complications from the relatively minor to those that can be life-threatening or even lead to death. Although the physiologic forces generated by coughing can result in acute and serious injury to an otherwise healthy individual, their effects may be magnified in patients in the following situations, especially when coughing is sustained: compromised by comorbid illnesses or extremes of age; undergoing surgery (eg, ocular) or procedures (eg, bronchoscopy, upper GI endoscopy); recovering from surgery (eg, cardiac or abdominal); and risk from the side-effects of medications (eg, corticosteroids or anticoagulants). Until definitive studies show the way forward, we speculate that it makes physiologic sense that, whenever possible, attempts to control coughing should be made before surgery to avoid wound dehiscence (eg, sternal or abdominal) or extrusion of ocular contents during eye surgery. This review also raises awareness of potential injury to self and others from uncontrolled coughing during automobile driving.
Our study was a scoping review and not a full systematic review; as such, we were able to identify a multitude of complications of cough and to categorize them for future study. The gap in the literature that this review identified is that we do not know how frequent all the complications are or the strength of their association with cough. However, until future research prospectively provides us with the answer, we are left to speculate about the frequency of some of the more common and/or most troublesome complications of chronic cough in those who presented to a Cough Clinic. For example, in our 1991 prospective study that was cited earlier, the frequency of different categories of complications were tabulated (Table 3).230 This table suggested that musculoskeletal adverse events that included rib fracture occurred in 44%, syncopal or near-syncopal events in 5%, and urinary incontinence, primarily in women, in 39%. It is interesting to note that another prospective study of ours, published 26 years later in 2017,87 with the use of the CQLQ, replicated the urinary incontinence finding of the 1991 study in that urinary incontinence, primarily in women, was cough-associated in 38.8% of subjects. Because of the importance of urinary incontinence in women, and especially women with cough,305 it is important to know that the CQLQ is the only commonly used cough quality of life instrument in research studies that specifically asks about this complication.306
Methodologic Considerations
As noted in the Methods section, our initial literature search returned 13,750 citations in PubMed alone. In reviewing the titles and abstracts of this large volume of literature, we noted a complex and heterogeneous nature of the data (eg, variety of complications, diversity of system affected, diversity of nature of evidence, and a diverse origin of the publications by specialty and country). Based on these findings, it was our opinion that the medical community and patients would be best served by our conducting a scoping review, with the intention of clarifying the conceptual boundaries for the next step of study of complications of cough. This was accomplished by identifying key concepts (actual complications) within the research area and by thematically categorizing them to clarify the working definition of complications of cough. Although this review has identified a multitude of potential complications of cough, we were not attempting to quantify the findings or to make recommendations that go beyond facilitating clinician awareness of the multitude and potential serious nature of the various complications and the importance of following the best available evidence for controlling cough. Because most of the complications were gleaned from case reports and small case series, it is possible that some of the complications occurred coincidentally with cough rather than being caused by coughing. That is the reason that we have used the term, associated with coughing, throughout this review. By thematically categorizing the large number of cough complications, we have provided an outline so that future studies of each system or each complication can be conducted. Only then will one be able to describe the findings in a manner that allows specific recommendations for avoiding these complications.
Although ours is not the only recent review of the complications that are associated with cough,307 it is the only one that has followed current established methods,10,11 which is similar to a systemic review because it is transparent, systematic, and replicable.308 This methodologic rigor makes our review different from both our 2006 publication1 and the more recent review.307
In summary, clinicians should not underestimate the impact of coughing to patients due to the potential for serious and life-threatening complications to themselves or to others and the adverse effect on quality of life. It is not an inconsequential problem or concern and should not be trivialized. As noted by Banyai and Joannides,301 in their 1956 seminal review that addressed cough hazards, “the assessment of cough can be made only in light of its possible advantages and harmful implications” and “obviously, there is an urgent need for greater awareness of the potential damage of cough so as to accomplish its satisfactory treatment as well as to prevent its serious sequelae.” Therefore, patients with cough should be evaluated and treated according to evidence-based guidelines to mitigate or prevent the myriad of potential complications associated with coughing.309,310 Additionally, clinicians should also make sure that patients are made aware of the potential unintended consequences of not following recommendations that are intended to ameliorate cough. The myriad complications that can occur from cough indicate the need both for further study and for aggressive treatment of cough when it occurs.
Acknowledgments
Author contributions: All authors had full access to all the data in the study; therefore, all take responsibility for the integrity of the data and the accuracy of the data analysis, including and especially any adverse effects. R. S. I. sered as the principal author. C. L. F. and N. D. contributed substantially to the study design, data analysis, and interpretation, and the writing of the manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following: R. S. I. and C. L. F., as co-developers of the Cough Quality of Life Questionnaire, report that they hold the copyright of this patient-reported outcome measure that is mentioned in this review. None declared (N. D.).
∗CHEST Expert Cough Panel Collaborators: Abd Moain Abu Dabrh, MBBCh, MS (Mayo Clinic, Jacksonville, FL); Kenneth W. Altman, MD, PhD (Geisinger Commonwealth School of Medicine, Danville, PA); Elie Azoulay, MD, PhD (University of Paris, Paris, France); Alan F. Barker, MD (Oregon Health & Science University, Portland, OR); Surinder S. Birring, MBChB, MD (Division of Asthma, Allergy and Lung Biology, King’s College London, Denmark Hill, London, United Kingdom); Donald C. Bolser, PhD, and Louis-Philippe Boulet, MD, FCCP (Institut universitaire de cardiologie et de pneumonlogie de Québec, Quebec, [IUCPQ], QC, Canada); Sidney S. Braman, MD, FCCP (Mount Sinai Hospital, New York, NY); Christopher Brightling, MBBS, PhD, FCCP (University of Leicester, Glenfield Hospital, Leicester, United Kingdom); Brendan Canning, PhD (Johns Hopkins Asthma and Allergy Center, Baltimore, MD); Anne B. Chang, MBBS, PhD, MPH (Royal Children’s Hospital, Queensland, Australia); Terrie Cowley (The TMJ Association, Milwaukee, WI); Paul Davenport, PhD (Department of Physiological Sciences, University of Florida, Gainesville, FL); Ali A. El Solh, MD, MPH (University at Buffalo, State University of New York, Buffalo, NY); Patricio Escalante, MD, FCCP (Mayo Clinic, Rochester, MN); Stephen K. Field, MD (University of Calgary, Calgary, AB, Canada); Dina Fisher, MD, MSc (University of Calgary, Respiratory Medicine, Calgary, AB, Canada); Cynthia T. French, PhD, FCCP (UMass Memorial Medical Center, Worcester, MA); Cameron Grant, MB ChB, PhD (University of Aukland, New Zealand); Susan M. Harding, MD, FCCP (Division of Pulmonary, Allergy and Critical Care Medicine, University of Alabama at Birmingham, Birmingham, AL); Anthony Harnden, MB ChB, MSc (University of Oxford, Oxford, England); Adam T. Hill, MB ChB, MD (Royal Infirmary and University of Edinburgh, Edinburgh, Scotland); Richard S. Irwin, MD, Master FCCP (UMass Memorial Medical Center, Worcester, MA); Vivek Iyer, MD, MPH Mayo Clinic, Rochester MN); Peter J. Kahrilas, MD (Feinberg School of Medicine, Northwestern University, Chicago, IL); Joanne Kavanagh, MBChB (Division of Asthma, Allergy and Lung Biology, King’s College London); Denmark Hill, London, United Kingdom); Karina A. Keogh, MD (Mayo Clinic, Rochester, MN); Kefang Lai, MD, PhD (First Affiliated Hospital of Guangzhou Medical College, Guangzhou, China); Andrew P. Lane, MD (Johns Hopkins University School of Medicine, Baltimore, MD); Kaiser Lim, MD (Mayo Clinic, Rochester, MN); J. Mark Madison, MD, FCCP (UMass Memorial Medical Center, Worcester, MA); Mark A. Malesker, PharmD, FCCP (Creighton University School of Pharmacy and Health Professions, Omaha, NE); Stuart Mazzone, PhD, FCCP (University of Melbourne, Victoria, Australia); Lorcan McGarvey, MD (The Queens University Belfast, Belfast, United Kingdom); Alex Molasoitis, PhD, RN (Hong Kong Polytechnic University, Hong Kong, China); Abigail Moore, BM BCh (University of Oxford, Oxford, England); M. Hassan Murad, MD, MPH (Mayo Clinic, Rochester, MN); Peter Newcombe, PhD (School of Psychology University of Queensland, QLD, Australia); John Oppenheimer, MD (UMDNJ-Rutgers University); Bruce Rubin, MEngr, MD (Virginia Commonwealth University, Richmond, VA); Richard J. Russell, MBBS (University of Leicester, Glenfield Hospital, Leicester, United Kingdom); Jay H. Ryu, MD, FCCP (Mayo Clinic, Rochester, MN); Sonal Singh, MD, MPH (UMass Memorial Medical Center, Worcester, MA); Jaclyn Smith, MB ChB, PhD (University of Manchester, Manchester, England); Susan M. Tarlo, MBBS, FCCP (Toronto Western Hospital, Toronto, ON, Canada); Anne E. Vertigan, PhD, BAppSc (SpPath) (John Hunter Hospital, NSW, Australia).
Other contributions: We thank Nancy Harger, MLS, clinical service librarian who works in the University of Massachusetts Medical School Library, Worcester, MA, who undertook all the searches for this systematic review.
Additional information: The e-Appendix and e-Table can be found in the Supplemental Materials section of the online article.
Footnotes
FUNDING/SUPPORT: The authors have reported to CHEST that no funding was received for this study.
Contributor Information
Richard S. Irwin, Email: Richard.Irwin@umassmemorial.org.
CHEST Expert Cough Panel:
Abd Moain Abu Dabrh, Kenneth W. Altman, Elie Azoulay, Alan F. Barker, Surinder S. Birring, Donald C. Bolser, Louis-Philippe Boulet, Sidney S. Braman, Christopher Brightling, Brendan Canning, Anne B. Chang, Terrie Cowley, Paul Davenport, Ali A. El Solh, Patricio Escalante, Stephen K. Field, Dina Fisher, Cynthia T. French, Cameron Grant, Susan M. Harding, Anthony Harnden, Adam T. Hill, Richard S. Irwin, Vivek Iyer, Peter J. Kahrilas, Joanne Kavanagh, Karina A. Keogh, Kefang Lai, Andrew P. Lane, Kaiser Lim, J. Mark Madison, Mark A. Malesker, Stuart Mazzone, Lorcan McGarvey, Alex Molasoitis, Abigail Moore, M. Hassan Murad, Peter Newcombe, John Oppenheimer, Bruce Rubin, Richard J. Russell, Jay H. Ryu, Sonal Singh, Jaclyn Smith, Susan M. Tarlo, and Anne E. Vertigan
Supplementary Data
References
- 1.Irwin R.S. Complications of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl1):54S–58S. doi: 10.1378/chest.129.1_suppl.54S. [DOI] [PubMed] [Google Scholar]
- 2.Irwin R.S., Baumann M.H., Bolser D.C., et al. Diagnosis and management of cough executive summary: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl1):1S–23S. doi: 10.1378/chest.129.1_suppl.1S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharpey-Schafer E.P. The mechanism of syncope after coughing. BMJ. 1953;2(4841):860–863. doi: 10.1136/bmj.2.4841.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Comroe J.H. Physiology of respiration: an introductory text. (2nd ed.) Yearbook Medical Publishers; Chicago: 1974:. Special acts involving breathing. 230-231. [Google Scholar]
- 5.LoMauro A., Aliverti A. Blood shift during cough: negligible or significant? Front Physiol. 2018;9(501) doi: 10.3389/fphys.2018.00501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wei J.Y., Greene H.L., Weisfeldt M.L. Cough-facilitated conversion of ventricular tachycardia. Am J Cardiol. 1980;45(1):174–176. doi: 10.1016/0002-9149(80)90235-0. [DOI] [PubMed] [Google Scholar]
- 7.Francis C.K., Singh J.B., Polansky B.J. Interruption of aberrant conduction of atrioventricular junctional tachycardia by cough. N Engl J Med. 1972;286(7):357–358. doi: 10.1056/NEJM197202172860707. [DOI] [PubMed] [Google Scholar]
- 8.Irani F., Sanchis J. Inspiration- and cough-induced atrioventricular block. CMAJ. 1971;105(7):735–736. [PMC free article] [PubMed] [Google Scholar]
- 9.Lewis S.Z., Diekemper R.L., French C.T., et al. Methodologies for the development of the management of cough: Chest guideline and expert panel report. Chest. 2014;146(5):1395–1402. doi: 10.1378/chest.14-1484. [DOI] [PubMed] [Google Scholar]
- 10.Tricco A.C., Lillie E., Zarin W., et al. Prisma extension for scoping reviews (prisma-scr): Checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 11.Peters M.D.J., Godfrey C., McInerney P., et al. In: Joanna Briggs Institute Reviewer’s Manual: The Joanna Briggs Institute. Aromataris E., Munn Z., editors. 2017. Chapter 11: Scoping reviews.https://reviewersmanual.joannabriggs.org/ [Google Scholar]
- 12.Stedman’s Medical Dictionary. Complication. Lippincott Williams & Wilkins; Baltimore: 2016. :336. [Google Scholar]
- 13.Runciman W.B. Shared meanings: preferred terms and definitions for safety and quality concepts. Med J Aust. 2006;184(S10):S41–S43. doi: 10.5694/j.1326-5377.2006.tb00360.x. [DOI] [PubMed] [Google Scholar]
- 14.Papadimos T.J., Hofmann J.P. Aortic dissection after forceful coughing. Anaesthesia. 2006;61(1):71–72. doi: 10.1111/j.1365-2044.2005.04487.x. [DOI] [PubMed] [Google Scholar]
- 15.Sharpey-Schafer E.P. Effects of coughing on intrathoracic pressure, arterial pressure and peripheral blood flow. J Physiol. 1953;122(2):351–357. doi: 10.1113/jphysiol.1953.sp005004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCann W.S., Bruce R.A. Tussive syncope; observations on the disease formerly called laryngeal epilepsy, with report of two cases. Arch Intern Med. 1949;84(6):845–856. doi: 10.1001/archinte.1949.00230060002001. [DOI] [PubMed] [Google Scholar]
- 17.McIntosh H.D., Estes E.H., Warren J.V. The mechanism of cough syncope. Am Heart J. 1956;52(1):70–82. doi: 10.1016/0002-8703(56)90119-3. [DOI] [PubMed] [Google Scholar]
- 18.Skolnick J.L., Dines D.E. Tussive syncope. Minn Med. 1969;52(10):1609–1613. [PubMed] [Google Scholar]
- 19.Kerr A., Jr., Derbes V.J. The syndrome of cough syncope. Ann Intern Med. 1953;39(6):1240–1253. doi: 10.7326/0003-4819-39-6-1240. [DOI] [PubMed] [Google Scholar]
- 20.Aliyev F., Kilickesmez K.O., Celiker C., Türkoğlu C. Cough-induced sinus arrest resulting in recurrent episodes of syncope: Is it really transient? J Cardiovasc Med (Hagerstown) 2012;13(7):468–470. doi: 10.2459/JCM.0b013e32833892c4. [DOI] [PubMed] [Google Scholar]
- 21.Baron S.B., Huang S.K. Cough syncope presenting as mobitz type ii atrioventricular block--an electrophysiologic correlation. Pacing Clin Electrophysiol. 1987;10(1):65–69. doi: 10.1111/j.1540-8159.1987.tb05925.x. [DOI] [PubMed] [Google Scholar]
- 22.Choi Y.S., Kim J.J., Oh B.H., et al. Cough syncope caused by sinus arrest in a patient with sick sinus syndrome. Pacing Clin Electrophysiol. 1989;12(6):883–886. doi: 10.1111/j.1540-8159.1989.tb05024.x. [DOI] [PubMed] [Google Scholar]
- 23.Hart G., Oldershaw P.J., Cull R.E., et al. Syncope caused by cough-induced complete atrioventricular block. Pacing Clin Electrophysiol. 1982;5(4):564–566. doi: 10.1111/j.1540-8159.1982.tb02279.x. [DOI] [PubMed] [Google Scholar]
- 24.Lee D., Beldner S., Pollaro F., et al. Cough-induced heart block. Pacing Clin Electrophysiol. 1999;22(8):1270–1271. doi: 10.1111/j.1540-8159.1999.tb00615.x. [DOI] [PubMed] [Google Scholar]
- 25.Littmann L., Miller R.F., Humphrey S.S. Cough drops. J Cardiovasc Electrophysiol. 2002;13(2):198. doi: 10.1046/j.1540-8167.2002.00198.x. [DOI] [PubMed] [Google Scholar]
- 26.Lopez-Candales A. Post-tussive sinus node slowing. Am J Geriatr Cardiol. 2001;10(2):102–103. doi: 10.1111/j.1076-7460.2001.90843.x. [DOI] [PubMed] [Google Scholar]
- 27.McIntyre W.F., Green M.S. Electrocardiographical clues to a mechanism of pre-syncope. Cardiol J. 2009;16(5):479–480. [PubMed] [Google Scholar]
- 28.Omori I., Yamada C., Inoue D., et al. Tachyarrhythmia provoked by coughing and other stimuli. Chest. 1984;86(5):797–799. doi: 10.1378/chest.86.5.797. [DOI] [PubMed] [Google Scholar]
- 29.Reisin L., Blaer Y., Jafari J., et al. Cough-induced nonsustained ventricular tachycardia. Chest. 1994;105(5):1583–1584. doi: 10.1378/chest.105.5.1583. [DOI] [PubMed] [Google Scholar]
- 30.Ruckdeschel E.S., Wolfel E., Nguyen D.T. A case of cough-induced ventricular tachycardia in a patient with a left ventricular assist device. Card Electrophysiol Clin. 2016;8(1):165–167. doi: 10.1016/j.ccep.2015.10.019. [DOI] [PubMed] [Google Scholar]
- 31.Sivam S., Yozghatlian V., Dentice R., et al. Spontaneous coronary artery dissection associated with coughing. J Cyst Fibros. 2014;13(2):235–237. doi: 10.1016/j.jcf.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 32.Yirerong J.A., Hurlburt H. Spontaneous coronary artery dissection in a man with intense coughing spasms. BMJ Case Rep. 2018;2018 doi: 10.1136/bcr-2018-225932. bcr2018225932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maury J.M., Pasquer A., Koffel C., et al. Cardiac luxation in icu after coughing effort following right pneumonectomy. Intensive Care Med. 2016;42(6):1071–1072. doi: 10.1007/s00134-015-4128-z. [DOI] [PubMed] [Google Scholar]
- 34.Butman S.M. Coughing-induced stress cardiomyopathy. Catheter Cardiovasc Interv. 2010;76(3):388–390. doi: 10.1002/ccd.22478. [DOI] [PubMed] [Google Scholar]
- 35.Ahn K.S., Yoo K., Cha I.H., et al. Spontaneously migrated tip of an implantable port catheter into the axillary vein in a patient with severe cough and the subsequent intervention to reposition it. Korean J Radiol. 2008;9(suppl):S81–S84. doi: 10.3348/kjr.2008.9.s.s81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bartel T., Bonatti J.O., Muller S. Device dislocation, probably due to paroxysmal coughing early after percutaneous closure of secundum type atrial septal defect. Am J Cardiol. 2008;101(4):548–549. doi: 10.1016/j.amjcard.2007.08.059. [DOI] [PubMed] [Google Scholar]
- 37.Cogbill T.H., Keimowitz R.M. Injection port silastic catheter dislodgement caused by tussive (cough) paroxysm. Wis Med J. 1987;86(11):21–22. [PubMed] [Google Scholar]
- 38.Dubey P., Prasad R.R. Expulsion of a peripherally placed “central” line by coughing. Anaesthesia. 2005;60(2):208–209. doi: 10.1111/j.1365-2044.2004.04103.x. [DOI] [PubMed] [Google Scholar]
- 39.Wu P.Y., Yeh Y.C., Huang C.H., et al. Spontaneous migration of a port-a-cath catheter into ipsilateral jugular vein in two patients with severe cough. Ann Vasc Surg. 2005;19(5):734–736. doi: 10.1007/s10016-005-4638-1. [DOI] [PubMed] [Google Scholar]
- 40.Jacobs W.R., Zaroukian M.H. Coughing and central venous catheter dislodgement. JPEN J Parenter Enteral Nutr. 1991;15(4):491–493. doi: 10.1177/0148607191015004491. [DOI] [PubMed] [Google Scholar]
- 41.Ishii K., Koga Y., Araki K. Idiopathic pneumopericardium induced by forced coughing during coronary arteriography. Jpn Circ J. 1987;51(2):157–159. doi: 10.1253/jcj.51.157. [DOI] [PubMed] [Google Scholar]
- 42.Irwin R.S., Rosen M.J., Braman S.S. Cough. A comprehensive review. Arch Intern Med. 1977;137(9):1186–1191. doi: 10.1001/archinte.137.9.1186. [DOI] [PubMed] [Google Scholar]
- 43.Kravitz P. The clinical picture of “cough purpura,” benign and non-thrombocytopenic eruption. Va Med. 1979;106(5):373–374. [PubMed] [Google Scholar]
- 44.Ramneesh G., Sheerin S., Surinder S., et al. A prospective study of predictors for post laparotomy abdominal wound dehiscence. J Clin Diagn Res. 2014;8(1):80–83. doi: 10.7860/JCDR/2014/7348.3921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Santarpino G., Pfeiffer S., Concistre G., et al. Sternal wound dehiscence from intense coughing in a cardiac surgery patient: vould it be prevented? G Chir. 2013;34(4) 112-111. [PMC free article] [PubMed] [Google Scholar]
- 46.Abid Q., Podila S.R., Kendall S. Sternal dehiscence after cardiac surgery and ace inhibitors [correction of ace type 1 inhibition] Eur J Cardiothorac Surg. 2001;20(1):203–204. doi: 10.1016/s1010-7940(01)00761-8. [DOI] [PubMed] [Google Scholar]
- 47.Hjalmarsson S., Asmundsson T., Sigurdsson J., et al. Major hemorrhage as a complication of cough fracture. Chest. 1993;104(4):1310. doi: 10.1378/chest.104.4.1310a. [DOI] [PubMed] [Google Scholar]
- 48.Jabr F.I., Skeik N. Spontaneous lateral abdominal wall hematoma complicating chronic obstructive pulmonary disease exacerbation. J Med Liban. 2011;59(3):160–161. [PubMed] [Google Scholar]
- 49.Kosalka J., Wawrzycka-Adamczyk K., Jurkiewicz P., et al. Cough-induced lung intercostal hernia. Pneumonol Alergol Pol. 2016;84(2):119–120. doi: 10.5603/PiAP.2016.0011. [DOI] [PubMed] [Google Scholar]
- 50.Tseng C.K., Tseng Y.C., Chen W.K., et al. A rare complication of cough. Intern Med. 2007;46(15):1269–1270. doi: 10.2169/internalmedicine.46.0216. [DOI] [PubMed] [Google Scholar]
- 51.Macias-Robles M.D., Peliz M.G., Gonzalez-Ordonez A.J. Prophylaxis with enoxaparin can produce a giant abdominal wall haematoma when associated with low doses of aspirin among elderly patients suffering cough attacks. Blood Coagul Fibrinolysis. 2005;16(3):217–219. doi: 10.1097/01.mbc.0000164433.43911.4f. [DOI] [PubMed] [Google Scholar]
- 52.Ozlu M.F., Ayhan S.S., Ozturk S., et al. Abdominal wall hematoma related to severe cough in a patient under antiaggregant and anticoagulant therapy. Intern Emerg Med. 2012;7(suppl 2):S157–S158. doi: 10.1007/s11739-012-0781-1. [DOI] [PubMed] [Google Scholar]
- 53.Cho R., Zamora F., Dincer H.E. Anteromedial arytenoid subluxation due to severe cough. J Bronchology Interv Pulmonol. 2018;25(1):57–59. doi: 10.1097/LBR.0000000000000403. [DOI] [PubMed] [Google Scholar]
- 54.Nerurkar N., Chhapola S. Arytenoid subluxation after a bout of coughing: a rare case. Am J Otolaryngol. 2012;33(2):275–278. doi: 10.1016/j.amjoto.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 55.Maqsood U., Ganaie M.B., Hasan M.I., et al. Unusual case of bilateral haemotympanum after endobronchial ultrasound-guided transbronchial fine needle aspiration (ebus-tbna) BMJ Case Rep. 2018;2018 doi: 10.1136/bcr-2018-225696. bcr2018225696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fenig M., Strasberg S., Cohen J.C., et al. Laryngeal fracture after coughing. Am J Emerg Med. 2013;31(9):1421.e1421–1421.e1423. doi: 10.1016/j.ajem.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 57.Nensa F., Stylianou E., Schroeder T. Progressive dyspnea after a heavy coughing attack. Gastroenterology. 2013;144(3):e9–e10. doi: 10.1053/j.gastro.2012.10.026. [DOI] [PubMed] [Google Scholar]
- 58.Lee C.H., Lan C.C., Wang C.C., et al. Spontaneous rupture of gastroduodenal artery pseudoaneurysm following vigorous cough. Am J Gastroenterol. 2009;104(2):529–530. doi: 10.1038/ajg.2008.52. [DOI] [PubMed] [Google Scholar]
- 59.Paterson W.G., Murat B.W. Combined ambulatory esophageal manometry and dual-probe ph-metry in evaluation of patients with chronic unexplained cough. Dig Dis Sci. 1994;39(5):1117–1125. doi: 10.1007/BF02087567. [DOI] [PubMed] [Google Scholar]
- 60.Ulla J.L., Almohalla C., Ledo L., et al. Coughing attacks as a cause of gastric hemorrhage in patients who have undergone percutaneous endoscopic gastrostomy: sn endoscopic solution. Endoscopy. 2001;33(9):821. doi: 10.1055/s-2001-16524. [DOI] [PubMed] [Google Scholar]
- 61.Wurm Johansson G., Nemeth A., Nielsen J., et al. Gastric rupture as a rare complication in diagnostic upper gastrointestinal endoscopy. Endoscopy. 2013;45(suppl 2 UCTN):E391. doi: 10.1055/s-0033-1344873. [DOI] [PubMed] [Google Scholar]
- 62.Shutsha E., Brenard R. Hepatic cyst rupture after a coughing fit. J Hepatol. 2003;38(6):870. doi: 10.1016/s0168-8278(03)00082-5. [DOI] [PubMed] [Google Scholar]
- 63.Kara E., Kaya Y., Zeybek R., et al. A case of a diaphragmatic rupture complicated with lacerations of stomach and spleen caused by a violent cough presenting with mediastinal shift. Ann Acad Med Singapore. 2004;33(5):649–650. [PubMed] [Google Scholar]
- 64.Sanyal A., Jefferson P.A., Kirby D.F. Percutaneous endoscopic gastrostomy button malfunction with severe cough. Gastrointest Endosc. 1989;35(2):118–119. doi: 10.1016/s0016-5107(89)72725-5. [DOI] [PubMed] [Google Scholar]
- 65.Weaver D.H., Maxwell J.G., Castleton K.B. Mallory-weiss syndrome. Am J Surg. 1969;118(6):887–892. doi: 10.1016/0002-9610(69)90252-9. [DOI] [PubMed] [Google Scholar]
- 66.Annunziata G.M., Gunasekaran T.S., Berman J.H., et al. Cough-induced mallory-weiss tear in a child. Clin Pediatr (Phila) 1996;35(8):417–419. doi: 10.1177/000992289603500808. [DOI] [PubMed] [Google Scholar]
- 67.Sengar M., Neogi S., Mohta A. Prolapse of the rectum associated with spontaneous rupture of the distal colon and evisceration of the small intestine through the anus in an infant. J Pediatr Surg. 2008;43(12):2291–2292. doi: 10.1016/j.jpedsurg.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 68.Leung T.Y., Yuen P.M. Small bowel herniation through subumbilical port site following laparoscopic surgery at the time of reversal of anesthesia. Gynecol Obstet Invest. 2000;49(3):209–210. doi: 10.1159/000010248. [DOI] [PubMed] [Google Scholar]
- 69.Stupnik T., Vidmar S., Hari P. Spontaneous rupture of a normal spleen following bronchoplastic left lung lower lobectomy. Interact Cardiovasc Thorac Surg. 2008;7(2):290–291. doi: 10.1510/icvts.2007.165803. [DOI] [PubMed] [Google Scholar]
- 70.Toubia N.T., Tawk M.M., Potts R.M., et al. Cough and spontaneous rupture of a normal spleen. Chest. 2005;128(3):1884–1886. doi: 10.1378/chest.128.3.1884. [DOI] [PubMed] [Google Scholar]
- 71.Wehbe E., Raffi S., Osborne D. Spontaneous splenic rupture precipitated by cough: A case report and a review of the literature. Scand J Gastroenterol. 2008;43(5):634–637. doi: 10.1080/00365520701763472. [DOI] [PubMed] [Google Scholar]
- 72.Wergowske G.L., Carmody T.J. Splenic rupture from coughing. Arch Surg. 1983;118(10):1227. doi: 10.1001/archsurg.1983.01390100089024. [DOI] [PubMed] [Google Scholar]
- 73.Won A.C., Ethell A. Spontaneous splenic rupture resulted from infectious mononucleosis. Int J Surg Case Rep. 2012;3(3):97–99. doi: 10.1016/j.ijscr.2011.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Karabulut Z., Dogan P. Conservative management of spontaneous retroperitoneal bleeding after severe coughing. Turk J Gastroenterol. 2014;25(6):733–734. doi: 10.5152/tjg.2014.6925. [DOI] [PubMed] [Google Scholar]
- 75.Ma H.R., Yang Y.H., Chiang B.L. Clinical observation between chronic sustained cough with asthma and childhood inguinal hernia. J Microbiol Immunol Infect. 2003;36(4):275–277. [PubMed] [Google Scholar]
- 76.Papanikitas J., Sutcliffe R.P., Rohatgi A., et al. Bilateral retrovascular femoral hernia. Ann R Coll Surg Engl. 2008;90(5):423–424. doi: 10.1308/003588408X301235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ozge C., Atis S., Ozge A., et al. Cough headache: frequency, characteristics and the relationship with the characteristics of cough. Eur J Pain. 2005;9(4):383–388. doi: 10.1016/j.ejpain.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 78.Park Y., Chung M., Lee M.A. Traumatic lumbar hernia: clinical features and management. Ann Surg Treat Res. 2018;95(6):340–344. doi: 10.4174/astr.2018.95.6.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sanjay P., Woodward A. Single strenuous event: does it predispose to inguinal herniation? Hernia. 2007;11(6):493–496. doi: 10.1007/s10029-007-0253-0. [DOI] [PubMed] [Google Scholar]
- 80.Vasquez J.C., Halasz N.A., Chu P. Traumatic abdominal wall hernia caused by persistent cough. South Med J. 1999;92(9):907–908. doi: 10.1097/00007611-199909000-00011. [DOI] [PubMed] [Google Scholar]
- 81.Lord R. Factors predisposing to inguinal hernia: an analysis of 1,100 cases. Aust N Z J Surg. 1968;37(4):377–381. [PubMed] [Google Scholar]
- 82.el-Hammady S., Ghoneim M. Acute complete inversion of the bladder. BMJ. 1971;3(5769):306–307. doi: 10.1136/bmj.3.5769.306-d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lee Y.J., Chiang Y.F., Tsai J.C. Severe nonproductive cough and cough-induced stress urinary incontinence in diabetic postmenopausal women treated with ace inhibitor. Diabetes Care. 2000;23(3):427–428. doi: 10.2337/diacare.23.3.427. [DOI] [PubMed] [Google Scholar]
- 84.Reichman G., De Boe V., Braeckman J., et al. Urinary incontinence in patients with cystic fibrosis. Scand J Urol. 2016;50(2):128–131. doi: 10.3109/21681805.2015.1096826. [DOI] [PubMed] [Google Scholar]
- 85.Swenson C.W., Kolenic G.E., Trowbridge E.R., et al. Obesity and stress urinary incontinence in women: Compromised continence mechanism or excess bladder pressure during cough? Int Urogynecol J. 2017;28(9):1377–1385. doi: 10.1007/s00192-017-3279-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.French C.T., Fletcher K.E., Irwin R.S. Gender differences in health-related quality of life in patients complaining of chronic cough. Chest. 2004;125(2):482–488. doi: 10.1378/chest.125.2.482. [DOI] [PubMed] [Google Scholar]
- 87.French C.L., Crawford S.L., Bova C., et al. Change in psychological, physiological, and situational factors in adults after treatment of chronic cough. Chest. 2017;152(3):547–562. doi: 10.1016/j.chest.2017.06.024. [DOI] [PubMed] [Google Scholar]
- 88.Ben Safta Y., Ghalleb M., Baccari A., et al. Vaginal cuff dehiscence and evisceration 11 years after a radical hysterectomy: a case report. Int J Surg Case Rep. 2017;41:234–237. doi: 10.1016/j.ijscr.2017.10.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gradwohl J.R., Mailliard J.A. Cough induced avulsion of the lesser trochanter. Nebr Med J. 1987;72(8):280–281. [PubMed] [Google Scholar]
- 90.Altman A.M., Akers D. Rectus sheath hematoma secondary to a tussive paroxysm. J La State Med Soc. 2007;159(5):250–251. [PubMed] [Google Scholar]
- 91.Anderton R.L. Rectus abdominal muscles pulled by coughing. JAMA. 1972;222(4):486. [PubMed] [Google Scholar]
- 92.Bayram B., Oray N.C., Acara C.A. Old man with groin bruising. West J Emerg Med. 2014;15(7):872–873. doi: 10.5811/westjem.2014.8.16095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cosgun I.G., Unal Y., Cetin M. Rectus sheath hematoma due to cough in an elderly patient under antiplatelet therapy. Clin Respir J. 2015;9(2):247–249. doi: 10.1111/crj.12109. [DOI] [PubMed] [Google Scholar]
- 94.Elango K., Murthi S., Devasahayam J., et al. Spontaneous rectus sheath haematoma due to cough on apixaban. BMJ Case Rep. 2018;2018 doi: 10.1136/bcr-2018-225136. bcr2018225136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Nelwan E.J., Angelina F., Adiwinata R., et al. Spontaneous rectus sheath hematomas in dengue hemorrhagic fever: a case report. IDCases. 2017;10:35–37. doi: 10.1016/j.idcr.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Patel S., Thyagarajan B., Lalani I. Spontaneous rectus sheath haematoma secondary to severe coughing in a patient with no other precipitating factors. BMJ Case Rep. 2016;2016 doi: 10.1136/bcr-2016-214362. :bcr2016214362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Stillman K., Kellar J. Rectus sheath hematoma: An unfortunate consequence of novel anticoagulants. West J Emerg Med. 2015;16(3):420–421. doi: 10.5811/westjem.2015.2.25631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Schen R.J., Zurkowski S. Increased serum creatine phosphokinase activity with violent coughing. N Engl J Med. 1973;289(6):328–329. doi: 10.1056/nejm197308092890624. [DOI] [PubMed] [Google Scholar]
- 99.Horsburgh A.G. Rupture of the rectus abdominis muscle. BMJ. 1962;2(5309):898. doi: 10.1136/bmj.2.5309.898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Love W. Rupture of rectus abdominis muscle. BMJ. 1962;2(5312):1130. [Google Scholar]
- 101.McCarthy D., Durkin T.E. Rupture of the rectus abdominis muscle. BMJ. 1963;1(5322):58–59. doi: 10.1136/bmj.1.5322.58-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ducatman B.S., Ludwig J., Hurt R.D. Fatal rectus sheath hematoma. JAMA. 1983;249(7):924–925. [PubMed] [Google Scholar]
- 103.Lee T.M., Greenberger P.A., Nahrwold D.L., et al. Rectus sheath hematoma complicating an exacerbation of asthma. J Allergy Clin Immunol. 1986;78(2):290–292. doi: 10.1016/s0091-6749(86)80078-1. [DOI] [PubMed] [Google Scholar]
- 104.Nakanishi H., Iwasaki S., Ohkawa Y., et al. Diaphragmatic rupture due to violent cough during tracheostomy. Auris Nasus Larynx. 2010;37(1):121–124. doi: 10.1016/j.anl.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 105.Reper P., Knafel M., Faraoni D., et al. Cough-induced rupture of the right diaphragm and abdominal herniation. Intensive Care Med. 2012;38(7):1237–1238. doi: 10.1007/s00134-012-2543-y. [DOI] [PubMed] [Google Scholar]
- 106.Kallay N., Crim L., Dunagan D.P., et al. Massive left diaphragmatic separation and rupture due to coughing during an asthma exacerbation. South Med J. 2000;93(7):729–731. [PubMed] [Google Scholar]
- 107.Wang Y., Shao F., Zhang L., et al. Increased 18f-fdg uptake in multiple muscles in a patient with violent cough. Clin Nucl Med. 2017;42(6):451–453. doi: 10.1097/RLU.0000000000001655. [DOI] [PubMed] [Google Scholar]
- 108.Cherian S.V., Ocazionez D., Estrada Y.M.R.M. Spontaneous lung hernia secondary to persistent cough: A rare entity. Arch Bronconeumol. 2018;54(2):101. doi: 10.1016/j.arbres.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 109.O’Shea M., Cleasby M. Images in clinical medicine: lung herniation after cough-induced rupture of intercostal muscle. N Engl J Med. 2012;366(1):74. doi: 10.1056/NEJMicm1106070. [DOI] [PubMed] [Google Scholar]
- 110.Tack D., Wattiez A., Schtickzelle J.C., et al. Spontaneous lung herniation after a single cough. Eur Radiol. 2000;10(3):500–502. doi: 10.1007/s003300050084. [DOI] [PubMed] [Google Scholar]
- 111.Habib A., Elsayed H., Dhanji A.R., et al. Spontaneous combined lung and bowel hernia following an episode of acute bronchitis. Interact Cardiovasc Thorac Surg. 2010;10(6):1042–1043. doi: 10.1510/icvts.2009.231845. [DOI] [PubMed] [Google Scholar]
- 112.De Luca G., Martucci N., La Rocca A., et al. Lung herniation: an unusual cause. Eur J Cardiothorac Surg. 2015;48(4):634–635. doi: 10.1093/ejcts/ezv022. [DOI] [PubMed] [Google Scholar]
- 113.Khan A.S., Bakhshi G.D., Khan A.A., et al. Transdiaphragmatic intercostal hernia due to chronic cough. Indian J Gastroenterol. 2006;25(2):92–93. [PubMed] [Google Scholar]
- 114.Yu W.Y., Wang C.P., Ng K.C., et al. Successful embolization of a ruptured intercostal artery after violent coughing. Am J Emerg Med. 2006;24(2):247–249. doi: 10.1016/j.ajem.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 115.Jang J.Y., Lim Y.S., Woo J.H., et al. Spontaneous rupture of intercostal artery after severe cough. Am J Emerg Med. 2015;33(1) doi: 10.1016/j.ajem.2014.06.033. 131.e131-133. [DOI] [PubMed] [Google Scholar]
- 116.Pareja Lopez A., Martin Esteve I.M., Alvarez Garcia A.F. Intercostal bleeding due to persistent cough in a case of acute exacerbation of copd: selective treatment by arterial embolization. Med Clin (Barc) 2017;148(8):384–385. doi: 10.1016/j.medcli.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 117.Han Y.M., Yoo J.H., Suh J.S. Sonographic appearance of a tear of the lateral internal oblique muscle resulting from cough. J Clin Ultrasound. 2005;33(9):471–473. doi: 10.1002/jcu.20170. [DOI] [PubMed] [Google Scholar]
- 118.Kodama K., Takase Y., Yamamoto H., et al. Cough-induced internal oblique hematoma. J Emerg Trauma Shock. 2013;6(2):132–134. doi: 10.4103/0974-2700.110789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Laitinen H., Kivikanervo K., Vareniskanen M. Coughing osteophytes of the ribs. Ann Med Intern Fenn. 1954;43(4):293–297. [PubMed] [Google Scholar]
- 120.Begley A., Wilson D.S., Shaw J. Cough fracture of the first rib. Injury. 1995;26(8):565–566. doi: 10.1016/0020-1383(95)00098-t. [DOI] [PubMed] [Google Scholar]
- 121.Bodenheimer J.M. Fractured ribs from coughing. New Orleans Med Surg J. 1948;100(10):474. [PubMed] [Google Scholar]
- 122.De Maeseneer M., De Mey J., Debaere C., et al. Rib fractures induced by coughing: an unusual cause of acute chest pain. Am J Emerg Med. 2000;18(2):194–197. doi: 10.1016/s0735-6757(00)90019-6. [DOI] [PubMed] [Google Scholar]
- 123.Dean N.C., Van Boerum D.H., Liou T.G. Rib plating of acute and sub-acute non-union rib fractures in an adult with cystic fibrosis: a case report. BMC Res Notes. 2014;7:681. doi: 10.1186/1756-0500-7-681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Fein B.T. Repeated multiple fractures of ribs by cough in bronchial asthma. J Allergy. 1958;29(3):209–213. doi: 10.1016/0021-8707(58)90003-0. [DOI] [PubMed] [Google Scholar]
- 125.Katrancioglu O., Akkas Y., Arslan S., et al. Spontaneous rib fractures. Asian Cardiovasc Thorac Ann. 2015;23(6):701–703. doi: 10.1177/0218492315586485. [DOI] [PubMed] [Google Scholar]
- 126.Kawahara H., Baba H., Wada M., et al. Multiple rib fractures associated with severe coughing: a case report. Int Orthop. 1997;21(4):279–281. doi: 10.1007/s002640050168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kopcsanyi I., Laczay A., Nagy L. Cough fracture of ribs in infants with dyspnoea. Acta Paediatr Acad Sci Hung. 1969;10(2):93–98. [PubMed] [Google Scholar]
- 128.Litch J.A., Tuggy M. Cough induced stress fracture and arthropathy of the ribs at extreme altitude. Int J Sports Med. 1998;19(3):220–222. doi: 10.1055/s-2007-971908. [DOI] [PubMed] [Google Scholar]
- 129.Long A.E. Stress fracture of the ribs associated with pregnancy. Surg Clin North Am. 1962;42:909–919. doi: 10.1016/s0039-6109(16)36731-7. [DOI] [PubMed] [Google Scholar]
- 130.Lorin M.I., Slovis T.L., Haller J.O. Fracture of ribs in psychogenic cough. N Y State J Med. 1978;78(13):2078–2079. [PubMed] [Google Scholar]
- 131.Musher D.M., Keitel W.A. Severe paroxysmal coughing and pleuritic pain in an adult. Hosp Pract (1995) 1995;30(12):65–67. doi: 10.1080/21548331.1995.11443303. [DOI] [PubMed] [Google Scholar]
- 132.Oren V., Kozenitzky I., Babiacki A., et al. Unusual cough related stress injuries. Eur J Nucl Med. 1988;14(2):108–111. doi: 10.1007/BF00253451. [DOI] [PubMed] [Google Scholar]
- 133.Paulley J.W., Lees D.H., Pearson A.C. Cough fracture in late pregnancy. BMJ. 1949;1(4594):135–137. doi: 10.1136/bmj.1.4594.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Prasad S., Baur L.A. Fracture of the first rib as a consequence of pertussis infection. J Paediatr Child Health. 2001;37(1):91–93. doi: 10.1046/j.1440-1754.2001.00568.x. [DOI] [PubMed] [Google Scholar]
- 135.Roberge R.J., Morgenstern M.J., Osborn H. Cough fracture of the ribs. Am J Emerg Med. 1984;2(6):513–517. doi: 10.1016/0735-6757(84)90077-9. [DOI] [PubMed] [Google Scholar]
- 136.Sano A., Tashiro K., Fukuda T. Cough-induced rib fractures. Asian Cardiovasc Thorac Ann. 2015;23(8):958–960. doi: 10.1177/0218492315596893. [DOI] [PubMed] [Google Scholar]
- 137.Sternfeld M., Hay E., Eliraz A. Postnasal drip causing multiple cough fractures. Ann Emerg Med. 1992;21(5):587. doi: 10.1016/s0196-0644(05)82549-1. [DOI] [PubMed] [Google Scholar]
- 138.Warmington W.T. Four cases of cough fracture. Ulster Med J. 1966;35(1):72–74. [PMC free article] [PubMed] [Google Scholar]
- 139.Yeh C.F., Su S.C. Cough-induced rib fracture in a young healthy man. J Formos Med Assoc. 2012;111(3):179–180. doi: 10.1016/j.jfma.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 140.Derbes V.J., Haran T. Rib fractures from muscular effort with particular reference to cough. Surgery. 1954;35(2):294–321. [PubMed] [Google Scholar]
- 141.Abu-Gazala M., Ratnayake A., Abu-Gazala S., et al. An enigma of spontaneous combined transdiaphragmatic, intercostal and abdominal wall hernia. Hernia. 2013;17(3):415–418. doi: 10.1007/s10029-012-0902-9. [DOI] [PubMed] [Google Scholar]
- 142.Chaar C.I., Attanasio P., Detterbeck F. Disruption of the costal margin with transdiaphragmatic abdominal herniation induced by coughing. Am Surg. 2008;74(4):350–353. [PubMed] [Google Scholar]
- 143.Daniel R., Naidu B., Khalil-Marzouk J. Cough-induced rib fracture and diaphragmatic rupture resulting in simultaneous abdominal visceral herniation into the left hemithorax and subcutaneously. Eur J Cardiothorac Surg. 2008;34(4):914–915. doi: 10.1016/j.ejcts.2008.06.048. [DOI] [PubMed] [Google Scholar]
- 144.Hillenbrand A., Henne-Bruns D., Wurl P. Cough induced rib fracture, rupture of the diaphragm and abdominal herniation. World J Emerg Surg. 2006;1:34. doi: 10.1186/1749-7922-1-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.George L., Rehman S.U., Khan F.A. Diaphragmatic rupture: a complication of violent cough. Chest. 2000;117(4):1200–1201. doi: 10.1378/chest.117.4.1200. [DOI] [PubMed] [Google Scholar]
- 146.Macedo A.C., Kay F.U., Terra R.M., et al. Transdiaphragmatic intercostal hernia: Imaging aspects in three cases. J Bras Pneumol. 2013;39(4):513–517. doi: 10.1590/S1806-37132013000400016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Rogers F.B., Leavitt B.J., Jensen P.E. Traumatic transdiaphragmatic intercostal hernia secondary to coughing: case report and review of the literature. J Trauma. 1996;41(5):902–903. doi: 10.1097/00005373-199611000-00026. [DOI] [PubMed] [Google Scholar]
- 148.Sala C., Bonaldi M., Mariani P., et al. Right post-traumatic diaphragmatic hernia with liver and intestinal dislocation. J Surg Case Rep. 2017;2017(3):rjw220. doi: 10.1093/jscr/rjw220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Butensky A.M., Gruss L.P., Gleit Z.L. Flank pseudohernia following posterior rib fracture: a case report. J Med Case Rep. 2016;10(1):273. doi: 10.1186/s13256-016-1054-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Mary Parks R., Jadoon M., Duffy J. Nontraumatic rupture of the costal margin: a single-center experience. Asian Cardiovasc Thorac Ann. 2019;27(2):105–109. doi: 10.1177/0218492318823367. [DOI] [PubMed] [Google Scholar]
- 151.Oostendorp S.E.V., Buijsman R., Zuidema W.P. Cough-induced nonunion rib fractures and herniation: surgical repair and review. Asian Cardiovasc Thorac Ann. 2018;26(5):416–418. doi: 10.1177/0218492318772769. [DOI] [PubMed] [Google Scholar]
- 152.Ayers D.E., LeFeuvre A., Barker P. Surgical repair of intercostal pulmonary hernia secondary to cough induced rib fracture. J R Nav Med Serv. 2002;88(2):55–56. [PubMed] [Google Scholar]
- 153.Sheka K.P., Williams L.G. Spontaneous intercostal lung hernia. J Natl Med Assoc. 1984;76(12):1210. 1212-1213. [PMC free article] [PubMed] [Google Scholar]
- 154.Sulaiman A., Cottin V., De Souza Neto E.P., et al. Cough-induced intercostal lung herniation requiring surgery: report of a case. Surg Today. 2006;36(11):978–980. doi: 10.1007/s00595-006-3284-8. [DOI] [PubMed] [Google Scholar]
- 155.Franco M., Albano L., Blaimont A., et al. Spontaneous fracture of the lower angle of scapula: possible role of cough. Joint Bone Spine. 2004;71(6):580–582. doi: 10.1016/j.jbspin.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 156.Torrington K.G., Adornato B.T. Cough radiculopathy: another cause of pain in the neck. West J Med. 1984;141(3):379–380. [PMC free article] [PubMed] [Google Scholar]
- 157.Enamorado J.E., Witsch J., Aviles A.H., et al. Neurological picture: acute appearance of a carotid pseudoaneurysm during coughing. J Neurol Neurosurg Psychiatry. 2015;86(1):120. doi: 10.1136/jnnp-2014-308412. [DOI] [PubMed] [Google Scholar]
- 158.Viticchi G., Falsetti L., Baruffaldi R., et al. Acute carotid dissection in an adult caused by pertussis. J Stroke Cerebrovasc Dis. 2013;22(8):e635–e636. doi: 10.1016/j.jstrokecerebrovasdis.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 159.Kau T., Rabitsch E., Celedin S., et al. When coughing can cause stroke: a case-based update on cerebral air embolism complicating biopsy of the lung. Cardiovasc Intervent Radiol. 2008;31(5):848–853. doi: 10.1007/s00270-008-9339-z. [DOI] [PubMed] [Google Scholar]
- 160.Ceponis P.J., Fox W., Tailor T.D., et al. Non-dysbaric arterial gas embolism associated with chronic necrotizing pneumonia, bullae and coughing: a case report. Undersea Hyperb Med. 2017;44(1):73–77. doi: 10.22462/1.2.2017.16. [DOI] [PubMed] [Google Scholar]
- 161.Ulyatt D.B., Judson J.A., Trubuhovich R.V., et al. Cerebral arterial air embolism associated with coughing on a continuous positive airway pressure circuit. Crit Care Med. 1991;19(7):985–987. doi: 10.1097/00003246-199107000-00029. [DOI] [PubMed] [Google Scholar]
- 162.Rivara C.B., Chevrolet J.C., Gasche Y., et al. Fatal brain gas embolism during non-invasive positive pressure ventilation. BMJ Case Rep. 2008;2008 doi: 10.1136/bcr.06.2008.0163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Shugar J.M., Som P.M., Eisman W., et al. Non-traumatic cerebrospinal fluid rhinorrhea. Laryngoscope. 1981;91(1):114–120. [PubMed] [Google Scholar]
- 164.Zlab M.K., Moore G.F., Daly D.T., et al. Cerebrospinal fluid rhinorrhea: a review of the literature. Ear Nose Throat J. 1992;71(7):314–317. [PubMed] [Google Scholar]
- 165.Berciano J., Poca M.A., Garcia A., et al. Paroxysmal cervicobrachial cough-induced pain in a patient with syringomyelia extending into spinal cord posterior gray horns. J Neurol. 2007;254(5):678–681. doi: 10.1007/s00415-006-0412-8. [DOI] [PubMed] [Google Scholar]
- 166.Vaya A., Resureccion M., Ricart J.M., et al. Spontaneous cervical epidural hematoma associated with oral anticoagulant therapy. Clin Appl Thromb Hemost. 2001;7(2):166–168. doi: 10.1177/107602960100700215. [DOI] [PubMed] [Google Scholar]
- 167.Aaronson D.W., Rovner R.N., Patterson R. Cough syncope: case presentation and review. J Allergy. 1970;46(6):359–363. doi: 10.1016/0021-8707(70)90087-0. [DOI] [PubMed] [Google Scholar]
- 168.Ariturk Z., Alici H., Cakici M., et al. A rare cause of syncope: cough. Eur Rev Med Pharmacol Sci. 2012;16(Suppl 1):71–72. [PubMed] [Google Scholar]
- 169.Awad J., Schiller O. Cough syncope with herpetic tracheobronchitis. Isr Med Assoc J. 2001;3(4):284–285. [PubMed] [Google Scholar]
- 170.Benditt D.G., Samniah N., Pham S., et al. Effect of cough on heart rate and blood pressure in patients with “cough syncope. Heart Rhythm. 2005;2(8):807–813. doi: 10.1016/j.hrthm.2005.04.022. [DOI] [PubMed] [Google Scholar]
- 171.Chadda K.D., Peters R., Bloomfield B., et al. Cough syncope treated with a long-term vasoconstrictor. JAMA. 1986;255(10):1289–1291. [PubMed] [Google Scholar]
- 172.Chen C.T., Lin J.C., Chang S.Y. Cough syncope induced by paraspinal abscess. Am J Med Sci. 2014;347(1):86–87. doi: 10.1097/MAJ.0000000000000201. [DOI] [PubMed] [Google Scholar]
- 173.Derbes V.J., Kerr A., Jr. After-cough fainting as a complication of bronchial asthma. South Med J. 1953;46(7):701–707. doi: 10.1097/00007611-195307000-00015. [DOI] [PubMed] [Google Scholar]
- 174.Dickinson O., Nijjar P.S., Detloff B.L., et al. Vasodepressor cough syncope masked by sleep apnea-induced asystole. J Cardiovasc Electrophysiol. 2012;23(9):1024–1027. doi: 10.1111/j.1540-8167.2012.02305.x. [DOI] [PubMed] [Google Scholar]
- 175.Fitzsimons M.G. Case report: cough syncope in a U.S. Army aviator. Aviat Space Environ Med. 1998;69(5):515–516. [PubMed] [Google Scholar]
- 176.Gelisse P., Genton P. Cough syncope misinterpreted as epileptic seizure. Epileptic Disord. 2008;10(3):223–224. doi: 10.1684/epd.2008.0204. [DOI] [PubMed] [Google Scholar]
- 177.Haslam R.H., Freigang B. Cough syncope mimicking epilepsy in asthmatic children. Can J Neurol Sci. 1985;12(1):45–47. doi: 10.1017/s0317167100046576. [DOI] [PubMed] [Google Scholar]
- 178.Ireland P.D., Mickelsen D., Rodenhouse T.G., et al. Evaluation of the autonomic cardiovascular response in arnold-chiari deformities and cough syncope syndrome. Arch Neurol. 1996;53(6):526–531. doi: 10.1001/archneur.1996.00550060068018. [DOI] [PubMed] [Google Scholar]
- 179.Ishizuka S., Yanai M., Yamaya M., et al. Cough syncope treated with imidapril in an elderly patient with dysphagia. Chest. 2000;118(1):279. doi: 10.1378/chest.118.1.279. [DOI] [PubMed] [Google Scholar]
- 180.Jenkins P., Clarke S.W. Cough syncope: a complication of adult whooping cough. Br J Dis Chest. 1981;75(3):311–313. doi: 10.1016/0007-0971(81)90012-7. [DOI] [PubMed] [Google Scholar]
- 181.Katz R.M. Cough syncope in children with asthma. J Pediatr. 1970;77(1):48–51. doi: 10.1016/s0022-3476(70)80043-9. [DOI] [PubMed] [Google Scholar]
- 182.Kerr A., Jr., Eich R.H. Cerebral concussion as a cause of cough syncope. Arch Intern Med. 1961;108:248–252. doi: 10.1001/archinte.1961.03620080080008. [DOI] [PubMed] [Google Scholar]
- 183.Krediet C.T., Wieling W., Edward P. Sharpey-schafer was right: evidence for systemic vasodilatation as a mechanism of hypotension in cough syncope. Europace. 2008;10(4):486–488. doi: 10.1093/europace/eun022. [DOI] [PubMed] [Google Scholar]
- 184.Kreitmann L., Collet F., Gouello J.P., et al. Cough syncope and multiple pulmonary nodules. Intern Emerg Med. 2011;6(4):377–379. doi: 10.1007/s11739-011-0532-8. [DOI] [PubMed] [Google Scholar]
- 185.Kusuyama T., Iida H., Kino N., et al. Cough syncope induced by gastroesophageal reflux disease. J Cardiol. 2009;54(2):300–303. doi: 10.1016/j.jjcc.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 186.Linzer M., McFarland T.A., Belkin M., et al. Critical carotid and vertebral arterial occlusive disease and cough syncope. Stroke. 1992;23(7):1017–1020. doi: 10.1161/01.str.23.7.1017. [DOI] [PubMed] [Google Scholar]
- 187.Marinella M.A. A car crash complicating influenza. Mayo Clin Proc. 2004;79(8):1087–1088. doi: 10.4065/79.8.1087-a. [DOI] [PubMed] [Google Scholar]
- 188.Mattle H.P., Nirkko A.C., Baumgartner R.W., et al. Transient cerebral circulatory arrest coincides with fainting in cough syncope. Neurology. 1995;45(3 Pt 1):498–501. doi: 10.1212/wnl.45.3.498. [DOI] [PubMed] [Google Scholar]
- 189.Maznyczka A., Squire I.B. Cough syncope: a diagnosis under pressure. Lancet. 2010;376(9739):486. doi: 10.1016/S0140-6736(10)60754-4. [DOI] [PubMed] [Google Scholar]
- 190.McCorry D.J., Chadwick D.W., Barber P., et al. Cough syncope in heavy goods vehicle drivers. QJM. 2004;97(9):631–632. doi: 10.1093/qjmed/hch100. [DOI] [PubMed] [Google Scholar]
- 191.Mereu R., Taraborrelli P., Sau A., et al. Diagnostic role of head-up tilt test in patients with cough syncope. Europace. 2016;18(8):1273–1279. doi: 10.1093/europace/euv283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.O’Doherty D.S. Tussive syncope and its relation to epilepsy. Neurology. 1953;3(1):16–21. doi: 10.1212/wnl.3.1.16. [DOI] [PubMed] [Google Scholar]
- 193.Peters J.T. Tussive unconsciousness. J La State Med Soc. 1961;113:6–8. [PubMed] [Google Scholar]
- 194.Puetz T.R., Vakil N. Gastroesophageal reflux-induced cough syncope. Am J Gastroenterol. 1995;90(12):2204–2206. [PubMed] [Google Scholar]
- 195.Strauss M.J., Longstreth W.T., Jr., Thiele B.L. Atypical cough syncope. JAMA. 1984;251(13):1731. [PubMed] [Google Scholar]
- 196.Styczynski G., Dobosiewicz A., Abramczyk P., et al. Internal jugular vein valve insufficiency in cough syncope. Neurology. 2008;70(10):812–813. doi: 10.1212/01.wnl.0000286951.38908.23. [DOI] [PubMed] [Google Scholar]
- 197.Takazawa T., Ikeda K., Kano O., et al. A case of sinus arrest and post-hiccup cough syncope in medullary infarction. J Stroke Cerebrovasc Dis. 2014;23(3):566–571. doi: 10.1016/j.jstrokecerebrovasdis.2013.04.016. [DOI] [PubMed] [Google Scholar]
- 198.Vincent J.L., Pinsky M.R. Cough-induced syncope. Intensive Care Med. 1988;14(6):591–594. doi: 10.1007/BF00256761. [DOI] [PubMed] [Google Scholar]
- 199.Waldmann V., Combes N., Narayanan K., et al. Cough syncope. Am J Med. 2017;130(7):e295–e296. doi: 10.1016/j.amjmed.2017.01.050. [DOI] [PubMed] [Google Scholar]
- 200.Zeng W., Deng H. Cough syncope: constrictive pericarditis. Intern Med. 2013;52(4):463–465. doi: 10.2169/internalmedicine.52.8818. [DOI] [PubMed] [Google Scholar]
- 201.Tanaka T., Inoue H., Aizawa H., et al. Case of cough syncope with seizure. Respiration. 1994;61(1):48–50. doi: 10.1159/000196303. [DOI] [PubMed] [Google Scholar]
- 202.Hamilton W.F., Woodbury R.A., Harper H.T.J. Arterial, cerebrospinal and venous pressues, in man during cough and strain. Am J Physiol. 1944;141(1):42–50. [Google Scholar]
- 203.Kapoor W.N., Karpf M., Wieand S., et al. A prospective evaluation and follow-up of patients with syncope. N Engl J Med. 1983;309(4):197–204. doi: 10.1056/NEJM198307283090401. [DOI] [PubMed] [Google Scholar]
- 204.White C.W., Zimmerman T.J., Ahmad M. Idiopathic hypertrophic subaortic stenosis presenting as cough syncope. Chest. 1975;68(2):250–253. doi: 10.1378/chest.68.2.250. [DOI] [PubMed] [Google Scholar]
- 205.Larson S.J., Sances A., Jr., Baker J.B., et al. Herniated cerebellar tonsils and cough syncope. J Neurosurg. 1974;40(4):524–528. doi: 10.3171/jns.1974.40.4.0524. [DOI] [PubMed] [Google Scholar]
- 206.Lindegaard K.F., Skalpe I.O., Sjaastad O. Cough syncope: the possible relation to hydrocephalus ex vacuo. Eur Neurol. 1977;15(6):340–344. doi: 10.1159/000114823. [DOI] [PubMed] [Google Scholar]
- 207.Wolman L. Cerebral damage in whooping-cough. BMJ. 1962;2(5307):775–776. doi: 10.1136/bmj.2.5307.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Perini F., Toso V. Benign cough “cluster” headache. Cephalalgia. 1998;18(7):493–494. doi: 10.1046/j.1468-2982.1998.1807493.x. [DOI] [PubMed] [Google Scholar]
- 209.Tsai S., Baig M.S., Abrantes-Pais F., et al. Cough-induced transient ischemic attack treated with revascularization of the external carotid artery. J Vasc Surg. 2014;60(6):1657–1660. doi: 10.1016/j.jvs.2014.06.124. [DOI] [PubMed] [Google Scholar]
- 210.Yagi T., Koizumi Y. 3D analysis of cough-induced nystagmus in a patient with superior semicircular canal dehiscence. Auris Nasus Larynx. 2009;36(5):590–593. doi: 10.1016/j.anl.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 211.Kuczkowski K.M., Benumof J.L. Postoperative cough-induced recurrence of spinal anaesthesia in the parturient. Anaesthesia. 2003;58(1):101. doi: 10.1046/j.1365-2044.2003.296823.x. [DOI] [PubMed] [Google Scholar]
- 212.Bahra A., Goadsby P.J. Cough headache responsive to methysergide. Cephalalgia. 1998;18(7):495–496. doi: 10.1046/j.1468-2982.1998.1807495.x. [DOI] [PubMed] [Google Scholar]
- 213.Buzzi M.G., Formisano R., Colonnese C., et al. Chiari-associated exertional, cough, and sneeze headache responsive to medical therapy. Headache. 2003;43(4):404–406. doi: 10.1046/j.1526-4610.2003.03076.x. [DOI] [PubMed] [Google Scholar]
- 214.Cordenier A., De Hertogh W., De Keyser J., et al. Headache associated with cough: a review. J Headache Pain. 2013;14:42. doi: 10.1186/1129-2377-14-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Ertsey C., Jelencsik I. Cough headache associated with chiari type-i malformation: Responsiveness to indomethacin. Cephalalgia. 2000;20(5):518–520. doi: 10.1046/j.1468-2982.2000.00072.x. [DOI] [PubMed] [Google Scholar]
- 216.Gupta V.K. Ocular compression maneuver aborts benign cough-induced headache. Headache. 2005;45(5):612–614. doi: 10.1111/j.1526-4610.2005.05117_4.x. [DOI] [PubMed] [Google Scholar]
- 217.Pascual J., Gonzalez-Mandly A., Martin R., et al. Headaches precipitated by cough, prolonged exercise or sexual activity: a prospective etiological and clinical study. J Headache Pain. 2008;9(5):259–266. doi: 10.1007/s10194-008-0063-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Pascual J., Iglesias F., Oterino A., et al. Cough, exertional, and sexual headaches: an analysis of 72 benign and symptomatic cases. Neurology. 1996;46(6):1520–1524. doi: 10.1212/wnl.46.6.1520. [DOI] [PubMed] [Google Scholar]
- 219.Pavao Martins I., Viana P. “Cough hemicrania” an overlapping form of headache: case reports. Headache. 2017;57(5):796–800. doi: 10.1111/head.13094. [DOI] [PubMed] [Google Scholar]
- 220.Sansur C.A., Heiss J.D., DeVroom H.L., et al. Pathophysiology of headache associated with cough in patients with chiari i malformation. J Neurosurg. 2003;98(3):453–458. doi: 10.3171/jns.2003.98.3.0453. [DOI] [PubMed] [Google Scholar]
- 221.Stern R.C., Horwitz S.J., Doershuk C.F. Neurologic symptoms during coughing paroxysms in cystic fibrosis. J Pediatr. 1988;112(6):909–912. doi: 10.1016/s0022-3476(88)80213-0. [DOI] [PubMed] [Google Scholar]
- 222.Symonds C. Cough headache. Brain. 1956;79(4):557–568. doi: 10.1093/brain/79.4.557. [DOI] [PubMed] [Google Scholar]
- 223.Williams B. Cough headache due to craniospinal pressure dissociation. Arch Neurol. 1980;37(4):226–230. doi: 10.1001/archneur.1980.00500530064010. [DOI] [PubMed] [Google Scholar]
- 224.Smith W.S., Messing R.O. Cerebral aneurysm presenting as cough headache. Headache. 1993;33(4):203–204. doi: 10.1111/j.1526-4610.1993.hed33040203.x. [DOI] [PubMed] [Google Scholar]
- 225.Sands G.H., Newman L., Lipton R. Cough, exertional, and other miscellaneous headaches. Med Clin North Am. 1991;75(3):733–747. doi: 10.1016/s0025-7125(16)30446-1. [DOI] [PubMed] [Google Scholar]
- 226.Moncada E., Graff-Radford S.B. Cough headache presenting as a toothache: a case report. Headache. 1993;33(5):240–243. doi: 10.1111/j.1526-4610.1993.hed3305240.x. [DOI] [PubMed] [Google Scholar]
- 227.Mahawish K. Cough-induced hemiparesis: an unusual manifestation of cord compression. BMJ Case Rep. 2016;2016 doi: 10.1136/bcr-2016-215537. :bcr2016215537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Rao D.S., Infeld M.D., Stern R.C., et al. Cough-induced hemiplegic migraine with impaired consciousness in cystic fibrosis. Pediatr Pulmonol. 2006;41(2):171–176. doi: 10.1002/ppul.20309. [DOI] [PubMed] [Google Scholar]
- 229.Lin Y.H., Chen S.Y., Liu K.L., et al. Queer consequence of cough: atrial myxoma embolization with acute occlusion of the abdominal aorta. Am J Emerg Med. 2010;28(2):261 e261–262. doi: 10.1016/j.ajem.2009.06.027. [DOI] [PubMed] [Google Scholar]
- 230.Irwin R.S., Curley F.J. The treatment of cough: a comprehensive review. Chest. 1991;99(6):1477–1484. doi: 10.1378/chest.99.6.1477. [DOI] [PubMed] [Google Scholar]
- 231.Morgan-Hughes J.A. Cough seizures in patients with cerebral lesions. BMJ. 1966;2(5512):494–496. doi: 10.1136/bmj.2.5512.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Natelson S.E., Molnar W. Malfunction of ventriculoatrial shunts caused by the circulatory dynamics of coughing. J Neurosurg. 1972;36(3):283–286. doi: 10.3171/jns.1972.36.3.0283. [DOI] [PubMed] [Google Scholar]
- 233.Oertel M.F., Korinth M.C., Reinges M.H., et al. Pneumorrhachis of the entire spinal canal. J Neurol Neurosurg Psychiatry. 2005;76(7):1036. doi: 10.1136/jnnp.2004.044636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Heckman A.J., Mohseni M., Villanueva A., et al. Concurrent spontaneous pneumomediastinum and pneumorrhachis. J Emerg Med. 2018;54(6):e117–e120. doi: 10.1016/j.jemermed.2018.02.036. [DOI] [PubMed] [Google Scholar]
- 235.Migeot M., Kessler R., Etxeberria Izal A., et al. Pneumorrhachis associated with a spontaneous pneumomediastinum. Rev Neurol (Paris) 2013;169(2):173–174. doi: 10.1016/j.neurol.2012.06.019. [DOI] [PubMed] [Google Scholar]
- 236.Tsuji H., Takazakura E., Terada Y., et al. Ct demonstration of spinal epidural emphysema complicating bronchial asthma and violent coughing. J Comput Assist Tomogr. 1989;13(1):38–39. doi: 10.1097/00004728-198901000-00007. [DOI] [PubMed] [Google Scholar]
- 237.Salameh A., Klein M., Klein N., et al. Coughing into the darkness. Lancet. 2011;377(9778):1718. doi: 10.1016/S0140-6736(11)60206-7. [DOI] [PubMed] [Google Scholar]
- 238.Herr R.D., Call G., Banks D. Vertebral artery dissection from neck flexion during paroxysmal coughing. Ann Emerg Med. 1992;21(1):88–91. doi: 10.1016/s0196-0644(05)82248-6. [DOI] [PubMed] [Google Scholar]
- 239.Nomura M., Kannuki S., Kuwayama K., et al. A patient with wallenberg’s syndrome induced by severe cough. J Clin Neurosci. 2004;11(2):179–182. doi: 10.1016/s0967-5868(03)00139-5. [DOI] [PubMed] [Google Scholar]
- 240.Sandford B., Naylor A.R. At the back of my mind. Eur J Vasc Endovasc Surg. 2015;49(6):660. doi: 10.1016/j.ejvs.2015.03.030. [DOI] [PubMed] [Google Scholar]
- 241.Siclari F., Hirt L., Meuli R., et al. Bilateral carotid thrombus formation after strenuous coughing. Eur J Neurol. 2009;16(7):e122–e123. doi: 10.1111/j.1468-1331.2009.02628.x. [DOI] [PubMed] [Google Scholar]
- 242.Romano P. On coughing and the open eye. Ophthalmic Surg. 1983;14(12):1041–1042. [PubMed] [Google Scholar]
- 243.Castelnuovo P., Mauri S., Bignami M. Spontaneous compressive orbital emphysema of rhinogenic origin. Eur Arch Otorhinolaryngol. 2000;257(10):533–536. doi: 10.1007/s004050000289. [DOI] [PubMed] [Google Scholar]
- 244.Reid J.M., Williams D. Panda sign due to severe coughing. J R Coll Physicians Edinb. 2013;43(1):35. doi: 10.4997/JRCPE.2013.107. [DOI] [PubMed] [Google Scholar]
- 245.Rieger G. A rare cause of complete “spectacle hematoma.”. Ger J Ophthalmol. 1996;5(6):415–416. [PubMed] [Google Scholar]
- 246.Marimuthu L.M., Ranjan R., Chandrasekaran V., et al. Sub-conjunctival hemorrhage following a bout of cough: a harbinger of underlying bleeding diathesis. Indian J Pediatr. 2017;84(10):804–805. doi: 10.1007/s12098-017-2358-5. [DOI] [PubMed] [Google Scholar]
- 247.Fajgenbaum M.A.P., Antonakis S.N., Membrey L., et al. Acute retinal detachment induced by the valsalva manoeuvre in morning glory disc anomaly. BMJ Case Rep. 2018;2018 doi: 10.1136/bcr-2017-223131. bcr2017223131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Kashani S., Aslam S.A., Bessant D. Valsalva retinopathy presenting with subhyaloid haemorrhage. Emerg Med J. 2009;26(1):74. doi: 10.1136/emj.2008.058701. [DOI] [PubMed] [Google Scholar]
- 249.Marous C.L., Sioufi K., Shields C.L., et al. Coughing-induced suprachoroidal hemorrhage simulating melanoma in two cases. Retin Cases Brief Rep. 2018;12(4):336–341. doi: 10.1097/ICB.0000000000000502. [DOI] [PubMed] [Google Scholar]
- 250.Pollack A.L., McDonald H.R., Ai E., et al. Massive suprachoroidal hemorrhage during pars plana vitrectomy associated with valsalva maneuver. Am J Ophthalmol. 2001;132(3):383–387. doi: 10.1016/s0002-9394(01)01049-2. [DOI] [PubMed] [Google Scholar]
- 251.Kwong S., Daniel A., Kalra S., et al. Transient cough-induced blindness in temporal arteritis. Neurology. 2006;67(8):1520. doi: 10.1212/01.wnl.0000240062.10793.15. [DOI] [PubMed] [Google Scholar]
- 252.Shaikh A., Ahmado A., James B. Severe cough: a cause of late bleb leak. J Glaucoma. 2003;12(2):181–183. doi: 10.1097/00061198-200304000-00014. [DOI] [PubMed] [Google Scholar]
- 253.Irwin R.S., French C.T., Fletcher K.E. Quality of life in coughers. Pulm Pharmacol Ther. 2002;15(3):283–286. doi: 10.1006/pupt.2002.0347. [DOI] [PubMed] [Google Scholar]
- 254.French C.L., Irwin R.S., Curley F.J., et al. Impact of chronic cough on quality of life. Arch Intern Med. 1998;158(15):1657–1661. doi: 10.1001/archinte.158.15.1657. [DOI] [PubMed] [Google Scholar]
- 255.French C.T., Irwin R.S., Fletcher K.E., et al. Evaluation of a cough-specific quality-of-life questionnaire. Chest. 2002;121(4):1123–1131. doi: 10.1378/chest.121.4.1123. [DOI] [PubMed] [Google Scholar]
- 256.Braido F., Baiardini I., Tarantini F., et al. Chronic cough and qol in allergic and respiratory diseases measured by a new specific validated tool-cciq. J Investig Allergol Clin Immunol. 2006;16(2):110–116. [PubMed] [Google Scholar]
- 257.Deslee G., Burgel P.R., Escamilla R., et al. Impact of current cough on health-related quality of life in patients with copd. Int J Chron Obstruct Pulmon Dis. 2016;11:2091–2097. doi: 10.2147/COPD.S106883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Glaspole I.N., Chapman S.A., Cooper W.A., et al. Health-related quality of life in idiopathic pulmonary fibrosis: data from the australian ipf registry. Respirology. 2017;22(5):950–956. doi: 10.1111/resp.12989. [DOI] [PubMed] [Google Scholar]
- 259.Hrisanfow E., Hagglund D. Impact of cough and urinary incontinence on quality of life in women and men with chronic obstructive pulmonary disease. J Clin Nurs. 2013;22(1-2):97–105. doi: 10.1111/j.1365-2702.2012.04143.x. [DOI] [PubMed] [Google Scholar]
- 260.Newcombe P.A., Sheffield J.K., Petsky H.L., et al. A child chronic cough-specific quality of life measure: development and validation. Thorax. 2016;71(8):695–700. doi: 10.1136/thoraxjnl-2015-207473. [DOI] [PubMed] [Google Scholar]
- 261.Petsios K.T., Priftis K.N., Tsoumakas C., et al. Cough affects quality of life in asthmatic children aged 8-14 more than other asthma symptoms. Allergol Immunopathol (Madr) 2009;37(2):80–88. doi: 10.1016/s0301-0546(09)71109-7. [DOI] [PubMed] [Google Scholar]
- 262.Shirai T., Mikamo M., Shishido Y., et al. Impaired cough-related quality of life in patients with controlled asthma with gastroesophageal reflux disease. Ann Allergy Asthma Immunol. 2012;108(5):379–380. doi: 10.1016/j.anai.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 263.Tashkin D.P., Volkmann E.R., Tseng C.H., et al. Improved cough and cough-specific quality of life in patients treated for scleroderma-related interstitial lung disease: results of scleroderma lung study II. Chest. 2017;151(4):813–820. doi: 10.1016/j.chest.2016.11.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Birring S.S., Prudon B., Carr A.J., et al. Development of a symptom specific health status measure for patients with chronic cough: Leicester cough questionnaire (lcq) Thorax. 2003;58(4):339–343. doi: 10.1136/thorax.58.4.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Mao A., Kammen B.F. Dynamic cervical lung herniation in a 10-year-old girl with cough. Pediatr Radiol. 2007;37(10):1058. doi: 10.1007/s00247-007-0504-3. [DOI] [PubMed] [Google Scholar]
- 266.Candas F., Yildizhan A., Gorur R., et al. Is bilateral chylothorax possible after simple cough? Yes. Asian Cardiovasc Thorac Ann. 2015;23(4):471–473. doi: 10.1177/0218492314540161. [DOI] [PubMed] [Google Scholar]
- 267.Kao P., Fang H.Y., Lu T.Y., et al. Strangulation of chronic transdiaphragmatic intercostal hernia. Ann Thorac Surg. 2014;97(6):e155–e157. doi: 10.1016/j.athoracsur.2014.01.085. [DOI] [PubMed] [Google Scholar]
- 268.Young S., Bitsakou H., Caric D., et al. Coughing can relieve or exacerbate symptoms in asthmatic patients. Respir Med. 1991;85(suppl A):7–12. doi: 10.1016/s0954-6111(06)80246-5. [DOI] [PubMed] [Google Scholar]
- 269.Sloth-Nielsen J., Jurik A.G. Spontaneous intercostal pulmonary hernia with subsegmental incarceration. Eur J Cardiothorac Surg. 1989;3(6):562–564. doi: 10.1016/1010-7940(89)90120-6. [DOI] [PubMed] [Google Scholar]
- 270.Asenjo M., Angelina M. Images in clinical medicine: lung herniation with coughing. N Engl J Med. 2015;372(5):464. doi: 10.1056/NEJMicm1307677. [DOI] [PubMed] [Google Scholar]
- 271.Hamid M., Ghani A.R., Ullah W., et al. Spontaneous lung herniation leading to extensive subcutaneous emphysema, pneumothorax, pneumomediastinum, and pneumopericardium. Cureus. 2018;10(6) doi: 10.7759/cureus.2861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Prasad R., Mukerji P.K., Gupta H. Herniation of the lung. Indian J Chest Dis Allied Sci. 1990;32(2):129–132. [PubMed] [Google Scholar]
- 273.Weissberg D., Refaely Y. Hernia of the lung. Ann Thorac Surg. 2002;74(6):1963–1966. doi: 10.1016/s0003-4975(02)04077-8. [DOI] [PubMed] [Google Scholar]
- 274.Bundy J.T., Pontier P.J. Cough-induced hydrothorax in peritoneal dialysis. Perit Dial Int. 1994;14(3):293. [PubMed] [Google Scholar]
- 275.Curley F.J., Irwin R.S., Pratter M.R., et al. Cough and the common cold. Am Rev Respir Dis. 1988;138(2):305–311. doi: 10.1164/ajrccm/138.2.305. [DOI] [PubMed] [Google Scholar]
- 276.Irwin R.S., Pratter M.R., Holland P.S., et al. Postnasal drip causes cough and is associated with reversible upper airway obstruction. Chest. 1984;85(3):346–352. doi: 10.1378/chest.85.3.346. [DOI] [PubMed] [Google Scholar]
- 277.Dearlove O.R., Bowen J. Air emphysema in the neck after excision of a thyroglossal cyst. Anaesthesia. 2004;59(2):193–194. doi: 10.1111/j.1365-2044.2003.03639.x. [DOI] [PubMed] [Google Scholar]
- 278.Hillman K.M. Severe coughing and pneumoperitoneum. Br Med J (Clin Res Ed) 1982;285(6348):1085. doi: 10.1136/bmj.285.6348.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Alves G.R., Silva R.V., Correa J.R., et al. Spontaneous pneumomediastinum (hamman’s syndrome) J Bras Pneumol. 2012;38(3):404–407. doi: 10.1590/s1806-37132012000300018. [DOI] [PubMed] [Google Scholar]
- 280.Bilir O., Yavasi O., Ersunan G., et al. Pneumomediastinum associated with pneumopericardium and epidural pneumatosis. Case Rep Emerg Med. 2014;2014:275490. doi: 10.1155/2014/275490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Chiba Y., Kakuta H. Massive subcutaneous emphysema, pneumomediastinum, and spinal epidural emphysema as complications of violent coughing: a case report. Auris Nasus Larynx. 1995;22(3):205–208. doi: 10.1016/s0385-8146(12)80061-7. [DOI] [PubMed] [Google Scholar]
- 282.Chua T.C., Brown K.M., Yan T.D. Sinister cause of abdominal wall bruising. ANZ J Surg. 2015;85(7-8):588–589. doi: 10.1111/ans.12459. [DOI] [PubMed] [Google Scholar]
- 283.Franco A.I., Arponen S., Hermoso F., et al. Subcutaneous emphysema, pneumothorax and pneumomediastinum as a complication of an asthma attack. Indian J Radiol Imaging. 2019;29(1):77–80. doi: 10.4103/ijri.IJRI_340_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Khayer B.L. Simple cough as a cause of subcutaneous emphysema. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2014-205123. :bcr2014205123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Park S.J., Park J.Y., Jung J., et al. Clinical manifestations of spontaneous pneumomediastinum. Korean J Thorac Cardiovasc Surg. 2016;49(4):287–291. doi: 10.5090/kjtcs.2016.49.4.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Roe P.F., Kulkarni B.N. Pneumomediastinum in children with cough. Br J Dis Chest. 1967;61(3):147–150. doi: 10.1016/s0007-0971(67)80042-1. [DOI] [PubMed] [Google Scholar]
- 287.Rousie C., Van Damme H., Radermecker M.A., et al. Spontaneous tracheal rupture: a case report. Acta Chir Belg. 2004;104(2):204–208. doi: 10.1080/00015458.2004.11679537. [DOI] [PubMed] [Google Scholar]
- 288.Rydell J.R., Jennings W.K. Emergency cervical mediastinotomy for massive mediastinal emphysema. AMA Arch Surg. 1955;70(5):647–653. doi: 10.1001/archsurg.1955.01270110019004. [DOI] [PubMed] [Google Scholar]
- 289.Sayhan M., Orak M., Ustundag M. Posttussive pneumomediastinum. Lung. 2008;186(6):351. doi: 10.1007/s00408-008-9117-3. [DOI] [PubMed] [Google Scholar]
- 290.Wang H., Nugent W.C. Cough-induced bilateral spontaneous pneumothorax. Ann Thorac Surg. 2010;90(4):1363–1365. doi: 10.1016/j.athoracsur.2010.04.024. [DOI] [PubMed] [Google Scholar]
- 291.Macklin M.T., Macklin C.C. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: an interpretation of the clinical literature in the light of laboratory experiment. Medicine. 1944;23(4):281–358. [Google Scholar]
- 292.Naggar C.Z. Pneumatosis intestinalis following common upper-respiratory-tract infection. JAMA. 1976;235(20):2221–2222. [PubMed] [Google Scholar]
- 293.Glauser F.L., Bartlett R.H. Pneumoperitoneum in association with pneumothorax. Chest. 1974;66(5):536–540. doi: 10.1378/chest.66.5.536. [DOI] [PubMed] [Google Scholar]
- 294.Benedict E.B. Rupture of the bronchus from bronchoscopy during a paroxysm of coughing. JAMA. 1961;178:509–510. doi: 10.1001/jama.1961.73040440023014c. [DOI] [PubMed] [Google Scholar]
- 295.Patolia S., Zahir M., Schmidt F., et al. Bilateral pneumothorax after bronchoscopy without biopsy--a rare complication: case presentation and literature review. J Bronchology Interv Pulmonol. 2012;19(1):57–60. doi: 10.1097/LBR.0b013e3182426243. [DOI] [PubMed] [Google Scholar]
- 296.Roh J.L., Lee J.H. Spontaneous tracheal rupture after severe coughing in a 7-year-old boy. Pediatrics. 2006;118(1):e224–e227. doi: 10.1542/peds.2005-3019. [DOI] [PubMed] [Google Scholar]
- 297.Irwin R.S., Ownbey R., Cagle P.T., et al. Interpreting the histopathology of chronic cough: a prospective, controlled, comparative study. Chest. 2006;130(2):362–370. doi: 10.1378/chest.130.2.362. [DOI] [PubMed] [Google Scholar]
- 298.Lindsley W.G., Pearce T.A., Hudnall J.B., et al. Quantity and size distribution of cough-generated aerosol particles produced by influenza patients during and after illness. J Occup Environ Hyg. 2012;9(7):443–449. doi: 10.1080/15459624.2012.684582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Field S.K., Escalante P., Fisher D.A., et al. Cough due to TB and other chronic infections: CHEST guideline and expert panel report. Chest. 2018;153(2):467–497. doi: 10.1016/j.chest.2017.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Irwin R.S., Widdicombe D.P. In: Textbook of respiratory medicine. 2nd ed. Murray J.F., Nadel J.A., editors. Saunders; Philadelphia: 1994. Cough; pp. 529–544. [Google Scholar]
- 301.Banyai A.L., Joannides M., Jr. Cough hazard. Dis Chest. 1956;29(1):52–61. doi: 10.1378/chest.29.1.52. [DOI] [PubMed] [Google Scholar]
- 302.Weinberger S.E., Braunwald E. In: Harrison’s principles of internal medicine. 14th ed. Fauci A.S., Braunwald E., Isselbacher K.J., et al., editors. McGraw-Hill; New York: 1998. Cough and hemoptysis; pp. 194–198. [Google Scholar]
- 303.Boulet L.P., Coeytaux R.R., McCrory D.C., et al. Tools for assessing outcomes in studies of chronic cough: CHEST guideline and expert panel report. Chest. 2015;147(3):804–814. doi: 10.1378/chest.14-2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Baiardini I., Braido F., Fassio O., et al. A new tool to assess and monitor the burden of chronic cough on quality of life: chronic cough impact questionnaire. Allergy. 2005;60(4):482–488. doi: 10.1111/j.1398-9995.2005.00743.x. [DOI] [PubMed] [Google Scholar]
- 305.Young E.C., Smith J.A. Quality of life in patients with chronic cough. Ther Adv Respir Dis. 2010;4(1):49–55. doi: 10.1177/1753465809358249. [DOI] [PubMed] [Google Scholar]
- 306.Polley L., Yaman N., Heaney L., et al. Impact of cough across different chronic respiratory diseases: comparison of two cough-specific health-related quality of life questionnaires. Chest. 2008;134(2):295–302. doi: 10.1378/chest.07-0141. [DOI] [PubMed] [Google Scholar]
- 307.Schattner A. The wide-ranging spectrum of cough-induced complications and patient harm. Am J Med. 2020;133(5):544-551. [DOI] [PubMed]
- 308.Grant M.J., Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- 309.Irwin R.S., French C.L., Chang A.B., et al. Classification of cough as a symptom in adults and management algorithms: CHEST guideline and expert panel report. Chest. 2018;153(1):196–209. doi: 10.1016/j.chest.2017.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Chang AB, Oppenheimer JJ, Irwin RS; CHEST Expert Cough Panel. Managing chronic cough as a symptom in children and management algorithms: CHEST guideline and expert panel report. Chest. 2020;158(1):303-329. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.