Abstract
Background
Spontaneous coronary artery dissection (SCAD) has emerged as an important cause of acute coronary syndrome (ACS) and sudden cardiac death. Physical or emotional stressors are the most commonly reported triggers for SCAD. Unemployment has been identified as a source of emotional stress and is linked to poor mental and physical health.
Objective
To examine the association between employment status and in-hospital and follow-up adverse cardiovascular events in patients with SCAD.
Methods
We conducted a retrospective, multi-center, observational study of patients undergoing coronary angiography for ACS between January 2011 and December 2017. The total number of patients enrolled was 198,000. Patients were diagnosed with SCAD based on angiographic and intravascular imaging modalities whenever available. There were 83 patients identified with SCAD from 30 medical centers in 4 Arab gulf countries. In-hospital (myocardial infarction, percutaneous intervention, ventricular tachycardia/ventricular fibrillation, cardiogenic shock, death, internal cardioverter/defibrillator placement, dissection extension) and follow-up (myocardial infarction, de novo SCAD, death, spontaneous superior mesenteric artery dissection) cardiac events were compared among those who were employed and those who were not.
Results
The median age of patients in the study was 44 (37- 55) years. There were 42 (50.6%) female patients, and 41 (49.4) male patients. Of the cohort, 50 (60%) of the patients were employed and the remaining 33 (40%) were unemployed. 66% of all men were employed and 76% of all women were unemployed. After adjusting for gender unemployment was associated with worse in-hospital and follow-up cardiac events (adjusted OR 7.1, [1.3, 37.9]), p = 0.021.
Conclusion
Adverse cardiovascular events were significantly worse for patients with SCAD who were unemployed.
Keywords: SCAD, coronary angiography, unemployment, arabian gulf, events, gender
1. INTRODUCTION
Employment can contribute to a person’s livelihood by ensuring a higher living standard [1]. Employment may improve one’s health status by providing psychological stability [2], economic benefits [3], and improved relationships [4]. Conversely, unemployment has been identified as a source of emotional stress and is linked to poor mental and physical health [1]. Also, recent studies demonstrate a correlation between unemployment and the risk of coronary artery disease (CAD) and mortality [5-11]. The effect of unemployment on CAD is not uniform across the exposed population and may vary by geographical region, age-group, sex, ethnicity, income level, and family status [8]. Unemployment rates in Arab Gulf countries have been high in the last 10 years [12], and 39% of patients with CAD in Arab Gulf countries are unemployed [13]. In a western registry the unemployment rate was found to be 79% among all patients with CAD, and 87% in male patients with CAD [14]. In the Kingdom of Saudi Arabia, the unemployment rate is nearly 13%, with a rate of 6.6% for males and 32% for females [15]. A key objective of the Kingdom of Saudi Arabia Vision 2030 is to increase the employment rate of women and reduce the total unemployment rate to 7% [16]. This intervention has the potential to alter the association between employment and the incidence of CAD in the Kingdom. Spontaneous Coronary Artery Dissection (SCAD) is emerging as an important cause of the acute coronary syndrome, especially in young females without conventional coronary risk factors [17-22]. SCAD is defined as an epicardial coronary artery dissection that is noniatrogenic and nontraumatic [23]. The presentation of SCAD is similar to atherosclerotic acute coronary syndrome [19-21, 24-26]. The causes of SCAD are hypothesized to be multifactorial with contributions from underlying arteriopathies, genetic factors, hormonal influences, and systemic inflammatory diseases. These are often compounded by environmental precipitants and stressors [27]. Extreme emotional stress is among the most commonly reported triggers for SCAD [20], more often reported in females than males [18, 28]. Adverse cardiovascular events after SCAD are relatively common and identification of triggers for such is warranted [17, 19, 20, 23-25, 29-31]. The present study aimed to investigate in-hospital and follow-up events in patients with SCAD, stratified by employment status, in four Arab Gulf countries.
2. METHODS
2.1. Study Population and Data Collection
The study was a retrospective, multi-center, observational study of patients undergoing coronary angiography for ACS between January 2011 and December 2017. The total number of patients enrolled was 198,000. All patients with angiographic findings of atherosclerotic plaque rupture or plaque erosion and occlusive thrombus were excluded. Of the remaining 299 patients, 216 had additional exclusion criteria. Excluded were those patients with coronary artery dissection due to blunt trauma, surgical instruments or catheters (153), atherosclerotic coronary plaque dissection (48), and cases with a diagnostic disagreement between the primary and principal cardiologists (15). The remaining 83 patients were diagnosed with SCAD. Thirty centers were represented, including 25 tertiary referral locations and 5 regional hospitals. Study locations were spread across four Arab Gulf countries: The Kingdom of Saudi Arabia (68 SCAD from 25 centers), The United Arab Emirates (8 SCAD from 2 centers), Kuwait (4 SCAD from 2 centers), and Bahrain (3 SCAD from 1 center). The diagnosis of SCAD was based on angiographic and intravascular imaging whenever available, for ambiguous lesions and according to physician discretion. Coronary angiograms were reviewed by the primary cardiologist from each center and confirmed by the principal cardiologist from King Faisal Specialist Hospital and Research Center (Jeddah branch), and if SCAD was confirmed, findings were classified as Type 1, Type 2, or Type 3 angiographic SCAD [32, 33]. Type 1 angiographic SCAD appears as the classic contrast dye staining of the arterial wall with multiple radiolucent lumen with or without the presence of dye hang-up or slow contrast clearing from the lumen. Type 2 angiographic SCAD appears as diffuse (typically 20 to 30 mm) and smooth narrowing that can vary in severity. Type 3 angiographic SCAD mimics atherosclerosis with focal or tubular stenosis. The number of dissected coronary arteries, location, stenosis severity and lesion length were recorded. Verbal consent for study entry was obtained via a phone call to each patient. No patients declined to participate in this registry. The study protocol was approved by the Institutional Review Board of King Faisal Specialist Hospital and Research Center and each of the participating hospitals. In the present analysis, we examined employment status and in-hospital and follow-up events in patients with SCAD. The patients were divided into two groups: those who reported unemployment and those who reported being employed (private, government, or self-employed). All patients remained unemployed or employed throughout the study and follow-up period. No patients reported a change in employment status.
2.2. Clinical Information
Variables included demographic characteristics, atherosclerotic risk factors, potential predisposing and precipitating stressors, marital and socioeconomic status, mental health history, gynecological history, presence of Fibromuscular Dysplasia (FMD), and systemic inflammatory conditions. Routine laboratory studies were obtained during hospitalization. Cardiologists provided an analysis of telemetry and 12-lead electrocardiogram data. For each patient with confirmed SCAD, transthoracic echocardiogram and coronary angiography reports were obtained. Management strategies and in-hospital events were compared between those employed and those unemployed. Our stress questionnaire was simplified as described by Doulah et al. [34]. In-hospital cardiac events were identified as those that were not present on the initial evaluation and occurred after being hospitalized. These included: Ventricular Tachycardia/Ventricular Fibrillation (VT/VF), cardiogenic shock, death, Implantable Cardioverter Defibrillator (ICD) implantation, and dissection extension. Follow-up events were those that occurred post-discharge from the hospital. They included MI, de novo SCAD, death, and spontaneous superior mesenteric artery dissection. Telephone follow-ups were conducted for all patients, as were full reviews of treating physician reports.
2.3. Definitions
Ventricular Arrhythmia (VA) was defined as sustained Ventricular Tachycardia (VT) or Ventricular Fibrillation (VF) assessed by electrocardiogram on admission and during hospitalization. Any episode of VT lasting longer than 30 seconds was considered sustained VT.
Recurrent ventricular arrhythmia was defined as an episode of VA that occurred within four days of hospitalization.
Cardiogenic shock was defined as hypotension with hypoperfusion that occurred during hospitalization post-acute intervention and requiring inotropes support.
De novo coronary artery dissection was defined as a new dissection in different epicardial vessels, with a resolution of the prior dissection in the originally affected vessels.
Extension of the dissection was defined as a continuation of an already-established dissection, either spontaneously or iatrogenically.
2.4. Statistical Analysis
Categorical data were summarized with absolute numbers and percentages. Numeric data were summarized with median and 25th- 75th quartiles. Comparison between different groups was performed using the Chi-square test or Fisher’s exact (if the expected frequency is less than 5) for categorical variables and independent sample t-test or Mann–Whitney U test for continuous variables. A Cox proportional hazard model was used to estimate the hazard ratios and its associated 95% confidence intervals, using the sex difference. A Kaplan-Meier analysis was used to plot the cumulative survival and differences between curves were assessed by the log-rank test. All analyses were performed using (STATA) software, Version (14.2) (StataCorp; College Station, Texas, USA). A p-value of less than 0.05 was considered statistically significant.
3. RESULTS
3.1. Baseline Characteristics of SCAD Patients According to Employment Status
Over a period of six years, eighty-three patients were retrospectively identified. The median follow-up time was 18.8 months (interquartile range: 9.06-40.1 months). As shown in (Table 1), fifty (60%) patients were employed (government, private, and self-employed). The remaining 33 (40%) patients with SCAD were unemployed. Of the 50 patients who were employed, the majority were working in the private sector 31 (62%), and the rest were self-employed 4 (8%) or in the government sector 15 (30%). The median age of patients in the study was 44 (37- 55) years. When comparing those employed and those unemployed, the age difference was not statistically significant (p = 0.36). In the 42 (50.6%) female patients, 76% were unemployed and 24% were employed (p < 0.01). The majority of the study participants were Arab 84.34%. When comparing those employed and unemployed, the difference in Arab ethnicity was statistically significant (p< 0.01). Employed patients were more likely to be married (44/50, 88%), and less likely to be divorced (3/50, 6%) or widowed 2% (1/50, 2%). For those unemployed, 57.6% (19/33) were married, 24% (8/33) were divorced, and 15% (5/33) were widowed, (p < 0.01).
Table 1.
Baseline characteristics of patients with scad according to their employment status.
| - | All Patients (n=83) |
Employed (n=50) Government=15 Private=31 Self-Employed=4 |
Unemployed (n=33) |
P-value |
|---|---|---|---|---|
| Demographics | - | - | - | - |
| Age, yrs | 44 (37- 55) | 42 (37-52) | 49 (34-60) | 0.36 |
| Female gender | 42 (50.6%) | 17 (34%) | 25 (75.75%) | < 0.01 |
| BMI (kg/m2) | 27 (24.8- 30) | 27 (25-30) | 27 (25-33) | 0.33 |
| Arabic ethnicity | 70 (84.34%) | 37 (74%) | 33 (100%) | <0.01 |
| Marital status | - | - | - | <0.01 |
| Divorced | 11 (13.25%) | 3 (6%) | 8 (24.24%) | - |
| Married | 63 (75.9%) | 44 (88%) | 19 (57.57%) | - |
| Single | 3 (3.61%) | 2 (4%) | 1 (3.03%) | - |
| Widowed | 6 (7.23%) | 1(2%) | 5 (15.15%) | - |
| Socio-economic factors | - | - | - | - |
| Secondary education Post-secondary education |
60 (72.29%) 23 (27.71%) |
32 (64%) 18 (36%) |
28 (84.84%) 5 (15.15%) |
0.05 |
| Monthly income ≥10 SAR/month Monthly income <10 SAR/month |
21 (25.30%) 62 (73.70%) |
17 (34%) 33 (66%) |
4 (12.12%) 29 (87.87%) |
0.04 |
| Smoker | 37 (44.58%) | 27 (54%) | 10 (30.30%) | 0.04 |
| Comorbidities | - | - | - | |
| Diabetes Mellitus | - | - | - | 0.77 |
| Insulin dependent diabetes mellitus | 4 (4.82%) | 3 (6%) | 1 (3.03%) | - |
| Non-insulin dependent diabetes mellitus | 17 (20.48%) | 9 (18%) | 8 (24.24%) | - |
| Arterial hypertension | 26 (31.33%) | 16 (32%) | 10 (30.30%) | 1.00 |
| Dyslipidaemia | 32 (38.55%) | 22 (44%) | 10 (30.30%) | 0.25 |
| Cerebral vascular accident | 1 (1.20%) | 1 (2%) | 0 (0.00%) | 1.00 |
| Anxiety | 28 (33.73%) | 13 (26%) | 15 (45.45%) | 0.10 |
| Depression | 12 (14.46%) | 5 (10%) | 7 (21.21%) | 0.21 |
| Migraine | 19 (22.89%) | 9 (18%) | 10 (30.30%) | 0.29 |
| Hypothyroid | 6 (7.23%) | 2 (4%) | 4 (12.12%) | 0.21 |
| Stress factor | - | - | - | 0.51 |
| None | 34 (40.96%) | 22 (44%) | 12 (36.36%) | - |
| Emotional stress | 33 (39.76%) | 16 (32%) | 17 (51.51%) | - |
| Physical stress | 9 (10.84%) | 6 (12%) | 3 (9.09%) | - |
| Combined (Physical & Emotional) stress | 7 (8.43%) | 6 (12%) | 1 (3.03%) | - |
Most patients (74%) had a monthly income of less than 10,000 SAR per month (66% of employed and 88% of unemployed patients). A monthly income greater than 10,000 SAR was reported by 34% of employed and 12% of unemployed patients (p = 0.04). Completion of secondary education was reported by 72% of patients (64% of employed and 85% of unemployed) and 28% reported completion of post-secondary education (36% of employed and 15% of unemployed, p = 0.05). Cardiac risk factors including diabetes mellitus, hypertension, and dyslipidemia were reported in 25%, 31%, and 39% of the cohort's respectively. However, no significant difference was found between employed and unemployed patients with regards to cardiac risk factors (p = 0.77, p = 1.00, and p = 0.25, respectively). Smoking was reported in 45% of patients (54% of employed and 30% of unemployed patients, p = 0.04). Reported anxiety, migraine, depression, and stress were not significantly different between employed and unemployed patients (p = 0.10, p = 0.29, p = 0.21, and p = 0.51, respectively).
3.2. Hospital Presentation and Angiographic Findings
As shown in (Table 2), acute ST segment elevation myocardial infarction (STEMI) was present in 48% of the patients, and 47% presented with non-ST-elevation acute coronary syndrome (NST-ACS). Acute STEMI was more common in the unemployed and NST-ACS was more common in the employed (p = 0.01). The median LV ejection fraction was 45% (40- 55%). There was no statistically significant difference between the two groups with regards to LV ejection fraction (p = 0.45). A reduced LV ejection fraction of less than 35% was found in 14 patients (17%). There was no significant difference between employed and unemployed patients in elevation of cardiac enzymes or elevation of White Blood Cell count (WBC). In terms of coronary vessel distribution, 12% of the patients had Left Main (LM) involvement, 43% of the patients had left anterior descending artery (LAD) involvement, 21.7% of the patients had right coronary artery (RCA) involvement, 9.6% of the patients had left circumflex artery involvement, and 9.6% of the patients had multi-vessel spontaneous coronary artery dissection. Branch vessel involvement was seen in 3.6% of the patients. There was no statically significant difference between the two groups with regards to coronary vessel distribution (p = 0.66). Type I SCAD was present in 52% of patients, type II SCAD in 42%, and type III SCAD in 3.6%. Two (2.4%) patients were felt to have multiple types of dissections. Most commonly, patients had TIMI-3 coronary grade flow in the affected artery (49%), followed by TIMI-2 flow (25%), with no statically significant difference between employed and unemployed patients (p = 0.50 and p = 0.65, respectively). Maximal stenosis severity of 80% (50- 95) and maximal lesion length of 25mm (18- 36) were similar in both groups (p = 0.45 and p = 0.08, respectively).
Table 2.
Hospital presentation and angiographic findings.
| - |
All Patients
(n=83) |
Employed
(n=50) Government=15 Private=31 Self-Employed=4 |
Unemployed
(n=33) |
P-value |
|---|---|---|---|---|
| Hospital presentation | - | - | - | - |
| Ventricular arrhythmia | 10 (12.05%) | 4 (8%) | 6 (18.18%) | 0.19 |
| Acute coronary syndrome | - | - | - | 0.01 |
| Angina | 3 (3.61%) | 2(4%) | 1(3.03%) | - |
| ST-elevation myocardial infarction | 41 (48%) | 22(44%) | 19(57.57%) | - |
| Non-ST-elevation acute coronary syndrome | 39 (46.99%) | 26(52%) | 13(39.39%) | - |
| 2-D Echocardiogram on admission | - | - | - | - |
| Left ventricular ejection fraction (%) Median (IQR) |
0.45 (0.4-0.55) | 0.45 (0.40-0.55) | 0.45 90.38-0.55) | 0.45 |
| LV EF < 0.35 | 14 (16.87%) | 6(12%) | 8(24.24%) | 0.23 |
| Lab test on admission | - | - | - | - |
| White Blood Cell Count (g/L) Median (IQR) |
10 (6.45-12) | 10 (7-11) | 10 (6-12) | 0.68 |
| Troponin (ng/L) Median (IQR) |
2.69 (0.05- 20) | 1.3 (0.1-10.0) | 9.3 (0.0-24.4) | 0.22 |
| Creatine Kinase (U/L) Median (IQR) |
265 (108.5- 737) | 265 (110-567) | 275 (72-900) | 0.84 |
| Creatine Kinase Mycardail Band (μg/L) Median (IQR) |
33 (5.85- 84.5) | 33 (7-72) | 33 (4-127) | 0.88 |
| Angiographic characteristics of the SCAD lesions | - | - | - | - |
| Coronary artery territory involved | - | - | - | 0.66 |
| Left main | 10 (12.05%) | 7 (14%) | 3 (9.09%) | - |
| Left anterior descending | 36 (43.37%) | 21(42%) | 15(45.45%) | - |
| Left circumflex artery | 8 (9.64%) | 5(10%) | 3(9.09%) | - |
| Right coronary artery | 18 (21.69%) | 9(18%) | 9(27.27%) | - |
| Multi-vessel | 8 (9.64%) | 5 (10%) | 3 (9.09%) | - |
| Branch vessel | 3 (3.61%) | 3 (6%) | 0 (00%) | - |
| Lesion characteristics | - | - | - | 0.50 |
| Type 1 | 43 (51.81%) | 24(48%) | 19(57.57%) | - |
| Type 2 | 35 (42.17%) | 24(48%) | 11(33.33%) | - |
| Type 3 | 3 (3.61%) | 1(2%) | 2(6.06%) | - |
| Multi-Type | 2 (2.41%) | 1(2%) | 1(3.03%) | - |
| Thrombolysis in Myocardial Infarction (TIMI) grade flow | - | - | - | 0.65 |
| TIMI 0 | 8 (9.64%) | 5(10%) | 3(9.09%) | - |
| TIMI 1 | 13 (15.68%) | 7(14%) | 6(18.18%) | - |
| TIMI 2 | 21 (25.30%) | 15(30%) | 6(18.18%) | - |
| TIMI 3 | 41 (49.40%) | 23(46%) | 18(54.54%) | - |
| Max stenosis severity (%) | 80 (50- 95) | 80 (50-95) | 90 (60-95) | 0.45 |
| Max dissection length (mm) | 25 (18- 36) | 28 (20-41) | 20 (14-30) | 0.08 |
3.3. Management Strategy
As shown in (Table 3), the management of SCAD was not statistically different between the employed and unemployed groups (p = 0.26). Forty percent of patients had only medical treatment. Over half of the patients underwent coronary revascularization, including percutaneous coronary intervention (53%) and coronary artery bypass grafting (7%). Medications prescribed at discharge and follow-up are shown (Table 3). Both groups received similar discharge medications. All patients in the study were prescribed aspirin. Most patients (91.5%) were prescribed a P2Y12 inhibitor (17 Ticagrelor, 3 Prasugrel and 55 Clopidogrel), 90% received beta-blocker therapy and 85% received statin therapy. By the median follow up time of 18.8 months (interquartile range: 9.06- 40.1 months), there was a major decrease in a P2Y12 inhibitor use (62%). This decrease was similar in the employed and unemployed groups. ACEI or ARB was used in 66% of cases and continued into the follow-up period. Calcium channel blockers and nitroglycerin were used in a minority of patients.
Table 3.
Management strategy.
| - | All Patients (n=83) |
Employed (n=50) Government=15 Private=31 Self-Employed=4 |
Unemployed (n=33) |
P-value |
|---|---|---|---|---|
| Intervention | - | - | - | 0.26 |
| Medical management only | 33 (39.76%) | 22(44%) | 11(33.33%) | - |
| Percutaneous coronary intervention | 44 (53.01%) | 23(46%) | 21(63.63%) | - |
| Coronary artery bypass grafting | 6 (7.23%) | 5(10%) | 1(3.03%) | - |
| Discharge medications [Total No (82)] | Total No (82) | Total No (50) | Total No (32) | - |
| Aspirin | 82 (100%) | 50(100%) | 32(100%) | 1.00 |
| P2Y12 inhibitor | 75 (91.46%) | 44(88%) | 31(96.87%) | 0.14 |
| Beta Blocker | 74 (90.24%) | 46(92%) | 28(87.5%) | 1.00 |
| Calcium Channel Blocker | 9 (10.97%) | 7(14%) | 2(6.25%) | 0.31 |
| Statin | 70 (85.36%) | 45(90%) | 25(78.12%) | 0.36 |
| Angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor blocker (ARB) | 54 (65.85%) | 35(70%) | 19(59.37%) | 0.64 |
| Nitroglycerin | 27 (32.92%) | 15(30%) | 12(37.5%) | 0.63 |
| Follow-up medication [Total No (81)] | Total No (81) | Total No (49) | Total No (32) | - |
| Aspirin | 79 (97.53%) | 47(95.91%) | 32(100%) | 0.52 |
| P2Y12 inhibitor | 50 (61.72%) | 33(67.34%) | 17(%) | 0.25 |
| Beta Blockers | 76 (93.82%) | 46(93.87%) | 30(93.75%) | 1.00 |
| Calcium Channel Blocker | 11 (13.58%) | 5(10.20%) | 6(18.75%) | 0.33 |
| Statins | 64 (79%) | 39(79.59%) | 25(87%) | 1.00 |
| Angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor blocker (ARB) | 53 (65.43%) | 31(63.26%) | 22(68.75%) | 0.64 |
| Nitroglycerin | 13 (16%) | 9(18.36%) | 4(12.5%) | 0.55 |
3.4. Events
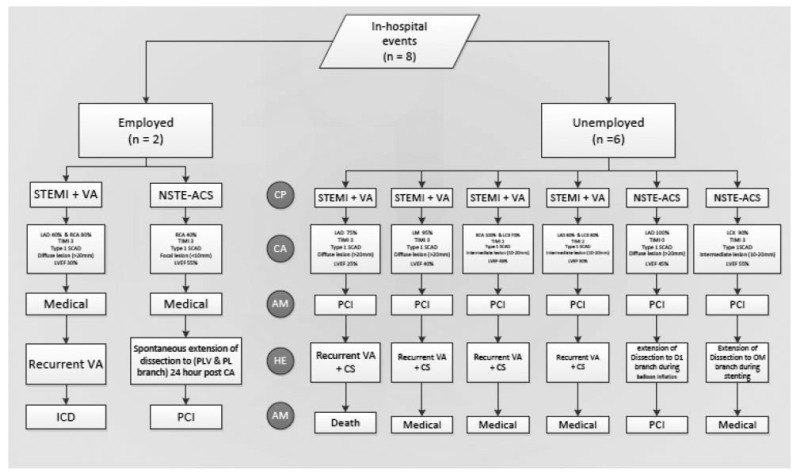
Detailed information regarding In-hospital events is displayed in (Fig. 1). There were 8 composite in-hospital events, 6 in the unemployed group, and 2 in the employed group. In the unemployed group, 4 patients had recurrent ventricular arrhythmia and cardiogenic shock. One patient died. The remaining 3 patients received IV amiodarone, inotropic support, and intra-aortic balloon pumps, and survived until discharge. The other 2 patients in the unemployed group had NSTE-ACS secondary to extension of the dissection. One patient had a retrograde extension of the dissection in a diagonal branch during balloon angioplasty of the LAD and was treated with PCI. The second patient had an extension of the dissection to an obtuse marginal branch during the stenting of the left circumflex artery and was treated medically. In the employed group, there were two in-hospital events. One patient underwent an Implantable Cardioverter Defibrillator (ICD) placement for recurrent ventricular arrhythmia and low LVEF (less than 35%). The other patient had a spontaneous extension of the dissection in the posterolateral branch 24 hours post coronary angiography and was treated with PCI. There was no statistically significant difference between the two groups in regards to composite in-hospital events (6 (18.18%) vs. 2 (4%), p = 0.10). Follow-up events are displayed in (Fig. 2).
Fig. (1).
Flow diagram of clinical presentation, angiographic finding, and acute management for SCAD patients who had developed in-hospital events. (A higher resolution / colour version of this figure is available in the electronic copy of the article).
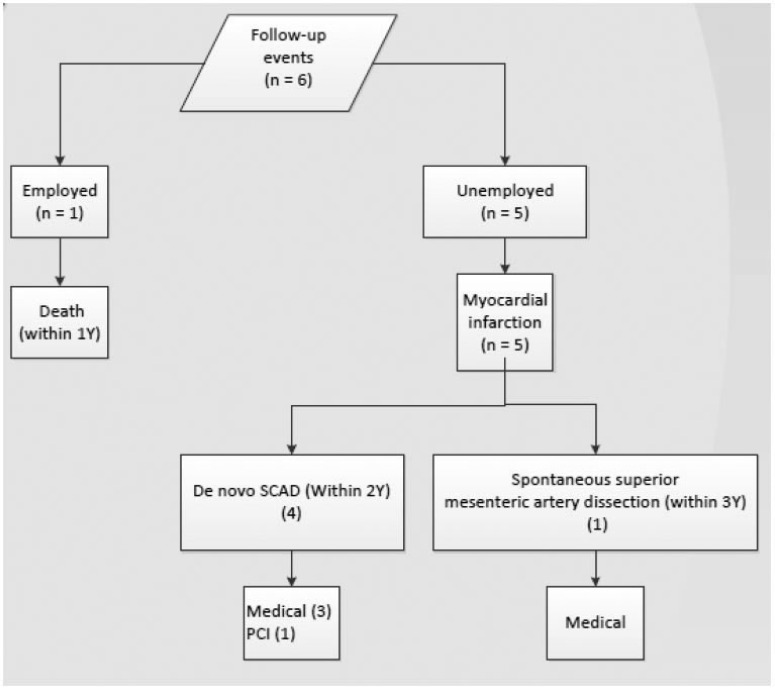
Fig. (2).
Flow diagram of SCAD patients who had developed events during follow up. (A higher resolution / colour version of this figure is available in the electronic copy of the article).
The composite follow-up events were statistically significant when comparing unemployed versus employed groups (5 (15.62%) vs. 1 (2%), p = 0.03). In the unemployed group, recurrent myocardial infarction occurred in all 5 patients, 4 of which were secondary to de novo coronary artery dissection. Three were treated medically and one underwent PCI. In the employed group, one patient died within one year of discharge from an unknown cause. In the employed group, there was no de novo coronary artery dissection as compared to four patients in the unemployed group, (4 (12.5%) vs. 0 (0%), p = 0.02), respectively. As shown in (Table 4), unemployment was significantly associated with all events (in-hospital and follow-up) in univariate and multivariate (adjusted for gender) logistic regression (OR 10.4 [2.1, 51.6] p = 0.001 and adjusted OR 7.1 [1.3, 37.9] p = 0.021, respectively).
Table 4.
Association between unemployment and gender on all events (in-hospital and follow-up) in univariate and multivariate logistic regression.
| - | Univariate OR (95% CI) | Multivariate Or (95% Ci) Adjusted For The Other Factor | ||
|---|---|---|---|---|
| Covariate | OR (95% CI) | P-value | OR (95% CI) | P-value |
| Unemployment | 10.4 (2.1− 51.6) | 0.001 | 7.1 (1.3− 37.9) | 0.021 |
| Female | 6.1 (1.2− 29.8) | 0.026 | 3.1 (0.6 − 16.9) | 0.197 |
4. DISCUSSION
The main finding of the current study was that unemployed patients with SCAD were more likely to experience in-hospital and follow-up cardiac events. Besides, our study found that 66% of males and 76% of female patients with SCAD were employed and unemployed, respectively. Factors associated with unemployment were lower education level, lower monthly income, and being single. Unemployment can lead to negative impacts on cardiovascular health [35]. Unemployment is associated with high reported levels of emotional stress [36], and unemployed individuals seeking employment increase their level of emotional stress [37]. Emotional stress is more prevalent as a trigger of SCAD than physical stress [36]. Potential mechanisms for unemployment and emotional stress contributing to SCAD include sympathetic activation, catecholamine discharge, systemic vasoconstriction, tachycardia, hypertension, and modified myocardial oxygen demand [38]. These pathways may contribute to coronary artery shear stress and other negative impacts responsible for SCAD and its prognosis [38-43]. Although this hypothesis has not been tested in SCAD patients, a similar mechanism has been proposed in other stress-induced cardiovascular conditions such as takotsubo cardiomyopathy [44, 45]. Catecholamine discharge can also induce inflammation, which plays an important role in the acute setting and during myocardial recovery after myocardial infarction [46-48]. Previous studies have shown that unemployment increases the risk of acute myocardial infarction and that the association is not accounted for by conventional social, behavioral, psychological, or clinical factors [11]. Other evidence indicates that the effect of unemployment on all-cause mortality is not uniform across the population: mortality due to unemployment is higher among the young, the unmarried, the less educated, and lower-income earners [8]. Previous evidence [49] has shown that there is a heterogeneous relationship between income and health status due to race and ethnicity. Therefore, no firm conclusions can be made from the latter observation regarding residence. As far as lower education level is concerned, it was previously shown that high educational levels might indicate an improved health status among unemployed individuals [50]. Unemployment is also linked with being divorced or widowed, financial insecurity, loss of social support, and loss of resources (including access to healthcare). Depression has been shown to be strongly associated with cardiovascular disease and may be a significant co-contributor with unemployment, especially in women [51]. These associations may add to the stress of unemployment and its potential negative impacts [52]. These effects may be even greater in a society with disparate access to resources, especially for women [53-55]. Interventions to manage these factors in patients with SCAD, either occupationally or therapeutically, may help reduce future adverse cardiac events and possibly improve prognosis. One potential countermeasure could be employment resources, which could provide recovery from stress by possibly reversing these mechanisms [56, 57].
This type of outreach would be consistent with Vision 2030 tenets [16]. In the previous study, Daoulah et al. [34] compared the Arab Gulf countries to western cohorts in relationship to SCAD [35]. Potential explanations for the differences between the Arab and western data would include differences in genetics, lifestyle, culture, and medical services utilization between the two populations [58].
5. STRENGTHS
This study provides information about patients with SCAD in a unique population, from the Arab Gulf countries. Also, the study drew patients from a large number of centers in that region. Finally, the study examines the association between employment status and in-hospital and follow-up adverse cardiovascular events in SCAD patients.
6. LIMITATIONS
The study is potentially limited by selection, referral, measurement, and attrition biases. Additionally, the retrospective analysis may have underestimated the prevalence of SCAD in the Arab Gulf region. For those who described themselves as unemployed (throughout the study period), the impact of specific circumstances of their unemployment was not investigated or recorded.
CONCLUSION
SCAD patients with unemployment are associated with worse in-hospital and follow-up events as compared to those employed. Attention to the employment status in patients with cardiovascular disease can improve outcomes beyond traditional effective therapies, and increase the quality of life for these patients. Larger epidemiological studies are needed, taking into consideration the confounding factors and supported by the appropriate sample size to confirm our findings globally.
COMPLETE LIST OF AUTHORS WHO CONTRIBUTED DETAILED CLINICAL DATA
Jairam K. Aithal, MD, Burjeel Hospital, Abu Dhabi, UAE; Tarek Farghali, MD, Ibrahim Bin Hamad Obidullah Hospital, Ras Al khaimah, UAE Mirvat Alasnag, MD, King Fahd Armed Forces Hospital, Jeddah, Saudi Arabia; Adel Khalifa Hamad, MD, Mohammed bin Khalifa Al Khalifa Cardiac Centre Bahrain Defence Force Hospital, Riffa, Bahrain; Mamdouh Morshid, MD, King Abdullah Medical City, Makkah, Saudi Arabia; Yosri M. A. Morsi, MD, Prince Abdullah Bin Musaed Cardiac Centre, Arar, Saudi Arabia; Ziad Dahdouh, MD, King Faisal Specialist Hospital & Research Center, Riyadh, Saudi Arabia; Osama ElSayed, MD, King Faisal Specialist Hospital & Research Center, Jeddah, Saudi Arabia; Mohamed Nabil Alama, MD, King Abdulaziz University Hospital, Jeddah, Saudi Arabia; Nader Alasousi, MD, Sabah Alahmad Cardiac Center, Amiri Hospital, Kuwait; Khalid Tammam, MD, International medical Center, Jeddah, Saudi Arabia; Mohammed Almansori, MD, Imam Abdulrahman Bin Faisal University, Alkhubar, Saudi Arabia; Mohamed A. Ghani, MD, Madinah Cardiac Center, Madinah, Saudi Arabia; Wael A. Refaat, MD, Prince Sultan Cardiac Center, Al Hassa, Saudi Arabia; Akram Eldesoky, MD, Prince Sultan Cardiac Center, Al Qassim, Saudi Arabia; Mohammed Balghith, MD, King Saud Bin Abdulaziz University for Health Science, Riyadh, Saudi Arabia Muhammad Adil Soofi, MD, King Salman Heart Center, King Fahad Medical City, Riyadh, Saudi Arabia; Ali A. Youssef, MD, Saud Al Babtain Cardiac Center, Dammam, Saudi Arabia; Fahad Baslaib, MD, Rashid Hospital, Dubai, UAE; Abdullah Alkhushail, MD, Prince Sultan Cardiac Center, Riyadh, Saudi Arabia; Mohammed Qutub, MD, King Abdulaziz University Jeddah, Saudi Arabia; Najeeb Jaha, MD, King Abdullah Medical City, Makkah, Saudi Arabia; Abdullah Al Abdulgader, MD, Prince Sultan Cardiac Center, Al Hassa, Saudi Arabia; Adel Ali Almasswary, MD, Aseer Centeral Hospital, Abha, Saudi Arabia; Taher Hassan, MD, Bugshan hospital, Jeddah, Saudi Arabia; Hamidullah Kazim, MD, AlHada Military Hospital, Taif, Saudi Arabia; Mosaad Abushabana, MD, Dubai Hospital, Dubai, UAE; Wael Aboushokka, MD, AlQassimi hospital, Sharjah, UAE; Sayed Abdou, MD, Saud Albabtin Cardiac Center, Dammam, Saudi Arabia; Amira Ali Taha Ibrahim, MD, Burjeel Hospital, Abu Dhabi, UAE; Ibrahim Abdulhabeeb, MD, Cardiac Center Aljouf Region, Sakaka, Saudi Arabia; Tahir Mohamed, MD, King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia Ahmad Alhamami, MD, King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia; Mamdouh Haddara, MD, King Faisal Specialist Hospital & Research Center, Riyadh, Saudi Arabia; Mirza Javed Iqbal, MD, Prince Abdullah Bin Musaed Cardiac Centre, Arar, Saudi Arabia; Abdelmaksoud Ahmed Elgandy, MD, Erfan and Bagedo general hospital, Jeddah, Saudi Arabia; Hisham M Husain, MD, Saud Al Babtain Cardiac Center, Dammam, Saudi Arabia.
ACKNOWLEDGEMENTS
Declared none.
ABBREVIATIONS AND ACRONYMS
- NST-ACS
Non-ST-Elevation Acute Coronary Syndrome
- STEMI
ST-Elevation Myocardial Infarction
- SCAD
Spontaneous Coronary Artery Dissection
- VA
Ventricular Arrhythmia
- VT
Ventricular Tachycardia
- VF
Ventricular Fibrillation
- PCI
Percutaneous Coronary Intervention
- CABG
Coronary Artery Bypass Grafting
- CAD
Coronary Artery Disease
- EF
Ejection Fraction
- WBC
White Blood Cell Count
- CK
Creatine Kinase
- CKMB
Creatine Kinase Muscle/Brain
- TIMI
Thrombolysis in Myocardial Infarction
- F
Female
- M
Male
- ICD
Implantable Cardioverter Defibrillator
- LAD
Left Anterior Descending Coronary Artery
- LM
Left Main Coronary Artery
- LCX
Left Circumflex Coronary Artery
- RCA
Right Coronary Artery
- IC
Intracoronary
- CA
Coronary Angiogram
- ACS
Acute Coronary Syndrome
- IVUS
Intravascular Ultrasound
- OCT
Optical Coherence Tomography
- CS
Cardiogenic Shock
- CP
Clinical Presentation
- AM
Acute Management
- HE
Hospital Event
AUTHOR CONTRIBUTIONS
All authors contributed to study design, development, data collection, and analysis of results.
A.D. produced the initial draft of the manuscript.
A.D. reviewed the manuscript and provided critical revision and final editing.
Statistician for this study: Prof Edward Bentz Devol. E-mail address: edevol@kfshrc.edu.sa
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the King Faisal Specialist Hospital and Research Center Institutional Review Board, RC-J/31/39, Saudia Arabia.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Consent to participate in this study was not required due to the design of our study. However, verbal consent was obtained via a phone call from each patient, if the patient agreed to participate in the study it will be documented in their medical record file. If they declined, they were excluded from the study.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author, [Amin Daoulah], upon reasonable request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
REFERENCES
- 1.Park S., Chan K.C., Williams E.C. Gain of employment and perceived health status among previously unemployed persons: evidence from a longitudinal study in the United States. Public Health. 2016;133:83–90. doi: 10.1016/j.puhe.2015.11.008. [DOI] [PubMed] [Google Scholar]
- 2.Cable N., Sacker A., Bartley M. The effect of employment on psychological health in mid-adulthood: findings from the 1970 British Cohort Study. J. Epidemiol. Community Health. 2008;62(5):e10. doi: 10.1136/jech.2007.063776. [DOI] [PubMed] [Google Scholar]
- 3.Dooley D. Unemployment, underemployment, and mental health: conceptualizing employment status as a continuum. Am. J. Community Psychol. 2003;32(1-2):9–20. doi: 10.1023/A:1025634504740. [DOI] [PubMed] [Google Scholar]
- 4.Lourel M., Hartmann A., Closon C., Mouda F., Petric-Tatu O. Social support and health: An overview of selected theoretical models for adaptation. In: Chen S., editor. Social support, gender and culture, and health benefits. Hauppauge, NY: Nova Science Publishers; 2013. pp. 1–20. [Google Scholar]
- 5.Price R.H., Choi J.N., Vinokur A.D. Links in the chain of adversity following job loss: how financial strain and loss of personal control lead to depression, impaired functioning, and poor health. J. Occup. Health Psychol. 2002;7(4):302–312. doi: 10.1037/1076-8998.7.4.302. [DOI] [PubMed] [Google Scholar]
- 6.Kasl S.V., Gore S., Cobb S. The experience of losing a job: reported changes in health, symptoms and illness behavior. Psychosom. Med. 1975;37(2):106–122. doi: 10.1097/00006842-197503000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Kessler R.C., House J.S., Turner J.B. Unemployment and health in a community sample. J. Health Soc. Behav. 1987;28(1):51–59. doi: 10.2307/2137140. [DOI] [PubMed] [Google Scholar]
- 8.VAgerA D., Garcy A.M. Does unemployment cause long-term mortality? Selection and causation after the 1992-96 deep Swedish recession. Eur J Public Health. 2016;26(5):778–783. doi: 10.1093/eurpub/ckw053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lundin A., Falkstedt D., Lundberg I., Hemmingsson T. Unemployment and coronary heart disease among middle-aged men in Sweden: 39 243 men followed for 8 years. Occup. Environ. Med. 2014;71(3):183–188. doi: 10.1136/oemed-2013-101721. [DOI] [PubMed] [Google Scholar]
- 10.ob losses linked to myocardial infarction in US cohort. BMJ. 2012;345:e7839. doi: 10.1136/bmj.e7839. [DOI] [PubMed] [Google Scholar]
- 11.Dupre M.E., George L.K., Liu G., Peterson E.D. The cumulative effect of unemployment on risks for acute myocardial infarction. Arch. Intern. Med. 2012;172(22):1731–1737. doi: 10.1001/2013.jamainternmed.447. [DOI] [PubMed] [Google Scholar]
- 12.The Statistical Centre for the Cooperation Council for the Arab Countries of the Gulf. Available from: https://gccstat.org.
- 13.Daoulah A., Elkhateeb O.E., Nasseri S.A., Al-Murayeh M., Al-Kaabi S., Lotfi A., Alama M.N., Al-Faifi S.M., Haddara M., Dixon C.M., Alzahrani I.S., Alghamdi A.A., Ahmed W., Fathey A., Haq E., Alsheikh-Ali A.A. Socioeconomic factors and severity of coronary artery disease in patients undergoing coronary angiography: A multicentre study of Arabian Gulf States. Open Cardiovasc Med J. 2017;11:47–57. doi: 10.2174/1874192401711010047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mark D.B., Lam L.C., Lee K.L., Clapp-Channing N.E., Williams R.B., Pryor D.B., Califf R.M., Hlatky M.A. Identification of patients with coronary disease at high risk for loss of employment. A prospective validation study. Circulation. 1992;86(5):1485–1494. doi: 10.1161/01.CIR.86.5.1485. [DOI] [PubMed] [Google Scholar]
- 15.The current statistics from the General Authority for Statistics. Available from: www.stats.gov.sa.
- 16.Strategic Objectives and Vision Realization Programs. [Google Scholar]
- 17.Tweet M.S., Hayes S.N., Pitta S.R., Simari R.D., Lerman A., Lennon R.J., Gersh B.J., Khambatta S., Best P.J., Rihal C.S., Gulati R. Clinical features, management, and prognosis of spontaneous coronary artery dissection. Circulation. 2012;126(5):579–588. doi: 10.1161/CIRCULATIONAHA.112.105718. [DOI] [PubMed] [Google Scholar]
- 18.Alfonso F., Paulo M., Lennie V., Dutary J., Bernardo E., JimA(c)nez-Quevedo P., Gonzalo N., Escaned J., Bauelos C., PA(c)rez-Vizcayno M.J., HernAndez R., Macaya C. Spontaneous coronary artery dissection: long-term follow-up of a large series of patients prospectively managed with a "conservative" therapeutic strategy. JACC Cardiovasc Interv. 2012;5(10):1062–1070. doi: 10.1016/j.jcin.2012.06.014. [DOI] [PubMed] [Google Scholar]
- 19.Lettieri C., Zavalloni D., Rossini R., Morici N., Ettori F., Leonzi O., Latib A., Ferlini M., Trabattoni D., Colombo P., Galli M., Tarantini G., Napodano M., Piccaluga E., Passamonti E., Sganzerla P., Ielasi A., Coccato M., Martinoni A., Musumeci G., Zanini R., Castiglioni B. Management and long-term prognosis of spontaneous coronary artery dissection. Am. J. Cardiol. 2015;116(1):66–73. doi: 10.1016/j.amjcard.2015.03.039. [DOI] [PubMed] [Google Scholar]
- 20.Saw J., Aymong E., Sedlak T., Buller C.E., Starovoytov A., Ricci D., Robinson S., Vuurmans T., Gao M., Humphries K., Mancini G.B. Spontaneous coronary artery dissection: association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ. Cardiovasc. Interv. 2014;7(5):645–655. doi: 10.1161/CIRCINTERVENTIONS.114.001760. [DOI] [PubMed] [Google Scholar]
- 21.Rashid H.N., Wong D.T., Wijesekera H., Gutman S.J., Shanmugam V.B., Gulati R., Malaipan Y., Meredith I.T., Psaltis P.J. Incidence and characterisation of spontaneous coronary artery dissection as a cause of acute coronary syndrome--A single-centre Australian experience. Int. J. Cardiol. 2016;202:336–338. doi: 10.1016/j.ijcard.2015.09.072. [DOI] [PubMed] [Google Scholar]
- 22.Saw J., Ricci D., Starovoytov A., Fox R., Buller C.E. Spontaneous coronary artery dissection: prevalence of predisposing conditions including fibromuscular dysplasia in a tertiary center cohort. JACC Cardiovasc. Interv. 2013;6(1):44–52. doi: 10.1016/j.jcin.2012.08.017. [DOI] [PubMed] [Google Scholar]
- 23.Saw J., Mancini G.B.J., Humphries K.H. Contemporary review on spontaneous coronary artery dissection. J. Am. Coll. Cardiol. 2016;68(3):297–312. doi: 10.1016/j.jacc.2016.05.034. [DOI] [PubMed] [Google Scholar]
- 24.Nakashima T., Noguchi T., Haruta S., Yamamoto Y., Oshima S., Nakao K., Taniguchi Y., Yamaguchi J., Tsuchihashi K., Seki A., Kawasaki T., Uchida T., Omura N., Kikuchi M., Kimura K., Ogawa H., Miyazaki S., Yasuda S. Prognostic impact of spontaneous coronary artery dissection in young female patients with acute myocardial infarction: A report from the Angina Pectoris-Myocardial Infarction Multicenter Investigators in Japan. Int. J. Cardiol. 2016;207:341–348. doi: 10.1016/j.ijcard.2016.01.188. [DOI] [PubMed] [Google Scholar]
- 25.Tweet M.S., Eleid M.F., Best P.J., Lennon R.J., Lerman A., Rihal C.S., Holmes D.R., Jr, Hayes S.N., Gulati R. Spontaneous coronary artery dissection: revascularization versus conservative therapy. Circ. Cardiovasc. Interv. 2014;7(6):777–786. doi: 10.1161/CIRCINTERVENTIONS.114.001659. [DOI] [PubMed] [Google Scholar]
- 26.Rogowski S., Maeder M.T., Weilenmann D., Haager P.K., Ammann P., Rohner F., Joerg L., Rickli H. Spontaneous coronary artery dissection: angiographic follow-up and long-term clinical outcome in a predominantly medically treated population. Catheter. Cardiovasc. Interv. 2017;89(1):59–68. doi: 10.1002/ccd.26383. [DOI] [PubMed] [Google Scholar]
- 27.Hayes S.N., Kim E.S.H., Saw J., Adlam D., Arslanian-Engoren C., Economy K.E., Ganesh S.K., Gulati R., Lindsay M.E., Mieres J.H., Naderi S., Shah S., Thaler D.E., Tweet M.S., Wood M.J. American Heart Association Council on Peripheral Vascular Disease. Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; Council on Genomic and Precision Medicine; and Stroke Council. Spontaneous Coronary Artery Dissection: Current State of the Science: A scientific statement from the American Heart Association. Circulation. 2018;137(19):e523–e557. doi: 10.1161/CIR.0000000000000564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fahmy P., Prakash R., Starovoytov A., Boone R., Saw J. Pre-disposing and precipitating factors in men with spontaneous coronary artery dissection. JACC Cardiovasc. Interv. 2016;9(8):866–868. doi: 10.1016/j.jcin.2016.02.024. [DOI] [PubMed] [Google Scholar]
- 29.Saw J., Humphries K., Aymong E., Sedlak T., Prakash R., Starovoytov A., Mancini G.B.J. Spontaneous coronary artery dissection: clinical outcomes and risk of recurrence. J. Am. Coll. Cardiol. 2017;70(9):1148–1158. doi: 10.1016/j.jacc.2017.06.053. [DOI] [PubMed] [Google Scholar]
- 30.Michelis K.C., Olin J.W., Kadian-Dodov D., d'Escamard V., Kovacic J.C. Coronary artery manifestations of fibromuscular dysplasia. J. Am. Coll. Cardiol. 2014;64(10):1033–1046. doi: 10.1016/j.jacc.2014.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Eleid M.F., Guddeti R.R., Tweet M.S., Lerman A., Singh M., Best P.J., Vrtiska T.J., Prasad M., Rihal C.S., Hayes S.N., Gulati R. Coronary artery tortuosity in spontaneous coronary artery dissection: angiographic characteristics and clinical implications. Circ. Cardiovasc. Interv. 2014;7(5):656–662. doi: 10.1161/CIRCINTERVENTIONS.114.001676. [DOI] [PubMed] [Google Scholar]
- 32.Saw J. Coronary angiogram classification of spontaneous coronary artery dissection. Catheter. Cardiovasc. Interv. 2014;84(7):1115–1122. doi: 10.1002/ccd.25293. [DOI] [PubMed] [Google Scholar]
- 33.Saw J., Mancini G.B., Humphries K., Fung A., Boone R., Starovoytov A., Aymong E. Angiographic appearance of spontaneous coronary artery dissection with intramural hematoma proven on intracoronary imaging. Catheter. Cardiovasc. Interv. 2016;87(2):E54–E61. doi: 10.1002/ccd.26022. [DOI] [PubMed] [Google Scholar]
- 34.Daoulah A., Al-Faifi S.M., Hersi A.S., Dinas P.C., Youssef A.A., Alshehri M., Baslaib F., Maghrabi M., Al-Murayeh M., Ghani M.A., Refaat W.A., Eldesoky A., Balghith M., Soofi M.A., Alasmari A., Alasnag M., Hamad A.K., Morshid M., Morsi Y.M.A., Dahdouh Z., ElSayed O., Alama M.N., Alasousi N., Tammam K., Almansori M., Khan A.S., Alkhushail A., Aithal J.K., Alqahtani A.H., Lotfi A. G-SCAD investigators. Spontaneous coronary artery dissection in relation to physical and emotional stress: A retrospective study in four Arab Gulf Countries. Curr. Probl. Cardiol. 2021;46(3):100484. doi: 10.1016/j.cpcardiol.2019.100484. [DOI] [PubMed] [Google Scholar]
- 35.Virtanen M., Nyberg S.T., Batty G.D., Jokela M., HeikkilA K., Fransson E.I., Alfredsson L., Bjorner J.B., Borritz M., Burr H., Casini A., Clays E., De Bacquer D., Dragano N., Elovainio M., Erbel R., Ferrie J.E., Hamer M., JAckel K.H., Kittel F., Knutsson A., Koskenvuo M., Koskinen A., Lunau T., Madsen I.E., Nielsen M.L., Nordin M., Oksanen T., Pahkin K., Pejtersen J.H., Pentti J., Rugulies R., Salo P., Shipley M.J., Siegrist J., Steptoe A., Suominen S.B., Theorell T., Toppinen-Tanner S., VAAnAnen A., Vahtera J., Westerholm P.J., Westerlund H., Slopen N., Kawachi I., Singh-Manoux A., KivimAki M. IPD-Work Consortium. Perceived job insecurity as a risk factor for incident coronary heart disease: systematic review and meta-analysis. BMJ. 2013;347:f4746. doi: 10.1136/bmj.f4746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mæhlisen M.H., Pasgaard A.A., Mortensen R.N., Vardinghus-Nielsen H., Torp-Pedersen C., Bøggild H. Perceived stress as a risk factor of unemployment: a register-based cohort study. BMC Public Health. 2018;18(1):728. doi: 10.1186/s12889-018-5618-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zandara M., Garcia-Lluch M., Villada C., Hidalgo V., Salvador A. Searching for a job: Cardiac responses to acute stress and the mediating role of threat appraisal in young people. Stress Health. 2018;34(1):15–23. doi: 10.1002/smi.2757. [DOI] [PubMed] [Google Scholar]
- 38.Mittleman M.A., Maclure M., Sherwood J.B., Mulry R.P., Tofler G.H., Jacobs S.C., Friedman R., Benson H., Muller J.E. Determinants of myocardial infarction onset study investigators. Triggering of acute myocardial infarction onset by episodes of anger. Circulation. 1995;92(7):1720–1725. doi: 10.1161/01.CIR.92.7.1720. [DOI] [PubMed] [Google Scholar]
- 39.Mittleman M.A., Mostofsky E. Physical, psychological and chemical triggers of acute cardiovascular events: preventive strategies. Circulation. 2011;124(3):346–354. doi: 10.1161/CIRCULATIONAHA.110.968776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Verrier R.L., Hagestad E.L., Lown B. Delayed myocardial ischemia induced by anger. Circulation. 1987;75(1):249–254. doi: 10.1161/01.CIR.75.1.249. [DOI] [PubMed] [Google Scholar]
- 41.Boltwood M.D., Taylor C.B., Burke M.B., Grogin H., Giacomini J. Anger report predicts coronary artery vasomotor response to mental stress in atherosclerotic segments. Am. J. Cardiol. 1993;72(18):1361–1365. doi: 10.1016/0002-9149(93)90180-K. [DOI] [PubMed] [Google Scholar]
- 42.Muller J.E., Kaufmann P.G., Luepker R.V., Weisfeldt M.L., Deedwania P.C., Willerson J.T. Mechanisms precipitating acute cardiac events: review and recommendations of an NHLBI workshop. National heart, lung, and blood institute. Mechanisms precipitating acute cardiac events participants. Circulation. 1997;96(9):3233–3239. doi: 10.1161/01.CIR.96.9.3233. [DOI] [PubMed] [Google Scholar]
- 43.Muller J.E., Tofler G.H., Stone P.H. Circadian variation and triggers of onset of acute cardiovascular disease. Circulation. 1989;79(4):733–743. doi: 10.1161/01.CIR.79.4.733. [DOI] [PubMed] [Google Scholar]
- 44.Smyth A., O'Donnell M., Lamelas P., Teo K., Rangarajan S., Yusuf S. INTERHEART Investigators. Physical activity and anger or emotional upset as triggers of acute myocardial infarction: the INTERHEART study. Circulation. 2016;134(15):1059–1067. doi: 10.1161/CIRCULATIONAHA.116.023142. [DOI] [PubMed] [Google Scholar]
- 45.Wittstein I.S., Thiemann D.R., Lima J.A., Baughman K.L., Schulman S.P., Gerstenblith G., Wu K.C., Rade J.J., Bivalacqua T.J., Champion H.C. Neurohumoral features of myocardial stunning due to sudden emotional stress. N. Engl. J. Med. 2005;352(6):539–548. doi: 10.1056/NEJMoa043046. [DOI] [PubMed] [Google Scholar]
- 46.Frangogiannis N.G., Smith C.W., Entman M.L. The inflammatory response in myocardial infarction. Cardiovasc. Res. 2002;53(1):31–47. doi: 10.1016/S0008-6363(01)00434-5. [DOI] [PubMed] [Google Scholar]
- 47.Metzler B., Mair J., Lercher A., Schaber C., Hintringer F., Pachinger O., Xu Q. Mouse model of myocardial remodelling after ischemia: role of intercellular adhesion molecule-1. Cardiovasc. Res. 2001;49(2):399–407. doi: 10.1016/S0008-6363(00)00261-3. [DOI] [PubMed] [Google Scholar]
- 48.Swiatkiewicz I., Kozinski M., Magielski P., Fabiszak T., Sukiennik A., Navarese E.P., Odrowaz-Sypniewska G., Kubica J. Value of C-reactive protein in predicting left ventricular remodelling in patients with a first ST-segment elevation myocardial infarction. Mediators Inflamm. 2012;2012:250867. doi: 10.1155/2012/250867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Meraya A.M., Dwibedi N., Innes K., Mitra S., Tan X., Sambamoorthi U. Heterogeneous relationships between labor income and health by race/ethnicity. Health Serv. Res. 2018;53(Suppl. 1):2910–2931. doi: 10.1111/1475-6773.12802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.De Moortel D., Hagedoorn P., Vanroelen C., Gadeyne S. Employment status and mortality in the context of high and low regional unemployment levels in Belgium (2001-2011): A test of the social norm hypothesis across educational levels. PLoS One. 2018;13(2):e0192526. doi: 10.1371/journal.pone.0192526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bucciarelli V., Caterino A.L., Bianco F., Caputi C.G., Salerni S., Sciomer S., Maffei S., Gallina S. Depression and cardiovascular disease: The deep blue sea of women’s heart. Trends Cardiovasc. Med. 2020;30(3):170–176. doi: 10.1016/j.tcm.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 52.KivimAki M., Nyberg S.T., Fransson E.I., HeikkilA K., Alfredsson L., Casini A., Clays E., De Bacquer D., Dragano N., Ferrie J.E., Goldberg M., Hamer M., Jokela M., Karasek R., Kittel F., Knutsson A., Koskenvuo M., Nordin M., Oksanen T., Pentti J., Rugulies R., Salo P., Siegrist J., Suominen S.B., Theorell T., Vahtera J., Virtanen M., Westerholm P.J., Westerlund H., Zins M., Steptoe A., Singh-Manoux A., Batty G.D. IPD-Work Consortium. Associations of job strain and lifestyle risk factors with risk of coronary artery disease: a meta-analysis of individual participant data. CMAJ. 2013;185(9):763–769. doi: 10.1503/cmaj.121735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rivero F., Bastante T., Cuesta J., Benedicto A., Salamanca J., Restrepo J.A., Aguilar R., Gordo F., Batlle M., Alfonso F. Factors associated with delays in seeking medical attention in patients with ST segment elevation acute coronary syndrome. Rev. Esp. Cardiol. (Engl. Ed.) 2016;69(3):279–285. doi: 10.1016/j.rec.2015.07.029. [DOI] [PubMed] [Google Scholar]
- 54.Alshahrani H., McConkey R., Wilson J., Youssef M., Fitzsimons D. Female gender doubles pre-hospital delay times for patients experiencing ST segment elevation myocardial infarction in Saudi Arabia. Eur. J. Cardiovasc. Nurs. 2014;13(5):399–407. doi: 10.1177/1474515113507159. [DOI] [PubMed] [Google Scholar]
- 55.Ferraz-Torres M., Belzunegui-Otano T., MarA-n-Fernandez B., Martinez-Garcia A"., Ibañez-Beroiz B. Differences in the treatment and evolution of acute coronary syndromes according to gender: what are the causes? J. Clin. Nurs. 2015;24(17-18):2468–2477. doi: 10.1111/jocn.12831. [DOI] [PubMed] [Google Scholar]
- 56.Gallo W.T., Bradley E.H., Siegel M., Kasl S.V. Health effects of involuntary job loss among older workers: findings from the health and retirement survey. J. Gerontol. B Psychol. Sci. Soc. Sci. 2000;55(3):S131–S140. doi: 10.1093/geronb/55.3.S131. [DOI] [PubMed] [Google Scholar]
- 57.Mandal B., Roe B. Job loss, retirement and the mental health of older Americans. J. Ment. Health Policy Econ. 2008;11(4):167–176. [PubMed] [Google Scholar]
- 58.Batniji R., Khatib L., Cammett M., Sweet J., Basu S., Jamal A., Wise P., Giacaman R. Governance and health in the Arab world. Lancet. 2014;383(9914):343–355. doi: 10.1016/S0140-6736(13)62185-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, [Amin Daoulah], upon reasonable request.