Highlights
-
•
Transcatheter occlusion of vertical vein in a partial anomalous pulmonary venous connection with dual drainage, case series with literature review.
-
•
In our manuscript we highlight the possibility of transcatheter Amplatzer device closure of PAPVD with dual drainage is an effective, safe and reproducible approach. It offers many advantages over surgical treatment such as fast recovery, avoidance of mechanical ventilation and PCICU stay, short in-hospital stay, low cost and more patient satisfaction.
-
•
In our series, it has been demonstrated that this approach showed appealing results, however larger scale studies and more follow-up periods are required to consolidate these findings.
Keywords: Device closure, Dual drainage, Partial anomalous pulmonary venous connection
Abstract
Partial anomalous pulmonary venous return (PAPVR) is an uncommon type of congenital heart disease occurring due to abnormal drainage of one or more, but not all the pulmonary veins to the systemic veins or directly to the right atrium. The PAPVR might have single (to the systemic veins) or dual drainage (to the systemic as well as left atrium). Management depends on the shunt impact on the heart and lungs, and it is usually surgical correction.
In case of PAPVR with dual drainage, there is a new trend of percutaneous occlusion of the vertical vein with dual drainage anatomy, so that the blood is obliged to flow to the left atrium as in normal hearts.
The scope of this manuscript is to highlight the availability of this alternative option and to present our experience and outcome in 6 PAPVR patients with dual drainage treated using this percutaneous approach.
1. Introduction
Partial anomalous pulmonary venous return (PAPVR) is a rare type of pulmonary vein anomalies. It is encountered in 0.5–0.7% of the population. Furthermore, almost 10–15% of patients with atrial septal defect (ASD) have PAPVR [1]. Various degree of right ventricular and right atrial dilatation is usually found as a result of chronic left to right shunt, and increased flow to the lungs may result in remodeling of pulmonary vascular bed which may lead to pulmonary arterial hypertension. In such pathology, the gold standard is the surgical redirection of the anomalous vein(s) to the left atrium. Nowadays there is a growing experience of percutaneous transcatheter device closure. We describe a series of cases in which successful transcatheter closure of vertical vein was performed.
2. Case 1
Six-year-old boy, diagnosed recently to have PAPVR of the left upper pulmonary vein to the left innominate vein through ascending vertical vein, dilated right atrium and right ventricle. After discussion in the combined pediatric cardiology and surgical meeting, the consensus was to proceed with diagnostic cardiac catheterization and possible transcatheter closure. In the catheterization laboratory, after the confirmation of PAPVR and dual drainage to the left atrium and left innominate vein, the vertical vein was occluded using patent ductus arteriosus occluder device 8/10 mm (Abbot Medical, Plymouth, MN). The patient was transferred to the ward and the echocardiogram showed device in good position, no residual flow to the left innominate vein and good cardiac function. A follow-up echocardiogram after 4 weeks from discharge confirmed the same findings. The patient was followed up for 5 years and the repeat of cardiac catheterization showed good outcome of the intervention and normal pulmonary artery pressure (PAP was 18/9 mean of 10 mmHg) and normal pulmonary vascular resistance.
3. Case 2
Eleven-year-old girl, diagnosed in the neonatal period to have mild pulmonary valve stenosis, at age of 7 years started to have mild exercise intolerance. The repeated echocardiography revealed non-obstructive PAPVR of the left upper pulmonary vein to the left innominate vein dilated right atrium and right ventricle in addition to mild pulmonary valve stenosis (Fig. 1, Fig. 2, Fig. 3). She underwent elective percutaneous transcatheter device closure using patent ductus arteriosus occluder device 8/10 mm (AGA, Medical, and Plymouth, MN). Subsequently, the patient was in regular follow up in six-month basis. The patient was doing well throughout the follow up and the echocardiography three years later showed device in good position, no leak, all pulmonary veins draining into the left atrium, no stenosis and no echocardiographic evidence of pulmonary hypertension.
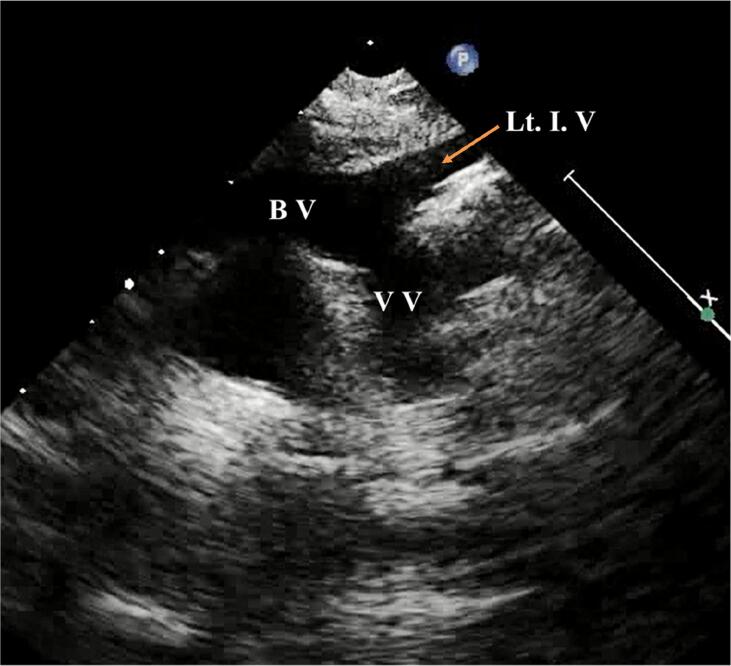
Fig. 1.
Suprasternal echocardiographic view showed anomalous pulmonary vein with ascending vertical vein (VV), left innominate vein (Lt. I. V) and Bridging vein (BV).
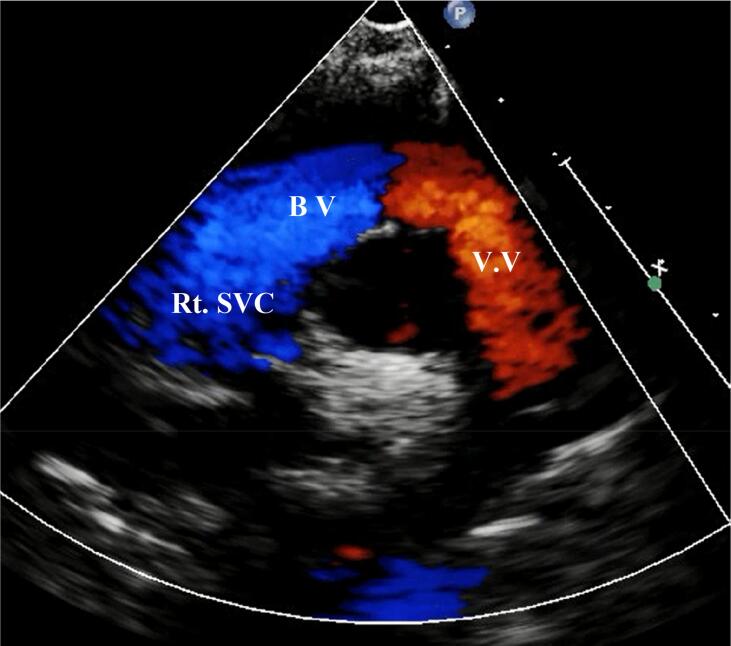
Fig. 2.
Suprasternal colour echocardiographic view showed left anomalous pulmonary vein with ascending vertical vein (VV), Bridging vein (BV) and right superior vena cava (Rt. SVC).
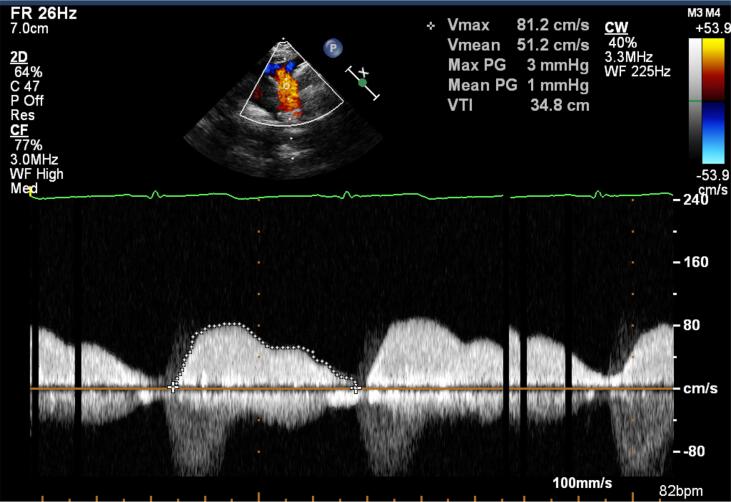
Fig. 3.
Suprasternal echocardiographic view showed non-obstructive anomalous pulmonary venous flow to ascending vertical vein, gradient mean of 1 mmHg.
4. Case 3
Sixteen-year-old boy diagnosed at the age of 9 months to have PAPVR of the left upper pulmonary vein through ascending vertical vein to the left innominate vein, small (ASD) secundum, dilated right ventricle and right atrium. The patient has disappeared from follow up till the age of 14 years. Then he showed up in the outpatient clinic and was admitted for diagnostic cardiac catheterization and possible PAPVR device closure. In cardiac catheterization laboratory the hemodynamic and angiographic data were obtained and were as follows: QP: QS was 2:1 and pulmonary artery pressure was 1/3rd systemic, left pulmonary artery angiograms with levophase showed anomalous drainage of left lung upper and middle lobes pulmonary veins through ascending vertical vein into a left innominate vein. Therefore, occlusion of vertical vein was carried out using vascular plug type-II 16 mm (St Jude Medical, Plymouth, MN). The patient remained stable and was discharged to home on the second day of the procedure after satisfactory echocardiographic findings. After discharge serial echocardiograms showed the device in a good position with no residual leaks and all the pulmonary veins are draining into the left atrium.
5. Case 4
Fourteen-year-old girl has repeated episode of palpitation. At the age of 2 years she underwent pediatric cardiac evaluation in a local hospital which revealed normal cardiac findings and rolled out any cardiac cause of arrhythmia. She had intermittent follow up elsewhere but she continued to have palpitations. At the age of 10 years, she was referred to our institution, where she underwent pediatric cardiac work up which included electrocardiography, Holter monitoring, review by pediatric cardiac electrophysiologist and echocardiography, which revealed PAPVR to the left innominate vein, dilated right ventricle and right atrium, mild mitral valve prolapse and mild mitral valve regurgitation. So, she underwent cardiac catheterization and occlusion of the ascending vertical vein using a vascular plug type-II 18 mm (St Jude Medical, Plymouth, MN). She was discharged to home after 24 h of observation in stable conditions after reassuring echocardiogram findings. Later serial echocardiograms showed device in a good position with no leak and good echocardiographic findings.
6. Case 5
A six-year-old girl with omitted diagnosis of PAPVR despite having a cardiac history of PDA device closure at the age of three years. Accidentally, during a follow up echocardiogram the PAPVR of the left upper pulmonary vein to the left innominate vein via ascending vertical vein was picked up. So, transcatheter closure of the ascending vertical vein was performed using vascular plug type-II 10 mm (Abbot Medical, Plymouth, MN). The patient was stable and the echocardiogram findings were satisfactory. So, she was discharged to home on the next day after the procedure in stable conditions. Echocardiographic follow up showed no residual leaks, the device in good position and all pulmonary veins drain to the left atrium.
7. Case 6
Eleven-year-old boy underwent coarctation repair and supra-mitral valve ring resection at the age of three years elsewhere. He was referred to our center for follow-up. He was found to have PAPVR of the left upper pulmonary vein to the left innominate vein with dilated right ventricle and right atrium. After routine work up he was taken to the catheterization laboratory, where the vertical vein was occluded using vascular plug-II 12 mm (Abbot Medical, Plymouth, MN). The patient was discharged to home after 24 h in stable condition with good echocardiographic findings. Follow up echocardiographic studies showed no residual leaks over the device, all pulmonary veins draining into the left atrium, no evidence of pulmonary hypertension.
8. Cardiac catheterization technique
All cardiac catheterization procedures performed under conscious sedation and local anesthesia using Lidocaine 1%. Right and left femoral venous accesses were obtained by 5F sheath. A 5F multipurpose (MPA2) catheter (Cordis Miami Lakes, USA) was advanced into the left pulmonary artery and the other 5F MPA2 catheter introduced into the left atrium over Terumo wire through right SVC, innominate vein (Fig. 4), blood gas samples were collected from SVC just above the left innominate vein, vertical vein, innominate vein, and pulmonary artery as well as from aorta, step-up (in cases of intact atrial septum) and shunt were calculated: (Qp: Qs) it was 2.8:1 (Table 1). Oxygen saturations were 98% in the vertical vein, 92% in the innominate vein and pulmonary artery, and 80% in high superior vena cava. Selective left pulmonary arteriograms with levophase were done showed left anomalous pulmonary veins joining to form a venous confluence that connected to the left atrium and a large vertical venous channel connected the confluence of anomalous pulmonary veins to the innominate vein (Fig. 5). After that right pulmonary arteriograms with levophase were done showed normal right pulmonary venous drainage to the left atrium. Vertical vein diameter ranged from 10 to 16 mm. Balloon wedge pressure catheter (Arrow International, Inc. USA) was introduced into the vertical vein, after occlusion of the vertical vein left pulmonary arteriograms with levophase were done showed unobstructed left pulmonary venous drainage to the left atrium with no holding up of die into the left upper pulmonary vein (LUPV) delineating that of dual drainage of an anomalous vein (Fig. 6). The vertical vein was occluded by different size Amplatzer vascular plug type-II 10–18 mm (St Jude Medical, Plymouth, MN), the device deployed using 8-10F Amplatzer long introducer sheath (AGA. Medical Plymouth, MN) (Table 1) with the proximal disc in the ascending vertical vain away from innominate vein, the device was released after re-confirming unobstructed pulmonary venous return to the left atrium (Fig. 7). The final left pulmonary artery and left innominate venograms showed a good position of the device (Fig. 8) with no residual leak. On late follow-up after two to six years echocardiogram showed no flow across the device, with good flow to the left atrium, and no evidence of pulmonary hypertension.
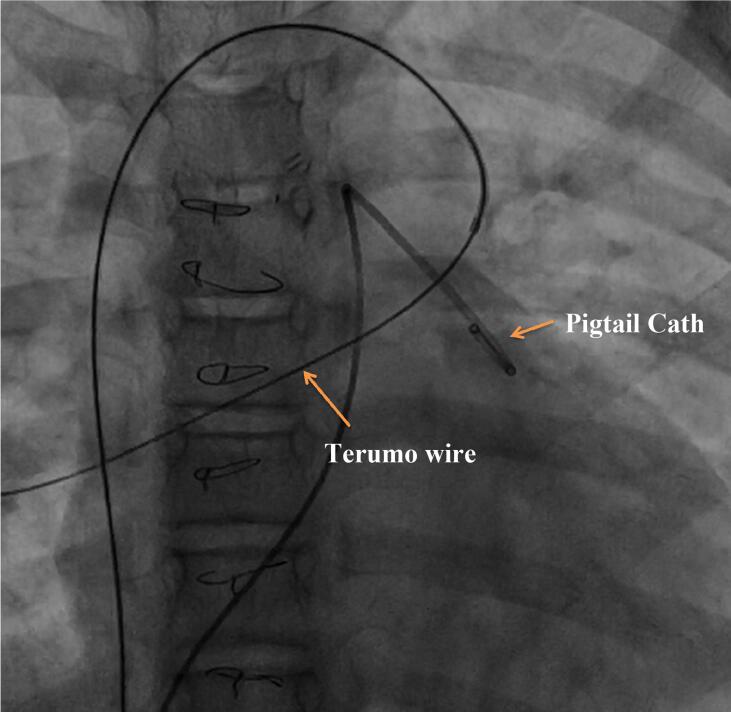
Fig. 4.
Anteroposterior fluoroscopic image showed the terumo wire advanced into multipurpose type-2 catheter through inferior vena cava to right superior vein cava, to bridging vein to ascending vertical vein to the left upper pulmonary vein to the left atrium indicating dual connection, pigtail catheter advanced into left pulmonary artery.
Table 1.
The table above showed age, type of device used, mean pulmonary artery pressure (mean PAP), anatomy and shunt (QP/QS).
| Age/year | device | Mean PAP mmHg |
Anatomy of PAPVR | QP/QS | |
|---|---|---|---|---|---|
| 1 | 6 | PDA occluder device-I 8/10 mm |
12 | Left upper pulmonary vein to left innominate vein | 1.5/1 |
| 2 | 7 | PDA occluder device-I 8/10 mm |
12 | Left upper pulmonary vein to left innominate vein | 1.3/1 |
| 3 | 16 | Vascular plug-II 16 mm |
13 | Left upper pulmonary vein to left innominate vein, ASDII | 2:1 |
| 4 | 14 | Vascular plug-II 18 mm |
12 | Left upper pulmonary vein to left innominate vein | 1.2/1 |
| 5 | 6 | Vascular plug-II 10 mm |
12 | Left upper pulmonary vein to left innominate vein | 1.2/1 |
| 6 | 11 | Vascular plug-II 12 mm |
12 | Left upper pulmonary vein to left innominate vein | 1.5/1 |
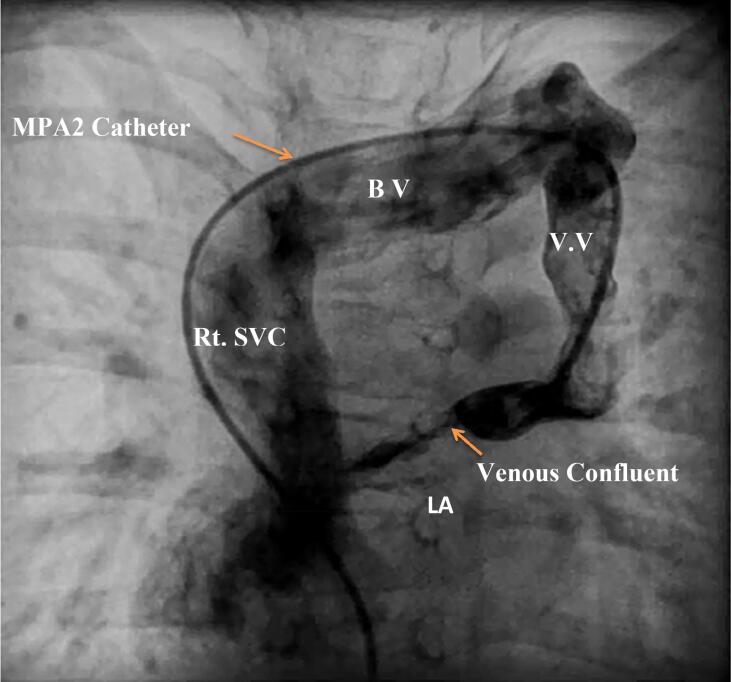
Fig. 5.
Anteroposterior angiographic image visualized contrast injected by multipurpose-2 with side hole (MPA2) venous catheter to the right upper pulmonary vein to the left atrium (LA) confirming dual connection. (Rt. SVC = right superior vena cava, BV = bridging vein, VV = vertical vein).
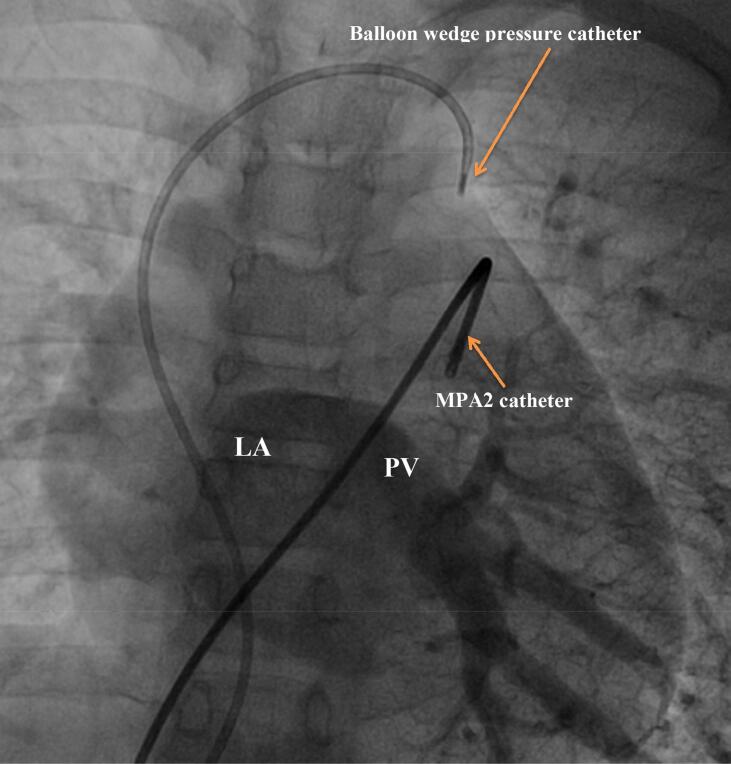
Fig. 6.
Anteroposterior angiograms view showed balloon wedge tipped catheter in the innominate vein and (Multipurpose catheter (MPA2) in the left pulmonary artery, all pulmonary veins (PV) draining into left atrium (LA).
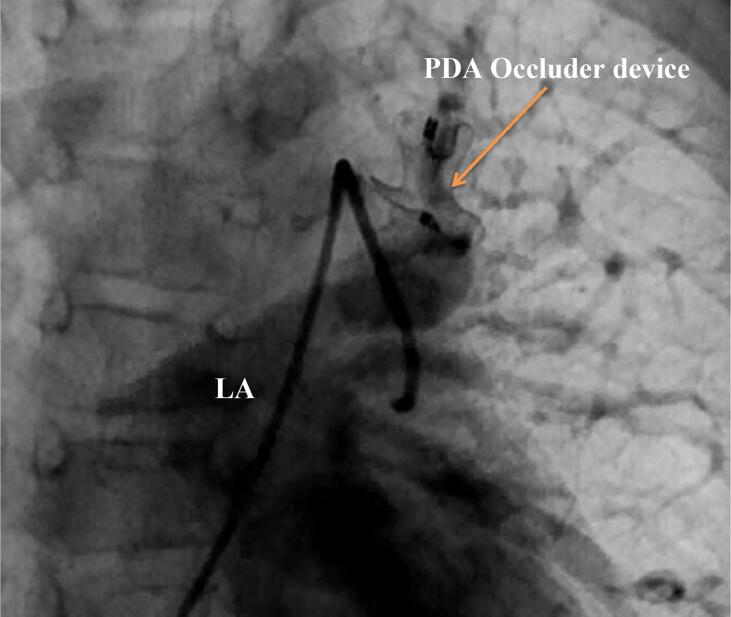
Fig. 7.
Left pulmonary artery angiograms in anteroposterior projection showed Amplatzer patent ductus arteriosus (PDA) occluder device deployed inside the ascending vertical vein, with no leak, unobstructed flow to the left atrium (LA).
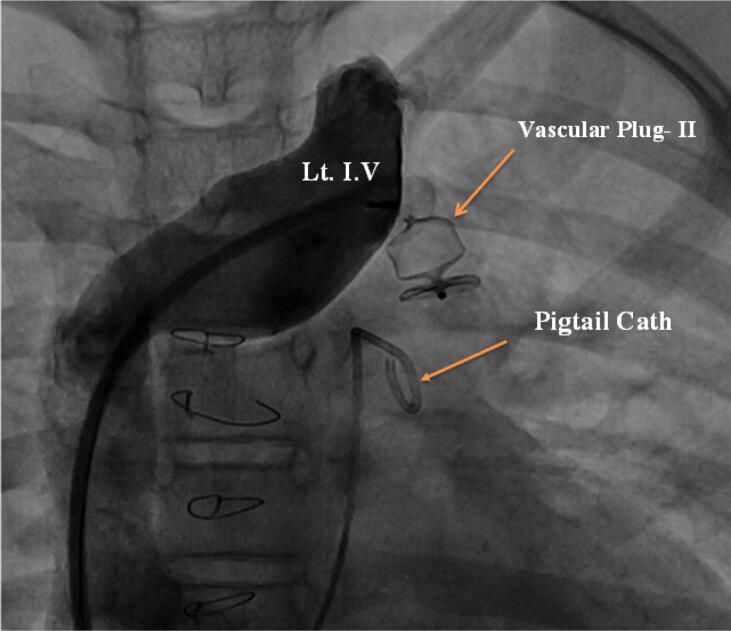
Fig. 8.
Anteroposterior angiographic view showed Amplatzer vascular plug type-II in ascending vertical vein, left innominate vein (Lt. I. V) angiograms showed no leak to vertical vein, with patent left innominate vein.
9. Discussion
The anomalous pulmonary venous drainage or connection occurs due to the failure of one or more pulmonary veins to connect to the left atrium during fetal life. Embryonic development of the pulmonary veins is a complicated process that takes place early in the development of the vascular system. The foremost theory of its development is that the initial drainage of pulmonary veins takes place via the splanchnic plexus into the cardinal and umbilical vitelline. Subsequently, a craniocaudal outpouching forms within the sinoatrial region of the heart extending to lung buds. As caudal regression occurs, the cranial portion develops into the common pulmonary vein, which becomes incorporated into the left atrial wall. The partial anomalous pulmonary venous drainage occurs due to failure of connection between the common pulmonary vein and the splanchnic plexus [1].
An anomalous pulmonary venous connection could be total or partial. PAPVR is a rare condition that can be found in 0.5–0.7% of the general population [2], [5]. The first description of PAPVR was by Winslow in 1739 [2]. In 2007 PAPVD was classified by Alsoufi into 5-types: right PAPVD to the SVC, right PAPVD to the right atrium, right PAPVR to the IVC, left PAPVD to left innominate vein via ascending vertical vein, and bilateral PAPVR, his classification didn’t include a dual pulmonary venous connection [3]. PAPVR is more frequently encountered on the right side and typically coexisted with sinus venosus ASD in 80–90% of the cases [2]. Right-sided anomalous pulmonary venous drainage into inferior vena cava (IVC) can be a component of Scimitar syndrome. Most patients with isolated PAPVR usually asymptomatic in early life and such anomaly can be missed in the neonatal period. The diagnosis is usually made in childhood or in adult age when the effect of the left to right shunt or signs of pulmonary hypertension appear. In 2020, Peirone et al. published a case report of a 43-years old woman post aortic coarctation repair at age of three years, later on, developed dyspnea and fatigue with exercise, associated with frequent palpitations. During work-up, she was found to have PAPVR of a right pulmonary vein with dual drainage. They closed the anomalous vein percutaneously using a vascular plug [4]. In 2019, Mehnaz et al., reported one case with aortic coarctation and PAPVR of the left pulmonary vein to the left innominate vein; he treated both the coarctation of the aorta and also the partial venous connection by transcatheter technique as a combined procedure [5]. In 2019, Gangadhara et al., published a case report of a 69-years old female with brain abscess and left side PAPVR with dual drainage to the VV and LA in which transcatheter occlusion was done using an 18 mm St. Jude Amplatzer Vascular Plug II [6]. In our series, all reported cases have left-sided PAPVR in which the anomalous veins are connected to the left innominate vein through an ascending vertical vein. All of the cases have dual drainage to the left innominate vein and left atrium. Our approach consisted of transcatheter occlusion of the ascending vertical vein, and redirecting the blood flow to the left atrium. The procedure was carried out under conscious sedation and local anesthesia. We did not encounter major complications, and all patients were discharged home after 24 h of the procedure. With such pathology since we started evaluating a patient for possible device closure, no patient was not a candidate for transcatheter closure, which indicate that most patient with PAPVR should go for evaluation and possible transcatheter device closure. We concluded that it was an acceptable practice not to send patients for surgery even if there are signs of right ventricle volume overload.
The limitations of our case series report lies in its small size due to narrow indication range as its feasible only in PAPVR with dual drainage and the relatively short follow-up period.
10. Conclusions
Transcatheter Amplatzer device closure of PAPVR with dual drainage is an effective, safe and reproducible approach. It offers many advantages over surgical treatment such as fast recovery, avoidance of mechanical ventilation and PCICU stay, short in-hospital stay, low cost and more patient satisfaction.
In our series, it has been demonstrated that this approach showed appealing results, however larger scale studies and more follow-up periods are required to consolidate these findings.
Declaration of Competing Interest
The authors report no relationships that could be construed as a conflict of interest.
Acknowledgement
None.
References
- 1.Christos Tourmousoglou, Christina Kalogeropoulou, Efstratios Koletsis, Nikolaos Charoulis, Christos Prokakis, Panagiotis Alexopoulos, Emmanoil Margaritis, and Dimitrios Dougenis, Hindawi Publishing Corporation. Right Upper Lobe Partial Anomalous Pulmonary. Venous Connection, case report, Vasc. Med. Vol. 2014, Article ID 249896, 3 pages. [DOI] [PMC free article] [PubMed]
- 2.Karim El-Kersh, Elie Homsy, Curt. Daniels, Shaun Smith, Partial anomalous pulmonary venous return: A case series with management approach, j.rmcr.27 (2019).100833. [DOI] [PMC free article] [PubMed]
- 3.Alsoufi Bahaaldin, Cai Sally, Van Arsdell Glen S., Williams William G., Caldarone Christopher A., Coles John G. Outcomes after surgical treatment of children with partial anomalous pulmonary venous connection. Ann. Thorac. Surg. 2007;84:2020–2026. doi: 10.1016/j.athoracsur.2007.05.046. [DOI] [PubMed] [Google Scholar]
- 4.Alejandro R. Peirone, Alejandro E. Contreras, Carolina Carrizo, Mailén Konicoff and Raúl O. Cayre, Percutaneous occlusion of right partial anomalous pulmonary venous connection with dual drainage to the innominate vein and the left atrium: a unique anatomical finding, DOI: 10.32604/CHD.2020.013199.
- 5.Atiq Mehnaz, Younis Muhammad Kamran, Amanullah Muneer, Transcatheter treatment of coarctation of aorta and dually connected anomalous vertical pulmonary vein as a combined procedure, DOI: 10.26717/BJSTR.2019.19.003372.
- 6.Gangadhara Madhu Bangalore, Magee Alan G., Magee Alan G. Transcatheter occlusion of partial anomalous pulmonary venous connection with dual drainage to left atrium. Ann. Pediatr. Card. 2019;12(2):144. doi: 10.4103/apc.APC_72_18. [DOI] [PMC free article] [PubMed] [Google Scholar]